Abstract
A 59-year-old man was found on the road with multiple injuries. CT scan showed a hypodense extra axial lesion in the left fronto-temporal region suggestive of chronic subdural haematoma. He was treated conservatively but did not improve. He underwent craniectomy after lesion was shown to be increasing in size, only solid tissue was seen which was not biopsied. Patient made good recovery after steroids were put on. He deteriorated again 6 weeks later and radiology showed the frontal lesion without involvement of the brain and with minimal enhancement and mass effect. He underwent biopsy decompression of the lesion with steroids, post-operatively he improved well, but deteriorated when the steroids were tapered. Histopathology report was Non-Hodgkin's lymphoma. No primary was found and the patient died during oncology treatment. This illustrates manifestation of primary dural lymphoma radiologically mimicking chronic subdural haematoma, another common disorder.
Keywords: Chronic subdural haematoma, extra-axial hypodense lesion, lymphoma
Introduction
Primary central nervous system lymphoma (PCNSL) is an uncommon tumour representing 1-2% of all primary brain tumours and the incidence seems to be increasing.[1,2,3] Lymphoma arising from the meninges without involvement of the brain and other systemic involvement is rarer still. Lechance, et al.,[4] reported this as about 7% of all PCNSL.
This is the report of a patient with radiological picture suggestive of a chronic subdural haematoma but the final diagnosis was a primary leptomeningeal non-Hodgkin's lymphoma. Primary leptomeningeal lymphoma can mimic many extra-axial lesions and the aim of this report is to bring out another of the manifestation of the disease, hitherto not described.
Case Report
A 59-year-old man was found lying on the road with multiple facial and scalp lacerations well past midnight. He was assumed to have been involved in a road traffic accident and taken to hospital. At admission he was drowsy, disoriented but obeying verbal commands with a Glasgow coma scale (GCS) of E3V4M6. Computed tomography (CT) scan showed a thin hypo-dense extra-axial lesion in the left frontal region without mass effect and midline shift [Figure 1]. Patient was treated conservatively but was slowly deteriorating. A repeat CT scan [Figure 2] showed some increase in the size of the hypodense lesion, so the attending surgeon decided to perform a frontoparietal craniectomy. During surgery no haematoma was seen but reddish thick fleshy tissue was seen. The trainee surgeon who operated unfortunately closed the incision without obtaining any biopsy. As there was no improvement, patient was taken to another centre where he was treated conservatively including steroids. The patient slowly improved, he was discharged, the steroids were made oral and tapered over one month.
Figure 1.
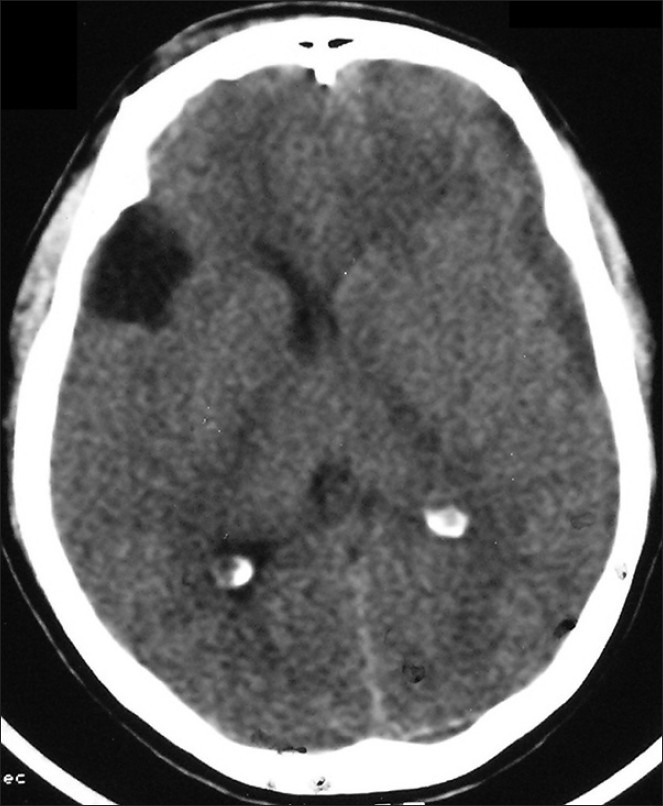
Computed tomography done at first admission showing the thin hypodense extraaxial lesion
Figure 2.
