Abstract
Previous studies on the impact of migration on health often face the difficulties of choosing the proper comparison group and addressing potential selection of migration. Using longitudinal data from Indonesia, this paper examines the effect of rural-urban migration on physical and psychological health, (1) by comparing the health of migrants with that of the appropriate group of comparison, people who remained in rural origins, and (2) studying health both prior to and after migration to adjust for possible selection bias. This research further explores various socioeconomic, psychosocial, and behavioral pathways mediating the migration effect. Results show that rural-urban labor migration increased the risk of psychological disorder as measured by depressive symptoms. This was largely a result of reduced social support due to family disruption, because the deleterious effect was particularly strong for migrants who moved alone and was negligible for migrants moving with family members. In contrast, migration had little impact on physical health in the medium term. This was largely attributed to the multiple offsetting influences of migration: migration improved economic status and living standards but led to increased work-related stressors and barriers to health utilization. In addition, despite earning higher income, migrants tend to underconsume and remit a large amount of earnings to original families, which hindered potential health gains from improved economic well-being.
Introduction
The potential health consequences of rural-urban migration have not been well understood. This is in contrast to increasing attention to the health implications of growing immigration to the developed world. Accumulating evidence suggests that, despite immigrants’ socioeconomic disadvantages that are thought to compromise health status, they are generally healthier than the native-born population as indicated by mortality rates and various dimensions of physical and mental health (Hayward & Heron, 1999; Marmot, Adelstein, & Bulusu, 1984; Singh & Siahpush, 2001; Williams & Collins, 1995). This pattern is particularly true in the U.S., though a few exceptions have been documented in other developed societies (Newbold & Danforth, 2003; Sungurova, Johansson, & Sundquist, 2006).
The prevailing explanation for the better health profile of immigrants is the “healthy migrant hypothesis”, which states that migrants represent a selectively healthier group than the average sending and receiving population (Palloni & Morenoff, 2001). Because most existing data come from the destinations and are gathered after migration, earlier research could not test this hypothesis, and thus could not disentangle the impact of migration from possible health selection of migration. Instead, previous work has focused on comparing immigrants of varying durations of stay. Such studies usually present a detrimental impact of migration assimilation, as the health advantage enjoyed by immigrants tends to deteriorate over time (Abraido-Lanza, Chao, & Florez, 2005; Landale, Oropesa, & Gorman, 2000).
Towards a more complete understanding of the health consequences of migration, it is crucial to study within-country movement. Fuelled by increased urbanization in many developing settings, internal migration, in particular that from rural to urban areas, occurs at an even more unprecedented scale than international migration (International Organization for Migration, 2005). However, the scholarly work on internal migration and health is very scarce. It concentrates almost exclusively on child survival and produces mixed findings. For instance, Brockerhoff (1995) finds that across several developing countries, children of urban migrants experience higher risk of mortality than those of urban residents. This is in opposite to what is documented by Ssengonzi et al. (2002) in Africa.
Challenges of studying the health consequences of migration
The study of the migration effect poses several difficulties (Bilsborrow, Oberai, & Standing, 1984; Jasso et al., 2004). First, it is not straightforward to conceptualize the appropriate group for comparison because the movement involves both the origin and the destination. Earlier studies largely concentrate on comparisons between migrants and the population at destination, of which data are readily available. Nevertheless, the native population is not the proper counterfactual, as it conflates the effect of migration with the long-standing socioeconomic and health disparities between the often poor sending regions and the more developed receiving regions (Benatar, 1998). Such a comparison tends to overstate the plight of migrants while neglecting potential benefits of moving from poor to better environments. The more appropriate approach is to contrast the situation of migrants to the benchmark —their situation had they stayed in the origin. This can be accomplished by comparing migrants with “similar” people who had stayed in sending regions.
Second, migration studies are further complicated by potential migration selection, not only on demographic and socioeconomic characteristics but on health and other personal attributes. Failure to adjust for potential migration selection likely leads to biased results. In such situations, the observed effect is not necessarily evidence of a migration effect, but may arise from the selective feature of migrants on attributes that also affect health status. Because migrants are often favorably selected, one may incorrectly conclude with a positive migration effect if failing to control for pre-existing differences between migrants and non-migrants. A few studies explicitly test this “healthy migrant effect” and lend some support to this view (Lu, 2008a; Rubalcava et al., 2008). This highlights the need to take account of potential selection when studying the health effect of migration. One approach is to adjust for migrants’ pre-existing circumstances prior to migration through the use of longitudinal data.
The approach and the study setting
Facilitated by high-quality longitudinal data from the Indonesian Family Life Survey (IFLS), which traced migrants from origin to destination places, the present study simultaneously addresses the two difficulties discussed above. This is accomplished by comparing the health of migrants with that of people who remained at the origins, while adjusting for health status prior to migration. Because the effect of migration is necessarily multifaceted and tends to operate through a complexity of mechanisms, this study examines multiple aspects of health and assesses how various socioeconomic, psychosocial, and behavioral factors may mediate the migration effect. Given the great heterogeneity of migrants, the focus is placed on rural-to-urban labor migration, which involves a significant life change and sparks the most theoretical contention in the internal migration literature. It is also the stream that most resembles international migration to developed countries given the similar driving forces and dynamics (Pryor, 1981).
Indonesia, the fourth most populous nation in the world, is drawn on as a case study. The country has enjoyed rapid economic growth over the past three decades, along with concomitant improvements in health care and common measures of health such as life expectancy and infant mortality (Frankenberg & Thomas, 2001). In addition to government sources of care at hospitals, health centers, and village level posyandus (health centers for children and mothers), various sources of private health care coexist. The distribution of health facilities varies in rural and urban areas (Brotowasisto et al. 1988): government hospitals are located in district capitals, limiting their access to rural residents, who instead rely on health centers and posyandus as the basic source of primary care; private services are also more accessible in urban than in rural areas.
