Abstract
OBJECTIVE
To compare neonatal neurologic complication rates of cesarean deliveries, forceps-assisted vaginal deliveries, and vacuum-assisted vaginal deliveries.
METHODS
Data on singleton live births at 34 weeks or greater gestation born to nulliparous women from 1995 to 2003 in New York City were linked to hospital discharge data. Any diagnosis of neonatal subdural hemorrhage, intraventricular hemorrhage, seizures, scalp laceration or cephalohematoma, fracture, facial nerve palsy, brachial plexus injury, or 5-minute Apgar score of less than 7 was considered significant. Multivariable logistic regression was used to estimate associations between delivery mode and these neonatal morbidities.
RESULTS
Forceps-assisted vaginal deliveries were associated with significantly fewer seizures and 5-minute Apgar scores less than 7 compared with vacuum-assisted vaginal deliveries and cesarean deliveries. Cesarean deliveries were linked to less subdural hemorrhages compared with forceps-assisted vaginal deliveries or vacuum-assisted vaginal deliveries. When seizure, intraventricular hemorrhage, and subdural hemorrhage were examined collectively to best predict neurologic outcome, forceps-assisted vaginal deliveries had an overall reduced risk compared with both vacuum-assisted vaginal deliveries (odds ratio [OR] 0.60, 95% confidence interval [CI] 0.40–0.90) and cesarean deliveries (OR 0.68, 95% CI 0.48–0.97). The number needed to treat to prevent one case of severe neurologic morbidity is 509 for forceps-assisted vaginal deliveries compared with vacuum-assisted vaginal deliveries and 559 for forceps-assisted vaginal deliveries compared with cesarean deliveries.
CONCLUSION
Compared with vacuum-assisted vaginal delivery or cesarean delivery, a forceps-assisted vaginal delivery is associated with a reduced risk of adverse neonatal neurologic outcomes.
The operative vaginal delivery rate in the United States has decreased from 9% in 1990 to 4.8% in 2005,1 largely as a result of a decrease in forceps-assisted vaginal delivery. In 1990, 1 in 20 neonates was delivered by forceps-assisted vaginal delivery compared with fewer than 1 in 100 in 2007.1 This change in operative delivery practice is coupled with a rise in the cesarean delivery rate from 21% of all live births in 1996 to 32% in 2007.2
When delivery must be expedited, the goal of intervention is often to avoid long-term neonatal neurologic complications, but the increasing perception that cesarean delivery is safer for the neonate has not been supported by well-designed studies.3 Clinicians may associate cesarean delivery with decreased risk of litigation compared with operative vaginal deliveries.4 When operative vaginal delivery is pursued, physicians increasingly select vacuum-assisted vaginal delivery instead of forceps-assisted vaginal delivery. This trend also is not based on evidence that vacuum-assisted vaginal delivery is safer for the neonate. In one of the few studies to compare neonatal outcomes in vacuum-assisted vaginal delivery, forceps-assisted vaginal delivery, and cesarean delivery, no significant difference was found between cesarean delivery during labor, forceps-assisted vaginal delivery, and vacuum-assisted vaginal delivery with regard to the rate of neonatal intraventricular hemorrhage or subdural or subarachnoid hemorrhage. Cesarean delivery during labor was associated with higher rates of neonatal convulsions compared with operative vaginal delivery but there was no significant difference between forceps-assisted vaginal delivery and vacuum-assisted vaginal delivery.5 Intraventricular hemorrhage, seizures, and subdural hemorrhage are the morbidities most predictive of future neurodevelopmental deficits because they often lead to cognitive impairments.6–8
To address gaps in the current literature, we examined the association between route of delivery and frequency of the neonatal complications linked to long-term neurodevelopmental disability in nulliparous women using New York City birth certificate and hospitalization data from 1995–2003. We were most interested in comparing outcomes by mode of delivery (forceps-assisted vaginal delivery, vacuum-assisted vaginal delivery, and cesarean delivery) when a normal spontaneous vaginal delivery could not be achieved.
