Abstract
Background & objectives:
Oxidative stress plays important roles in the pathophysiology of type 2 diabetes mellitus (T2DM). The diacron reactive oxygen metabolites (d-ROMs) test has been used in the clinics. The present study was aimed to investigate the correlation of the oxidative stress status, as evaluated by the d-ROMs, with atherosclerotic risk factors in T2DM patients, in comparison to controls.
Methods:
The study included 200 subjects (100 patients with T2DM and 100 controls; 86 males/114 females; mean age 59.0 yr). Clinical variables including the body mass index, blood pressure (BP), glucose and lipid panels, in addition to the d-ROMs, were measured.
Results:
Patients with T2DM showed significantly higher d-ROMs levels than controls (322 ± 60 vs. 345 ± 64 U. Carr., P<0.05). A multiple linear regression analysis revealed that systolic BP (β=0.26, P<0.05) and high-density lipoprotein cholesterol (HDL-C: β= -0.30, P<0.05) were independently and significantly correlated with the d-ROMs levels in patients with T2DM, although these correlations were not significant in the controls. The gender-based analysis showed that systolic BP (β = 0.44, P<0.05) and HDL-C (β = -0.36, P<0.05) were independently and significantly correlated with the d-ROMs levels in females with T2DM, while there was a marginally significant correlation between HDL-C and the d-ROMs levels (β = -0.36, P=0.06) in males with T2DM.
Interpretation & conclusions:
The present findings may reinforce the importance of BP control in female patients with T2DM, as well as the management of HDL-C in male and female patients with T2DM, under the linkage between oxidative stress and atherosclerosis.
Keywords: Atherosclerotic risk factor, blood pressure, d-ROMs test, HDL cholesterol, hypertension, oxidative stress
Patients with type 2 diabetes mellitus (T2DM) are recognized to be at an increased risk of atherosclerotic diseases, including cardiovascular disease (CVD), and this is a public health issue in Asian populations1,2. This risk may be partly due to the presence of other well-known atherosclerotic risk factors, such as dyslipidaemia and elevated blood pressure (BP)3,4. Oxidative stress occurs when there is an imbalance between the generation of reactive oxygen species (ROS) and the antioxidant system, and the oxidative stress burden also plays relevant roles in the development of T2DM-related CVD5,6.
Despite the accumulated knowledge concerning the roles of oxidative stress in T2DM and its related CVD, there have been only a few indices available to analyze the oxidative stress status of patients in daily clinical practice, and such an index is required urgently5,6. The diacron reactive oxygen metabolites (d-ROMs) test (Diacron, Italy) can quantify the oxidative stress status by measuring the hydroperoxides of organic compounds (lipids, proteins, nucleic acids, etc.), and has been introduced as an oxidative stress-related marker in the clinic7,8,9,10,11. But there have been no studies that have conclusively investigated the comprehensive association between the d-ROMs and various atherosclerotic risk factors in patients with T2DM. To address these shortcomings, the objective of the present study was to observe the correlation of the oxidative stress status, as evaluated by the d-ROMs, with several atherosclerotic risk factors in T2DM patients, in comparison to controls.
Material & Methods
A total of 200 Japanese subjects (males/females = 86/114; mean age = 59.0 yr) were randomly recruited from outpatient clinics and health check-ups and patient's education classes in Jichi Medical University (Tochigi), Koto Medical Centre (Kyoto) and Tottori University (Tottori) in Japan, between 2006 and 2010. Patients with T2DM and controls (without T2DM) were matched for age, gender and current smoking habits. The sample size was estimated as approximately 100 subjects in each group with a significance level (α) of 5 per cent (a two tailed) and a power (1-β) of 80 per cent, based on our pilot study of the different levels of the d-ROM level (mean, 20U. Carr; standard deviation, 60U. Carr). T2DM was diagnosed on the basis of the World Health Organization (WHO) and American Diabetes Association (ADA) criteria12,13, and the population of T2DM patients included the patients with a well-controlled glycaemic conditions under dietary treatment and/or treatment with oral antihyperglycaemic drugs such as biguanides (metformin) and sulphonylureas. The control population included subjects who had not been diagnosed with diabetes mellitus and/or had a fasting plasma glucose (FPG) level < 7.0 mmol/l12,13. The exclusion criteria of the present study were individuals who were pregnant, had acute infections such as the common cold, were alcohol abusers or had a history of cardio/cerebrovascular, thyroid, collagen, severe kidney or liver diseases, as well as those treated with insulin injections, lipid-lowering drugs, antihypertensive drugs, oral contraceptives and antioxidant agents. The study protocol was approved by the Institutional Ethics Committee, and all subjects gave written informed consent.
