Sir,
We encountered a 58 year old male patient who presented to us with complaints of neck pain for last 2 months associated with gradual onset weakness in all four limbs which was progressively increasing since 1and ½ months. He also had reduced sensations below the level of neck and frequent retention of urine. On examination, he was having spinal tenderness at C3,4 levels with spastic quadriplegia except for grade III power in left upper extremity. Sensory level was determined at C 5 level with generalized hyperreflexia. MRI cervical spine showed complete collapse of C4 vertebral body with cord compression and presence of pre-vertebral soft tissues suggestive of Pott's spine [Figure 1]. He was not a known case of tuberculosis and rest of the work up was negative. The patient was taken up for surgery and decompression (C4 corpectomy) followed by instrumentation by titanium cage and anterior cervical plating involving C3 and C5 vertebrae. The cord was seen well pulsating at the end. The patient did a remarkable recovery in the post–operative period and achieved grade IV power in all the limbs at the time of discharge so that he was made ambulatory with a cervical orthosis. The post-operative X-ray was satisfactory with screws well in position [Figure 2]. The histopathology confirmed the tuberculous etiology with the presence of langerhans giant cells and epithelioid granulomas along with caseous necrosis. He was started on five drug anti- tubercular therapy (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol and Streptomycin). Patient came back after 2 months with history of recurrence of neck pain although he was still ambulatory. Repeat x-ray showed resorption of the C5 vertebral body and screw pull out along with cage displacement [Figure 3]. This was unusual as the patient was on anti- tubercular treatment and evidence of bony fusion was expected, not resorption or what we termed as “Ghost vertebra” [Figure 4]. The culture after 8 weeks grew atypical mycobacterium although by that time the graft was already displaced. We searched the literature regarding continuing destructive tuberculous pathology despite on treatment and whether in such a scenario grafts should be placed or not, as chances of failure may remain high. The only hypothesis in our patient was the involvement of C5 vertebra at the time of surgery which was not picked up on imaging. The question regarding screw pull outs in tuberculous spine looms mainly because of hematogenous spread of the infection to the contiguous vertebra. Moorthy et al. have studied almost 14 patients of sub-axial cervical spine tuberculosis following uninstrumented anterior decompression surgery and medical treatment.[1] All patients were decompressed and autologous bone graft was used after corpectomies without cervical plating. The patients were subjected to bed rest for 4-6 weeks. Patients improved in the follow up with increase in their Nurick grades and maintenance of spinal curvature in most of them. There was evidence of bony fusion in 12 out of the 14 patients. The authors infer that graft subsidence is a common phenomenon in tuberculosis where early mobilization has been attempted and bed rest increases the chance of fusion and reduces the rate of graft subsidence by taking off axial loads. Authors also point out the pre-existing osteopenia in tuberculosis patients may be responsible for graft subsidence and hardware malposition. Tye, et al. also noted graft subsidence following instrumented fusion in degenerative spinal conditions.[2] These chances may further increase if the marrow is involved beforehand as in tuberculosis. Also, as the culture for tuberculosis takes at least 6 weeks, atypical infection will not be detected before mobilization. In retrospect, we think that resorption of vertebral body happened despite the patient being on anti-tubercular regimen because of atypical infection and early ambulation in our case may have added to the graft subsidence. Hence, though it argues against the advantages of instrumentation, in tuberculous cervical spine, it may be worth following a slow and gradual ambulation even after anterior cervical plating. This time period will help us titrate the anti-tuberculous regimen according to the culture reports and will make us more proactive in starting 2nd line drugs. This strategy may help prevent such happenings in future and further, we need to study the effect of anti-tubercular therapy on contiguous vertebra which are not prima-facie involved on imaging.
Figure 1.
