Abstract
Objective
Children who are prenatally exposed to drugs may be at risk for emotion dysregulation, including childhood anxiety/depression and aggression, potentially increasing their risk for peer victimization. The objectives were to investigate how prenatal drug exposure relates to adolescent peer victimization and the mediating effects of childhood anxiety/depression and aggression.
Methods
76 prenatally drug exposed (PDE) and 38 non-exposed (NE) adolescent-caregiver dyads followed since birth and middle childhood, respectively, participated in an evaluation during adolescence. In middle childhood, caregivers reported on their child’s anxiety/depression and aggression, and children reported on violence exposure. In adolescence, caregivers and adolescents responded to a parallel single-item measure of peer victimization. Analyses were conducted using multivariate linear and logistic regression models, adjusting for covariates, including violence exposure.
Results
One third (33.3%, n=35) of the sample endorsed peer victimization: 40.8% PDE and 17.6% NE, p=.01. In middle childhood, PDE youth had more aggressive behaviors (11.92 vs. 7.45, p<.01) and anxiety/depression symptoms (3.43 vs. 1.76, p<.01) than NE youth. Anxious/depressed behavior during childhood mediated the association between prenatal drug exposure and adolescent peer victimization. Aggression was not a significant mediator.
Conclusions
The consequences of prenatal drug exposure extend into adolescence. Prenatal drug exposure may interfere with emotion regulation, resulting in anxious/depressed behavior during childhood, and significantly increasing the risk for peer victimization during adolescence, even in the presence of violence exposure. Strategies to reduce anxious/depressed behavior among children with a history of prenatal drug exposure may reduce adolescent peer victimization.
Key terms: prenatal drug exposure, peer victimization, emotion dysregulation, adolescence, anxiety
Urban, low income, prenatally drug exposed (PDE; cocaine/heroin), African American adolescents are at risk for multiple problems in behavior, attention, language, and cognition. Less is known about their social functioning, including peer victimization.1 From a behavioral perspective, both aggression/externalizing problems and depression/internalizing problems have been described through middle childhood.1–3 The limited research that extends to adolescence identifies a risk for aggression/externalizing behaviors 4, 5 and suggestions of an elevated risk for depression/internalizing behaviors.4, 5
Evidence from preclinical and human studies suggest that prenatal drug exposure may disrupt the neural basis of emotion regulation,6 potentially increasing the risk for multiple behavior problems and poor social functioning, including peer victimization. Disruptions in the neural pathways regulating arousal states and emotion regulation diminish the capacity for managing attentional states and executive functioning.6 As a result, information processing and learning are disrupted, interfering with socialization.6 Specifically, emotion regulation represents the capacity to respond flexibly and strategically in emotionally arousing situations, such as conflict.7 Childhood aggression and other externalizing problems have been linked to emotion dysregulation in children’s capability to regulate negative affect in interpersonal interactions.7 Children who rely on aggressive or rigid responses can be irritating to peers, particularly when they interrupt conversations, demonstrate impatience, and take turns inappropriately.8 These irritating behaviors may elicit bullying and peer victimization from peers. Thus, the aggression described among PDE children may increase their vulnerability to peer victimization.
Emotion dysregulation may also be reflected in anxiety/depression, as children avoid social interaction or exhibit awkward behavior. Children characterized as anxious or depressed are also at increased risk for peer victimization.9, 10 Since PDE increases the risk for both aggression and/or anxiety/depression,2, 3, 11 it is plausible that social interactive behaviors characteristic of emotion dysregulation increase PDE children’s risk for peer victimization.
Behavior problems may also reflect environmental exposures related to a drug-using lifestyle, including violence exposure.12, 13 Not only is violence exposure relatively common among youth with PDE, but it has been linked to multiple problem behaviors in adolescence.14
The goals of this paper are to examine the association between PDE and adolescent peer victimization and to investigate whether emotional dysregulation, characterized as aggression and/or anxiety/depression mediates that association with peer victimization, adjusting for covariates, including violence exposure. The examination was conducted using longitudinal data from a sample of PDE adolescents and caregivers and a non-exposed (NE) comparison group. We tested two hypotheses. First, we hypothesized that PDE adolescents experience more peer victimization than NE adolescents. Second, we hypothesized that emotional dysregulation, secondary to PDE and characterized as either aggression or anxious/depressed behaviors, mediates the relation with peer victimization.
