Abstract
Objective:
To study the prevalence of psychiatric co-morbidity in patients of chronic daily headache (CDH) and compare the efficacy of treatment between various type of headache associated with psychiatric co-morbidity.
Materials and Methods:
Prospective case control cohort study, 92 consecutive patients of CDH meeting eligibility criteria. The diagnosis of various subtypes of CDH was made according to the IHS criteria. Age, sex, educational, marital and socioeconomic status, matched controls were also selected. Patients were evaluated with the Mini International Neuropsychiatric Interview (MINI) scale at the time of enrolment and at 3 months.
Results:
CDH accounted for 28% of all headache patients. The mean age of presentation was 30.2 ± 10.3 years, male: Female ratio of 28:64 and mean duration of 4.56 ± 0.56 years. Chronic migraine (CM) accounted for 59 patients, chronic tension type headache (CTTH) 22 patients, new daily persistent headache (NDPH) 3 patients and miscellaneous 8 patients. Psychiatric co-morbidity was present in 53.3% patients with CDH, and was more common in CM (62.7%) as compared to CTTH (36.4%). Single psychiatric co-morbidity was seen in 26 patients, while 23 patients had multiple co-morbidity. Major depressive episode, anxiety disorder, agoraphobia and dysthymia were significant psychiatric co-morbidities. Patients with CM were treated with topiramate or divalproex sodium ER and CTTH were treated with amitriptyline. 55 patients came for follow up at 3 months, improvement in headache was seen in 29 patients.
Conclusion:
Psychiatric co-morbidity was present in more than 50% patients with CDH and its presence along with a duration of ≥2 years was associated with a poor response to treatment.
Keywords: Chronic daily headache, chronic migraine, chronic tension type headache, psychiatric co-morbidity
Introduction
Chronic daily headache (CDH) is the most common headache problem seen in clinics specifically devoted to headache management and its prevalence in the general population is almost 5%.[1,2] Co-morbid factors play a significant role in the development and maintenance of headache that occurs on a daily or near daily basis. The prevalence of psychiatric co-morbidity in patients with CDH ranges from 64-90%,[3,4] mostly in the form of anxiety and mood disorders with higher rates in women with CDH than in men.[5] Psychiatric issues are prominent among patients with more difficult headache problems, particularly CDH.[6,7,8,9,10] Association between CDH and psychiatric co-morbidity may be explained by shared mechanism in structures of the central nervous system between pain and affective disorders, perhaps involving Limbic activation.[7] Common pathogenic mechanisms between migraine and mood disorders have been implicated, including a decrease of platelet serotonin concentration, an increase of urinary 5-hydroxytryptamine and a possible increase of 5-hydroxyindole acetic acid.[11] Another small study using MMPI-2 with CDH patients, significantly high scores have been reported for the scales measuring hysteria, hypochondriasis, psychasthenia, depression, and social introversion.[12] Presence of psychiatric co-morbidity complicates headache management and portends a poorer prognosis for headache treatment.[13,14,15]
In experimental studies, it has been shown that chronic use of analgesics may alter the functioning of the central 5-HT system.[16] A co-morbid psychiatric disorder may cause a stronger need to take analgesics in headache patient.[17,18] Depressive patients may have decreased pain threshold or may feel more unpleasant pain, resulting in analgesic overuse for the relief of their headache.[19]
Early diagnosis and management of psychiatric co-morbidity is important because several prospective studies have shown that many psychiatric disorders are significant risk factors for both the onset and chronicization of primary headaches.[6,7] It is also suspected that headache triggers psychiatric disorder, mostly of affective nature, and affects both their cause and outcome.[11] The majority of studies reporting maladaptive behaviour or genuine psychopathology among headache patients have employed Minnesota Multiphasic Personality Inventory or other validated psychometric measures of psychological symptoms or personality such as Beck depression inventory,[14,20,21] Spielberger state/Trait anxiety inventory or Eysenck personality inventory. However, none of these is adequate for conferring a psychiatric diagnosis following DSM-IV criteria. The Mini-International Neuropsychiatric Interview (MINI) is a structured interview that focuses on mood and anxiety disorders.[22] It is based on DSM-IV and ICD-10 diagnostic criteria and has been shown to have high reliability with other more comprehensive structured interviews.[23,24] It has been translated into 39 different languages and validation studies have been performed. The administration of the instrument requires about 15 minutes and it can be used by clinicians after a brief training session.
CDH remains a relatively unexplored entity in India. There is only one study by Chakravarty.[25] in which 50% of patients also had a psychiatric diagnosis; however no formal psychiatric referral was made by them. The present study has been conducted to find out the prevalence of psychiatric co-morbidity in CDH using the Mini International Neuropsychiatric Interview (MINI) which is a simple, easily administrable, bedside clinical tool and compare the efficacy of treatment between various type of headache associated with psychiatric co-morbidity
Materials and Methods
The present study was done in the outpatients department (OPD) of a large teaching hospital attached to the King George's Medical University (CSM Medical University), Lucknow located in North India and providing secondary/tertiary medical care. The study was approved by the Institutional Ethics Committee and an informed written consent was obtained.