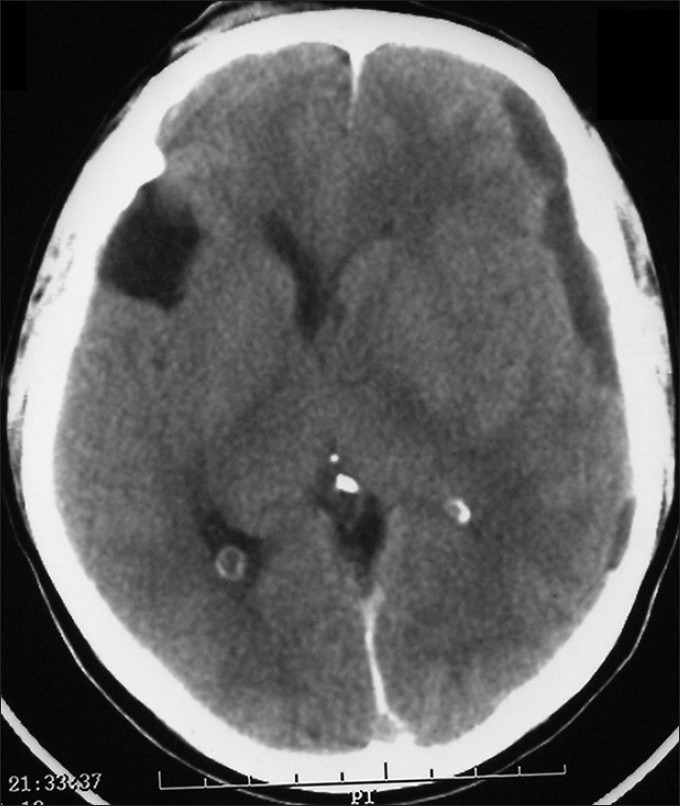
CT scan repeated after a week showing increase in size of lesion and mass effect/midline shift
The patient was brought to our centre, six weeks later with spikes of high fever. During inter-rogation it was understood that the patient has been slowly deteriorating a few days after discharge. At admission he was febrile, drowsy, GCS E2V2M5. CT scan showed a hypodense extra-axial lesion in the left fronto-temporal region with mass effect and midline shift [Figure 3] with some enhancement on contrast CT. An incidental type 1 sylvian arachnoid cyst was also noticed on the right side. Magnetic resonance imaging (MRI) showed an isodense to hypo-dense lesion extra-axial lesion with a rim of cerebrospinal fluid (CSF) below [Figures 4 and 5]. The brain was seen fungating through the craniectomy site. An enplaque meningioma or an organized subdural haematoma was considered and surgery was planned.
Figure 3.

Precraniotomy CT showing the hypodense lesion with some enhancement and mass effect
Figure 4.
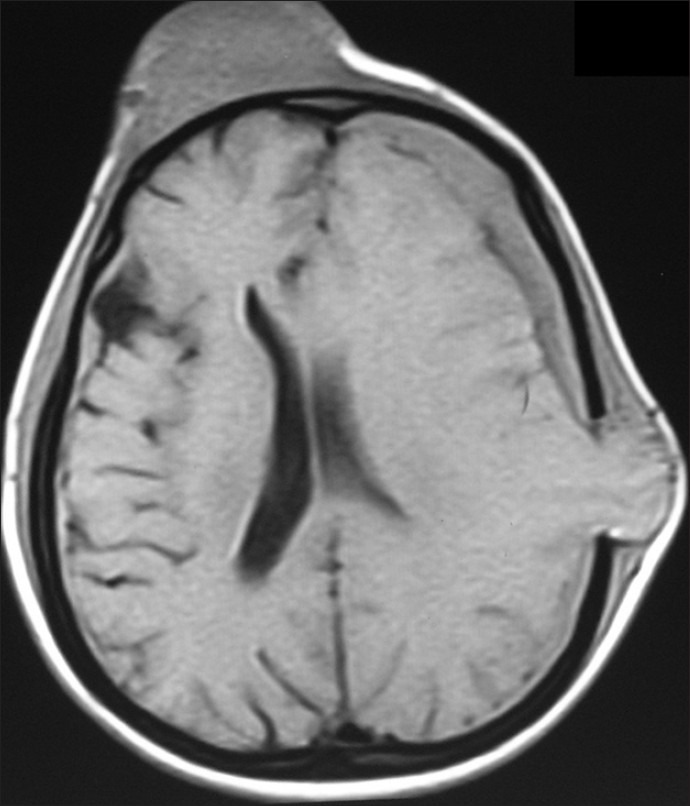
Precraniotomy MRI T1WI showing the isodense lesion with brain fungus. The brain parenchyma is normal
Figure 5.
