Abstract
Outdoor recreation settings, such as swimming pools, provide a promising venue to assess UVR exposure and sun protection practices among individuals who are minimally clothed and exposed to potentially high levels of UVR. Most studies assessing sun exposure/protection practices rely on self-reported data, which are subject to bias. The aim of this study was to establish the feasibility of conducting a multimethod study to examine the validity of self-reported measures within a swimming pool setting. Data were collected from 27 lifeguards, children and parents in Hawaii. Each participant filled out a survey and a 4 day sun habits diary. On two occasions, researchers assessed observable sun protection behaviors (wearing hats, shirts, sunglasses), swabbed the skin to detect the presence of sunscreen, and subjects wore polysulphone dosimeters to measure UVR exposure. Overall, observed sun protection behaviors were more highly correlated with diary reports than with survey reports. While lifeguards and children reported spending comparable amounts of time in the sun, dosimeter measures showed that lifeguards received twice as much UVR exposure. This study demonstrated the feasibility of implementing a multimethod validity study within a broader population of swimming pools.
INTRODUCTION
Skin cancer, the most common form of cancer in the United States, is increasing (1,2). Most skin cancers can be prevented by reducing sun exposure—seeking shade, using sunscreen properly, and wearing protective hats and clothing (1).
Outdoor recreation settings such as swimming pools provide a unique environment in which to implement a skin cancer prevention intervention. It is a setting where children and adults are minimally clothed (3) and exposed to potentially high levels of UVR. The Pool Cool Diffusion Trial is a multicomponent education and environmental intervention aimed at improving sun protection practices and reducing UVR exposure through changes in behaviors and the environment (3). Evaluation of the behavioral impact of Pool Cool is based primarily on self-reported measures (i.e. surveys) completed by lifeguards and parents (4). Pool Cool is a nationally disseminated project that includes 400 pools, over 5000 lifeguards, and approximately 10 000 parent–child surveys per year. Given the logistics of collecting data from this many people, self-report is the most practical type of measure and the most commonly used (5). However, self-report is also prone to limitations due to systematic error introduced by problems with recall and reporting of “usual behavior,” and the potential for social desirability bias (5). One approach to circumvent these well recognized limitations would be to undertake a validation study with recognized objective measures of UVR exposure and sun protection practices within a randomized subset of the population.
Previous research examining the agreement between an objective measure of UVR exposure (polysulphone dosimeters— PSDs) and a 4-day daily diary revealed a fair correlation for mothers (r = 0.32) and children (r = 0.33) (6). Similarly, survey items pertaining to habitual or usual sun exposure of adolescent school children obtained fair agreement for “Time in the sun” (r = 0.35–0.38) and “Time spent outdoors” (r = 0.29–0.32) when compared with PSDs (7). Both studies assessed personal UVR exposure with polysulphone placed on the dorsum of the right hand.
Validation of self-reported sun protection practices is usually undertaken using direct visual observation (5). While this approach has provided moderate to substantial agreement (κ = 0.41–0.89) for adult populations of outdoor workers (8), postal workers (9) and beachgoers (10), there has been greater variability among school children with substantial agreement being obtained for headwear (κ = 0.70) and fair agreement for clothing worn on the upper (κ = 0.34) and lower (κ = 0.35) body (11). Objective assessments of sunscreen use have been problematic. The recent introduction of sunscreen swabbing provides a quick, cost-effective, noninvasive, approach to assess the presence of sunscreen on the skin (12,13). Reported sunscreen use and sunscreen swabbing has provided moderate to substantial levels of agreement (κ = 0.42–0.77) among beachgoers (10).
To our knowledge, no studies have been reported that incorporate objective measures of UVR exposure, sun protection and sunscreen use to validate similar self-report items. Therefore, the aim of this paper was to establish the feasibility of conducting a multimeasure study to examine the validity of self-reported measures within a swimming pool setting.
METHODS
Setting and sample
This pilot study was conducted at a local swimming pool in Honolulu, Hawaii (21°19′N). The pool was 50 m long, with the only available shade provided to lifeguards on the lifeguard stand, which was covered by an umbrella. This setting was chosen to maximize cooperation of the pool management and study participants, as the staff had been involved in sun safety intervention studies at the pool for several years (3). Participants were lifeguards at the pool, and parent–child pairs with a child who was 5–10 years of age.
