This issue of the Journal features the results of a prospective sentinel surveillance for Haemophilus influenzae B (Hib) meningitis1. The National Technical Advisory Group on Immunization (NTAGI) in its meeting of August 26, 2010 recommended that pentavalent vaccine containing Hib be introduced in the States of Kerala and Tamil Nadu2. Since there was concern about its adverse effects (AEFI), this was to be monitored in the two States. Further roll-out to other States was to be based on the impact assessment after one year. The NTAGI suggested the Indian Council of Medical Research (ICMR), New Delhi, to prepare a protocol for the surveillance of Hib meningitis in selected hospitals to understand the trends over time2. The data in the issue represent the first of these surveillance reports1.
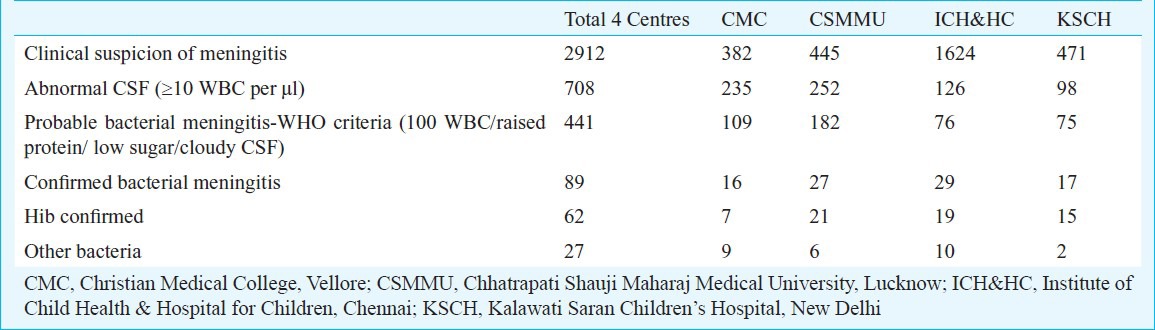
Four centres, two in Tamil Nadu (ICH&HC, Chennai and CMC, Vellore), one from Uttar Pradesh (CSMMU, Lucknow) and one in Delhi (KSCH) participated. The four centres followed different protocols. The latex agglutination test (LAT) was employed to detect antigens and identify the causative organism. During the surveillance period 2912 children under 2 yr of age with suspected meningitis, were enrolled in the four centres and 62 were found to have Hib meningitis. The break-up of incidence at each centre (not reported in the paper) was provided by the authors (Table I). They do not total up accurately but is useful to get the overall picture.
Table I.
Break-up of patients enrolled in the study and with Hib meningitis
Comparison with IBIS Study
The low incidence of Hib meningitis (62 cases) seen in these four centres over the study period, is reminiscent of the results of the invasive bacterial infection surveillance (IBIS) study conducted over four years in six hospitals between 1993 and 1997 where only 125 cases of Hib were identified3. The present study, done two decades later employing sensitive tools like LAT for Hib antigen detection, validates the findings of the IBIS study, which depended mostly on culture techniques.
Exaggeration of disease burden
The authors state in the abstract that the cases of probable meningitis caused by Hib were 58 per cent lower at Vellore. This is misleading as it exaggerates the problem of Hib meningitis. Using the definitions employed by the authors, there were 441 children with ‘probable bacterial meningitis’. There were 60 cases of Hib meningitis among them. Hib was found in only 13.6 per cent of the cases with probable meningitis. Two additional cases were detected in children with abnormal CSF but not fulfilling the CSF criteria for ‘probable bacterial meningitis’. On the whole, 62 cases of Hib meningitis were detected among 708 patients with abnormal CSF. Hib antigen was detected only in 8.75 per cent of patients with an abnormal CSF cytology. The mortality from Hib meningitis was 11 per cent1.
