Abstract
Background
Although no ideal sedative exists, dexmedetomidine is unique because it produces sedation and analgesia without decreasing the respiratory drive. Hemodynamic responses to dexmedetomidine are variable and dependent on the patient population. Our initial experience was associated with an unacceptable incidence of hypotension and bradycardia. We evaluated occurrence of hypotension and bradycardia in critically ill surgical patients receiving dexmedetomidine before and after implementation of a dosing protocol.
Methods
This is a retrospective chart review of all admissions to a university medical center–based, 44-bed surgical intensive care unit pre and post protocol implementation.
Results
Forty-four patients received dexmedetomidine including 19 historic controls and 25 dosed via protocol. Both groups had comparable demographics and initial and maximum dosages of dexmedetomidine. Use of the dosing protocol resulted in fewer dosage changes (mean ± standard deviation, 4.8 ± 3.8 compared to 7.8 ± 3.9; P = .014) and fewer episodes of hypotension (16% vs 68.4%; P = .0006) but did not influence bradycardic episodes (20% vs 15.5%; P > .99).
Conclusion
We found that use of a protocol that increases the time interval between dosage adjustments may reduce dexmedetomidine-associated hypotension.
Keywords: Dexmedetomidine, Intensive care unit, Hypotension
1. Introduction
After publication of Too Err is Human: Building a Safer Health System in 1999 by the Institute of Medicine, medication safety has become a top priority in health care [1]. That report focused on the observation that many medical errors involve medications and concluded that health care providers need to design safer systems [2,3]. Because of complexities of critical illness, patients in the intensive care unit (ICU) are considered to be at increased risk of medication errors and adverse drug events, particularly with intravenous medications [2–5]. Proposed strategies to improve medication safety in the ICU include intensivist-lead, multidisciplinary rounds with pharmacist participation; standardized drug preparation and administration; computerized prescriber order entry; bar coding technology; computerized intravenous infusion devices; education; and developing a culture of safety [2,6]. Because most medication errors and many adverse drug events are considered preventable, development of surveillance systems targeting strategies for improvement should help decrease adverse drug events in both the outpatient and the inpatient setting, including the ICU [6].
An essential part of ICU care is to protect patients from themselves during agitation, and this often requires use of sedatives such as propofol or benzodiazepines [7]. In addition, opioids are used to treat pain, a common contributor to agitation in surgical patients. Unfortunately, use of these medications is associated with adverse drug events such as respiratory depression, resulting in increased duration of mechanical ventilation, and development of ventilator-associated pneumonia, all of which increase ICU length of stay [8].
Dexmedetomidine is a sedative with a unique mechanism of action that became available in the United States in 1999 for sedation of critically ill patients [9]. Desirable properties of dexmedetomidine include induction of sedation and analgesia via stimulation of α2-receptors without concomitant respiratory depression by γ-aminobutric acid-mimetic properties that accompany use of many other sedatives [9]. Additional advantages of dexmedetomidine include a relatively short half-life and hepatic metabolism [9]. Described adverse drug reactions with dexmedetomidine include altered blood pressure, nausea, and bradycardia [10,11]. Hypotension, which is the most commonly reported adverse effect, results from a sympatholytic effect mediated by activation of central α2a-receptors causing vasodilation [9,12]. Thus, dexmedetomidine has the desirable characteristic of inducing sedation without causing respiratory depression, but it also has potential side effects that might preclude its use during critical illness.
Despite an initial enthusiasm for dexmedetomidine to treat agitation in our surgical ICU, data from our drug surveillance monitoring system suggested an unacceptable incidence of hypotension and bradycardia associated with its use. Closer evaluation revealed that hypotension often occurred when dexmedetomidine dosage was titrated rapidly (more frequently than every 20 minutes) compared with slower rates of titration [13]. Based upon these data, a dosing protocol for dexmedetomidine was developed that allows titration no more frequently than every 30 minutes. In this report, we described reduced occurrence of hypotension associated with dexmedetomidine in our surgical ICU after institution of this dosing protocol.