Procedure
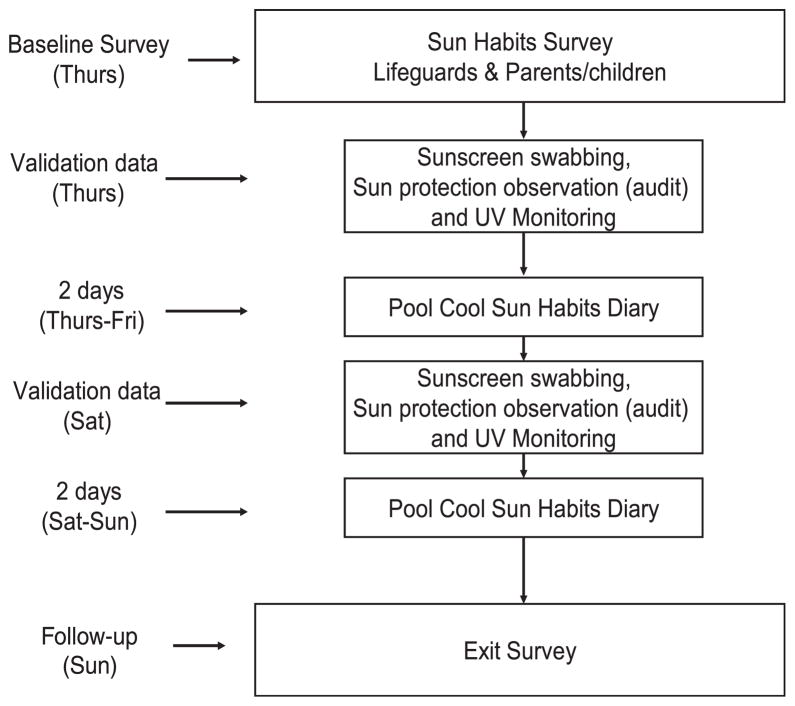
Data collection took place over 4 days (Thursday– Sunday) in September 2005 (Fig. 1). The project was publicized in advance at the swimming pool via signs, fliers and word-of-mouth with assistance from the pool manager. Participants were recruited prior to swimming lessons on Thursday morning. Potential participants received an explanation of what was required and signed a consent form (parents signing for their child with the child present and consenting verbally). Once consent was obtained, participants completed a sun habits survey (parents completed for themselves and their child). If a parent had more than one eligible child aged 5–10 years, the oldest child was enrolled. At this time, researchers conducted objective assessments of sunscreen use by swabbing the right forearm and thigh, and completed direct observation of sun protection practices (e.g. hats, protective clothing and sunglasses). Researchers also attached a PSD in a “bracelet” on the right wrist of participants with instructions to wear the dosimeter until 4 P.M. that day, then remove the dosimeter and place it in the light-proof envelope provided. Participants were then provided a sun habits diary with instructions to complete the diary each day for the next 4 days. Participants were also asked to return to the pool on Saturday to receive a second dosimeter (to be worn until 4 P.M. that day), a second sunscreen swab and repeated observation of sun safety habits.
Figure 1.
Data collection procedure for lifeguards, parents and children.
Throughout the 2 days that objective assessments of sun habits were completed, research staff monitored levels of ambient UVR by exposing two PSDs to sunlight hourly between 9 A.M. and 4 P.M. On the final day of data collection, participants returned to the pool after 4 P.M. to return their materials (exposed PSDs within the light-proof envelope and sun habits diary). Participants completed a brief exit survey to provide feedback regarding their experiences as a result of being involved in the study and were given a gift card for their participation. All procedures for this study were approved by the Institutional Review Board at the University of Hawaii.
Measures
Self-report measures
The sun habits survey assessed demographic characteristics including gender, age, ethnicity, education level, income, marital status and number of children. Usual sun protection practices were assessed by questions pertaining to the frequency of usually practicing five protective behaviors (wearing a shirt with sleeves, wearing a hat, wearing sunglasses, using sunscreen and seeking shade) on a 4-point ordinal scale ranging from 1 (rarely/never) to 4 (always). Sun exposure was determined by asking the average number of hours (1 or less, 2, 3, 4, 5 or 6) spent in the sun between 10 A.M. and 4 P.M. during the summer on weekdays and on weekends. Items on the survey have been used previously (3) and were found to have acceptable to good levels of internal consistency (14).
