Abstract
The safety, stability, and ability for repeat homologous vaccination makes the DNA vaccine platform an excellent candidate for an effective HIV-1 vaccine. However, the immunogenicity of early DNA vaccines did not translate from small animal models into larger non-human primates and was markedly lower than viral vectors. In addition to improvements to the DNA vector itself, delivery with electroporation, the inclusion of molecular adjuvants, and heterologous prime-boost strategies have dramatically improved the immunogenicity of DNA vaccines for HIV and currently makes them a leading platform with many areas warranting further research and clinical development.
Introduction
Owing to recent technical improvements, which have shown improved immune potency in vivo, plasmid DNA vaccines are again gaining importance as parts of potential HIV-vaccine platforms. DNA vaccines have an impeccable safety profile, are relatively easy to manufacture and to manipulate, and are remarkably stable making for ideal distribution in developing nations. Despite promising initial studies in small animal models [1–4], immunogenicity in larger species including non-human primates (NHP) and humans was disappointing [5,6]. Following up on these early studies, improvements to the vectors, insert sequence optimization, novel delivery methods and the inclusion of gene adjuvants has greatly improved both cellular and humoral immune responses induced by this platform so that HIV DNA vaccines are now performing as well as highly immunogenic viral vectors [7••]. These improvements make DNA vaccines more attractive as components of prime-boost platforms as well as in particular stand alone situations. This brief review will illustrate some important ways that have served to improve the immunogenicity of DNA vaccines to HIV-1 such as improved delivery, the inclusion of molecular adjuvants, as well as prime-boosting.
Delivery
An important approach to improve DNA vaccine immunogenicity is to increase the amount of DNA/plasmid delivered to cells, as this increases antigen expression. Various plasmid needle-free delivery devices have been studied in this regard, such as the gene gun, patch systems or jet injection devices. Jet injection involves using high pressure to deliver a liquid formulation of DNA mm to cm below the skin’s surface. It has been reported effective in delivery of DNA through the skin deep into the muscle below and has been studied in the clinic. One issue with the performance of jet injection is a limitation on the volume of liquid that can be loaded into the delivery system, which is usually 1 ml. Accordingly, formulations require high concentrations of DNA. This technique is very adaptable and more studies are in progress. A more superficial delivery system is DNA administration by gene gun. This platform utilizes high pressure to deliver DNA coated gold nanoparticles to the dermis, an antigen presenting cell rich area. This approach has been particularly effective at driving antibody production in vivo. Only a small amount of DNA is needed for this approach and seroconversion can be observed with very low doses of DNA delivered in diverse animal systems as well as humans, resulting in very encouraging results. There are limitations in scaling up delivery with this platform, as the amount of gold beads that can be loaded with DNA and delivered at a single time is limited, thus effectively reducing the volume that can be delivered. More recently needle-free delivery as well as patch systems has been studied successfully in smaller animal systems. These are desirable vaccine delivery approaches and while these technologies are early in their study they will continue to receive attention in the future [8,9].
An older technology that has been reinvented and reapplied with vigor the DNA delivery area is in vivo electroporation (EP). EP has been used to transfect cells in vitro for almost 30 years. Recently it has been explored to increase the transfection efficiency of DNA vaccines in vivo [10]. Electroporation involves applying a small electric field across the site of injection in order to cause temporary membrane instability and produce an electric gradient, which increases cellular uptake of locally delivered macromolecules such as DNA [11,12]. Intramuscular vaccination has been extensively studied in NHP and safely used in humans. Initial studies with an HIV-1 DNA vaccine in rhesus macaques demonstrated that delivery with EP resulted in 10–40 fold increases in HIV-specific ELISpot responses compared with a fivefold higher dose of naked DNA [13••]. In vivo, EP has also been shown to increase the quality of the HIV-specific immune responses by increasing CD8+ T-cell proliferation and functionality compared with naked HIV-DNA vaccination alone [14]. Though DNA vaccines were traditionally largely considered a platform for induction of cellular immunity, delivery with EP generates robust humoral immunity to SIV as well [15]. DNA vaccines to influenza virus delivered by EP induce titers of 1:40 tested by a hemagglutination inhibition assays in ferrets, and thus the benchmark for product development against this pathogen [16]. The safety and immunogenicity of a HIV DNA vaccine delivered with IM EP has recently been evaluated in phase I clinical trials (HVTN 080) and preliminary reports demonstrate enhanced cellular immunity compared with IM DNA delivery without EP.
Though IM EP has been extensively studied and results in consistently and reproducibly enhanced immune responses, many variations on this theme are in development. The field is focusing on alternative targets for DNA delivery by EP. Current research has led to new devices capable of highly efficient delivery to intradermal tissues for example. Furthermore, microneedles and needle-free electroporation arrays are being studied [17,18]. In addition to being easier to administer, dermal delivery may increase or uniquely modulate immunogenicity by directly transfecting APCs, which exist at high density in the skin [19]. Delivery of a DNA vaccine with a minimally invasive, low voltage EP device has been reported to induce protective immunity against an influenza challenge [20]. Newer devices do not generate tissue damage during routine vaccine delivery. How these new devices will impact current HIV DNA vaccines still needs to be evaluated in NHPs and humans but these approaches represent a straightforward improvement in vaccine delivery.
Molecular adjuvants
Molecular adjuvants are commonly used to increase or modify the immunogenicity of DNA-based vaccines. Molecular adjuvants can be divided into two groups: cytokine and chemokine molecules. Unlike traditional adjuvants, molecular adjuvants are delivered as plasmid vector along with the antigen-encoded vector. Upon delivery, the vector encoding the molecular adjuvant transduces cells at the site of vaccination that can then secrete the adjuvant molecule.
