Abstract
Background & objectives:
A substance dependent person in the family affects almost all aspects of family life. This leads to problems, difficulties or adverse events which impact the lives of family members and causes enormous burden on family caregivers. The present study aimed to assess the pattern of burden borne by the family caregivers of men with alcohol and opioid dependence.
Methods:
A cross-sectional study was conducted with ICD-10 diagnosed substance dependence subjects and their family caregivers attending a de-addiction centre at a multispecialty teaching hospital in north India. Family Burden Interview Schedule was used to assess the pattern of burden borne by the family caregivers of 120 men with alcohol and/or opioid dependence.
Results:
Compared to opioid and alcohol+opioid dependence groups, more often the alcohol dependence group was older, married, currently working, having a higher income and with the wife as a caregiver. Family burden was moderate or severe in 95-100 per cent cases in all three groups and more for ‘disruption of family routine’, ‘financial burden’, ‘disruption of family interactions’ and ‘disruption of family leisure’. Family burden was associated with low income and rural location. It was associated neither with age, education or duration of dependence of the patients, nor with family size, type of caregiver or caregiver's education and occupation.
Interpretation & conclusions:
Almost all (95-100%) caregivers reported a moderate or severe burden, which indicates the gravity of the situation and the need for further work in this area.
Keywords: Family burden, subjective and objective burden, substance dependence
Family is the key resource in the care of patients including those with mental illness in India. This has been attributed to the Indian tradition of inter-dependence, and the concern of close relatives in adversity, as also to the paucity of mental health professionals1. The family caregivers are those who provide care to other family members who need supervision or assistance in illness or disability2 or those who provide unpaid care to the family members with special needs3.
An illness adversely affects the individual as well as those around in terms of physical, emotional, and financial distress, and social and occupational dysfunction. This leads to problems, difficulties or adverse events which impact the lives of the significant others. This adverse impact has been described as burden4. Burden is said to be largely determined by family environment in terms of coping styles of different family members and their tolerance of the patients’ aberrant behaviour5.
Even though substance abuse is well recognized as a complex biopsychosocial phenomenon, substance dependence is considered as a ‘family disease’6. A substance dependent person in the family affects almost all aspects of family life, e.g., interpersonal and social relationships, leisure time activities, and finances. Substance dependence invariably increases conflicts, negatively affects family members, and burdens the families. The psychological and behavioural impact on others is often far greater than on the substance dependent family member. Yet, because of the historical emphasis on substance dependence as an individual's problem, the study of family's problems has been relatively neglected. Consequently, systematic research on substance dependence related burden among the family members is very limited.
Traditionally the research on families with substance dependent members has examined the family and the family process almost exclusively as an aetiological entity that affects the subject's substance use7. The burden is more often related to disruptive activities of the substance dependent person, and financial difficulties due to loss of income and/or diversion of funds to substance dependence8. The families of alcoholics, specially the spouses, have increased risk of stressful life events, medical and psychiatric disorders, and greater use of medical care services9,10,11,12,13.
An earlier study14 from India compared families of 30 subjects each with alcohol dependence, opioid dependence, and schizophrenia. The burden was assessed by the Family Burden Interview Schedule (FBIS)15. Moderately-severe objective, subjective, and different domain burden were reported for alcohol dependence, opioid dependence and schizophrenia groups14. Another study from India16 used FBIS to assess burden in wives of men with opioid dependence syndrome. The patients were aged 31-40 yr, urban, and educated below 12th standard. Severe burden was reported more often than moderate burden on both subjective and objective assessment16. A study from Nepal compared FBIS assessed family burden in 30 subjects each with intravenous drug use and alcohol dependence; the overall burden was higher with the former, and compared to other family caregivers, the spouses were more tolerant and reported a lower perceived burden17.
Alcohol and opioids being the commonest substances for treatment seeking in India18, the present investigation aimed to study the pattern of burden borne by the family caregivers of men seeking treatment for alcohol or/and opioid dependence in a de-addiction centre in north India.