This information is important for estimating the burden of Hib meningitis and the benefits of vaccination. There are at least two previous attempts to estimates of the burden of the disease in the country. The Core Committee on Immunization has estimated that there are 52,000 new cases of Hib meningitis in the country each year4. This estimate was made projecting data from a surveillance study done in a district of Kerala between July 1999 and June 20015. The surveillance involved collection of reports of clinical disease from within the district - with or without laboratory confirmation. The authors assumed that about one third of the cases of clinical meningitis were pyogenic meningitis and the Core Committee assumed that one third of the cases of pyogenic meningitis were caused by Hib. In the first year of this surveillance there were 75 cases of suspected meningitis and it was presumed by the authors5 that 27 would be due to pyogenic meningitis and the Core Committee4 assumed that nine of them must have been due to Hib. Thus about 12 per cent of clinical meningitis was presumed to be due to Hib by the Core Committee. In the next year of surveillance, there were only 23 cases of clinical meningitis and it was presumed that there were nine cases of pyogenic meningitis and three cases of Hib meningitis5. The Core Committee selected the first year of surveillance (when there were 9 cases of presumed Hib meningitis), to make its nationwide projection of 52,000 cases. No justification was provided as to why the data from the next year (when there were only 3 cases of Hib) were not used4. In the present study1, 62 cases of Hib were found among 2912 children with clinically suspected meningitis and it represents 2.1 per cent of the clinically suspected cases (not 12% as used in the Kerala projection).
Minz et al6 performed meticulous surveillance in a population of 6.5 lac persons, over a two year period (1997 to 1999). The study involved house-to-house visits every 2 wk. They found the incidence of Hib meningitis as 7 per 100,000 children under 5. In real terms, if the year's birth cohort of about 25 million is vaccinated against Hib, nation-wide it will prevent 1750 cases of Hib meningitis and would save less than 200 lives (11% mortality). After the short term subsidies provided by the Global Alliance for Vaccines and Immunization (GAVI) are withdrawn, vaccinating the birth cohort of 25 million with a pentavalent vaccine that costs  525/child (3 doses)7 would entail an expenditure of
525/child (3 doses)7 would entail an expenditure of  1300 crores. This is more than the entire immunization budget for 2011-2012 (of
1300 crores. This is more than the entire immunization budget for 2011-2012 (of  1200 crores)8. After five years of the Programme vaccinating each birth cohort (with 125 million children vaccinated), 8750 cases of Hib meningitis and 962 deaths will be prevented yearly. The evidence from the present study1 and that from the Minz study6 will enable the Core Committee to revise its projection of Hib meningitis in the country.
1200 crores)8. After five years of the Programme vaccinating each birth cohort (with 125 million children vaccinated), 8750 cases of Hib meningitis and 962 deaths will be prevented yearly. The evidence from the present study1 and that from the Minz study6 will enable the Core Committee to revise its projection of Hib meningitis in the country.
Inappropriate use of LAT for detection of other organisms
In the present surveillance1, the organism was identified by LAT in 84 of 89 samples. However, LAT is not uniformly sensitive in detecting all organisms. It is positive in 93 per cent of H. influenzae type b infections but only in 60 per cent of Streptococcus pneumoniae and 39 per cent of Neisseria meningitides9. Therefore, while LAT can identify most cases of Hib, because of its lower sensitivity for other organisms, it is not very useful to examine the relative incidence of different bacteria.
Over-interpretation of benefits of vaccination
In the study reported here1, in Vellore 7 of the 16 cases of bacterial meningitis where a pathogen was identified, were due to Hib (44% Hib) compared to 55 out of 73 in the other centers (75% Hib) (P<0.05). The authors utilized these differences in proportions, to build up a hypothesis that the ‘lower proportion’ of Hib in Vellore was due to the herd effect of 41 per cent coverage with Hib vaccine (compared to the other centres where only 1 to 8 per cent had received even 1 dose of Hib)1. This conclusion is perhaps not entirely justified. The study reported that maternal educational levels were higher, the proportion of children with severely malnourished were significantly lower and the immunization coverage was higher in Tamil Nadu as compared to other sites. These factors could be contributing to better background immunity of the children there, as compared to other sites and hence the observed lower incidence of Hib could be due to these background differences. Further, as indicated by the authors, one of the seven confirmed Hib cases in Vellore was vaccinated. These factors themselves could be giving better background immunity to the children there, as compared to other sites and hence the observed lower incidence of Hib could be due to these background differences. Assuming that 41 per cent of the total number of children with suspected meningitis (382) is vaccinated against Hib, the probable picture in Vellore is shown in Table II.
Table II.