MATERIALS AND METHODS
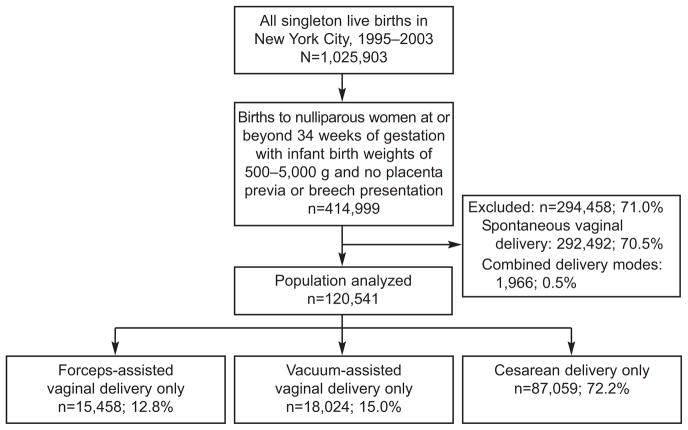
Data on singleton births from 1995–2003 (n=1,025,903) were obtained from a data set linking birth certificate data from the New York City Department of Health and Mental Hygiene to hospital discharge data from the Statewide Planning and Research Cooperative System. The Statewide Planning and Research Cooperative System data include both the mother’s and neonate’s records at delivery. Our study population was limited to nulliparous women delivering singleton neonates at 34 weeks of gestation or greater weighing between 500 and 5,000 g in which a single mode of delivery was identified. Women with placenta previa, breech fetuses, and birth weight greater than 5,000 g were excluded in an attempt to limit our study population to women who labored, resulting in 414,999 total deliveries. There were 292,492 exclusive normal spontaneous vaginal deliveries leaving 122,507 operative deliveries for analysis. Operative delivery mode was determined using combined data from the birth certificate and hospital discharge record. Operative delivery mode was categorized exclusively as vacuum-assisted vaginal delivery, forceps-assisted vaginal delivery, or cesarean delivery as noted in either the birth record or the discharge records. Combining the two databases significantly improves the likelihood of true-positives with regard to intrapartum procedures.9 Deliveries in which forceps and vacuum were used together or where either or both operative delivery modes were combined with a cesarean delivery were excluded from the main analysis but analyzed as part of a subanalysis as the occurrence was rare (less than 0.5%, n=1,966) (Fig. 1).
Fig. 1.
Study population.
Werner. Delivery Mode and Neonatal Outcome. Obstet Gynecol 2011.
Neonatal morbidity, including subdural or cerebral hemorrhage, scalp injury (including cephalohematoma), skeletal fracture, facial nerve palsy, and injury to the brachial plexus, was ascertained using International Classification of Diseases, 9th Revision, Clinical Modification codes (listed in Table 1) from the child’s hospitalization record. Neonatal seizure was defined by the presence of this complication in either the Statewide Planning and Research Cooperative System or the birth certificate data because seizure is the only neonatal complication of interest identified on the birth certificate. A 5-minute Apgar score less than 7 was ascertained using birth certificate data because information on Apgar score is not included in hospitalization data. We also created a composite variable that included the neurologic complications most predictive of long-term neurodevelopmental outcome (seizures, intraventricular hemorrhage, or sub-dural hemorrhage). Multiple complications in the same neonate (ie, seizure and intraventricular hemorrhage) were not considered separately from having only one of the complications of interest.
Table 1.
Discharge Diagnoses Used to Identify Neonatal Complications
| Neonatal Complication | ICD-9-CM Code(s) |
|---|---|
| Cephalohematoma or scalp laceration | 767.1x |
| Fracture | 767.2, 767.3 |
| Facial nerve palsy | 767.5 |
| Brachial plexus injury | 767.6 |
| Intraventricular hemorrhage | 772.1x |
| Subdural hemorrhage | 767.0 |
| Seizures | 779.0 |
| Forceps-assisted vaginal delivery | 72.0, 72.4, 72.51, 72.53, 72.6 |
| Vacuum-assisted vaginal delivery | 72.7 |
| Cesarean delivery | 74.0, 74.1, 74.2, 74.4, 74.99, 669.7x |
ICD-9, International Classification of Diseases, 9th Revision, Clinical Modification.