Material & Methods
This study was conducted at the Drug De-addiction and Treatment Centre, Department of Psychiatry, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh - a multispecialty teaching hospital providing services to a major area of north India. Most patients come by family or self referral, and some are referred from other hospitals or other departments of our Institute. The services are run by a team of psychiatrists, social workers, clinical psychologists, and nurses. The services include outpatient, inpatient, basic laboratory, active and passive aftercare/follow up, and liaison with governmental and non-governmental agencies and self-help groups. The assessments include comprehensive physical and psychosocial evaluation, including for physical and psychiatric comorbidities. The treatment modalities used include pharmacotherapy, psycho-behavioural therapies, and social-occupational rehabilitation.
The study protocol was approved by the institutional research ethics committee. The data collection was done from January 1 to August 30, 2010. A cross-sectional design was used. The sample of convenience was recruited from the outpatient service. A written informed consent was obtained from both the patients and the caregivers included the study.
The primary sample consisted of the care giving family members of the patients seeking treatment for substance dependence. The family members accompanying the patients were included in the study if they were living together with the patients and were involved in their care indirectly in terms of general life care (sharing kitchen, expenses, social relations and obligation, and household chores including the care of children, aged, and the sick family members), and directly in terms of his substance dependence and its treatment related assistance or supervision for >1 year. The >1 year cut-off for caring was taken for the sake of comparability as majority of studies from India have used this cut-off19,20,21,22. In case of more than one family caregiver being available, the caregiver selected for the study was the one staying together longer and being involved in the care more, as agreed by a consensus among the patient, caregivers and the treating clinician. The caregivers were aged >18 yr, of either gender, and healthy by general clinical assessment.
The patients were males, aged >18 yr, with alcohol, opioid, and alcohol+opioid dependence (40 for each group, total 120) diagnosed as per ICD-1023. Most of them (100 subjects) were on medications for withdrawal management (chlordiazepoxide/lorazepam for alcohol dependence, clonidine-NSAID-nitrazepam combinations for opiate dependence), while others (20 subjects) were on anti-craving medications or deterrent agent (naltrexone for opiates, and disulfiram, acamprosate, topiramate, or naltrexone for alcohol). The patients and caregivers were excluded from the study if they had any major debilitating physical illness, organic brain syndrome, or mental retardation.
Relevant demographic and clinical data for the caregivers and the patients were collected from the patients, caregivers and the case notes as appropriate. The selected family caregivers were assessed on family burden interview schedule (FBIS)15. FBIS is a semi-structured interview schedule that covers six areas: Financial burden, Disruption of family routine activities, Disruption of family leisure, Disruption of family interaction, Effect on physical health of others and Effect on mental health of others. It has 24 items, each rated on a 3-point scale (mild, moderate, severe). Inter-rater reliability for all items is 0.78 and the correlational validity is 0.72. One question to assess the global subjective burden is also included. The contrast between objective and subjective burden reflects the fact that many relatives may be more or less tolerant and may under- or over-play their problems. The scale has been widely used in India with the families of patients with mental retardation, chronic physical, alcohol use, and schizophrenic, affective, and neurotic disorders19,20,21,22.
Statistical analysis: The data were analyzed using SPSS version 14.0 for Windows (Chicago, Illinois, USA). Descriptive data were analyzed by frequency, percentage, mean, standard deviation, ANOVA and post-hoc analysis with Bonferroni's correction. The substance groups as well as moderate vs. severe burden groups were compared for demographic and clinical variables, with the continuous normally distributed variables by independent t test, and the discrete variables by chi-square test. Binomial logistic regression analysis was used to find out the predictors of severe objective or subjective family burden.
Results
Patients
Demography: Compared to the opioid dependence and alcohol+opioid dependence groups, the alcohol dependence group was older (44.72 ± 8.95 yr vs. 28.12 ± 7.06 and 32.15 ± 9.13 yr, respectively, P<0.01), was more often working (82.5 vs. 47.5 and 37.5, respectively, P<0.01), with income of  >6000 per month (67.5 vs. 15 and 27.5%, respectively, P<0.001), and less often with no income (12.5 vs. 55 and 67.5%, respectively, P<0.001), and was mostly married (95 vs. 47.5 and 62.5%, respectively, P<0.01). The three groups were comparable for education, religion, family type, family size and rural-urban location (Table I). On Post-hoc analysis with Bonferroni’ correction, patients with alcohol dependence were significantly older than in opioid dependence group (44.72 ± 8.95 vs. 28.12 ± 7.06 yr, P<0.001), and alcohol+opioid dependence group (44.72 ± 8.95 vs. 32.15 ± 9.13 yr, P<0.001).
