Abstract
Background:
Nephrolithiasis is a recurrent disease, and one of the most effective methods for prevention of stone recurrence is increasing the urine output (>2 L/day), but it is difficult to achieve it. The aim of this study was to evaluate the effect of behavioral intervention by measurement of urine specific gravity using dipstick on 24-h urine volume in first renal stone patients.
Materials and Methods:
In this prospective randomize clinical study, 80 adult patients with history of first renal stone were included. Patients were divided into two groups with 40 patients in each group. We explained the importance of high fluid intake and high urine volume in the prevention of renal stones for all patients. Group A patients were trained to measure 24-h urine volume every 15 days, and group B patients were trained to keep urine specific gravity below 1.010 by using dipstick. We measured 24-h urine volume in each group before intervention, and at 3 months and 6 months after intervention and compared them.
Results:
There were no significant differences between the two groups in 24-h urine volume before intervention (P = 0.41), but it was significant 3 months (P = 0.01) and 6 months (P = 0.01) after intervention. Patients’ compliance was 20% in group A and 90% in group B (P < 0.05).
Conclusion:
The use of behavioral modification with dipstick is an effective method for control and maintenance of optimal urine volume, and it has resulted in more patient compliance for drinking water and is more effective for prevention of renal stone.
Keywords: Behavioral Intervention, dipstick, lifestyle, nephrolithiasis, urine 24 hour volume
INTRODUCTION
Renal stones (nephrolithiasis) affect approximately 12% of men and 5% of women by age 70. Fortunately, available treatments effectively manage most renal stones, but some steps should be taken to prevent their recurrence. Recurrence rate is about 5% per year in people who are not treated.[1]
The amount and type of food and drink that a person consumes can play an important role in the formation of renal stones. The amount of fluid intake directly affects the volume of urine output. Previous studies showed that increasing the recommended fluid intake would decrease the recurrence rate of kidney stone (12% compared with 27%).[2]
So, experts recommend drinking enough fluids so that the kidneys make approximately 2 L of urine per day.[3,4] Although it looks simple to reach adequate 24-h urine volume (2 L/day), it is difficult to have because most of the patients have no compliance to intake of high volume of fluid for a long time.[5]
Furthermore, most of the urologists pay attention only to the surgical aspects of stone disease and the biochemical aspects of stone formation are always neglected. At best, the advice given is restricted to high fluid intake to avoid high urinary solute concentration. Although high fluid intake is beneficial for all kinds of stone formers, experience has shown that it is difficult to maintain high fluid intake lifelong. Most certainly, very few, if any, of our patients are capable of coping satisfactorily with that kind of advice. It stands to reason that appropriate prevention of further stone formation requires a much deeper understanding of why and how stones can develop in the urinary tract.[6]
Eating habits is a main component of lifestyle. Lifestyle has a direct effect on lithogenic urinary risk factors.[7] A suitable diet style for patient with nephrolithiasis is characterized by a high intake of fluids as a healthy behavior.[8] Making changes in the lifestyle can reduce the risk of recurrence. Behavior modification is the behavior change techniques to increase or decrease the frequency of behavior.
The aim of the study was to examine the effect of behavioral intervention with measurement of urine specific gravity by dipstick on 24-h urine volume in first renal stone patients.
MATERIALS AND METHODS
In this prospective, randomized clinical trial study, we surveyed 80 adult patients with normal creatinine (<1.5 mg/dL) and history of first renal stone (existence of stone on imaging: kidney sonography, abdominal KUB, IVP, CT.) who referred to urology clinic of Alzahra Hospital in Isfahan. The study was done in the first 6 months of 2011. Patients were randomly divided into two groups, A and B, with 40 patients in each group. Physician explained the importance of increasing drinking fluids and urinary output.
Patients in group A were forced to drink fluids and trained to measure 24-h urine volume every 15 days.
24-h urine was kept in 250–500 mL glass, and after measurement, was shifted to larger store. If the urine volume was 2 L or more, it showed adequate fluid intake.