METHODS
Design and Participants
This study used existing data from a randomized, controlled trial of a home-based intervention for substance abusing women and their infants beginning at delivery and tracking through middle childhood.15 Participants were recruited from an urban University Hospital and were predominantly African-American (99%). Eligibility included gestational age ≥ 32 weeks, birth weight ≥ 1,750g, no admission to the neonatal intensive care unit, and positive (cocaine and/or heroin) maternal and/or infant urine toxicology at delivery and/or maternal self-report of cocaine and/or heroin use during pregnancy. The study was conducted during a time when toxicology screens were conducted routinely. The study was approved by the University’s Institutional Review Board. Seventy-two percent of mothers (n=265) agreed to participate.16 Families were randomized to either an intervention or control group. Intervention families received developmentally-oriented home visits for 1 year. Control families received monthly tracking visits for 1 year. All families were assessed at 6-month intervals through middle childhood by research assistants who were unaware of intervention status.16
A comparison group of 70 participants from a NE cohort was recruited from a primary care clinic serving the University Hospital when the PDE participants in the original study were 5 years old. Medical records were reviewed to identify children delivered at the University Hospital at the same time as children from the PDE group who had negative toxicology screens and no evidence of substance use; 58% of mothers agreed to participate.17 Participants in the NE group resided in the same community as participants in the PDE group and were matched for socioeconomic status (i.e., maternal education), maternal age at first pregnancy, and child age, gender, and race.
During middle childhood (approximately age 7), 201 (PDE n=138, NE n=63) child-caregiver pairs were assessed. During the adolescent assessment (approximately age 14), 57% of the child-caregiver pairs in middle childhood sample was available (55% PDE, n=76 and 60% NE, n=38). Families lost to follow up did not differ from retained families on birth weight, maternal education, maternal age at first pregnancy, maternal age at the target child’s birth, neonatal abstinence scores, child gender, or receipt of public assistance. In the intervening years, there was a gap in funding, many families were reassigned to health care providers away from the University Hospital through changes in Medicaid Managed Care, and there was significant housing relocation/demolition in the study area.
Measures
Demographics
Child birth date, gender, and race were obtained from medical charts at the time of recruitment. Because caregiver changes are common among substance using women18, at each visit, the mother’s status as the primary caregiver was evaluated. As an indicator of the stability of the caregiving context during adolescence, we included the caregiver’s marital status during adolescence as a covariate.
Alcohol and Tobacco Exposure
For the PDE group, alcohol exposure was determined through a positive mother and/or baby urine sample and/or maternal self-report at delivery. Tobacco exposure was determined through maternal self-report at delivery. In the NE group, alcohol and tobacco exposure were determined thorough retrospective self-report at recruitment in middle childhood. If youth were determined to have been exposed to either alcohol or tobacco, they were categorized as alcohol/tobacco exposed.
Adolescent Peer Victimization
The Strengths and Difficulties Questionnaire (SDQ) was administered to caregivers and adolescents separately. The SDQ is a brief behavioral screening questionnaire that asks about 25 positive and negative attributes.19 Previously published investigations report that scores on the SDQ subscales (caregiver report) are correlated with scores on the Child Behavior Checklist subscales (r=0.59–0.87), indicating high validity.20 A score for peer victimization was created using a parallel item for adolescents (“Other children or young people pick on me or bully me”) and caregivers (“Is picked on or bullied by other youth”). Items were originally scored 0=Not True, 1=Somewhat True, 2=Certainly True for each respondent. For the present analyses, scores for Somewhat True and Certainly True were collapsed, resulting in dichotomous scores of Not True (0) and True (1). Adolescent and caregiver reports were combined; if either respondent endorsed peer victimization, the indicator was scored affirmatively.
Middle Childhood Aggressive Behaviors and Anxiety/Depression
The Child Behavior Checklist (CBCL)21 is a 120-item questionnaire used to assess children’s behavioral and emotional problems that was administered to caregivers in middle childhood. Each item is rated by caregivers on a 3-point scale, from Not True (0) to Sometimes True (1) to Often True (2). The behaviors are summed to form several subscales with higher scores indicating worse behavior. In the current study, we used two scales, aggressive behavior and anxious/depressed. In the standardization sample, both the aggressive behavior and anxious/depressed scales demonstrated high internal consistency among boys (Cronbach’s alpha=0.92) and girls (Cronbach’s alpha=0.86–0.88).21 The current sample demonstrated excellent internal consistency for the aggressive behavior scale (Cronbach’s alpha=0.91) and acceptable internal consistency for the anxious/depressed scale (Cronbach’s alpha=0.67).