Important for the purpose of this study, Indonesia has rapidly urbanized, exceeding many other developing countries (United Nations 2002), and is recognized as one of the world’s major sources of unskilled migrant workers (Hugo, 2002). In the most recent census, one in ten Indonesians was classified as a migrant, roughly 23 million people. This stream is largely characterized by rural to urban and economically motivated migration, with the largest cities such as Jakarta, Surabaya, and Makassar as the main destinations. In comparison, the scale of international migration is relatively small, with about 2.5 million Indonesians working overseas.
Analytic Framework
Migration tends to have multiple impacts on different aspects of health, hurting in some respects and helping in others. The impact and mediating pathways are summarized in Figure 1. The impact of migration on psychological health tends to be detrimental and immediate as a result of the family separation due to migration (Sluzki, 1992). This disruption of family life likely leads to reduced size and level of social support, which costs migrants of their emotional well-being. This is consistent with the well-documented role of social support for health, which not only can have a direct and positive effect but can buffer the detrimental influences of various life stressors (Cohen and Wills 1985).
Figure 1.
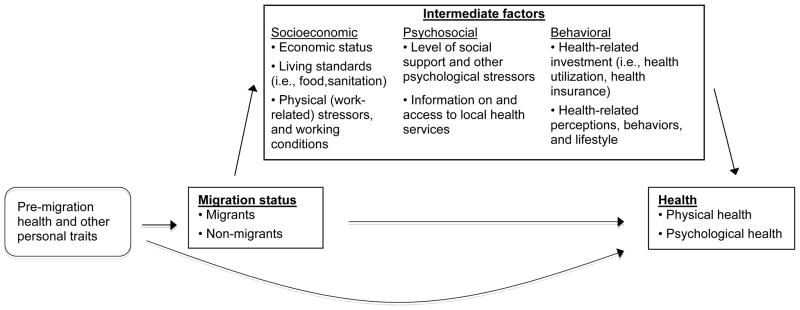
Health as a function of migration status and intermediate factors.
The impact of migration on physical health tends to be less immediate, as it is channeled through changes in living circumstances and behaviors in the course of migration and settlement. One of the most noticeable changes associated with labor migration is the economic benefits and subsequent improvement in living standards, as people typically migrate to attain better economic conditions. Such changes are usually conducive to health status. In addition, as a result of continued concentration of public health resources in urban areas, cities are generally equipped with better health infrastructures with greater availability than villages. This aspect of urban life can provide migrants with better health care services and may have positive implications for health.
However, the improved economics do not necessarily lead to improved use of health services. Health care system and resources can be complicated to navigate. A common scenario is that migrants may be less well informed about how much local health service is available, or how to access it (Newbold, 2005). It may take a fair amount of time for them to adjust to the new environment and begin using urban services effectively. The extent to which migrants make better use of health services also depends on their investment behavior. Potential improvements may be hindered if migrants curtail spending at the destination in order to send large remittances back to families at origin.
In addition, migrants often face increased life and work-related stressors and unfavorable working environments, as they have to cope with new conditions and are over-represented in labor-intensive jobs (Walsh & Walsh, 1987). The elevated stress tends to put migrants at higher risks for stress-related health deficits. Lastly, migrants are also exposed to different social and cultural contexts that may compel them to adjust to new perceptions, lifestyle, and behaviors, which can either be beneficial or disruptive (Lindstrom & Muñoz-Francoa, 2006).
On these grounds, I expect to observe a deleterious impact of migration on psychological health. As for physical health, the effect of migration is not clear, which should be understood as the consequence of the offsetting mechanisms mentioned above. To evaluate these conjectures, I first study the impact of migration on health indicators, and next explore various socioeconomic, psychosocial, and behavioral pathways. The latter step will also yield valuable information on migrants’ actual living circumstances at the destinations, of which very little is known.
Data and Methods
Data
Data used are from the 1997 and 2000 waves of the Indonesia Family Life Survey (IFLS), a high-quality panel survey of individuals, households and communities. The survey was conducted by the RAND Corporation and is publicly available. The IFLS was conducted in 13 out of 27 provinces in Indonesia, representing 83% of the population. The first round (IFLS1) was collected in 1993 and it included interviews with 7,224 households and 22,347 individuals (Frankenberg & Karoly, 1995). In each household, representative members provided detailed household demographic and socioeconomic information, and a few members were selected and interviewed on a broad range of topics.
In 1997, IFLS2 was conducted to reinterview all IFLS1 households and respondents (and also all members not interviewed in 1993) (Frankenberg & Thomas, 2000). The IFLS has very low sample attrition. It represents one of the first efforts in developing settings to track respondents who had moved out of their original households. IFLS2 succeeded in interviewing 94% of IFLS1 households and over 90% of target individuals, including over 1,500 respondents who had moved out and were successfully tracked in a new household. Following the practice of IFLS2, IFLS3, which was conducted in 2000, successfully interviewed over 90% of the households and over 80% of the individuals in both IFLS1 and IFLS2 (Strauss et al., 2004). The high follow-up rate substantially reduces data concerns that can arise from selective attrition.
The IFLS collected a broad array of demographic, socioeconomic, and health information on individuals, households, and communities. Much of these information was repeated across waves. Importantly, the IFLS contains detailed migration histories and a wide range of health indicators. In the migration history module, information on each trip longer than six months since age 12 and certain characteristics associated with each trip (e.g., date, purpose, whether moved with other family members) was gathered. In all three waves, self-reported health measures were available. IFLS2 and IFLS3 included additional physical assessments such as hemoglobin level and blood pressure, which are more accurate indicators of health than subjective reports. For this reason and because IFLS2 and IFLS3 included a larger number of respondents, the study mainly uses the second and third waves.