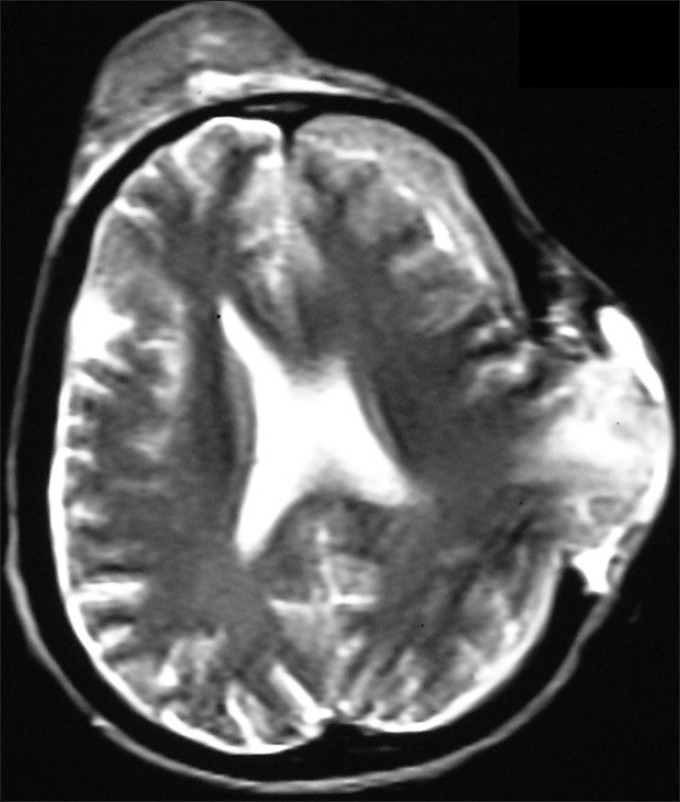
Precraniotomy MRI T2WI showing the isodense lesion with brain fungus. The brain parenchyma is normal. There is a thin layer of CSF between the brain and the lesion
Patient underwent left front otemperoparietal craniotomy, during surgery there was a reddish fleshy vascular lesion just under the bone flap. Biopsy de-compression of the lesion was done. Patient was continued on steroids and improved dramatically only to deteriorate with features of increased intra-cranial pressure and papilloedema when steroids were tapered. The histo-pathology was Non-Hodgkin's lymphoma. Immuno histo-chemistry stains were positive for Cytokeratin and Leucocyte Common Antigen. The B-cell markers CD20 and CD79a were positive. Glial fibrillary acidic protein (GFAP) and Vimentin stains were negative. The Ki67 index was 8-10%. The blastic markers CD99 and Tdt were positive in focal areas. Biopsy obtained from brain tissue was reported normal. An extensive search for the primary including detailed clinical assessment, CT scans of abdomen and chest and bone marrow analysis were done but all these were negative. Immune status compromise and HIV were ruled out. The patient was referred to the oncologist but unfortunately deteriorated and died without the radio-therapy being completed.
When the patient was with us he had a small swelling in the forehead which was reddish and firm and was attributed to the fall he had just before admission. During craniotomy a biopsy was taken from this site also and was suggestive of Non-Hodgkin's lymphoma.
