Abstract
Colloid cyst in the third ventricle is a common entity, whereas a variant of it, namely xanthogranulomatous, is quite rare. The closest imaging differential diagnosis is a purely third ventricular craniopharyngioma. We herein describe a case of xanthogranulomatous colloid cyst presenting with hydrocephalus.
Keywords: Colloid cyst, third ventricle, xanthogranuloma
Introduction
Colloid cysts of the third ventricle are a common entity usually presenting with obstructive hydrocephalus. Imaging and microscopic findings of the colloid cysts have been clearly defined, with the imaging characteristics depending on the protein content and inspissations of the contents to the formation of calcium stones. The colloid contents are proteinaceous, amorphous, and acellular. Microscopically, it is cystic and lined by a single or a multilayered ciliated, cuboidal epithelium.[1] Occasionally, the epithelial lining becomes more complex, composed of several layers and lacking cilia[2] and very rarely it is associated with a “xanthogranuloma.”[3]
Case Report
A 30-year-old male presented with complaints of holocranial headache with transient episodes of blurring of vision for 1 month. His neurological examination was normal. Fundoscopy revealed bilateral florid papilledema.
He was investigated with MRI brain, which revealed a hyperintense (T1W and T2W) solid cystic lesion measuring 3 × 2.9 × 3 cm3 in the anterior third ventricle causing hydrocephalus with enhancement on contrast imaging. The solid portion was hypointense on T2W images and was nonenhancing on T1W-Gadolinium contrast images [Figure 1a-c]. The imaging differential diagnosis was colloid cyst with inspissated protein contents or craniopharyngioma.
Figure 1.
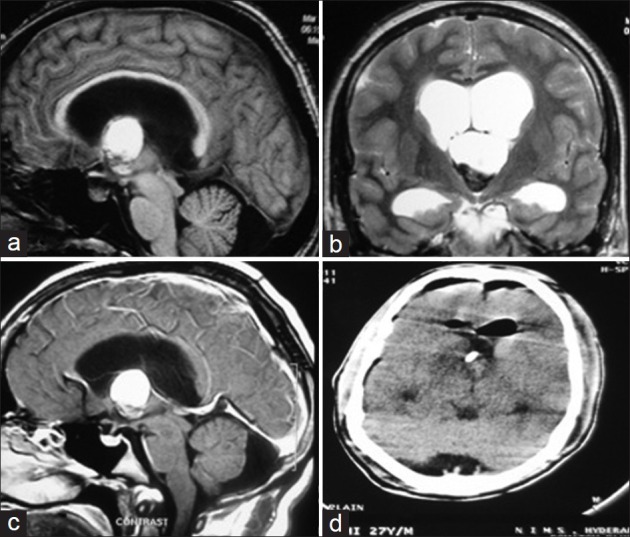
MRI T1W sagittal (a), T2W coronal (b), T1 contrast sagittal (c) images showing a solid cystic third ventricular lesion hyper on T1W and T2W images with hypointense solid portion and no enhancement on contrast (d) Post-operative CT scan demonstrating the complete excision of the lesion with the catheter tip in the third ventricle
The patient underwent right frontal craniotomy, and the lesion was approached through interhemispheric transcallosal interforniceal route as the lesion was large and would have been difficult to excise from transforaminal variation of the transcallosal approach. The lesion was solid cystic located in the third ventricle near the foramen of Monro and contained about 2-3 mL of machine oil like fluid which was drained. The solid part of the lesion was avascular, firm, and grayish black in color which was excised. The capsule was removed completely except for the part which was densely adherent to the floor of the third ventricle. An Ommaya reservoir was kept in the third ventricle for external ventricular drainage [Figure 1d]. The external drain was removed on postoperative day 5, and a CT scan was repeated on day 7 to look for the residual blood in the ventricles. There was dilatation of the ventricles with periventricular lucency for which a right ventriculo-peritoneal shunt was performed. There was no residual tumor left in the third ventricle.
Histopathological examination of excised specimen revealed all the typical diagnostic features of a colloid cyst except for certain parts of the cyst wall where the simple, compressed, ciliated, cuboidal lining lacked a brush border and was sometimes entirely missing. Moreover, the cyst wall was multilayered and thickened by granulomatous tissue which was composed of a potpourri of cells. There was a predominance of epithelioid cells and macrophages, many of which contained refractile material and hemosiderin. Polymorphonuclear leukocytes were diffusely scattered throughout the granuloma, and lymphocytes were seen in focal collections. Foreign body giant cells were not a conspicuous feature. Cholesterol clefts were also noted [Figure 2a-d].
Figure 2.