Measures of health
Health status is difficult to measure because the concept of health is multi-dimensional. For this reason, distinct indicators of health are examined separately. Self-reported general health was dichotomized to differentiate between good health and poor or fair health. ADL (Activities of daily living), an indicator of physical functioning, was the single measure available that reflected chronic health conditions and disabilities. It was coded 1 if the respondent reported having difficulties performing any of the nine tasks in the IFLS. Similarly, I constructed a dichotomous measure of self-reported minor conditions, from the series of questions: “whether you had any acute morbidity symptoms in the last four weeks” including fever, diarrhea, etc.
I also studied several physical assessment measures that are common health concerns in Indonesia. Underweight (a low level of Body Mass Index), an indicator of nutritional status and infectious diseases, was constructed as a dichotomous measure based on the WHO cut-off of BMI 18.5. Hypertension has multiple risk factors including unhealthy lifestyles and excessive stress. It was created using the standard cut-offs, a systolic blood pressure of at least 140 or a diastolic blood pressure of at least 90. Anemia, measured by hemoglobin level, is a measure of nutritional status and a chronic disease marker for adults. It was created using the WHO cut-off of 12g/dl for women and 13g/dl for men.
I studied mental health status with respect to depressive symptoms. The IFLS included a question designed to measure depressive symptoms, “have you experienced sadness in the last 4 weeks” in 2000, but not in 1997. It was treated as a dichotomous variable. Although the measure is less than ideal for studying depression, it has been adopted in other studies (Salomon et al., 2003), and is the only information available.
The rational for dichotomizing these measures is to evaluate health conditions based on clinically meaningful thresholds, rather than picking up small shifts, which can be within the normal range and may result from measurement errors. I conducted sensitivity analysis studying health as continuous wherever feasible, which did not change the findings.
Migration status
The major predictor, migration status, was constructed using information from the two consecutive waves on place of residence and the migration histories. I restricted the analysis to respondents who lived in rural areas in 1997 and focus on contrasting rural-to-urban migrants with rural non-migrants. An individual was considered a rural-to-urban migrant if the person moved from a rural area after the 1997 interview and lived in an urban area in 2000. Those who stayed in the same rural area and never moved between the two waves were considered rural non-migrants. I excluded return migrants (those moved out and then moved back) because they may contaminate the results if they returned home due to health deterioration (referred to as the “Salmon Bias”). I further distinguished rural-urban migrants for work-related reasons and for all other reasons, and compared them with rural non-migrants.
Other covariates
Other covariates include standard demographic and socioeconomic characteristics of the individual and household that may be important predictors of health and migration. They are controlled for throughout the analysis: age, gender, years of schooling, logged per capita annual household income, marital status, household size, household economic shocks (whether the household experienced any economic shocks in the past five years; directly available in the data); province of residence.
Measures of intermediate factors
Although not all of the intermediate factors in Figure 1 can be tested with the data at hand, some can, albeit sometimes with rough proxy measures. The economic condition was proxied by per capita household annual income. This variable was adjusted for inflation and log transformed in the analysis. I used the following indicators of household living standards and sanitation, following earlier work (Brockerhoff, 1995): (1) whether the floor was made of dirt; (2) whether the household used piped water as drinking water; (3) whether the household had flush toilet; and (4) weekly per capita expenditure on meat.
Physical stressor was proxied by the usual hours worked per week. As for information on health services, I used whether the household knew about where various types of local health facilities were located (hospital, health center, midwife, etc.). A continuous scale (0–9) counting the number of health facilities known was used. Behaviors factors measuring health-related investment included whether the respondent sought preventive health care (public and private) in the last month, and whether he or she had health insurance. I focused on preventive care because it is less contaminated by health conditions but more likely to reflect actual health utilization behaviors. In constructing this measure, I excluded care utilization for treatment of illness and medication. Health-related behavior was measured by whether the respondent was currently smoking. It would be desirable to examine other aspects of working conditions as well as health-related perceptions and lifestyles, but such measures were unavailable.
Statistical procedure
Two analytic approaches were undertaken to disentangle the migration effect from potential migration selection. I first compared the health status of rural-urban migrants with that of rural non-migrants in 2000, while controlling for their pre-migration health status and other characteristics in 1997 that may influence the propensity to migrate and later health. This was implemented using a form of dynamic regression, the lagged dependent variable model (LDV), where the lag of the dependent variable is included as an explanatory variable (Wooldridge, 2002). This approach effectively addresses possible selection bias to the extent preexisting (pre-migration) differences between migrants and non-migrants are captured in the lagged measure. I estimated robust standard errors to take account of clustering of multiple individuals within the same IFLS3 household (White, 1980). Some studies suggest that the LDV estimates are subject to state dependency when the lagged dependent variable is correlated with the disturbance. But empirical research demonstrates that such bias is usually small in practice (Keele & Kelly, 2006). Because mental health was not measured in 1997, this analysis used a variant of the LDV approach, by including a lag measure of self-reported general health as proxy. This was because previous work shows a strong association between self-report of general health and psychological ailments (Heidrich, 1993).
I also supplemented the LDV analysis using the fixed-effect models (FE), another way of adjusting for selection bias (Wooldridge, 2002). This is done by comparing the health change of rural-to-urban labor migrants with that of comparable rural non-migrants between successive IFLS waves, that is, before and after migration takes place. The FE models essentially use each individual as his or her own control, and purge out stable but unmeasured attributes at the individual-, family-, and community-level that may predispose migrants to worsen or improve their health over time. A caveat of the approach is that when the outcome is dichotomous, FE models delete individuals without outcome variations over time, which reduces the sample size. Although I cannot rule out all possible biases, examining results from both the LDV and FE models helps increase the confidence that the findings are not completely driven by selection bias.