2. Materials and methods
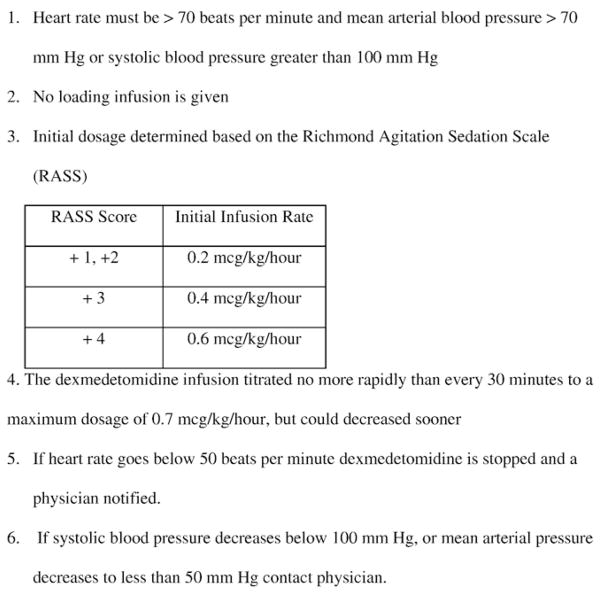
Dexmedetomidine was added to the Formulary of Accepted Medications at The Ohio State University Medical Center in 2001 and was restricted to use in the surgical ICU. We previously reported a medication use evaluation performance improvement project of patients receiving dexmedetomidine in the surgical ICU between October 2001 and December 2004 [13]. These data suggested that hypotension occurred more frequently when dexmedetomidine is rapidly titrated. Based on these data, a dosing protocol was developed (Fig. 1). This protocol was reviewed and approved by the surgical ICU quality committee with representation from surgery, nursing, and pharmacy.
Fig. 1.
Dexmedetomidine dosing protocol.
Between April 2005 and March 2006, patients received dexmedetomidine via this new protocol and were compared with historic controls that received dexmedetomidine rapidly titrated (<20 minutes between dosage adjustments) between October 2001 and December 2004. Patients were excluded if they were less than 18 or more than 89 years old, pregnant, incarcerated, or receiving vasopressors before initiation of dexmedetomidine. Data collected included demographics, Acute Physiology and Chronic Health Evaluation II (APACHE II) score on admission, sedation score, indication, dosage titration, length of therapy, time between dosing adjustments, and adverse drug reactions attributed to dexmedetomidine from start of infusion to end of infusion. Data were retrospectively collected from our electronic ICU charting system (CliniComp International, San Diego, Calif). Vitals signs can be automatically imported at the touch of a computer key with this system. The primary outcome was the occurrence of hypotension, defined as a mean arterial blood pressure less than 60 mm Hg attributed to dexmedetomidine, as determined by one of the investigators (AG). Development of bradycardia was also studied and defined as heart rate less than 50 beats per minute attributed to dexmedetomidine. Hemodynamic parameters were monitored for 2 hours before initiation of dexmedetomidine to 12 hours after discontinuation. Sedation scores (Ramsay Sedation Score was collected in the control group and Richmond Agitation Sedation Score [RASS] for the protocol group) were collected between 30 and 120 minutes of initiation and within 2 hours before or after the development of an adverse drug reaction [7,14]. To allow comparison between these different scales, patients are reported to be agitated, calm, or sedated. Our retrospective chart review received institutional review board exemption.
Statistical analysis was performed by Fisher exact test for nominal data or Student t test for continuous data. The Mann-Whitney U test was used for nonparametric data. Continuous data are presented as mean ± standard deviation or median (25%–75% interquartile range). P values less than .05 were considered significant.
3. Results
Forty-four patients were included in analysis, including 25 patients that received dexmedetomidine after protocol institution and 19 historic controls that received rapidly titrated dexmedetomidine. Both groups had comparable demographics and admitting services (Tables 1 and 2). Median {25%–75% interquartile range} APACHE II scores upon admission were similar between groups (21 {15–25} protocol group vs 22 {15–29} historic control; P = .38). The mean duration of mechanical ventilation (protocol 10.7 ± 11.1 days vs 10.2 ± 12.1 days for controls; P = .89) and ICU length of stay (protocol 14.5 ± 11.1 days, controls 11.8 ± 11.4; P = .48) were similar between groups. Additional sedation was required in 8% of protocol patients (propofol in 1 patient with subarachnoid hemorrhage and lorazepam in 1 patient after trauma).
