Abstract
Objective
To determine the impact of state Medicaid diabetes disease management programs on emergency admissions and inpatient costs.
Data
National InPatient Sample sponsored by the Agency for Healthcare Research and Quality Project for the years from 2000 to 2008 using 18 states.
Study Design
A difference-in-difference methodology compares costs and number of emergency admissions for Washington, Texas, and Georgia, which implemented disease management programs between 2000 and 2008, to states that did not undergo the transition to managed care (N = 103).
Data Extraction
Costs and emergency admissions were extracted for diabetic Medicaid enrollees diagnosed in the reform and non-reform states and collapsed into state and year cells.
Principal Findings
In the three treatment states, the implementation of disease management programs did not have statistically significant impacts on the outcome variables when compared to the control states.
Conclusions
States that implemented disease management programs did not achieve improvements in costs or the number of emergency of admissions; thus, these programs do not appear to be an effective way to reduce the burden of this chronic disease.
Keywords: Disease management, diabetes, Medicaid, cost analysis
Background
Introduction
Americans spend over 16.2 percent ($2.3 trillion) of U.S. gross domestic product (GDP) on health care, or approximately twice as much as most other developed nations. After many of the baby boomers retire by 2035, health care costs will approximately double to 31 percent of GDP (Congressional Budget Office 2007). Medicaid and Medicare spending is projected to grow from 4 percent of GDP, which is 26 percent of total spending on health care, to 9 percent of GDP, or 30 percent of total health care spending, by 2035 (Congressional Budget Office 2007). The Centers for Disease Control and Prevention estimates that 75 percent ($1.72 trillion) of health care spending goes to treating chronic conditions (Centers for Disease Control and Prevention 2009). In addition, 80 percent of this spending treats just 20 percent of the population (Stanton and Rutherford 2005). Only 15 medical conditions, most of which were chronic illnesses, accounted for roughly 50 percent of the increase in health care costs and spending between 1987 and 2000 (Thorpe, Florence, and Joski 2004).
As a result of increasing costs for those chronic illnesses, disease management programs have been put forward as a potential way to control costs and improve the quality of care of chronic diseases. Disease management programs are coordinated health care interventions for patients with chronic conditions in which self-care efforts have significant impacts on health outcomes (Bott et al. 2009). The most recent economic stimulus package included $2.2 billion for cost-effectiveness work in health care focusing on chronic disease prevention and disease management initiatives (Jutkowitz 2009). These programs look to address increasing health care costs for a number of diseases, including obesity, diabetes, heart disease, cancer, and smoking-related illnesses (Partnership to Fight Chronic Disease 2009). Their primary purpose is to improve health outcomes and reduce the costs that occur due to acute aggravations or worsening symptoms by aligning patient care with the evidence base (Bott et al. 2009). Most of these programs pay a fixed monthly capitation rate per enrollee to providers to treat patients using a set of services defined by Medicaid (Kaiser Commission on Medicaid and the Uninsured 2011a). This payment system encourages providers to treat health complications before they become more difficult and expensive to control (Kaiser Commission on Medicaid and the Uninsured 2011a). These programs typically use telephonic inventions by nurses to manage low-risk patients while provider-based interventions in physicians' offices are used to manage high-risk patients (Bott et al. 2009).
In the past decade, some states have implemented disease management programs for Medicaid patients to improve the quality of care, reduce emergency admissions, and to control the costs of treating clients with chronic diseases. Medicaid spending consumes about 8 percent of federal and 16 percent of state budgets (Kaiser Commission on Medicaid and the Uninsured 2011b). It also accounts for one-sixth of total health care spending in America (Kaiser Commission on Medicaid and the Uninsured 2011b). Currently, over 58 million Americans are enrolled in Medicaid, which represents 19 percent of the total population, and this number is expected to increase by 27.4 percent over the next 10 years with 16 of the 32 million Americans who will receive health insurance through the Affordable Care Act obtaining their coverage from state Medicaid programs (Henry J. Kaiser Family Foundation 2011). High medical costs relative to income level, such as those generated by chronic conditions, is one avenue through which many recipients become eligible for the Medicaid program. Disease management programs are a popular way that state Medicaid programs attempt to control costs for patients with chronic conditions. Consequently, the impact that these programs have on controlling costs and improving the quality of care is an important area of research, which has as of yet been underdeveloped.