RESULTS
Descriptive statistics
Table 1 presents the summary statistics for the sample—panel respondents aged 18–45 and lived in rural areas in 1997. I focused on this age group because they accounted for the bulk of rural-urban migration in Indonesia. This also avoids bias due to the possibility of older adults moving for health-related considerations (Lu, 2008a). The mean age of respondents was 30 in 1997, and males accounted for about 46% of the sample. The series of health deficits generally showed an upward trend, a result of the aging of the population. There is clear evidence that mental health problems, as measured by depressive symptoms, were prevalent in the country, exceeding most other health indicators.
Table 1.
Percentages and Means of Individual and Household Characteristics of the Sample by Survey Year: Indonesia Family Life Survey (1997 and 2000)
| 1997 | 2000 | |
|---|---|---|
| Health outcomes | ||
| Self-reported poor health | 7.5 | 10.6 |
| Problem with ADL | 18.2 | 22.4 |
| Minor morbidities last month | 75.2 | 77.0 |
| Hypertension | 18.6 | 20.7 |
| Anemia | 30.0 | 29.7 |
| Underweight | 16.1 | 13.8 |
| Experienced sadness last month | — | 30.3 |
| Covariates | ||
| Age | 29.7 | 32.9 |
| Male | 45.8 | 45.8 |
| Years of education | 5.9 | 6.1 |
| Marital status | ||
| Never married | 24.5 | 18.5 |
| Currently married | 71.9 | 77.1 |
| Other | 3.6 | 4.4 |
| Rural-urban migrants | — | 6.2 |
| HH size | 5.5 | 4.7 |
| HH economic shocks in past 5 years | 45.5 | 39.1 |
| Proximate health-related outcomes | ||
| Per capita HH annual income a | 1,348,807 | 1,566,491 |
| Usual weekly hours worked last yr. | 38.9 | 40.0 |
| Dirt floor | 25.6 | 19.4 |
| Piped water | 12.8 | 15.6 |
| Flush toilet | 28.1 | 31.4 |
| Weekly per capita meat expenditure a | 4,900 | 5,406 |
| Having health insurance | 7.8 | 7.6 |
| Used preventive health care last month | 4.7 | 4.6 |
| Currently smoking | 30.7 | 34.6 |
| HH information about local health facilities (scale 0–9) | 5.3 | 6.1 |
| N | 5,597 | |
Note. The sample consists of rural Indonesians aged 15–45 in the 1997 wave.
The measures are adjusted for inflation throughout the analysis and represents the real values based on December 2000 Jarkata price values. 1 U.S. dollar = 8,290 Indonesian Rupiah in 2000. 1kg of chicken or pork can be purchased for under 5,000 Rupiah.
As for intermediate factors, results show that in Indonesia, the sanitation infrastructures were inadequate, with only 15% of the respondents having used piped water and 30% having had own flush toilets. The use of health services and insurance coverage was also very limited. With respect to migration, rural-urban migration made up 6% of the sample. Most of them moved for work-related reasons. This is lower than the national-level migration rate (10%) because migration of other directions was not taken into account.
The sample attrition rate is roughly 20%, which is considered low since the sample consists of the most mobile young population. Additional analysis suggests that, after controlling for background factors, attrition is not associated with previous health conditions. As for missing data, most variables have only a few dozen with the exception of health outcomes. When taking into account all explanatory variables and the health outcomes, around 5% of the cases, or about 300 cases, were missing and the rate is similar for migrants and nonmigrants. This quantity of missing information is usually considered small. Thus, the analysis was based on complete cases for each outcome examined.
The effect of migration on psychological health
There is strong evidence of psychological costs associated with migration (Table 2). Labor migrants were much more likely to report depressive symptoms than non-migrants (OR=1.99, p<0.001), presumably due to family separation and reduced social support. To evaluate this conjecture, I disaggregated the dichotomous migration status to distinguish rural-urban labor migrants moving with (49%) and without family members (51%). If the psychological cost was a result of reduced social support, we should observe a stronger impact for migrants moving alone. This conjecture was supported by the analysis. The detrimental impact of migration on mental health existed only for solo migrants (OR=2.17, p<0.001), but not for migrants accompanied by family members (OR=1.99, p=0.28). It should be noted that this effect on mental health may be somewhat underestimated because the question on depressive systems was restricted to a short time frame. The effect for other types of migrants was less consistent, though the emotional costs of moving along seemed to remain. This was largely a result of the great heterogeneity among non-labor migrants, who may move for various different reasons (family-related reasons, marriage, social visit, etc.).
Table 2.
Results of Logitic Regressions Predicting Depressive Symptoms in 2000 on Rural-urban Migration Status between 1997–2000, Controlling for Initial Health Status and Other Characteristics in 1997: IFLS 1997–2000.
| Dependent variable (experienced sadness last month) | OR a (95% CI) Labor migrants |
OR b (95% CI) Other types of migrants |
|---|---|---|
| Overall sample | ||
| Dichotomous comparison (migrants vs. rural non-migrants) | 1.99 *** (1.33, 2.99) | 1.26 (0.86, 1.85) |
| By whether moving with other family members | ||
| Yes (vs. rural non-migrants) | 1.57 (0.69, 3.54) | 1.53 (0.94, 2.50) |
| No (vs. rural non-migrants) | 2.17 *** (1.37, 3.43) | 1.57 * (1.12, 2.22) |
| N | 5,380 | 5,392 |
| Males | ||
| Dichotomous comparison (migrants vs. rural non-migrants) | 2.15 *** (1.24, 3.72) | 0.73 (0.36, 1.47) |
| N | 2,369 | 2,350 |
| Females | ||
| Dichotomous comparison (migrants vs. rural non-migrants) | 1.84 *** (1.04, 3.27) | 1.74 * (1.08, 2.80) |
| N | 3,013 | 3,042 |
Note: Adjusted odds ratios and confidence intervals are shown. Other covariates are omitted from the table. They include age, gender, years of education, marital status, household size, economic shocks, log per capital household income, province of residence, and whether the respondent initially reported poor health, all of which are measured in 1997 prior to migration.