Cytokine molecular adjuvants can be generally classified as either Th1 promoting or Th2 promoting. Th1 adjuvants include IL-2, IFN-γ, IL-12, and IL-15 and generally work to augment cellular immunity [21–23]. By contrast, Th2 cytokines such as granulocyte-macrophage cell stimulating factor (GM-CSF), IL-1, and IL-4 enhance humoral immunity [24–26]. Because the activation of the Th1 or Th2 pathway inhibits the activation of the alternate pathway, care has to be taken with molecular adjuvants to not overly skew the response towards either pathway and inhibit induction of potentially crucial effector mechanisms [27].
Research into molecular adjuvants began over 10 years ago. GM-CSF was one of the first adjuvants to clearly demonstrate that a cytokine vector could modulate vaccine induced immunity. In mice receiving a rabies DNA vaccine alone, or co-administered with a GM-CSF expressing plasmid, GM-CSF adjuvanted mice showed enhanced cytotoxic T-cell, Th1 T-helper cell, and binding antibody titers [28]. Similarly, HIV vaccination with GM-CSF increased antibody responses and lymphopro-liferation in mice [29]. Recently, inclusion of a GM-CSF expressing plasmid delivered with a DNA-prime that was followed by a Modified Vaccinia Ankara virus (MVA)-boost resulted in enhanced IgG, neutralization, and increased protection from a repeat low dose SIVsmE660 challenge in vaccinated rhesus macaques [30].
Like GM-CSF, IL-12 was another early molecular adjuvant and the first Th1 adjuvant studied. As a Th1 adjuvant IL-12 has had profound positive effects on vaccines tested in nonhuman primates. In mouse models, IL-12 increased CD8+ T-cell mediated lysis of target cells 4.5 fold [31]. HIV-1 vaccination of non-human primates with IL-12 demonstrated increased cellular responses that corresponded with control of viremia and improved clinical outcomes following a SHIV98.6P challenge [32]. The ability of IL-12 as a genetic adjuvant to increase HIV-1-specific responses following HIV-1 DNA vaccination with gag, env and pol is currently being examined in the clinic through the HIV Vaccine Trials Network. These IL-12 adjuvanted DNA vaccines have been well tolerated and they were shown to be immunogenic in humans.
IL-15 alone and in combination with IL-12 has also been extensively studied as an adjuvant to DNA vaccination. Together with IL-7 and IL-2, IL-15 provides signals important for T-cell survival. Rhesus macaques vaccinated with an HIV DNA vaccine and IL-15 demonstrated increased levels of effector memory CD8+ T-cells [33]. Unlike most Th1 adjuvants, IL-15 has also been shown to enhance DNA vaccine-induced humoral immunity [34]. The ability to augment both humoral and cellular immunity makes IL-15 an interesting adjuvant for HIV vaccine development, where efficacious vaccines need to induce both humoral and cellular immunity.
Chemokine adjuvants
Chemokines are molecules that control the trafficking of lymphocytes and direct them to sites of inflammation. By utilizing chemokine molecular adjuvants, it is possible to modulate the magnitude and characteristics of DNA vaccine-induced mucosal immunity. This may be particularly important for an HIV vaccine that needs to induce mucosal protection to prevent infection. CCL27 (CTECK) has been shown to increase mucosal homing of antigen-specific cells in mice and monkeys following a HIV-1 DNA vaccination [35]. Though studies with mucosal chemokines are ongoing, these data support the concept that a HIV DNA vaccine delivered IM could induce mucosal immunity, which would be highly advantageous to ward off pathogens that invade through the airway, the genital, or the intestinal surfaces.
Prime-boosting
An effective HIV-1 vaccine will probably need to induce robust effector T-cell responses as well as broadly neutralizing and binding antibody responses. One method of improving the magnitude and quality of the overall HIV-specific response is the use of heterologous prime-boost strategies. By combining DNA vaccines with either viral vectors or a recombinant protein a synergistic enhancement of immunity can improve challenge outcome. This concept has received a significant boost in attention owing to the success in the RV-144 ‘Thai’ HIV vaccine trail [36••]. After two clear failures in the attempt to show vaccine efficacy in clinical trials, RV-144 achieved a modest but important success. A prior trial of one of the RV-144 components, that is, Vaxgen recombinant protein immunization for induction of antibody responses was unsuccessful in preventing HIV infection. Similarly, vaccines designed to only induce T-cell responses such as a recombinant adenoviral vector of serotype 5 (Merck STEP trial), were also not effective at preventing HIV infection, or lowering viral load [37• •]. By contrast, the RV-144 trial used viral vector priming with a recombinant poxviral vector, followed by boosting with the Vaxgen recombinant envelope antigen. This trial showed partial effectiveness at preventing infection for up to 6 months post the full vaccine protocol. Table 1 provides some strengths and weaknesses of these major vaccine development platforms.
Table 1.
Comparison of some advantages/disadvantages of important vector vaccine platforms for generating HIV-specific cellular immunity
| Vaccine platforms | Advantages | Disadvantages |
|---|---|---|
| DNA vectors | can be used for homologous boosting | Immune responses have historically been low – EP strategies look improved |
| stable | Limited local site delivery of antigen | |
| generates cellular and humoral immunity | Delivery enhancement is important to overcome current limitations | |
| successful licensure of veterinary vaccines | Improved vaccine formulations important | |
| Adenovirus vectors | robust CD8+ responses, combination serotypes and species unique viruses improve responses | pre-existing immunity in many populations limits effectiveness |
| efficiently transduces mammalian cells | safety concerns in seropositive | |
| Most potent viral platform to drive cellular immunity in humans | need for complementing cell lines | |
| poxvirus vectors | limited pre-existing immunity | anti-vector immunity |
| successful licensure of veterinary vaccines | reduced immunogenicity compared with other viral vector platforms | |
| Promising results in RV-144 Thai trial |
The inability to induce HIV-1-specific broadly neutralizing antibodies through traditional immunization strategies has led many in the field of HIV vaccine development to focus on the need for cellular immune responses capable of clearing virally infected cells. Among the most potent approaches for induction of a focused CD8+ T cell response is DNA-prime followed by viral-vector-boost. This dual modality approach drives effective improvement in T cell expansion that allows partial bypass of anti-vector induced immunity. DNA vaccine priming has been shown to focus the immune response on the plasmid-encoded antigen. When followed by the viral vector boost, expansion of the immune response is now focused on the vector-encoded vaccine antigens, rather than the nonrelevant antigens that are part of the viral vector.