Violence Exposure
The Things I’ve Seen and Heard-Child Scale (TISHC) measures violence a child witnesses in the home and neighborhood.22, 23 Youth completed the paper and pencil questionnaire at the middle childhood assessment. The child is asked about witnessed violence (e.g., seeing someone stabbed) and implied violence (e.g., heard gunshots) occurring in both the home and the community. Each question includes five response choices: 0, 1, 2, 3, or many times over the course of the child’s life. Higher scores indicate more violence exposure. This measure demonstrates adequate internal consistency in other samples (Cronbach’s alpha=0.74–0.76)22, 23 and in the current sample (Cronbach’s alpha=0.81).
Data Analysis
Covariates were selected based on theoretical importance and bivariate correlations with peer victimization (see Table 1). Analyses adjusted for the following covariates: prenatal alcohol and tobacco exposure, middle childhood violence exposure, caregiver changes between middle childhood and adolescent assessment, and adolescent age, gender, and caregiver marital status.
Table 1.
Intercorrelations Among Prenatal Drug Exposure, Peer Victimization, Childhood Anxiety/Depression, Childhood Aggression, and Covariates, n = 114
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| PDE status (PDE = 1; NE = 0) | 1 | ||||||||
| Prenatal alcohol and/or tobacco exposure | 0.43* | 1 | |||||||
| Adolescent age | 0.23** | 0.04 | 1 | ||||||
| Adolescent gender | −0.02 | 0.02 | −0.02 | 1 | |||||
| Caregiver marital status | 0.14 | 0.07 | 0.09 | 0.00 | 1 | ||||
| Caregiver changes | 0.29* | 0.11 | −0.03 | 0.07 | −0.09 | 1 | |||
| Childhood exposure to violence | 0.00 | −0.14 | 0.30* | 0.12 | −0.10 | 0.19 | 1 | ||
| Childhood aggression | 0.27** | 0.23** | 0.30* | −0.09 | 0.09 | 0.14 | 0.11 | 1 | |
| Childhood anxiety/depression | 0.26** | 0.07 | 0.24** | 0.07 | 0.01 | 0.04 | 0.18 | 0.61* | 1 |
| Adolescent peer victimization | 0.23** | 0.10 | 0.06 | 0.04 | −0.12 | 0.13 | 0.24** | 0.20 | 0.28** |
PDE, prenatal drug exposure; NE, nondrug exposed.
p < .01.
p < .05.
Agreements between adolescent and caregiver reports of peer victimization were examined using descriptive statistics and chi-square analyses. Hypothesis 1, the association between PDE and peer victimization, was tested by regressing peer victimization on PDE using logistic regression, adjusting for covariates. Hypothesis 2, the mediating effects of aggressive behaviors and anxiety/depression, were tested using Baron and Kenny’s24 criteria and significance tests of the indirect effect.25, 26 Mediation was considered to occur if (a) PDE predicted peer victimization, (b) PDE predicted the mediator (anxiety/depression or aggression), and (c) the effect of PDE on peer victimization was attenuated by the mediator. Given the categorical outcome and continuous mediators, both logistic and linear regressions were used in mediation models. Logistic regression was used to investigate the associations in (a) and (c), while linear regression was used to investigate the associations in (b). Coefficients from the regressions were standardized27, 28 to allow for significance tests of the indirect effects.25, 26
RESULTS
Sample Description
One hundred and fourteen adolescent-caregiver dyads participated in the adolescent assessment (Table 2). The sample was evenly divided by gender (49% male), and was predominantly African-American (99%). Overall, adolescents were a mean age of 14.05 years (SD=1.13, Range=11.93–16.20), and in middle childhood the mean age was 7.03 years (SD=.06, Range=6.93–7.31). There were no age differences in childhood; in adolescence the PDE group was significantly older than the NE group (14.26 vs. 13.67 years, p=.01). All of the NE group and 75% of the PDE group had the same caregiver at both the middle childhood and early adolescent evaluations. At the middle childhood and adolescent evaluations, 1% of PDE caregivers and none of the NE caregivers reported illegal substance use over the past 30 days; neither predicted adolescent peer victimization. Caregiver drug use was not included in further analyses.
Table 2.