Maternal demographic and pregnancy characteristics were obtained from birth records and the Statewide Planning and Research Cooperative System database and were examined as covariables and potential confounders based on previous literature. Maternal demographic characteristics derived from birth certificates included age (younger than 20, 20–35, 35 years or older), race or ethnicity, level of education (high school or less, more than high school), insurance status, and prepregnancy weight. Prepregnancy weight was used as a surrogate for body mass index because mother’s height was not available.10–12 We used categorical variables for maternal age because advanced maternal age and teenage pregnancy are associated with increased risk for some complications. Presence of maternal diabetes and gestational diabetes were determined by a previously described algorithm that used information from both the hospital discharge and birth data.13 We combined diabetes and gestational diabetes because both are associated with macrosomia and birth injuries.14
Birth outcomes used as covariables included gestational age of delivery based on the clinical estimate reported on the birth certificate and whether the child was born at less than the tenth percentile of birth weight for gestational age based on gender-specific U.S. standard birth weights (small for gestational age).15 Because it is difficult to predict which neonates will be small for gestational age and there is no variable for intrauterine growth restriction in the data set, we controlled for small for gestational age to adjust for confounding caused by potential intrauterine growth restriction. We also performed a subanalysis excluding all neonates weighing less than 1,500 g (0.23% of the population).
We assessed bivariable associations between delivery mode and neonatal outcomes using the χ2 statistic. Logistic regression was used to determine the odds of neonatal neurologic morbidity for forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery, forceps-assisted vaginal delivery compared with cesarean delivery, and vacuum-assisted vaginal delivery compared with cesarean delivery adjusting for maternal characteristics, pregnancy characteristics, and birth outcomes. We assessed confounding for variables that were both a risk factor for the outcome and associated with the exposures of interest. Covariables were considered for inclusion in the multivariable model if the bivariable χ2 P values were<.05. All potential confounders were found to be significant based on this criterion and thus included. Analyses were conducted using SAS 9.2. This study was approved by the Yale University institutional review board.
RESULTS
Of the 413,033 nulliparous singleton births with a solitary mode of delivery, 292,492 (70.8%) were un-instrumented vaginal deliveries, 87,059 (21.1%) were cesarean delivery, 15,458 were forceps-assisted vaginal delivery (3.7%), and 18,024 (4.4%) were vacuum-assisted vaginal delivery. Baseline characteristics for those delivered by forceps-assisted vaginal delivery, vacuum-assisted vaginal delivery, and cesarean delivery are presented in Table 2. All maternal and pregnancy characteristics differed between comparison groups (P<.01) except for the frequency of small-for-gestational-age neonates in the forceps compared with vacuum groups (P=.41). In particular, obese women and African American women were more likely to have cesarean delivery than forceps-assisted vaginal delivery or vaginal-assisted vaginal delivery.
Table 2.
Frequency of Maternal and Neonatal Characteristics by Mode of Delivery for Singleton Live Births to Nulliparous Women, New York City, 1995–2003 (Entire Study Population)
| Forceps-Assisted Vaginal Delivery Only (n=15,458) | Vacuum-Assisted Vaginal Delivery Only (n=18,024) | Cesarean Delivery Only (n=87,059) | |
|---|---|---|---|
| Maternal age (y) | |||
| Younger than 20 | 8.6 | 9.7 | 8.4 |
| 20–35 | 73.5 | 76.7 | 71.5 |
| 35 or older | 18.0 | 13.6 | 20.1 |
| Mother’s race or ethnicity | |||
| White, non-Hispanic | 41.8 | 33.6 | 30.4 |
| African American, non-Hispanic | 10.8 | 14.9 | 26.5 |
| Hispanic | 27.8 | 28.2 | 32.0 |
| Asian or Pacific Islander | 18.5 | 22.5 | 10.6 |
| Other | 1.1 | 0.8 | 0.6 |
| Maternal education | |||
| High school or less | 43.5 | 49.4 | 46.2 |
| More than high school | 56.5 | 50.6 | 53.8 |
| Primary payer | |||
| Medicaid | 41.4 | 45.2 | 42.6 |
| Health maintenance organization | 13.6 | 15.3 | 15.6 |
| Third party | 40.0 | 36.1 | 38.4 |
| Self-pay | 5.0 | 3.3 | 3.4 |
| Prepregnancy weight (lb) | |||
| 99 or less | 4.1 | 5.1 | 2.8 |
| 100–149 | 77.2 | 75.6 | 61.7 |
| 150–199 | 22.7 | 17.1 | 27.5 |
| 200 or more | 2.0 | 2.2 | 8.0 |
| Diabetes* | 5.5 | 4.8 | 7.8 |
| Small for gestational age† | 14.0 | 13.7 | 13.0 |
| Gestational age at delivery (wk) | |||
| 34 to less than 37 | 3.8 | 3.7 | 5.1 |
| 37 to less than 40 | 41.5 | 43.6 | 39.1 |
| At least 40 | 54.7 | 52.7 | 55.8 |
Data are %.
