Abstract
Objective
We recently reported that a randomized controlled trial of a family-focused intervention for parentally-bereaved youth predicted higher cortisol output 6 years later relative to a control group of bereaved youth (Luecken et al., 2010). The current study evaluated longitudinal mediators of the preventive intervention effect on cortisol 6 years later.
Method
Parentally bereaved children (N=139; mean age 11.4, SD = 2.4; age range = 8-16 years; 54% male; 61% Caucasian, 17% Hispanic, 7% African American, 15% other ethnicities) were randomly assigned to the 12-week preventive intervention (n=78) or a self-study control (n=61) condition. Six years later (mean age 17.5, SD 2.4), cortisol was sampled as youth participated in a parent-child conflict interaction task. Using 4 waves of data across the 6 years, longitudinal mediators of the program impact on cortisol were evaluated.
Results
Program-induced increases in positive parenting, decreases in child exposure to negative life events, and lower externalizing symptoms significantly mediated the intervention effect on cortisol 6 years later.
Conclusions
An intervention targeting improved parenting and reduced child exposure to additional life stressors following the death of a parent may have long-term neuroendocrine effects.
Keywords: parental loss, bereavement, cortisol, intervention, mediation
The death of a parent during childhood can have a lasting impact on the mental and physical health of affected youth. Among the approximately 2.5 million youth who experience the loss of a parent each year, the majority experience additional stressors and life changes such as family relocation, decreased economic resources, increased home responsibilities, and less time with the surviving caregiver (Sandler, Ramirez, R., & Reynolds, 1986; Social Security Administration, 2000). Given the stressors bereaved caregivers face, youth may also receive less support from the surviving caregiver. The constellation of changes increases children's short-term risk of depression, anxiety disorder, conduct problems, and impaired academic and social competence, and lifespan risk of psychological disorder (Luecken, 2008).
The early death of a parent has also been linked to increased lifespan physical health problems (Luecken, 2008; Luecken & Roubinov, 2012), potentially through its influence on the development of neuroendocrine systems. Although less studied than other forms of adversity, early parental loss can negatively impact functioning of the hypothalamic-pituitary-adrenal (HPA) axis, a primary pathway of the neuroendocrine system. The HPA axis is activated as a result of emotional and physical stress signals to the hypothalamus that lead to the release of the hormone cortisol from the adrenal glands. Cortisol participates in a variety of bodily changes including an increase in cardiovascular activity, lowering of sensory and attention thresholds, an increase in alertness, and consolidation of emotional memory.
Exposure to chronic stress has been shown to cumulatively dysregulate HPA responses to subsequent stress, and affect brain and behavioral functioning in the process (Davies, Sturge-Apple, Cicchetti, & Cummings, 2007). Neuroendocrine alterations associated with childhood adversity are complex, as both exaggerated and blunted forms of dysregulation have been found. However, both exaggerated and attenuated activity indicate potential pathology and heightened risk of a host of psychological and physical health disorders (Heim, Ehlert, & Hellhammer, 2000; McEwen, 2002). Further, patterns of cortisol dysregulation linked to psychopathology in lower risk populations may be indicative of positive functioning in high risk children. Cicchetti & Rogosch (2007) found that higher morning cortisol was associated with less resilient functioning in non-maltreated children, but higher resilience among maltreated children. Studies specific to bereavement similarly suggest that early parental death can increase the risk of cortisol dysregulation. Children who lost a caregiver in the September, 11, 2001 terrorist attack exhibited persistently higher basal cortisol levels two years later relative to non-bereaved children (Pfeffer, Altemus, Heo, & Jiang, 2007). However, bereaved children with PTSD exhibited lower cortisol than bereaved children without a psychiatric disorder. Adults who experienced parental death during childhood had higher diurnal cortisol relative to non-bereaved comparison groups (Nicolson, 2004).
The evidence that childhood adversity can impact lifespan health is sufficiently strong that prominent researchers have called for focused attention to the development of interventions capable of mitigating the negative effects of adversity (e.g., Shonkoff, Boyce, & McEwen, 2009). Randomized experimental studies offer a powerful way to assess the plasticity of the neuroendocrine system following childhood adversity. Recent studies offer preliminary evidence that interventions with high risk children may prevent or reverse dysregulated patterns of cortisol output in the short- (Brotman, Gouley, Huang, Kamboukos, Fratto, & Pine, 2007; Fisher, Stoolmiller, Gunnar, & Burraston, 2007) and long-term (Luecken et al., 2010). While the results of these trials are promising, little is known about the mechanisms by which adversity leads to cortisol alterations, or the most effective methods by which interventions might prevent or change those relations. An important step for intervention research is to advance understanding of the modifiable psychosocial determinants of adversity-induced changes to the HPA axis.
The current study examines potential pathways linking participation in the Family Bereavement Program (FBP), a randomized clinical trial of a brief intervention designed to prevent mental health problems among parentally bereaved children and adolescents, to cortisol activity in late adolescence/young adulthood. Although there are many agencies that provide services for bereaved children, the FBP is the only evidence-based intervention for parentally-bereaved children with demonstrated long-term benefits for child mental health outcomes in a randomized experimental trial. The FBP is a group-based intervention that was designed to modify social environmental risk and protective factors at an early developmental period, positing effects on the development of problems and disorder at later developmental periods. The FBP targeted multiple modifiable factors theorized to be causally related to youth mental health over time. Analyses of mediation are useful for testing hypotheses about how interventions such as the FBP work: if the theorized mediating variable causes the outcome variable, then an intervention that changes the mediating variable will subsequently change the outcome variable. The FBP successfully decreased caregiver depression and child exposure to stressful life events, and increased positive parenting, child self-esteem, and some aspects of child coping skills (Hagan et al., 2012; Sandler et al., 2003; Sandler et al., 2010). As reported in Luecken et al. (2010), youth randomized to the FBP also exhibited higher total cortisol output across a parent-child conflict discussion task 6 years later relative to youth in the control condition, p = .026, Cohen's d = .39.