By contrast, viral vector priming results in significant anti-vector immunity that reduces the ability of further homologous vaccination to boost responses primed by the initial dose [38].
The most extensively studied viral vectors for an HIV heterologous prime-boost vaccine include those based on adenoviruses and poxviruses (Table 1). The replication defective adenovirus serotype 5 (Ad5) vector gained popularity owing to its ability to generate robust effector CD8+ T-cell responses and impact viral load following a SHIV, SIVmac239 and SIVmac251 challenge when used alone or in combination with a DNA-prime [39•,40•,41•,42•]. These vectors remain the most robust ever developed for driving a T cell response in humans. However, reduced efficacy and safety concerns pertaining to vaccinating subjects naturally seropositive to Ad5 lead to the development of alternative rAd vectors with a naturally lower seroprevalence than Ad5 [37••,43]. This is particularly important in the developing world vaccine setting, where Ad seropositivity is particularly common.
Several classes of rare Ad vectors have been explored recently. These include rare human serotypes such as Ad11, Ad35, and Ad26 that have a seroprevalence of 5–15% in developed countries compared with the 50–90% observed for Ad5 [44,45]. Another approach involves using rAd vectors based on chimpanzee Ads that have a seroprevelence of less than 10%, even in zoo workers and populations living in close proximity with wild chimpanzees [46]. Rare Ad vectors have the ability to induce robust HIV-specific cellular responses in NHP [47,48]. However, limited work has been done to determine whether an HIV DNA-prime can further increase efficacy. Additionally, owing to a 90% capsid sequence homology between all Ad serotypes, human trials will be crucial to determine the safety and efficacy of these vectors as even seronegative subjects have cross-reactive Ad-specific T-cells, which may react to Ad vector vaccination [49] and modulate vector driven immunity.
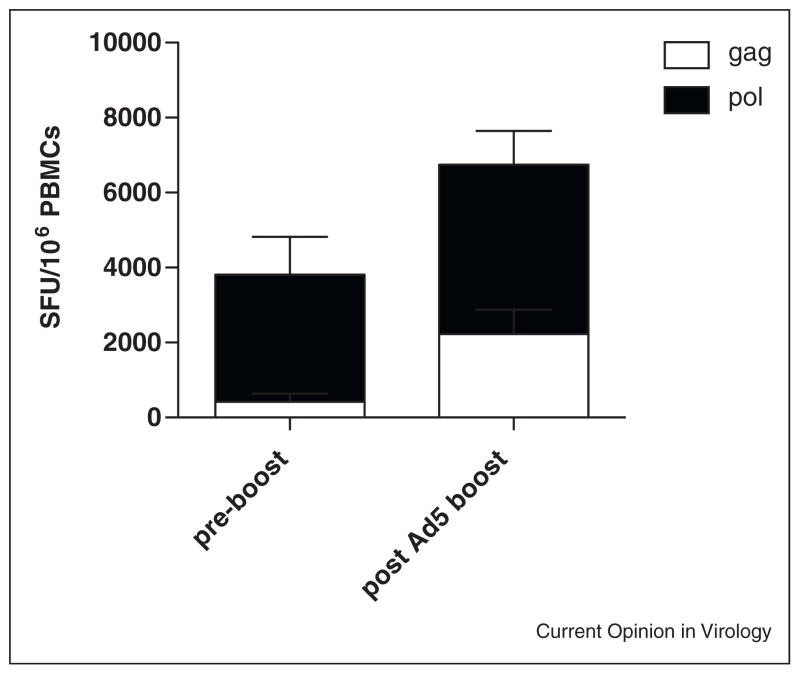
The development of modern EP technology has provided a new option for DNA-prime viral vector boosting. In the literature, most DNA prime-boost studies were performed with older DNA strategies that generated weak immunity when administered alone. We have previously shown that repeated immunization with a highly optimized SIV DNA with IL-12 and electroporation can induce cellular responses as good or better than rAd5 [7••]. By combining priming with a highly optimized DNA vaccine we were not only capable of generating robust T-cell responses [7••], but we also observed that a year after priming, these responses were efficiently boosted with only two doses of a highly immunogenic rAd5-SIV vaccine (Figure 1). These data warrant further studies to optimize prime-boost strategies utilizing newer, more robust HIV DNA vaccine platforms.
Figure 1.
An SIV DNA-prime Ad5-boost enhances cellular immunity. Five Indian rhesus macaques received three doses of 1.0 mg each pVax consensus SIV gag/pol/env at weeks 0, 6, 12, and 18 delivered intramuscular with electroporation (Inovio Pharmaceuticals, Inc.) followed by two doses of 1 × 1010 viral particles (vp) Ad5 SIV gag/pol/nef (Merck and Company) at weeks 52 and 56. Following two doses of an Ad5 boost, IFN-g responses were significantly increased from pre-boost levels (p < 0.03).
In addition to rAd vectors, extensive research has gone into the use of poxvirus vectors such as NYVAC, a highly attenuated vaccinia virus strain, canarypox, and MVA. Though comparative studies have suggested that Ad5 is more immunogenic than poxviral vectors [39•,41•] for driving cellular immune responses, studies in both NHP and humans demonstrated that a DNA-prime MVA-boost can generate enhanced antibody and cellular responses to HIV/SIV antigens [50].