Patient sample
Consecutive patients of chronic daily headache (CDH) attending the neurology OPD between July-October 2005 were enrolled for the study and followed up for 3 months till January 2006.
The inclusion and exclusion criteria for subjects in the study group are as given below.
Inclusion criteria
Age ≥15 years and ≤65 years
Onset of symptoms at age <50 years
Exclusion criteria
Presence of concomitant medical illness such as end stage organ failures e.g., hepatic, renal, cardiac, respiratory, Secondary cause of CDH,
Patients already taking prophylactic treatment,
Pregnancy or lactation,
The control group was obtained from the healthy relatives of the patient preferably from the same family as well as hospital employees. The subjects included as control had either no headache during the last one year or less than ten days per year and not more than one day per month. None of them had any concomitant medical illness, pregnancy or lactation.
Diagnosis of chronic daily headache and its subtypes
The diagnosis of CDH was based on the criteria given by Silberstein et al.,[2] which are headache occurring for ≥ 15 days per month with a duration of ≥ 4 hours per day for more than 3 months. The diagnosis of various types of CDH was based on the criteria given by the International Headache Society (International Classification of Headache Disorders, 2nd edition).[26]
Plan of study
A detailed history was obtained and thorough examination done using a pre-designed structured proforma to exclude secondary causes of CDH. Neuroimaging (CT/MRI) of brain was done wherever indicated. Headache severity was graded on a four point scale (0-3), where 0 is no pain, 1 is mild pain; which does not interfere with the patient's daily activities; 2 is moderate pain which interferes with the patient's daily activities but patient can continue his work; 3 is severe headache patient has to take bed rest. Patients were asked about details of medication use during last 3 months including over the counter medication and during follow up period details were recorded on the basis of headache diary which were provided to the patient. The patients with CTTH were prescribed amitriptyline 10 mg/day increasing to 20 mg after a week and 25 mg/day after 4 weeks. Patients with migraine were given either divalproex Sodium ER 500 mg/day or topiramate 25 mg twice a day for 2 weeks after which the dose of topiramate was increased to 50 mg twice a day. Patients of NDPH were treated like CTTH. A combination of Paracetamol (500 mg) plus domperidone (20 mg) was used for acute treatment of headache. All the subjects were given a headache diary at the initial evaluation and asked to come back after 3 months. The number of days of headache was also recorded and the number of analgesic tablets taken as acute medication during a month was noted down. The overall response was graded (on the basis of % reduction in the number of days with headache per month) into poor = up to 25%, fair = 26-50%, and good = ≥50% reduction.
Psychiatric evaluation
The psychiatric evaluation of the subjects in the study and control group was done by one of the authors (AKS) at the baseline and after 3 months. A validated Hindi translation of MINI (version 5.0.0) was used for psychiatric assessment. The initial evaluation was done within 3 days of enrolment and at the same time patients were given an appointment for second evaluation. Patients who did not keep their appointments were given a telephonic reminder following which a postal reminder was sent to their address. If they still did not respond, the patient was considered to be a dropout.
Statistical analysis
The values are depicted as Mean ± SD. Student's t-test was used for comparison between patients with CDH and control group. A univariate analysis was done to evaluate the various factors associated with the presence of psychiatric co-morbidity as well as its improvement at 3 months. The Chi square test with Yates correction was used for comparison of groups and the odd's ratio and confidence interval (CI) was also calculated. A P value less than 0.05 were considered significant.
Results
Ninety two consecutive patients of CDH were recruited. A flow chart showing the sample selection is shown in Figure 1. CDH accounted for 28% of all patients presenting with a complaint of headache to the neurology OPD. The demographic characteristics of subjects are shown in Table 1. The study group was well matched to the controls with respect to age, sex, education, marital status, and socioeconomic status. Chronic migraine was the commonest type of CDH, seen in 64% followed by CTTH in 23.9% and NDPH in 3.3%. No case of hemicrania continua was seen. More than one type of headache was seen in 8.7%. Medication overuse was seen in 4.3%.
Figure 1.