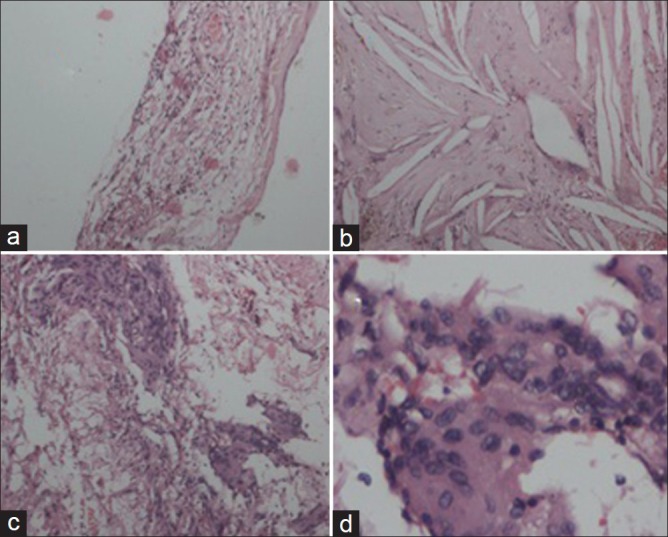
Histopathological sections (a) cyst wall lined by a single layer of cuboidal cells with underlying eosinophilic, homogenous colloid, and xanthogranulomatous reaction (hematoxylin and eosin stain [H and E], ×100); (b) colloid contents cross-hatched by cholesterol clefts (H and E, ×400); (c) magnified view of granulomatous reaction showing giant cells, scattered lymphocytes admixed with neuropil material (H and E, ×200); and (d) high power view showing multinucleated giant cells (H and E, ×400)
The patient is under regular follow-up and doing well with no fresh neurological deficits at end of 1 year.
Discussion
Colloid cysts represent 0.5-1% of intracranial neoplasms and 55% of third ventricular lesions.[4,5,6] These benign neoplasms are usually located in the anterior third ventricles and are usually detected following obstruction of foramina of Monro[4,6] with features of raised intracranial pressure or sudden drop attacks due to intermittent cerebrospinal fluid pathway obstruction. It may also present as memory disturbance due to forniceal compression or positional headache in minority of patients.[4,7,8] Seizures and recurrent aseptic meningitis are exceptional.[9,10] Wang et al. reported a case of colloid cyst in the fourth ventricle with two episodes of aseptic meningitis, managed by subtotal excision and repeated lumbar punctures.[11] Webb et al. reported acute vasospasm involving all the four major vessels following transcallosal excision of a xanthogranulomatous colloid cyst and attributed it to chemical meningitis due to spillage of cyst contents akin to inflammatory reaction to craniopharyngioma fluid.[12]
Their tissue derivation is debated, but their congenital nature is generally accepted.[1,13,14,15,16] Possible sources for these tumors include the choroid plexus,[3] ependyma,[13] primitive neuroectoderm,[14] and primitive endoderm,[15,16] whereas ultrastructural and immunohistochemical evidence argues against a simple choroid plexus or ependymal origin.[1,13,14,15] Microscopically, the tumors are often described as being cystic and lined by a single-or a multilayered ciliated, cuboidal epithelium. Very rarely, xanthogranulomas such as cholesterol crystal clefts, foreign-body giant cells, foamy cells, and inflammatory infiltrates of varying degree are seen in the wall of colloid cyst.[3,17,18]
According to Shuangshoti et al.,[3] the xanthogranulomatous reaction associated with the colloid cyst may be due to desquamation of the lining epithelium and accumulation of lipid in the detached cells as they degenerate. The lipids are released from the disintegrating cells producing a xanthogranulomatous response in the denuded stroma. They also postulated that the lining cells could serve as fixed histiocytes which could become wandering macrophages (granulomatous cells) after detachment. Other probable theories being hemorrhage and cyst rupture with colloid material inciting a granulomatous reaction.[17]
Colloid cysts are hyperdense in two-third of cases and iso to-hypodense in one-third of cases, and density has been described to depending upon the cholesterol content of the lesion.[5,19] It usually does not enhance on contrast except for occasional rim enhancement. The predominance of cholesterol content in the cyst gives the colloid cyst its characteristic MR appearance of being hyperintense on T1 and iso-to hypo intense on the T2 weighted images. Marshman et al.[20] suggested that xanthogranulomatous change in a colloid cyst could result in decreased cyst radiodensity. However, other case reports suggest that as xanthogranulomas have different CT densities in different patients, varying from hyper to hypodense with no enhancement on contrast with perilesional enhancement in few patients, it may not be possible to distinguish them radiographically from the colloid cyst.[9] Similar limitation has been expressed for MRI also.[21,22] Intraventricular glioma, ependymoma, craniopharyngioma, and small dermoid should be considered in the differential diagnosis.[9]