The subjects’ current smoking habits were based on self-reports. The systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in the right arm with a mercury sphygmomanometer with the subject in the seated position. In addition to the body mass index (BMI), the fasting serum total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C) and FPG levels were measured by standard enzymatic methods (Sekisui Co. Ltd., Tokyo, Japan). The intra- and inter-assay coefficients of variation were 0.4 and 1.1 per cent in TC, 0.5 and 0.4 per cent in TG, 1.7 and 2.9 per cent in HDL-C, and 0.8 and 1.0 per cent in FPG, respectively. The d-ROMs values were obtained using a kinetic spectrophotometric assay (the F.R.E.E system; Diacron, Italy) with intra- and inter-assay coefficients of variation of 2.1 and 3.1 per cent, respectively7,9. Fresh serum samples were mixed with a buffered solution, and a chromogenic substrate was added to the mixture. The mixture was centrifuged, and then incubated in the thermostatic block of the system. The absorbance was recorded at 505 nm. The measurement is expressed in U. Carr., where 1 U. Carr. corresponds to 0.08 mg/dl H2O2.
Statistical analysis: The data are expressed as the means ± standard deviation (SD) or the medians plus the interquartile range. The data between the groups were compared using an unpaired t-test or one-way analysis of variance (ANOVA). A simple correlation analysis (Pearson's test) and a multiple linear regression analysis were utilized to calculate the correlations between the d-ROMs and other factors. The TG values were log-transformed for these analyses because of their skewed distribution. All of the measured factors were used in the multiple linear regression analyses. However, because of the close correlation between the SBP and DBP as well as the overlapping significance of FPG and HbA1c, only the SBP and HbA1c were entered into the multiple linear regression analysis model. Because there was also a close correlation between the TG and HDL-C in the gender-based analyses, only the HDL-C was entered into the multiple linear regression analysis model. P<0.05 was considered statistically significant.