The current study applies longitudinal path analysis to evaluate potential mediators of the FBP effect on cortisol. Three of the factors significantly improved by the FBP, positive parenting, exposure to negative life events, and caregiver depression, are the focus of analysis because prior studies suggest that each is particularly important to the development and ongoing functioning of the neuroendocrine system, particularly for children exposed to significant adversity. In addition, theoretical models commonly cite similar factors as having significant impact on developing neuroendocrine systems (e.g., Repetti, Taylor, & Seeman, 2002; Luecken & Roubinov, 2012).
Promotion of positive parenting was a primary focus of the FBP. Positive parenting, characterized by warmth, acceptance and effective discipline, has been consistently associated with better mental health outcomes in parentally-bereaved youth (Kwok, Haine, Sandler, Ayers, & Wolchik, 2005). Positive parent-child relationships are also associated with lower neuroendocrine stress response system functioning in bereaved youth (Hagan et al., 2011; Luecken 2000; Luecken and Appelhans 2006). Grounded in cognitive-behavioral theory, FBP session activities were designed to teach skills such as expressing warmth and praise, active listening, communicating clear, consistent, and age-appropriate expectations for behavior, and planning family and one-on-one time with the child.
The death of a spouse is commonly associated with elevated depressive symptoms in the surviving spouse, and high levels of caregiver grief and/or depression negatively impact the mental health of bereaved youth (Lutzke, Ayers, Sandler, & Barr, 1997). Exposure to caregiver depression in childhood has also been associated with non-normative patterns of HPA axis functioning (Bouma, Riese, Ormel, Verhulst, & Oldehinkel, 2011; Wichers et al., 2008). Prior studies have examined relations between parent depression and offspring cortisol activity in non-bereaved families, however, and it is not known if similar relations exist in the complicated context of bereavement. The FBP directly targeted caregiver mental health through caregiver-focused activities such as positive reframing, increasing support-seeking and self-care, as well as teaching ways to manage distress without overwhelming their children.
Finally, bereaved children typically face a number of stressors in the years following the death. Negative life events have been identified as a mediator of the impact of bereavement on child mental health problems (Thompson, Kaslow, Price, Williams, & Kingree, 1998). A number of studies have found that stressful environments in childhood are associated with dysregulated HPA activity in childhood and young adulthood (e.g., Lupien et al., 2009). The effects on the HPA axis of additional stressful events may be potentiated following childhood traumas (Bevans, Cerbone, & Overstreet, 2008; Hagan, Luecken, Sandler, & Tein, 2010). The FBP included a focus on reducing exposure to negative life events by teaching caregivers skills for reducing controllable stressors and shielding children from stressors that were not preventable.
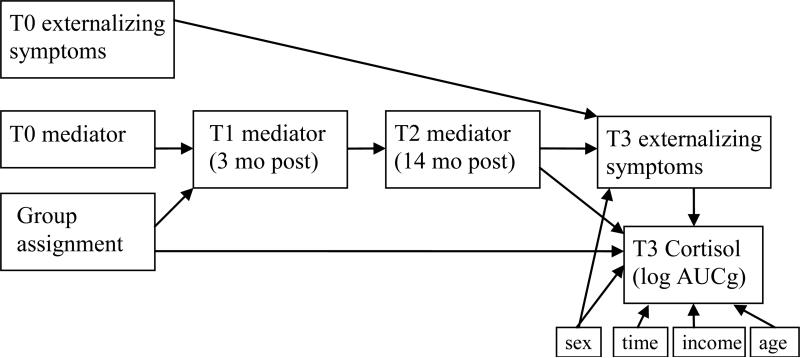
As shown in Figure 1, positive parenting, lower caregiver depression, and fewer negative life events across childhood and adolescence may cumulatively explain the intervention effect on cortisol output in late adolescence/young adulthood. However, intervention effects on these factors may also impact neuroendocrine functioning through beneficial effects on mental health. Estimates suggest that 10-21% of bereaved children develop clinical levels of internalizing and/or externalizing disorder (Gersten, Beals, & Kallgren, 1991). Prospective studies have linked positive parenting, caregiver depression, and negative life events to mental health outcomes, particularly externalizing disorders, in bereaved youth (Thompson et al., 1998). Because previous analyses found no relation of internalizing symptoms to cortisol output, we focus analyses on externalizing symptoms. A growing literature links externalizing problems to blunted HPA output and reactivity in non-bereaved (Alink et al., 2008; van Goozen, Fairchild, Snoek, & Harold, 2007) and bereaved youth (Luecken et al., 2010). The majority of studies evaluate concurrent associations between externalizing problems and cortisol activity. The direction of effects has been mixed, with evidence that HPA alterations precede externalizing symptoms (e.g., Davies et al., 2007; O'Neal et al., 2010) and that chronic externalizing symptoms precede HPA alterations (e.g., Haltigan, Roisman, Susman, Barnett-Walkier, & Monohan 2011; Ruttle, Shirtcliff, Serbin, Ben-Dat Fisher, Stack, & Schwartzman, 2011). The relation is most likely reciprocal across time, such that each influences the other (Shirtcliff, Granger, Booth, & Johnson, 2005).
Figure 1.
General mediation model
The current analyses evaluated a multiple linkage model of longitudinal mediation of the FBP effect on cortisol in late adolescence/young adulthood. We adopted a model-building approach by evaluating paths from group assignment (FBP or control) to cortisol through each putative mediator (positive parenting, caregiver depression, and negative life events) and recent externalizing symptoms across 4 waves of data collection spanning 6 years. Based on theory and previous empirical findings, it was hypothesized that participation in the FBP would predict higher positive parenting, lower caregiver depression, and less child exposure to negative life events. These benefits were expected to predict lower externalizing symptoms, which would be associated with higher cortisol in the intervention group relative to the control group.
