Abstract
Purpose
Dysregulation of the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) pathway is seen in 40–60% of colorectal cancer (CRC) patients. Everolimus, an oral inhibitor of mTOR, demonstrated efficacy in metastatic CRC (mCRC) patients in phase I studies.
Experimental Design
In sequential phase II studies assessing 2 dosing schedules, mCRC patients refractory to bevacizumab-, fluoropyrimidine-, oxaliplatin-, and irinotecan-based regimens received everolimus 70 mg/week (N=99) or 10 mg/d (N=100). Primary endpoints were disease control rate (DCR) and objective response rate; secondary endpoints included progression-free survival (PFS), overall survival (OS), and duration of response or stable disease (SD). Tumor tissue was collected from all patients for predefined exploratory biomarker analyses.
Results
71 patients were included in the per protocol set for each cohort. DCRs of 31.0% and 32.4% (all SD) were seen in the weekly and daily schedules, respectively. Median duration of SD was 3.9 months in each cohort. Median PFS and OS were 1.8 months and 4.9 months and 1.8 months and 5.9 months, respectively, for the weekly and daily schedules. Among patients receiving daily everolimus, those with a KRAS mutation experienced significantly shorter median OS (P = .008) and lower DCR (P = .035) compared with those with wild-type KRAS in exploratory biomarker analyses.
Conclusions
Everolimus 70 mg/week or 10 mg/day was well tolerated but did not confer meaningful efficacy in heavily pretreated mCRC patients. Future studies may consider evaluating everolimus in combination with other agents or in patients with dysregulation of the PI3K/Akt/mTOR pathway.
Keywords: Clinical trial, Colorectal cancer, Everolimus, mTOR, Phase II
INTRODUCTION
Colorectal cancer (CRC) is the third most common cause of cancer and cancer mortality in the United States [1]. Approximately 20% of patients have distant metastases at presentation [1], and 20% to 50% of patients will relapse after treatment and progress to metastatic CRC (mCRC) [2]. Treatments available for CRC have changed greatly in the past 10 years and have resulted in substantial improvements in survival. Despite these medical advancements, novel therapeutic agents targeting specific molecular signaling pathways are needed when standard treatments fail and patients develop progressive disease.
Mammalian target of rapamycin (mTOR), a serine-threonine tyrosine kinase, is a key regulatory protein of normal cell division and growth that lies downstream of the phosphatidylinositol 3-kinase (PI3K)/Akt signaling pathway and is activated in response to mitogens, extracellular growth factors such as epidermal growth factor (EGF), vascular endothelial growth factor (VEGF), and insulin-like growth factor (IGF), and nutrients such as glucose, amino acids, and oxygen. Upon activation, mTOR relays the cellular signal to downstream effectors to stimulate cell growth, proliferation, and angiogenesis [3,4]. PI3K gene mutation and amplification, AKT mutation and amplification, and loss of the PTEN tumor suppressor gene lead to constitutive activation of the PI3K/Akt/mTOR pathway, which contributes to the pathophysiology of several human malignancies, including CRC [3–5]. Mutations in PI3K have been observed in 10% to 20% of patients with CRC [6,7], and loss of PTEN in approximately 40% [6,8]. Moreover, approximately 30% to 40% of patients with CRC harbor mutations in KRAS, another upstream regulator of PI3K/Akt/mTOR [9–11].
Everolimus is an oral inhibitor of mTOR. In two phase I studies of everolimus in patients with solid tumors, two patients with mCRC achieved partial responses (PR) [12,13]. Based on the prevalence of PI3K/Akt/mTOR activation in patients with CRC and the promising antitumor activity of everolimus, we conducted a multicenter phase II study to assess the disease control rate provided by everolimus in patients with mCRC who experience progressive disease after standard therapies.
METHODS
Patients and Study Design
This prospective, open-label, multicenter phase II trial (ClinicalTrials.gov identifier NCT00419159) enrolled patients from December 1, 2006 to June 3, 2008. Inclusion criteria included age ≥18 years, histologically confirmed mCRC, ≥1 measurable lesion, and radiologically documented progressive disease per the Response Evaluation Criteria in Solid Tumors (RECIST) [14] during or within 6 months of the most recent dose of chemotherapy including a fluoropyrimidine, oxaliplatin, irinotecan, or a targeted agent. Previous treatment with bevacizumab-, fluoropyrimidine-, oxaliplatin-, and irinotecan-based regimens, was required. For patients with EGFR-positive tumors as determined by staining 2+ or 3+ on immunohistochemistry, previous treatment with cetuximab or panitumumab was required per standard practice; KRAS mutation status had not yet emerged as a predictive marker of anti-EGFR agent efficacy during the accrual period of the study. Additional eligibility criteria included no previous treatment with everolimus or other mTOR inhibitors, sufficient and obtainable tumor tissue for biomarker analysis (only the original surgical resection was acceptable), a World Health Organization (WHO) performance status of 0–2, and adequate bone marrow, hepatic, and renal function. Patients with untreated or neurologically unstable central nervous system metastases and/or uncontrolled medical conditions or other conditions that could affect their participation in the study were excluded. All subjects provided written informed consent, and the study was approved by the Institutional Review Boards of all participating institutions.