Table 1.
Demographics and admitting services
| Protocol (n = 25) | Historical control (n = 19) | P | |
|---|---|---|---|
| Age (y) | 47.1 ± 18.3 | 55.5 ± 19.9 | .15 |
| Female (%) | 24 | 15.5 | .71 |
| APACHE II a | 21 {15–25} | 22 {15–29} | .38 |
| ICU length of stay (d) | 13.7 ± 10.6 | 11.8 ±11.4 | .61 |
| Days with mechanical ventilation | 9.5 ± 9.6 | 10.2 ± 12.1 | .85 |
| Admitting services, n (%) | |||
| Trauma | 12 (48) | 6 (31.6) | |
| Neurosurgery | 10 (40) | 6 (31.6) | |
| Cardiothoracic surgery | 1 (4) | 4 (21.0) | |
| General surgery | 2 (8) | 0 | |
| Peripheral vascular surgery | 0 | 3 (15.8) |
Data are presented as mean ± standard deviation.
Data are presented as median {25%–75% interquartile range}.
Table 2.
Dosing and hemodynamic findings
| Protocol (n = 25) | Historical control (n = 19) | P | |
|---|---|---|---|
| Loading infusion administered (%) | 0 | 7.7 | .19 |
| Initial dosage (μg kg−1 h−1) | 0.24 ± 0.08 | 0.22 ± 0.07 | .42 |
| Maximum dosage (μg kg−1 h−1) | 0.43 ± 0.02 | 0.54 ± 0.16 | .08 |
| Mean shortest time between titration (min) | 110.8 ± 173.6 | 12.8 ± 6.6 | .02 |
| Median length of infusion (h) | 19.2 | 16.6 | .14 |
| No. of dosing changes | 4.8 ± 3.8 | 7.8 ± 3.9 | .014 |
| Mean time to maximum dosage (h) | 4.8 ± 7.5 | 2.03 ± 2.51 | .14 |
| Hypotension (%) | 16 | 68.4 | .0006 |
| Bradycardia (%) | 20 | 15.4 | >.99 |
| Mean time to adverse effect (h) | 7.9 ± 7.7 | 3.8 ± 3 | .18 |
| Nadir mean arterial pressure (mm Hg) | 51.8 ± 2.2 | 51.1 ± 7.6 | .87 |
Continuous data presented as mean ± standard deviation.
The mean initial dosage of dexmedetomidine (0.24 ± 0.11 μg kg−1 h−1 protocol vs 0.22 ± 0.07 μg kg−1 h−1 controls; P = .42), the maximum dosage (0.43 ± 0.19 μg kg−1 h−1 protocol vs 0.54 ± 0.16 μg kg−1 h−1 controls; P = .08), and time to maximal dosage (259 ± 429 minutes protocol vs 153 ± 150 minutes controls; P = .4) were not statistically different between the groups (Table 2). Patients treated via protocol had significantly fewer dosage adjustments than historic control patients (protocol 4.8 ± 3.8 vs 7.8 ± 3.9 in controls; P = .014). Median durations of dexmedetomidine infusion were 19.2 {10.7–52.1} hours in the protocol group and 16.6 {7–33} hours in historic controls (P = .14). Sixteen patients received dexmedetomidine longer than 24 hours (11/25 [25%] for protocol, 5/19 [26%] for historic controls; P = .34). Two patients received loading infusions of dexmedetomidine, both historic controls (P = .19).
