Abstract
Background:
Diabetes mellitus (DM) is a common metabolic disorder that can cause various complications including, peripheral neuropathy (PNP). Some possible risk-factors such as blood glucose level, hyperglycemia, duration of diabetes, and lipid profiles are assumed to be important in diabetic PNP incidence. The aim of this study is to evaluate the prevalence and possible risk-factors of PNP in children with insulin dependent DM.
Materials and Methods:
Among diabetic children, 146 patients (up to 18-years old) were evaluated in this cross-sectional study. All patients were examined for signs and symptoms of neuropathy and nerve conduction studies were performed. Blood level of glucose and lipid profiles were also tested. The relation between variables was compared by independent t-test and logistic regression test.
Results:
The mean age of diabetic children was 11.9 ± 3.3 years whereas mean diabetes duration was 3.8 ± 2.9 years. PNP was detected in 40 patients (27.4%) that 62.5% of them have subclinical and 37.5% have clinical neuropathy. According to logistic regression analysis, duration of diabetes was the most important factor in prevalence of PNP (5.7 ± 3.5 and 3.1 ± 2.5 years in patients with and without neuropathy respectively, P < 0.001, 95% confidence interval [1.15-1.54]).
Conclusion:
As most of the patients had subclinical PN, neurological assessment is recommended to detect subclinical neuropathy in asymptomatic type 1 diabetic children and it seems that the best way to prevent this complication is still rigid blood glucose control and periodic evaluations.
Keywords: Diabetes mellitus, peripheral neuropathy, prevalence, risk factors, type 1
INTRODUCTION
Diabetes mellitus (DM) is the most common metabolic disease with a prevalence of 1-4%.[1,2,3] Diabetic patients may experience various long-term complications including, neuropathy, retinopathy, nephropathy, and macrovascular disease. Diabetic neuropathy (DN) is a significant source of morbidity and decrease quality of life. The prevalence estimates of DN vary largely, depending on specific diagnostic criteria but ranges from 5% to 66% in the most conclusive epidemiological studies involving both adult and pediatric patients.[2,4,5]
DN is known as a set of varied clinical syndromes with sensory, motor, and/or autonomic nerve fiber dysfunction, although the most common type is symmetrical distal sensory polyneuropathy.[6,7] The signs and symptoms of peripheral neuropathy (PNP) infrequently occur in diabetic children[8] and clinical examination had less sensitivity and specificity than nerve conduction studies, which serves as a gold standard to detect subclinical neuropathy in these patients.[9] However, little is known about the prevalence of subclinical neuropathy in children with DM and studies are needed to evaluate the prevalence and incidence of neuropathy in children to make suitable decisions for decreasing the burden of the disease.
Some of the recent studies have addressed multiple risk-factors, which may affect the development or progression of DN such as age, disease duration, lipid profile, and Hemoglobin-A1c.[10,11,12] However, other studies reported controversial results.[6,13,14] The aim of this study was to evaluate the prevalence and possible risk-factors of PNP in children with insulin dependent DM.
MATERIALS AND METHODS
In this cross-sectional study (2008-2009) among 500 diabetic patients who referred to Endocrinology and Metabolic Research Center (EMRC) of Isfahan University of Medical Sciences (IUMS), 150 children up to 18-year-old were enrolled of which 146 of them completed our study. Patients who suffered from seizure, non-diabetic known neuropathy, uncontrolled hypothyroidism, and mental retardation were excluded from our study.
Data collection
In all the patients: Age, duration of diabetes, and other demographic characteristics were written, then subjective neuropathic symptoms, neurological assessment, and electrophysiological results were evaluated. The subjective symptoms which were asked included numbness, muscle weakness, and history of previously diagnosed retinopathy or nephropathy.
Each patient underwent clinical neurological examination including the conventional investigations of muscle weakness, fine touch, pinprick, pain, temperature, vibration, proprioception, and deep tendon reflexes.