Patients were enrolled in two consecutive phase II cohorts. The initial cohort received everolimus 70 mg once weekly, and the second cohort received everolimus 10 mg once daily. In both cohorts, treatment was administered continuously until disease progression, unacceptable toxicity, or study discontinuation. Two everolimus dose reductions were allowed for unacceptable toxicity: 70 mg/week to 50 mg/week and then 40 mg/week in the weekly cohort and 10 mg/day to 5 mg/day and then 5 mg every other day in the daily cohort. If treatment was interrupted due to toxicity, everolimus was not resumed until recovery to grade ≤1 and was reintroduced at the initial dose or lower dose level depending on the toxicity and grade. Patients with interruptions lasting longer than 21 days or who were intolerant of the lowest dose level were discontinued from the study. Adverse events associated with everolimus treatment (stomatitis, non-infectious pneumonitis, hyperlipidemia, and hyperglycemia) were treated using prespecified management algorithms.
Efficacy and Safety Assessments
Tumor measurements were obtained via computed tomography or magnetic resonance imaging of the chest/abdomen and pelvis at baseline, every 8 weeks until determination of disease progression per the local investigator and radiologist, and at end of study, according to RECIST version 1.0 [14]. Patients were followed every 3 months for survival. Exploratory biomarker analyses were performed using formalin-fixed/paraffin-embedded archival tumor tissue and, if available, tissue from the most recent post-diagnosis biopsy or optional biopsy of a metastatic site. The mutational status of PIK3CA, KRAS, and BRAF was assessed by sequencing tumor DNA using the Sanger method. Protein expression of PTEN, phosphorylated Akt(Ser473), phosphorylated S6(Ser240), and p53 was assessed by immunohistochemistry using clones 6H2.1 (Dako), 736E11 (Cell Signaling Technologies), DAK-S6-240 (Dako), and DO-7 (Dako), respectively.
Safety assessments consisted of collecting all adverse events (AEs) and serious AEs during study treatment and for 28 days thereafter. AEs were assessed according to the Common Toxicity Criteria for Adverse Events, version 3.0. Hematology, blood chemistry, urine, and vital signs were regularly monitored, and physical examinations, WHO performance status, and body weight were regularly assessed.
Statistical Analyses
The full analysis set (FAS) included all patients who were evaluabe for efficacy, defined as patients who received at least one everolimus dose. The safety population included all patients who received at least one dose of everolimus and had at least one post-baseline safety assessment. The per protocol set (PPS) included all patients from the FAS who were evaluable for efficacy without any major protocol deviation and either completed a minimum exposure requirement (defined as having a relative dose intensity over the first eight weeks of treatment of at least 50%) or progressed before the minimum exposure requirement could be met.
Primary efficacy endpoints were the disease control rate (DCR) and objective response rate (ORR). DCR was defined as the proportion of patients with best overall response of complete response (CR), PR, or stable disease (SD). ORR was defined as the proportion of patients with best overall response of CR or PR. Secondary efficacy endpoints included progression-free survival (PFS), overall survival (OS), duration of SD, and duration of response. Exploratory endpoints included analyses of DCR, PFS, and OS by subgroups of key clinical factors and predefined molecular biomarkers.
Within each of the two consecutive phase II cohorts, a Simon two-stage design was used based on DCR in the PPS at week 8. This endpoint provided a signal of anti-tumor activity that was available relatively quickly in patients, and captured both disease stabilization and objective tumor shrinkage. A DCR of ≤30% would preclude further study; the targeted DCR for efficacy was set at 45%. Within each cohort, the study design required a total of 34 patients in the PPS at week 8 in the first stage using a significance level of 10% and a power of 90%. If ≤10 patients achieved disease control, then the treatment schedule would be stopped; otherwise, an additional 41 patients would be included in the PPS at week 8. If ≥28 patients in the overall PPS achieved disease control, then that treatment schedule of everolimus would be considered worthy of further study. The primary measure of efficacy at the end of the trial was ORR. The primary endpoints of DCR and ORR were calculated in the PPS and FAS, respectively. Supportive analyses of DCR and ORR were determined in the FAS and PPS, respectively. Patients with best overall response of “unknown” were treated as nonresponders. It was estimated that up to 100 patients would need to be enrolled onto each treatment schedule in the FAS in order to attain the required 75 patients for each PPS.
All secondary efficacy endpoints were determined in the FAS for each treatment schedule. PFS was defined as the time from date of first study treatment to the date of the first documented disease progression or death due to any cause. OS was defined as the time from start of treatment to the date of death due to any cause. Duration of SD was defined as the time from start of treatment to documented disease progression or death due to underlying cancer. Duration of response was defined as the time from first documented response to documented disease progression or death due to underlying cancer. Potential relationships between biomarkers and PFS and OS were explored using Cox regression analysis. Hazard ratios with 95% confidence intervals (CI)s for the patient groups (ie, KRAS/BRAF mutated vs wild type and PTEN expression low vs normal) were determined based on the Cox model adjusted for two prognostic factors: WHO performance status (0 vs ≥1) and baseline lactate dehydrogenase. For assessment of potential relationships between biomarkers and DCR, odds ratios and 95% CIs were determined based on logistic regression models adjusted for the two prognostic factors.
RESULTS
Patient Characteristics and Disposition
Between December 2006 and June 2008, 99 and 100 patients were enrolled in the everolimus 70 mg weekly and 10 mg daily schedules, respectively. Demographic and baseline characteristics were similar among patients in both schedules (Table 1). All patients in each treatment schedule received at least one everolimus dose and were included in both the FAS and the safety population. At the time of database lock, all patients had discontinued treatment, most commonly for disease progression (79.8% of patients in the weekly schedule and 76.0% of patients in the daily schedule) (Table 2). A total of 71 patients were included in the PPS in each treatment schedule; reasons for exclusion from the PPS included unknown best overall response based on investigator review (n=35), insufficient treatment exposure (n=17), baseline tumor assessment >21 days prior to first dose of everolimus (n=15), lack of treatment with all required previous chemotherapy agents (n=13), receipt of anticancer therapy within 4 weeks prior to first dose of everolimus (n=2), lack of histological or cytological confirmation of CRC diagnosis (n=1), and initiation of the weekly treatment schedule instead of the assigned daily schedule (n=1).