Seventeen patients developed hypotension, but this occurred significantly less frequently in protocol patients compared with historic controls (4 [16%] vs 13 [68.4%]; P = .0006). Bradycardia was not significantly different between groups (5 [20%] vs 3 [15.8%]; P > .99). A total of 22 patients developed hypotension and/or bradycardia (6 [24%] in the protocol group vs 16 [84%] in the historic controls; P = .0002) including 3 patients developing both (2 [8%] in the protocol group and 1 [5.3%] of the controls; P > .99). The total number of adverse drug reactions was significantly less in patients treated via protocol (7 [28%] vs 15 [78.9%]; P = .0019) than historic controls. For patients that developed hypotension, there was no statistical difference in mean arterial pressure between groups (mean nadir mean arterial pressure 51.8 ± 2.2 mm Hg protocol group vs 51.1 ± 7.6 mm Hg for historic controls; P = .87), and the mean nadir heart rates were similar for those that developed bradycardia (39.3 ± 9.9 beats per minutes for historic controls vs 37.8 ± 9.9 for controls). Time from initiation of therapy to development of hypotension was similar between protocol and historic control groups (4.2 ± 3.6 vs 3.8 ± 2.8 hours, respectively; P = .84) as was the time from initiation of therapy to bradycardia (12 ± 9.2 vs 5.9 ± 3.6 hours; P = .32). Hypotension (3.9 ±3 hours) tended to occur before bradycardia (9.7 ± 7.9 hours) in all patients, but this difference did not reach significance (P = .059). Only 2 of the 17 patients that developed hypotension had received dexmedetomidine for more than 24 hours (P > .99). For patients developing hypotension or bradycardia, all but 1 case were treated by stopping the dexmedetomidine infusion. In addition, hypotension was treated with administration of intravenous fluids in 5 patients (1 protocol patient and 4 historic controls). Four historic control patients required transient vasopressors, and 2 patients received atropine (1 in each group; P > .99).
The level of sedation or agitation 30 to 120 minutes after dexmedetomidine initiation was documented in 41 patients (24 [96%] protocol vs 17 [89.5%] historic controls; P = .57) and within 2 hours of the development of an adverse effect in all but 1 patient in the control group (Table 3). In the first hours of sedation, the median sedation scores {25%–75% interquartile range} for both groups were calm (median RASS was 0 {−2,1} for the protocol group and median Ramsay Sedation Score was 2 {1,3} for the historical controls). Around the time of development of hypotension and bradycardia, the median RASS in the protocol group was lightly sedated (−1 {−3,1}), and the median Ramsay Sedation Score for the historic controls was calm (2 {1,3}). The mean time from development of an adverse effect and documentation of sedation levels was 0.74 ± 0.7 hours.
Table 3.
Sedation/Agitation at initiation and time of adverse effects (hypotension or bradycardia)
| Protocol (n = 25) | Historical control (n = 19) | |
|---|---|---|
| Initial sedation score a, n (%) | ||
| Agitated (RASS 4 to 1, Ramsay 1) | 9 (36) | 7 (37) |
| Calm (RASS 0, Ramsay 2) | 5 (25) | 6 (32) |
| Sedated (RASS −1 to −5, Ramsay 3 to 6) | 10 (40) | 4 (21) |
| Not documented | 1 (5) | 2 (10) |
| Sedation score at time of adverse drug reaction a, n (%) | ||
| Agitated (RASS 4 to 1, Ramsay 1) | 2 (8) | 4 (21) |
| Calm (RASS 0, Ramsay 2) | 0 | 4 (21) |
| Sedated (RASS −1 to −5, Ramsay 3 to 6) | 5 (20) | 4 (21) |
| Not documented | 0 | 1 (5) |
4. Discussion
This study suggests that occurrence of hypotension associated with dexmedetomidine use in postoperative ICU patients can be significantly reduced by implementation of a dosing protocol. Although hypotension is a potential adverse effect of any sedative agent [15–22], our initial experience with dexmedetomidine showed a somewhat higher incidence of hypotension (approximately 69%) than reported by others (Table 4) [16,17,23]. Some have suggested that dexmedetomidine-associated hypotension and bradycardia are consequent to activation of α2-receptors resulting in sympatholysis [11,15,17], and others have reported that administration of dexmedetomidine without loading infusions can achieve satisfactory sedation [21,23]. We chose a slightly different approach, which was to slow down the rate of titration, and report that our protocol may reduce dexmedetomidine-associated hypotension to levels lower than previously reported (16%) [13,16,17,23].
Table 4.