Methods
Participants
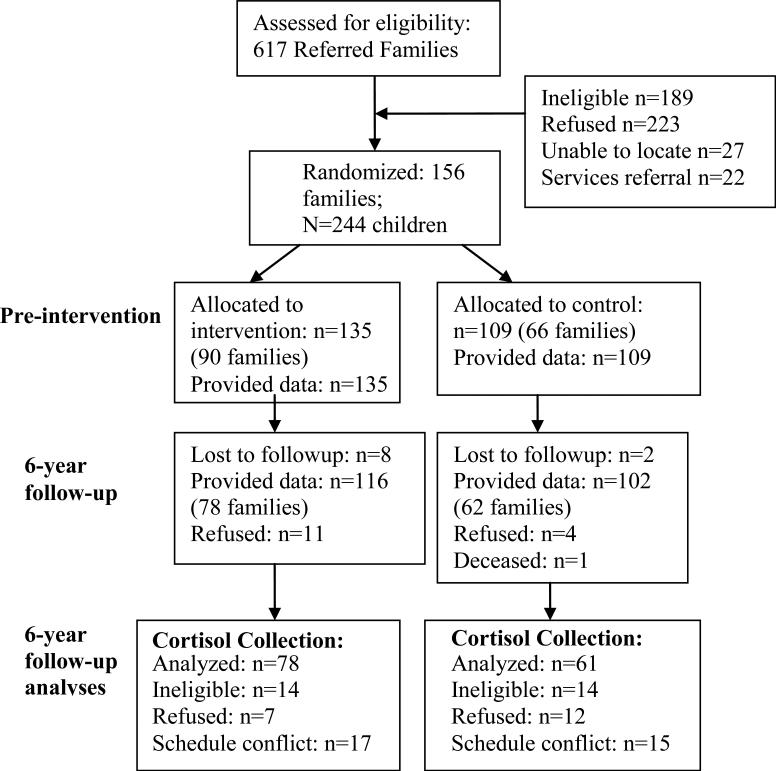
Recently bereaved families with at least one child in the age range of 8-16 years were recruited from the Phoenix, Arizona metropolitan area through community presentations and mail solicitation. The average time since parental death at the start of the intervention was 10 months (range 3 – 28 months). The cause of death was illness (75%), accident (15%) or homicide/suicide (10%). There were four assessment points: baseline (T0; prior to assignment to condition), 3 months post-baseline (T1), 14 months post-baseline (T2), and 6 years post-baseline (T3). Families were randomly assigned to either the group-based FBP intervention or a home-based self-study (control) condition. See Figure 2 for a participant flowchart.
Figure 2.
Flow of Study Participants
Salivary cortisol data was collected at the 6 year follow-up from a subsample of adolescents/young adults. To reduce the response burden for caregivers, a maximum of two offspring were randomly selected; this resulted in 19 youth from 16 families being ineligible. Youth were also ineligible if they reported less than three verbal contacts in the last month with the caregiver. Cortisol was collected from 139 youth in 106 families: 73 families sampled from 1 child only, and 33 families sampled from 2 children (mean age 17.5, SD 2.4; age range = 14-23 years; 61% Caucasian, 17% Hispanic, 7% African American, 15% other ethnicities; n=78 in the intervention group, n=61 in the control group; 81 male, 58 female).
Procedures
Intervention and control conditions
Delivered to children, adolescents and surviving caregivers in separate but concurrent groups that met for 12 weekly two-hour sessions, the FBP utilized cognitive and behavior change methods such as modeling and role-playing to teach skills. Activities in the caregiver program focused on increasing the positive quality of the caregiver-child relationship, enhancing caregivers’ use of effective discipline, decreasing caregiver mental health problems, and decreasing children's exposure to stressful events. The youth component focuses on improving the caregiver-child relationship, improving youth coping skills, and promoting adaptive beliefs about why negative events occur. In the literature control condition, three books related to grief were given to caregivers and youth across 3 months, along with outlines summarizing the main points. Complete details can be found in Ayers et al. (2010).
Conflict Discussion Task
At the six-year follow-up home visit, adolescents/young adults participated in a conflict discussion task with their caregiver approximately 20 minutes after the interviewer's arrival at the home. The task was a 12-minute videotaped behavioral observation interaction in which the adolescent/young adult and caregiver discussed current problems common to late adolescence and young adulthood (see Luecken et al., 2010 for details).
Measures
Positive Parenting
Consistent with the view that parenting is best captured by a multidimensional construct, positive parenting was assessed at T0, T1, and T2 using a composite of the standardized scores of multiple indicators including: the Acceptance subscale of the Child Report of Parental Behavior Inventory (CRPBI; Schaefer, 1965; α= .92); Rejection subscale of the CRPBI (Schaefer, 1965; α = .87); the caregiver–child Dyadic Routines Scale (Wolchik et al., 2000; α=.74); Stable Positive Events Scale (Sandler, Wolchik, Braver, & Fogas, 1991); and a Sharing of Feelings Scale (Ayers, Sandler, Twohey, & Haine, 1998; α=.85). Caregiver reports consisted of parallel versions of the four scales described above: Acceptance (α= .91), Rejection (α = .87), Dyadic Routines (α = .76), and Stable Positive Events. In addition, we assessed how caregivers communicate with their children about stressful events with the Talk with Reassurance subscale of the Caregiver Expression of Emotion Questionnaire (Jones & Twohey, 1998; α = .74). Caregiver and child reports of discipline were assessed using parallel forms of two scales: the Inconsistency of Discipline subscale of CRPBI (α = .86, caregiver; α = .80, child) and an adaptation of the Parent Perception Inventory (Hazzard, Christensen, & Margolin, 1983) to assess use of positive reinforcement (α= .92, caregiver; α = .91, child). Caregivers also completed an adaptation of the Discipline Follow-Through subscale of the Oregon Discipline Scale (Oregon Social Learning Center, 1991; α= .82). Twelve-minute videotaped dyadic discussions between caregiver and child were coded to reflect positive parenting (positive affective tone, back channeling, and head nods). Details of the validity of this measure of positive parenting can be found in Kwok et al. (2005).
Caregiver depression
Caregiver depression was assessed at T0, T1, and T2 with the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996).