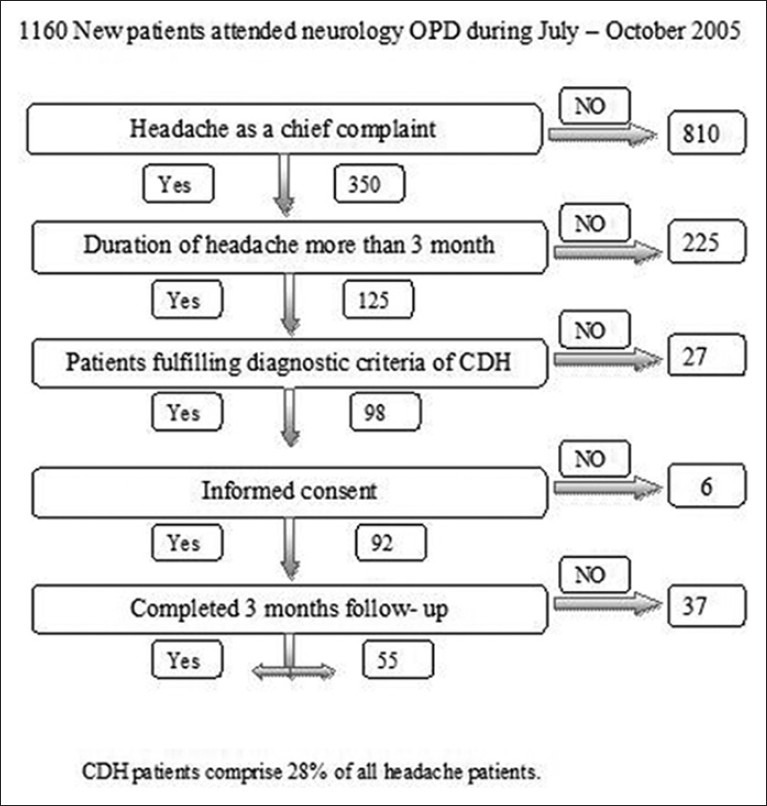
Flow chart showing sample selection
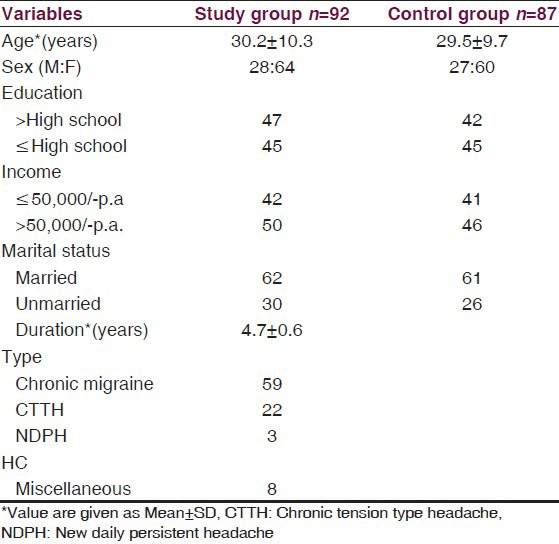
Table 1.
Demographic data
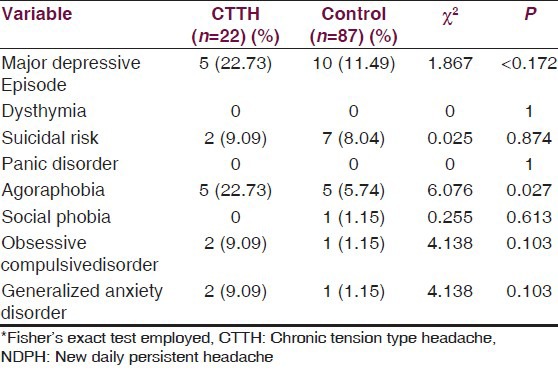
Psychiatric co-morbidity was present in 49 patients with CDH, with 26 patients having single and 23 patients multiple co-morbidity [Figure 2]. Presence of psychiatric co-morbidity did not have any clear correlation with age, sex, marital status, education, socioeconomic status and duration of headache [Table 2]. Major depressive episode, dysthymia, agoraphobia and generalized anxiety disorder were significantly more common in patients with CDH [Table 3]. Comparison of patients with CM and control group revealed that major depressive episode, dysthymia, suicidal risk, panic disorder, agoraphobia and generalized anxiety disorder were significantly more prevalent in CM [Table 4]. Whereas in patients with CTTH only agoraphobia was significantly more prevalent as compared to controls [Table 5]. Comparison of patients with CM and CTTH did not reveal any significant difference in various psychiatric co-morbidities in the two groups.
Figure 2.
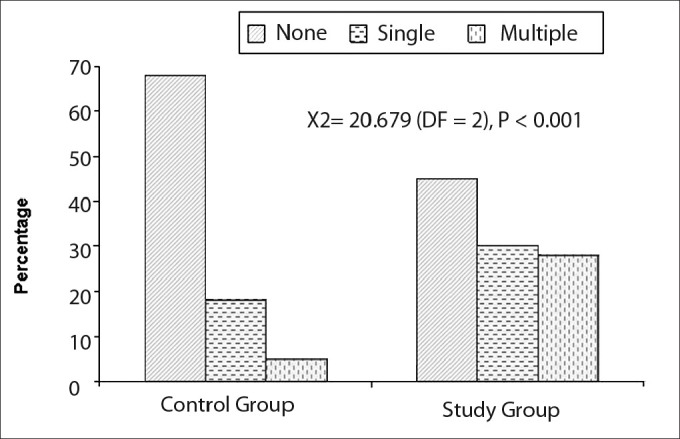
Histogram showing presence of psychiatric co-morbidity in control and study group
Table 2.