Diabetes, in particular, consumes a significant amount of resources. About 1 in 10 of every health care dollar is used to treat diabetes and diabetes-related complications (Dall et al. 2008). In 2007, over $174 billion in health care expenditures were attributed to diabetes, which accounts for approximately 7.6 percent of overall health care spending in the United States (Dall et al. 2008). In addition, the prevalence of diabetes is expected to more than double from 5.6 to 12 percent of the U.S. population between 2005 and 2050 (Dall et al. 2008).
This article studies diabetic disease management programs in three states, Washington, Texas, and Georgia, and it uses difference-in-differences models and ordinary least squares regressions to determine the effects of these programs, which began in 2002, 2004, and 2005, respectively. Difference-in-differences models compare outcomes before and after the intervention in treated states against the same changes in states without reforms. The non-reform states act as a comparison sample establishing the time trend in outcomes that would have existed in the absence of intervention. After controlling for state and year effects with dummy variables, plus other covariates measuring year-specific state characteristics, there is no statistically significant impact of management programs on inpatient costs or emergency department admissions. Graphical analyses using time-series plots also illustrate that trends in inpatient costs and emergency department admissions in treatment states do not vary significantly after the intervention and tend to follow the same pattern of the control states. Consequently, the results indicate that these diabetic Medicaid disease management programs were ineffective at reducing inpatient costs and emergency admissions.
Literature Review
Disease management programs have been shown to better align care with evidence-based practices, but studies have not conclusively demonstrated improved outcomes such as a reduction in emergency room visits. By studying changes in health status metrics such as low-density lipoprotein (LDL) levels, which are a measure of cholesterol, and glycated hemoglobin (hemoglobin A1C) levels, which are a test of plasma glucose concentrations over time, numerous studies, including Lind and Kaplan (2007), McEwen et al. (2009), Morisky et al. (2009), and Rosenzweig et al. (2010), have found improvements in adherence to evidence-based practices. Considerably less work has focused on improved health outcomes such as a decreased number of emergency room visits.
In addition, the cost-effectiveness of disease management programs has not been well established. Lind and Kaplan (2007) examined a disease management program of Washington and found that diseases such as heart failure and asthma took 4 years after the program began before savings occurred, but diabetes and chronic obstructive pulmonary disease provided savings to the state after only 1 year of program operation (Lind and Kaplan 2007). Katz et al. (2009) also found that the Indiana Medicaid disease management programs were cost-effective by slowing the rate of increase in costs. Rosenzweig et al. (2010) showed that these programs assist in slowing the rate of increase or even decrease spending for chronic illnesses. In contrast, Esposito et al. (2008) and Bott et al. (2009) did not find substantial cost savings or reductions in the increase in the rate of growth of health care costs when disease management programs were implemented. Many of these studies lack sufficient controls in their models and only focus on the cost-effectiveness of managed care for an individual state. They also suffer from small datasets that provide only a few years of information before and after the implementation of the disease management program. Consequently, a more thorough examination of disease management programs is warranted.
The next section outlines the National InPatient Sample data from the Agency for Health Care Research and Quality that was used to address the research question and then explicate the difference-in-differences regression models employed. Subsequently, the results will be explained followed by a conclusion.
Data
Data
State Medicaid plans began to implement disease management programs over the last 15 years. Consequently, the analysis for this research needed to use a nationwide dataset over this period that was separated by state and year and included total costs, payer, and conditions for each patient. The National InPatient Sample (NIS) from the Health Care Cost and Utilization Project (HCUP) met these requirements. HCUP is a group of health care databases and software tools, which include patient-level and longitudinal hospital care data, sponsored by the Agency for Health Care Research and Quality (AHRQ). The NIS is a specific database within HCUP that contains information on patient-level hospital inpatient stays, including cost and payer. Other variables contained in this dataset are admission type (e.g., emergency, urgent, elective, newborn, and other), age, gender, primary payer, and total charges.