Negative life events
Experiences of negative events assessed at T0, T1, and T2 were used in the current analyses and were assessed by youth report using the 51-item Negative Life Events Scale (NLES), derived from the General Life Events Schedule for Children (Sandler, Ramirez, & Reynolds, 1986) and the Parent Death Events List (Sandler & Guenther, 1985). Scores were calculated by summing the number of events in the month prior to the assessment. Evidence of validity for the NLES is provided in Tein, Sandler, Ayers, & Wolchik (2006).
Youth externalizing problems
Baseline (T0) youth externalizing symptoms in the past 30 days were assessed with the Child Behavior Checklist (CBCL; Achenbach, 1991; α = .87). At T3, reports of externalizing symptoms in the past 30 days were assessed with the YSR (externalizing α = .88) for participants 14-18 years old, or the Young Adult Self Report (YASR; externalizing α = .87) for participants over 18 (Achenbach, 1991; 1997). Because adolescents and young adults completed different scales, item response theory was used to conduct an equating transformation that put the scores on a common metric for the two scales.
Cortisol sampling
Salivary cortisol samples were collected at T3 from adolescents/young adults before, immediately after, and at 15 and 30-minutes after the conflict discussion task. Because the intervention effect was only significant for total output across the task, area under the curve with respect to ground (AUCg), log-transformed to correct for deviations from normality, served as the primary dependent variable. Outlier analyses identified one participant with log-transformed AUCg > 3 SD from the mean. Because examination of the data did not reveal a clear explanation for the elevated cortisol levels that would suggest removal from the dataset, winsorizing was used and the participant's AUCg was set to the next highest AUCg.
Data analysis
There are several tests for mediation, but common to each is a test of the effect of the intervention on the mediator, and a test of the relation of the mediator to the outcome adjusting for the effect of the intervention (MacKinnon et al., 2002). The current analyses used Mplus 6.0 (Muthen & Muthen, 2010), which is capable of adjusting for data dependence associated with multiple children from one family. Although intraclass correlations (ICC) for cortisol were relatively low (.17), ICC for positive parenting were high (.55-.72). Mplus uses full information maximum likelihood to manage missing data. T0 measures of positive parenting, caregiver depression, negative life events, and externalizing symptoms were control variables. Covariates included sex, age, income, and time of day. Age, time of day, and income were modeled with paths to AUCg only. Age was allowed to covary with T3 externalizing symptoms. Sex was modeled with paths to T3 externalizing symptoms and AUCg. Initially, each proposed mediators was evaluated separately, and then a final multiple-mediator model was evaluated.
Model fit was examined using Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR), using criteria by Hu & Bentler (1999) to interpret fit indices. Although the evaluation of single-mediator models has been extensively researched, the methods do not easily extend to long-chain mediation models such as the 4-path model proposed here (Taylor, MacKinnon, & Tein, 2007). Therefore, we evaluated mediation using a causal-steps approach, termed the joint significance test (MacKinnon et al., 2002), which finds evidence for mediation if each of the individual paths in the model is statistically significant. The joint significance test is advantageous because it has good power and controls for Type 1 error; however, it does not provide the means to construct confidence intervals for the estimate of the mediated effect.1
Results
Preliminary Group Comparisons
Table 1 presents zero-order correlations. Skewness and kurtosis of all variables fell within acceptable ranges. Participants were randomly assigned to study condition, and previous reports of the FBP found no evidence for a failure of randomization or of baseline group differences that could explain cortisol at T3. Chi-square and t-tests found no group differences in gender, ethnicity, age, gender of deceased parent, cause of death, elapsed time since the death, baseline family income, hormonal contraceptive use, psychiatric medications, smoking status, or alcohol problems (all p's> .19). On the day of testing, the groups did not differ in the time of day of testing, cigarettes smoked, exercise, caffeine, or time of last meal (all p's > .68).
Table 1.
Zero-order correlations of study variables
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T0 Pos par | .75** | .62** | -.32** | -.36** | -.12 | -.23** | -.16† | -.19* | -.27** | -.21* | .01 |
| 2. T1 Pos par | 1.0 | .67** | -.23** | -.34** | -.18* | -.23** | -.25** | -.21* | -.20* | -22** | .01 |
| 3. T2 Pos par | 1.0 | -.21* | -.25** | -.13 | -.20* | -.28** | -.22* | -.23** | -.25** | -.09 | |
| 4. T0 C-dep | 1.0 | .66** | .52** | .20* | 0.00 | .21* | .12 | .11 | -.04 | ||
| 5. T1 C-dep | 1.0 | .35** | .23** | .12 | .21* | .15† | .14† | -.13 | |||
| 6. T2 C-dep | 1.0 | .17† | .16 | .17† | .13 | .03 | -.08 | ||||
| 7. T0 NLE | 1.0 | .50** | .51** | .29** | .13 | .04 | |||||
| 8. T1 NLE | 1.0 | .50** | .34** | .15† | -.14 | ||||||
| 9. T2 NLE | 1.0 | .19* | .27** | -.09 | |||||||
| 10. T0 Ext | 1.0 | .29** | 0.0 | ||||||||
| 11. T3 Ext | 1.0 | -.34** | |||||||||
| 12. T3 AUCg | 1.0 |
p < .10
p < .05
p < .01
“Pos par” = Positive parenting; C-dep = caregiver depression; NLE = child exposure to negative life events; “Ext” = externalizing symptoms; “AUCg” = non-transformed Cortisol AUCg
Attrition rates did not differ across intervention and control conditions (p = .12). Attrition status did not predict baseline risk, participant age, ethnicity, gender, months since parental death or family income (all p's >.14). The group by attrition interaction was not associated with baseline risk, age, ethnicity, gender, months since parental death, or income (all p's > .36).
