Abstract
Background:
Functional constipation is one of the most prevalent childhood gastrointestinal disorders. We evaluated effects of adding a probiotic to mineral oil in the treatment of functional constipation in children.
Materials and Methods:
This controlled trial was conducted on 60 children (2 to 14 years old) with functional constipation (Rome III criteria). Children were allocated to receive the synbiotic (Lactol®, composed of Lactobacillus Sporogenes, 1 Tab/20 kg/d) plus mineral oil (Paraffin 1 ml/kg/d) or the mineral oil alone for two months. Symptoms of constipation including defecation frequency, stool form, strain and pain at defecation, incomplete evacuation and soiling were assessed and compared before and after the intervention. After the treatment period, the two groups were also compared with regards to subjective global assessment of improvement.
Results:
After the treatment, stool frequency increased in both groups (P < 0.001), with greater increase in synbiotic + mineral oil group (P = 0.001). Frequency of hard/very hard stool and frequency of painful defecation decreased similarly in both groups (P < 0.001). Straining at defecation, incomplete evacuation, and soiling decreased in both groups (P < 0.001), but more decrease was seen in the synbiotic + mineral oil group (P < 0.05). Finally, there was a better global improvement in the synbiotic + mineral oil group (P < 0.05). No severe side-effects were observed in any group.
Conclusion:
Adding the synbiotic Lactol® (containing Lactobacillus Sporogenes) to mineral oil can increase the improvement in the constipation symptoms of children without specific side-effects.
Keywords: Constipation, mineral oil, probiotics, synbiotics
INTRODUCTION
Constipation is one of the most prevalent gastrointestinal disorders among children with the reported prevalence varying from about 1-8% in the pediatric population. It accounts for 3-5% of visits to pediatricians and up to 25% of visits to pediatric gastroenterologists.[1] Disease burden and estimated healthcare costs are considerable and it can significantly impair quality of life of patients in both mental and physical health aspects.[2,3] In most of the cases (90-95%), no organic cause is found for constipation leading to the diagnosis of functional constipation in the child.[4] Thus, treatment strategy mainly involves educating the family and dietary modification. Disimpaction and maintenance oral/rectal medications are administered when needed. Common current medications for maintenance therapy include mineral oil, lactulose, milk of magnesia, polyethylene glycol powder, and sorbitol.[5,6] Because the etiology of the disease is not clearly understood, there is no specific treatment for functional constipation, and despite various treatments, only about half of the children with functional constipation demonstrate long-term improvement.[5]
There is growing interest about the efficacy of probiotics in the treatment of functional as well as organic gastrointestinal disorders. Probiotics have been reported to be effective in the treatment of various disorders including inflammatory bowel disease, irritable bowel syndrome, travelers’ diarrhea, and constipation. Because colonic microflora can affect the motility of the colon, an imbalance in the colonic microflora is proposed to have a role in the pathophysiology of chronic constipation. Also, some kind of probiotics, such as bifidobacteria and lactobacilli, by producing acids (lactic, acetic), result in lowering the pH of the colon, which in turn can enhance peristalsis of the colon and decrease colonic transit time.[7,8]
Several reports are available on the beneficial effects of probiotics on symptoms of constipation, mainly in adults.[8] Studies showed that probiotic strains, such as B. Infantis, increase defecation frequency and soften stools. However, limited information is available on the efficacy and safety of probiotics in the treatment of children with constipation and available studies have had controversial results.[8] We evaluated the effects of adding a synbiotic containing Lactobacillus Sporogenes strain to mineral oil in the treatment of functional constipation in children.