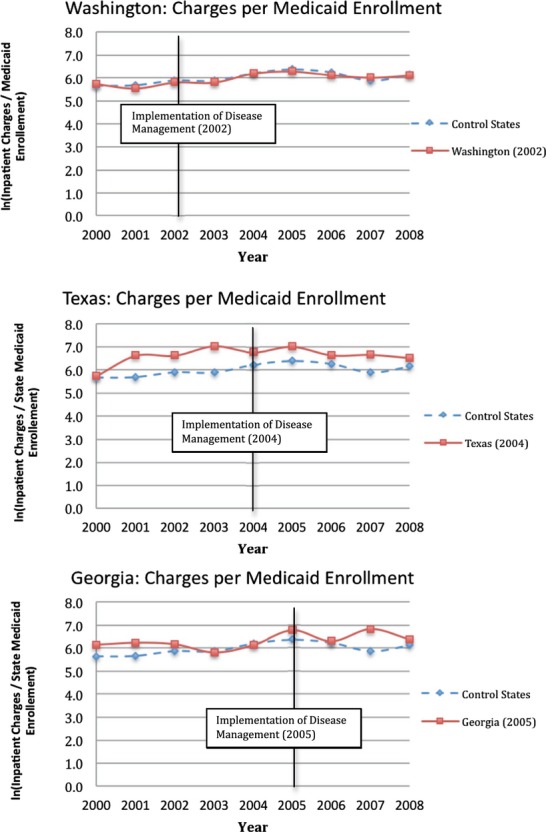
The Medicaid disease management programs chosen were mandatory enrollment for eligible patients or ones in which patients were automatically enrolled in the program and had to explicitly opt-out in order to ensure that patients whose care is paid by Medicaid are likely to be enrolled in the disease management program.1 In addition, states must have data for a few years before and after the implementation of the disease management program in the NIS, which led to Washington (2002),2 Texas (2004),3 and Georgia (2005)4 being selected. The years in parentheses are the years that the state began its disease management program. The criteria for selection into the control group were that there was no change in disease management status over this period and that they had the same trend in their state Medicaid enrollment population as the treatment states. To empirically determine which states had the same trend in their Medicaid enrollment population as the treatment states before their disease management programs began, a regression model by year (i) and state (j) of the form
 |
was used where ln_MEDENROLLij is the ln(Medicaid enrollment) by state and year, YEAR_TRENDi is a trend variable that equals 1 in 2000, 2 in 2001, and so on, HOSP_STj is a dummy variable for all treatment and potential control hospital states, STATE_TRENDik is an interaction variable between the YEAR_TREND and HOSP_ST variable only for the control hospital states, MED_AGEij is the median age of the state population by year, OBESE_RATEij is the obesity rate of the state population by year, MEDINCij is the median income of the state population by year, and STATE_POPij is the state population by year. Thus, control states that had a statistically insignificant θ1 coefficient for the STATE_TREND variable had the same trend in Medicaid enrollment as the treatment states before their disease management programs began. The control states include Hawaii, Kentucky, Massachusetts, Maryland, Maine, which is missing data from 2003 to 2006, North Carolina, Nebraska, which entered the dataset in 2001, South Carolina, and Tennessee. All of the states remained in the dataset unless otherwise noted. The change in diabetic inpatient costs and emergency admissions for Washington, Texas, and Georgia will be compared to the change in costs and emergency admissions for treating those chronic illnesses in the control group using a difference-in-differences model.
Limitations
This study is limited by the NIS data because the data only include treatment costs for diabetic patients whose care requires an overnight (inpatient) stay. However, inpatient care for treating diabetes-related complications accounts for greater than 60 percent of spending on diabetes, and people with diabetes have a high incidence of hospitalizations (Jiang et al. 2003). Thus, inpatient observations provide a good indication of the effectiveness of disease management programs for diabetes.
This study also could not differentiate between patients who were enrolled in disease management programs and those who were not. Therefore, the study cannot identify the impact of “treatment on the treated” but instead can only identify the reduced-form impact, which is the average impact on the entire system. However, in the states that were chosen, large percentages of Medicaid patients with diabetes were enrolled in the disease management programs so that the effects of cost savings, if present, could be observed. In addition, this study eliminated any states that had large fluctuations in the proportion of admissions to total Medicaid enrollment and tried to remove the sampling problem by using proportions in the outcome variables (e.g., total inpatient costs/total Medicaid enrollment).