Comparison of hypotension and bradycardia associated with dexmedetomidine in comparative studies
| Reference (y) | Study characteristics | Hypotension | Blood pressure (mm Hg) | Bradycardia | Heart rate (beats/min) |
|---|---|---|---|---|---|
| Corbett et al (2005) [20] | DEX n = 43 Propofol n = 46 |
Not reported | Lowest SBP 79.1 ± 12.8 83.2 ± 10 P = .096 |
Not reported | Lowest 68.1 ±10.1 74.9 ± 11.2 P = .003 |
| Elbardie et al (2004) [15] | DEX n = 30 Propofol n = 30 |
Not reported | Not reported | Not reported | Mean HR at 8 h 75 88 P = .041 |
| Herr et al (2003) [18] | DEX n = 148 Propofol n = 147 |
26% 16% P = .11 |
3% 1% P = .44 |
Similar | |
| Pandharipande et al (2007) [17] | DEX n = 52 Lorazepam n = 51 |
SBP <80 mm Hg 25% 20% P =0.51 |
17% 4% P = .03 |
||
| Riker et al (2009) [22] | DEX n = 244 Midazolam n = 122 |
SBP <80, DBP <50 or 30% ↓ 56.1% 55.7% P = .99 |
HR <40 or 30% ↓ 42.2% 18.9% P < .001 |
||
| Venn and Grounds (2001) [19] | DEX n = 20 Propofol n = 20 |
Not reported | Similar | Not reported | Mean HR 75 90 P = .0034 |
| Venn et al (1999) [16] | DEX n = 66 Placebo n = 51 |
23% Not reported |
During first hour SBP and DBP significant lower in DEX group | 15% Not reported |
Significant lower heart rate during infusion in DEX group |
DBP indicates diastolic blood pressure; DEX, dexmedetomidine; HR, heart rate; SBP, systolic blood pressure.
Although the cause is not known for certain, there are several possible mechanisms for development of dexmedetomidine-associated hypotension, especially in patients receiving rapid dosage titration. The first is an opposing effect on α2a and α2b receptors. Work by others has shown that heart rate, cardiac output, and norepinephrine concentrations decrease progressively with increasing dexmedetomidine concentrations, but dexmedetomidine causes a biphasic change in blood pressure [24]. At low concentrations (<1.9 ng/mL), mean arterial pressure decreases, followed by increasing mean arterial pressures observed with increasing dexmedetomidine concentrations [24]. It is thought that activation of peripheral α2b-receptors at higher concentrations causes vasoconstriction, thereby offsetting the vasodilation from activation of α2a-receptors. Critically ill patients receiving a maximum dosage of 0.7 μg kg−1 h−1 have demonstrated peak serum dexmedetomidine concentrations of 1.2 ng/mL with a range of 0.71–1.7 ng/mL [25]. This is below the point where the activation of α2b starts to predominate and may explain why hypotension is the most common adverse effect.
A second possible mechanism contributing to hypotension induced by dexmedetomidine relates to its pharmaco-kinetic properties. Dexmedetomidine requires extensive metabolism by the liver but appears to have minimal interaction with the cytochrome p450 enzymes [10,11]. Dexmedetomidine exhibits linear pharmacokinetics with distribution (α) half-life range of 6.0 to 8.6 minutes and elimination (β) half-life of approximately 2 to 3.1 hours in both healthy volunteers and critically ill patients [10,11,25]. Thus, completion of distribution from the central to peripheral compartments requires approximately 30 to 45 minutes, whereas steady-state drug concentrations do not occur until approximately 10 to 15 hours. Rapid titration (sooner than every 20–30 minutes) therefore provides additional drug before distribution of the previous dose is complete. This could therefore result in drug accumulation in the central compartment with development of hypotension after completion of distribution. There was a trend toward lower mean maximum dosage in the protocol group (0.43 ± 0.02 vs 0.54 ± 0.16 μg kg−1 h−1; P = .08). Because we did not measure dexmedetomidine serum concentrations, this remains a hypothesis consistent with our clinical data that can be tested in future studies.