Includes pregestational and gestational diabetes.
P values were calculated for forceps-assisted vaginal delivery and vacuum-assisted vaginal delivery compared with cesarean delivery and for forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery using the χ2 statistic. All P values were statistically significant at a P value <.01, except for the frequency of small-for-gestational-age neonates in the forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery groups (P=.41). In multivariable analysis, all characteristics listed in this table were adjusted, except small for gestational age in the forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery analysis.
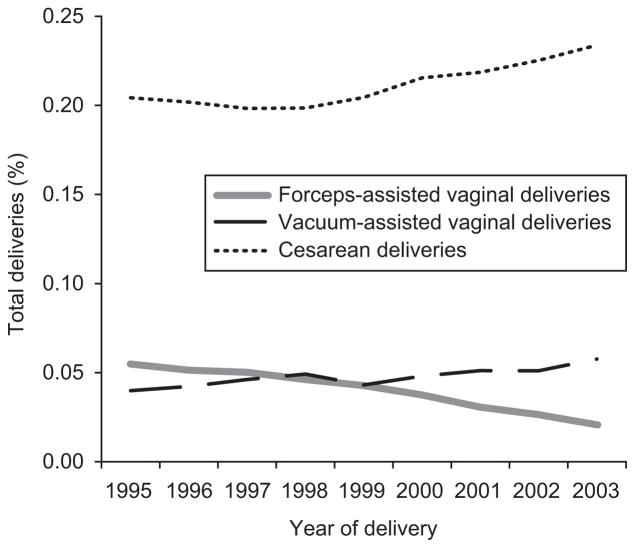
As occurred nationally,1 forceps-assisted vaginal delivery in New York City declined during the study period and cesarean delivery increased (Fig. 2). Vacuum-assisted vaginal delivery also increased over the course of the study, surpassing forceps-assisted vaginal delivery in year 2000. The incidence of forceps-assisted vaginal delivery, vacuum-assisted vaginal delivery, and cesarean delivery was 5.6%, 4%, and 20.4%, respectively, in 1995 and 2.1%, 5.8%, and 23.4%, respectively, in 2003.
Fig. 2.
Mode of delivery trends in nulliparous women in New York City, 1995–2003.
Werner. Delivery Mode and Neonatal Outcome. Obstet Gynecol 2011.
Table 3 presents the incidence of neonatal complications associated with forceps-assisted vaginal delivery, vacuum-assisted vaginal delivery, and cesarean delivery. Neonates born by cesarean delivery had a higher incidence of seizure and 5-minute Apgar less than 7 compared with forceps-assisted vaginal delivery and vacuum-assisted vaginal delivery. Cesarean delivery was also associated with a higher incidence of intraventricular hemorrhage, although the difference was not statistically significant. Neonates delivered by either operative vaginal delivery modality had a higher incidence of subdural hemorrhage compared with those delivered by cesarean (0.19% for vacuum-assisted vaginal delivery, 0.14% for forceps-assisted vaginal delivery, and 0.09% for cesarean delivery). Children delivered by vacuum-assisted vaginal delivery were more likely to have cephalohematomas, scalp lacerations, and fractures compared with those delivered by forceps-assisted vaginal delivery or cesarean delivery. Neonates delivered by forceps-assisted vaginal delivery had a higher incidence of nerve injury (facial and brachial plexus) compared with all other delivery modes.
Table 3.