Results
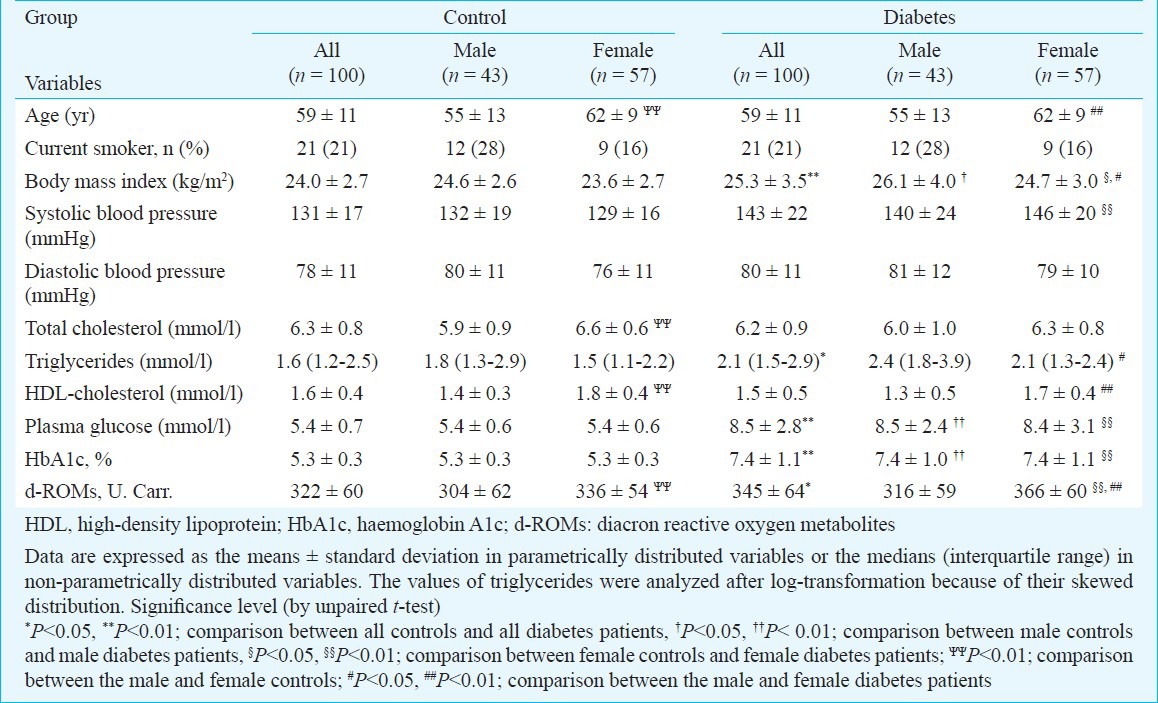
Forty patients with T2DM were treated with oral antihyperglycaemic drugs (21 patients received metformin therapy and 27 patients were treated with sulphonylureas). Patients with T2DM had significantly higher levels of their BMI (P<0.01), SBP (P<0.01), TG (P=0.01), FPG (P<0.01) and HbA1c (P<0.01) and d-ROMs (P=0.01) than controls. Male patients with T2DM had significantly higher levels of their BMI (P<0.05), FPG (P<0.01) and HbA1c (P<0.01) than male controls, while female patients with T2DM had significantly higher levels of their BMI (P=0.04), SBP (P<0.01), FPG (P<0.01) and HbA1c (P<0.01) and d-ROMs (P<0.01) than female controls. In addition, female controls had a significantly higher age (P<0.01), TC (P<0.01), HDL-C (P<0.01) and d-ROMs (P=0.01) than male controls, while female patients with T2DM had significantly lower levels of BMI (P=0.04) and TG (P=0.01), as well as higher levels of HDL-C (P<0.01) and d-ROMs (P<0.01), than male patients with T2DM (Table I).
Table I.
Clinical characteristics of the patients with type 2 diabetes mellitus and control subjects by gender
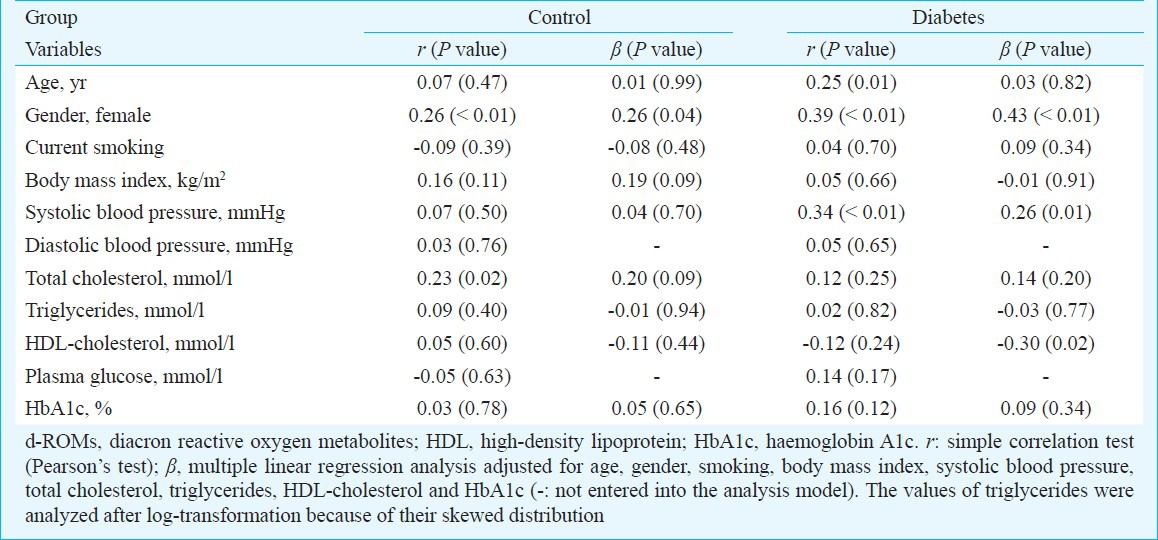
The results of a simple correlation analysis and multiple linear regression analysis on the d-ROMs, adjusted for age, gender, smoking, BMI, SBP, TC, TG, HDL-C and HbA1c in all patients with T2DM and controls are listed in Table II. The simple correlation analysis showed that female gender (r = 0.26, P<0.01) and TC (r = 0.23, P=0.02) were significantly correlated with the d-ROMs levels in controls, and the subsequent multiple linear regression analysis revealed that only female gender remained significantly correlated with the d-ROMs levels (β = 0.26, P=0.04), independent of other factors, in controls. On the other hand, while there were significant correlations between