>6000 per month (67.5 vs. 15 and 27.5%, respectively, P<0.001), and less often with no income (12.5 vs. 55 and 67.5%, respectively, P<0.001), and was mostly married (95 vs. 47.5 and 62.5%, respectively, P<0.01). The three groups were comparable for education, religion, family type, family size and rural-urban location (Table I). On Post-hoc analysis with Bonferroni’ correction, patients with alcohol dependence were significantly older than in opioid dependence group (44.72 ± 8.95 vs. 28.12 ± 7.06 yr, P<0.001), and alcohol+opioid dependence group (44.72 ± 8.95 vs. 32.15 ± 9.13 yr, P<0.001).
Table I.
Socio-demographic and clinical profile of patients
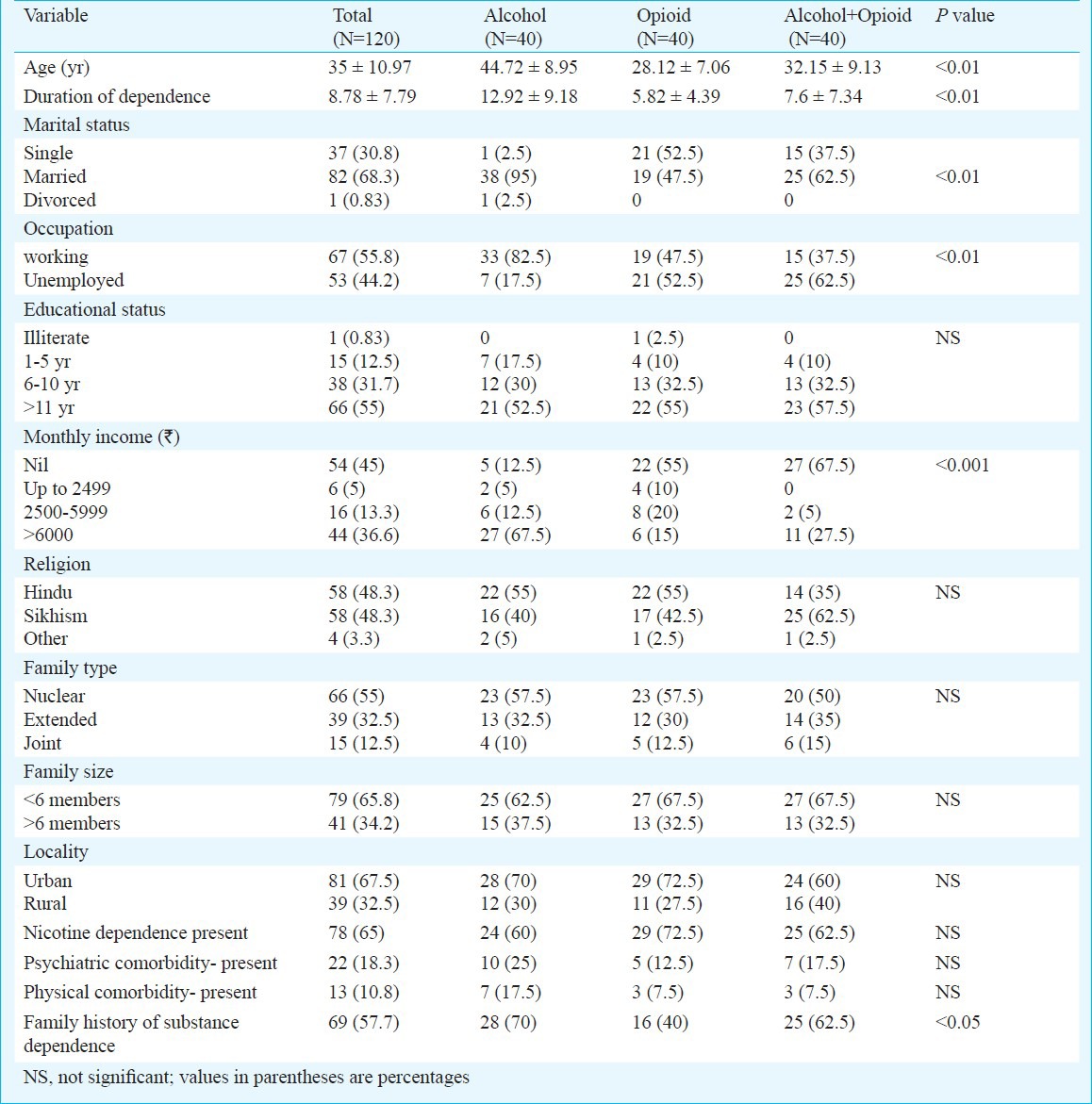
Clinical profile: Compared to the opioid dependence and alcohol+opioid dependence groups, the alcohol dependence group had a significantly longer duration of substance dependence (P<0.01). The duration of dependence was >5 yr in 64.2 per cent patients; more in alcohol dependence group than in opioid dependence and alcohol+opioid dependence groups (75 vs. 60 and 57.5%, respectively). Comorbid nicotine dependence was present in 65 per cent patients; more in opioid dependence group than in alcohol dependence and alcohol+opioid dependence groups (Table I). On Post-hoc analysis with Bonferroni’ correction, patients with alcohol dependence had longer duration of dependence than opioid dependence group (12.92 ± 9.18 vs. 5.82 ± 4.39 yr, P<0.001), and alcohol+opioid dependence group (12.92 ± 9.18 vs. 7.6 ± 7.34 yr, P=0.004).