The sun habits diary was used to record sun exposure and sun protective behaviors over four consecutive days (two weekdays and two weekend days). This instrument has been described previously (15). Briefly, parents were asked to complete diaries for themselves and their child. To report sun exposure, participants were asked to record their primary activity for each hour of the day between 10 A.M. and 4 P.M. For each hour they were outside between 10 A.M. and 4 P.M., participants were asked to indicate the sun protection practices they used (wearing a shirt with sleeves, wearing a hat, wearing sunglasses, using sunscreen and seeking shade).
Objective assessments
Direct observation of sun protection practices was completed by research staff on one weekday and one weekend day using an adaptation of a protocol that was reported previously (10). A precoded form was used to record the observations. Information collected included date, time of assessment, and the type of clothing worn on the head, upper body, and lower body, type of footwear and use of sunglasses.
Sunscreen swabbing provides an objective measure of sunscreen use (12,13). We used BD Alcohol Swabs (70% isopropyl alcohol) (12). Participants’ skin was swabbed at two anatomic sites (right forearm and lower right thigh). Staff wore polyurethane gloves while swabbing subjects. The alcohol swab was wiped over a 2.5 cm × 4 cm area at the specific site. Swabs were then placed in a vial that contained 4 mL of 100% ethanol. Eluted washings (0.5 mL) from the vial where swabs were placed were transferred to a UV-rated cuvette (BrandTech UVB ultra micro; 70–880 μL). Absorbance was determined using a UV-Visible Spectrophotometer (Beckman DU-530) at 5 nm intervals over the wavelength 280–400 nm (the UV-A and UV-B spectrum), using a procedure described previously (10,12). Sunscreen absorbance readings obtained from swab samples were assessed at a wavelength of 320 nm as it has been recognized as a reliable indicator of sunscreen use (12,13). A cutoff at an absorbance (ΔA) of 0.147 was used to classify a swab as either sunscreen positive or negative. This absorbance reading has demonstrated a high level of sensitivity and specificity using the same protocol in an indoor setting (12) and was also found suitable in an outdoor setting (10).
Personal UVR exposure was assessed using PSDs worn on the right wrist. The dorsum of the wrist was considered an appropriate anatomic location because it has been reported to receive the highest levels of unprotected exposure (16) and this procedure has been adopted previously (6). The PSDs were laminated into a hospital identification bracelet that had an aperture of approximately 10 mm diameter to insure that the dosimeter was unimpeded from exposure to any available UVR.
Levels of ambient UVR were collected from 9 A.M. to 4 P.M. on each day when objective assessments were undertaken (Thursday and Saturday) at a shade-free site within the pool area. The data collection protocol consisted of two polysulphone badges being simultaneously exposed and replaced every hour, and then placed in a light-proof envelope to prevent further photo-degradation. This was done to insure that the dosimeters did not exceed a level of absorbance (ΔA) of 0.5 at which point the changes become nonlinear (17). The mean of the two readings was used in the analysis.
Polysulphone dosimeters (personal and ambient) were calibrated against simultaneous spectral measurements of solar UVR made with a double monochromator spectroradiometer at the Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) in Melbourne, as has been reported in previous studies (17–19).
Data preparation and statistical analysis
Participants’ diaries and surveys were inspected for incomplete entries. All analyses were conducted using SPSS, version 14 (20). First, descriptive statistics were examined for participants’ baseline surveys, diaries and researcher observation measures. Personal UVR exposure obtained from PSDs is reported as a standard erythemal dose (SED), which is equivalent to 100 J m−2 (21).
Diary reports of time spent outside (Thursday, Friday, Saturday, Sunday) were re-coded for comparison with survey measures of reported time spent outside on weekdays and weekends. Mean time spent outside on Thursday and Friday was coded as time spent outside on weekdays. Similarly, mean time spent outside on Saturday and Sunday was coded as time spent outside on the weekend.