Table 1.
Baseline Demographic and Disease Characteristics (Full Analysis Set)
| Characteristic | Everolimus 70 mg/week (N = 99) | Everolimus 10 mg/day (N = 100) |
|---|---|---|
| Age, median y (range) | 61.0 (32–81) | 61.5 (25–84) |
| Sex, N (%) | ||
| Male | 52 (52.5) | 52 (52.0) |
| Female | 47 (47.5) | 48 (48.0) |
| WHO PS, N (%) | ||
| 0 | 45 (45.5) | 50 (50.0) |
| 1 | 52 (52.5) | 44 (44.0) |
| 2 | 2 (2.0) | 5 (5.0) |
| ≥1 | 54 (54.5) | 49 (49.0) |
| Missing | 0 | 1 (1.0) |
| Primary site of cancer, N (%) | ||
| Colon | 72 (72.7) | 76 (76.0) |
| Rectum | 21 (21.2) | 14 (14.0) |
| Other a | 6 (6.1) | 10 (10.0) |
| Histology/cytology, N (%) | ||
| Adenocarcinoma | 93 (93.9) | 95 (95.0) |
| Mucinous adenocarcinoma | 6(6.1) | 4 (4.0) |
| Other | 0 | 1 (1.0) |
| Histologic grade, N (%) | ||
| Well differentiated | 9 (9.1) | 13 (13.0) |
| Moderately differentiated | 78 (78.8) | 64 (64.0) |
| Poorly differentiated | 11 (11.1) | 17 (17.0) |
| Unknown | 1 (1.0) | 6 (6.0) |
| Time since initial diagnosis, N (%) | ||
| ≤12 months | 2 (2.0) | 3 (3.0) |
| >12 months to ≤ 24 months | 23 (23.2) | 23 (23.0) |
| >24 months | 74 (74.7) | 74 (74.0) |
| Number of organs involved, N (%) | ||
| ≤2 | 47 (47.5) | 52 (52.0) |
| >2 | 52 (52.5) | 48 (48.0) |
| Visceral involvement, N (%) | 97 (98.0) | 100 (100) |
| PIK3CA, N (%) | ||
| Wild-type | 76 (76.8) | 76 (76.0) |
| Mutation | 3 (3.0) | 5 (5.0) |
| Missing | 20 (20.2) | 19 (19.0) |
| PTEN expression, N (%) | ||
| Low | 43 (43.4) | 26 (26.0) |
| Normal | 30 (30.3) | 46 (46.0) |
| Missing | 26 (26.3) | 28 (28.0) |
| KRAS, N (%) | ||
| Wild type | 46 (46.5) | 40 (40.0) |
| Mutation | 33 (33.3) | 41 (41.0) |
| Missing | 20 (20.2) | 19 (19.0) |
| BRAF, N (%) | ||
| Wild type | 71 (71.2) | 72 (72.0) |
| Mutation | 8 (8.1) | 7 (7.0) |
| Missing | 20 (20.2) | 21 (21.0) |
Includes cecum (N = 5), colon and rectum (N = 3), rectosigmoid (N = 4), sigmoid colon (N = 2), colorectal (N = 1), and splenic-colon corner (N = 1).
PIK3CA, phosphatidylinositol 3-kinase catalytic subunit; PTEN, phosphatase and tensin homolog; WHO PS, World Health Organization performance status.
Table 2.
Reasons for Treatment Discontinuation (Full Analysis Set)
| Reason for Treatment Discontinuation | Everolimus 70 mg/week (N = 99) | Everolimus 10 mg/day (N = 100) |
|---|---|---|
| Discontinued, N (%) | 99 (100.0) | 100 (100.0) |
| Disease progression | 79 (79.8) | 76 (76.0) |
| Adverse event(s) | 7 (7.1) | 15 (15.0) |
| Abnormal laboratory value(s) | 0 | 2 (2.0) |
| Subject’s condition no longer required study drug | 0 | 1 (1.0) |
| Protocol violation | 1 (1.0) | 0 |
| Subject withdrew consent | 10 (10.1) | 3 (3.0) |
| Lost to follow-up | 0 | 1 (1.0) |
| Death | 2 (2.0) | 2 (2.0) |
Treatment Exposure and Dose Reductions
The median duration of exposure was 8.0 weeks (range, 1.0 to 31.0 weeks) in the weekly schedule and 8.0 weeks (range, 1.0 to 44.0 weeks) in the daily schedule. The percentage of patients who had at least one everolimus dose reduction/interruption was 31.3% and 42.0% in the weekly and daily schedules, respectively. Mean relative dose intensity was 0.90 in the weekly schedule and 0.92 in the daily schedule.
Efficacy
In both the weekly and daily everolimus schedules, disease stabilization was achieved by 12 of the first 34 patients in the PPS, thus meeting the Simon two-stage requirement to expand enrollment for both schedules. Regardless of the population of analysis, no CRs or PRs were observed, and the best overall response was SD. The protocol-defined primary endpoint, the DCR in the PPS, was 31.0% in the weekly schedule and 32.4% in the daily schedule (Table 3).
Table 3.