Psychiatric comorbidity was present in 17.5 per cent patients; more in alcohol dependence group than in opioid dependence and alcohol+opioid dependence groups; and included psychosis (N=6), depression (N=5), bipolar and anxiety disorder (N=4 each), and personality disorder (N=2). Physical comorbidity was present in 10.8 per cent patients; more in alcohol dependence group (17.5%) than in opioid dependence and alcohol+opioid dependence groups (7.5% each); and included seizure disorder (N=9), gout, hepatitis and alcoholic liver disease (N=2 each), and diabetes mellitus, pulmonary tuberculosis and hypertension (1 each). Family history of substance dependence was present in 57.5 per cent; more in alcohol dependence and alcohol+opioid dependence groups than in opioid dependence group (P<0.05) (Table I).
Caregivers
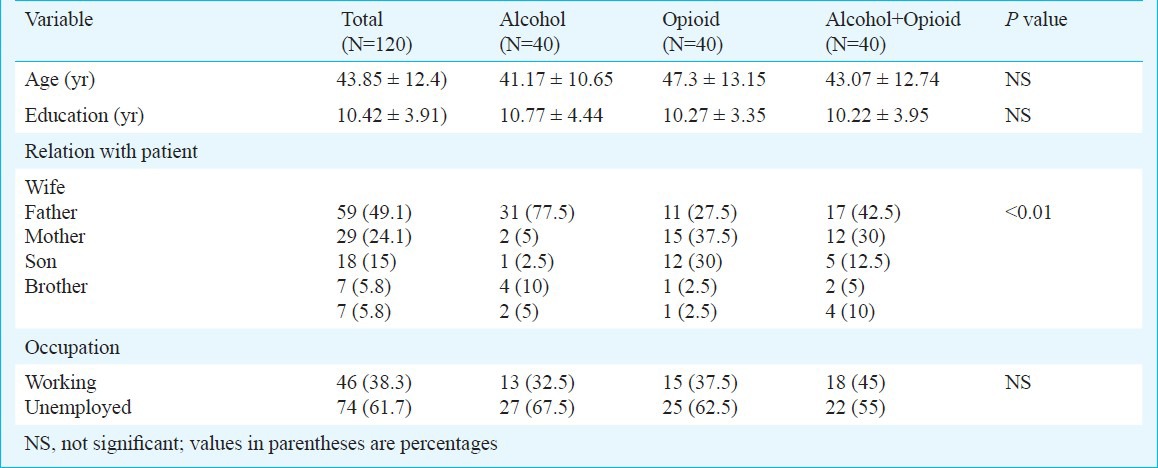
Demography - Mean age and education of caregivers were 43.8 ± 12.4 and 10.42 ± 3.91 yr, respectively. Compared to the opioid dependence and alcohol+opioid dependence groups, the alcohol dependence group had higher proportion of caregiver being the wife (P<0.01). The family caregivers of the three substance dependence groups were comparable for age, education and occupation (Table II).