Electrophysiological tests were done in recommended standard situations[15] for all patients by Synergy (Medelec) electromyograph machine, which included ulnar and median nerves (sensory and motor fibers) in upper extremities and sural (sensory), deep peroneal and tibial (motor) nerves in lower extremities. In motor nerves, the values for distal latencies and amplitude of compound muscle action potential, nerve conduction velocity (NCV) and F-waves were measured while in sensory nerves the parameters of distal latencies and amplitude of sensory nerve action potential and NCV were investigated. These electrophysiological tests were performed by a physiatrist who was blinded to clinical information and medical history of the subjects. The criteria for abnormal values of these tests were: Distal latency > mean + 2SD, amplitude < mean − 2SD, F-wave > mean + 2SD, NCV < mean − 2SD.[15] At least two abnormal independent neurophysiological nerve parameters were required as the criteria of peripheral nervous system involvement and therefore the subjects were divided into two groups: The patients with PNP and the patients without PNP. Then the mean level of three measurements for HbA1c index, fasting blood sugar (FBS), and lipid profile (cholesterol, low-density lipoprotein [LDL], high-density lipoprotein, and triglyceride) were evaluated during a period of 12 months.
This study was approved by the Ethics’ Committee of EMRC affiliated to IUMS. Written informed consent from the parents and children was obtained prior to study.
Data analysis
All statistical analyses were done using SPSS software (version 16.0, Chicago, IL, USA) for Windows. All data were expressed as the mean ± SD and a P value < 0.05 were considered to be a significant meaningful. The independent t-test was used for quantitative variables (age, disease duration, glycated hemoglobin, FBS, and lipid profile) between two groups of PNP and without PNP. Association between the PNP and different variables was analyzed with logistic regression.
RESULTS
Among 146 diabetic children, 57.5% (84) were female and 42.5% (62) were male with the mean age 11.9 ± 3.3 years (4.1-18.4). The mean diabetes duration was 3.8 ± 2.9 years (0.5-13).
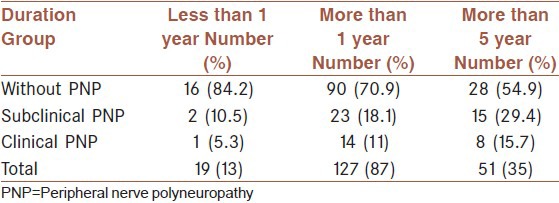
Based on the above mentioned neurophysiological criteria, 27.4% (40 patients) were classified as PNP group with 62.5% (25) female and 37.5% (15) male. Twenty five patients (62.5%) were clinically asymptomatic which classified as subclinical neuropathy and 15 cases (37.5%) had at least one of the PNP signs or symptoms (17.1% and 10.3% of all subjects respectively) [Tables 1 and 2].
Table 1.
Sign and symptoms of neuropathy in diabetic patients
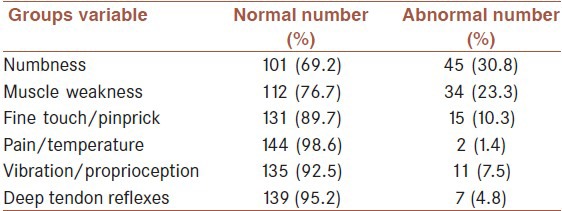
Table 2.
Frequency of clinical and subclinical neuropathy in relation to duration of diabetes mellitus
Mean HbA1c, FBS and other variables evaluated in patients are presented in Tables 3 and 4 classified in two groups of patients with and without PNP.
Table 3.
The comparison between patients with and without neuropathy based on age, duration, lipid profile, blood sugar, and HbA1c
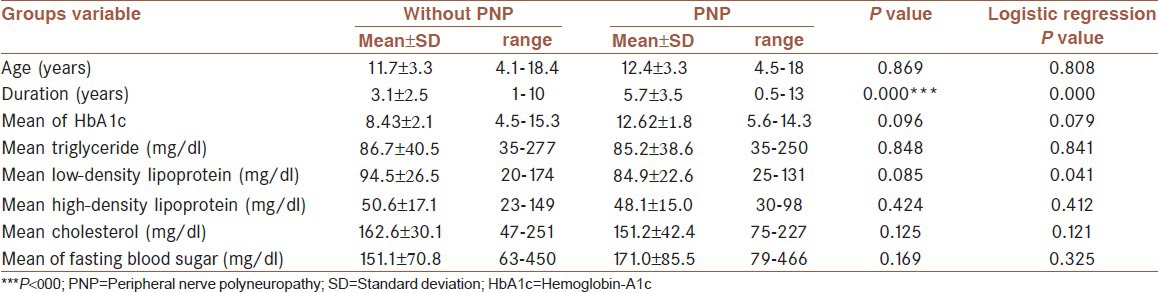
Table 4.