Methods
This study uses difference-in-differences models to explore the effects of a disease management program in states that implemented these programs between 2000 and 2008. A difference-in-differences model simulates a random assignment experiment with treatment and comparison groups. In the ideal situation, the comparison group provides an estimate of the time-path of outcomes that would have occurred in the treatment group without the intervention. Thus, difference-in-differences models allow for analysis of results before and after the implementation of disease management program within the state and analysis of results between the treatment and comparison groups. The regressions were performed using ordinary least squares (OLS) allowing for within-state correlation in errors to control for repeated observations from the same state. To determine whether these programs were effective, two outcome variables were used: ln(total charges/state Medicaid enrollment), which was used to determine if disease management programs had any effect on costs, and emergency admissions/state Medicaid inpatient admissions, which was used to explore whether disease management programs had been successful in preventing acute aggravations. The models used to estimate the outcome variables by year (i) and state (j) is of the form
| (1) |
where Yij is the dependent or outcome variable, REFORMij = 1 if the state is a treatment state and has a disease management program that year, MED_AGEij is the median age of the state population by year, OBESE_RATEij is the obesity rate of the state population by year, ln_MEDINCij is the ln(median income of the state population by year), and MEDENROLLij is the state Medicaid enrollment by year. The variables γj and λi measure state and year effects, which are captured by a set of mutually exclusive dummy variables. State dummy variables are used to capture the differences between the states that are constant over time, and year dummy variables are used to capture the differences over time that are common to all of the states. The covariates MED_AGEij, OBESE_RATEij, ln_MEDINCij, γj, and λi were used to control for differences among states to isolate the effect of disease management programs on total costs per Medicaid enrollee and emergency admissions per total admissions. The variable MEDENROLLij is in parentheses because it was not used as a covariate in the total costs per Medicaid enrollee regression. MEDENROLLij was used in the model for the outcome variable emergency admissions/state Medicaid inpatient admissions in which the dependent variable did not have state Medicaid enrollment as a denominator. Consequently, the REFORMij variable should account for any changes between states that implemented disease management programs and those that did not.
Results
Summary Statistics
The difference-in-differences methodology isolates the effect of the disease management programs by comparing the time series in outcomes for these programs to the same values in states that did not undergo the transition to managed care. The unit of observation is a state/year value, and there are a total of 103 observations in each regression. Some states do not have data for all years, and these incomplete series include Maine, which is missing data from 2003 to 2006, and Nebraska, which entered the dataset in 2001. Every other state was in the dataset continuously from 2000 to 2008.
Table 1 shows summary statistics for each of the outcome variables. These summary statistics include both treatment and control states. All dollar values are converted into real 2008 dollars using the Consumer Price Index. The number of admissions reported only includes diabetic Medicaid inpatient admissions. The average proportion of emergency department admissions to total admissions was 0.37, or 37 percent of the Medicaid population with a standard deviation of 0.12. The average cost for diabetic-related inpatient stays (total charges/state Medicaid enrollment) accounted for approximately $430 per Medicaid enrollee, and the cost within one standard deviation was between $265 and $700. The total charges were divided by the state Medicaid enrollment to standardize this number across states.
Table 1.
Summary Statistics
| Outcome Variables | Summary Statistics | ||||
|---|---|---|---|---|---|
| Number of Observations | Mean | Standard Deviation | Minimum | Maximum | |
| Number of emergency admissions/total admissions | 103 | 0.3666 | 0.1167 | 0.0690 | 0.6197 |
| ln(inpatient charges/state Medicaid enrollment) | 103 | 6.0662 | 0.4850 | 4.7573 | 7.0198 |
Graphical Analysis
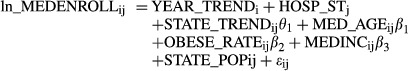
A time-series plot of outcomes for treatment and comparison states provides evidence of the likely impact of disease management programs on outcomes. In the first graph, the proportion of emergency Medicaid diabetic admissions compared to total Medicaid diabetic admissions is plotted for the treatment states from 2000 to 2008, and each plot contains this proportion for the control states over that same period of time (Figure 1). The trend in the treatment states follows closely the trend of the control states before and after the interventions, and consequently, there seems to be no improvement in diabetic care after a disease management program has been put into practice.
Figure 1.
Emergency Admissions per Total Admissions Note. These charts illustrate how emergency admissions per total admissions for both the treatment and control states change from 2000 to 2008.
