Abstract
To identify challenges encountered in the care of children with special health care needs in a resource limited environment a 10 year-old child with a diagnosis of Tuberous Sclerosis was studied. Challenges identified were in: making a definitive diagnosis, provision of adequate care, cost of care, meeting parental expectations and accessing community support for the child and family. Available specialist health care and related services, including community rehabilitation, were provided for the child and family. The study highlights the need for improved community awareness, development in the provision of specialist health care services and institution of governmental policies that identify, support and protect children with special health care needs.
Keywords: Care, challenges, tuberous sclerosis
Introduction
The care of children with special health care needs (CSHCN), children who have or are at risk of a chronic disorder which requires more than usual health and related services, is becoming a significant public health issue.[1] Tuberous Sclerosis is an exemplary condition. This is a neuro-cutaneous disorder inherited as an autosomal dominant trait with variable penetrance and a prevalence of 1/6000 people.[2] In Africa the first case was reported in 1967 and from then there has been case reports from West, East and North Africa.[3] Tuberous Sclerosis is characterized by adenoma sebaceum, intractable seizures, mental retardation, cognitive and behavioral abnormalities that warrant long-term special health care services is an exemplary disorder.[2] There are challenges in providing care for these children which could be overwhelming.[1,2,3,4] The aim of this study was to identify challenges of care in CSHCN using a child with Tuberous Sclerosis in a resource limited environment.
Case Report
We present a 10 year old male, who presented with a history of recurrent seizures and impaired speech development from the age of 6 months, hyperactivity, aggressive behavior and poor academic performance of 5 years duration. Informant was the mother. The seizures were described as afebrile and generalized tonic-clonic in nature. The child received several medications, from the hospital of his birth and other secondary health care facilities, for the seizures. Parents introduced traditional herbal oral medication at 2 years when seizures remained intractable, and which he continued till presentation at the CAMH unit. Speech has remained audible but incomprehensible since the 6th month of life till date and has not received any specific therapy for this. Though described as socially interactive with people he was observed to be hyperactive and aggressive in the past 5 years. These features, in addition to the recurrent seizures even in school had resulted in poor academic performance. Persistent complaints and rejection by schools culminated in complete withdrawal from school. Pregnancy and delivery were uneventful. Developmental motor milestones were described as normal until the 9th month of life when parents observed comparative weakness in the left upper and lower limbs. He started walking with a limp at 2 years. He developed a facial rash at 5 years which has increased in spread and defied repeated administration of a variety of topical skin creams. He was first diagnosed as having cerebral palsy at 2 years. It was at 5 years of age that a diagnosis of Tuberous Sclerosis was made in a tertiary health facility. After 2 years of several visits to this facility, the parents stopped attending due to lack of significant improvement in the child's condition and non availability of the special health services such as speech therapy. Currently he is at home and away from school. He is being tendered to by his mother, who had to relinquish her career pursuit, and two hired house helps. There was no family history of seizures. Father is a 37 year old salesman. The child has two younger siblings who have no growth or developmental challenges. Expenses incurred in the care of child were described as prohibitive and have been borne exclusively by the parents. On a monthly basis, his care is said to consume over a third of the family resources. Parents are not aware of any support group or supportive governmental program they can access. Increasing inappropriate hostility towards parents, relatives and other caregivers in addition to the associated difficulty in restraining him and the embarrassment the parents feel from his untoward activities informed his presentation to the CAMH Unit. On examination at presentation he was hyperactive but well kempt. He had Adenoma Sebaceum [Figure 1]. Weight, height and occipito- frontal circumference were appropriate for age. Other significant findings were expressive language disorder and left hemiplegia. Chest x-ray, abdominal ultra sonography and audiogram were normal. Electroencephalogram (EEG) indicated generalized tonic clonic-seizures. A CT-Scan showed intra-ventricular subependymal calcifications [Figure 2]. He had features of Attention Deficit Hyperactivity Disorder (ADHD). Outcome of draw-a-person test was very poor. Overall, a diagnosis of Tuberous Sclerosis with mental retardation, left hemiplegia and ADHD was made. Outlined management included parental counseling, physiotherapy for the hemiplegia, sodium valproate and methyl phenidate were prescribed for seizures and ADHD respectively. The frequency of the seizures and the degree of hyperactivity reduced with commencement of the drugs. The child and parents were subsequently introduced to a special education and rehabilitation facility in the community.
Figure 1.

Adenoma sebaceum and fibrous plaques
Figure 2.