Several versions of poxviral prime-boost studies are in development. One such study that has recently started is RV-262, which examines the ability of a highly optimized DNA vaccine delivered by EP to be boosted by a HIV recombinant poxviral vaccine. In this phase I study, called RV262, evaluation of a combination DNA-prime MVA vector-boost vaccine regimen is being studied. This approach seeks to drive immune responses against diverse subtypes of HIV-1 prevalent in North America, Europe, Africa and South America. The study is being conducted by the U.S. Military HIV Research Program (MHRP) through its clinical research network in the U.S., East Africa and Thailand. This clinical trial was designed to test a unique prime-boost preventive HIV vaccination strategy aimed at global coverage. The prime is a plasmid DNA vaccine, PENNVAX-G, and the boost is a virus vector vaccine, MVA-Chiang Mai Double Recombinant (MVA-CMDR). Together, the vaccines are designed to deliver a diverse mixture of antigens for HIV-1 subtypes A, B, C, D and E. The results of this study will have important implications for EP-DNA prime-MVA-boost approaches.
The success of preclinical studies evaluating a DNA-prime viral vector-boost has lead to the initiation of two large clinical trials to further access the protective efficacy of these strategies in humans. One of the most prominent trials, HVTN 505, is a phase II study enrolling 1350 subjects to test the safety and efficacy of a DNA-prime followed by an Ad5-boost vaccination strategy developed by the Vaccine Research Center (VRC). Another phase II study is being conducted to evaluate the efficacy of a DNA-prime followed by a MVA-boost (HVTN 205).
In addition to viral vector boosting, DNA priming can expand host B cell immunity, which can be further boosted by a recombinant protein. In addition to improving the magnitude of HIV-specific immune responses, heterologous prime-boost strategies afford the possibility to modify the ‘quality’ of the immune response. In a study comparing a DNA-prime recombinant protein-boost versus either platform alone, the inclusion of a DNA-prime enhanced the avidity and neutralization of HIV-specific antibodies [51]. Importantly, the success of this approach achieved in animal models has translated to humans with the first report of neutralizing antibodies against clade A–E primary isolates elicited by a multiclade DNA-prime recombinant protein-boost strategy HIV-1 vaccine [52•,53•].
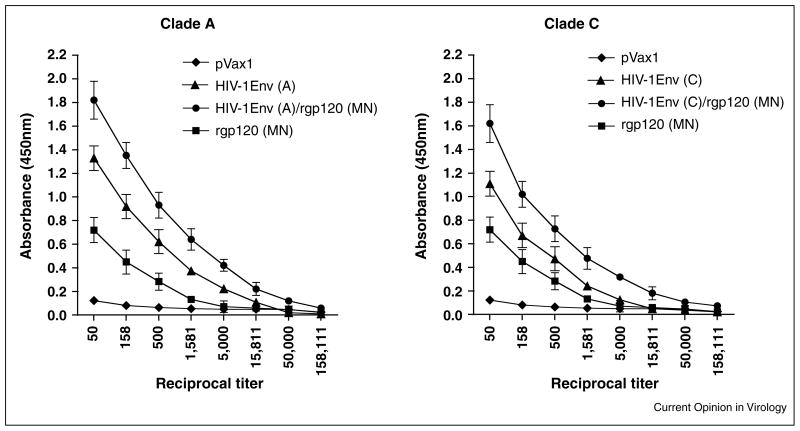
Though these results are promising, they may be further improved by delivery of a DNA priming with EP. In a study comparing a HIV clade A and C DNA vaccine delivered with IM EP and followed by a gp120 boost either alone or in combination in BALB/c mice, we observed that three doses of DNA alone induced a higher binding antibody titers than a single dose of protein alone (Figure 2). However, a prime-boost strategy resulted in the most robust antibody titers. The promising results of these studies are being confirmed in rabbits and NHPs where not just binding, but neutralizing titers can be studied. Currently, the ability of a multivalent HIV DNA-prime, recombinant envelope protein-boost to enhance cellular immune responses and induce cross-subtype neutralizing antibodies is being evaluated in a phase I clinical trial (DP6-001) [53•].
Figure 2.
Improvement of antigp120IgG responses after protein boosts in Balb/C mice primed with HIV-1 Envelope DNA vaccine. Four groups of 4 mice were immunized either three times with pVax DNA (diamond) or HIV-1Env DNA (triangle) in 2 weeks interval, three doses of HIV-1 env DNA followed by a protein boost (HIV-1Env/rgp120, circle), or a single dose of rgp120 (square). Sera were collected two weeks after the final vaccination. Binding of antisera against subtype A or C gp120s to envelope proteins from clade B viruses (MN). Values represent mean (n = 4) and the SEM.
Conclusions
Intensive research over the past 20 years has lead to remarkable improvements in the immunogenicity of HIV DNA vaccines. Following years of failures, the recent RV-144 trial, showing a modest prevention of heterosexual transmission, has been viewed as an important achievement that is refocusing efforts in the HIV vaccine field, and engendered a renewed interest in prime-boost strategies. Many clinical trials are ongoing and will provide important data for further development. New developments in DNA technologies are likely to play a more and more important role in future HIV vaccine studies. Further research into delivery, molecular adjuvants and prime-boost strategies may generate the magnitude, quality and breadth of cellular and humoral responses needed for an effective HIV vaccine.
Footnotes
Disclosure statement
DBW notes that he has important commercial relationships that should be taken into consideration when reviewing this publication. These are associated with this work from consulting fees, stock ownership, Advisory Board or Review Board Service, speaking support that include the following companies: Pfizer, Inovio, BMS, VGXI, Virxsys, Ichor, Merck, Althea, Aldevron, Novartis, and possibly others.