History of Hib immunization in the group studied at Vellore
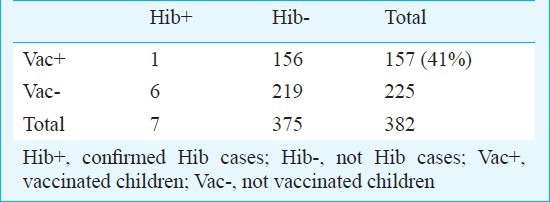
The odds of Hib disease with vaccination is 23 per cent of those without vaccination, this may be promising. However, the exact probability of this is 0.25 which is statistically not significant. In view of this, it is too early to conclude that vaccine has prevented a sizable incidence of Hib. At best it can be an early indicator of the effect that needs to be confirmed with larger numbers and with more in-depth analysis.
One major limitation at this stage is that we do not know the background incidence of Hib in Vellore before vaccination. Just comparing present incidence in Vellore with other regions which happened to be without vaccination could be misleading as these areas could had a higher incidence of Hib than in Vellore from the beginning itself. A better indicator would be reduction in Hib incidence comparing pre- and post-vaccination periods in the same region.
Conflicts of interest
One of the authors of the present surveillance study has reported possible conflicts of interest. Als-Nielsen and colleagues10 showed that when the authors of an article were associated with for-profit organizations, it had little impact on the results or data reported but it influenced the interpretation of the results and the conclusions drawn. The fact that the data are not impacted by conflicts of interest provides persuasive reason to publish the figures from large trials such as this, regardless of the declared conflicts of interests. Publication allows data to be put out in the public domain. It can be interpreted by the scientific community, separately from the interpretations of the authors. Discerning readers and decision makers can use the data provided for health policy, based on sound cost–benefit calculations.
References
- 1.Ramachandran P, Fitzwater SP, Aneja S, Verghese VP, Kumar V, Krishnamoorthy N, et al. for Bacterial Meningitis Surveillance Working Group. Prospective multi-centre sentinel surveillance for Haemophilus influenzae type b & other bacterial meningitis in Indian children. Indian J Med Res. 2013;137:712–20. [PMC free article] [PubMed] [Google Scholar]
- 2.Delhi: 2010. Aug, [accessed on April 4, 2013]. Government of India. Minutes of Meeting of National Technical Advisory Group on Immunization 26th August 2010, R. No. 155A, Nirman Bhawan [Internet] Available from: http://jacob.puliyel.com/#paper_293 . [Google Scholar]
- 3.Invasive Bacterial Infections Surveillance (IBIS) Group of the International Clinical Epidemiology Network. Are Haemophilus influenzae infections a significant problem in India? A prospective study and review. Clin Infect Dis. 2002;34:949–57. doi: 10.1086/339327. [DOI] [PubMed] [Google Scholar]
- 4.Government of India. Minutes of the meeting of the Core Committee on Vaccines [Internet] [accessed on April 4, 2013]. Available from: http://jacob.puliyel.com/#paper_288 .
- 5.John TJ, Rajappan K, Arjunan KK. Communicable diseases monitored by disease surveillance in Kottayam district, Kerala state, India. Indian J Med Res. 2004;120:86–93. [PubMed] [Google Scholar]
- 6.Minz S, Balraj V, Lalitha MK, Murali N, Cherian T, Manoharan G, et al. Incidence of Haemophilus influenzae type b meningitis in India. Indian J Med Res. 2008;128:57–64. [PubMed] [Google Scholar]
- 7.Panacea to cut pentavalent vaccine price. The Hindu Business Line. [accessed on November 10, 2012]. Available from: http://www.thehindubusinessline.com/companies/panacea-to-cut-pentavalent-vaccine-price/article2081435.ece .
- 8.Bhadoria V, Gobinath A, Mitra P, Narayan M. Mumbai: McKinsey & Company; 2012. [accessed on April 4, 2013]. Transforming India's vaccine market; Saving lives, creating value. Available from: http://www.mckinsey.com/client_service/pharmaceuticals_and_medical_products/people/%7E/media/mckinsey/dotcom/client_service/pharma%20and%20medical%20products/pmp%20new/pdfs/transforming_indias_vaccines_market.ashx . [Google Scholar]
- 9.Finlay FO, Witherow H, Rudd PT. Latex agglutination testing in bacterial meningitis. Arch Dis Child. 1995;73:160–1. doi: 10.1136/adc.73.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Als-Nielsen B, Chen W, Gluud C, Kjaergard LL. Association of funding and conclusions in randomized drug trials: a reflection of treatment effect or adverse events? JAMA. 2003;290:921–8. doi: 10.1001/jama.290.7.921. [DOI] [PubMed] [Google Scholar]