Clinical features related to presence of psychiatric comorbidity of chronic daily headache
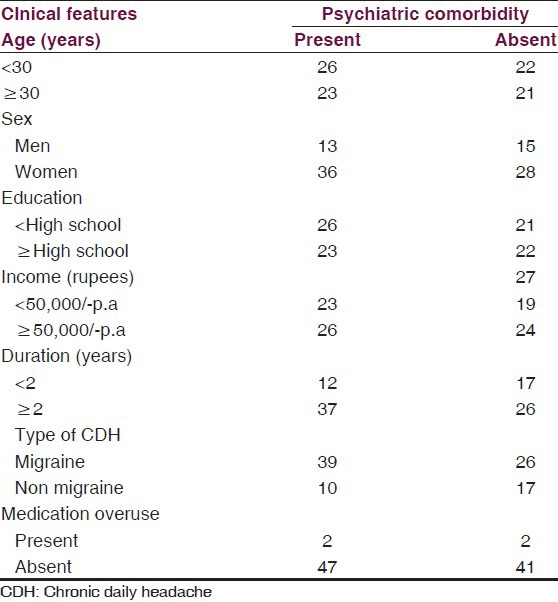
Table 3.
Various psychiatric comorbidities in study and control groups before
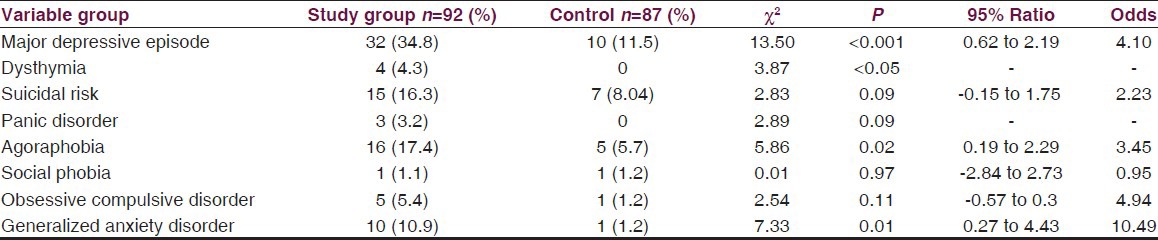
Table 4.
Association of different variables in chronic migraine and controls-before treatment
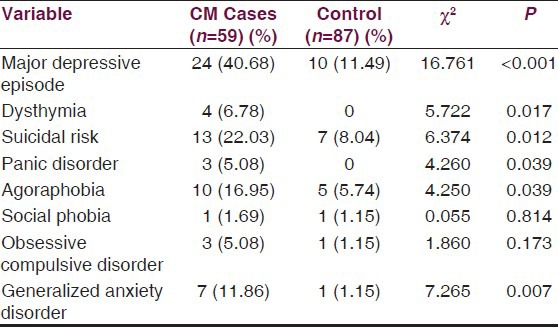
Table 5.
Association of different variables in chronic tension type headacheand controls-before treatment
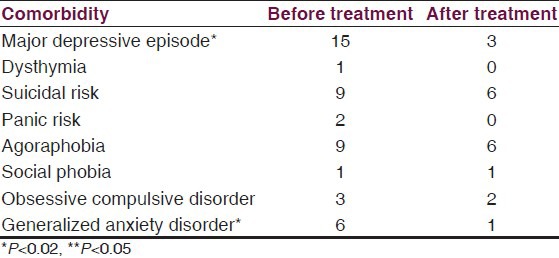
Patients with CM were treated with topiramate (100 mg/day) or divalproex Sodium ER (500 mg/day), while those having CTTH were given amitriptyline (25 mg/day). Fifty five patients came for follow up examination at 3 months. Twenty six patients had psychiatric co-morbidity on initial examination while it was present in only 12 patients on follow-up examination. Improvement in headache was seen in 29 patients. Improvement in headache was significantly more likely in those without psychiatric co-morbidity and a duration of headache of < 2 years. There was no relationship of improvement in headache with age, sex marital status, educational status and socioeconomic status [Figure 3]. Analysis of improvement with respect to type of psychiatric co-morbidity shows that patients with major depressive episode and generalized anxiety disorder show a significant improvement [Table 6]. There was also a significant decrease in medication use after treatment as compared to before treatment (Analgesic intake: Before treatment 5.2 ± 7.8 tablets/month; after treatment 2.9 ± 3.6 tablets/month, P = 0.017).
Figure 3.