Best Overall Response Per Investigator According to RECIST
| Response | Everolimus 70 mg/week | Everolimus 10 mg/day |
|---|---|---|
| Per protocol set | N = 71 | N = 71 |
| CR | 0 | 0 |
| PR | 0 | 0 |
| SD | 22 (31.0) | 23 (32.4) |
| PD | 49 (69.0) | 48 (67.6) |
| Unknown | 0 | 0 |
| DCR, a % (95% CI) | 31.0 (20.5–43.1) | 32.4 (21.8–44.5) |
| Full analysis set | n = 99 | n = 100 |
| CR | 0 | 0 |
| PR | 0 | 0 |
| SD | 25 (25.3) | 26 (26.0) |
| PD | 58 (58.6) | 55 (55.0) |
| Unknown | 16 (16.2) | 19 (19.0) |
| DCR, % (95% CI) | 25.3 (17.1–35.0) | 26.0 (17.7–35.7) |
Unless otherwise noted, all data are presented as n (%).
Primary study endpoint.
CI, confidence interval; CR, complete response; DCR, disease control rate (CR+PR+SD); PD, progressive disease; PR, partial response; RECIST, Response Evaluation Criteria in Solid Tumors; SD, stable disease.
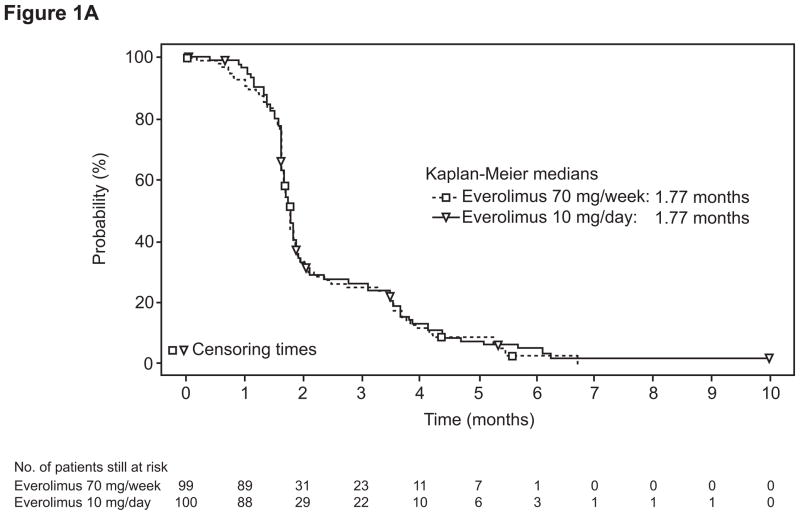
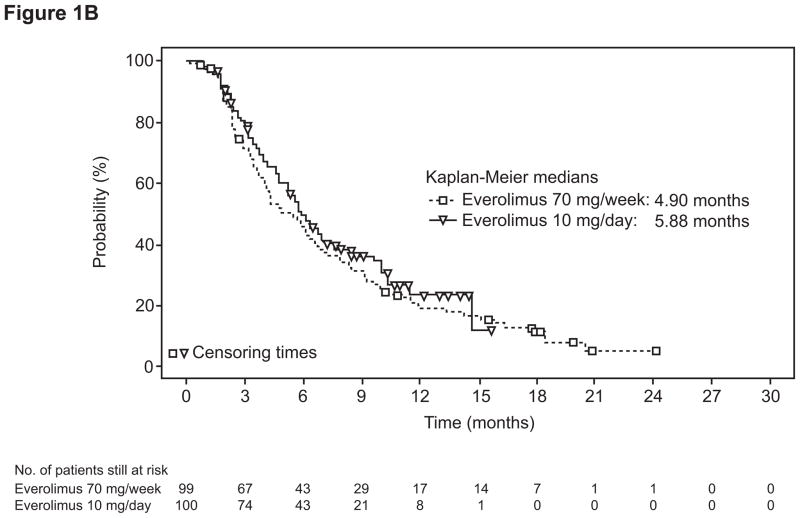
In the FAS, the DCR was 25.3% in the weekly schedule and 26.0% in the daily schedule (Table 3). In the FAS, median duration of SD was 3.9 months (95% CI, 3.6 to 5.3 months) in the weekly schedule and 3.9 months (95% CI, 3.6 to 4.7 months) in the daily schedule. Median PFS in the FAS was 1.8 months (95% CI, 1.7 to 1.8 months) in the weekly schedule and 1.8 months (95% CI, 1.7 to 1.9 months) in the daily schedule (Figure 1A). Median OS was 4.9 months (95% CI, 4.0 to 6.6 months) and 5.9 months (95% CI, 4.7 to 7.1 months), respectively (Figure 1B).
Figure 1.
Kaplan-Meier estimates of progression-free survival by investigator review (A) and overall survival (B) by treatment group in the full analysis set.
Exploratory Biomarker Analyses
Of the 199 enrolled patients, KRAS mutation status was available for 160 (80.4%), and 74 of those evaluable (46.2%) had a confirmed mutation. In exploratory analyses and after adjustment for key prognostic variables, KRAS mutational status did not significantly influence PFS in either the weekly (P = .372) or daily (P = .216) everolimus schedules or OS or DCR in the weekly schedule (P = .487 and .127, respectively) (Table 4). However, among patients receiving daily everolimus, those with a KRAS mutation experienced significantly shorter median OS (P = .008) and lower DCR (P = .035) compared with those with wild-type KRAS (Table 4). PTEN expression was low in 69 of the 145 patients (47.6%) for whom expression data were available. PTEN expression did not significantly influence the DCR or median PFS or OS in either treatment schedule (Table 4).
Table 4.