MATERIALS AND METHODS
Patients and setting
This controlled clinical trial was conducted on children referring with complaint of constipation to an outpatient clinic of pediatric gastroenterology, at the Alzahra University Hospital, Isfahan city (IRAN), from 2010 to 2011. Children 2 to 14 years of age diagnosed to have functional constipation based on the Rome III criteria were included consecutively.[9] Those with immunocompromised condition or other severe diseases, and those receiving antibiotic in the previous four weeks were not included.[10] Exclusion criteria included experiencing severe side-effects, gastroenteritis, or receiving antibiotic for any reason during the study period. Considering alpha = 5%, study power = 80%, and expecting at least one score change in stool consistency scale, the sample size was calculated as 25 subjects in each group. The study was approved by the ethics committee of the Azad University, Najaf Abad Branch, and informed consent was obtained from all children's parents. Also, the study was registered in the Iranian Registry of Clinical Trials (IRCT201207311579N1).
Intervention
Children were alternately allocated to the synbiotic and control groups. In the synbiotic group, subjects received synbiotic (Lactol®, Bioplus Life Sciences Pvt. 1 Tab/20 kg/d) plus mineral oil (Paraffin 1 ml/kg/d) for eight weeks. The synbiotic used in this study was composed of the following; Lactobacillus Sporogenes (15 × 107 Spores), Fructo-Oligosaccharides, Microcrystalline Cellulose, Sodium starch Glycolate, Povidone, Hypermellose Stearate, Sillicon Dioxide, and Propylene Glycol. Subjects in the control group received mineral oil (Paraffin 1 ml/kg/d) for eight weeks. Toilet training and dietary advice were equally administered for both groups.[11]
Assessments
Diagnosis of functional constipation was made according to the Rome III criteria by a pediatric gastroenterology specialist. The criteria were two or more of the following: 1) Two or fewer stools per week, 2) hard or very hard stools or painful stool, 3) Passage of very large stool, 4) Stool retention “once a week” or more often, 5) History of large fecal mass in rectum, and 6) Soiling “once a week” or more often. Those who fulfiled the criteria for irritable bowel syndrome were not included into the study.[9] A trained general physician interviewed with each subject, and a questionnaire including demographic data and symptoms of constipation, based on the Questionnaire on Pediatric Gastrointestinal Symptoms-Rome III Version, was completed.[12] Major symptoms included defecation frequency (1 = two times a week or less to 5 = more than three times a day), stool consistency (1 = very hard to 5 = watery), stool retention (yes/no), and painful defecation (yes/no). Other symptoms included urgency, straining, passing mucus, and feeling of incomplete evacuation which were scored from 0 (never) to 4 (always) and soiling which was scored from 0 (never) to 5 (every day). Subjects were interviewed at the end of the intervention (8th week) with the same questionnaire including compliance and side-effects as well, and a subjective global improvement (SGI) scale which was scored from 0 (significantly worsen) to 7 (completely improved).[13]
Statistical analyses
Data were analyzed using SPSS software for windows Version 16.0. Statistical tests included independent sample t-test for comparison of parametric data and Mann-Whitney test for comparison of non-parametric data between the two groups. Multivariate analysis using regression model was applied to find factors independently associated with global improvement. A P value of <0.05 was considered significant in all analyses.
RESULTS
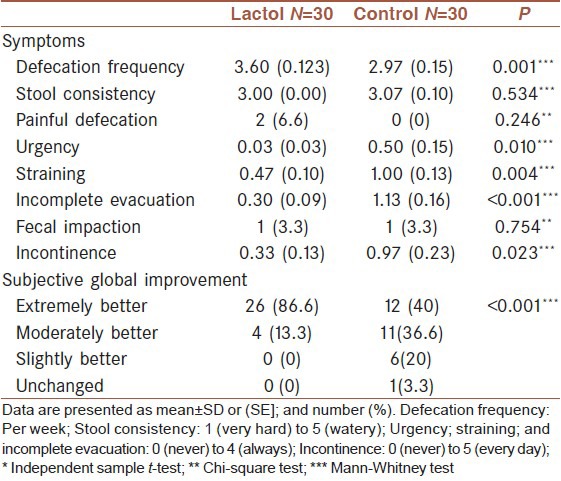
During the study period 30 children were included in each group (mean age = 5.0 ± 2.9 years, 55% female); all of them completed the study [Figure 1]. The two groups were similar in age, gender, and baseline symptoms except stool frequency which was slightly lower in the control group (P = 0.024) [Table 1]. After the study, there was a significant improvement in most symptoms of constipation in both the synbiotic and control groups. However, improvements were greater in the synbiotic group regarding defecation frequency (even after controlling for baseline difference by ordinal regression test), straining, sense of incomplete evacuation, and the frequency of fecal incontinence (P < 0.05 to <0.001) [Table 2]. According to the SGI scale, symptoms were moderately and significantly improved in 13.3% and 86.6% of the subjects respectively, in the symbiotic group, while in the control group, improvement of symptoms was moderate in 36.6% and significant in 40% of subjects, which showed a significantly better global improvement in the synbiotic group (P < 0.001) [Table 2].