Results of logistic regression analysis in diabetic patients
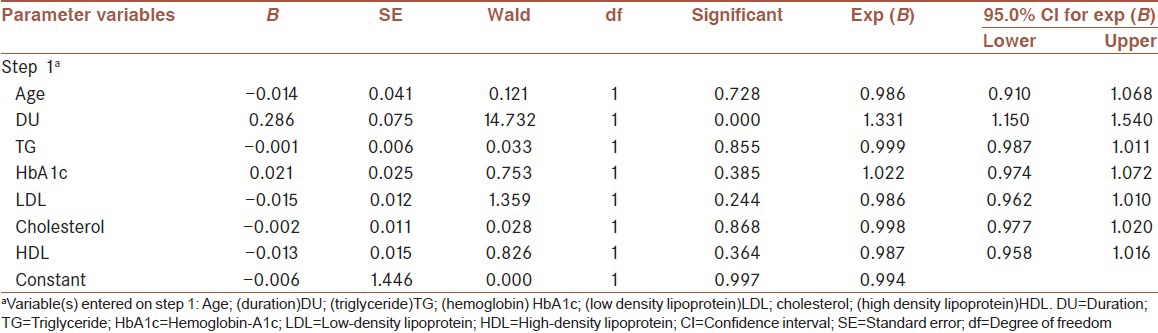
The mean duration of DM was 3.8 ± 2.9 years which were 5.7 ± 3.5 and 3.1 ± 2.5 years in patients with and without PNP respectively. Based on comparing means between groups by independent t-test just the duration of disease plays a significant role in DN (P value = 0.000), and neither the HbA1c nor the age, lipid profile, and FBS of the subjects do not show significant correlation with nerve dysfunction [Tables 3 and 4]. Based on assessment with binary logistic regression test among different evaluated variables, in the patients with longer duration of disease, LDL level of serum can affect the developing of diabetic PNP.
DISCUSSION
PNP is a complication of DM observed in one-third of our patients. DN is the result of nerve ischemia from microvascular disease, direct effects of hyperglycemia on neurons, and intracellular metabolic changes that impair nerve function. The prevalence of PNP in children with DM has been reported between 10% and 68%.[10,16] A community-based study[1] revealed that 1.3% of the population had some form of clinically recognized DM (27%, type 1 DM; 73%, type 2 DM). Among the patients with type 1 DM, 66% had some form of neuropathy. However, the estimation of DN is not as accurate since it tends to be subclinical in this age group. In fact subclinical DN is not uncommon between young patients with type 1 DM, just about one-fourth of young patients with a recent diagnosis of this disease have been reported to have pathological findings in the distal nerves.[17] Ghorbani et al. in a study on type two diabetic patients in Isfahan city reported the prevalence of 77.4% for sensorimotor polyneuropathy in the patients.[18] We found DN in 27.4% of patients which 62.5% were subclinical.
Many studies introduced the diabetes duration as a major factor in developing DN.[11,13,19,20] However, it is not confirmed in other studies.[14,21,22] Nelson et al. reported a prevalence of 57% of subclinical neuropathy based on nerve conduction findings in Canadian children and adolescents with at least 5 years duration of type 1 DM.[6] In our study, 51 patients (35%) had diabetes duration of 5 years or longer and 23 of them (45.1%) showed electrophysiological evidences of DN which 65% (15 in 23 patients) were clinically asymptomatic.
On the other hand, one of the published series reported a prevalence of 7.5% for DN at the time of diagnosis of diabetes, which the prevalence increasing constantly thereafter with no apparent plateau.[23] Also other studies suggested that the most rapid worsening of nerve function occurs soon after the onset of type 1 diabetes, and within 2-3 year, there is a slowing of the progress.[9,24] In another study, it was found that 25% of pediatric patients with newly diagnosed diabetes already have abnormal findings on nerve conduction studies.[13] In our study, 3 cases of 19 (15.8%) patients with diabetes duration less than one year had DN.
Although, patients with DN have few complications but their physical examination may reveal variable degrees of sensory loss.[11] In our study, 30.8% of subjects had numbness, about 7-10% showed large myelinated nerve fiber dysfunction while only 1.4% had impairment in pain or temperature sensation.