Table II.
Demographic profile of caregivers
Burden - Across the three groups, the global severity of care giver's objective and subjective burden was broadly similar, and reported as either moderate (52.5%) or severe (45.8%) and rarely as absent (1.7%). For the different areas of burden under consideration, the profile of severity was similar across the three groups; except for disruption of family leisure being reported as severe more often in alcohol+opioid dependence group than in alcohol dependence or opioid dependence groups (17.5 vs. 2.5% in other groups) (P=0.01) (Table III).
Table III.
Family burden
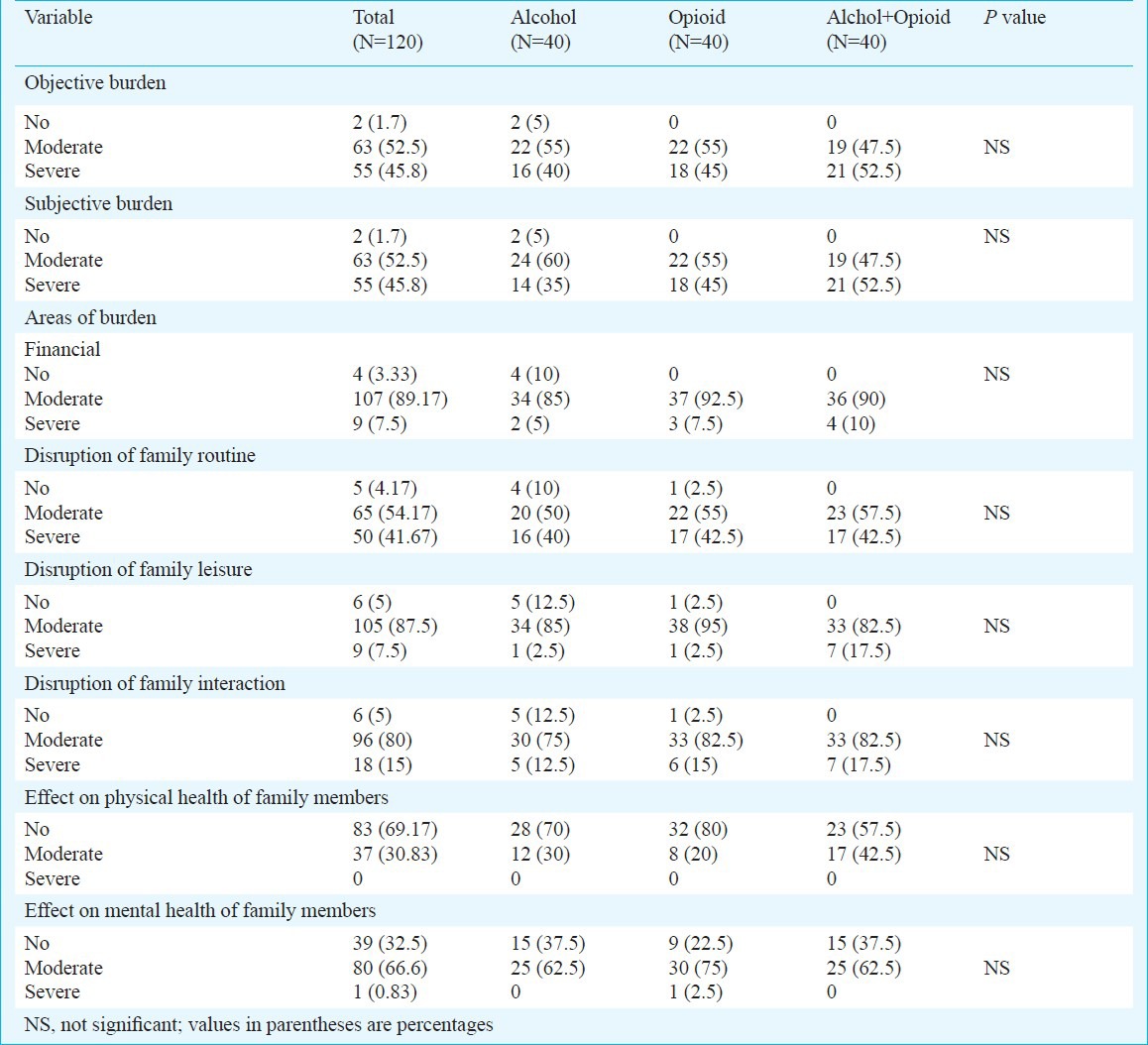
In terms of burden severity scores, the scores were comparable across the three groups except for the areas of ‘disruption of family leisure’ and ‘effect on physical health of family members’ for which alcohol+opioids dependence group had higher scores (P<0.05). For objective and subjective burden the differences were not significant for the duration of substance dependence of <5 vs. >5 yr and as reported by wives vs. other caregivers.
On comparing the demographic and clinical variables of subjects (N=120) with severe vs moderate subjective or objective burden, higher proportion of rural subjects reported severe subjective burden (61.53 vs. 39.24%, P<0.05) compared to urban subjects. When similar comparison was made for various areas of burden, significantly higher burden was seen in unemployed subjects in the areas of financial burden (13.20 vs. 2.98, P<0.05), disruption of family routine (54.71 vs. 31.34%, P<0.05) and disruption of family interaction (20.75 vs. 10.44%, P<0.05) compared to employed subjects. Higher proportion of rural subjects reported moderate-severe burden in the effect on physical health of family members (42.59 vs. 24.62%, P=0.05) compared to urban subjects.