Figure 1.
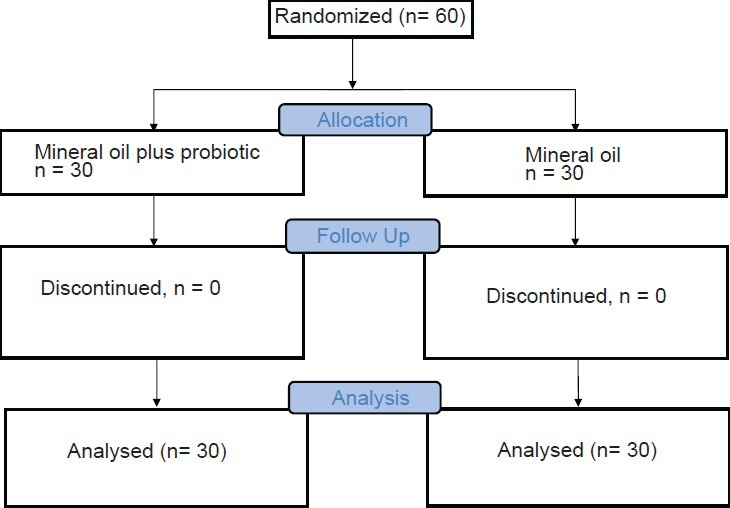
Patients flow diagram
Table 1.
Comparison of demographic data and baseline clinical characteristics between the two groups
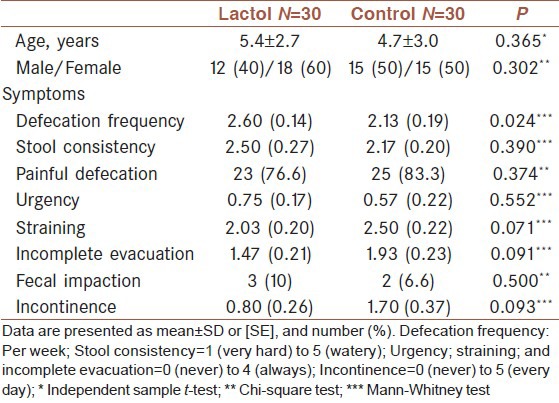
Table 2.
Comparison of symptoms at the end of intervention between the two groups
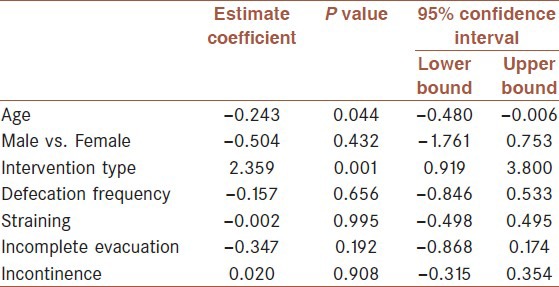
Multivariate analysis
According to a difference between the two groups in baseline defecation frequency, we conducted a multivariate analysis to find factors associated with SGI results by controlling age, gender, kind of intervention, and baseline symptoms. Among the mentioned factors, only receiving synbiotic plus mineral oil compared with mineral oil alone was significantly associated with more global improvement (estimate coefficient = 2.359, CI95%: 0.862 to 3.857, P = 0.002) [Table 3].
Table 3.