Among the studied nerves, deep peroneal and then sural were the most common affected nerves. Meh et al. also reported the same result,[21] but some other studies reported sural nerve as the most affected nerve.[14,20]
Hyperglycemia plays a main role in progression of the DN but it is now obvious that neuropathy can occur with the absence of hyperglycemia.[25,26] In most studies, HbA1c is used as an index of glycemic control and the role of it as a risk-factor for DN is proved in some studies,[10,13] but it is not confirmed by other studies[6,21] just like our study. However, in our study 70% of children with DN had a mean of HbA1c more than 7, it seems that good blood glucose control may play a significant role in DN prevention and/or postponement.[27,28,29]
CONCLUSION
Regarding to the point that duration of diabetes is the most important factor in causing peripheral neuropathy, and a considerable number of patients had not shown any symptoms of neuropathy (prevalence of DN was 27.4% of all patients which 62.5% were subclinical), so neurological assessment including nerve conduction studies as well as meticulous physical examination for evaluating the function of large sensory and motor fibers is recommended, to detect subclinical neuropathy in asymptomatic type 1 diabetic children. It seems that, the best way to prevent this complication is still rigid blood glucose control and periodic evaluations.
Footnotes
Source of Support: This research was approved by ethics’ committee of Endocrine and Metabolism Research Center affiliated to Isfahan University of Medical Sciences and financially supported by Isfahan University of Medical Sciences (Grant No. 286007)
Conflict of Interest: None declared.
REFERENCES
- 1.Dyck PJ, Kratz KM, Karnes JL, Litchy WJ, Klein R, Pach JM, et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: The Rochester Diabetic Neuropathy Study. Neurology. 1993;43:817–24. doi: 10.1212/wnl.43.4.817. [DOI] [PubMed] [Google Scholar]
- 2.Partanen J, Niskanen L, Lehtinen J, Mervaala E, Siitonen O, Uusitupa M. Natural history of peripheral neuropathy in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:89–94. doi: 10.1056/NEJM199507133330203. [DOI] [PubMed] [Google Scholar]
- 3.Ross MA. Neuropathies associated with diabetes. Med Clin North Am. 1993;77:111–24. doi: 10.1016/s0025-7125(16)30275-9. [DOI] [PubMed] [Google Scholar]
- 4.Verrotti A, Catino M, Di Ricco L, Casani A, Chiarelli F. Prevention of microvascular complications in diabetic children and adolescents. Acta Paediatr Suppl. 1999;88:35–8. doi: 10.1111/j.1651-2227.1999.tb14338.x. [DOI] [PubMed] [Google Scholar]
- 5.Melton LJ, Dyck PJ. Clinical features of the diabetic neuropathies. In: Dyck PI, Thomas PK, Asbury AK, editors. Diabetic Neuropathy. Philadelphia: W.B. Saunders; 1987. pp. 27–35. [Google Scholar]
- 6.Nelson D, Mah JK, Adams C, Hui S, Crawford S, Darwish H, et al. Comparison of conventional and non-invasive techniques for the early identification of diabetic neuropathy in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2006;7:305–10. doi: 10.1111/j.1399-5448.2006.00208.x. [DOI] [PubMed] [Google Scholar]
- 7.Maser RE, Steenkiste AR, Dorman JS, Nielsen VK, Bass EB, Manjoo Q, et al. Epidemiological correlates of diabetic neuropathy. Report from Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes. 1989;38:1456–61. doi: 10.2337/diab.38.11.1456. [DOI] [PubMed] [Google Scholar]
- 8.Paivi H. Peripheral nerve function is increasingly impaired during puberty in adolescents with type 1 diabetes. Diabetes Care. 2001;24:421–6. doi: 10.2337/diacare.24.6.1087. [DOI] [PubMed] [Google Scholar]
- 9.Vinik A. Neuropathies in children and adolescents with diabetes: The tip of the iceberg. Pediatr Diabetes. 2006;7:301–4. doi: 10.1111/j.1399-5448.2006.00213.x. [DOI] [PubMed] [Google Scholar]
- 10.Bao XH, Wong V, Wang Q, Low LC. Prevalence of peripheral neuropathy with insulin-dependent diabetes mellitus. Pediatr Neurol. 1999;20:204–9. doi: 10.1016/s0887-8994(98)00141-6. [DOI] [PubMed] [Google Scholar]