Sun protection practices reported in the diary were calculated as a percentage of time that each behavior was performed while outside, for each of the sun protection practices (using sunscreen, wearing a hat, seeking shade, covering up and wearing sunglasses). To compare diary records with survey data, the proportion of time spent using various sun protection practices over the 4 days of data collection was calculated. Sun protection practices reported on or around the time that the two observations were conducted (Thursday and Saturday) were used to compare with direct visual observation for hat wearing, use of a shirt with sleeves and use of sunglasses. To compare direct observation with survey data, observed use of each practice on the two occasions was assigned a score: 0 = did not observe; 1 = observed. By summing across the two observation periods a score ranging from 0 to 2 was obtained (0 = was not observed using at all; 1 = was observed using on at least one occasion; and 2 = was observed using on both occasions).
Results from sunscreen swabs on the forearm and lower thigh were combined to provide an objective measure of any use of sunscreen at the time of assessment. To compare diary records with this objective assessment, reported use of sunscreen up to and including the time of assessment was determined. For diary and survey comparisons of sunscreen use, the same recoding procedure that was used for other sun habits was adopted.
Kappa coefficients were used to assess agreement between direct observation and diary entries for all sun protection practices at the time observations were completed. Spearman rank correlations (rs) were used to assess agreement between all measures of sun protection, time outside and personal UVR exposure using survey, diary and objective measures (observation and PSDs). Interpretation of agreement was based on guidelines proposed by Landis and Koch (22). Coefficients were categorized on a 6-point ordinal scale: poor (<0.0); slight (0.0–0.20); fair (0.21–0.40); moderate (0.41–0.60); substantial (0.61–0.80); and almost perfect (0.81–1.0) (22). ANOVAs were conducted to compare independent variables such as participants (parent, child, lifeguard) and period of the week (weekday, weekend) with dependant variables including personal UVR exposure and proportion of time using sun protection. Chi-squared statistics were used to examine differences between participants regarding sun habits as reported in the survey.
RESULTS
Participant characteristics
A total of 27 individuals completed the pilot study (seven lifeguards, 10 parents, and 10 children 5–10 years of age) and were predominantly Caucasian (70%). The response rate was 90.0% of those approached. In terms of gender, most parents (80%), 57% of lifeguards and 30% of children were female. The mean age was: parents (36.9 ± 5.8 years); children (6.5 ± 1.8 years); and lifeguards (36.9 ± 13.3 years). Sixty percent of parents and 29% of lifeguards completed 4 years of college or more. All parents reported having at least two children.
Ambient and personal UVR exposure
The mean amount of ambient UVR recorded between 10 A.M. and 4 P.M. over the 2 days was 37.2 SEDs. The correlation between the two dosimeters exposed each hour over the 2 days provided a high level of agreement (r = 0.95).
Survey data revealed that participants reported spending on average 3.4 h (95% CI = 2.6–4.2) outside between 10 A.M. and 4 P.M. last summer. Participants reported in their diary that they spent on average 4 h (95% CI = 3.3–4.8) outside between 10 A.M. and 4 P.M. over the 4 days. While there was no significant difference (F = 0.16, d.f. = 2, P = 0.9) in terms of time participants wore dosimeters (mean 3.8 h; 95% CI = 2.9– 4.6), lifeguards received significantly higher (F = 7.0, d.f. = 2, P = 0.004) levels of ambient UVR exposure (9.2 SED; 95% CI = 5.1–13.2; median = 10.5) when compared with parents (3.7 SED; 95% CI = 2.2–5.4; median = 2.9) or their children (4.6 SED; 95% CI = 2.6–6.5; median = 4.3). The proportion of ambient UVR exposure that participants received during the 2 days of objective assessment was 25.2% for lifeguards, 12.8% for children and 9.4% for parents.
Agreement between personal UVR exposure (PSDs) and reported time outside (diary) was fair (rs = 0.32; P = 0.03). Agreement between diary and survey items revealed moderate to substantial levels of agreement for recall of time outside on weekends (rs = 0.50; P = 0.04) and weekdays (rs = 0.67; P = 0.003). Agreement between PSDs and survey items provided a moderate level of agreement for recall of average number of hours spent outside in the sun on weekdays (rs = 0.45; P = 0.09) and weekends (rs = 0.30; P = 0.3). Only five personal dosimeters were lost throughout the study, resulting in a loss of 9.3%. This was generally a result of spending a prolonged period of time in the water while wearing the dosimeter bracelet.