Regression ordinal model on possible predictors of global improvement
Side-effects
No severe side-effect was reported in any group. Reported side-effects were bloating (3.3%), diarrhea (3.3%), mild epigastric pain (3.3%), vomiting (3.3%), and abdominal pain plus itching and scar in the anal region in one case (3.3%). No side-effects were reported in the intervention group. There was no significant difference between the two groups in this regard.
DISCUSSION
The aim of the present study was to evaluate the effectiveness of adding probiotic to the conventional treatment of childhood functional constipation. According to the results, adding a synbiotic which contained Lactobacillus Sporogenes to mineral oil resulted in more improvement in several symptoms of constipation compared with mineral oil alone. These results were also observed by the global improvement scale. Multivariate analysis with control of baseline symptoms and age and gender also approved these results.
Limited data are available on the efficacy of probiotics in the treatment of constipation in children. In one study conducted by Bekkali and colleagues, children with functional constipation received a mixture of probiotics composed of Bifidobacteria and Lactobacili for 4 weeks. Results showed that the average of defecation frequency increased from 2/week at the beginning to 3.8/week at the end of the therapy. In contrast to our results, in the study by Bekkali et al., no significant change was observed in stool form. However, similar to our results, fecal incontinence decreased and no important side-effect was observed.[14] In another study by Bu and colleagues, children with constipation were allocated to three groups of Lactobacillus casei rhamnosus, Magnesium Oxide, and placebo. The results of this study showed that the probiotic was as effective as the magnesium oxide, while it did not have its possible side-effects.[15] In a study conducted by Khodadad and colleagues, children with constipation received Paraffin (1.5 ml/kg/d), synbiotic composed of Lactobacillus and Bifidobacteria, or a combination of synbiotic and Paraffin. The results showed that defecation frequency increased significantly in the combination group compared with the paraffin alone. But no beneficial effect was observed for stool form, incontinence, or painful defecation. Similar to our study, no side-effect was reported in the combination group while leakage of paraffin was a reported side-effect in those who received paraffin alone.[16] In contrast to the above mentioned trials showing the beneficial effects of probiotics in the treatment of childhood constipation, Banaszkiewicz and colleagues did not find beneficial effects of adding Lactobacillus GG to Lactose 70% over Lactose alone.[17] Differences among the results of available reports could be due to differences in the probiotic that was used; some studies used mixture compound while others used a single-strain probiotic. Therefore, further trials are needed in this regard. Available reports, however, are in favor of using probiotics as an adjunctive to other conventional therapies of childhood constipation. The possible mechanisms by which probiotics are beneficial in the treatment of constipation are not well studied. Available reports are focused on colonic transit time; however, more studies are needed in this regard.[8]
There are some limitations of our study. There was a difference between the two groups in baseline characteristics possibly because of alternate allocation which is not qualified as randomization; however, we conducted a multivariate analysis to control the covariates and the results confirmed the beneficial effects of adding synbiotic to mineral oil. Also, it was ethically not possible to run a placebo-controlled group which received placebo alone; however, it was possible to add a placebo in the mineral oil group and our study has an important limitation in this regard. Therefore, our study was not blinded and the possibility of investigator bias exists. And finally, we had no follow-up to investigate the long-term effects of the intervention.
CONCLUSIONS
The results of the present study showed that adding a synbiotic containing Lactobacillus Sporogenes to the routine treatment (mineral oil) of constipation in children can significantly increase improvement in symptoms, without specific side-effects. Further studies evaluating and comparing other synbiotic agents, either alone or along with other standard treatments, single or mixture of probiotics, and studies with longer follow-ups are warranted. Also, studies are needed on the possible mechanisms of action of probiotics in this regard.