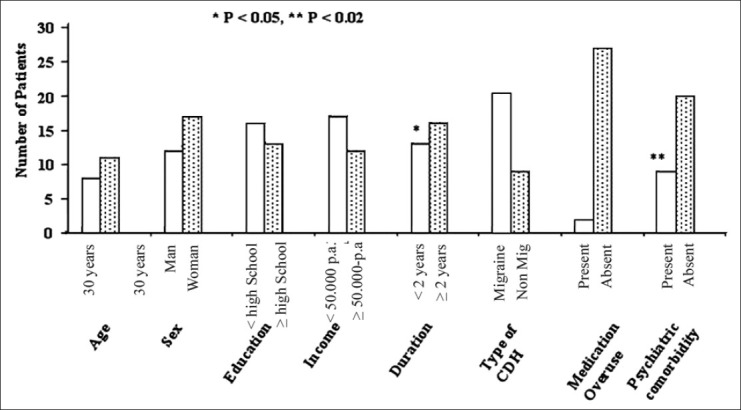
Histogram showing various clinical features and improvement in chronic dailyheadache. Univariate analysis shows that patients having CDH for ≥ two years* and presence of psychiatric co-morbidity** were associated with a significantly lower improvement (*P < 0.05 and **P < 0.02) respectively
Table 6.
Treatment response of psychiatric comorbidity
Discussion
The present prospective case control study done in the neurology OPD of a medical college hospital revealed that CDH accounted for 28% of all patients presenting with headache as the chief complaint. Our findings are similar to those reported in the West where the prevalence of CDH has been reported to vary from 30-40% of all patients visiting headache speciality clinics.[27] In contrast to this, Chakravarty in the only other study of patients with CDH from India found it to be responsible for 49.6% of all primary headaches.[25] The mean age of patients in the present study was 30.2 years and the ratio of women: Men were 2.29:1. This is comparable to other studies where the % of female patients has been reported to vary from 65-80%.[3,28] The mean age of patients in the study done by Chakravarty,[25] was 39 years and 80% of patients were women.[29]
Psychiatric co-morbidity was seen in 53.3% patients of CDH in the present study using the MINI scale for evaluation of patients. Chakravarty also found that CDH was associated with a psychiatric diagnosis in 50%, however no formal psychiatric evaluation was done in their study.[25] A recent community based study of adolescents with CDH in whom MINI-kid was used showed that 47% subjects had one or more psychiatric co-morbidity.[29] In the study by Juang et al., who also employed MINI for psychiatric evaluation 73% of patients with CDH have some psychiatric disorders.[3] On the other hand Verri, et al.,[4] found that psychiatric disorders were present in nearly 90% patients. CM was the commonest subtype of CDH, seen in 64% followed by CTTH in 23.9%. This is comparable to the figures reported by Juang et al.,[3] where 58% patients had transformed migraine and 35% had CTTH, whereas Chakravarty[25] had 82.4% patients with chronic/transformed migraine and 16.1% had CTTH.
Major depressive episode, generalized anxiety disorder, dysthymia and agoraphobia were the significant psychiatric co-morbidities observed in patients with CDH in the present study. There was no significant difference in the various types of psychiatric co-morbidities in patients having CM in comparison to CTTH. In the headache and anxiety depressive disorder co-morbidity: The HADAS study, where a naturalistic sample of pure migraine without aura and two control group of patients (pure tension-type headache and combined migraine and tension type headache) were evaluated, it was observed that the prevalence of depression and anxiety was to the same extent. The figures for depression in migraine (59.9%), tension-type headache (68.3%), combined migraine and tension-type headache (69.6%) and anxiety (migraine 18.4%, tension-type headache 19.3%, combined migraine and tension-type headache 18.4%) did not show a significant difference.[30] The frequency of depression found in the present study (34.8%) is similar to that observed by Verri, et al.,[4] (25 %), while Mathew et al.,[27] and Juang et al.,[3] observed it in 61% and 57% respectively. In 116 consecutive adult out patients with a diagnosis of CDH, De Fillipis et al.,[31] found that 28% had moderate to severe depression and 35% had severe hopelessness. Suicidal risk may play a central role in affecting quality of life of patients with chronic headache. Verri, et al.,[4] found an association between CDH and at least one psychiatric disorder in 90% of their cases, mainly generalized anxiety disorders in 69.3% cases, followed by major depression in 25% and dysthymia in 17%.[4] Juang et al.,[3] found that frequency of any type of anxiety disorder was significantly higher in patients with chronic migraine than in those with CTTH. Our figures of generalized anxiety disorder are similar to those observed by Juang et al.,[3] In contrast to our findings Chakravarty[25] reported anxiety and mood disorder to be more common (58.6%) than major depression (20.9%). In contrast to previous reports where psychiatric co-morbidity was high in women,[3,32] we did not find any significant relation between age, sex, duration of disease, educational status, socioeconomic status and marital status with the presence of psychiatric co-morbidity. Cardona castrillon, et al.,[33] evaluated patients aged 18-65 years with migraine according to IHS criteria using the hospital anxiety and depression scale, followed by semi-structured interview according to DSMD-IV, text revision and they observed major depression in 21.3%, dysthymic disorder 4.5%, panic disorders 5.6%, GAD 14.6%, PTSD 4.5%, social phobia 6.7%, specific phobia 5.6%, OCD 2.2%, and 19.1% had two mental disorders.