Simple binary logistic regression analysis with enter method was used to study the relationship among independent variables (demographic and clinical variables) which were more frequently present in subjects with severe burden. Living in rural locality was the only significant predictor of severe subjective burden with odds ratio of 2.47 (CI=1.12-5.44, P<0.05). Other parameters like marital status, occupation (employed or unemployed), family type, duration of dependence, presence of psychiatric or physical comorbidity and family history were not found to be predicting severe subjective burden.
Discussion
Substance abuse impacts the functioning of the family and the society, and the families of substance abusers experience considerable burden of care. The study of family burden in substance dependence assumes importance because the profile of the associated factors can both influence the outcome of the problem, and be useful in designing and planning interventions to help the families cope with substance dependence.
The traditional family in India is the joint family. It is a group with several family subunits living in separate rooms of the same house24. Substance abuse related family burden is important for India and other developing countries because joint family is a more common pattern. Also, it assumes greater relevance because of the needed emphasis on developing community mental health services under the primary health care and community participation25. The aim is to focus not only on the treatment of the patients, but also to meet the needs of the caregivers. Similar approach has been used successfully in other psychiatric disorders, especially schizophrenia26.
The demographic and clinical profile of our sample was generally similar to that reported in earlier studies from our centre14,27. However, compared to a study from another centre in north India16, our opioid dependence group being more educated, and more unemployed; and fewer urban subjects in our study, could be the effect of the other centre being located in a metropolis. In contrast, our alcohol dependence group was similar to a study from Nepal17 with more of urban subjects and more wives as caregiver.