age (r = 0.25, P=0.01), female gender (r = 0.39, P<0.01), SBP (r = 0.34, P<0.01) and the d-ROMs levels in all patients with T2DM in the simple correlation analysis, female gender (β = 0.43, P<0.01), SBP (β = 0.26, P=0.01) and HDL-C (β = -0.30, P=0.02) were identified to be independently and significantly correlated with the d-ROMs levels in the subsequent multiple linear regression analysis in all patients with T2DM.
Table II.
Correlation of each variable on the d-ROMs in patients with type 2 diabetes mellitus and control subjects
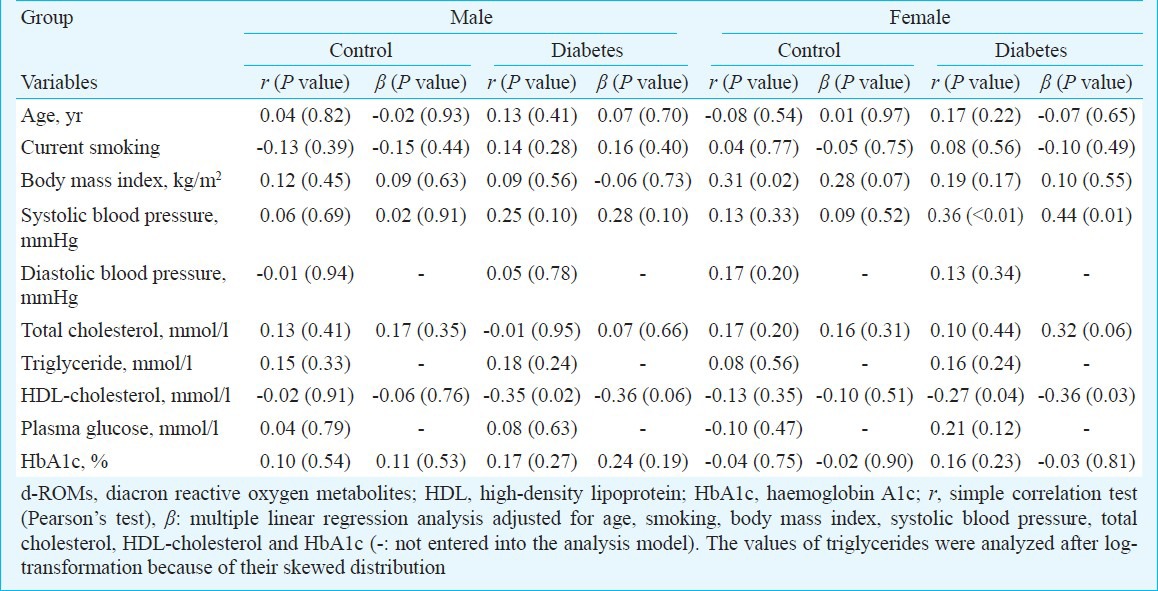
The results of a simple correlation analysis and multiple linear regression analysis on the d-ROMs, adjusted for age, smoking, BMI, SBP, TC, HDL-C and HbA1c, in patients with T2DM and controls, by gender, are listed in Table III. Neither the simple correlation analysis nor the multiple linear regression analysis showed any factors significantly associated with the d-ROMs in male controls. The simple correlation analysis showed that HDL-C (r = -0.35, P=0.02) was significantly correlated with the d-ROMs levels in male patients with T2DM, and the subsequent multiple linear regression analysis revealed that a marginally significant correlation was maintained between HDL-C and the d-ROMs levels (β = -0.36, P=0.06). On the other hand, the simple correlation analysis showed that BMI (r = 0.31, P=0.02) was significantly correlated with the d-ROMs levels in female controls, and the subsequent multiple linear regression analysis revealed that the correlation between BMI and the d-ROMs was not significant. The simple correlation analysis showed that SBP (r = 0.36, P<0.01) and HDL-C (r = -0.27, P=0.04) were significantly correlated with the d-ROMs levels in female patients with T2DM, and the subsequent multiple linear regression analysis revealed that there was an independent and significant correlation between SBP and the d-ROMs levels (β = 0.44, P=0.01) as well as between HDL-C and the d-ROMs levels (β = -0.36, P=0.03).