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
- 1.Tang DC, DeVit M, Johnston SA. Genetic immunization is a simple method for eliciting an immune response. Nature. 1992;356:152–154. doi: 10.1038/356152a0. One of the initial study demonstrating that balistic delivery of plasmid DNA coated gold particles can serve as a vaccine strategy. [DOI] [PubMed] [Google Scholar]
- 2.Fynan EF, Webster RG, Fuller DH, Haynes JR, Santoro JC, Robinson HL. DNA vaccines: protective immunizations by parenteral, mucosal, and genegun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–11482. doi: 10.1073/pnas.90.24.11478. Naked DNA vaccination was improved with gene gun delivery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ulmer JB, Donnelly JJ, Parker SE, Rhodes GH, Felgner PL, Dwarki VJ, Gromkowski SH, Deck RR, DeWitt CM, Friedman A, et al. Heterologous protection against influenza by injection of DNA encoding a viral protein. Science. 1993;259:1745–1749. doi: 10.1126/science.8456302. One of the initial studies demonstrating that naked DNA may serve as an effective vaccine platform. [DOI] [PubMed] [Google Scholar]
- 4.Wang B, Ugen KE, Srikantan V, Agadjanyan MG, Dang K, Refaeli Y, Sato AI, Boyer J, Williams WV, Weiner DB. Gene inoculation generates immune responses against human immunodeficiency virus type 1. Proc Natl Acad Sci USA. 1993;90:4156–4160. doi: 10.1073/pnas.90.9.4156. First use of naked DNA as an HIV-1 vaccine in mice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyer JD, Wang B, Ugen KE, Agadjanyan M, Javadian A, Frost P, Dang K, Carrano RA, Ciccarelli R, Coney L, et al. In vivo protective anti-HIV immune responses in non-human primates through DNA immunization. J Med Primatol. 1996;25:242–250. doi: 10.1111/j.1600-0684.1996.tb00022.x. Initial study of a HIV-1 DNA vaccine in non-human primates. [DOI] [PubMed] [Google Scholar]
- 6.MacGregor RR, Boyer JD, Ugen KE, Lacy KE, Gluckman SJ, Bagarazzi ML, Chattergoon MA, Baine Y, Higgins TJ, Ciccarelli RB, et al. First human trial of a DNA-based vaccine for treatment of human immunodeficiency virus type 1 infection: safety and host response. J Infect Dis. 1998;178:92–100. doi: 10.1086/515613. First study showing the safe delivery of a DNA vaccine in HIV infected humans. [DOI] [PubMed] [Google Scholar]
- 7.Hirao LA, Wu L, Satishchandran A, Khan AS, Draghia-Akli R, Finnefrock AC, Bett AJ, Betts MR, Casimiro DR, Sardesai NY, et al. Comparative analysis of immune responses induced by vaccination with SIV antigens by recombinant Ad5 vector or plasmid DNA in rhesus macaques. Mol Ther. 2010;18:1568–1576. doi: 10.1038/mt.2010.112. SIV DNA vaccination with EP induced similar or better cellular immunity when compared with the Merck Ad5 SIV vaccine in rhesus macaques. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanke T, Neumann VC, Blanchard TJ, Sweeney P, Hill AV, Smith GL, McMichael A. Effective induction of HIV-specific CTL by multiepitope using gene gun in a combined vaccination regime. Vaccine. 1999;17:589–596. doi: 10.1016/s0264-410x(98)00238-2. Intradermal DNA vaccination with gene gun delivery alone was not as immunogenic as IM vaccination, however IM prime, ID genegun boost may represent a novel method for improved immunity. [DOI] [PubMed] [Google Scholar]
- 9.Yoshizawa I, Soda Y, Mizuochi T, Yasuda S, Rizvi TA, Takemori T, Tsunetsugu-Yokota Y. Enhancement of mucosal immune response against HIV-1 Gag by DNA immunization. Vaccine. 2001;19:2995–3003. doi: 10.1016/s0264-410x(00)00539-9. Improved HIV responses followin IM vaccination compared with genegun delivery. [DOI] [PubMed] [Google Scholar]
- 10.Neumann E, Schaefer-Ridder M, Wang Y, Hofschneider PH. Gene transfer into mouse lyoma cells by electroporation in high electric fields. EMBO J. 1982;1:841–845. doi: 10.1002/j.1460-2075.1982.tb01257.x. Classic study illustrating the electroporation can increase DNA vector uptake by cells in vitro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tieleman DP. The molecular basis of electroporation. BMC Biochem. 2004;5:10. doi: 10.1186/1471-2091-5-10. Electroporation induced transient holes in a lipid membrane. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tarek M. Membrane electroporation: a molecular dynamics simulation. Biophys J. 2005;88:4045–4053. doi: 10.1529/biophysj.104.050617. Simulation of the effect of electroporation of membrane permeability and DNA vector uptake. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13••.Luckay A, Sidhu MK, Kjeken R, Megati S, Chong SY, Roopchand V, Garcia-Hand D, Abdullah R, Braun R, Montefiori DC, et al. Effect of plasmid DNA vaccine design and in vivo electroporation on the resulting vaccine-specific immune responses in rhesus macaques. J Virol. 2007;81:5257–5269. doi: 10.1128/JVI.00055-07. Delivery of a HIV DNA vaccine with EP in NHP enhanced immunogenicity in NHPs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hirao LA, Wu L, Khan AS, Hokey DA, Yan J, Dai A, Betts MR, Draghia-Akli R, Weiner DB. Combined effects of IL-12 and electroporation enhances the potency of DNA vaccination in macaques. Vaccine. 2008;26:3112–3120. doi: 10.1016/j.vaccine.2008.02.036. Initial NHP study demonstrating enhanced DNA vaccine immunogenicity with IM EP delivery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yin J, Dai A, Lecureux J, Arango T, Kutzler MA, Yan J, Lewis MG, Khan A, Sardesai NY, Montefiore D, et al. High antibody and cellular responses induced to HIV-1 clade C envelope following DNA vaccines delivered by electroporation. Vaccine. 2010 doi: 10.1016/j.vaccine.2010.12.055. Demonstration of rubost humoral and cellular immunity in NHP by a HIV DNA vaccine delivered with EP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broderick KE, Shen X, Soderholm J, Lin F, McCoy J, Khan AS, Yan J, Morrow MP, Patel A, Kobinger GP, et al. Prototype development and preclinical immunogenicity analysis of a novel minimally invasive electroporation device. Gene Ther. 2011:18258–18265. doi: 10.1038/gt.2010.137. [DOI] [PubMed] [Google Scholar]