Primary Analyses
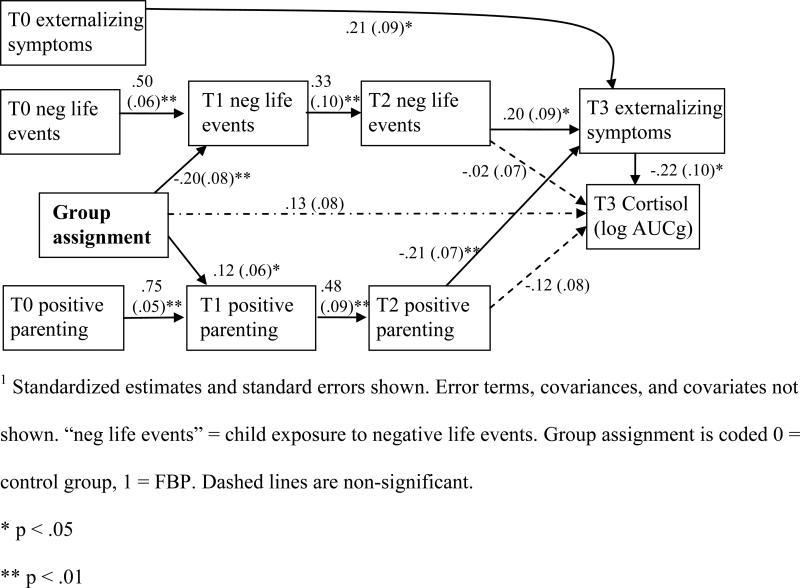
Positive Parenting
We first evaluated paths linking positive parenting to T3 externalizing symptoms and cortisol. T0 externalizing symptoms was allowed to covary with T0 positive parenting. The model represented a good fit to the data, χ2 (19) = 14.5, p = .75, CFI = 1.0, RMSEA=0.0, {0.0; 0.054}, SRMR = .029, but the path from T2 positive parenting to cortisol was not significant (p = .14). Consistent with the joint significance test for mediation, all other linkages in the hypothesized causal pathway were significant at p < .05, and the path from group to cortisol was not significant (p = .11). Participation in the FBP significantly predicted higher T1 positive parenting, which predicted higher T2 positive parenting, which predicted lower T3 externalizing symptoms, which predicted higher cortisol.
Caregiver depression
Evaluation of mediation by caregiver depression was evaluated found an adequate model fit: χ2 (16) = 19.9, p = .22, CFI = .97, RMSEA=0.042, {0.0; 0.094}, SRMR = .045. However, the path from T2 caregiver depression to cortisol was not significant (p = .14), and the path from T2 caregiver depression to T3 externalizing symptoms was not significant (p = .92). Therefore caregiver depression was not considered further as a mediator.
Negative Life Events
Next, we evaluated child exposure to negative life events as a mediator of the intervention effect on cortisol. For this model, T0 externalizing symptoms was allowed to covary with T0 negative life events. The model was a good fit: χ2 (19) = 19.4, p = .43, CFI = .997, RMSEA=0.013, {0.00; 0.076}, SRMR = .038, but the path from T2 negative life events to AUCg was not significant (p = .95). Consistent with mediation, all other linkages in the hypothesized causal pathway were significant at p < .05 and the path from group to cortisol was not significant (p = .13). Participation in the FBP predicted lower T1 exposure to negative life events, which predicted lower T2 negative life events, which predicted lower T3 externalizing symptoms, which predicted higher cortisol.
Final model
A final multiple mediator model evaluating paths linking positive parenting and negative life events to externalizing symptoms and cortisol (see Figure 3) represented a good fit: χ2 (40) = 33.8, p = .74, CFI = 1.0, RMSEA =0.00, {0.00; 0.044}, SRMR = .045. The paths from T2 negative life events (p = .82) and T2 positive parenting (p = .14) to AUCg were not significant. Consistent with mediation, all other linkages in the hypothesized causal pathway were significant at p < .05, and the group effect on cortisol was not significant, p = .12.
Figure 3.
Final model1
Discussion
Informed by a comprehensive, integrative model of processes of adaptation following parental death, the Family Bereavement Program (FBP) targeted key factors involved in youth adaptation following parental death. The theoretically- and empirically-driven design of the intervention, use of a randomized controlled trial, and inclusion of multiple follow-ups spanning six years provide a powerful test of plausible pathways linking parental death to youth adaptation. The current study extends prior findings by evaluating pathways by which the program affected cortisol output six years later. Three contextual-level factors targeted by the program were hypothesized to mediate the FBP effect on youth cortisol output: positive parenting, caregiver depression, and exposure to negative life events. Support was found for two of the three putative mediators in the multiple linkage model. Relative to the control condition, participation in the FBP predicted increased positive parenting and lower child exposure to negative life events immediately after the intervention and at the 3-month follow-up. These benefits predicted lower externalizing symptoms at the 6-year follow-up, which were associated with higher cortisol. Reduced caregiver depression did not predict recent externalizing symptoms or cortisol output, and thus did not appear to mediate the program effect on cortisol.
Our results suggest that impaired parenting and negative life events may impact cortisol via relations with mental health. Although others have linked parenting and negative events directly to cortisol, these factors are often measured concurrently with cortisol, either representing recent stress exposure or retrospective accounts of parenting and stress. There is a great deal of evidence implicating negative parenting behaviors and stressful conditions in the development and/or maintenance of behavior problems among youth. From the perspective of social learning theory, harsh parenting practices model maladaptive ways of approaching interpersonal interactions, leading to acting out behaviors (Schwartz, Dodge, Pettit, & Bates, 1997). Relatedly, cumulative exposure to negative events has been theorized to overwhelm the adaptive capacities of individuals, leading to problematic behavior patterns (Aseltine, Gore, & Gordon, 2000). Growing evidence links externalizing symptoms to neuroendocrine activity, however, as reviewed earlier, cortisol alterations may precede or follow externalizing symptoms. We cannot determine with our data if cortisol alterations preceded externalizing symptoms, but the relations are likely reciprocal across time, such that externalizing symptoms influence HPA activity, and HPA activity influences externalizing symptoms.