Table III.
Correlation of each variable on the d-ROMs in patients with type 2 diabetes mellitus and control subjects by gender
The d-ROMs levels associated with medications were also analyzed in patients with T2DM, because of the reported influence of drugs such as metformin on oxidative stress14,15. There was no significant difference in the d-ROMs levels among the patients who received metformin therapy (331 ± 64 U. Carr.), those treated with sulphonylureas (362 ± 58 U. Carr.) and those with dietary treatment only (342 ± 66 U. Carr.) in these patients (ANOVA, P=0.22). The multiple linear regression analysis, after adjusting for the use of antihyperglycemic drugs (metformin and sulphonylureas) in addition to factors such as age, gender, smoking, BMI, SBP, TC, TG, HDL-C and HbA1c, revealed that female gender (β = 0.45, P<0.01), SBP (β = 0.26, P=0.01) and HDL-C (β = -0.31, P=0.01) continued to be independently and significantly correlated with the d-ROMs levels, while the use of antihyperglycaemic drugs was not identified as the factor significantly associated with the d-ROMs (β = 0.11, P=0.29), in patients with T2DM (all data not shown).
Discussion
The present study showed that patients with T2DM had a significantly higher level of the oxidative stress status, as evaluated by the d-ROMs, than controls. This difference was significant in T2DM females patients in particular. This finding is consistent with an earlier study, which did not examine the correlation of the d-ROMs with other factors in detail8. These findings seem to support the general idea that T2DM is an oxidative stress condition, associated with various complications5,6, although whether this idea is more applicable to female patients than male patients with T2DM requires further consideration.
The present study showed that there were independent and significant correlations of the d-ROMs levels with the BP (positive) and HDL-C (inverse) in all patients with T2DM, but not in controls. The female gender was found to be significantly correlated with the d-ROMs levels in both patients with T2DM and controls, as reported in an earlier study from Japan11. The gender-based analyses in the present study showed a significant correlation between BP and the d-ROMs levels in female patients with T2DM, as well as between HDL-C and the d-ROMs levels in male and female patients with T2DM (though this correlation was marginally significant in male patients). Because tight BP control has been shown to reduce the CVD risks in diabetic patients16 and a low HDL-C level increases the CVD risks in these patients17,18, the present findings may emphasize the importance of BP control in female patients with T2DM, as well as the management of HDL-C in male and female patients with T2DM.
The mechanistic explanation for these results remains to be elucidated for this observational study. The understanding of the association between oxidative stress and the disease pathophysiology is generally difficult with a complex interdependency, because oxidative stress can be involved as both a primary event and a consequence of an elevated BP and metabolic disorders, causing a vicious cycle of the oxidative stress-disease pathophysiology relationship19,20. The HDL particle is well-known to have anti-atherogenic effects. Although T2DM is associated with a dysregulation in HDL metabolism and dysfunctional properties of HDL particles including HDL-mediated reverse cholesterol transport, the inverse correlation of HDL-C with oxidative stress can be a reflection to the anti-oxidative exertion of HDL particle18. With regard to the positive correlation between the BP and oxidative stress, the most crucial is the oxidative stress-induced inactivation of endothelium-derived nitric oxide (NO), promoting vasoconstriction21,22. For instance, the upregulation of the renin-angiotensin system, which can raise the BP, is seen in diabetic patients, and angiotensin II induces oxidative stress, leading to a reduction in the availability of NO4. Microvascular insulin resistance is also present in diabetes patients, and this insulin resistance abolishes the NO-induced vasodilatation, leading to an elevated BP, and therefore, oxidative stress4. The gender difference in the correlation patterns of BP with the d-ROMs may occur because the mechanisms responsible for BP levels in males and females can be different in association with cardiometabolic factors, although the reasons remained undetermined23. Female patients with T2DM had significantly higher SBP and d-ROMs levels than male patients with T2DM in the present study, and this may, in part, affect the results of gender difference in the correlation between BP and the d-ROMs levels. Further research is warranted to clarify the biological mechanisms involved in the present study results.