The optimal method to safely titrate dexmedetomidine in critically ill patients has not been definitively established, but available data support the practice of slower titration. Timing of dexmedetomidine titration has only been described in 2 studies of critically ill patients: one in adults and one in children [26,27]. In adult ICU patients receiving dexmedetomidine longer than 24 hours (median, 71.5 hours), dexmedetomidine was titrated no sooner than every 15 minutes [26]. Mean systolic blood pressures decreased approximately 16% within 2 to 4 hours of initiating therapy, and the lowest single systolic blood pressure was reported 12 hours after starting therapy. Beyond 12 hours (presumably at/near steady state), systolic blood pressures showed minimal change (± 10%) during dexmedetomidine infusion. In pediatric ICU patients (median age, 5 months) receiving dexmedetomidine without loading infusions titrated with changes more than 1 hour apart, there were no episodes of dexmedetomidine-associated hypotension [27]. One patient (6%) developed hypotension when dexmedetomidine was titrated less than 1 hour after the previous change. Thus, these studies taken together with the current study suggest that a slow titration may minimize the incidence of hypotension; once again, further studies are needed to confirm.
The optimal dosage and dosing titration frequency that balance safety and efficacy are also unknown. Dexmedetomidine was approved for use in the United States, based on 2 randomized, double-blind, placebo-controlled trials with the maximum dosage of 0.7 μg kg−1 h−1 [9,16]. In our study, the maximum dosage of dexmedetomidine was also 0.7 μg kg−1 h−1, although many studies have reported higher dosages [9]. The revised labeling for procedures or surgery in nonintubated patients increases the maximal dosage to 1.0 μg kg−1 h−1 [10]. In a phase II trial in 12 medical patients, Venn et al [28] have reported maximal dosages of 2.5 μg kg−1 h−1 after their first 4 patients required additional sedation. Pandharipande et al [17] compared sedation with dexmedetomidine or lorazepam in 106 critically ill patients and used a maximal dosage of dexmedetomidine of 1.5 μg kg−1 h−1. Hypotension, reported as a systolic blood pressure less than 80 mm Hg, occurred in 25% of those receiving dexmedetomidine and 20% of those receiving lorazepam (P = .51), but significantly more patients receiving dexmedetomidine developed bradycardia (17% vs 4%; P = .03). Riker et al [22] compared dexmedetomidine to midazolam in a randomized trial where 61% of 244 patients received between 0.71 and 1.4 μg kg−1 h−1 of dexmedetomidine. Significantly more patients receiving dexmedetomidine developed bradycardia compared with those receiving midazolam (42.2% vs 18.9%; P < .001), with similar incidence of hypotension (56.1% vs 55.7%; P > .99). In our study, rate of titration did not appear to influence incidence of bradycardia, but we used a lower maximum dosage and our sample size may be too small to detect a change. Further studies are needed to determine if dosages greater than 0.7 μg kg−1 h−1 are associated with a higher rate of hypotension or bradycardia.
The time to hypotension and bradycardia was documented in only a few studies [16,18]. Venn et al [16] report 18 of 66 patients receiving dexmedetomidine after general or cardiac surgery developed hypotension and/or bradycardia. Most of these events (11/18) occurred with the loading infusion. The other 7 patients developed hypotension between 1 and 11 hours of initiation. Herr et al [18] reported that hypotension occurred in 24% of 148 patients receiving dexmedetomidine, and 8% developed hypotension within an hour and most during the loading infusion. In 20 critically ill patients, Shehabi et al [26] report that when dexmedetomidine is started without a loading infusion at 0.4 μg kg−1 h−1 and titrated to Ramsay Sedation Score between 2 and 4 for a median of 71.5 hours, mean systolic blood pressure dropped 16% within 2 hours then gradually stabilized. Heart rate decreased gradually over 12 hours by 21% with minimal changes thereafter. This is similar to our results where the mean time to hypotension was 3.9 hours compared to 9.7 hours for bradycardia. It could be that hypotension occurs sooner in critically ill patients than bradycardia, especially if the patients have intravascular volume depletion and are dependent on their adrenergic response, and this was not measured in our study.