Patients in group B were forced to drink fluids and trained to measure 24-h specific gravity using dipstick. In this group, each patient got 300 dipsticks and was trained to measure urine specific gravity in different hours. Urine samples after took tasted with dipstick at room temperature (15–20°C). Then, specific gravity marker on dipstick (primary green) was compared with the container chart (1000-(-1005-1010-1015-1020-1025-1030 mg/L. If urine specific gravity was more than 1.010, it showed inadequate fluid intake and patient understood that he/she should drink more fluids. Then, with this method, we measured 24-h urine volume in the two groups before intervention, and at 3 months and 6 months after intervention.
To compare the mean of urine volume collected three times in the two groups, we used repeated measure analysis of variance (ANOVA). To compare the mean of urine volume in the two groups at the same time, we used independent t-test. All data were analyzed with PASW-18 software.
RESULTS
The mean age of patients was 42.3 ± 7.0 years (range 23–61 years; group A 42.1 ± 6.2 years and group B 42.7 ± 7.1 years) with no significant difference between the two groups (P = 0.83). There were 33 (41.25%) women and 47 (58.75%) men. In group A, there were 23 (57.5%) men and 17 (42.5%) women, and in group B there were 24 (60%) men and 16 (40%) women, with no significant difference between the two groups (P = 0.90).
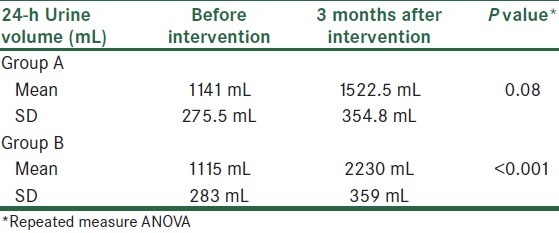
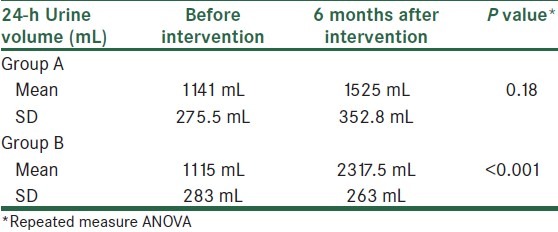
On comparing the two groups before intervention, and at 3 and 6 months after the intervention, significant difference was found with repeated measure ANOVA (P < 0.001) [Tables 1,2].
Table 1.
Comparing the 24-h urine volume between patients who did not use dipstick (group A) and patients who used dipstick (group B) for measurement of 24-h urine volumes
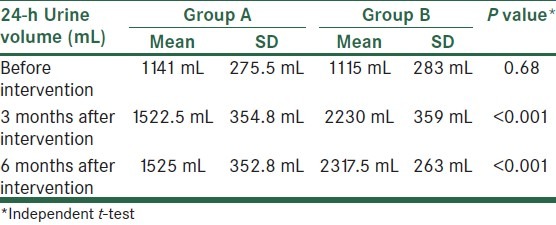
Table 2.
Comparing 24-h urine volume between before intervention and 3 months after intervention in group A and group B
Results showed after 6 months, 90% of patients in group B (patients who used dipstick) recorded and reported their urine specific gravity and daily urine volume, but in group A (patients who did not use dipstick) only 20% of patients recorded and reported their daily urine volume (P = 0.01). It shows that patients who used dipstick had more compliance for much more fluid intake.
DISCUSSION
Renal stone disease is a relatively common problem[1,2] . A report from the third National Health and Nutrition Examination Survey shows that the population prevalence increased from 3.8% in the period 1976–1980 to 5.2% during 1988–1994.[5]
Dietary factors can play an important role in promoting stone formation, primarily by affecting the composition of the urine[3] . There are several dietary factors that may play an important role in many patients: Fluid, calcium, oxalate, potassium, sodium, animal protein, phytate, sucrose, fructose, and vitamin C intake. A low fluid intake will lead to a low urine output, thereby promoting stone formation by increasing the concentration of calcium and oxalate and accordingly increasing the supersaturation with calcium oxalate.