ACKNOWLEDGMENTS
This study was collaboration between the Isfahan University of Medical Sciences and Azad University, Najaf Abad Branch. Authors are thankful to Noosh Darou Teb Co. (Tehran, IRAN) for helping us in providing the drugs.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Rubin G, Dale A. Chronic constipation in children. BMJ. 2006;333:1051–5. doi: 10.1136/bmj.39007.760174.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mugie SM, Di LC, Benninga MA. Constipation in childhood. Nat Rev Gastroenterol Hepatol. 2011;8:502–11. doi: 10.1038/nrgastro.2011.130. [DOI] [PubMed] [Google Scholar]
- 3.Belsey J, Greenfield S, Candy D, Geraint M. Systematic review: Impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31:938–49. doi: 10.1111/j.1365-2036.2010.04273.x. [DOI] [PubMed] [Google Scholar]
- 4.Greenwald BJ. Clinical practice guidelines for pediatric constipation. J Am Acad Nurse Pract. 2010;22:332–8. doi: 10.1111/j.1745-7599.2010.00517.x. [DOI] [PubMed] [Google Scholar]
- 5.North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Evaluation and treatment of constipation in children: Summary of updated recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006;43:405–7. doi: 10.1097/01.mpg.0000232574.41149.0a. [DOI] [PubMed] [Google Scholar]
- 6.Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician. 2006;73:469–77. [PubMed] [Google Scholar]
- 7.Menees S, Saad R, Chey WD. Agents that act luminally to treat diarrhoea and constipation. Nat Rev Gastroenterol Hepatol. 2012;9:661–74. doi: 10.1038/nrgastro.2012.162. [DOI] [PubMed] [Google Scholar]
- 8.Chmielewska A, Szajewska H. Systematic review of randomised controlled trials: Probiotics for functional constipation. World J Gastroenterol. 2010;16:69–75. doi: 10.3748/wjg.v16.i1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology. 2006;130:1527–37. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas DW, Greer FR. American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Section on Gastroenterology, Hepatology and Nutrition. Probiotics and prebiotics in pediatrics. Pediatrics. 2010;126:1217–31. doi: 10.1542/peds.2010-2548. [DOI] [PubMed] [Google Scholar]
- 11.Jennings A, Davies GJ, Costarelli V, Dettmar PW. Dietary fibre, fluids and physical activity in relation to constipation symptoms in pre-adolescent children. J Child Health Care. 2009;13:116–27. doi: 10.1177/1367493509102469. [DOI] [PubMed] [Google Scholar]
- 12.Walker LS, Caplan-Dover A, Rasquin-Weber A. Questionnaire on Pediatric Gastrointestinal Symptoms, Rome III Version (QPGS-RIII) In: Drossman DA, Corazziari E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, et al., editors. Rome III: The Functional Gastrointestinal Disorders. 3rd ed. McLean Virginia: Degnon Associates Inc; 2006. pp. 963–9. [Google Scholar]
- 13.Brandt LJ, Prather CM, Quigley EM, Schiller LR, Schoenfeld P, Talley NJ. Systematic review on the management of chronic constipation in North America. Am J Gastroenterol. 2005;100:S5–21. doi: 10.1111/j.1572-0241.2005.50613_2.x. [DOI] [PubMed] [Google Scholar]
- 14.Bekkali NL, Bongers ME, Van den Berg MM, Liem O, Benninga MA. The role of a probiotics mixture in the treatment of childhood constipation: A pilot study. Nutr J. 2007;6:17. doi: 10.1186/1475-2891-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bu LN, Chang MH, Ni YH, Chen HL, Cheng CC. Lactobacillus casei rhamnosus Lcr35 in children with chronic constipation. Pediatr Int. 2007;49:485–90. doi: 10.1111/j.1442-200X.2007.02397.x. [DOI] [PubMed] [Google Scholar]
- 16.Khodadad A, Sabbaghian M. Role of synbiotics in the treatment of childhood constipation: A double-blind randomized placebo controlled trial. Iran J Pediatr. 2010;20:387–92. [PMC free article] [PubMed] [Google Scholar]
- 17.Banaszkiewicz A, Szajewska H. Ineffectiveness of Lactobacillus GG as an adjunct to lactulose for the treatment of constipation in children: A double-blind, placebo-controlled randomized trial. J Pediatr. 2005;146:364–9. doi: 10.1016/j.jpeds.2004.10.022. [DOI] [PubMed] [Google Scholar]