Discussion
Subdural Haematoma is the commonest hypo-dense extra-axial lesions in the brain and the radio-logical features of chronic subdural haematoma are well described.[5] There have been many reports of metastatic disease mimicking subdural haematomas. Similarly some articles have described how primary leptomeningeal diseases have been diagnosed as subdural haematomas. Goetz, et al.,[6] described one patient with an extra-axial lesion diagnosed as acute subdural haematoma on CT scan. This patient had a good recovery with a resolution of the lesion with short course of steroids but had recurrence of symptoms on stopping steroids. Histology showed that the lesion was a lymphoma. They also looked at seven previous cases which were histological surprises, all were diagnosed as meningioma or subdural haematoma but turned out to be dural lymphomas. Reyes and co-workers,[7] reported one patient who was diagnosed as encapsulated subdural haematoma but at surgery the patient turned out to be having malignant lymphoma. Matano[8] also presented a case of leptomeningeal lymphoma complicated with subdural haematoma. Altundag et al.,[9] presented a lady with syncope and seizures. Her CT scan was suggestive of a subdural effusion. Histo-pathology of the solid dural lesion was lymphoma. There have also been reports of this tumour mimicking a meningioma.[6,10,11]
Lechance et al.,[4] reported nine cases with neoplastic meningitis but no brain parenchymal or systemic disease was ever identified. They coined the term primary leptomeningeal lymphoma for this entity. Kumar et al.,[12] described the clinico-pathological features of five cases of primary dural lymphomas. They had also brought out the importance of clinical and pathological correlation in these situations. They concluded that low-grade B-cell lymphomas arising in the intra-cranial dura are rare but appear to be similar to other low-grade B-cell lymphomas arising in extra-nodal sites in terms of clinical presentation with an indolent behavior and favorable response to treatment, suggesting that they may be part of the mucosa associated lymphoid tissue (MALT) lymphoma spectrum. They appear to arise at dural sites where meningothelial cells are concentrated. Kambham and co-workers[13] added two cases to those reported by Kumar et al. They stressed that it is important that this entity be recognized and distinguished from other small B-cell non-Hodgkin's lymphomas since localized low grade MALT lymphomas are usually clinically indolent proliferations which may require only minimally aggressive therapy. Iwamoto, DeAngelis and Abrey[14] pointed out that standardized treatment was not available due to paucity of these cases. They suggested surgical resection of these tumours followed by radiotherapy as these tumours are very radiosensitive. They also opined that even though these lesions are indolent, the risk of systemic recurrence was high.
Iwamoto and Abrey[15] reviewed primary dural lymphomas and suggested that primary dural lymphoma arises from the dura mater and differs bio-logically from other CNS lymphomas. It is usually a low-grade B-cell Marginal zone lymphoma (MZBCL), whereas other types of Primary CNS lymphomas (PCNSL) are usually high grade malignancies. The disease occurs more in females. The pathogenesis of periodontal ligament (PDL) is not well understood because the dura is devoid of any lymphoid tissue. One hypothesis is that a benign inflammatory condition of the dura could attract polyclonal lymphocytes from which a monoclonal lymphoma could arise. They reported that the most important differential diagnosis is meningioma and the most frequent histo-pathological diagnosis is marginal zone lymphoma (MZL). They also commented on the indolent course but stressed on the need for longer follow up.
This patient was found on the road with injuries and the first CT scan showed a hypo-dense lesion which was diagnosed as chronic subdural haematoma. He was taken up for surgery when he clinically deteriorated with radio-logical increase in size of the lesion but a biopsy was not done. When a final histology was obtained there was delay of many months. This case is being reported because the radiological diagnosis was confusing causing a delay in getting correct treatment and to stress again the classical teaching of obtaining a biopsy when abnormal tissue is seen. The fact that organized subdural haematoma can be seen as an extra-parenchymal mass also needs to be kept in view and hence the study is important.
The patient in this report also developed a swelling over the frontal region which was also of the same histology. Abdullah et al.,[16] and Mongia et al.,[17] reported patients who presented with lumps in the frontoparietal skin. Radiology of the first patient showed an associated extra-axial lesion. Both the patients had histo-pathology of the lesions confirmed as lymphoma.