- 11.Malgrange D, Richard JL, Leymarie F French Working Group on The Diabetic Foot. Screening diabetic patients at risk for foot ulceration. A multi-centre hospital-based study in France. Diabetes Metab. 2003;29:261–8. doi: 10.1016/s1262-3636(07)70035-6. [DOI] [PubMed] [Google Scholar]
- 12.Aring AM, Jones DE, Falko JM. Evaluation and prevention of diabetic neuropathy. Am Fam Physician. 2005;71:2123–8. [PubMed] [Google Scholar]
- 13.Weintrob N, Amitay I, Lilos P, Shalitin S, Lazar L, Josefsberg Z. Bedside neuropathy disability score compared to quantitative sensory testing for measurement of diabetic neuropathy in children, adolescents, and young adults with type 1 diabetes. J Diabetes Complications. 2007;21:13–9. doi: 10.1016/j.jdiacomp.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Karsidag S, Morali S, Sargin M, Salman S, Karsidag K, Us O. The electrophysiological findings of subclinical neuropathy in patients with recently diagnosed type 1 diabetes mellitus. Diabetes Res Clin Pract. 2005;67:211–9. doi: 10.1016/j.diabres.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Dumitru D, Amato AA, Zwarts MJ. Nerve conduction studies. In: Dumitru D, editor. Electrodiagnostic Medicine. 2nd ed. Philadelphia: Hanley and Belfus Inc; 2002. pp. 194–217. [Google Scholar]
- 16.Gamstorp I, Shelburne SA, Jr, Engleson G, Redondo D, Traisman HS. Peripheral neuropathy in juvenile diabetes. Diabetes. 1966;15:411–8. doi: 10.2337/diab.15.6.411. [DOI] [PubMed] [Google Scholar]
- 17.Trotta D, Verrotti A, Salladini C, Chiarelli F. Diabetic neuropathy in children and adolescents. Pediatr Diabetes. 2004;5:44–57. doi: 10.1111/j.1399-543X.2004.00041.x. [DOI] [PubMed] [Google Scholar]
- 18.Ghorbani A, Rezvanian H, Kazemi A, Saberi A. Determination of diabetic-polyneuropathy prevalence through clinical examination and electrodiognostic findings. J Birjand Univ Med Sci. 2007;14:9–15. [Google Scholar]
- 19.Booya F, Bandarian F, Larijani B, Pajouhi M, Nooraei M, Lotfi J. Potential risk factors for diabetic neuropathy: A case control study. BMC Neurol. 2005;5:24–31. doi: 10.1186/1471-2377-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riihimaa PH, Suominen K, Tolonen U, Jäntti V, Knip M, Tapanainen P. Peripheral nerve function is increasingly impaired during puberty in adolescents with type 1 diabetes. Diabetes Care. 2001;24:1087–92. doi: 10.2337/diacare.24.6.1087. [DOI] [PubMed] [Google Scholar]
- 21.Meh D, Denislic M. Subclinical neuropathy in type I diabetic children. Electroencephalogr Clin Neurophysiol. 1998;109:274–80. doi: 10.1016/s0924-980x(98)00017-4. [DOI] [PubMed] [Google Scholar]
- 22.Karavanaki K, Baum JD. Prevalence of microvascular and neurologic abnormalities in a population of diabetic children. J Pediatr Endocrinol Metab. 1999;12:411–22. doi: 10.1515/jpem.1999.12.3.411. [DOI] [PubMed] [Google Scholar]
- 23.Semiz S, Fişenk F, Akçurin S, Bircan I. Temporary multiple cranial nerve palsies in a patient with type 1 diabetes mellitus. Diabetes Metab. 2002;28:413–6. [PubMed] [Google Scholar]
- 24.Ziegler D, Cicmir I, Mayer P, Wiefels K, Gries FA. Somatic and autonomic nerve function during the first year after diagnosis of type 1 (insulin-dependent) diabetes. Diabetes Res. 1988;7:123–7. [PubMed] [Google Scholar]
- 25.Smith AG, Ramachandran P, Tripp S, Singleton JR. Epidermal nerve innervation in impaired glucose tolerance and diabetes-associated neuropathy. Neurology. 2001;57:1701–4. doi: 10.1212/wnl.57.9.1701. [DOI] [PubMed] [Google Scholar]
- 26.Kikkawa Y, Kuwabara S, Misawa S, Tamura N, Kitano Y, Ogawara K, et al. The acute effects of glycemic control on nerve conduction in human diabetics. Clin Neurophysiol. 2005;116:270–4. doi: 10.1016/j.clinph.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 27.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 28.The Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes therapy on the development and progression of neuropathy. Ann Intern Med. 1995;122:561–8. doi: 10.7326/0003-4819-122-8-199504150-00001. [DOI] [PubMed] [Google Scholar]
- 29.Ghavami H, Ahmadi F, Mehin S, Meamarian R, Entezami H. Assessment of the relation between diabetic neuropathy and HbA1C concentration. Razi J Med Sci. 2007;13:141–7. [Google Scholar]