Use of the protocol did not seem to compromise sedation, but because there were not consistent time points mandated for sedation documentation, this comparison was not perfect. At initiation of therapy, the groups had comparable sedation levels with the median in each group reported as calm (RASS 0, Ramsay Sedation Score 2) (Table 3). Our best surrogates of later sedation were sedation scores around the time of adverse drug effects or need for additional sedation. Sedation scores were documented within 2 hours of the development of hypotension or bradycardia in all but 1 patient, and median scores were similar between the protocol and control groups (protocol group median RASS −1 [light sedation] vs control group median Ramsey sedation score 2 [calm]). Use of additional sedation was allowed in the protocol, but additional sedation was required in only 2 (8%) patients, which is consistent with other comparative studies [17,20,22]. Nonetheless, because the level of sedation was not documented during the occurrence of each adverse drug event, it is unknown if there was truly a difference in this retrospective review.
Because of its retrospective nature, this study has several additional limitations. The results are hypothesis generating, and there is a potential for selection bias in our historical control group. Next, there were no predefined clinical criteria to insure that patients in each group had comparable volume status. It is also possible that protocol patients developed less hypotension because they received slightly less dexmedetomidine, but this question will require a larger sample size. Finally, we switched from using the Ramsay Sedation Scale to the Richmond Agitation Sedation Scale during the study period, and as mentioned, frequency of documentation for sedation scores was variable between patients. Although we attempted to equate the 2 sedation scores by normalizing the values, this has not been tested. For these reasons, we feel that our results will need to be confirmed independently, taking care to address these issues.
5. Conclusions
Dexmedetomidine is a sedative agent with several unique properties that make it attractive for use in critically ill patients. Although our initial experience demonstrated an unacceptably high incidence of hypotension, use of a dosing protocol was associated with significant reduction in hypotension incidence. Further prospective studies will be required to validate this protocol for use during critical illness and to determine the influence of preadministration volume status upon dexmedetomidine complications.
Footnotes
Joseph F. Dasta is a consultant and member of the Hospira Speakers Bureau for dexmedetomidine. None of the other authors have anything to disclose.
No outside finances were used to fund this study.
Author contributions—trial design: AG, SS, LM, CC; data collection: AG; data analysis: AG, SS, LM, CC.
Contributor Information
Anthony T. Gerlach, Email: gerlach.6@osu.edu.
Joseph F. Dasta, Email: jdasta@mail.utexas.edu.
Steven Steinberg, Email: steven.steinberg@osumc.edu.
Larry C. Martin, Email: larry.martin@surgery.ufl.edu.
Charles H. Cook, Email: cook.131@osu.edu.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: Building a safer health system. Washington. DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 2.Hussain E, Kao E. Medication safety and transfusion errors in the ICU and beyond. Crit Care Clin. 2005;21:91–110. doi: 10.1016/j.ccc.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Pronovost P, Wu AW, Dorman T, Morlock L. Building safety into ICU care. J Crit Care. 2002;17:78–85. doi: 10.1053/jcrc.2002.34363. [DOI] [PubMed] [Google Scholar]
- 4.Calabrese AD, Erstad BL, Brandl K, Barletta J, Kane SL, Sherman D. Medication administration errors in adult patient in the intensive care unit. Intensive Care Med. 2001;27(15):92–1598. doi: 10.1007/s001340101065. [DOI] [PubMed] [Google Scholar]
- 5.Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: a comparison of intensive care and general care units. Crit Care Med. 1997;25:1289–97. doi: 10.1097/00003246-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Kane-Gill SL, Weber RJ. Principles and practices of medication errors in the ICU. Crit Care Clin. 2006;22:273–90. doi: 10.1016/j.ccc.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–41. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Kollef MH, Levy NT, Ahrens TS, Schaiff R, Prentice D, Sherman G. The use of continuous i.v. sedation is associated with prolongation of mechanical ventilation. Chest. 1998;114:541–8. doi: 10.1378/chest.114.2.541. [DOI] [PubMed] [Google Scholar]