Frequency of Neonatal Outcomes by Mode of Operative Delivery for Singleton Live Births to Nulliparous Women, New York City, 1995–2003
| Forceps (n=15,458) | Vacuum (n=18,024) | Forceps-Assisted Vaginal Delivery Compared With Vacuum-Assisted Vaginal Delivery (P) | Cesarean Delivery (n=87,059) | Forceps-Assisted Vaginal Delivery Compared With Cesarean Delivery (P) | Vacuum-Assisted Vaginal Delivery Compared With Cesarean Delivery (P) | |
|---|---|---|---|---|---|---|
| Cephalohematoma or scalp laceration | 12 (0.08) | 48 (0.27) | <.01 | 62 (0.07) | .78 | <.01 |
| Skeletal fracture | 118 (0.76) | 151 (0.84) | .45 | 127 (0.15) | <.01 | <.01 |
| Facial nerve palsy | 87 (0.56) | 9 (0.05) | <.01 | 19 (0.02) | <.01 | .04 |
| Brachial plexus injury | 87 (0.56) | 78 (0.43) | .09 | 11 (0.01) | <.01 | <.01 |
| Intraventricular hemorrhage | 8 (0.05) | 12 (.07) | .58 | 72 (0.08) | .20 | .49 |
| Subdural hemorrhage | 22 (0.14) | 35 (0.19) | .25 | 75 (0.09) | .04 | <.01 |
| Seizures | 19 (0.12) | 52 (0.29) | <.01 | 280 (0.32) | <.01 | .47 |
| 5-min Apgar score less than 7 | 66 (0.43) | 137 (0.76) | <.01 | 857 (0.98) | <.01 | .01 |
| Neurologic complication* | 40 (0.26) | 82 (0.45) | <.01 | 381 (0.44) | <.01 | .75 |
Data are n (%) unless otherwise specified.
Includes seizure, intraventricular hemorrhage, and subdural hemorrhage.
Table 4 presents the adjusted odds ratios (ORs) for neonates delivered by forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery, forceps-assisted vaginal delivery compared with cesarean delivery, and vacuum-assisted vaginal delivery compared with cesarean delivery adjusting for maternal age, race, education, insurance status, prepregnancy weight, diabetes, small for gestational age, and gestational age at delivery. Forceps-assisted vaginal delivery was associated with fewer composite neurologic complications than either vacuum-assisted vaginal delivery or cesarean delivery (adjusted OR 0.60, 95% confidence interval [CI] 0.4–0.9 for forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery and adjusted OR 0.68 95% CI 0.48–0.97 for forceps-assisted vaginal delivery compared with cesarean delivery). Overall, given the relatively low frequency of severe neurologic complications, 509 forceps-assisted vaginal deliveries compared with vacuum-assisted vaginal deliveries and 559 forceps-assisted vaginal deliveries compared with cesarean deliveries must be performed to prevent one case of severe morbidity. When Apgar score less than 7 at 5 minutes was added to the composite neurologic outcome, forceps-assisted vaginal delivery continued to be protective compared with vacuum-assisted vaginal delivery and cesarean delivery with no change in the adjusted OR for forceps-assisted vaginal delivery compared with vacuum-assisted vaginal delivery and an adjusted OR of 0.59 (95% CI 0.43–0.82) for forceps-assisted vaginal delivery compared with cesarean delivery.
Table 4.
Adjusted Odds Ratios for Adverse Neonatal Outcomes by Mode of Delivery*
| Forceps-Assisted Vaginal Delivery Compared With Vacuum-Assisted Vaginal Delivery | Forceps-Assisted Vaginal Delivery Compared With Cesarean Delivery | Vacuum-Assisted Vaginal Delivery Compared With Cesarean Delivery | |
|---|---|---|---|
| Cephalohematoma or scalp laceration | 0.33 (0.17–0.62) | 1.16 (0.62–2.17) | 3.54 (2.40–5.23) |
| Fracture | 0.93 (0.72–1.20) | 5.93 (4.51–7.80) | 6.55 (5.06–8.49) |
| Facial nerve palsy | 16.52 (7.19–37.93) | 27.95 (16.57–47.16) | 1.78 (0.69–4.57) |
| Brachial plexus injury | 1.20 (0.86–1.68) | 50.98 (25.13–103.44) | 49.92 (24.60–101.28) |
| Intraventricular hemorrhage | 0.93 (0.35–2.45) | 0.78 (0.35–1.71) | 0.86 (0.44–1.71) |
| Subdural hemorrhage | 0.78 (0.44–1.36) | 2.17 (1.30–3.63) | 2.94 (1.90–4.53) |
| Neonatal seizures | 0.45 (0.26–0.78) | 0.45 (0.26–0.78) | 0.93 (0.69–1.27) |
| 5-min Apgar score less than 7 | 0.61 (0.45–0.83) | 0.52 (0.40–0.68) | 0.84 (0.67–1.02) |
| Neurologic complication† | 0.60 (0.40–0.90) | 0.68 (0.48–0.97) | 1.17 (0.91–1.52) |
Data are odds ratio (95% confidence interval).