Sun protection practices
Survey information revealed that 53.6% of participants always/usually wear a hat, 42.9% always/usually wear a shirt with sleeves and 46.4% always/usually use shade. There were no significant differences between parents, children and lifeguards for these sun protection strategies. There was a significant difference for reported use of sunglasses (χ2 = 7.1, d.f. = 2, P = 0.03) with fewer children (20%) likely to usually/always wear sunglasses compared to parents (70.0%) and lifeguards (75%). In contrast, diary reports revealed that participants used individual sun protection practices less than 50% of the time they were outside during the 4 days of data collection (shirt with sleeves = 41.9%; shade use = 27.4%; sunglasses = 27.4%; hat wearing = 17.7%). There were no significant differences between participants for use of shirt with sleeves, shade use or hat wearing, but children were less frequent users (F = 14.0, d.f. = 2, P = 0.000) of sunglasses (mean = 0.4%; 95% CI = −0.45 to 1.2) compared to parents (mean = 33.9%; 95% CI = 14.8–53.1) and lifeguards (mean = 56.6%; 95% CI = 29.2–84.1). For the 2 days direct observations were undertaken, most people were observed at least once to be wearing a shirt with sleeves (81.5%), and 48.1% were observed with sunglasses. The least observed practice was the use of hats with only 29.6% observed wearing them. The only significant difference between participants was for use of sunglasses (χ2 = 11.8, d.f. = 1, P = 0.02), with children less likely to have been observed wearing sunglasses (10%) compared to parents (60%) and lifeguards (85.7%).
Substantial agreement between diary and survey sun protection items was obtained for wearing a hat (rs = 0.72; P = 0.000), sunglasses (rs = 0.78; P = 0.000) and a shirt with sleeves (rs = 0.81; P = 0.000), with a fair level of agreement being obtained for using shade (rs = 0.21; P = 0.30). Agreement between direct visual observation and the survey instrument revealed a moderate level of agreement for wearing sunglasses (rs = 0.57; P = 0.002) and hat wearing (rs = 0.40; P = 0.05), with a fair level of agreement being obtained for wearing a shirt with sleeves (rs = 0.29; P = 0.14). Agreement between direct visual observation and reported sun protection habits at time of observation (diary) provided moderate to substantial agreement (k = 0.48–0.84) for weekday observations (Table 1). For the weekend, substantial agreement was obtained for hat wearing and use of a shirt with sleeves. A fair level of agreement was obtained for sunglasses at this time.
Table 1.
Agreement between observed and reported sun safety practices from diaries.
| Reported sun protection practices* (diary) | Observed sun protection
|
k (95% CI) | |
|---|---|---|---|
| No, n (%) | Yes, n (%) | ||
| Weekday (n = 25) | |||
| Hat wearing | |||
| No | 14 (93.3) | 1 (6.7) | 0.56 (0.21–0.90) |
| Yes | 4 (40.0) | 6 (60.0) | |
| Shirt with sleeves | |||
| No | 6 (60.0) | 4 (40.0) | 0.48 (0.12–0.84) |
| Yes | 2 (13.3) | 13 (86.7) | |
| Sunglasses | |||
| No | 12 (100) | 0 (0) | 0.84 (0.63–1.0) |
| Yes | 2 (15.4) | 11 (84.6) | |
| Weekend (n = 21) | |||
| Hat wearing | |||
| No | 16 (100) | 0 (0) | 0.70 (0.30–1.0) |
| Yes | 2 (40.0) | 3 (60.0) | |
| Shirt with sleeves | |||
| No | 5 (50.0) | 5 (50.0) | 0.51 (0.13–0.89) |
| Yes | 0 (0) | 11 (100) | |
| Sunglasses | |||
| No | 9 (75.0) | 3 (25.0) | 0.31 (0.0–0.72) |
| Yes | 4 (44.4) | 5 (55.6) | |
Reported sun protection practices were assessed at the time direct observations were undertaken rather than reported practices for the day.