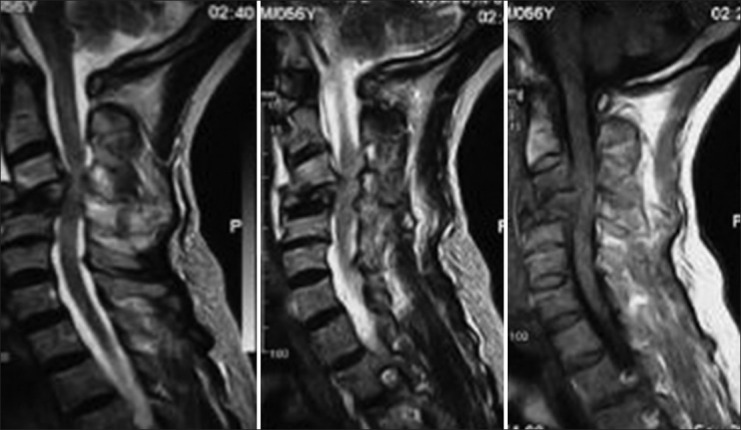
Magnetic resonance imaging showing C4 vertebral body collapse with cord compression with intact C5 body
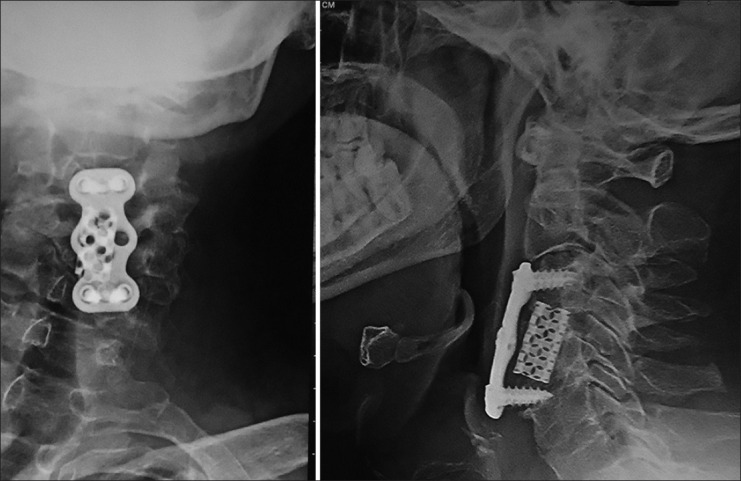
Figure 2.

Post-operative X-ray showing implants in situ with lower screws well in position in the centre of C5 body
Figure 3.
X-ray after 2 months showing resorption of C5 vertebral body and screw pull out with cage subsidence
Figure 4.
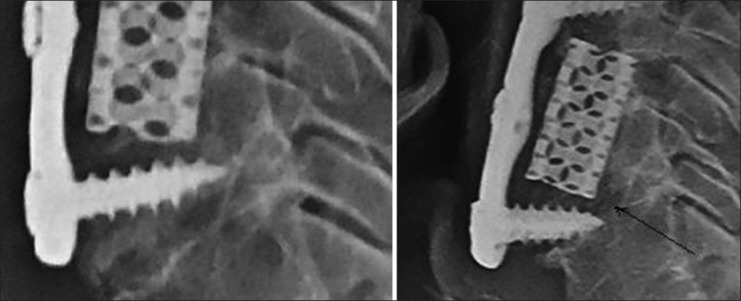
Magnified view showing anterior half of C5 vertebral body and upper and lower endplates of C5 before and after resorption (arrow)
References
- 1.Moorthy RK, Arunkumar MJ, Rajshekhar V. Uninstrumented ventral surgery for sub-axial cervical spine tuberculosis: Clinical and radiological outcome. Br J Neurosurg. 2004;18:584–9. doi: 10.1080/02688690400022839. [DOI] [PubMed] [Google Scholar]
- 2.Tye GW, Graham RS, Broaddus WC, Young HF. Graft subsidence after instrument- associated anterior cervical fusion. J Neurosurg. 2002;97:128–34. doi: 10.3171/spi.2002.97.2.0186. [DOI] [PubMed] [Google Scholar]