The regression models compare psychological health between rural-urban labor migrants and rural non-migrants, with the latter being the reference category.
The regression models compare psychological health between rural-urban migrants for other purposes and rural non-migrants, with the latter being the reference category.
p value < 0.001;
p value < 0.01;
p value < 0.05
When males and females were studied separately, the disruptive effect of labor migration on mental health held for both groups. I did not further disaggregate the sample to preserve sufficient cases. All above findings remained when I relaxed the age restriction and studied all adults. The estimates of other explanatory variables are not shown, but are generally as expected. Older people, males, and those of low SES were more likely to report depressive symptoms. Earlier self-reported general health strongly predicted mental health later in life.
To demonstrate the importance of using the proper group for comparison, I compared rural-urban migrants with urban non-migrants, which showed a much smaller difference between the two groups (OR=1.38, p=0.03). This was largely due to the higher prevalence of depressive symptoms in urban areas than in rural areas, because urbanicity was usually associated with more adverse social environment and greater awareness of mental well-being. As a result, the contrast between migrants and the receiving population (urban) conflated the effect of migration with the rural-urban disparities in mental health. This biased the migration effect estimates.
The effect of migration on physical health
Table 3 shows no clear effects of migration on physical health, with the exception of minor morbidities in the LDV model: rural-urban labor migration tended to increase the risk of contrasting acute morbidities. The findings were confirmed by several sensitivity analysis treating health outcomes as continuous, using differenced health status as the outcome, relaxing the age restrictions to study all adults, and estimating separate models for males and females. The LDV and FE models were very comparable, lending support to the robustness of the results.
Table 3.
Results of Dynamic Logistic Regressions and Fixed-effect Logistic Regression of Physical Health Status: IFLS 1997–2000.
| Dependent variables (health outcomes) | Dynamic models | Fixed-effect models | ||
|---|---|---|---|---|
|
| ||||
| OR a (95% CI) Labor migrants |
OR b (95% CI) Other types of migrants |
OR a (95% CI) Labor migrants |
OR b (95% CI) Other types of migrants |
|
| Self-reported poor health | 0.67 (0.29, 1.55) | 1.11 (0.58, 2.15) | 1.42 (0.25, 8.01) | 1.19 (0.42, 3.37) |
| Problem with ADL | 0.98 (0.59, 1.62) | 1.35 (0.88, 2.05) | 1.99 (0.61, 6.52) | 1.04 (0.52, 2.10) |
| Minor Morbidities last month | 1.76 * (1.01, 3.07) | 0.97 (0.61, 1.52) | 1.15 (0.50, 2.68) | 0.73 (0.36, 1.48) |
| Hypertension | 1.06 (0.56, 2.00) | 0.86 (0.52, 1.44) | 0.72 (0.28, 1.87) | 0.71 (0.29, 1.69) |
| Anemia | 1.06 (0.65, 1.75) | 0.89 (0.57, 1.39) | 1.06 (0.46, 2.43) | 0.90 (0.47, 1.71) |
| Underweight | 0.83 (0.37, 1.91) | 1.71 (0.94, 3.10) | 0.63 (0.19, 2.14) c | 0.93 (0.34, 2.60) d |
| N | 5,380 | 5,392 | ||
Note: Adjusted odds ratios and confidence intervals are shown. The first two columns present results from dynamic models predicting physical health in 2000 on rural-urban migration status between 1997–2000, controlling for initial health status and other characteristics in 1997. Other covariates are omitted from the table (same as Table 2). The last two columns present results from the corresponding fixed-effect models, with the same set of control variables.
The regression models compare each health outcome between rural-urban labor migrants and rural non-migrants, with the latter being the reference category.
The regression models compare each health outcome between rural-urban migrants for other purposes and rural non-migrants, with the latter being the reference category.
The sample sizes of the fixed-effect models are reduced by design and vary by health outcomes. They are, respectively, 1518, 2686, 2448, 1756, 2766, and 1030.
The sample sizes of the fixed-effect models are reduced by design and vary by health outcomes. They are, respectively, 1538, 2732, 2468, 1764, 2800, and 1042.
p value < 0.05
The estimates of other explanatory variables are not shown, but are generally as expected. Aging led to worse health conditions, whereas higher socioeconomic status improved health. The initial health status was a strong predictor of later health. The dearth of an effect on physical health in the short- and medium-term is not entirely surprising. Because labor migrants consist of a young age group, migration may have long-term effects on physical health later in life as they start experiencing diminished physiological functions.
Multiple effects of migration on intermediate factors
To offer more insight into the health consequences of migration, I examined whether labor migration affects intermediate socioeconomic, psychosocial, and behavioral factors. A similar set of linear and logit LDV and FE models was used, which treated the mediating factors as the outcomes and controlled for the same set of covariates. The results from the two sets of estimates were highly comparable (Table 4). They illustrate both the benefits and costs of migration and help explain the lack of a migration effect on physical health.
Table 4.