Effect of Biomarkers on Clinical Efficacy (Full Analysis Set)
| Biomarker Parameters | Everolimus 70 mg/week | Everolimus 10 mg/day | ||
|---|---|---|---|---|
| KRAS | Mutant | Wild-type | Mutant | Wild-type |
| N | 33 | 46 | 41 | 40 |
| DCR, N (%) | 11 (33.3) | 10 (21.7) | 7 (17.1) | 14 (35.0) |
| OR (95% CI) | 2.357 (0.784–7.085) | 0.301 (0.099–0.917) | ||
| P value | .127 | .035 | ||
| PFS, mo, median (95% CI) | 1.77 (1.64–2.37) | 1.71 (1.64–1.81) | 1.71 (1.68–1.84) | 1.77 (1.64–3.22) |
| HR (95% CI) | 0.803 (0.495–1.301) | 1.357 (0.837–2.201) | ||
| P value | .372 | .216 | ||
| OS, mo, median (95% CI) | 6.18 (2.40–8.05) | 4.90 (3.65–6.60) | 5.59 (4.24–7.69) | 7.06 (5.32-NA) |
| HR (95% CI) | 1.196 (0.723–1.978) | 2.210 (1.225–3.989) | ||
| P value | 0.487 | 0.008 | ||
| PTEN expression | Low | Normal | Low | Normal |
| N | 43 | 30 | 26 | 46 |
| DCR, N (%) | 9 (20.9) | 10 (33.3) | 7 (26.9) | 12 (26.1) |
| OR (95% CI) | 0.533 (0.167–1.700) | 0.933 (0.289–3.015) | ||
| P value | .287 | .908 | ||
| PFS, mo, median (95% CI) | 1.71 (1.64–1.81) | 1.77 (1.64–3.48) | 1.81 (1.68–2.14) | 1.68 (1.64–1.94) |
| HR (95% CI) | 1.543 (0.898–2.651) | 0.976 (0.555–1.715) | ||
| P value | .117 | .932 | ||
| OS, mo, median (95% CI) | 5.98 (3.48–7.92) | 4.37 (2.43–7.26) | 10.38 (5.52–14.69) | 6.34 (4.63–9.63) |
| HR (95% CI) | 1.333 (0.789–2.254) | 0.687 (0.343–1.376) | ||
| P value | .283 | .290 | ||
ORs and accompanying 95% CIs for DCR were obtained using a logistic regression model adjusted for WHO performance status (0 vs ≥1) and baseline lactate dehydrogenase. HRs and accompanying 95% CIs for PFS and OS were obtained using a Cox model adjusted for WHO performance status (0 vs ≥1) and baseline lactate dehydrogenase.
CI, confidence interval; DCR, disease control rate; HR, hazard ratio; OR, odds ratio; OS, overall survival; PFS, progression-free survival; WHO, World Health Organization.
Among the 158 patients (79.4%) evaluated for BRAF, mutation was detected in 15 (9.5%). Median PFS in the combined weekly and daily schedules was 1.6 months in patients with a BRAF mutation and 1.7 months in patients with wild-type BRAF. In an adjusted Cox analysis, patients with BRAF mutation had a greater risk of death or progression than patients with wild-type BRAF (HR, 1.7; 95% CI, 1.0 to 3.0; P = .048). PIK3CA mutations were found in only 8 of 160 patients (5%) for whom mutation status was available, precluding determination of the impact of PIK3CA mutations on survival. Baseline tumor expression of phosphorylated Akt, phosphorylated S6, and p53 showed no correlation with PFS or OS (data not shown).
Safety
All patients in the study reported at least one AE. Grade 3/4 AEs were reported for 58.6% of patients in the everolimus weekly schedule and 50.0% of patients in the daily schedule. Dose reductions and/or interruptions due to an AE were reported for 24.2% of patients in the weekly schedule and 35.0% of patients in the daily schedule.
The overall AE profile in both groups was consistent with the known safety profile of everolimus (Table 5). For most AEs, the percentage of patients who experienced a given AE was higher in the weekly schedule compared with the daily schedule. The most common AEs (any grade) in the everolimus 70 mg weekly schedule were fatigue (50.5%), nausea (41.4%), rash (34.3%), and decreased appetite (31.3%). In the 10 mg daily schedule, the most common AEs (any grade) were fatigue (37.0%), rash (29.0%), diarrhea (26.0%), and decreased appetite (25.0%). Pneumonitis was reported in two patients in each treatment schedule, with one patient in each schedule experiencing a grade 3 event.
Table 5.