In one report, for example, patients who had a first kidney stone had a baseline daily urine output that was 250–350 mL less than controls.[4] A related concern arises among individuals who work in a very hot environment, in whom the risk of nephrolithiasis is markedly increased without adequate fluid intake.[5]
The importance of fluid intake on the risk of incident stone formation was illustrated by data from several cohort studies.[2,9,10,11] In these reports of over 200,000 men and women, there was a 30% lower risk of developing symptomatic kidney stones in participants in the highest quintile of fluid intake compared with those in the lowest quintile. In addition to low fluid intake as a risk factor for incident stone disease, increasing the fluid intake can lead to a reduction in recurrent stone formation. Surveys over a 15-year period for recurrent stone disease reported their frequencies of urinary abnormalities. 15% of patients had low urine volume (<1 L/day) as a risk factor.[12]
Therefore, forced increase in fluid intake is the most important component of conservative management for recurrent kidney stones.[2] Moreover, intermittent compliance is not effective because more stones may form even in a period of intense dehydration.[5,13]
Parks et al. showed the mean of increased urinary output was 300 mL/day in patients at private clinics and academic centers.[14]
In our study, we compared the 24-h urine volume between patients who used dipstick for measurement of urine volume and others. Our intervention was using dipstick, and the results showed that in patients who used dipstick, urinary volume significantly increased compared with before using dipstick (P < 0.001), but in those who did not use dipstick, there was no difference (P = 0.68) [Table 1]. Also, urine volume had significantly increased in patients who used dipstick, at 6 months after the intervention (P < 0.001), but in control group it was not significant (P = 0.18) [Table 3].
Table 3.
Comparing 24-h urine volume between before intervention and 6 months after intervention in group A and group B
McCormack and colleagues surveyed the correlation between 24-h urine volumes and mean urine specific gravity in 263 randomly chosen patients. They showed an inverse relationship between urine specific gravity and 24-h urine volume, with a correlation coefficient of 0.522 (y = 1.0207 − 0.00374x). Most patients (81.6%) with 24-h urine volumes of less than 2.1 L had a urine specific gravity of more than 1.010. Results showed that using specific gravity dipsticks as a tool for evaluation helped 24 patients increase the 24-h urine volume [Figure 1]. The 24-h urine volume increased significantly (P < 0.05, paired Student's t test) in patients with the feedback from specific gravity dipsticks, as they were instructed to keep the urine specific gravity at or less than 1.010 (average 24-h urine volume increased 192%).[15]
Figure 1.
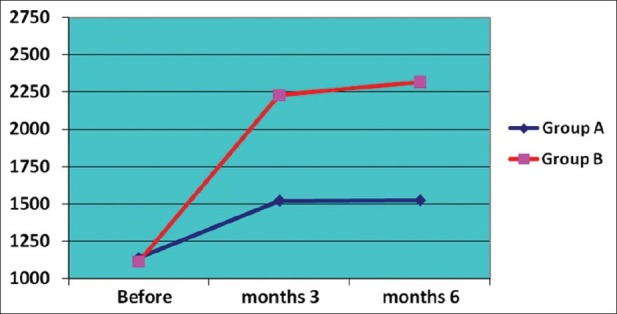
24-h urine volume curves in two groups before, and at 3 and 6 months after intervention
This intervention is a behavior change technique used to increase the frequency of fluid intake as an appropriate behavior in the lifestyle of patients for managing their condition. In this procedure, getting feedback by dipstick showing urine specific gravity plays the role of a stimulus for adaptive behavior. Fluid intake as the adaptive behavior is the reaction to that stimulus. Also, in this technique, maintaining the specific gravity is reinforcement for adaptive behavior. Then, the patient learns to keep the volume automatically by this conditioned behavior. High fluid intake decreased the risk of recurrent nephrolithiasis. An increase in fluids by increased adaptive behavior may reduce the urinary concentration of calcium, oxalate, and uric acid. The patients gain self-management skill by this behavioral method. Self-management can be described as a set of skilled behaviors that patients carry out for managing their condition.
This study confirmed the effectiveness of behavior intervention to prevent recurrent nephrolithiasis. Regarding the results of this study, it is suggested that in treatment of patients with kidney stones, behavior techniques should be considered for changing lifestyle.
According to above, using dipstick is beneficial. Dipstick is an inexpensive device and easy to manipulate for more patients. Our study results show most of the patients could not estimate the true volume of urine and so they could not estimate adequate liquid intake per day. Paying attention to drink water and even measurement of daily urine volume could not increase the urine output to more than 2 L/day in patients.