Results of Dynamic Regressions and Fixed-effect Regressions of Intermediate Health-related Outcomes: IFLS 1997–2000.
| Dependent variables (intermediate health- related outcomes) | Dynamic models | Fixed-effect models | ||
|---|---|---|---|---|
|
| ||||
| OR or b
a (95% CI) Labor migrants |
OR b or b (95% CI) Other types of migrants |
OR or b
a (95% CI) Labor migrants |
OR b or b (95% CI) Other types of migrants |
|
| Economic status and work stressors | ||||
| Log (per capita HH annual income) c | 0.97 *** (0.49, 1.53) | −5.12 *** (−6.38, −3.86) | 1.24 * (0.29, 2.20) | −5.37 *** (−6.32, −4.42) |
| Usual weekly hours worked last yr c, d | 13.78 ** (4.99, 22.6) | 0.10 (−6.52, 6.73) | 15.24 ** (5.83, 24.65) | −0.64 (−11.12, 9.85) |
| Living Standards | ||||
| log(weekly per capita meat expenditure) c | −2.81 *** (−3.74, −1.87) | −2.21 *** (−3.07, −1.35) | −2.35 *** (−2.86, −1.84) | −2.02 *** (−2.51, −1.54) |
| Piped water | 6.41 *** (3.97, 10.36) | 3.95 *** (2.10, 7.41) | 3.89 *** (1.90, 7.94) | 1.78 * (1.01, 3.13) |
| Flush toilet | 3.44 *** (2.10, 5.65) | 2.24 ** (1.35, 3.70) | 2.74 *** (1.56, 4.80) | 1.17 (0.67, 2.01) |
| Dirt floor | 0.08 ** (0.20, 0.34) | 0.09 *** (0.03, 0.32) | 0.27 † (0.07, 1.07) | 0.13 † (0.01, 1.18) |
| Health-related information, investment and behaviors | ||||
| HH information about local health facilities c | −1.47 *** (−1.91, −1.04) | −0.98 *** (−1.38, −0.58) | −1.40 *** (−1.79, −0.99) | −0.86 *** (−1.24, −0.48) |
| Having health insurance | 4.59 *** (2.15, 9.82) | 1.59 (0.62, 4.06) | 1.75 (0.71, 4.31) | 0.97 (0.39, 2.41) |
| Used preventive health care last month | 1.16 (0.78, 1.72) | 0.71 (0.44, 1.14) | 0.85 (0.28, 2.58) | 0.77 (0.25, 2.39) |
| Currently smoking | 1.21 (0.67, 2.17) | 0.52 (0.23, 1.18) | 1.84 (0.76, 4.45) e | 2.03 (0.35, 11.87) f |
| N | 5,380 | 5,392 | ||
Note: Adjusted odds ratios or linear regression coefficients and associated confidence intervals are shown. The first two columns present results from dynamic models predicting proximate health-related outcomes on rural-urban migration status between 1997–2000, controlling for initial conditions and other characteristics in 1997. Other covariates are omitted from the table (same as Table 2). The last two columns present results from the corresponding fixed-effect models, with the same set of control variables.
The regressions compare proximate health-related outcomes between rural-urban labor migrants and rural non-migrants, with the latter being the reference category.
The regressions compare proximate health-related outcomes between rural-urban migrants for other purposes and rural non-migrants, with the latter being the reference category.
Indicate dynamic linear regression models. All others are dynamic logistic regression models.
The sample size is 3,186 because the question is restricted to respondents who were currently working at the time of the interview.
The sample sizes of the fixed-effect models are reduced by design and vary by health outcomes. They are, respectively, 5673, 2577, 5703, 1624, 2636, 476, 5703, 1482, 1064, and 744.
The sample sizes of the fixed-effect models are reduced by design and vary by outcomes. They are, respectively, 5771, 2569, 5720, 1640, 2632, 450, 5720, 1474, 1062, and 748.
p value < 0.001;
p value < 0.01;
p value < 0.05;
p value < 0.1
There were unambiguous economic gains from migration, with labor migrants earning twice as much as rural non-migrants. However, the higher earnings came with a cost, as migrants faced much longer working hours. They usually worked 15 hours longer per week than rural non-migrants, which may have adverse health effects.
There is clear evidence that migrants in Indonesia improved household sanitation by moving to cities. Migrants were more likely than rural stayers to live in dwelling units that have piped water, flush toilet, and durable floor material. In retrospect, this reflected the greater availability of hygienic facilities in urban areas. This finding is consistent with previous work that shows while some migrants are found in urban slum areas, many manage to stay away and live in typical dwelling units similar to urban residents, in factory dormitories, or with urban families (domestic service workers) (Akiyama & Larson, 2004). However, migrants seemed to spend less on meat products, which may be due to the higher costs of living and the need to save for remittances, as sanctioned by local culture that emphasizes interdependence.
Migrants seemed more likely to have insurance coverage, because health insurance in Indonesia was made available primarily through urban employers. A likely consequence is that migrants are more willing to seek treatment when they fall ill. This improvement, however, was likely offset by the unfamiliarity with local health facilities, as migrants experienced deterioration in health information. While this result is as expected, it does reveal a real danger for migrants—if they encountered health difficulties they would probably not know where to get medical attention.
The use of preventive health care was not influenced by migration. This perhaps resulted from the fact that migrants often came from places where health utilization is limited and health care is traditionally confined to treating disease. Migrants’ use of modern health care may be further hindered by factors such as higher costs of health services in cities, unfamiliarity with local health facilities, and the need to save for remittances. Results for other types of migrants revealed some expected differences. Because they moved for non-work related reasons, the economic benefits, increased work stressors, and employment-based insurance advantage disappeared.