- 17.Hirao LA, Wu L, Khan AS, Satishchandran A, Draghia-Akli R, Weiner DB, et al. Intradermal/subcutaneous immunization by electroporation improves plasmid vaccine delivery and potency in pigs and rhesus macaques. Vaccine. 2008;26:440–448. doi: 10.1016/j.vaccine.2007.10.041. Skin electroporation enhanced DNA vaccine immunogenicity compared with naked DNA vaccinaiton alone and was predominantly Th1 type. [DOI] [PubMed] [Google Scholar]
- 18.Prausnitz MR, Mikszta JA, Cormier M, Andrianov AK. Microneedle-based vaccines. Curr Top Microbiol Immunol. 2009;333:369–393. doi: 10.1007/978-3-540-92165-3_18. Effective delivery of a DNA vaccine to NHP by microneedle array. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Condon C, Watkins SC, Celluzzi CM, Thompson K, Falo LD., Jr DNA-based immunization by in vivo transfection of dendritic cells. Nat Med. 1996;2:1122–1128. doi: 10.1038/nm1096-1122. Intradermal DNA vaccination results in transfection of skin resident DCs that traffic to the draining lymph node. [DOI] [PubMed] [Google Scholar]
- 20.Broderick KE, Shen X, Soderholm J, Lin F, McCoy J, Khan AS, Yan J, Morrow MP, Patel A, Kobinger GP, et al. Prototype development and preclinical immunogenicity analysis of a novel minimally invasive electroporation device. Gene Ther. 2011;18:258–265. doi: 10.1038/gt.2010.137. A novel, low voltage, minimally invasive dermal EP device ia capable of inducing protective HAI titers following influenza H1N1 vaccination. [DOI] [PubMed] [Google Scholar]
- 21.Kim JJ, Ayyavoo V, Bagarazzi ML, Chattergoon MA, Dang K, Wang B, Boyer JD, Weiner DB. In vivo engineering of a cellular immune response by coadministration of IL-12 expression vector with a DNA immunogen. J Immunol. 1997;158:816–826. Enhanced HIV CTL responses observed with the co-administration of IL-12 and GM-CSF adjuvants. [PubMed] [Google Scholar]
- 22.Kim JJ, Yang JS, Lee DJ, Wilson DM, Nottingham LK, Morrison L, Tsai A, Oh J, Dang K, Dentchev T, et al. Macrophage colony-stimulating factor can modulate immune responses and attract dendritic cells in vivo. Hum Gene Ther. 2000;11:305–321. doi: 10.1089/10430340050016049. Co-administration of M-CSF enhanced CTL responses while GM-CSF enhanced antibodies following HIV-1 DNA vaccination. [DOI] [PubMed] [Google Scholar]
- 23.Boyer JD, Robinson TM, Kutzler MA, Parkinson R, Calarota SA, Sidhu MK, Muthumani K, Lewis M, Pavlakis G, Felber B, Weiner D. SIV DNA vaccine co-administered with IL-12 expression plasmid enhances CD8 SIV cellular immune responses in cynomolgus macaques. J Med Primatol. 2005;34:262–270. doi: 10.1111/j.1600-0684.2005.00124.x. Cynomolgus macaques immunized with plasmid expressing SIVgag in combination with IL-12 had expanded antigen-specific IFN-gamma positive effector cells as well as granzyme B production. [DOI] [PubMed] [Google Scholar]
- 24.Kayamuro H, Yoshioka Y, Abe Y, Arita S, Katayama K, Nomura T, Yoshikawa T, Kubota-Koketsu R, Ikuta K, Okamoto S, et al. Interleukin-1 family cytokines as mucosal vaccine adjuvants for induction of protective immunity against influenza virus. J Virol. 2010;84:12703–12712. doi: 10.1128/JVI.01182-10. IL-1 family cytokines as vaccine adjuvants increase serum IgG and mucosal IgA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim JJ, Yang JS, Montaner L, Lee DJ, Chalian AA, Weiner DB. Coimmunization with IFN-gamma or IL-2, but not IL-13 or IL-4 cDNA can enhance Th1-type DNA vaccine-induced immune responses in vivo. J Interferon Cytokine Res. 2000;20:311–319. doi: 10.1089/107999000312450. Comparison of molectula adjuvants IL-2, IL-4 IFN-g and IL-13 illustrates that IFN-g can drive a Th1 type antigen specific immune response following vaccination. [DOI] [PubMed] [Google Scholar]
- 26.Chu Y, Xia M, Lin Y, Li A, Wang Y, Liu R, Xiong S. Th2-dominated antitumor immunity induced by DNA immunization with the genes coding for a basal core peptide PDTRP and GM-CSF. Cancer Gene Ther. 2006;13:510–519. doi: 10.1038/sj.cgt.7700913. GMCSF adjuvanting of a tumor vaccine improved tumor challenge associated with an enhanced Th2 response. [DOI] [PubMed] [Google Scholar]
- 27.Yin J, Dai A, Laddy DJ, Yan J, Arango T, Khan AS, Lewis MG, Andersen H, Kutzler MA, Draghia-Akli R, et al. High dose of plasmid IL-15 inhibits immune responses in an influenza non-human primates immunogenicity model. Virology. 2009;393:49–55. doi: 10.1016/j.virol.2009.07.017. Dosing of plasmid encoded moleular adjuvants is crucial to enhance DNA vaccine immunogenicity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiang Z, Ertl HC. Manipulation of the immune response to a plasmid-encoded viral antigen by coinoculation with plasmids expressing cytokines. Immunity. 1995;2:129–135. doi: 10.1016/s1074-7613(95)80001-8. First study of GM-CSF as a DNA vaccine adjuvant. [DOI] [PubMed] [Google Scholar]