Given that all our patients were staying with their families, it was not unexpected to find ‘disruption of family routine’, ‘interactions’ or ‘leisure’ as the common areas of burden. It is well recognized that the maximum impact of a psychiatric disorder is borne by the family and often leads to a complete disruption in its functioning8. Also, our finding of the most commonly reported burden being financial is understandable as well. Globally, psychiatric illness in general and substance abuse in particular are costly disorders to have. For substance abuse in particular a lot of money is spent on procuring and using the substances and living through the consequences like accidents and crime, and seeking treatment in terms of travelling to treatment centers, paying for healers - including faith healers, and buying medications and services8.
In our study higher objective and subjective burden was found in low income and rural subjects. Rural location invariably reduces work and income opportunities. The low income group was more burdened in terms of finances, disruption of family routine and family interaction, as well as mental health of family members. Higher disruption of family interaction was seen in singles while significant disruption of family leisure was seen in subjects in opioid groups and in extended families. Higher disruption of family interaction might be a common factor for both the subject remaining single as also his family caregiver perceiving greater burden. Rural subjects staying in extended families with higher family history/risk of substance dependence reflects a combined effect of family environment and its impact on health of the family members.
We found more disruption of family leisure in singles in comparison to the earlier study from our centre that reported married subjects to be more burdened especially for domains of finance, disruption of family routine, effects on mental and physical health14. That study also reported higher burden being associated with severe dependence while such an association was not determined in the present study. Also, that study reported the rural population to be more burdened for financial domain, and disruption of family leisure was reported more in married, elderly and female caregivers14.
Our study had several limitations. The sample size was small and recruited from a tertiary care centre; hence the findings could not be generalized to other treatment centres. As per our centre's usual client profile all patients were men. Assessments of burden were cross-sectional and non-blind, and all information was obtained from a single family caregiver. Assessment of subjective burden was global, and several mediators such as coping, appraisal, expressed emotions and social support were not assessed. Future research should be conducted in a large sample with prospective design, to further study the exact effects of substance and other mediators such as family type, coping and social support on the family burden.
In conclusion, our study showed that substance dependence was associated with substantial burden for the family members, more for subjective and objective burdens in rural location with low income, and more for alcohol+opioid dependence group followed by opioid dependence group. These findings may suggest directions for future research in this area.
References
- 1.Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry. 2010;52:113–26. doi: 10.4103/0019-5545.64582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Family caregiver. Medical Condition Dictionary. 2010-2011. [accessed on August 16, 2011]. Available from: http://medconditions.net/familycaregiver.html .
- 3.Caregiving in the U.S. (2009) [accessed on August 16, 2011]. Available from: http://www.caregiving.org/.../Caregiving _in_the_US_2009_full_report.pdf .
- 4.Platt S. Measuring the burden of psychiatric illness on the family: an evaluation of some rating scales. Psychol Med. 1985;15:383–94. doi: 10.1017/s0033291700023680. [DOI] [PubMed] [Google Scholar]
- 5.Steinglass P. The alcoholic family at home: Patterns of interaction in Dry, Wet, and Transitional Stages of Alcoholism. Arch Gen Psychiatry. 1981;38:578–84. doi: 10.1001/archpsyc.1980.01780300090011. [DOI] [PubMed] [Google Scholar]