Adverse Events Occurring in ≥ 10% of Patients in Either Treatment Schedule (Safety Set)
| Adverse events, N (%) | Everolimus 70 mg/week (N = 99) | Everolimus 10 mg/day (N = 100) | ||
|---|---|---|---|---|
|
| ||||
| All grades | Grade 3/4 | All grades | Grade 3/4 | |
| Fatigue | 50 (50.5) | 7 (7.1) | 37 (37.0) | 5 (5.0) |
| Nausea | 41 (41.4) | 3 (3.0) | 22 (22.0) | 0 |
| Rash | 34 (34.3) | 0 | 29 (29.0) | 0 |
| Decreased appetite | 31 (31.3) | 1 (1.0) | 25 (25.0) | 1 (1.0) |
| Diarrhea | 29 (29.3) | 2 (2.0) | 26 (26.0) | 2 (2.0) |
| Vomiting | 29 (29.3) | 4 (4.0) | 14 (14.0) | 2 (2.0) |
| Anemia | 26 (26.3) | 5 (5.1) | 19 (19.0) | 3 (3.0) |
| Constipation | 24 (24.2) | 2 (2.0) | 13 (13.0) | 0 |
| Dyspnea | 21 (21.2) | 3 (3.0) | 21 (21.0) | 4 (4.0) |
| Abdominal pain | 20 (20.2) | 3 (3.0) | 15 (15.0) | 3 (3.0) |
| Stomatitis | 18 (18.2) | 2 (2.0) | 22 (22.0) | 4 (4.0) |
| Mucosal inflammation | 17 (17.2) | 0 | 11 (11.0) | 0 |
| Edema peripheral | 16 (16.2) | 0 | 14 (14.0) | 0 |
| Thrombocytopenia | 16 (16.2) | 2 (2.0) | 18 (18.0) | 3 (3.0) |
| Asthenia | 15 (15.2) | 3 (3.0) | 23 (23.0) | 5 (5.0) |
| Pyrexia | 14 (14.1) | 0 | 16 (16.0) | 0 |
| Weight decreased | 14 (14.1) | 0 | 14 (14.0) | 0 |
| Cough | 13 (13.1) | 1 (1.0) | 16 (16.0) | 0 |
| Dehydration | 13 (13.1) | 3 (3.0) | 11 (11.0) | 3 (3.0) |
| Hypercholesterolemia | 13 (13.1) | 3 (3.0) | 10 (10.0) | 2 (2.0) |
| Hyperglycemia | 13 (13.1) | 4 (4.0) | 9 (9.0) | 4 (4.0) |
| Back pain | 10 (10.1) | 0 | 8 (8.0) | 2 (2.0) |
| Headache | 10 (10.1) | 0 | 7 (7.0) | 0 |
| Gamma-glutamyltransferase increased | 9 (9.1) | 6 (6.1) | 13 (13.0) | 7 (7.0) |
| Epistaxis | 5 (5.1) | 1 (1.0) | 10 (10.0) | 0 |
Eleven patients (11.1%) in the weekly schedule and 14 patients (14.0%) in the daily schedule experienced death while on treatment or within the 28-day follow-up period. All deaths were considered unrelated to study drug. The cause of death was disease progression in 22 patients and renal failure, multiple organ failure, and pneumonia in one patient each.
DISCUSSION
In this study, single-agent everolimus demonstrated minimal activity in patients with heavily pretreated mCRC who had progressive disease after treatment with several targeted and chemotherapeutic agents. Administration of everolimus 70 mg weekly or 10 mg daily resulted in disease stabilization in approximately 30% of patients in the PPS (protocol-defined primary endpoint) and approximately 25% of patients in the FAS. No patients experienced a PR or CR. Both the weekly and daily everolimus schedules were well tolerated in this patient population, and the AEs observed were consistent with the overall clinical experience with everolimus in cancer [15–18].
Considerable data exist to support a role for the PI3K/Akt/mTOR pathway in CRC pathogenesis. Akt overexpression and activated Akt activation have been detected in colorectal neoplasms [19], as has overexpression of Raptor and Rictor, two regulatory proteins bound to the mTOR complex [20,21]. Preclinical studies have shown CRC cell growth and progression when the pathway is activated [22], and decreased proliferation, increased apoptosis, and attenuated cell cycle progression when mTOR is inhibited [21]. In addition, increased mRNA levels of mTOR are seen in tumor samples from patients with advanced stages of CRC compared with samples from patients with earlier stages of disease, with mTOR inhibition attenuating migration and invasion in vitro [20].
KRAS is mutated in approximately 30% to 40% of CRC patients [9–11], leading to activation of several downstream pathways, including the PI3K/Akt/mTOR and RAF/MEK/ERK pathways. In our study, 46% of evaluable patients had a KRAS mutation. In exploratory analyses of our patient population adjusted for key prognostic factors, the presence of KRAS mutation did not significantly affect PFS; however, among patients who received daily everolimus, those with KRAS-mutant tumors experienced a significantly shorter median OS than those with KRAS wild-type tumors. The shorter median OS in patients with KRAS-mutant tumors who received daily everolimus is consistent with preclinical data showing that human cells harboring KRAS mutations were less sensitive to mTOR inhibition and clinical data showing that patients whose tumors harbored KRAS mutations did not derive benefit from everolimus monotherapy [23]. However, these results are hypothesis-generating and further research is necessary to determine whether they are reproducible or whether they are an artifact of the multiple comparisons performed. Overall, no patient subset defined by KRAS mutation, BRAF mutation, or tumoral expression of PTEN, phosphorylated Akt, phosphorylated S6, or p53 appeared to experience a uniquely improved outcome in this population of subjects treated with everolimus.
One possible explanation for the lack of significant single-agent everolimus activity in CRC may be the presence of a negative feedback loop within the PI3K/Akt/mTOR pathway, mediated by ribosomal S6 kinase 1 (S6K1) and insulin receptor substrates (IRS) 1 and 2 [24]. Upon inhibition of mTOR, this negative feedback may be lost, resulting in a paradoxical increase in PI3K signaling, Akt activation, and consequent cell growth and survival [12,25,26]. Future studies should therefore evaluate inhibitors of mTOR in combination with inhibitors of PI3K and insulin-like growth factor-1 receptor (IGF-1R), as well as agents targeted at other upstream components of the pathway. Of note, in a phase I study of everolimus in combination with the IGF-1R inhibitor OSI-906, dose-limiting toxicities of mucositis, nausea/vomiting, thrombocytopenia, and neutropenia were observed, and the maximum tolerated dose of the combination (everolimus 5 mg once daily plus OSI-906 50 mg twice daily) was the lowest dose level tested; this dose level showed no significant sign of clinical activity in refractory mCRC [27]. Results of the ongoing phase I dose-finding study of everolimus in combination with the IGF-1R inhibitor AMG 479 for patients with advanced solid tumors, which has a planned extension cohort of patients with mCRC, may provide more information on the safety and efficacy of combining mTOR and IGF-1R inhibition [28]. Everolimus has also been studied in combination with bevacizumab in patients with mCRC. In a phase II study of 50 patients with mCRC who progressed on standard therapies including bevacizumab, the combination of everolimus 10 mg/day with bevacizumab 10 mg/kg every 2 weeks was tolerable, but failed to show significant clinical activity as the best overall response was SD, observed in 46% of patients [29]. Currently, everolimus is being evaluated as part of combination therapy with panitumumab and irinotecan as second-line therapy (NCT01139138) and with FOLFOX and bevacizumab as first-line therapy (NCT01047293).