Surgery is the treatment of choice, which can be accomplished either by endoscopic or microscopic techniques as per the expertise of the operating surgeon. We operated through interhemispheric, transcallosal, interforniceal variation as described by Apuzzo et al., for large lesions in the anterior third ventricle region.[23] Although the interforniceal approach carries the risk of memory impairment due to injury to fornices, it allows access to the middle and posterior parts of the third ventricle. The transcortical approach is associated with the risk of postoperative seizures and deterioration thereof. As compared to the plain colloid cyst these lesions are difficult to excise in toto as the inflammatory reaction to the xanthomatous material leads to adhesions, and thence difficult total excision.[24,25] We were able to excise the cyst near totally except for the small part densely adherent to the floor of third ventricle. Kudesia et al., reported iatrogenic aseptic meningitis in the postoperative period in their case, attributing it to spillage of cyst contents.[25]
Histopathologically, it may be confused with a ruptured epidermoid cyst,[1] a degenerated choroid plexus,[26,27,28] or a choroid plexus papilloma with xanthomatous changes.[2,29]
Conclusion
Xanthomatous degeneration of the colloid cyst must be kept as a differential diagnosis in purely third ventricular solid-cystic lesions. Colloid cysts with xanthomatous changes are usually adherent to the walls of the ventricle, and it is advisable to aspirate cyst contents without spillage and achieve safe maximal resection of cyst wall.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Russell DS, Rubinstein LJ. Pathology of tumors the nervous system.4 th ed. Baltimore: Williams and Wilkins; 7 Pathology of tumors the nervous system 4 th ed Baltimore: Williams and Wilkins; 1977 p 225-6. [Google Scholar]
- 2.Zeitlin H, Lichtenstein BW. Cystic tumor of the third ventricle containing colloid material. Arch Neurol Psychiatry. 1937;38:268. [Google Scholar]
- 3.Shuangshoti S, Phonprasert C, Suwanwela N, Netsky MG. Combined neuroepithelial (colloid) cyst and xanthogranuloma (xanthoma) in the third ventricle. Neurology. 1975;25:547–52. doi: 10.1212/wnl.25.6.547. [DOI] [PubMed] [Google Scholar]
- 4.Antunes JL, Louis KM, Ganti SR. Colloid cysts of third ventricle. Neurosurgery. 1980;7:450–5. doi: 10.1227/00006123-198011000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Desai KI, Nadkarni TD, Muzumdar DP, Goel AH. Surgical management of colloid cyst of the third ventricle-a study of 105 cases. Surg Neurol. 2002;57:295–304. doi: 10.1016/s0090-3019(02)00701-2. [DOI] [PubMed] [Google Scholar]
- 6.de Witt Hamer PC, Verstegen MJ, De Haan RJ, Vandertop WP, Thomeer RT, Mooij JJ, et al. , High risk of acute deterioration in patients harboring symptomatic colloid cysts of the third ventricle. J Neurosurg. 2002;96:1041–5. doi: 10.3171/jns.2002.96.6.1041. [DOI] [PubMed] [Google Scholar]
- 7.Camacho A, Abernathey CD, Kelly PJ, Laws ER Jr. Colloid cysts: Experience with the management of 84 cases since the introduction of computed tomography. Neurosurgery. 1989;24:693–700. doi: 10.1227/00006123-198905000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Fritsch H. Colloid cysts-a review including 19 own cases. Neurosurg Rev. 1988;11:159–66. doi: 10.1007/BF01794682. [DOI] [PubMed] [Google Scholar]
- 9.Montaldi S, Deruaz JP, Cai ZT, de Tribolet N. Symptomatic xanthogranuloma of the third ventricle: Report of two cases and review of the literature. Surg Neurol. 1989;32:200–5. doi: 10.1016/0090-3019(89)90179-1. [DOI] [PubMed] [Google Scholar]
- 10.Terao H, Kobayashi S, Teraoka A, Okeda R. Xanthogranulomas of the choroid plexus in a neuro-epileptic child.Case report. J Neurosurg. 1978;48:649–53. doi: 10.3171/jns.1978.48.4.0649. [DOI] [PubMed] [Google Scholar]