Adjusted for maternal age, race, education, insurance status, prepregnancy weight, diabetes, small for gestational age, and gestational age at birth.
Includes seizure, intraventricular hemorrhage, and subdural hemorrhage.
To evaluate the effect of women who failed operative deliveries and then required a cesarean delivery, we performed a secondary analysis in which these women were added into their respective operative delivery categories. The addition of these deliveries did not alter our findings. Additionally, when we performed a subanalysis excluding all neonates weighing less than 1,500 g, the results did not change.
DISCUSSION
Although all neonatal and maternal risks must be considered when delivery needs to be assisted or expedited, long-term cognitive outcome may be of paramount importance. We focused on neonatal seizures, intraventricular hemorrhage, and subdural hemorrhage, because evidence exists that these three complications may limit future neurologic potential. In a study of term neonates, almost 50% with neonatal seizures had a Mental Development Index less than 85 at 1 year of life.6 Intraventricular hemorrhage also forecasts poor neurologic outcomes. Studies have found moderate to severe disability in as many as 36% of term neonates with intraventricular hemorrhage.8 The longitudinal prognosis for term neonates with subdural hemorrhage has been inferred from studies on preterm neonates, but in one of the few studies to examine neurodevelopemental outcomes in term neonates, five of 15 neonates with subdural hemorrhage had moderate to severe deficits at 2–15 years of life.7
Although forceps-assisted vaginal delivery was associated with fewer total neurologic complications compared with vacuum-assisted vaginal delivery and cesarean delivery, subdural hemorrhage was significantly more frequent in both operative delivery cohorts than in the cesarean delivery group. Although this is a statistically significant independent finding, the increased incidence of seizure after cesarean delivery and vacuum-assisted vaginal delivery compared with forceps-assisted vaginal delivery may be more clinically relevant because seizures are more predictive of poor long-term outcome than subdural hemorrhage.
We did not include 5-minute Apgar score less than 7 in our composite variable because at the time of the study, 5-minute Apgar score less than 7 had not been shown to predict long-term neurologic outcome. However, Stuart et al recently demonstrated that 5-minute Apgar score less than 7 correlated with less academic achievement at 16 years of age.16 This suggests that 5-minute Apgar score less than 7 may be a proxy for even subtle hypoxia. Including 5-minute Apgar less than 7 in our composite variable strengthened the association between forceps-assisted vaginal delivery and fewer neurologic complications compared with cesarean delivery. Therefore, forceps-assisted vaginal delivery may be associated with even better odds of neurodevelopmental health than our current composite OR implies.
Given that the risk of moderate to severe disability is almost 50% with neonatal seizures, 36% with intraventricular hemorrhage, and 33% with subdural hemorrhage, the association between forceps-assisted vaginal delivery and a lower composite rate of these complications as well as fewer 5-minute Apgar scores less than 7 suggests that forceps-assisted vaginal delivery may be protective against hypoxia compared with vacuum-assisted vaginal delivery and cesarean delivery. A possible explanation for this may be that cesarean deliveries are performed preferentially when the clinical situation is more ominous such as when fetal heart tracings suggest fetal acidemia. Another possible explanation is that the cesarean delivery group includes neonates who required expedited delivery before the second stage of labor. Fetuses that exhibit distress earlier in labor may be at greater risk for neurologic compromise. Our study is limited by an inability to adjust for delivery indication and timing, which may affect both mode of delivery and fetal neurologic outcome. Despite this limitation, we chose to include the comparison between cesarean delivery and both operative vaginal delivery routes because the ORs highlighted a difference that deserves future prospective investigation. This limitation should have affected both the comparison of cesarean delivery to vacuum-assisted vaginal delivery and cesarean delivery to forceps-assisted vaginal delivery equally, yet the neurologic complication OR for cesarean delivery to vacuum-assisted vaginal delivery was insignificant, whereas the OR for cesarean delivery to forceps-assisted vaginal delivery was quite striking.
