Abstract
Exophytic retinal capillary hemangiomas (RCH) can be a diagnostic challenge in subjects without von Hippel-Lin-dau disease (VHL). This report of two cases describes the optical coherence tomographic (OCT) characteristics of RCH in two eyes of a subject with VHL and in one eye of an otherwise normal subject. Three different OCT instruments were used (Stratus, Cirrus and/or custom high resolution Fourier-domain OCT with 4.5 μm axial resolution) depending on availability. All instruments localized the tumor to the outer retina. A sharp border between the tumor and overlying inner retina was noted. The tumor bulged into the subretinal space and showed marked shadowing. Associated cystoid macular edema and sub-retinal fluid were noted. High-resolution Fourier-domain OCT showed a focal photoreceptor layer rip in the adjacent tumor-free macula in one eye with poor vision after treatment. OCT may be a useful tool in diagnosing RCH and studying associated morphologic changes.
INTRODUCTION
Retinal capillary hemangioma (RCH) is a clinically and histopathologically distinct tumor that may occur sporadically or as a manifestation of von Hippel-Lindau disease (VHL). These tumors are often endophytic and peripheral spherical masses classically associated with a dilated tortuous feeding artery and a draining vein.1 Alternatively, RCH may be exophy-tic and arise from the outer retinal layers. Exophytic tumors are not usually associated with arteriovenous shunting. They tend to develop in the juxtapapillary region and is frequently misdiagnosed as papilledema, choroidal neovascularization or tumors of the retinal pigment epithelium or choroid.1 In this report of two cases (three eyes) of exophytic RCH that were imaged with Stratus (Zeiss, Time-domain OCT) or one of two Fourier-domain optical coherence tomography (Fd-OCT) systems-(Zeiss, Cirrus or custom high-resolution Fd-OCT instrument made at our institution with 4.5 μm axial resolution and 10 to 15 μm transverse resolution2), we show that OCT localized the tumor to the outer retinal layers and helped differentiate it from other simulating tumors. In addition, morphologic changes in the surrounding tumor-free macula could be appreciated that may be predictive of visual outcome after treatment.
REPORT OF CASES
Case 1
A 13-year-old girl with VHL presented with gradual vision loss OS for 6 months. Examination revealed a best-corrected visual acuity (BCVA) of 20/20 OD and 20/400 OS. Fundoscopic examination OD showed a well-circumscribed pale orange lesion superior-temporal to the macula with exudation into the macula (Fig. 1A). Fundoscopic examination OS showed a similar spherical orange-red macular lesion adjacent to the optic disc with some retinal hemorrhage and serous macular detachment (Fig. 1B). Fluo-rescein angiography showed intense hyperfluorescence of the lesions with minimal leakage in late views (Figs. 1C, D). Fd-OCT (Zeiss, Cirrus) images of both eyes showed a round mass with dense shadowing contiguous with the outer retina protruding into the subretinal space with adjacent cystoid macular edema (Fig. 1E). In addition, submacular fluid was noted OS (Fig. 1F).
Figure 1.
(A) Fundus photograph OD of Case #1 showing a sub-retinal mass and a circinate ring of exudates extending to the fovea. (B) Fundus photograph OS of Case #1 showing a peripapillary submacular mass. (C) and (D) Fluorescein angiography of OD and OS, respectively, showing intense hyperfluorescence of the mass with minimal leakage. (E) Cirrus Fourier-domain optical coherence tomography (Fd-OCT) image of the subretinal mass OD showing a lesion contiguous with the outer retina with dense shadowing with adjacent cystoid macular edema. (F) Cirrus Fd-OCT image of subretinal mass OS showing a lesion contiguous with the outer macula with dense shadowing. Adjacent cystoid macular edema and subretinal fluid are also seen.
Case 2
A 19-year-old woman presented with vision loss OS for over 3 months. Examination revealed a BCVA of 20/20 OD and 20/400 OS. Fundoscopic examination was normal OD, but OS showed a peripapillary subretinal mass with some overlying gliosis and associated serous macular detachment (Fig. 2A). Some retinal hemorrhages were noted adjacent to the tumor. Fluorescein angiography showed intense hyper-fluorescence of the lesion with minimal late leakage (Fig. 2B). Stratus OCT showed subretinal fluid involving the macula (Fig. 2C) with a peripapillary round mass bulging from the outer retina into the subretinal space with intense shadowing. The detached retina adjacent to the tumor appeared to have focal loss of the outer retinal layers. High-resolution Fd-OCT of the tumor obtained after informed consent showed similar intense shadowing of the mass continuous with the outer retina (Fig. 2D). The detached macula adjacent to the tumor showed extensive disruption of the photoreceptor layer, which was partially ripped from the inner retina (Fig. 2E). Thermal laser photocoagulation of the tumor resulted in complete resolution of the subretinal fluid after 4 weeks, but thinning of the central macula was noted on Stratus OCT (Fig. 3A). Visual acuity remained 20/400 after six months. High-resolution Fd-OCT image obtained after informed consent showed diffuse loss of photoreceptor layer in the macula adjacent to the regressed tumor (Fig. 3C).