A few research programs have evaluated the potential for randomized experimental interventions to shed light on the nature of the effects of early adversity on neurobiological systems, finding program effects on different aspects of cortisol stress regulation, including effects on anticipatory cortisol prior to a social stressor (Brotman et al., 2007), diurnal cortisol patterns (Fisher et al., 2007), total cortisol across a parent-child conflict discussion (Luecken et al., 2010), and cortisol reactivity (O'Neal et al). In combination, these studies are intriguing but leave open the question of which aspect of cortisol regulation is most responsive to intervention. Further, the complex neuroendocrine consequences of adversity complicate efforts to predict or interpret intervention effects. In the current study, higher cortisol was associated with lower externalizing symptoms, suggesting that higher cortisol is representative of better adaptation.
The goal of studies like ours is to obtain information on the causal relations among theoretically-supported variables for purposes of demonstrating long-term processes of adaptation. For prevention purposes, if a causal predictor of an outcome variable is identified, then interventions can be designed to change that causal predictor. Our results suggest that negative life events and positive parenting behaviors have substantial relations to child problem behaviors, which are associated with cortisol activity. Before drawing causal inferences, it is useful to consider possible confounders. For example, an unmeasured general parenting variable may be related to positive parenting behavior, and may represent the true causal relation. There may also be some general personality factor that predicts exposure to negative life events, positive parenting behaviors, and child behaviors in a way that could explain the results. However, the randomization of participants to conditions and the consistent relations among variables across four waves of data collection reduces the likelihood of alternative explanations or alternative missing confounder explanations of the results of the study.
There are limitations to the analyses. First, although the lack of a cortisol assessment prior to assignment to condition prevents evaluation of developmental changes in cortisol regulation across time, the randomized controlled design of the FBP is considered a “gold standard for establishing causation because randomization creates probabilistically equivalent treatment and control groups” (Mercer, DeVinney, Fine, Green, & Dougherty, 2007, p. 143). We found no evidence of pre-intervention group differences that might explain intervention effects on cortisol. Further evidence to support a possible causal process is provided by our finding that longitudinal mediators significantly explain the group effect (e.g., Morgan & Winship, 2007). Second, externalizing symptoms were measured at the same time-point as cortisol. Because the measure reported symptoms in the 30 days prior to cortisol sampling, there is some evidence for temporal precedence, and it would not be appropriate to model cortisol as a predictor of externalizing symptoms. Nonetheless, other pathways (e.g., emotion regulation, social competence) may contribute to a better specified model. The sample size (n=139) was relatively small and does not allow evaluation of moderators or potentially high risk subgroups. SEM models with small sample sizes can perform well with reliable measures (Iacobucci, 2010); therefore we used reliable, validated measures, and limited the models to variables with strong empirical and theoretical support. We used the joint significance test in our analyses of a 4-path mediated effect because simulation studies for the 3-path mediated effect showed that it had the best balance of power and type 1 error rates (Taylor et al., 2008). However, as methods for longitudinal mediation are further investigated, Bayesian or Monte Carlo methods may prove to be better tools for conducting significance tests of more complex indirect effects.
While advancing the investigation of the role of neuroendocrine functioning in psychopathology, prior research on interventions for at-risk children has not systematically examined the mechanisms by which the program influenced cortisol activity. The combination of a randomized experimental design and theoretically- and empirically-driven mediation analyses offers a promising way to 1) test theory of how early adversity affects biology, 2) identify how a prevention/intervention program achieves effects on neurobiological functioning, and 3) design cost-effective, targeted interventions. Given clear evidence that childhood adversity is an established risk factor for mental and physical health disorders, a better understanding of underlying mechanisms is critical for the development of effective interventions with at-risk families. Our results, notable for the use of a randomized controlled trial and examination of multiple linkage models, can be used to guide intervention re-design and advance theoretical understanding of processes that affect long-term adaptation of bereaved children. Our findings suggest that a focus on improving the child's relationship with the surviving caregiver and decreasing child exposure to negative life events may improve child mental health and, in combination, represent important pathways to minimize neuroendocrine alterations associated with childhood adversity.
ACKNOWLEDGMENTS
Support for this research was provided by NIMH R01 Grant MH49155 and P30 MH0686856
Footnotes
Resampling methods such as the bias-corrected bootstrap are often recommended for multiple path analyses particularly for smaller sample sizes, however they may lead to inflated Type I error (Taylor et al., 2007) and are not available for clustered data (e.g., children in families). Thus, these methods were not employed in the current analyses.
References
- Achenbach TM. Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. University of Vermont, Department of Psychiatry; Burlington, VT: 1997. [Google Scholar]
- Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. University of Vermont, Department of Psychology; Burlington, VT: 1991. [Google Scholar]
- Alink LR, van IJzendoorn MH, Bakermans-Kranenburg MJ, Mesman J, Juffer F, Koot HM. Cortisol and externalizing behavior in children and adolescents: mixed meta-analytic evidence for the inverse relation of basal cortisol and cortisol reactivity with externalizing behavior. Developmental Psychobiology. 2008;50:427–450. doi: 10.1002/dev.20300. doi: 10.1002/dev.20300. [DOI] [PubMed] [Google Scholar]