We focused on complications with cognitive long-term implications, but the other complications associated with mode of delivery should not be minimized. With regard to other significant neonatal outcomes, like other studies, we found that forceps-assisted vaginal delivery was linked to more facial nerve injuries than either vacuum-assisted vaginal delivery or cesarean delivery, vacuum-assisted vaginal delivery was associated with more cephalohematomas or scalp lacerations than forceps-assisted vaginal delivery or cesarean delivery, and both operative vaginal delivery techniques were associated with increased odds of brachial plexus injury and fracture compared with cesarean delivery.5 Maternal injury was not evaluated by this study but others have shown vaginal lacerations and third- or fourth-degree tears are more frequent with operative delivers than cesarean delivery.17–19 Thus, when spontaneous vaginal delivery is not possible, mode of delivery must be guided by patient–physician risk assessment because maternal and some neonatal risks are greatest with forceps-assisted vaginal delivery and other neonatal risks are greatest with vacuum-assisted vaginal delivery or cesarean delivery.
Our study has several strengths compared with prior studies. New York City provides an ideal study population as the cohort is large and diverse. Additionally, the timeframe of our study is more recent than many other frequently cited studies. We were also able to use a data set that matched all birth certificate data with hospital discharge data for both the mother and neonate from the Statewide Planning and Research Cooperative System database, significantly improving the quality of our data.9
There were several limitations to our study. Because this was a cross-sectional study, there was no randomization. Additionally, because the study was based on birth certificate and hospitalization data, misclassification of gestational age, mode of delivery, and neonatal outcome may have occurred in some cases. We used obstetric and clinical estimates of gestational age, because several studies have suggested that this provides a good approximation of dating.20 Although the accuracy of delivery mode and neonatal outcome improves by using the combined birth certificate and hospitalization data set, there is likely still underreporting of complications.21 The intention of our study was to compare delivery modes in laboring patients when spontaneous vaginal delivery was not possible, but as noted previously, despite limiting our study to nulliparous women without previa or breech presentation, some study patients likely had cesarean deliveries before labor.
Despite the aforementioned limitations, this is one of the largest studies to examine neonatal outcomes based on mode of delivery using current obstetric practices. In this cohort, total neurologic complications that frequently result in cognitive deficits were significantly lower in forceps-assisted vaginal delivery compared with both vacuum-assisted vaginal delivery and cesarean delivery. Future studies exploring neonatal outcomes based on mode of delivery are imperative, especially when comparing forceps-assisted vaginal delivery with vacuum-assisted vaginal delivery. Our findings also showed increasing use of vacuum-assisted vaginal delivery and declining forceps-assisted vaginal delivery rates. This trend will result in fewer opportunities to train residents and an obstetric workforce less experienced and able to perform forceps-assisted vaginal delivery.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Kirmeyer S, et al. Births: final data for 2007. Natl Vital Stat Rep. 2010;58:1–85. [PubMed] [Google Scholar]
- 2.Menacker F, Martin JA. Expanded health data from the new birth certificate, 2005. Natl Vital Stat Rep. 2008;58:1–24. [PubMed] [Google Scholar]
- 3.Yeomans ER. Operative vaginal delivery. Obstet Gynecol. 2010;115:645–53. doi: 10.1097/AOG.0b013e3181cfbefd. [DOI] [PubMed] [Google Scholar]