Figure 2.
(A) Fundus photography OD of Case # 2 showing a peripapillary subretinal mass with associated retinal striae and hemorrhages, and serous macular detachment. Some peripapillary subretinal gliosis is seen over the mass. (B) Fluorescein angiography showing intense late view hyperfluorescence of the mass with minimal leakage. (C) Stratus Optical Coherence Tomography (OCT) image OS showing the mass contiguous with the outer retina with associated macular detachment. The macula adjacent to the mass (*) shows loss of the outer retinal layers. (D) High resolution Fourier-domain OCT image OS showing a peripapillary round mass bulging from the outer retina into the subretinal space with intense shadowing. (E) High resolution Fourier-domain OCT image of the left macula (*) adjacent to the mass showing severe disruption of the photoreceptor layer which appears partially ripped from the overlying detached macula (arrow). The high resolution Fourier-domain OCT instrument used was developed at the University of California Davis and provides axial resolution of 4.5 μm and transverse resolution 10 to 15 μm.2 ON—optic nerve; RCH—retinal capillary hemangioma
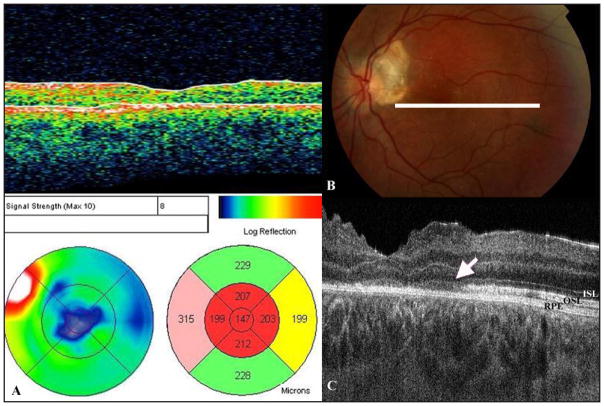
Figure 3.

(A) Stratus Optical Coherence Tomography (OCT) image OS of Case #2 4 weeks after thermal laser photocoagulation of the retinal hemangioma showing complete resolution of the macular detachment and some thinning of the macula. (B) Fundus photography OS of Case #2 after laser treatment. The white line represents the orientation of the scan in Fig 3C. (C) High resolution Fourier-domain OCT image OS of Case # 2 6 months after laser treatment showing diffuse loss of the outer segment layer photoreceptors in the central macula (arrow). ISL-- inner segment layer; OSL-- outer segment layer; RPE-- retinal pigmented epithelium
COMMENT
A solitary RCH may be idiopathic or associated with VHL irrespective of growth pattern and location of the tumor.1,3 The diagnosis of exophytic RCH can be challenging in patients without known VHL because these lesions grow into the subretinal space and lack the characteristic feeder vessels associated with endo-phytic RCH. Currently, fluorescein angiography is a valuable tool in characterizing the vascular nature of RCH and in distinguishing it from some simulating entities. However, angiographic findings are not specific to RCH and fluorescein angiogram cannot localize this tumor to the outer retina. Thus, diagnosis of a solitary exophytic RCH remains a challenge.4 The present report shows the OCT characteristics of exophytic RCH, which may aid in diagnosis of this condition. All three OCT instruments localized the tumor to the outer retina. In addition, intense shadowing of the tumor was noted on OCT due to its high flow and vascularity. These features help differentiate it from other stimulating entities, such as choroidal neovascular membranes or tumors of the retinal pigment epithelium or choroid.1,4
In the second case, thermal laser treatment resulted in complete resolution of the subretinal fluid. However, visual acuity remained poor after treatment. High-resolution Fd-OCT showed diffuse loss of photoreceptors in the macula. This may be from chronic retinal detachment or damage to the papillomacular bundle from thermal laser. However, pre-treatment Fd-OCT showed a rip in the macular photoreceptor layer adjacent to RCH, possibly secondary to traction from growth of the adjacent tumor. This morphologic change is likely to be a poor prognostic sign for visual recovery after therapy. Photoreceptor loss, cystoid macular edema, pre-retinal traction and disorganization of the adjacent retina have been described on Stratus OCT imaging of eyes with other intraocular tumors.5–7 Our case demonstrates that photoreceptor layer rip and disinsertion from inner retinal layers adjacent to tumor can occur in some eyes with exophytic RCH. This morphologic change was noted pre-treatment using the custom high-resolution Fd-OCT made at our institution but not appreciated on Stratus OCT, which has lower image resolution and limited number of scans of the macula.2