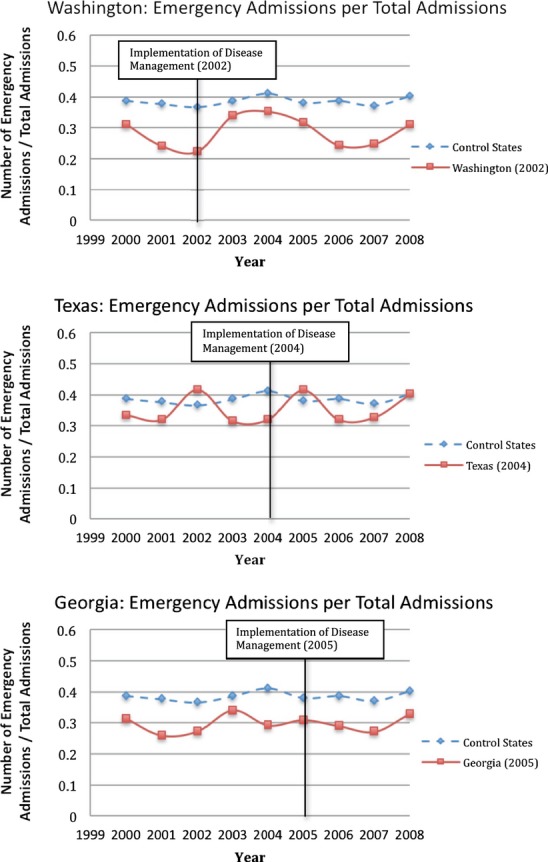
The second set of graphs illustrate that disease management programs have not had any discernible effects on costs (Figure 2). Costs in the control states rise steadily from 2000 to 2008. All of the treatment states follow this upward trend, and disease management programs do not appear to have any impact on inpatients costs. Thus, this suggests that disease management programs do not affect the costs of diabetic care in Medicaid. Disease management programs do not appear to change the costs that Medicaid must pay in the years after a program has been implemented. In general, this study finds that these specific disease management programs do not have any effect on the cost or emergency admission outcome variables defined here.
Figure 2.
Inpatient Charges per State Medicaid Enrollment Note. These charts illustrate how inpatient charges per state Medicaid enrollment for both the treatment and controls states change from 2000 to 2008.
OLS Regression Results
A difference-in-differences model estimated via ordinary least squares regressions was employed to produce estimates for the effects of disease management programs on the outcome variables. The graphical evidence presented above suggests that disease management programs do not have a noticeable effect on any of the outcome variables, and these results are borne out in the regression models as well. The Reform variable was used to determine the isolated effects of having a disease management program compared to the control states. The Reform variable was estimated for each outcome variable, and Table 2 shows these values with the clustered standard errors in the parentheses. In addition, the R2 values are given to show how well each model fits the data. Table 2 summarizes the major results all of the regressions performed in this study. If disease management programs were successful in affecting the outcome variables that were tested, then one would expect to see a negative value for the coefficient of the Reform variable, which would indicate that the implementation of a disease management decreases inpatient costs or the proportion of emergency inpatient admissions.
Table 2.
OLS Regression Estimates for Reform Variables for Outcomes
| Covariates | Outcomes | |
|---|---|---|
| Number of Emergency Admissions/Total Admissions | ln(Inpatient Charges/State Medicaid Enrollment) | |
| Reform | −0.0091 (0.0140) | 0.1647 (0.1007) |
| R2 | 0.8100 | 0.5006 |
This table provides the ordinary least squares regression coefficients for the Reform variables for each model. In addition, R2 values are reported for each regression. Clustered standard errors are in parentheses.
Ultimately, the Reform variable is not statistically significant in any of the models. The p-value for the Reform variable is never less than .13 for any of the outcome variables. These results suggest that disease management programs do not have a significant impact on inpatient costs or the proportion of emergency admissions to total admissions. The high R2 values suggest that the models fit the data well.
The difference-in-differences models using ordinary least squares regressions provide a statistical foundation for the trends that can be seen readily in the time-series plots above. The OLS regression results corroborate these visual results presented in the “Graphical Analysis” section. Consequently, disease management programs in the three treatment states do not have any effect on the outcome variables that were presented in this study.
Conclusion
In this article, the effectiveness of disease management programs was studied using individual inpatient observations from the National InPatient Sample from 2000 to 2008. Disease management programs have been proposed as a way to increase the quality of care of chronic conditions while simultaneously decreasing the costs of treating these illnesses; however, there has not been conclusive evidence in determining the impact on costs or health outcomes of these programs.