Sunscreen use
Based on survey information, over 92% of participants reported that they usually or always use sunscreen, with no significant differences (χ2 = 1.2, d.f. = 2, P = 0.5) between children (100%), parents (90.0%) and lifeguards (87.5%). In contrast, diary estimates of the proportion of time spent outside using sunscreen revealed a significant difference (F = 3.8, d.f. = 2, P = 0.04), with lifeguards spending more time outside using sunscreen (mean = 66.8%; 95% CI = 48.8–84.9) than parents (mean = 37.5%; 95% CI = 9.3–65.7) or children (mean = 28.9%; 95% CI = 15.3–42.6).
The agreement between the sunscreen swabbing procedure and diary reports of sunscreen use up to and including the time the swab was undertaken revealed a fair level of agreement (k = 0.36; 95% CI = 0.1–0.68). Agreement for sunscreen use as reported in the diary and use of sunscreen when outdoors as reported in the survey revealed a fair level of agreement (rs = 0.30; P = 0.13). Poor levels of agreement were obtained when comparing survey results with the swabbing procedure (k = 0.16; 95% CI = 0.0–0.37).
DISCUSSION
This pilot study established the feasibility of conducting this type of validity study in a swimming pool setting and helped the research team to improve the methods and procedures for a larger study the following summer. This study has helped to improve the methods to incorporate objective instruments and procedures into the measurement of sun habits and provided invaluable information regarding the implementation of the procedures on a larger scale. Overall, participants stated (via exit survey) that they did not experience any major difficulties as a result of being involved, and they reported the study to be an interesting, enjoyable and noninvasive experience. They did not report any difficulties in scheduling around the requirements of this study. This was demonstrated by obtaining a complete set of data from all participants recruited, except for one (lifeguard) who withdrew after completing the baseline survey. Finally, laminating the polysulphone film within the hospital identification bracelet was an effective approach to reduce the loss of personal dosimeters as a result of wear and tear. This multimethod approach represents important progress in efforts to increase our understanding of the strengths and limitations of self-reported data collection methodologies.
Lifeguards received higher levels of UVR exposure compared to parents and children, despite no significant differences in the amount of time spent outside. This may reflect the insensitivity of self-reported measures, transient factors such as weather and cloud cover, and/or the impact of shade use. Lifeguards received levels of UVR that were in excess of occupational guidelines proposed by the International Commission on Non- Ionizing Radiation Protection (23). The proportion of ambient UVR obtained by lifeguards was comparable to that previously reported for outdoor workers and people involved in recreation activities (17,24,25). The variation in the levels of UVR received between groups of participants in this study is consistent with those reported previously (26,27).
Agreement between PSDs and diary reports of time outside provided levels of agreement consistent with those findings reported previously (6,7). Survey estimates of time spent outside between 10 A.M. and 4 P.M. were similar to the time participants reported being outside over four consecutive days in their diary, and the results provided a moderate to substantial level of agreement between the two measures. This finding indicates that usual practices of time spent outside between 10 A.M. and 4 P.M. reported in the survey are consistent with diary reports.
For sun protection behaviors, a moderate to substantial level of agreement was found for comparisons between observation and diary (k: 0.31–0.84), diary and survey (rs: 0.72–0.81), and fair to moderate agreement was obtained between direct observation and survey (rs: 0.29–0.57). Observations for clothing worn and sunglasses are all comparable with data from previous studies conducted at various settings such as schools (11), workplaces (9) and the beach (10). Survey data of usual sun habits revealed that participants were more likely to report frequent use (usually/always) of various practices than what was recorded in the 4 day diaries, alluding to a propensity for participants to over-report their usual sun protection practices.