There were some limitations to this study. The sample size was relatively small. The data on the complications and the disease duration in patients with T2DM were not available in this study. Oral glucose tolerance testing (OGTT) was not used to diagnose T2DM. Although this is often seen and permitted in epidemiological studies24, the control population might not fully exclude patients with T2DM who are detectable using the OGTT. Although the present study did not find any significant influence of antihyperglycaemic drugs such as metformin (which can reportedly reduce the oxidative stress status14,15) on the d-ROMs levels, the present study design could not completely determine the cause-and-effects. Future studies with a larger number of subjects, with the inclusion of various T2DM-related data and a prospective/interventional study design will clarify this issue.
In summary, patients with T2DM, in particular female patients, displayed a significantly higher level of the oxidative stress status, as evaluated by the d-ROMs test, than controls. The present study showed a positive correlation between BP and the d-ROMs in female patients with T2DM in particular, and an inverse correlation between HDL-C and the d-ROMs levels in male and female patients with T2DM; however, these correlations were not clearly observed in the controls. These findings suggest that more focus on BP and HDL-C in patients with T2DM may be relevant to the concept of the oxidative stress-CVD linkage. Further studies are required to establish the observed relationship.
References
- 1.Ali MK, Narayan KM, Tandon N. Diabetes & coronary heart disease: current perspectives. Indian J Med Res. 2010;132:584–97. [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar S, Mukherjee S, Mukhopadhyay P, Pandit K, Raychaudhuri M, Sengupta N, et al. Prevalence of diabetes and impaired fasting glucose in a selected population with special reference to influence of family history and anthropometric measurements - the Kolkata policeman study. J Assoc Physicians India. 2008;56:841–4. [PubMed] [Google Scholar]
- 3.Taskinen MR. Diabetic dyslipidemia. Atheroscler Suppl. 2002;3:47–51. doi: 10.1016/s1567-5688(01)00006-x. [DOI] [PubMed] [Google Scholar]
- 4.Ko SH, Cao W, Liu Z. Hypertension management and microvascular insulin resistance in diabetes. Curr Hypertens Rep. 2010;12:243–51. doi: 10.1007/s11906-010-0114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piconi L, Quagliaro L, Ceriello A. Oxidative stress in diabetes. Clin Chem Lab Med. 2003;41:1144–9. doi: 10.1515/CCLM.2003.177. [DOI] [PubMed] [Google Scholar]
- 6.Stephens JW, Khanolkar MP, Bain SC. The biological relevance and measurement of plasma markers of oxidative stress in diabetes and cardiovascular disease. Atherosclerosis. 2009;202:321–9. doi: 10.1016/j.atherosclerosis.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Iamele L, Fiocchi R, Vernocchi A. Evaluation of an automated spectrophotometric assay for reactive oxygen metabolites in serum. Clin Chem Lab Med. 2002;40:673–6. doi: 10.1515/CCLM.2002.115. [DOI] [PubMed] [Google Scholar]
- 8.Vîrgolici B, Mohora M, Stoian I, Lixandru D, Găman L, Paveliu F. A comparative oxidative stress study - obesity with and without diabetes mellitus. Rom J Intern Med. 2005;43:261–8. [PubMed] [Google Scholar]
- 9.Vassalle C. An easy and reliable automated method to estimate oxidative stress in the clinical setting. Methods Mol Biol. 2008;477:31–9. doi: 10.1007/978-1-60327-517-0_3. [DOI] [PubMed] [Google Scholar]