- Aseltine RH, Gore S, Gordon J. Life stress, anger and anxiety, and delinquency: An empirical test of general strain theory. Journal of Health and Social Behavior. 2000;41:256–275. [PubMed] [Google Scholar]
- Ayers TS, Wolchik SA, Sandler IN, Towhey JL, Lutzke Weyer JR, Jones S, Kriege G. The Family Bereavement Program: Description of a theory-based prevention program for parentally-bereaved children and adolescent. Omega: Journal of Death and Dying. 2010;78:131–143. doi: 10.2190/om.68.4.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers TS, Sandler IN, Twohey JL, Haine R. Three views of emotional expression in parentally bereaved children: Stress and coping in children and adolescents.. Poster presented at the 106th Annual Convention of the American Psychological Association; San Francisco. 1998, August. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bevans K, Cerbone A, Overstreet S. Relations between recurrent trauma exposure and recent life stress and salivary cortisol among children. Development and Psychopathology. 2008;20:257–272. doi: 10.1017/S0954579408000126. doi: 10.1017/S0954579408000126. [DOI] [PubMed] [Google Scholar]
- Bouma EMC, Riese H, Ormel J, Verhulst FC, Oldehinkel AJ. Self-assessed parental depressive problems are associated with blunted cortisol responses to a social stress test in daughters. The TRAILS study. Psychoneuroendocrinology. 2011;36:854–863. doi: 10.1016/j.psyneuen.2010.11.008. doi: 10.1016/j.psyneuen.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Gouley KK, Huang KY, Kamboukos D, Fratto C, Pine DS. Effects of a psychosocial family-based preventive intervention on cortisol response to a social challenge in preschoolers at high risk for antisocial behavior. Archives of General Psychiatry. 2007;64:1172–1179. doi: 10.1001/archpsyc.64.10.1172. doi:10.1001/archpsyc.64.10.1172. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Personality, adrenal steroid hormones, and resilience in maltreated children: A multilevel perspective. Developmental Psychopatholology. 2007;19:787–809. doi: 10.1017/S0954579407000399. doi: 10.1017/S0954579407000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cicchetti D, Cummings EM. The role of child adrenocortical functioning in pathways between interparental conflict and child maladjustment. Developmental Psychology. 2007;43:918–930. doi: 10.1037/0012-1649.43.4.918. doi: 10.1037/0012-1649.43.4.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology. 2007;32:892–905. doi: 10.1016/j.psyneuen.2007.06.008. doi: 10.1016/j.psyneuen.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersten J, Beals J, Kallgren C. Epidemiology and preventive interventions: Parental death in childhood as a case example. American Journal of Community Psychology. 1991;19:481–499. doi: 10.1007/BF00937988. doi: 10.1007/BF00937988. [DOI] [PubMed] [Google Scholar]
- Hagan M, Tein JY, Sandler IN, Wolchik S, Ayers T, Luecken LJ. Strengthening effective parenting practices over the long-term: Effects of a preventive intervention for parentally bereaved families. Journal of Clinical Child and Adolescent Psychology. 2012;41:177–188. doi: 10.1080/15374416.2012.651996. doi: 10.1080/15374416.2012.651996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan M, Luecken LJ, Sandler IN, Tien JY. Prospective effects of post-bereavement negative events on cortisol activity in parentally bereaved youth. Developmental Psychobiology. 2010;52:394–400. doi: 10.1002/dev.20433. doi: 10.1002/dev.20433. [DOI] [PubMed] [Google Scholar]
- Hagan M, Roubinov D, Gress J, Luecken LJ, Sandler I, Wolchik S. Positive parenting during childhood moderates the impact of recent negative events on on cortisol activity in parentally bereaved youth. Psychopharmacology. 2011;214:231–238. doi: 10.1007/s00213-010-1889-5. doi: 10.1007/s00213-010-1889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haltigan JD, Roisman GI, Susman EJ, Barnett-Walkier K, Monohan KC. Elevated trajectories of externalizing problems are associated with lower awakening cortisol levels in midadolescence. Developmental Psychology. 2011;47:472–478. doi: 10.1037/a0021911. doi: 10.1037/a0021911. [DOI] [PubMed] [Google Scholar]
- Hazzard A, Christensen A, Margolin G. Children's perception of parental behaviors. Journal of Abnormal Clinical Psychology. 1983;11:49–60. doi: 10.1007/BF00912177. doi: 10.1007/BF00912177. [DOI] [PubMed] [Google Scholar]
- Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25:1–35. doi: 10.1016/s0306-4530(99)00035-9. doi: 10.1016/S0306-4530(99)00035-9. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [Google Scholar]
- Iacobucci D. Structural equations modeling: Fit Indices, sample size, and advanced topics. Journal of Consumer Psychology. 2010;20:90–98. doi: 10.1016/j.jcps.2009.09.003. [Google Scholar]
- Jones S, Twohey JL. Parents’ expression of emotions questionnaire: Psychometric properties.. Paper presented at the 106th Annual Convention of the American Psychological Association; San Francisco. 1998, August. [Google Scholar]
- Kwok OM, Haine R, Sandler IN, Ayers TS, Wolchik SA. Positive parenting as a mediator of the relations between parental psychological distress and mental health problems of parentally-bereaved children. Journal of Clinical Child and Adolescent Psychology. 2005;34:261–272. doi: 10.1207/s15374424jccp3402_5. doi: 10.1207/s15374424jccp3402_5. [DOI] [PubMed] [Google Scholar]
- Luecken LJ. Parental caring and loss during childhood and adult cortisol responses to stress. Psychology and Health. 2000;15:841–851. doi: 10.1080/08870440008405586. [Google Scholar]
- Luecken LJ. Long-term consequences of parental death in childhood: Physiological and psychological manifestations. In: Stroebe M, Hansson RO, Schut H, Stroebe W, editors. Handbook of Bereavement Research and Practice: 21st Century Perspectives. American Psychological Association Press; 2008. [Google Scholar]