Means (SDs) of Sample Characteristics and Variables of Interest
| Drug Exposed | Nondrug Exposed | P | |
|---|---|---|---|
| N | 58 | 32 | |
| Gender (% male) | 49 | 47 | ns |
| Exposed to alcohol and/or tobacco (% yes) | 87.3 | 47.1 | .001 |
| Middle childhood | |||
| Age | 7.19 (0.06) | 7.03 (0.07) | ns |
| Mother primary caregiver (% yes) | 58.3 | 100 | .001 |
| Exposure to violence (score) | 22.28 (12.78) | 22.27 (11.15) | ns |
| Exposure to ≥10 acts of violence (%) | 75 | 81.8 | ns |
| Anxiety/depression | 3.43 (3.43) | 1.76 (2.21) | .01 |
| Aggression | 11.92 (8.71) | 7.45 (6.02) | .01 |
| Early Adolescence | |||
| Age | 14.26 (1.13) | 13.67 (0.99) | .01 |
| Primary caregiver marital status (% single) | 63.6 | 52.2 | ns |
| Mother primary caregiver (% yes) | 62.3 | 100 | .001 |
| Peer victimization (% yes) | 40.8 | 17.6 | .02 |
ns, not significant
Across the sample in middle childhood, all children reported exposure to at least one act of violence, and 77% of children reported that they had been exposed to violence at least 10 times. Of children who reported violence exposure, 74% heard gun shots, 89% saw an arrest, 62% witnessed drug deals, 79% saw a beating, 40% saw a stabbing, 46% saw a shooting, 19% saw a dead body, and 13% saw a shooting or stabbing in their own home. PDE status did not differ by the violence exposure score (t(99)=.14, p>.10) or the individual acts of violence.
In middle childhood, caregivers of PDE youth reported higher scores on the CBCL, indicating more aggressive behaviors (11.92 vs. 7.45, p<.01) and anxiety/depression symptoms (3.43 vs. 1.76, p<.01) than NE youth (Table 2). In adolescence, fewer adolescents (12%, n=14) than caregivers (27%, n=28) reported peer victimization (χ2(N=104) = 5.47, p<.02). Adolescent and caregiver reports of peer victimization were statistically significantly correlated using Spearman’s rank order correlation (r=0.23, p<.02). After combining data from multiple respondents, 33.3% (n=35) endorsed peer victimization.
Covariates
Peer victimization was significantly correlated with violence exposure, anxiety/depression, and PDE status, but not with gender, adolescent age, caregiver changes or marital status (Table 1). In middle childhood, violence exposure was marginally correlated with anxiety/depression (r=.18, p=.08).
Peer victimization
Hypothesis 1 was tested using adjusted logistic regression. To test the first hypothesis, we found that youth with a history of PDE were twice as likely to experience peer victimization compared to NE youth (OR=2.01; 95% CI: 1.03, 3.95, p=.04; see Table 3), adjusting for covariates. Exposure to violence was the only covariate statistically significantly associated with peer victimization (see Table 3). The significant association between PDE and peer victimization is step (a) in the mediation models tested in the second hypothesis.
Table 3.
Logistic Regression Models Predicting Peer Victimization by PDE With and Without Childhood Anxiety/Depression
| Direct Effects of PDE (Without Anxiety/Depression)
|
Indirect Effects of PDE (With Anxiety/Depression)
|
|||||
|---|---|---|---|---|---|---|
| b (SE) | 95% CI | OR | b (SE) | 95% CI | OR | |
| Prenatal alcohol and/or tobacco exposure | 0.23 (0.36) | 0.66, 2.70 | 1.33 | 0.34 (0.37) | 0.68, 2.89 | 1.40 |
| Adolescent age | −0.15 (0.25) | 0.53, 1.39 | 0.86 | −0.22 (0.26) | 0.49, 1.32 | 0.80 |
| Adolescent gender | 0.36 (0.49) | 0.55, 3.79 | 1.44 | 0.30 (0.51) | 0.50, 366 | 1.36 |
| Childhood exposure to violence | 0.05 (0.02) | 1.01, 1.10 | 1.05* | 0.05 (0.02) | 1.01, 1.10 | 1.05* |
| Caregiver marital status | −0.46 (0.30) | 0.36, 1.13 | 0.63 | −0.49 (0.31) | 0.61, 0.33 | 0.61 |
| Caregiver changes | −0.21 (0.72) | 0.20, 3.32 | 0.81 | −0.12 (0.73) | 0.21, 3,72 | 0.89 |
| Childhood anxiety/depression | — | — | — | 0.14 (0.08) | 0.99, 1.34 | 1.15 |
| PDE (PDE = 1; NE = 0) | 0.70 (0.34) | 1.03, 3.95 | 2.01* | 0.60 (0.36) | 0.90, 3.67 | 1.82 |
PDE, prenatal drug exposure; NE, nondrug exposed; CI, confidence interval; OR, odds ratio.
p < .05.