- 10.Kotani K, Sakane N, Tsuzaki K, Matsuoka Y, Sano Y, Hamada T, et al. Lifestyles and oxidative stress in type 2 diabetic patients. Scand J Clin Lab Invest. 2008;68:516–8. doi: 10.1080/00365510802023090. [DOI] [PubMed] [Google Scholar]
- 11.Hirose H, Kawabe H, Komiya N, Saito I. Relations between serum reactive oxygen metabolites (ROMs) and various inflammatory and metabolic parameters in a Japanese population. J Atheroscler Thromb. 2009;16:77–82. doi: 10.5551/jat.e265. [DOI] [PubMed] [Google Scholar]
- 12.Geneva: World Health Organization; 2006. World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. [Google Scholar]
- 13.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31(Suppl 1):S55–60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- 14.Bonnefont-Rousselot D, Raji B, Walrand S, Gardès-Albert M, Jore D, Legrand A, et al. An intracellular modulation of free radical production could contribute to the beneficial effects of metformin towards oxidative stress. Metabolism. 2003;52:586–9. doi: 10.1053/meta.2003.50093. [DOI] [PubMed] [Google Scholar]
- 15.Rösen P, Wiernsperger NF. Metformin delays the manifestation of diabetes and vascular dysfunction in Goto-Kakizaki rats by reduction of mitochondrial oxidative stress. Diabetes Metab Res Rev. 2006;22:323–30. doi: 10.1002/dmrr.623. [DOI] [PubMed] [Google Scholar]
- 16.Smith A. The treatment of hypertension in patients with diabetes. Nurs Clin North Am. 2001;36:273–89. [PubMed] [Google Scholar]
- 17.Goldbourt U, Yaari S, Medalie JH. Isolated low HDL cholesterol as a risk factor for coronary heart disease mortality. A 21-year follow-up of 8000 men. Arterioscler Thromb Vasc Biol. 1997;17:107–13. doi: 10.1161/01.atv.17.1.107. [DOI] [PubMed] [Google Scholar]
- 18.Van Linthout S, Spillmann F, Schultheiss HP, Tschöpe C. High-density lipoprotein at the interface of type 2 diabetes mellitus and cardiovascular disorders. Curr Pharm Des. 2010;16:1504–16. doi: 10.2174/138161210791051031. [DOI] [PubMed] [Google Scholar]
- 19.John S, Schmieder RE. Potential mechanisms of impaired endothelial function in arterial hypertension and hypercholesterolemia. Curr Hypertens Rep. 2003;5:199–207. doi: 10.1007/s11906-003-0021-1. [DOI] [PubMed] [Google Scholar]
- 20.Madamanchi NR, Hakim ZS, Runge MS. Oxidative stress in atherogenesis and arterial thrombosis: the disconnect between cellular studies and clinical outcomes. J Thromb Haemost. 2005;3:254–67. doi: 10.1111/j.1538-7836.2004.01085.x. [DOI] [PubMed] [Google Scholar]
- 21.Lassègue B, Griendling KK. Reactive oxygen species in hypertension; An update. Am J Hypertens. 2004;17:852–60. doi: 10.1016/j.amjhyper.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Rodrigo R, González J, Paoletto F. The role of oxidative stress in the pathophysiology of hypertension. Hypertens Res. 2011;34:431–40. doi: 10.1038/hr.2010.264. [DOI] [PubMed] [Google Scholar]
- 23.Kim JK, Alley D, Seeman T, Karlamangla A, Crimmins E. Recent changes in cardiovascular risk factors among women and men. J Womens Health (Larchmt) 2006;15:734–46. doi: 10.1089/jwh.2006.15.734. [DOI] [PubMed] [Google Scholar]
- 24.Mohan V, Goldhaber-Fiebert JD, Radha V, Gokulakrishnan K. Screening with OGTT alone or in combination with the Indian diabetes risk score or genotyping of TCF7L2 to detect undiagnosed type 2 diabetes in Asian Indians. Indian J Med Res. 2011;133:294–9. [PMC free article] [PubMed] [Google Scholar]