Discussion
Over the past few decades, migration has become an integral feature of the national economy and family life in many parts of the developing world. A core element in assessing the consequences of migration is to understand its impact on social well-being with respect to health, as it is critical in facilitating migrants’ socioeconomic attainments and integration into host communities. This paper has exploited longitudinal data to study the effect of rural-urban migration on health. It extends the literature by examining the understudied internal migration, considering the multiple impacts of migration on various dimensions of health (physical and psychological), uncovering underlying mechanisms, and simultaneously addressing potential migration selection and using the proper group for comparison.
Results showed an adverse effect of migration on psychological health, as measured by depressive symptoms. This was largely due to family separation because the effect was restricted to migrants moving alone. In contrast, migration had no clear impact on physical health, at least in the medium term. The effect was not immediate because it was largely channeled through various offsetting mechanisms. I showed that the economic benefits and improved living standards associated with rural-urban migration occurred in the context of considerable physical and psychological stressors and health utilization barriers. While the positive aspects of migration could lower the risks of morbidities and improve health environment and health care opportunities in general, the negative sides may very well have unfavorable health consequences such as stress-related health deficits and underuse of health services. Given that health has multiple contributing factors, these offsetting effects led to little concomitant change in overall physical health status. By contrast, the detrimental impact of migration was clearly manifested in psychological health, which is a more direct consequence of migration and requires a shorter time lag. In the long run, these psychological health costs may also be implicated in physical health.
The results also challenged the anticipated association between migrants’ economic gains and health. Findings suggest that the association does not only depend on whether migrants eventually achieve better economic status, but on whether migrants use increased income to make a serious investment in health. In Indonesia, migrants tended to underconsume at destination places but remit a large fraction of earnings to original families. This reduced their disposable income and hindered potential health gains from improved economic conditions. Specifically, the data showed that over 85% of rural-urban labor migrants sent money to family members living apart in the past year, and the amount of monetary transfers accounted for almost 50% of their total income. Hence, family income may not be an accurate reflection of the financial resources available to the migrants. This result highlights the importance of considering the circumstances under which sending remittances may constitute a burden on migrants and reduce their resources for expenditures, when studying the outcomes and attainment of migrants.
A few limitations need to be acknowledged. The relative small sample size of migrants limit my ability to further differentiate the analysis by a combination of factors such as gender, reasons for migration, durations of stay, and whether moving with family members. Additionally, information on a few important intermediate factors is missing (i.e., job characteristics, health-related knowledge, and perceptions). I will be able to address some of these limitations with the upcoming wave of the IFLS (IFLS4). The data will offer a larger sample of migrants and provide basis for examining the long-run impact of migration. It will also allow me to incorporate better measures of mental health and intervening factors.
While the dearth of the migration effect on physical health is largely a result of the offsetting pathways, other explanations might also contribute to this finding, though they cannot be directly tested. The study sample, a relatively younger group (18–45), may show great resilience to health risks. A likely outcome is that migration will have long-term effects on physical health as migrants age and start experiencing diminished physiological function.
Overall, the study identifies several important challenges facing migrants including the psychological distress, information barriers, and limited use of preventive care, all of which may have far-reaching health implications. Migrants would benefit from programs that help them cope with family separation and rebuild social ties in destination places. This can be accomplished by improving access to communication and transportation services that foster regular communication between migrants and families left behind. Another way of helping migrants overcome psychological burdens is through local mobilization that offers emotional and social support among migrants. Further, interventions that help disseminate information on the availability of and ways to access local health services and that promote preventive health screening and use would considerably eliminate health-related information barriers while improving health utilization among migrants in general.
This research demonstrates that the influence of migration tends to depend on the broader socioeconomic context within which migration occurs. The present study examines one developing setting. To advance the themes addressed here, comparative work in other socioeconomic contexts will be particularly illuminating. Considerable similarities across settings are expected, as migration streams are largely generated by similar forces (economic) and, hence, lead to similar circumstances. Nevertheless, institutional variations across settings likely imply a different set of constraints. While internal migration in Indonesia represents an example of “open” movement, there are many well-established examples of “constrained” migration that are fundamentally hampered by restrictive migration policies and associated legal and social barriers (i.e., international migration to developed countries, the hukou system and internal migration in China, the influx control in South Africa during apartheid). Such institutional factors tend to have direct health consequences such as the limited access to health and social services, which may render migrants especially vulnerable to health risks. Therefore, the health consequences of migration may be manifested in distinct ways across diverse socio-cultural environments.
While comparative research should be conducted to assess the generalizeability of the findings, the study design I have used is applicable across settings. One major goal of this research is to lay out a systematic framework and an analytic approach that is adaptable elsewhere, rather than to develop a model specific to the Indonesian setting. The approach utilized represents a more appropriate analytic strategy for understanding the impacts of migration on health than many earlier studies. This is largely facilitated by high quality longitudinal data with comprehensive information on migration, health, and intermediating factors. I hope this study motivates more data collection efforts, not only quantitative data but in-depth interviews, that permit better exploration of questions related to migration and health.
Footnotes
An earlier version of this paper was presented at the Annual Meeting of the Population Association of America, New Orleans, April 2008. The author would like to thank the senior editor and anonymous reviewers for their helpful comments.