Furthermore, patients who used dipstick for measurement of urine specific gravity had more visibility for optimal water intake and urine volume, and more than 90% of patients used dipstick after 6 months, so they had much more urine output. It shows the use of dipstick is a cheap and effective method for control and maintenance of optimal urine volume and it leads to more patient compliance for drinking water and more effectiveness for prevention of renal stone.
We should mention that the non-measurement of specific gravity before and after completing the study and also the absence of a non-recorded diet recall in all of the participants are the limitations of our study.
CONCLUSION
We conclude that urine specific gravity measurement with dipstick is a powerful tool to reach adequate urine output. Also, it is suggested that in treatment of patients with renal stones, behavior techniques should be considered for changing the lifestyle.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Glowacki LS, Beecroft ML, Cook RJ, Pahl D, Churchill DN. The natural history of asymptomatic urolithiasis. J Urol. 1992;147:319–21. doi: 10.1016/s0022-5347(17)37225-7. [DOI] [PubMed] [Google Scholar]
- 2.Borghi L, Meschi T, Amato F, Briganti A, Novarini A, Giannini A. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: A 5-year randomized prospective study. J Urol. 1996;155:839–43. [PubMed] [Google Scholar]
- 3.Borghi L, Schianchi T, Meschi T, Guerra A. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med. 2002;346:77–84. doi: 10.1056/NEJMoa010369. [DOI] [PubMed] [Google Scholar]
- 4.Curhan GC, Willett WC, Speizer FE, Spiegelman D, Stampfer MJ. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann Intern Med. 1997;126:497–504. doi: 10.7326/0003-4819-126-7-199704010-00001. [DOI] [PubMed] [Google Scholar]
- 5.Campbell-Walsh Urology 2012. Imprint of Elsevier. Chapter 45 – Urinary Lithiasis: Etiology, Epidemiology, and Pathogenesis. (10th ed) 2012:520–40. [Google Scholar]
- 6.Tiselius HG. Who forms stones and why? Euro Urol Supp. 2011;10:408–14. [Google Scholar]
- 7.Meschi T, Nouvenne A, Borghi L. Lifestyle recommendations to reduce the risk of kidney stones. Urol Clin North Am. 2011;38:313–20. doi: 10.1016/j.ucl.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Fink HA, Akornor JW, Garimella PS, MacDonald R, Cutting A, Rutks IR, et al. Diet, fluid, or supplements for secondary prevention of nephrolithiasis: A systematic review and meta-analysis of randomized trials. Eur Urol. 2009;56:72–80. doi: 10.1016/j.eururo.2009.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson CM, Wilson DM, O’Fallon WM. Renal stone epidemiology: A 25-year study in Rochester, Minnesota. Kidney Int. 1979;16:624–31. doi: 10.1038/ki.1979.173. [DOI] [PubMed] [Google Scholar]
- 10.Stamatelou KK, Francis ME, Jones CA, Nyberg LM. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003;63:1817–23. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 11.Parivar F, Low RK, Stoller ML. Influence of diet on urinary stone disease. J Urol. 1996;155:432–40. [PubMed] [Google Scholar]
- 12.Atan L, Andreoni C, Ortiz V, Silva EK, Pitta R, Atan F, et al. High kidney stone risk in men working in steel industry at hot temperatures. Urology. 2005;65:858–61. doi: 10.1016/j.urology.2004.11.048. [DOI] [PubMed] [Google Scholar]
- 13.Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med. 1993;328:833–8. doi: 10.1056/NEJM199303253281203. [DOI] [PubMed] [Google Scholar]
- 14.Parks JH, Goldfischer ER, Coe FL. Changes in urine volume accomplished by physicians treating nephrolithiasis. J Urol. 2003;169:863–6. doi: 10.1097/01.ju.0000044922.22478.32. [DOI] [PubMed] [Google Scholar]
- 15.McCormack M, Dessureault J, Guitard M. The urine specific gravity dipstick: A useful tool to increase fluid intake in stone forming patients. J Urol. 1991;146:1475–7. doi: 10.1016/s0022-5347(17)38143-0. [DOI] [PubMed] [Google Scholar]