A difference-in-differences model was employed to isolate the effects of diabetic disease management programs in three states: Washington (2002), Texas (2004), and Georgia (2005). Ordinary least squares regressions using clustered standard errors to control for repeated observations from the same state were used to estimate the coefficients of the Reform variable. The regression models controlled for state and year effects with dummy variables as well as median state income, state obesity rate, and state Medicaid enrollment to isolate the effects of the disease management programs on the two outcome variables. These outcomes include emergency inpatient admissions/total inpatient admissions and ln(total charges/state Medicaid enrollment). Graphical analysis using a time-series plot of the change in the number of diabetic Medicaid emergency admissions and inpatient costs of care in the treatment states illustrate that the trends in the three treatment states are closely correlated with the trends in the control states. OLS regression analysis supports this claim because the Reform variable is not statistically significant for any of the outcomes. The results of this study suggest that these programs do not produce the desired outcomes of limiting inpatient costs and emergency admissions.
Previous studies have focused on the improvements made by individual state disease management programs, and they have often studied costs by looking at aggregate state data. This study has the advantage of using individual patient-level observations in a national dataset. A difference-in-differences model was then used to isolate the effects of implementing a disease management program over time by controlling for changes in health care inpatient costs and emergency admissions in states that did not implement a new Medicaid disease management program for diabetic patients between 2000 and 2008. In addition, trends in inpatient costs and emergency admissions could be observed before and after the implementation of the disease management programs in Washington, Texas, and Georgia. This study finds that the disease management programs enacted in Washington, Texas, and Georgia were not effective at controlling inpatient diabetic costs or reducing emergency department admissions.
Acknowledgments
Joint Acknowledgment/Disclosure Statement:
Disclaimers: None.
Footnotes
Although there is no master list of disease management programs, http://www.ncsl.org/issues-research/health/state-medicaid-disease-management-programs.aspx provided an initial guide. Additional information was obtained by reviewing each state's Medicaid website. Finally, academic papers that explained the disease management status of states and are cited in the References section of the paper were used.
The Washington disease management program began in 2002 for clients in its fee-for-service program (Lind and Kaplan 2007). Washington contracted its program to external vendors, who were to take on patients with asthma, heart failure, chronic obstructive pulmonary disease, and diabetes (Lind and Kaplan 2007). Patients were automatically enrolled in the program unless they opted out (Lind and Kaplan 2007). About 35 percent of the target population participated in the disease management program at any point in time (Lind and Kaplan 2007). The patients who were in the program received a phone call from a nurse who performed an initial health assessment that allowed the patient to be put into a high-risk, medium-risk, or low-risk group (Lind and Kaplan 2007). A reassessment of clients' health occurred every 6 months; thus, all data for the health assessments were self-reported (Lind and Kaplan 2007).
The Texas disease management program began in 2004 and included patients that were diagnosed with asthma, diabetes, congestive heart failure, coronary artery disease, and chronic obstructive pulmonary disease (Agency for Health Care Research and Quality 2008). The state decided to contract to an outside vendor to manage the program (Agency for Health Care Research and Quality 2008). The Texas program is an opt-out program in which eligible clients are automatically enrolled but can choose to opt-out of the program (Agency for Health Care Research and Quality 2008). The interventions conducted by the Texas disease management program included an initial health assessment, education materials, telephone calls by community-based nurses with a few visits to patients' homes, a 24-hour nurse call line, self-management guidelines for patients, and education for providers (Agency for Health Care Research and Quality 2008).
The Georgia disease management program, which began in 2005, is similar to the Texas program with interventions that include a 24-hour nurse call center, education materials, an initial health assessment, development of an action plan, and education for providers (Georgia Department of Community Health 2005). The Georgia program is managed by outside vendors as well (Georgia Department of Community Health 2005).
References
- Agency for Health care Research and Quality. Rockville, MD: Agency for Health Care Policy and Research; 2008. “Designing and Implementing Medicaid Disease and Care Management Programs: A User's Guide.”. AHRQ Publication No. 07(08)-0063. [Google Scholar]
- Bott DM, Kapp MC, Johnson LB, Magno LM. “Disease Management for Chronically Ill Beneficiaries in Traditional Medicine”. Health Affairs. 2009;28(1):86–98. doi: 10.1377/hlthaff.28.1.86. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2009. “The Power of Prevention, 2009” [accessed on February 24, 2011]. Available at http://www.cdc.gov/chronicdisease/pdf/2009-Power-of-Prevention.pdf.