Reported use of sunscreen demonstrated a pattern of association similar to that reported for other sun protection practices, with survey reports of usual practices indicating that participants were more likely to report being frequent users (usually/always) of sunscreen when compared with what they reported in a 4 day diary. Agreement between the swabbing procedure and diary reports of sunscreen use at the time objective assessments were undertaken was lower than the coefficients that have previously been reported for beachgoers (10), and the swabbing procedure provided only slight agreement with survey items for usual sunscreen use. The poor agreement for this study may be due to participants responding to a question related to any use of sunscreen, while the swabbing procedure assessed the presence of sunscreen at two anatomic sites (forearm and thigh). Had the questions asked specifically about where sunscreen was applied, agreement between the measures may have been higher. Alternately, another anatomic site that is representative of where individuals usually apply sunscreen (such as nose or cheek) may need to be considered. Given the astringency of the alcohol swabs, however, the forearm and thigh were considered a better alternative than sites on the face.
Because of the small sample size, these findings are not generalizable to the pool-going public. However, findings provide important preliminary data for a larger study to be conducted at 16 swimming pools in four regions of the United States. This pilot study has compared self-report of sun protection practices, observations and objective biologic assessments of UVR exposure and sunscreen use, within a defined sample of parents, children and lifeguards attending a swimming pool. These data collected within a larger population at several settings will allow for a strong test of the validity of self-report and can help identify the best quality data on sun exposure and protection and sources of systematic error, help improve research methods and interpret findings from skin cancer prevention studies.
Acknowledgments
We thank Janeen Heldt for undertaking this study; Kailua Pool lifeguards, parents and children for their involvement in this study; Leslie Welsh, Kevin Lunde and Katie Suyderhoud for their assistance with participant recruitment and data collection. The research reported here was supported by Grant CA 92505-S1 from the National Cancer Institute.
References
- 1.American Cancer Society. Cancer Facts & Figures 2006. American Cancer Society; Atlanta, GA: 2006. [Google Scholar]
- 2.Jemal A, Devesa SS, Fears TT, Hartge P. Cancer surveillance series: Changing patterns of cutaneous malignant melanoma mortality rates among whites in the United States. J Natl Cancer Inst. 2000;92:811–818. doi: 10.1093/jnci/92.10.811. [DOI] [PubMed] [Google Scholar]
- 3.Glanz K, Geller AC, Shigaki D, Maddock JE, Isnac MR. A randomized trial of skin cancer prevention in aquatics settings: The Pool Cool program. Health Psychol. 2002;21:576–587. [PubMed] [Google Scholar]
- 4.Glanz K, Steffen A, Elliott T, O’Riordan DL. Diffusion of an effective skin cancer prevention program: Design, theoretical foundations, and first-year implementation. Health Psychol. 2005;24:477–487. doi: 10.1037/0278-6133.24.5.477. [DOI] [PubMed] [Google Scholar]
- 5.Glanz K, Mayer JA. Reducing ultraviolet radiation exposure to prevent skin cancer methodology and measurement. Am J Prev Med. 2005;29:131–142. doi: 10.1016/j.amepre.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 6.O’Riordan DL, Stanton WR, Eyeson-Annan M, Gies P, Roy C. Correlations between reported and measured ultraviolet radiation exposure of mothers and young children. Photochem Photobiol. 2000;71:60–64. doi: 10.1562/0031-8655(2000)071<0060:cbramu>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 7.Dwyer T, Blizzard L, Gies PH, Ashbolt R, Roy C. Assessment of habitual sun exposure in adolescents via questionnaire— A comparison with objective measurement using polysulphone badges. Melanoma Res. 1996;6:231–239. doi: 10.1097/00008390-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Girgis A, Sanson-Fisher RW, Watson A. A workplace intervention for increasing outdoor workers’ use of solar protection. Am J Public Health. 