- 11.Wang Z, Yan H, Wang D, Wang S, Liu R, Zhang Y. A colloid cyst in the fourth ventricle complicated with aseptic meningitis: A case report. Clin Neurol Neurosurg. 2012;114:1095–8. doi: 10.1016/j.clineuro.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Webb AJ, Gillies MJ, Cadoux-Hudson TA. Acute vasospasm following transcallosal resection of a xanthogranulomatous colloid cyst of the 3 rd ventricle. Clin Neurol Neurosurg. 2010;112:512–5. doi: 10.1016/j.clineuro.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Coxe WS, Luse SA. Colloid cyst of third ventricle.An electron microscopic study. J Neuropathol Exp Neurol. 1964;23:431–45. doi: 10.1097/00005072-196407000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Kondziolka D, Bilbao JM. An immunohistochemical study of neuroepithelial (colloid) cysts. J Neurosurg. 1989;71:91–7. doi: 10.3171/jns.1989.71.1.0091. [DOI] [PubMed] [Google Scholar]
- 15.Lach B, Scheithauer BW, Gregor A, Wick MR. Colloid cyst of the third ventricle.A comparative immunohistochemical study of neuraxis cysts and choroid plexus epithelium. J Neurosurg. 1993;78:101–11. doi: 10.3171/jns.1993.78.1.0101. [DOI] [PubMed] [Google Scholar]
- 16.Mackenzie IR, Gilbert JJ. Cysts of the neuraxis of endodermal origin. J Neurol Neurosurg Psychiatry. 1991;54:572–5. doi: 10.1136/jnnp.54.7.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadfield MG, Ghatak NR, Wanger GP. Xanthogranulomatous colloid cyst of the third ventricle. Acta Neuropathol. 1985;66:343–6. doi: 10.1007/BF00690969. [DOI] [PubMed] [Google Scholar]
- 18.Matsushima T, Fukui M, Kitamura K, Soejima T, Ohta M, Okano H. Mixed colloid cyst-xanthogranuloma of the third ventricle.A light and electron microscopic study. Surg Neurol. 1985;24:457–62. doi: 10.1016/0090-3019(85)90308-8. [DOI] [PubMed] [Google Scholar]
- 19.Kachhara R, Das K, Nair S, Gupta AK. Changing characteristics of a colloid cyst of the third ventricle. Neuroradiology. 1999;41:188–9. doi: 10.1007/s002340050731. [DOI] [PubMed] [Google Scholar]
- 20.Marshman LA, Chawda SJ, David KM. Change in CT radiodensity of a colloid cyst of the third ventricle: Case report and literature review. Neuroradiology. 2004;46:984–7. doi: 10.1007/s00234-004-1303-2. [DOI] [PubMed] [Google Scholar]
- 21.Tatter SB, Ogilvy CS, Golden JA, Ojemann RG, Louis DN. Third ventricular xanthogranulomas clinically and radiologically mimicking colloid cysts.report of two cases. J Neurosurg. 1994;81:605–9. doi: 10.3171/jns.1994.81.4.0605. [DOI] [PubMed] [Google Scholar]
- 22.Wiot JG, Lukin RR, Tomsick TA. Xanthogranuloma of the third ventricle. AJNR Am J Neuroradiol. 1989;10:S57. [PMC free article] [PubMed] [Google Scholar]
- 23.Apuzzo ML, Gianotta SL. Transcallosal interforniceal approach.In: Apuzzo ML, editor. Surgery of Third Ventricle. Transcallosal interforniceal approach In: Apuzzo ML, editor Surgery of Third Ventricle Baltimore, MD: Williams and Wilkins; 1987 p 354-80. [Google Scholar]
- 24.Ayres WW, Haymaker W. Xanthoma and cholesterol granuloma of the choroid plexus.Report of the pathological aspects in 29 cases. J Neuropathol Exp Neurol. 1960;19:280–95. doi: 10.1097/00005072-196004000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Kudesia S, Das S, Shankar SK, Santosh V, Reddy AK. Colloid cyst xanthogranuloma of the third ventricle-a case report. Indian J Pathol Microbiol. 1996;39:221–3. [PubMed] [Google Scholar]
- 26.Dunn J Jr, Kernohan JW. Histologic changes within the choroid plexus of the lateral ventricle: Their relation to age. Proc Staff Meet Mayo Clin. 1955;30:607–16. [PubMed] [Google Scholar]
- 27.Shuangshoti S, Netsky MG. Human choroid plexus Morphologic and histochemical alterations with age. Am J Anat. 1970;128:73–95. doi: 10.1002/aja.1001280107. [DOI] [PubMed] [Google Scholar]
- 28.Shuangshoti S, Netsky MG. Xanthogranuloma (xanthoma) of choroid plexus.The origin of foamy (xanthoma) cells. Am J Pathol. 1966;48:503–33. [PMC free article] [PubMed] [Google Scholar]
- 29.Szper I, Oi S, Leestma J, Kim KS, Wetzel NE. Xanthogranuloma of the third ventricle.Case report. J Neurosurg. 1979;51:565–8. doi: 10.3171/jns.1979.51.4.0565. [DOI] [PubMed] [Google Scholar]