- Luecken LJ, Appelhans BM. Early parental loss and cortisol stress responses in young adulthood: The moderating role of family environment. Development and Psychopathology. 2006;18:295–308. doi: 10.1017/S0954579406060160. doi: 10.1017/S0954579406060160. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Hagan MJ, Sandler IN, Tien J, Ayers TS, Wolchik SA. Cortisol levels six-years after participation in the Family Bereavement Program. Psychoneuroendocrinology. 2010;35:785–789. doi: 10.1016/j.psyneuen.2009.11.002. doi: 10.1016/j.psyneuen.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ, Roubinov DS. Pathways to lifespan health following childhood parental death. Social and Personality Psychology Compass. 2012;6:243–257. doi: 10.1111/j.1751-9004.2011.00422.x. doi: 10.1111/j.1751-9004.2011.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on brain, behavior, and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. doi:10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Lutzke JR, Ayers TS, Sandler IN, Barr A. Risks and interventions for the parentally bereaved child. In: Wolchik S, Sandler I, editors. Handbook of children's coping: Linking theory and intervention. Plenum Press; New York: 1997. pp. 215–244. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Sex, stress, and the hippocampus: allostasis, allostatic load, and the aging process. Neurobiology of Aging. 2002;23:921–939. doi: 10.1016/s0197-4580(02)00027-1. [DOI] [PubMed] [Google Scholar]
- Mercer SL, DeVinney BJ, Fine LJ, Green LG, Dougherty D. Study designs for effectiveness and translation research: Identifying trade-offs. American Journal of Preventive Medicine. 2007;33(2):139–154. doi: 10.1016/j.amepre.2007.04.005. doi: 10.1016/j.amepre.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Morgan SL, Winship C. Counterfactuals and Causal Inference. Cambridge University Press; New York, New York: 2007. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 5th Ed. Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- Nicolson NA. Childhood parental loss and cortisol levels in adult men. Psychoneuroendocrinology. 2004;29:1012–1018. doi: 10.1016/j.psyneuen.2003.09.005. doi: 10/1016/j.psyneuen.2003.09.005. [DOI] [PubMed] [Google Scholar]
- O'Neal CR, Brotman LM, Huang K, Gouley KK, Kamboukos D, Calzada EJ, Pine DS. Understanding relations among early family environment, cortisol response, and child aggression via a prevention experiment. Child Development. 2010;81:290–305. doi: 10.1111/j.1467-8624.2009.01395.x. doi: 10.1111/j.1467-8624.2009.01395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oregon Social Learning Center . LIFT Parent Interview. 1991. Unpublished manuscript. [Google Scholar]
- Pfeffer CR, Altemus M, Heo M, Jiang H. Salivary cortisol and psychopathology in children bereaved by the September 11, 2001 terror attacks. Biological Psychiatry. 2007;61:957–965. doi: 10.1016/j.biopsych.2006.07.037. doi: 10.1016/j.biopsych.2006.07.037. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. doi: 10.1037/0033-2909.128.2.330. [PubMed] [Google Scholar]
- Ruttle PL, Shirtcliff EA, Serbin LA, Ben-Dat Fisher D, Stack DM, Schwartzman AE. Disentangling psychogiological mechanisms underlying internalizing and externalizing behaviors in youth: longitudinal and concurrent associations. Hormones and Behavior. 2011;59:123–132. doi: 10.1016/j.yhbeh.2010.10.015. doi: 10.1016/j.yhbeh.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler I, Ayers TS, Tein JY, Wolchik A, Millsap R, Khoo ST, Coxe S. Six-year follow-up of a preventive intervention for parentally-bereaved youth: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2010;164:907–914. doi: 10.1001/archpediatrics.2010.173. doi:10.1001/archpediatrics.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein JY, Kwok OM, Haine RA, Kriege GM. The Family Bereavement Program: Efficacy evaluation of a theory-based prevention program for parentally bereaved children and adolescents. Journal of Consulting and Clinical Psychology. 2003;71:587–600. doi: 10.1037/0022-006x.71.3.587. doi: 10.1037/0022-006X.71.3.587. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Guenther RT. Assessment of life stress events. In: Karoly P, editor. Measurement strategies in health psychology. Wiley; New York: 1985. pp. 555–600. [Google Scholar]
- Sandler IN, Ramirez R, Reynolds KD. Life stress for children of divorce, bereaved children and asthmatic children.. Paper presented at the 94th Annual Convention of the American Psychological Association; Washington, D.C.. 1986. [Google Scholar]
- Sandler I, Wolchik S, Braver S, Fogas B. Stability and quality of life events and psychological symptomatology in children of divorce. American Journal of Community Psychology. 1991;19:501–520. doi: 10.1007/BF00937989. doi: 10.1007/BF00937989. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. Children's Report of Parental Behavior: An inventory. Child Development. 1965;36(2):413–424. [PubMed] [Google Scholar]
- Schwartz D, Dodge KA, Pettit GS, Bates JE. The early socialization of aggressive victims of bullying. Child Development. 1997;68:665–675. doi: 10.1111/j.1467-8624.1997.tb04228.x. [PubMed] [Google Scholar]
- Shirtcliff EA, Granger DA, Booth A, Johnson D. Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology. 2005;17:167–184. doi: 10.1017/s0954579405050091. doi: 10.10170S0954579405050091. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. doi:10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Social Security Administration . Intermediate assumptions of the 2000 Trustees Report. Office of the Chief Actuary of the Social Security Administration; Washington, DC: 2000. [Google Scholar]
- Taylor AB, MacKinnon DP, Tein JY. Tests of the three-path mediated effect. Organizational Research Methods. 2008;11:241–269. doi:10.1177/1094428107300344. [Google Scholar]
- Tein J, Sandler IN, Ayers TS, Wolchik SA. Mediation of the effects of the Family Bereavement Program on mental health problems of bereaved children and adolescents. Prevention Science. 2006;7:179–195. doi: 10.1007/s11121-006-0037-2. doi: 10.1007/s11121-006-0037-2. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kaslow NJ, Price AW, Williams K, Kingree JB. Role of secondary stressors in the parental death-child distress relation. Journal of Abnormal Child Psychology. 1998;26:357–366. doi: 10.1023/a:1021951806281. doi: 10.1023/A:1021951806281. [DOI] [PubMed] [Google Scholar]
- van Goozen SHM, Fairchild G, Snoek H, Harold GT. The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin. 2007;133:149–182. doi: 10.1037/0033-2909.133.1.149. doi: 10.1037/0033-2909.133.1.149. [DOI] [PubMed] [Google Scholar]
- Wichers MC, Myin-Germeys I, Jacobs N, Kenis G, Derom C, Vlietinck R, Van Os J. Susceptibility to depression expressed as alterations in cortisol day curve: a cross-twin, cross-trait study. Psychosomatic Medicine. 2008;70:314–318. doi: 10.1097/PSY.0b013e31816b1eee. doi: 10.1097/ PSY.0b013e31816b1eee. [DOI] [PubMed] [Google Scholar]
- Wolchik SA, West SG, Sandler IN, Tein JY, Coatsworth D, Lengua L, Griffin WA. An experimental evaluation of theory-based mother and mother-child programs for children of divorce. Journal of Consulting and Clinical Psychology. 2000;68:843–856. doi: 10.1037/0022-006X.68.5.843. [PubMed] [Google Scholar]