Aggressive Behaviors
To test the second hypothesis, we found that PDE did not predict aggression in middle childhood (b=0.78, p>.40). Therefore, the conditions for mediation were not met and the subsequent steps of mediation testing were not conducted. Violence exposure was significantly associated with peer victimization in the multivariate model (b=.05, p<.05).
Anxiety/depression
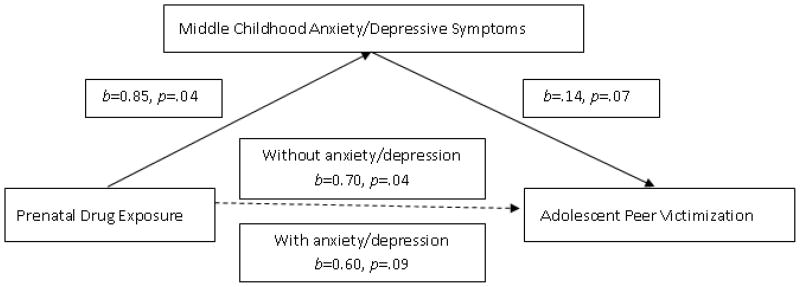
We examined whether anxiety/depression in middle childhood mediated the association between PDE and peer victimization, adjusting for covariates. Using linear regression, step (b) conditions were met with PDE significantly predicting anxiety/depression (b=0.85, p=.04). Using logistic regression, Step (c) conditions of mediation were met because when anxiety/depression was included in the model to predict peer victimization, the association with PDE was attenuated (b=0.60, p=.09; Table 3; Figure 1). After standardizing the coefficients between linear and logistic regressions,25 the test of the indirect effect was statistically significant (z′=1.35, p<.05). Violence exposure was the only other covariate significantly associated with peer victimization in the multivariate model (see Table 3).
Figure 1. Middle Childhood Anxiety/Depression Mediates the Association Between Prenatal Drug Exposure and Adolescent Peer Victimization.
Note. All analyses control for prenatal alcohol and tobacco exposure, adolescent age, adolescent gender, caregiver marital status, caregiver changes, and exposure to neighborhood violence in middle childhood.
DISCUSSION
These findings illustrate that the consequences of PDE extend through childhood and into adolescence. Not only are adolescents with a history of PDE at increased likelihood of experiencing peer victimization (40.8% vs. 17.6%), but the association between PDE and adolescent peer victimization is explained by childhood anxiety/depression.
During middle childhood, caregivers reported higher rates of childhood anxiety/depression among the PDE group, compared to the NE group, consistent with findings reported by other investigators.2, 5 Anxiety/depression symptoms often correlate with peer victimization, making it difficult to determine causality. However, by testing how middle childhood anxiety/depression relates to later adolescent peer victimization, we ascertained temporality. Symptoms of anxiety/depression represent an inability to effectively regulate emotions. The behavioral manifestations of anxiety/depression, which often include social avoidance or awkwardness, appear to increase youths’ vulnerability to peer victimization.9, 10 These findings suggest that childhood emotion dysregulation in the form of anxiety/depression, together with the resulting behaviors that interfere with interpersonal relations, are important mechanisms in linking PDE exposure with adolescent peer victimization.
The finding that aggressive behavior in middle childhood did not mediate the association between PDE and peer victimization was unexpected. Previous research suggests that PDE predicts aggression and other symptoms of emotion dysregulation1, 6, possibly related to the effects of PDE on neural substrates.6 In bivariate relations, PDE youth had significantly higher rates of aggressive behaviors than NE adolescents. However, in a multivariate, covariate-adjusted model, PDE did not predict childhood aggressive behaviors, suggesting that once environmental factors are considered, PDE does not play a direct role in childhood aggression. There are several additional possible explanations for the absence of a PDE-aggressive behavior relationship. One possibility is that aggressive children may misidentify or underreport their own victimization because emotion dysregulation may cause youth to have difficulty interpreting threats from peers as victimization. Alternatively, children who exhibit aggressive behavior may be more likely to perpetrate victimizing behavior than to be the recipient of victimization. Additionally, violence exposure was a significant predictor of peer victimization, and this might be an explanatory variable. Violence exposure might be explored further in subsequent research. Finally, caregivers of aggressive children may report aggression, rather than peer victimization, because aggression is more easily recognizable and typically of more immediate concern than peer victimization, which may be covert.