- 6.O’Farrell TJ, Fals-Stewart W. Treatment models and methods: Family models. In: McCrady BS, Epstein EE, editors. Addictions: A comprehensive guidebook. New York: Oxford University Press; 1999. pp. 287–305. [Google Scholar]
- 7.Rosemary A, Webester MH. Peer and parental influences on adolescent's substance use: a path analysis. Int J Addiction. 1994;29:647–57. doi: 10.3109/10826089409047405. [DOI] [PubMed] [Google Scholar]
- 8.Bush M, Caronna FB, Spratt SE. Substance abuse and family dynamics. In: Friedman L, Fleming NF, Roberts DH, Hyman, editors. Source book of substance abuse and addiction. Baltimore: Williams and Wilkins; 1996. pp. 57–71. [Google Scholar]
- 9.Lennox RD, Scott-Lennox JA, Holder HD. Substance abuse and family illness: Evidence from health care utilization and cost-offset research. J Behav Health Serv Res. 1992;19:83–95. doi: 10.1007/BF02521310. [DOI] [PubMed] [Google Scholar]
- 10.Holder HD. The cost offsets of alcoholism treatment. In: Galanter M, editor. Recent developments in alcoholism. New York: Plenum Press; 1998. pp. 361–74. [DOI] [PubMed] [Google Scholar]
- 11.Connors GJ, Donovan DM, DiClemente CC. New York: Guilford Press; 2001. Substance abuse treatment and the stages of change: selecting and planning interventions. [Google Scholar]
- 12.Bhowmick P, Tripathi BM, Jhingan HP, Pandey RM. Social support, coping resources and codependence in spouses of individuals with alcohol and drug dependence. Indian J Psychiatry. 2001;43:219–24. [PMC free article] [PubMed] [Google Scholar]
- 13.Ray GT, Mertens JR, Weisner C. The excess medical cost and health problems of family members diagnosed with alcohol or drug problems. Medical Care. 2007;45:116–22. doi: 10.1097/01.mlr.0000241109.55054.04. [DOI] [PubMed] [Google Scholar]
- 14.Chandra K. Chandigarh, India: Postgraduate Institute of Medical Education & Research; 2004. Burden and coping in caregivers of men with alcohol and opioid dependence, MD dissertation. [Google Scholar]
- 15.Pai S, Kapur KL. The burden on the family of a psychiatric patient: development of an assessment scale. Br J Psychiatry. 1981;138:332–5. doi: 10.1192/bjp.138.4.332. [DOI] [PubMed] [Google Scholar]
- 16.Shyangwa PM, Tripathi BM, Lal R. Family burden in opioid dependence syndrome in tertiary care centre. J Nepal Med Assoc. 2008;47:113–9. [PubMed] [Google Scholar]
- 17.Lamichhane N, Shyangwa PM, Shakya R. Family burden in substance dependence syndrome. [accessed on October 21, 2011]. Available from: http://www.thikthak.com/ WEBSITES/gmc/journal .
- 18.Ray R. New Delhi: Ministery of Social Justice and Empowerment, Government of India and United Nations Office on Drugs and Crime, Regional office for South Asia; 2004. The extent, pattern and trends of drug abuse in India: National survey. [Google Scholar]
- 19.Chakraborti S, Kulhara P, Verma SK. Extent and determinants of burden among families of patients with affective disorders. Acta Psychiatr Scand. 1992;86:247–52. doi: 10.1111/j.1600-0447.1992.tb03261.x. [DOI] [PubMed] [Google Scholar]
- 20.Chakraborti S, Kulhara P, Verma SK. Family burden of neurosis: extent & determinants. Hong Kong J Psychiatry. 1996;6:23–8. [Google Scholar]
- 21.Gautam S, Nijhawan M. Burden on families of schizophrenia and chronic lung disease patients. Indian J Psychiatry. 1984;26:156–9. [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta M, Giridhar C, Kulhara P. Burden of care of neurotic patients: correlates and coping strategies in relatives. Indian J Soc Psychiatry. 1991;7:8–21. [Google Scholar]
- 23.Geneva: WHO; 1992. WHO. The ICD-10 classifcation of mental and behavioral disorders: Guidelines. [Google Scholar]
- 24.Bhushan V, Sachdev DR. The family. In: Bhushan V, Sachdev DR, editors. Introduction to sociology. 26th ed. Allahbad: Kitabmahal Publishers; 2006. pp. 291–322. [Google Scholar]
- 25.New Delhi, India: Ministry of Health and Family Welfare; 1982. National Mental Health Programme for India. [Google Scholar]
- 26.Scazufca M, Kuipers E. Stability of expressed emotion in relatives of those with schizophrenia and its relationship with burden of care and perception of patients’ social functioning. Psychol Med. 1998;28:453–61. doi: 10.1017/s0033291797005977. [DOI] [PubMed] [Google Scholar]
- 27.Mattoo SK, Chakraborti S, Anjaiah M. Psychosocial factors associated with relapse in men with alcohol or opioid dependence. Indian J Med Res. 2009;130:702–8. [PubMed] [Google Scholar]