- 9.Gerlach AT, Dasta JF. Dexmedetomidine: an updated review. Ann Pharmacother. 2007;41:245–54. doi: 10.1345/aph.1H314. [DOI] [PubMed] [Google Scholar]
- 10.Product Information Precedex (dexmedetomidine) Lake Forrest, IL: Hospira; 2008. [Google Scholar]
- 11.Bhana N, Goa KL, McClellan K. Dexmedetomidine Drugs. 2000;59:263–8. doi: 10.2165/00003495-200059020-00012. [DOI] [PubMed] [Google Scholar]
- 12.Pandharipande PP, Ely EW, Maze M. Dexmedetomidine for sedation and perioperative management of critically ill patients. Semin Anesth Periop Med Pain. 2006;25:43–50. [Google Scholar]
- 13.Gerlach AT, Dasta JF, Martin LM, Cook CH. Effect of titration methods on adverse reactions to dexmedetomidine (abstr) Crit Care Med. 2005;33:A112. [Google Scholar]
- 14.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 15.Elbaradie S, El Mahalawy FH, Solyman AH. Dexmedetomidine versus propofol for short-term sedation of postoperative mechanically ventilated patients. J Egyptian Nat Cancer Inst. 2004;16:153–8. [PubMed] [Google Scholar]
- 16.Venn RM, Bradshaw CJ, Spencer R, Brealey D, Caudwell E, Naughton C, et al. Preliminary UK experience of dexmedetomidine, a novel agent for postoperative sedation in the intensive care unit. Anaesth. 1999;54:1136–42. doi: 10.1046/j.1365-2044.1999.01114.x. [DOI] [PubMed] [Google Scholar]
- 17.Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TG, Miller R, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients. JAMA. 2007;298:2644–53. doi: 10.1001/jama.298.22.2644. [DOI] [PubMed] [Google Scholar]
- 18.Herr DL, Sum-Ping ST, England M. ICU sedation after coronary artery bypass surgery: dexmedetomidine-based versus propofol-based sedation regimens. J Cardiothor Vasc Anesth. 2003;17:576–84. doi: 10.1016/s1053-0770(03)00200-3. [DOI] [PubMed] [Google Scholar]
- 19.Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth. 2001;87:884–90. doi: 10.1093/bja/87.5.684. [DOI] [PubMed] [Google Scholar]
- 20.Corbett SM, Rebuck JA, Greene CM, Callas PW, Neale BW, Healey MA, et al. Dexmedetomidine does not improve patients satisfaction when compared to propofol during mechanical ventilation. Crit Care Med. 2005;33:940–5. doi: 10.1097/01.ccm.0000162565.18193.e5. [DOI] [PubMed] [Google Scholar]
- 21.Ickeringill M, Shehabi Y, Adamson H, Reuttimann U. Dexmedetomidine infusion without loading infusion in surgical patients requiring mechanical ventilation; hemodynamic effects and efficacy. Anaesth Intensive Care. 2004;32:741–5. doi: 10.1177/0310057X0403200602. [DOI] [PubMed] [Google Scholar]
- 22.Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489–99. doi: 10.1001/jama.2009.56. [DOI] [PubMed] [Google Scholar]
- 23.Dasta JF, Kane-Gill SL, Durtschi AJ. Comparing dexmedetomidine prescribing patterns and safety in the naturalistic setting versus published data. Ann Pharmacother. 2004;38:1130–5. doi: 10.1345/aph.1D615. [DOI] [PubMed] [Google Scholar]
- 24.Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94. doi: 10.1097/00000542-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Venn RM, Karol MD, Grounds RM. Pharmacokinetics of dexmedetomidine infusion for sedation of postoperative patients requiring intensive care. Br J Anesth. 2002;88:669–75. doi: 10.1093/bja/88.5.669. [DOI] [PubMed] [Google Scholar]
- 26.Shehabi Y, Ruettimann U, Adamson H, Innes R, Ickeringill M. Dexmedetomidine infusion for more than 24 hours in critically ill patients: sedative and cardiovascular effects. Intensive Care Med. 2004;30:2188–96. doi: 10.1007/s00134-004-2417-z. [DOI] [PubMed] [Google Scholar]
- 27.Buck ML, Willson DF. Use of dexmedetomidine in the pediatric intensive care unit. Pharmacotherapy. 2008;28:51–7. doi: 10.1592/phco.28.1.51. [DOI] [PubMed] [Google Scholar]
- 28.Venn RM, Newmann PJ, Grounds RM. A phase II study to evaluate the efficacy of dexmedetomidine for sedation in the medical intensive care units. Intensive Care Med. 2003;29:201–7. doi: 10.1007/s00134-002-1579-9. [DOI] [PubMed] [Google Scholar]