In this paper, three different OCT instruments were used depending on the instrument availability. Thus, all three instruments were not used for both cases. Nonetheless, all three instruments showed similar features of the tumor itself, i.e. a well-circumscribed round-shaped lesion contiguous with the outer retina with marked shadowing. Marked shadowing on OCT has been described with other tumors such as retinal astro-cytic hamartomas, but the distinct transition between normal overlying inner retina and exophytic RCH on OCT is a new finding that appears unique to this tumor and is similar to that noted on histopathology.5–7 It is unlike the gradual transition between tumor and retina described on OCT imaging of retinal astrocytic hamartomas, retinoblastoma and combined hamartomas of the retina and retinal pigment epithelium.5,8,9
To our knowledge, the OCT findings described in this report appear characteristic for exophytic RCH. Thus, OCT may be a useful tool to use in conjunction with fluorescein angiogram in diagnosing this tumor. Furthermore, high-resolution Fd-OCT showed morphologic changes in the adjacent retina that may affect vision. In addition to cystoid macular edema and subretinal fluid in the adjacent tumor-free macula, structural changes in the photoreceptor layer could be appreciated. Thus, Fd-OCT may be potentially useful in predicting visual potential in some eyes with this tumor. Future larger studies may shed more light on the sensitivity and specificity of OCT features in diagnosing exophytic RCH. In addition, these larger studies may reveal more information on the range of morphologic changes associated with this tumor growth that may affect vision.
Footnotes
The authors have no financial or proprietary interest in the materials presented herein.
References
- 1.Gass JDM. Steroscopic Atlas of Macular Diseases Diagnosis and Treatment. St. Louis, Mo: Mosby-Year Book, Inc; 1997. Retinal Vascular Hamartomas; pp. 850–858. [Google Scholar]
- 2.Alam S, Zawadzki RJ, Choi SS, et al. Clinical applications of rapid serial Fourier-domain optical coherence tomography for macular imaging. Ophthalmology. 2006;113:1425–1431. doi: 10.1016/j.ophtha.2006.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kreusel KM, Bechrakis NE, Neumann HPH, et al. Solitary juxtapapillary capillary retinal angioma and von Hippel-Lindau disease. Can J Ophthalmol. 2007;42:251–255. [PubMed] [Google Scholar]
- 4.McDonald HR. Diagnostic and therapeutic challenges. Retina. 2003;23:86–91. doi: 10.1097/00006982-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Shields CL, Benevides R, Materin MA, Shields JA. Optical coherence tomography of retinal astrocytic hamartoma in 15 cases. Ophthalmology. 2006;113:1553–1557. doi: 10.1016/j.ophtha.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 6.Joussen AM, Kirchhof B. Solitary peripapillary hemangioblastoma: a histopathological case report. Acta Ophthalmologica Scandinavica. 2001;79:83–87. doi: 10.1034/j.1600-0420.2001.079001083.x. [DOI] [PubMed] [Google Scholar]
- 7.Knapp CM, Woodruff G, Roberts F. Ophthalmic pathology of genotypically confirmed von Hippel Lindau disease type 1. Br J Ophthalmol. 2006;90:242–243. doi: 10.1136/bjo.2005.079152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shields CL, Mashayekhi A, Dai VV, Materin MA, Shields JA. Optical coherence tomographic findings of combined hamartoma of the retina and retinal pigment epithelium in 11 patients. Arch Ophthalmol. 2005;123:1746–1749. doi: 10.1001/archopht.123.12.1746. [DOI] [PubMed] [Google Scholar]
- 9.Shields CL, Materin MA, Shields JA. Review of optical coherence tomography for intraocular tumors. Curr Opin Ophthalmol. 2005;16:141–154. doi: 10.1097/01.icu.0000158258.01681.40. [DOI] [PubMed] [Google Scholar]