Conclusions
Chronic subdural haematoma is a very common disease and primary leptomeningeal lymphoma is being reported more and more. This case is presented to show another manifestation of primary leptomeningeal lymphoma and also to re-emphasize the issue of obtaining biopsy when suspicious tissue is seen.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Hochberg FH, Miller DC. Primary central nervous system lymphoma. J Neurosurg. 1988;68:835–53. doi: 10.3171/jns.1988.68.6.0835. [DOI] [PubMed] [Google Scholar]
- 2.Murphy JK, O’Brien CJ, Ironside JW. Morphologic and immunophenotypic characterization of primary brain lymphomas using paraffin-embedded tissue. Histopathology. 1989;15:449–60. doi: 10.1111/j.1365-2559.1989.tb01605.x. [DOI] [PubMed] [Google Scholar]
- 3.O’Neill BP, Illig JJ. Primary central nervous system lymphoma. Mayo Clin Proc. 1989;64:1005–20. doi: 10.1016/s0025-6196(12)61228-2. [DOI] [PubMed] [Google Scholar]
- 4.Lachance DH, O’Neill BP, Macdonald DR, Jaeckle KA, Witzig TE, Li CY, et al. Primary leptomeningeal lymphoma: Report of 9 cases, diagnosis with immunocytochemical analysis, and review of the literature. Neurology. 1991;41:95–100. doi: 10.1212/wnl.41.1.95. [DOI] [PubMed] [Google Scholar]
- 5.Scotti G, Terbrugge K, Melancon D, Belanger G. Evaluation of the age of subdural hematomas by computerized tomography. J Neurosurg. 1977;47:311–5. doi: 10.3171/jns.1977.47.3.0311. [DOI] [PubMed] [Google Scholar]
- 6.Goetz P, Lafuente J, Revesz T, Galloway M, Dogan A, Kitchen N. Primary low-grade B-cell lymphoma of mucosa-associated lymphoid tissue of the dura mimicking the presentation of an acute subdural hematoma.Case report and review of the literature. J Neurosurg. 2002;96:611–4. doi: 10.3171/jns.2002.96.3.0611. [DOI] [PubMed] [Google Scholar]
- 7.Reyes MG, Homsi MF, Mangkornkanong M, Stone J, Glick RP. Malignant lymphoma presenting as a chronic subdural hematoma. Surg Neurol. 1990;33:35–6. doi: 10.1016/0090-3019(90)90222-b. [DOI] [PubMed] [Google Scholar]
- 8.Matano S, Sakashita Y, Furusho H, Ohashi M, Terahata S, Kakuma K, et al. Primary leptomeningeal lymphoma. J Neurooncol. 2001;52:81–3. doi: 10.1023/a:1010628924066. [DOI] [PubMed] [Google Scholar]
- 9.Altundag MK, Ozosik Y, Yalcin S, Akyol F, Uner A. Primary low grade B-cell lymphoma of the dura in an immunocompetent patient. J Exp Clin Cancer Res. 2000;19:249–51. [PubMed] [Google Scholar]
- 10.Amaker BH, Ghatak NR, Jebraili SA, Ferreira-Gonzalez A, Kornstein MJ. Primary T-cell-rich B-cell lymphoma masquerading as a meningioma. Arch Pathol Lab Med. 2000;124:1700–3. doi: 10.5858/2000-124-1700-PTCRBC. [DOI] [PubMed] [Google Scholar]
- 11.Freudenstein D, Bornemann A, Ernemann U, Boldt R, Duffner F. Intracranial malignant B-cell lymphoma of the dura. Clin Neuropathol. 2000;19:34–7. [PubMed] [Google Scholar]
- 12.Kumar S, Kumar D, Kaldjian EP, Bauserman S, Raffeld M, Jaffe ES. Primary low-grade B-cell lymphoma of the dura: A mucosa associated lymphoid tissue-type lymphoma. Am J Surg Pathol. 1997;21:81–7. doi: 10.1097/00000478-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Kambham N, Chang Y, Matsushima AY. Primary low-grade B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) arising in dura. Clin Neuropathol. 1998;17:311–7. [PubMed] [Google Scholar]
- 14.Iwamoto FM, DeAngelis LM, Abrey LE. Primary dural lymphomas: A clinicopathologic study of treatment and outcome in eight patients. Neurology. 2006;66:1763–5. doi: 10.1212/01.wnl.0000218284.23872.eb. [DOI] [PubMed] [Google Scholar]
- 15.Iwamoto FM, Abrey LE. Primary dural lymphomas: a review. Neurosurg Focus. 2006;15:21:E5. doi: 10.3171/foc.2006.21.5.6. [DOI] [PubMed] [Google Scholar]
- 16.Abdullah S, Morgensztern D, Rosado MF, Lossos IS. Primary lymphoblastic B-cell lymphoma of the cranial dura mater: A case report and review of the literature. Leuk Lymphoma. 2005;46:1651–7. doi: 10.1080/10428190500215126. [DOI] [PubMed] [Google Scholar]
- 17.Mongia S, Shukla D, Indira Devi B, Reddy TV. Primary cranial vault non-Hodgkin's lymphoma. Neurol India. 2003;51:293–4. [PubMed] [Google Scholar]