- Congressional Budget Office. Washington, DC: US Government Printing Office; 2007. “The Long-Term Outlook for Health Care Spending.”. Publication No. 3085. [Google Scholar]
- Dall T, Mann SE, Zhang Y, Martin J, Chen Y, Hogan P. “Economic Costs of Diabetes in the U.S. in 2007”. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- Esposito D, Brown R, Chen A, Schore J, Shapiro R. “Impacts of a Disease Management Program for Dually Eligible Beneficiaries”. Health Care Financing Review. 2008;30(1):27–45. [PMC free article] [PubMed] [Google Scholar]
- Georgia Department of Community Health. 2005. “Disease Management Contracts Awarded to APS and United Health Care” [accessed on March 1, 2011]. Available at http://www.georgia.gov/vgn/images/portal/cit_1210/4/12/41422416DSM_Release_2005.pdf.
- Henry J. Kaiser Family Foundation. 2011. “Medicaid & CHIP” [accessed on February 14, 2011]. Available at http://www.statehealthfacts.org.
- Jiang HJ, Stryer D, Freidman B, Andrews R. “Multiple Hospitalizations for Patients with Diabetes”. Diabetes Care. 2003;26(5):1421–6. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- Jutkowitz E. “Stimulus Money and Health Care Research and Investment”. Health Policy Newsletter. 2009;22(2) Thomas Jefferson University [accessed on March 10, 2011]. Available at http://jdc.jefferson.edu/cgi/viewcontent.cgi?article=1633&context=hpn&sei-redir=1#search=%22$2.2+billion+cost+effectiveness+stimulus+health+care%22. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. 2011a. “Key Questions about Medicaid and Its Role in State/Federal Budgets and Health Reform” [accessed on February 24, 2011]. Available at http://www.kff.org/medicaid/upload/8139.pdf.
- Kaiser Commission on Medicaid and the Uninsured. 2011b. “Medicaid and Managed Care: Key Data, Trends, and Issues” [accessed on February 24, 2011]. Available at http://www.kff.org/medicaid/upload/8046.pdf.
- Katz BP, Holmes AM, Stump TE, Downs SM, Zillich AJ, Ackermann RT, Inui TS. “The Indiana Chronic Disease Management Program's Impact on Medicaid Claims: A Longitudinal, Statewide Evaluation”. American Journal of Respiratory and Critical Care Medicine. 2009;47(2):154–60. doi: 10.1097/MLR.0b013e3181844df7. [DOI] [PubMed] [Google Scholar]
- Lind A, Kaplan L. “An Evaluation of Washington's Medicaid Disease-Management Program”. Managed Care Interface. 2007;20(10):45–50. [PubMed] [Google Scholar]
- McEwen LN, Hsiao VC, Nota-Kirby EM, Kulpa GJ, Schmidt KG, Herman WH. “Effect of a Managed Care Disease Management Program on Diabetes Care”. The American Journal of Managed Care. 2009;15(9):575–80. [PMC free article] [PubMed] [Google Scholar]
- Morisky ED, Kominski GF, Afifi AA, Kotlerman JB. “The Effects of a Disease Management Program on Self-Reported Health Behaviors and Health Outcomes: Evidence from the “Florida: A Healthy State (FAHS)” Medicaid Program”. Health Education and Behavior. 2009;36(3):505–17. doi: 10.1177/1090198107311279. [DOI] [PubMed] [Google Scholar]
- Partnership to Fight Chronic Disease. 2009. “Inclusion of Prevention and Disease Management Funding a Major Step Forward” [accessed on March 10, 2011]. Available at http://www.fightchronicdisease.org/media/statements/pfcd/Stimuluspackage.cfm.
- Rosenzweig JL, Taitel MS, Norman GK, Moore TJ. “Diabetes Disease Management in Medicare Advantage Reduces Hospitalizations and Costs”. The American Journal of Managed Care. 2010;16(7):e157–62. [PubMed] [Google Scholar]
- Stanton MW, Rutherford MK. Rockville, MD: Agency for Healthcare Research and Quality; 2005. “The High Concentration of U.S. Health Care Expenditures”. Research in Action Issue 19 AHRQ Pub. No. 06-0060. [Google Scholar]
- Thorpe KE, Florence CS, Joski P. “Which Medical Conditions Account for the Rise in Health Care Spending?”. Health Affairs. 2004;W4:437–45. doi: 10.1377/hlthaff.w4.437. [DOI] [PubMed] [Google Scholar]