- 4.Localio AR, Lawthers AG, Bengtson JM, Hebert LE, Weaver SL, Brennan TA, et al. Relationship between malpractice claims and cesarean delivery. JAMA. 1993;269:366–73. [PubMed] [Google Scholar]
- 5.Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709–14. doi: 10.1056/NEJM199912023412301. [DOI] [PubMed] [Google Scholar]
- 6.Tekgul H, Gauvreau K, Soul J, Murphy L, Robertson R, Stewart J, et al. The current etiologic profile and neurodevelopmental outcome of seizures in term newborn infants. Pediatrics. 2006;117:1270–80. doi: 10.1542/peds.2005-1178. [DOI] [PubMed] [Google Scholar]
- 7.Vergani P, Strobelt N, Locatelli A, Paterlini G, Tagliabue P, Parravicini E, et al. Clinical significance of fetal intracranial hemorrhage. Am J Obstet Gynecol. 1996;175:536–43. doi: 10.1053/ob.1996.v175.a73598. [DOI] [PubMed] [Google Scholar]
- 8.Jocelyn LJ, Casiro OG. Neurodevelopmental outcome of term infants with intraventricular hemorrhage. Am J Dis Child. 1992;146:194–7. doi: 10.1001/archpedi.1992.02160140060021. [DOI] [PubMed] [Google Scholar]
- 9.Lydon-Rochelle MT, Holt VL, Cárdenas V, Nelson JC, Easterling TR, Gardella C, et al. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol. 2005;193:125–34. doi: 10.1016/j.ajog.2005.02.096. [DOI] [PubMed] [Google Scholar]
- 10.Lipkind HS, Duzyj C, Rosenberg TJ, Funai EF, Chavkin W, Chiasson MA. Disparities in cesarean delivery rates and associated adverse neonatal outcomes in New York City hospitals. Obstet Gynecol. 2009;113:1239–47. doi: 10.1097/AOG.0b013e3181a4c3e5. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA. Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol. 2003;102:1022–7. doi: 10.1016/j.obstetgynecol.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg TJ, Garbers S, Lipkind H, Chiasson MA. Maternal obesity and diabetes as risk factors for adverse pregnancy outcomes: differences among 4 racial/ethnic groups. Am J Public Health. 2005;95:1545–51. doi: 10.2105/AJPH.2005.065680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savitz DA, Janevic TM, Engel SM, Kaufman JS, Herring AH. Ethnicity and gestational diabetes in New York City, 1995–2003. BJOG. 2008;115:969–78. doi: 10.1111/j.1471-0528.2008.01763.x. [DOI] [PubMed] [Google Scholar]
- 14.Aljohani N, Rempel BM, Ludwig S, Morris M, Cheang M, Murray R, et al. Impact of diabetes on maternal-fetal outcomes in Manitoba: relationship with ethnic and environmental factors. Clin Invest Med. 2008;31:E338–45. doi: 10.25011/cim.v31i6.4919. [DOI] [PubMed] [Google Scholar]
- 15.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stuart A, Otterblad Olausson P, Källen K. Apgar scores at 5 minutes after birth in relation to school performance at 16 years of age. Obstet Gynecol. 2011;118:201–8. doi: 10.1097/AOG.0b013e31822200eb. [DOI] [PubMed] [Google Scholar]
- 17.Johnson JH, Figueroa R, Garry D, Elimian A, Maulik D. Immediate maternal and neonatal effects of forceps and vacuum-assisted deliveries. Obstet Gynecol. 2004;103:513–8. doi: 10.1097/01.AOG.0000114985.22844.6d. [DOI] [PubMed] [Google Scholar]
- 18.Bofill JA, Rust OA, Schorr SJ, Brown RC, Martin RW, Martin JN, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol. 1996;175:1325–30. doi: 10.1016/s0002-9378(96)70049-2. [DOI] [PubMed] [Google Scholar]
- 19.O’Mahony F, Hofmeyr GJ, Menon V. Choice of instruments for assisted vaginal delivery. The Cochrane Database of Systematic Reviews. 2010;(11):Art. No.: CD005455. doi: 10.1002/14651858.CD005455.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Ananth CV. Menstrual versus clinical estimate of gestational age dating in the United States: temporal trends and variability in indices of perinatal outcomes. Paediatr Perinat Epidemiol. 2007;21(suppl 2):22–30. doi: 10.1111/j.1365-3016.2007.00858.x. [DOI] [PubMed] [Google Scholar]
- 21.Vinikoor LC, Messer LC, Laraia BA, Kaufman JS. Reliability of variables on the North Carolina birth certificate: a comparison with directly queried values from a cohort study. Paediatr Perinat Epidemiol. 2010;24:102–12. doi: 10.1111/j.1365-3016.2009.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]