PDE was not associated with violence exposure, but violence exposure was common among the youth in this sample, ranging in severity from hearing adults in the house yell at each other to seeing someone shot. Youth were reared in similar neighborhoods, and it is likely that, regardless of PDE status, they witnessed similar acts of violence within their neighborhoods and schools. Findings from the National Survey of Children’s Exposure to Violence indicate that violence exposure is relatively common in middle childhood, with 16% of 6 to 9 year olds witnessing family assault and 14% witnessing assault in the community.29 Rates of violence exposure are even higher among urban, low-income children; for example, in one sample of African American youth ages 7 to 9 living in public housing, 28% had witnessed a shooting and 26% had witnessed a stabbing.30 In this sample, violence exposure during middle childhood was a significant predictor of adolescent peer victimization in both models. This finding is consistent with findings reported by others.13, 31–33 Trauma associated with violence exposure may disrupt the development of emotion regulation and condition youth to be victimized. Previous research indicates that the stress, anxiety, and fear generated by violence exposure interferes with the development of trust, sense of safety, regulations of emotions, explorations of the environment, and the ability to form social relationships.32, 33 Our findings illustrate that even in the presence of substantial violence exposure, PDE exposure increases the risk of peer victimization during adolescence, mediated through anxiety/depression during childhood. Future research might further explore the role of violence exposure and how it relates to aggression, anxiety/depression, and peer victimization because it is possible that violence exposure moderates the association between PDE and aggression, anxiety/depression and peer victimization.
Limitations to the current study should be considered when interpreting the findings. First, although peer victimization was measured with a single item, responses were gathered from both caregivers and adolescents. Further qualitative and quantitative research on peer victimization utilizing more comprehensive assessments is warranted. These findings are significant because there is currently very little research examining the social development of PDE adolescents, but the findings should be treated as preliminary until replicated. Second, PDE and peer victimization were associated, and there may be a change in underlying neural strata that causes symptoms of emotion dysregulation (i.e., anxiety/depression) to emerge and interfere with social functioning.6 This study demonstrates the need to conceptualize emotion dysregulation as a potential mechanism linking PDE with childhood and possibly adolescent behavioral problems. Alternatively, the association between PDE and peer victimization might be explained through unmeasured family and environmental conditions associated with a drug-using lifestyle (i.e., violence exposure or caregiver continued drug use). Third, the relationship between peer victimization and bullying needs to be explored further. Many victimized children engage in bullying, suggesting that peer victimization and bullying are inter-related.34 Bullying was not measured in this study, but should be examined in future research to examine how emotion dysregulation and environmental conditions relate to the victimization/bullying process in PDE youth. Fourth, the samples were recruited at differing times; the PDE sample responded to questions about their children’s prenatal tobacco exposure shortly after delivery and the NE sample had to recall their child’s prenatal tobacco exposure over several years, raising concerns about recall bias. Finally, the small sample size and high attrition suggest that the study should be replicated in a larger sample of youth varying in PDE. The homogeneity of the high risk sample limits generalization to other populations. The findings linking violence exposure during middle childhood with peer victimization during adolescence were present, regardless of PDE status, underscoring concerns about the effects of urban violence on children’s development.29
Additionally, there are several strengths to consider. This study relied on theory (i.e., emotion regulation) to formulate hypotheses. The longitudinal study design, including well characterized samples of PDE and NE groups, based on toxicology screens, maternal report, and medical record review, enabled us to examine both the effects of prenatal drug exposure on distal factors in adolescence, and also the intervening role of middle childhood behavior, while adjusting for environmental factors. This design allows for understanding the impact of multiple factors throughout children’s development. The use of multiple informants (caregivers and youth) enabled the construction of strong models that are not biased by single perceptions of the behavior and environment. Finally, the inclusion of violence exposure allowed for the examination of an important contextual factor that many urban children, regardless of PDE status, experience.