- 29.Kim JJ, Yang JS, VanCott TC, Lee DJ, Manson KH, Wyand MS, Boyer JD, Ugen KE, Weiner DB. Modulation of antigen-specific humoral responses in rhesus macaques by using cytokine cDNAs as DNA vaccine adjuvants. J Virol. 2000;74:3427–3429. doi: 10.1128/jvi.74.7.3427-3429.2000. Plasmid encoded IL-2 and IL-4 as adjuvants for HIV DNA vaccine in NHP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lai L, Kwa S, Kozlowski PA, Montefiori DC, Ferrari G, Johnson WE, Hirsch V, Villinger F, Chennareddi L, Earl PL, et al. Prevention of infection by a granulocyte-macrophage colony-stimulating factor co-expressing DNA/Modified Vaccinia Ankara Simian Immunodeficiency Virus Vaccine. J Infect Dis. 2011;204:164–173. doi: 10.1093/infdis/jir199. A SIV DNA prime with GM-CSF, MVA boost enhanced antibody avidity in NHP and protection from E660 challenge. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim JJ, Simbiri KA, Sin JI, Dang K, Oh J, Dentchev T, Lee D, Nottingham LK, Chalian AA, McCallus D, et al. Cytokine molecular adjuvants modulate immune responses induced by DNA vaccine constructs for HIV-1 and SIV. J Interferon Cytokine Res. 1999;19:77–84. doi: 10.1089/107999099314441. Co-administration of Th1 cytokines, Th2 cytokines or GMCSF can modulte DNA vaccine induced immunity. [DOI] [PubMed] [Google Scholar]
- 32.Chong SY, Egan MA, Kutzler MA, Megati S, Masood A, Roopchard V, Garcia-Hand D, Montefiori DC, Quiroz J, Rosati M, et al. Comparative ability of plasmid IL-12 and IL-15 to enhance cellular and humoral immune responses elicited by a SIVgag plasmid DNA vaccine and alter disease progression following SHIV(89.6P) challenge in rhesus macaques. Vaccine. 2007;25:4967–4982. doi: 10.1016/j.vaccine.2006.11.070. Co-immunization with IL-12 or IL-12 and IL-15 improved cellular and humoral immunity as well as challenge outcome. [DOI] [PubMed] [Google Scholar]
- 33.Li S, Qi X, Gao Y, Hao Y, Cui L, Ruan L, He W. IL-15 increases the frequency of effector memory CD8+ T cells in rhesus monkeys immunized with HIV vaccine. Cell Mol Immunol. 2010;7:491–494. doi: 10.1038/cmi.2010.44. Plasmid IL-15 delivered with a DNA prime recombinant vaccinia boost improved HIV-specific CD8+ memory responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramanathan MP, Kutzler MA, Kuo YC, Yan J, Liu H, Shah V, Bawa A, Selling B, Sardesai NY, Kim JJ, Weiner DB. Coimmunization with an optimized IL15 plasmid adjuvant enhances humoral immunity via stimulating B cells induced by genetically engineered DNA vaccines expressing consensus JEV and WNV E DIII. Vaccine. 2009;27:4370–4380. doi: 10.1016/j.vaccine.2009.01.137. Inclusion of an IL-15 molecular adjuvant stimulates B-cells and enhanced the humoral immunity induced by multiple DNA vaccines. [DOI] [PubMed] [Google Scholar]
- 35.Kraynyak KA, Kutzler MA, Cisper NJ, Khan AS, Draghia-Akli R, Sardesal NY, Lewis MG, Yan J, Weiner DB. Systemic immunization with CCL27/CTACK modulates immune responses at mucosal sites in mice and macaques. Vaccine. 2010;28:1942–1951. doi: 10.1016/j.vaccine.2009.10.095. First study illustrating the mucosal chemokine adjuvants can modulate mucosal vaccine immunity in NHP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36••.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Premsri N, Namwat C, de Souza M, Adams E, et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med. 2009;361:2209–2220. doi: 10.1056/NEJMoa0908492. A MVA prime rgp120 boost (Thai trial) showed 26.4% efficacy in the intention-to-treat analysis involving 16,402 subjects. The first demonstration of protective efficacy for a HIV vaccine in humans. [DOI] [PubMed] [Google Scholar]
- 37••.Buchbinder SP, Mehrotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, Gilbert PB, Lama JR, Marmor M, Del Rio C, et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet. 2008;372:1881–1893. doi: 10.1016/S0140-6736(08)61591-3. Ad5 HIV STEP trial failed to show protective responses and may have increased the risk of HIV-nfection in subjects with pre-existing Ad5 serology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Casimiro DR, Chen L, Fu TM, Evans RK, Caulfield MJ, Davies ME, Tang A, Chen M, Huang L, Harris V, et al. Comparative immunogenicity in rhesus monkeys of DNA plasmid, recombinant vaccinia virus, and replication-defective adenovirus vectors expressing a human immunodeficiency virus type 1 gag gene. J Virol. 2003;77:6305–6313. doi: 10.1128/JVI.77.11.6305-6313.2003. Ad5 or a DNA prime Ad5 boost induced the most robust effector T-cell responses in vacinated NHP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39•.Shiver JW, Fu TM, Chen L, Casimiro DR, Davies ME, Evans RK, Zhang ZQ, Simon AJ, Trigona WL, Dubey SA, et al. Replication-incompetent adenoviral vaccine vector elicits effective anti-immunodeficiency-virus immunity. Nature. 2002;415:331–335. doi: 10.1038/415331a. DNA prime Ad5 boost and Ad5 alone show enhanced immunogenicity and protection from SHIV challenge compared with MVA. [DOI] [PubMed] [Google Scholar]
- 40•.Letvin NL, Huang Y, Chakrabarti BK, Xu L, Seaman MS, Beaudry K, Korioth-Schmitz B, Yu F, Rohne D, Martin KL, et al. Heterologous envelope immunogens contribute to AIDS vaccine protection in rhesus monkeys. J Virol. 2004;78:7490–7497. doi: 10.1128/JVI.78.14.7490-7497.2004. A DNA prime Ad boost containing envelope immunogens can protect NHP from SHIV challenge. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41•.Shiver JW, Emini EA. Recent advances in the development of HIV-1 vaccines using replication-incompetent adenovirus vectors. Annu Rev Med. 2004;55:355–372. doi: 10.1146/annurev.med.55.091902.104344. Overview of comparative immunogenicity studies that demonstrate recombinant Ad5 vectors generate robust cellular immunity that may provide protection from HIV infection or improve viral outcome. [DOI] [PubMed] [Google Scholar]