1994;84:77–81. doi: 10.2105/ajph.84.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oh SS, Mayer JA, Lewis EC, Slymen DJ, Sallis JF, Elder JP, Eckhardt L, Achter A, Weinstock M, Eichenfield L. Validating outdoor workers’ self-report of sun protection. Prev Med. 2004;39:798–803. doi: 10.1016/j.ypmed.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 10.O’Riordan DL, Lunde KB, Steffen AD, Maddock JE. Validity of self-report sun habits of beachgoers. Arch Dermatol. 2006;142:1304–1311. doi: 10.1001/archderm.142.10.1304. [DOI] [PubMed] [Google Scholar]
- 11.Girgis A, Sanson-Fisher RW, Tripodi D, Golding T. Evaluation of interventions to improve solar protection in primary schools. Health Educ Q. 1993;20:275–287. doi: 10.1177/109019819302000217. [DOI] [PubMed] [Google Scholar]
- 12.O’Riordan DL, Lunde KB, Urschitz J, Glanz K. A non-invasive objective measure of sunscreen use and reapplication. Cancer Epidemiol Biomarkers Prev. 2005;14:722–726. doi: 10.1158/1055-9965.EPI-04-0636. [DOI] [PubMed] [Google Scholar]
- 13.Whiteman DC, Brown RM, Xu C, Paterson CL, Miller D, Parsons PG. A rapid method for determining recent sunscreen use in field studies. J Photochem Photobiol B, Biol. 2003;69:59–63. doi: 10.1016/s1011-1344(02)00409-8. [DOI] [PubMed] [Google Scholar]
- 14.Glanz K, Lew RA, Song V, Murakami-Akatsuka L. Skin cancer prevention in outdoor recreation settings: Effects of the Hawaii SunSmart Program. Eff Clin Pract. 2000;3:53–61. [PubMed] [Google Scholar]
- 15.Glanz K, Silverio R, Farmer A. Diary reveals sun protective practices. The Skin Cancer Foundation Journal. 1996;14:27–28. [Google Scholar]
- 16.Trénel M. Testing a Conceptual Model of Body Exposure to the Sun: Investigating Sun Protection Behaviour and Tanning in Australia. Department of Psychology, Free University of Berlin; Berlin: 1998. p. 148. [Google Scholar]
- 17.Gies HP, Roy CR, Toomey S, MacLennan R, Watson M. Solar UVR exposures of the three groups of outdoor workers on the sunshine coast, Queensland. Photochem Photobiol. 1995;62:1015–1021. [Google Scholar]
- 18.Herlihy E, Gies PH, Roy CR, Jones M. Personal dosimetry of solar UV radiation for different outdoor activities. Photochem Photobiol. 1994;60:288–294. doi: 10.1111/j.1751-1097.1994.tb05106.x. [DOI] [PubMed] [Google Scholar]
- 19.Gies P, Roy C, Toomey S, MacLennan R, Watson M. Solar UVR exposures of primary school children at three locations in Queensland. Photochem Photobiol. 1998;68:78–83. [PubMed] [Google Scholar]
- 20.SPSS Inc. SPSS Version 13.0. SPSS; Chicago, IL: 2004. [Google Scholar]
- 21.CIE Standard. Erythema Action Spectrum and Standard Erythema Dose. Commission Internationale de l’Eclairage, CIE S 007/E-1998; Vienna: 1998. [Google Scholar]
- 22.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.International Commission on Non-Ionizing Radiation Protection. Guidelines on limits of exposure to ultraviolet radiation of wavelengths between 180 nm and 400 nm (incoherent optical radiation) Health Phys. 2004;87:171–186. doi: 10.1097/00004032-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Holman CDJ, I, Gibson M, Stephenson M, Armstrong BK. Ultraviolet irradiation of human body sites in relation to occupation and outdoor activity: Field studies using personal UVR dosimeters. Clin Exp Dermatol. 1983;8:269–277. doi: 10.1111/j.1365-2230.1983.tb01779.x. [DOI] [PubMed] [Google Scholar]
- 25.Wright CY, Reeder AI. Youth solar ultraviolet radiation exposure, concurrent activities and sun-protective practices: A review. Photochem Photobiol. 2005;81:1331–1342. doi: 10.1562/2005-8-19-IR-655. [DOI] [PubMed] [Google Scholar]
- 26.Diffey BL, Gibson CJ, Haylock R, McKinlay AF. Outdoor ultraviolet exposure of children and adolescents. Br J Dermatol. 1996;134:1030–1034. [PubMed] [Google Scholar]
- 27.Thieden E, Philipsen PA, Sandby-Moller J, Wulf HC. Sunburn related to UV radiation exposure, age, sex, occupation, and sun bed use based on time-stamped personal dosimetry and sun behavior diaries. Arch Dermatol. 2005;141:482–488. doi: 10.1001/archderm.141.4.482. [DOI] [PubMed] [Google Scholar]