Clinical Implications.
There are important clinical implications of this study. Strategies to prevent anxiety and depressive symptoms among PDE children may enable them to develop more adaptive emotion regulation and protect them from peer victimization during adolescence. For children identified with existing anxiety and depressive symptoms, therapy would allow them to identify ways to self-regulate, identify their negative feelings, and adopt adaptive coping strategies may prevent peer victimization.35, 36 Interventions that include the peer context and the larger environment31, 37 and specific training in how to understand and interpret social cues38 may be particularly effective in protecting youth from peer victimization. By learning appropriate emotion regulation strategies regarding feelings of anxiety or depression, youth may be able to avoid negative interactions with peers and thus, avoid subsequent peer victimization.
Acknowledgments
Funding: This study was supported by the National Institute of Drug Abuse (R01-DA07432 and R01-DA021059).
Footnotes
Disclaimer: The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the U.S. Department of Health and Human Services.
References
- 1.Lester BM, Lagasse LL. Children of addicted women. Journal of Addictive Diseases. 2010;29:259–276. doi: 10.1080/10550881003684921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bada HS, Das A, Bauer CR, et al. Impact of prenatal cocaine exposure on child behavior problems through school age. Pediatrics. 2007;119:e348–59. doi: 10.1542/peds.2006-1404. [DOI] [PubMed] [Google Scholar]
- 3.Chasnoff IJ, Anson A, Hatcher R, Stenson H, Iaukea K, Randolph LA. Prenatal exposure to cocaine and other drugs. Outcome at four to six years. Ann N Y Acad Sci. 1998;846:314–328. [PubMed] [Google Scholar]
- 4.Whitaker TM, Bada HS, Bann CM, et al. Serial Pediatric Symptom Checklist screening in children with prenatal drug exposure. Journal of Developmental and Behavioral Pediatrics. 2011;32:206–215. doi: 10.1097/DBP.0b013e318208ee3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bada HS, Bann CM, Bauer CR, et al. Preadolescent behavior problems after prenatal cocaine exposure: Relationship between teacher and caretaker ratings (Maternal Lifestyle Study) Neurotoxicol Teratol. 2011;33:78–87. doi: 10.1016/j.ntt.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayes LC. A behavioral teratogenic model of the impact of prenatal cocaine exposure on arousal regulatory systems. Neurotoxicol Teratol. 2002;24:385–395. doi: 10.1016/s0892-0362(02)00200-3. [DOI] [PubMed] [Google Scholar]
- 7.Cole PM, Michel MK, Teti LO. The development of emotion regulation and dysregulation: a clinical perspective. Monogr Soc Res Child Dev. 1994;59:73–100. [PubMed] [Google Scholar]
- 8.Greene M. Bullying and harassment in schools. In: Moser R, Franz C, editors. Shocking Violence: Youth Perpetrators and Victims-A Multidisciplinary Perspective. Springfield: Charles C. Thomas; 2000. pp. 72–101. [Google Scholar]
- 9.Siegel RS, La Greca AM, Harrison HM. Peer victimization and social anxiety in adolescents: prospective and reciprocal relationships. J Youth Adolesc. 2009;38:1096–1109. doi: 10.1007/s10964-009-9392-1. [DOI] [PubMed] [Google Scholar]
- 10.Sweeting H, Young R, West P, Der G. Peer victimization and depression in early-mid adolescence: a longitudinal study. Br J Educ Psychol. 2006;76:577–594. doi: 10.1348/000709905X49890. [DOI] [PubMed] [Google Scholar]
- 11.Sood B, Delaney-Black V, Covington C, et al. Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. dose-response effect. Pediatrics. 2001;108:E34. doi: 10.1542/peds.108.2.e34. [DOI] [PubMed] [Google Scholar]
- 12.The National Center on Addiction and Substance Abuse at Columbia University. Family Matters: Substance Abuse and the American Family. New York, NY: Columbia University; 2005. [Google Scholar]
- 13.Jones DJ, Foster S, Forehand G, O’Connell C. Neighborhood Violence and Psychosocial Adjustment in Low-Income Urban African American Children: Physical Symptoms as a Marker of Child Adjustment. J Child Fam Stud. 2005;14:237–249. [Google Scholar]