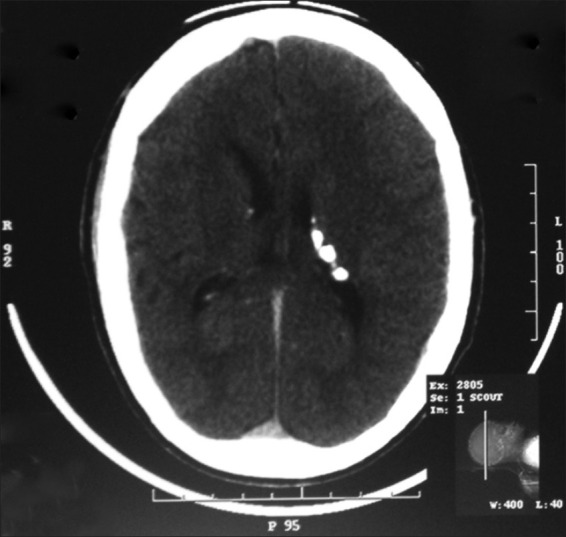
Intra-ventricular subependymal calcifications
Discussion
It took 5 years before a conclusive diagnosis of Tuberous Sclerosis was made in this child. Ogunrin in Midwestern Nigeria reported that diagnosis was made in a girl at 13 years.[3] This delay has been attributed to the uncommon nature of the disorder and its plethora of clinical features. This is not peculiar to Tuberous Sclerosis in our environment. In two cases of muscular dystrophy reported in Northern Nigeria the diagnosis was made at 8 and 10 years of age respectively.[4] Early diagnosis thus requires a high index of suspicion, articulation of presenting features, availability and utilization of appropriate facilities for investigations.[3] Consequences of delayed diagnosis such as itinerant shopping for remedy, clinical deterioration and exposure to the risks of unorthodox medication were all observed in this child.
Care was limited to that provided by parents. Special health care and related services such as that provided by occupational therapists, speech therapists, clinical psychologists and special educationists were either not available or not accessed by the parents. Furthermore all expenses incurred in the care of the child were borne by parents alone. The burdensome nature of care even among very caring parents or caregivers could lead to suboptimal care and generally reduced capacity of caregiver to provide more care and meet other obligations.
The expectations of parents or caregivers of CSHCN could be very idealistic and compounded by the inability to provide a definitive diagnosis, appropriate counseling or special health services as observed in this study. It resulted in the use of multiple health care options and non compliance with instituted management in this study. Community based rehabilitation has been noted to play a significant role in optimizing care of CSHCN.[5] Community or governmental support was lacking in the care of this child. For these children providing support in or through schools is an important aspect of community support. Negative attitude towards children with seizures and in schools have been reported in the country.[6] This could have contributed to school rejection in this case. The overall implication would include child isolation, susceptibility to abuse or neglect by over burdened parents and being stigmatized or discriminated against. Absence or non implementation of governmental policies geared towards special needs, lack of awareness on CSHCN or basic management skills in community and not knowing where to source for such support by parents are some of the factors that could also contribute to non communal participation.
The identified challenges could be addressed through: Development of a national registry, for CSHCN, which has been noted to facilitate formulation and implementation of relevant policies,[7] sensitization of child health care providers, improved availability of rehabilitative and support services, and promoting community awareness.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Goldson E, Louch G, Washington K, Sheu H. Guidelines for the care of the child with special health care needs. Adv Pediatr. 2006;53:165–82. doi: 10.1016/j.yapd.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Haslan RH. WB Saunders: Philadelphia; 2007. Nelson textbook of Pediatrics; pp. 2485–7. [Google Scholar]
- 3.Ogunrin OA. Misdiagnosis of tuberous sclerosis in a Nigerian girl: A case report and review of literature. Ann Afr Med. 2010;9:95–101. doi: 10.4103/1596-3519.64754. [DOI] [PubMed] [Google Scholar]
- 4.Eseigbe EE, Anyiam JO, Wammanda RD. Care of the Child with Special Health Care Needs: A report on 2 Nigerian children with muscular dystrophy. Ann Nigerian Med. 2006;2:29–31. [Google Scholar]
- 5.Brewer EJ, McPherson M, Magrab PR, Hutchings VL. Family-centered, community based, coordinated care for children with special health care needs. Pediatrics. 1989;83:1055–9. [PubMed] [Google Scholar]
- 6.Ojinnaka NC. Teachers’ perception of epilepsy in Nigeria: A community-based study. Seizure. 2002;11:386–91. doi: 10.1053/seiz.2001.0664. [DOI] [PubMed] [Google Scholar]
- 7.Chitambira B. Importance of preliminary epidemiology studies in rural areas of developing countries. J Neurosci Rural Pract. 2012;3:2–3. doi: 10.4103/0976-3147.91920. [DOI] [PMC free article] [PubMed] [Google Scholar]