References
- Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science and Medicine. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akiyama T, Larson DF. Rural development and agricultural growth in Indonesia, the Philippines and Thailand. Washington, D.C: World Bank; 2004. [Google Scholar]
- Benatar SR. Global disparities in health and human rights: a critical commentary. American Journal of Public Health. 1998;88:295–300. doi: 10.2105/ajph.88.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilsborrow RE, Oberai AS, Standing G. Migration surveys in low-income countries: guidelines for survey and questionnaire design. London: Routledge Kegan & Paul; 1984. [Google Scholar]
- Brockerhoff M. Child survival in big cities: the disadvantages of migrants. Social Science and Medicine. 1995;40:1371–1383. doi: 10.1016/0277-9536(94)00268-x. [DOI] [PubMed] [Google Scholar]
- Brotowasisto OG, Malik R, Sudharto P. Health care financing in Indonesia. Health Policy and Planning. 1988;3:131–40. [Google Scholar]
- Cohen S, Willis T. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Frankenberg E, Karoly L. Publication No DRU-1195/1-NICHD/AID. Santa Monica, CA: Rand Corporation; 1995. The 1993 Indonesian Family Life Survey: Overview and field report. [Google Scholar]
- Frankenberg E, Thomas D. Publication No DRU-2238/Volume1/NIA/NICHD. Santa Monica, CA: Rand Corporation; 2000. The Indonesia Family Life Survey (IFLS): study design and results from waves 1 and 2. [Google Scholar]
- Frankenberg E, Thomas D. Women’s health and pregnancy outcomes: Do services make a difference? Demography. 2001;38:253–265. doi: 10.1353/dem.2001.0014. [DOI] [PubMed] [Google Scholar]
- Frisbie WF, Youngtae C, Hummer RA. Immigration and the health of Asian and Pacific Islander adults in the United States. American Journal of Epidemiology. 2001;153:372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Heron M. Racial inequality in active life among adult Americans. Demography. 1999;36:77–91. [PubMed] [Google Scholar]
- Heidrich SM. The relationship between physical health and psychological well-being in elderly women: a developmental perspective. Research in Nursing and Health. 1993;16:123–130. doi: 10.1002/nur.4770160207. [DOI] [PubMed] [Google Scholar]
- Hugo G. Effects of international migration on the family in Indonesia. Asian and Pacific Migration Journal. 2002;11:13–46. [Google Scholar]
- International Organization for Migration. Internal migration and development: a global perspective. IOM; Geneva, Switzerland: 2005. Migration Research Series 19. [Google Scholar]
- Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press; 2004. pp. 227–266. [PubMed] [Google Scholar]
- Keele L, Kelly NJ. Dynamic models for dynamic theories: the ins and outs of lagged dependent variables. Political Analysis. 2006;14:186–205. [Google Scholar]
- Landale N, Oropesa RS, Gorman BK. Migration and infant death: assimilation or selective migration among Puerto Ricans? American Sociological Review. 2000;65:888–909. [Google Scholar]
- Lindstrom DP, Muñoz-Francoa E. Migration and maternal health services utilization in rural Guatemala. Social Science and Medicine. 2006;63:706–721. doi: 10.1016/j.socscimed.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Lu Y. Test of the “healthy migrant hypothesis”: a longitudinal analysis of health selectivity of internal migration in Indonesia. Social Science and Medicine. 2008;67:1331–1339. doi: 10.1016/j.socscimed.2008.06.017. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Adelstein MA, Bulusu L. Lessons from the study of immigrant mortality. Lancet. 1984;323:1455–1457. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- Newbold KB. Health status and health care of immigrants in Canada: a longitudinal analysis. Journal of Health Services Research and Policy. 2005;10:77–83. doi: 10.1258/1355819053559074. [DOI] [PubMed] [Google Scholar]
- Newbold B, Danforth J. Health status and Canada’s immigrant population. Social Science and Medicine. 2003;57:1981–1995. doi: 10.1016/s0277-9536(03)00064-9. [DOI] [PubMed] [Google Scholar]
- Palloni A, Morenoff J. Interpreting the paradoxical in the “Hispanic paradox”: demographic and epidemiological approaches. In: Weinstein M, Hermalin A, Stoto M, editors. Population Health and Aging. New York: New York Academy of Sciences; 2001. pp. 140–74. [DOI] [PubMed] [Google Scholar]
- Pryor RJ. Integrating international and internal migration theories. In: Kritz MM, Keely CB, Tomasi SM, editors. Global trends in migration: theory and research on international population movements. New York: Center for Migration Studies; 1981. pp. 110–129. [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: new findings from the Mexican Family Life Survey. American Journal of Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Murray C, Ustun TB, Chatterji S. Health state valuations in summary measures of population health. In: Murray C, Evans D, editors. Health systems performance assessment: debate, methods and empiricism. Geneva: World Health Organization; 2003. pp. 407–420. [Google Scholar]
- Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health. 2001;91:392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sluzki CE. Disruption and reconstruction of networks following migration/relocation. Family Systems Medicine. 1992;10:359–363. [Google Scholar]
- Ssengonzi R, De Jong G, Stokes S. The effect of female migration on infant and child survival in Uganda. Population Research and Policy Review. 2002;21:403–431. [Google Scholar]
- Strauss J, Beegle K, Sikok B, Dwiyanto A, Herawati Y, Witoelar F. Publication No WR-144/1-NIA/NICHD. Santa Monica, CA: Rand Corporation; 2004. The third wave of the Indonesia Family Life Survey (IFLS3): overview and field report. [Google Scholar]
- Sungurova Y, Johansson SE, Sundquist J. East-west health divide and East-west migration: self-reported health of immigrants from Eastern Europe and the former Soviet Union in Sweden. Scandinavian Journal of Public Health. 2006;34:217–221. doi: 10.1080/14034940500327406. [DOI] [PubMed] [Google Scholar]
- United Nations. Human development report 2002: deepening democracy in a fragmented world. New York: United Nations; 2002. [Google Scholar]
- Walsh A, Walsh PA. Social support, assimilation, and biological effective blood pressure levels. International Migration Review. 1987;21:577–591. [Google Scholar]
- White H. A Heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–30. [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual Reviews in Sociology. 1995;21:349–386. [Google Scholar]
- Wooldridge J. Econometric analysis of cross section and panel data. Cambridge, Mass: MIT Press; 2002. [Google Scholar]