- 14.Frank DA, Rose Jacobs R, Crooks D, et al. Adolescent initiation of licit and illicit substance use: Impact of intrauterine exposures and post-natal exposure to violence. Neurotoxicol Teratol. 2011;33:100–109. doi: 10.1016/j.ntt.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuler ME, Nair P, Black MM. Ongoing maternal drug use, parenting attitudes, and a home intervention: effects on mother-child interaction at 18 months. J Dev Behav Pediatr. 2002;23:87–94. doi: 10.1097/00004703-200204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schuler ME, Nair P, Black MM, Kettinger L. Mother-infant interaction: effects of a home intervention and ongoing maternal drug use. J Clin Child Psychol. 2000;29:424–431. doi: 10.1207/S15374424JCCP2903_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nair P, Black MM, Ackerman JP, Schuler ME, Keane VA. Children’s cognitive-behavioral functioning at age 6 and 7: prenatal drug exposure and caregiving environment. Ambul Pediatr. 2008;8:154–162. doi: 10.1016/j.ambp.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown JV, Bakeman R, Coles CD, Platzman KA, Lynch ME. Prenatal cocaine exposure: a comparison of 2-year-old children in parental and nonparental care. Child Dev. 2004;75:1282–1295. doi: 10.1111/j.1467-8624.2004.00739.x. [DOI] [PubMed] [Google Scholar]
- 19.Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 20.Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: is small beautiful? J Abnorm Child Psychol. 1999;27:17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- 21.Achenbach T. Manual for the Child Behavior Checklist and 1991 Profile. Burlington, VT: University of Vermont; 1990. [Google Scholar]
- 22.Richters JE, Martinez PE. Violent communities, family choices, and children’s chances: An algorithm for improving the odds. Dev Psychopathol. 1993;5:609–627. [Google Scholar]
- 23.Richters JE, Martinez PE. Things I have seen and Heard: An Interview for Young Children about Exposure to Violence. Rockville, MD: Child and Adolescent Disorders Research Branch, National Institute of Mental Health; 1990. [Google Scholar]
- 24.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sobel S. Asymptotic intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociolocial Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- 27.MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 28.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- 29.Finkelhor D, Turner H, Ormrod R, Hamby S, Kracke K. Children’s exposure to violence: A comprehensive national survey. U.S. Department of Justice: Office of Juvenile Justice and Delinquency Prevention; 2009. [Google Scholar]
- 30.Sheehan K, DiCara JA, LeBailly S, Christoffel KK. Children’s exposure to violence in an urban setting. Arch Pediatr Adolesc Med. 1997;151:502–504. doi: 10.1001/archpedi.1997.02170420072012. [DOI] [PubMed] [Google Scholar]
- 31.Osofsky JD. The impact of violence on children. The Future of Children. 1999;9:33–49. [PubMed] [Google Scholar]
- 32.Salzinger S, Feldman RS, Stockhammer T, Hood J. An ecological framework for understanding risk for exposure to community violence and the effects of exposure on children and adolescents. Aggression and Violent Behavior. 2002;7:423–451. [Google Scholar]
- 33.Kelly BM, Schwartz D, Gorman AH, Nakamoto J. Violent victimization in the community and children’s subsequent peer rejection: the mediating role of emotion dysregulation. J Abnorm Child Psychol. 2008;36:175–185. doi: 10.1007/s10802-007-9168-6. [DOI] [PubMed] [Google Scholar]
- 34.Olweus D. Bullying at School: What we Know and what we can do. Oxford, UK: Blackwell; 1993. [Google Scholar]
- 35.DuRant RH, Treiber F, Getts A, McCloud K, Linder CW, Woods ER. Comparison of two violence prevention curricula for middle school adolescents. J Adolesc Health. 1996;19:111–117. doi: 10.1016/1054-139X(96)00030-4. [DOI] [PubMed] [Google Scholar]
- 36.Williams M, Shellenbarger S. How does Your Engine Run? A leader’s Guide to the Alert Program for Self-Regulation. Albuquerque, NM: Therapy Works; 1994. [Google Scholar]
- 37.Blechman E, Dumas J, Prinz R. Prosocial coping by youth exposed to violence. Journal of Child and Adolescent Group Therapy. 1994;4:205–227. [Google Scholar]
- 38.O’Connor MJ, Frankel F, Paley B, et al. A controlled social skills training for children with fetal alcohol spectrum disorders. J Consult Clin Psychol. 2006;74:639–648. doi: 10.1037/0022-006X.74.4.639. [DOI] [PMC free article] [PubMed] [Google Scholar]