Strengths of this phase II study include the evaluation of two separate dosing schedules of everolimus with adequate power, and the multi-center nature of the study with enrollment of patients across two continents, supporting the generalizability of the results. The biomarker data reported is also hypothesis-generating and contributes further to our understanding of the PI3K/Akt/mTOR pathway. Limitations of the trial include the enrollment of a large number of subjects in order to obtain the required population for analysis, and the high rate of unknown best overall response in the study cohort, although this is not uncommon in studies of refractory metastatic colorectal cancer patients.
While the ongoing studies described above may demonstrate improved efficacy when everolimus is used in combinations, our results suggest that single-agent everolimus does not confer meaningful efficacy for refractory mCRC. Future studies of everolimus in combination with other targeted agents may benefit from enrolling patients with molecularly confirmed dysregulation of the PI3K/Akt/mTOR pathway.
STATEMENT OF TRANSLATIONAL RELEVANCE.
Dysregulation of the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) pathway is seen in 40–60% of colorectal cancer (CRC) patients, and represents a promising target for CRC therapy. Herein we report the results of a large phase II study of two dose schedules of everolimus, an mTOR inhibitor, in 199 multiply-refractory, metastatic CRC patients. We definitively show that there is no meaningful benefit of everolimus when administered as a single agent in this large, highly-refractory population. Extensive biomarker analyses demonstrate that KRAS-mutated patients receiving daily everolimus experienced significantly poorer outcomes compared with wild-type KRAS patients. We also confirmed that patients with BRAF mutation had worse survival compared to patients with wild-type BRAF. As a result of this important study, future research can now be guided towards combination studies targeting the PI3K/Akt/mTOR and other related pathways, and trials focused on selected patients with dysregulation of the pathway.
Acknowledgments
We thank Melanie Leiby, PhD, of ApotheCom (Yardley, PA) for providing editorial assistance in support of this manuscript.
GRANT SUPPORT
This work was supported by Novartis Pharmaceuticals Corporation.
Financial Support: Financial support for this study was provided by Novartis Oncology.
Footnotes
Potential Conflicts of Interest:
Consultant or Advisory Role:
Dr. Tabernero: Amgen, Bristol-Myers Squibb, Genentech, Merck KGaA, Millennium, Novartis, Onyx, Pfizer, ImClone, Roche, Sanofi
Dr. Sharma: Novartis
Dr. Ryan: Genomic Health, Boehringer Ingelheim
Dr. Fuchs: Sanofi, Pfizer, Amgen, Metamark Genetics, Bristol-Myers Squibb, Bayer
Honoraria:
Dr. Tabernero: Amgen, Merck KGaA, Novartis, Roche, Sanofi
Research Funding:
Dr. Sharma: Novartis
Employment or Leadership:
Dr. Sedova: Novartis Pharma AG (Statistician)
Dr. Jin: Novartis Pharmaceuticals Corporation (Expert Clinical Manager)
Dr. Malek: Novartis Pharma AG (Global Clinical Leader)
Stock Ownership:
Dr. Sedova: Novartis Pharma AG
Dr. Malek: Novartis Pharma AG
All remaining authors have declared no conflicts of interest.