The commonest psychiatric co-morbidity in patients with CM seen in the present study was major depressive episode (40.68%). This is similar to the observations of Juang et al.,[3] (57%), Beghi, et al.,[30] (59.9%). On the other hand Chakravarty et al.,[25] and Cardona-Castrillon, et al.,[33] had lower figures 24.85% and 21.3% respectively. Breslau et al.,[34,35] have reported a bidirectional relationship between migraine and depression with migraine signaling an increased risk for the first onset of major depression, and major depression signaling an increased risk for the first time occurrence of migraine. The lifetime prevalence of major depression was threefold higher (hazard ratio 3.6) in persons with migraine and in persons with severe headache, compared with persons having no history of severe headache. Major depression was found in 40.7%of persons with migraine and 35.8% of those with other severe headaches. The suicidal risk seen in the present study was 22.03%, which is similar to the observations of Wang et al., (20%),[29] CDH subtypes, headache frequencies or medication overuse are not correlated with suicidal behavior.[29] Multiple somatic symptoms and longer duration (≥6 months) are particularly useful indicators of major depressive episode (age adjusted odds ratio: 3.1, 95% CI: 1.7-10.6 and 3.9, 95% CI: 1.2-8.1 respectively).[26]
Prevalence of panic disorder in our study was 5% in chronic migraine which is similar to Cardona-Castrillon, et al.,[33] study of 5.6%. In CTTH group none of the patients showed panic disorder. In study of E Beghi.[30] 12.7% of migraine, 5.5% TTH and 14.2% of combined migraine and tension-type headache patients had panic disorders. Obsessive compulsive disorders was found in 5.0% in chronic migraine, and 9.0% in CTTH patients in our study and E Beghi.[30] observed 2.3% in migraine, 1.1% in TTH, and 9.4% in combined migraine and tension-type headache. Migraine and other severe headaches were associated with an increased risk for first onset of panic disorder (hazard ratio of 3.55 and 5.75). Panic disorder was associated with an increased risk for first onset of other severe headaches, although the influences in this direction were lower (hazards ratio 2.10 and 1.85).[36]
Improvement in headache is more likely to occur in patients without a psychiatric co-morbidity and those with duration of headache less than 2 years. There was a significant decrease in major depressive episode and generalized anxiety disorder at 3 months follow up after appropriate treatment. Medication overuse was seen in only 4 patients in the present study whereas it has been reported to be present in 72%-91% in other studies.[34,37,38] Chakravarty,[25] reported analgesic over use in 28.4%, however they did not use the IHS criteria to define analgesic overuse. However, there was a significant decrease in the analgesic tablets taken per month from 5.2 ± 7.8-2.9 ± 3.6 after treatment at 3 months, so it is possible that medication overuse may have been underestimated due to recall bias in the present study. In another study from India, in which one thousand patients attending a headache clinic were analysed, medication overuse leading to headache was not found to be a major problem.[39] Guidetti V et al.,[7] studied the relationship between psychiatric disorders at initial evaluation and headache status at follow up and they found that patients with two or more psychiatric disorders at initial evaluation exhibited no improvement or deterioration in headache in 57% of the cases at follow up; 29% of cases were improved and only 14% cases were headache free.[7] In contrast patients with no or only one psychiatric disorder exhibited greater headache improvement 8 years after the initial evaluation. Only 15% of cases were the same or worse, while 53% of cases were improved and 40% cases were headache free.[7] Migraine and depression independently exert a significant negative influence on quality of life.[40]
A major drawback of the present study was the high dropout ratio (40.2%), small number of patients studied (92 patient) and short duration of follow-up (3 months). Chakravarty,[25] had commented on this problem of high dropout in their study where out of a patient sample of 849 cases seen over 2 years, follow up data at one year was available in only 205 patients (24.2%). Several reasons for this were given by them, such as people probably accept headache as a part of their life and do not take it as a serious malady, change of doctor/clinic for better treatment in those who do not get adequate benefit and recourse to alternative forms of therapy which are cheaper and easily available. The same may be true for the present study also.