- 42•.Letvin NL, Mascola JR, Sun Y, Gorgone DA, Buzby AP, Xu L, Yang ZY, Chakrabarti B, Rao SS, Schmitz JE, et al. Preserved CD4+ central memory T cells and survival in vaccinated SIV-challenged monkeys. Science. 2006;312:1530–1533. doi: 10.1126/science.1124226. Improved SIV challenge outcome following a DNA prime Ad boost SIV vaccine in NHP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Priddy FH, Brown D, Kublin J, Monahan K, Wright DP, Lalezari J, Santiago S, Marmor M, Lally M, Novak RM, et al. Safety and immunogenicity of a replication-incompetent adenovirus type 5 HIV-1 clade B gag/pol/nef vaccine in healthy adults. Clin Infect Dis. 2008;46:1769–1781. doi: 10.1086/587993. Phase I Merck HIV Ad5 trial demonstrating reduced efficacy in baseline Ad5 seropositive humans. [DOI] [PubMed] [Google Scholar]
- 44.Farina SF, Gao GP, Xiang ZQ, Rux JJ, Burnett RM, Alvira MR, Marsh J, Ertl HC, Wilson JM. Replication-defective vector based on a chimpanzee adenovirus. J Virol. 2001;75:11603–11613. doi: 10.1128/JVI.75.23.11603-11613.2001. Chimpanzee adenvorus serotypes can serve as effective vaccine vectors and have a lower natural serology in humans than human Ad serotypes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vogels R, Zuijdgeest D, van Rijnsoever R, Hartkoorn E, Damen I, de Bethune MP, Kostense S, Penders G, Helmus N, Koudstaal W, et al. Replication-deficient human adenovirus type 35 vectors for gene transfer and vaccination: efficient human cell infection and bypass of preexisting adenovirus immunity. J Virol. 2003;77:8263–8271. doi: 10.1128/JVI.77.15.8263-8271.2003. Demonstration that alternative rare serotype Ad can also serve as effective viral vectors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xiang Z, Li Y, Cun A, Yang W, Ellenberg S, Switzer WM, Kalish ML, Ertl HC. Chimpanzee adenovirus antibodies in humans, sub-Saharan Africa. Emerg Infect Dis. 2006;12:1596–1599. doi: 10.3201/eid1210.060078. Humans have a low natural seropositivieity to chimpanzee Ad worldwide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu J, O’Brien KL, Lynch DM, Simmons NL, La Porte A, Riggs AM, Abbink P, Coffey RT, Grandpre LE, Seaman MS, et al. Immune control of an SIV challenge by a T-cell-based vaccine in rhesus monkeys. Nature. 2009;457:87–91. doi: 10.1038/nature07469. A heterologous rAd26 prime/rAd5 boost vaccine regimen augmented cellular immune responses compared with the homologous rAd5 regimen and lead to a 1.5 log reduction in viral load following SIVmac251 challenge. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Santra S, Sun Y, Korioth-Schmitz B, Fitzgerald J, Charbonneau C, Santos G, Seaman MS, Ratcliffe SJ, Montefiori DC, Nabel GJ, et al. Heterologous prime/boost immunizations of rhesus monkeys using chimpanzee adenovirus vectors. Vaccine. 2009;27:5837–5845. doi: 10.1016/j.vaccine.2009.07.050. Immunogenicity of chimpanzee derived Ad vectors in NHP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hutnick NA, Carnathan D, Demers K, Makedonas G, Ertl HC, Betts MR. Adenovirus-specific human T cells are pervasive, polyfunctional, and cross-reactive. Vaccine. 2010;28:1932–1941. doi: 10.1016/j.vaccine.2009.10.091. Adenovirus specific T-cells are common in humans and recognize diverse serotypes regardless of serology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Amara RR, Villinger F, Altman JD, Lydy SL, O’Neil SP, Staprans SI, Montefiori DC, Xu Y, Herndon JG, Wyatt LS, et al. Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA/MVA vaccine. Science. 2001;292:69–74. doi: 10.1126/science.1058915. DNA-prime MVA-boost HIV vaccine strategy can control mucosal SHIV challenge. [DOI] [PubMed] [Google Scholar]
- 51.Vaine M, Wang S, Hackett A, Arthos J, Lu S. Antibody responses elicited through homologous or heterologous prime-boost DNA and protein vaccinations differ in functional activity and avidity. Vaccine. 2010;28:2999–3007. doi: 10.1016/j.vaccine.2010.02.006. Antibody responses are improved with a DNA prime protein boost compared with either stategy alone. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52•.Pal R, Kalyanaraman VS, Nair BC, Whitney S, Keen T, Hocker L, Hudacik L, Rose N, Mboudjeka I, Shen S, et al. Immunization of rhesus macaques with a polyvalent DNA prime/protein boost human immunodeficiency virus type 1 vaccine elicits protective antibody response against simian human immunodeficiency virus of R5 phenotype. Virology. 2006;348:341–353. doi: 10.1016/j.virol.2005.12.029. Broad envelope antibody responses following amultivalent DNA prime, recombinant R5 envelope boost. [DOI] [PubMed] [Google Scholar]
- 53•.Wang S, Kennedy JS, West K, Montefiori DC, Coley S, Lawrence J, Shen S, Green S, Rothman AL, Ennis FA, et al. Cross-subtype antibody and cellular immune responses induced by a polyvalent DNA prime-protein boost HIV-1 vaccine in healthy human volunteers. Vaccine. 2008;26:3947–3957. doi: 10.1016/j.vaccine.2007.12.060. Broad antibody responses induced by a DNA prime recombinant protein boost HIV vaccine in humans. [DOI] [PMC free article] [PubMed] [Google Scholar]