Reference List
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Field K, Lipton L. Metastatic colorectal cancer-past, progress, and future. World J Gastroenterol. 2007;13:3806–15. doi: 10.3748/wjg.v13.i28.3806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–84. doi: 10.1016/j.cell.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes Dev. 2004;18:1926–45. doi: 10.1101/gad.1212704. [DOI] [PubMed] [Google Scholar]
- 5.Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 6.Frattini M, Signoroni S, Pilotti S, Bertario L, Benvenuti S, Zanon C, et al. Phosphatase protein homologue to tensin expression and phosphatidylinositol-3 phosphate kinase mutations in colorectal cancer. Cancer Res. 2005;65:11227. doi: 10.1158/0008-5472.CAN-05-2780. [DOI] [PubMed] [Google Scholar]
- 7.Velho S, Oliveira C, Ferreira A, Ferreira AC, Suriano G, Schwartz S, Jr, et al. The prevalence of PIK3CA mutations in gastric and colon cancer. Eur J Cancer. 2005;41:1649–54. doi: 10.1016/j.ejca.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 8.Goel A, Arnold CN, Niedzwiecki D, Carethers JM, Dowell JM, Wasserman L, et al. Frequent inactivation of PTEN by promoter hypermethylation in microsatellite instability-high sporadic colorectal cancers. Cancer Res. 2004;64:3014–21. doi: 10.1158/0008-5472.can-2401-2. [DOI] [PubMed] [Google Scholar]
- 9.Andreyev HJ, Norman AR, Cunningham D, Oates JR, Clarke PA. Kirsten ras mutations in patients with colorectal cancer: the multicenter “RASCAL” study. J Natl Cancer Inst. 1998;90:675–84. doi: 10.1093/jnci/90.9.675. [DOI] [PubMed] [Google Scholar]
- 10.Andreyev HJ, Norman AR, Cunningham D, Oates J, Dix BR, Iacopetta BJ, et al. Kirsten ras mutations in patients with colorectal cancer: the ‘RASCAL II’ study. Br J Cancer. 2001;85:692–6. doi: 10.1054/bjoc.2001.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML. Relationship of Ki-ras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomarkers Prev. 2000;9:1193–7. [PubMed] [Google Scholar]
- 12.Tabernero J, Rojo F, Calvo E, Burris H, Judson I, Hazell K, et al. Dose- and schedule-dependent inhibition of the mammalian target of rapamycin pathway with everolimus: a phase I tumor pharmacodynamic study in patients with advanced solid tumors. J Clin Oncol. 2008;26:1603–10. doi: 10.1200/JCO.2007.14.5482. [DOI] [PubMed] [Google Scholar]
- 13.O’Donnell A, Faivre S, Burris HA, 3rd, Rea D, Papadimitrakopoulou V, Shand N, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol. 2008;26:1588–95. doi: 10.1200/JCO.2007.14.0988. [DOI] [PubMed] [Google Scholar]
- 14.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 15.Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, et al. Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer. 2010;116:4256–65. doi: 10.1002/cncr.25219. [DOI] [PubMed] [Google Scholar]
- 16.Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:514–23. doi: 10.1056/NEJMoa1009290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pavel ME, Hainsworth JD, Baudin E, Peeters M, Hörsch D, Winkler RE, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT 2): A randomised, placebo-controlled, phase 3 study. Lancet. 2011;378:2005–12. doi: 10.1016/S0140-6736(11)61742-X. [DOI] [PubMed] [Google Scholar]
- 18.Baselga J, Campone M, Piccart M, Burris HA, 3rd, Rugo HS, Sahmoud T, et al. Everolimus in postmenopausal hormone receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520–9. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roy HK, Olusola BF, Clemens DL, Karolski WJ, Ratashak A, Lynch HT, et al. AKT proto-oncogene overexpression is an early event during sporadic colon carcinogenesis. Carcinogenesis. 2002;23:201–5. doi: 10.1093/carcin/23.1.201. [DOI] [PubMed] [Google Scholar]
- 20.Gulhati P, Bowen KA, Liu J, Stevens PD, Rychahou PG, Chen M, et al. mTORC1 and mTORC2 regulate EMT, motility, and metastasis of colorectal cancer via RhoA and Rac1 signaling pathways. Cancer Res. 2011;71:3246–56. doi: 10.1158/0008-5472.CAN-10-4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gulhati P, Cai Q, Li J, Liu J, Rychahou PG, Qiu S, et al. Targeted inhibition of mammalian target of rapamycin signaling inhibits tumorigenesis of colorectal cancer. Clin Cancer Res. 2009;15:7207–16. doi: 10.1158/1078-0432.CCR-09-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Philp AJ, Campbell IG, Leet C, Vincan E, Rockman SP, Whitehead RH, et al. The phosphatidylinositol 3′-kinase p85alpha gene is an oncogene in human ovarian and colon tumors. Cancer Res. 2001;61:7426–9. [PubMed] [Google Scholar]
- 23.Di Nicolantonio F, Arena S, Tabernero J, Grosso S, Molinari F, Macarulla T, et al. Deregulation of the PI3K and KRAS signaling pathways in human cancer cells determines their response to everolimus. J Clin Invest. 2010;120:2858–66. doi: 10.1172/JCI37539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabatini DM. mTOR and cancer: insights into a complex relationship. Nat Rev Cancer. 2006;6:729–34. doi: 10.1038/nrc1974. [DOI] [PubMed] [Google Scholar]
- 25.Shi Y, Yan H, Frost P, Gera J, Lichtenstein A. Mammalian target of rapamycin inhibitors activate the AKT kinase in multiple myeloma cells by up-regulating the insulin-like growth factor receptor/insulin receptor substrate-1/phosphatidylinositol 3-kinase cascade. Mol Cancer Ther. 2005;4:1533–40. doi: 10.1158/1535-7163.MCT-05-0068. [DOI] [PubMed] [Google Scholar]
- 26.O’Reilly KE, Rojo F, She QB, Solit D, Mills GB, Lane H, et al. mTOR inhibition induces upstream receptor tyrosine kinase signaling and activates Akt. Cancer Res. 2006;66:1500–8. doi: 10.1158/0008-5472.CAN-05-2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hart L, Burris HA, Infante JR, Jones SF, Spigel DR, Bendell JC, et al. mTOR inhibitor everolimus (Ev) and IGFR inhibitor OSI-906 (OSI) for the treatment of patients (pts) with refractory metastatic colorectal cancer (mCRC): a Sarah Cannon Research phase 1 trial. J Clin Oncol. 2011;29:abstr e14054. [Google Scholar]
- 28.Khawaja MR, Younger A, Funke JM, Waddell MJ, Jones DR, Pollok K, et al. Phase I study of everolimus (RAD001) and AMG 479 in patients (pts) with advanced solid tumors and colorectal cancer (CRC) J Clin Oncol. 2011;29:abstr TPS157. [Google Scholar]
- 29.Altomare I, Bendell JC, Bullock KE, Uronis HE, Morse MA, Hsu SD, et al. A phase II trial of bevacizumab plus everolimus for patients with refractory metastatic colorectal cancer. Oncologist. 2011;16:1131–7. doi: 10.1634/theoncologist.2011-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]