Despite these shortcomings our findings are important in that they confirm the high prevalence of psychiatric co-morbidity in patients with CDH in a prospective case control cohort sample of consecutive patients, using an easily applicable bedside instrument. No significant difference was found in the psychiatric co-morbidities, in the two commonest types of primary headaches i.e., CM and CTTH. Thus our study shows that psychopathology is not the hallmark of a specific headache category rather it could be a reflection of the burden of disease. Both genetic and environmental factors as well as some common neurotransmitter dysfunction could be other contributing causes. The second aim of study comparing the efficacy of treatment between various types of headache associated with psychiatric co-morbidity remains as an explorative aspect which needs further studies involving larger patient population, and should be investigated in future studies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Castillo J, Munoz P, Guitera V, Pascual J. Epidemiology of chronic daily headache in the general population. Headache. 1999;39:190–6. doi: 10.1046/j.1526-4610.1999.3903190.x. [DOI] [PubMed] [Google Scholar]
- 2.Silberstein SD, Lipton RB. Chronic daily headache. Curr Opin Neurol. 2000;13:277–83. doi: 10.1097/00019052-200006000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Juang KD, Wang SJ, Fuh JL, Lu SR, Su TP. Co-morbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache. 2000;40:818–23. doi: 10.1046/j.1526-4610.2000.00148.x. [DOI] [PubMed] [Google Scholar]
- 4.Verri AP, Proletti Cecchini A, Galli C, Granella F, Sandrini G, Nappi G. Psychiatric co-morbidity in chronic daily headache. Cephalalgia. 1998;18:45–9. doi: 10.1177/0333102498018s2112. [DOI] [PubMed] [Google Scholar]
- 5.Mitsikostas DD, Thomas AM. Co-morbidity of headache and depressive disorders. Cephalalgia. 1999;19:211–7. doi: 10.1046/j.1468-2982.1999.019004211.x. [DOI] [PubMed] [Google Scholar]
- 6.Cerbo R, Prudenzano MP, Barbanti P. The importance of anxiety and depression as factors in chronicisation of primary headaches. J Headache Pain. 2000;1:S45–54. [Google Scholar]
- 7.Guidetti V, Galli F. Psychiatric co-morbidity in chronic daily headache: Pathophysiology, etiology, and diagnosis. Curr Pain Headache Rep. 2002;6:492–7. doi: 10.1007/s11916-002-0069-7. [DOI] [PubMed] [Google Scholar]
- 8.Torelli P, Lambru G, Manzoni GC. Psychiatric co-morbidity and headache: Clinical and therapeutic aspects. Neurol Sci. 2006;27:S73–6. doi: 10.1007/s10072-006-0574-2. [DOI] [PubMed] [Google Scholar]
- 9.Hamelsky SW, Lipton RB. Psychiatric co-morbidity of migraine. Headache. 2006;46:1327–33. doi: 10.1111/j.1526-4610.2006.00576.x. [DOI] [PubMed] [Google Scholar]
- 10.Heckman BD, Holroyd KA. Tension-type headache and psychiatric co-morbidity. Curr Pain Headache Rep. 2006;10:439–47. doi: 10.1007/s11916-006-0075-2. [DOI] [PubMed] [Google Scholar]
- 11.Ferrari MD, Odnik J, Tapparelli C, Van Kempen GM, Pennings EJ, Bruyn GW. Serotonin metabolism in migraine. Neurology. 1989;39:1239–42. doi: 10.1212/wnl.39.9.1239. [DOI] [PubMed] [Google Scholar]
- 12.Karakurum B, Soylu O, Karatas M, Giray S, Tan M, Arlier Z, et al. Personality, depression and anxiety as a risk factor for chronic migraine. Int J Neurosci. 2004;114:1391–9. doi: 10.1080/00207450490476002. [DOI] [PubMed] [Google Scholar]
- 13.Wang SJ, Juang KD. Psychiatric co-morbidity of chronic daily headache: Impact, treatment, outcome, and future studies. Curr Pain Headache Rep. 2002;6:505–10. doi: 10.1007/s11916-002-0071-0. [DOI] [PubMed] [Google Scholar]
- 14.Lake AE, 3rd, Rains JC, Penzien DB, Lipchik GL. Headache and psychiatric co-morbidity: Historical context, clinical implications, and research relevance. Headache. 2005;45:493–506. doi: 10.1111/j.1526-4610.2005.05101.x. [DOI] [PubMed] [Google Scholar]
- 15.Gentili C, Panicucci P, Guazzelli M. Psychiatric co-morbidity and chronicisation in primary headache. J Headache Pain. 2005;6:338–40. doi: 10.1007/s10194-005-0226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sandrini M, Vitale G, Pini LA, Sternieri E, Bertolini A. Effects of chronic treatment with phenazone on the hot-plate test and [3H] serotonin binding sites in pons and cortex membranes of the Rat. Pharmacology. 1993;47:84–90. doi: 10.1159/000139082. [DOI] [PubMed] [Google Scholar]
- 17.Fishbain DA. Approaches to treatment decisions for psychiatric co-morbidity in the management of the chronic pain patient. Med Clin North Am. 1999;83:737–60. doi: 10.1016/s0025-7125(05)70132-2. [DOI] [PubMed] [Google Scholar]
- 18.Katon WJ. Depression in patients with inflammatory bowel disease. J Clin Psychiatry. 1997;58:20–3. [Google Scholar]
- 19.Nisbett RE, Schachter S. Cognitive manipulation of Pain. J Exp Soc Psychol. 1966;2:227–36. [Google Scholar]
- 20.Rapoport NB, McAnulty DP, Waggoner CD, Brantley PJ. Cluster analysis of Minnesota Multiphasic Personality Inventory (MMPI) profiles in a chronic headache population. J Behav Med. 1987;10:49–60. doi: 10.1007/BF00845127. [DOI] [PubMed] [Google Scholar]
- 21.Holm JE, Penzien DB, Holroyd KA, Brown TA. Headache and depression: Confounding effects of trans-diagnostic symptoms. Headache. 1994;34:418–23. doi: 10.1111/j.1526-4610.1994.hed3407418.x. [DOI] [PubMed] [Google Scholar]
- 22.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (M.I.N.I.): The development and validatation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 23.Lecrubier Y, Sheehan D, Weiller E. The MINI International Neuropsychiatric Interview (M.I.N.I.): A short Diagnostic Structured Interview: Reliability and Validity according to the CIDI. Eur Psychiatry. 1997;12:224–31. [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Harneth-Sheehan K. Reliability and validity of the MINI International Neuropsychiatric Interview (M.I.N.I.): According to the SCID-P. Eur Psychiatry. 1997;12:232–41. [Google Scholar]
- 25.Chakravarty A. Chronic daily headaches: Clinical profile in Indian patients. Cephalalgia. 2003;23:348–53. doi: 10.1046/j.1468-2982.2003.00514.x. [DOI] [PubMed] [Google Scholar]
- 26.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. Cephalalgia. (2nd ed) 2004;24:9–160. [Google Scholar]
- 27.Mathew NT, Reuveni U, Perez F. Transformed or evolutive migraine. Headache. 1987;27:102–6. doi: 10.1111/j.1526-4610.1987.hed2702102.x. [DOI] [PubMed] [Google Scholar]
- 28.Bigal ME, Sheftell FD, Rapoport AM, Tepper SJ, Lipton RB. Chronic daily headache: Identification of factors associated with induction and transformation. Headache. 2002;42:575–81. doi: 10.1046/j.1526-4610.2002.02143.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang SJ, Juang KD, Fuh JL, Lu SR. Psychiatric comorbidity and suicide risk in adolescents with chronic daily headache. Neurology. 2007;68:1468–73. doi: 10.1212/01.wnl.0000260607.90634.d6. [DOI] [PubMed] [Google Scholar]
- 30.Beghi E, Allais G, Cortelli P, D’Amico D, De Simone R, d’Onofrio F, et al. Headache and anxiety depressive disorder comorbidity: The HADAS study. Neurol Sci. 2007;28:S217–9. doi: 10.1007/s10072-007-0780-6. [DOI] [PubMed] [Google Scholar]
- 31.De Flippis S, Erbuto D, Gentiti F, Innamorati M, Lester D, Tatarelli R, et al. Mental turmoil, suicide risk, illness perception and temperament, and there impact on quality of life in chronic daily headache. J Headache Pain. 2008;9:349–57. doi: 10.1007/s10194-008-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puca F. Psychopathological factors in chronic headache: An overview. J Headache Pain. 2000;1:S95–9. Supp l. [Google Scholar]
- 33.Cardona-Castrillon GP, Isaza R, Zapata-Soto AP, Franco JG, Gonzalez-Berrio C, Tamayo-Diaz CP. The comorbidity of major depressive disorder, dysthymic disorder and anxiety disorders with migraine. Rev Neurol. 2007;45:272–5. [PubMed] [Google Scholar]
- 34.Breslau N, Schultz LR, Stewart WF, Lipton RB, Lucia VC, Welch KM. Headache and major depression: Is the association specific to migraine? Neurology. 2000;54:308–13. doi: 10.1212/wnl.54.2.308. [DOI] [PubMed] [Google Scholar]
- 35.Breslau N, Schultz LR, Stewart WF, Lipton R, Welch KM. Headache types and panic disorder: Directionality and specificity. Neurology. 2001;56:350–4. doi: 10.1212/wnl.56.3.350. [DOI] [PubMed] [Google Scholar]
- 36.Breslau N, Davis GC, Andreski P. Migraine, psychiatric disorders, and sucide attempts. An epidemiological study of young adults. Psychiatry Res. 1991;37:11–23. doi: 10.1016/0165-1781(91)90102-u. [DOI] [PubMed] [Google Scholar]
- 37.Silberstein SD, Schulman EA, Hopkins MM. Repetitive intravenous DHE in the treatment of refractory headache. Headache. 1990;30:334–9. doi: 10.1111/j.1526-4610.1990.hed3006334.x. [DOI] [PubMed] [Google Scholar]
- 38.Konno S, Meyer JS, Margishvili GM, Rauch RA, Haque A. Transformed migraine is a cause of chronic daily headaches. Headache. 1999;39:95–100. doi: 10.1046/j.1526-4610.1999.3902095.x. [DOI] [PubMed] [Google Scholar]
- 39.Ravishanker K. Headache pattern in India: A headache clinic analysis of 1000 patients. Cephalalgia. 1997;17:316–31. [Google Scholar]
- 40.Lipton RB, Hamelsky SW, Kolodner KB, Steiner TJ, Stewart WF. Migraine, quality of life, and depression: A population-based case-control study. Neurology. 2000;55:629–35. doi: 10.1212/wnl.55.5.629. [DOI] [PubMed] [Google Scholar]


