Abstract
Inspiration of a high concentration of oxygen, a therapy for acute lung injury (ALI), could unexpectedly lead to reactive oxygen species (ROS) production and hyperoxia-induced acute lung injury (HALI). Nucleotide-binding domain and leucine-rich repeat PYD-containing protein 3 (NLRP3) senses the ROS, triggering inflammasome activation and interleukin-1β (IL-1β) production and secretion. However, the role of NLRP3 inflammasome in HALI is unclear. The main aim of this study is to determine the effect of NLRP3 gene deletion on inflammatory response and lung epithelial cell death. Wild-type (WT) and NLRP3−/− mice were exposed to 100% O2 for 48–72 h. Bronchoalveolar lavage fluid and lung tissues were examined for proinflammatory cytokine production and lung inflammation. Hyperoxia-induced lung pathological score was suppressed in NLRP3−/− mice compared with WT mice. Hyperoxia-induced recruitment of inflammatory cells and elevation of IL-1β, TNFα, macrophage inflammatory protein-2, and monocyte chemoattractant protein-1 were attenuated in NLRP3−/− mice. NLRP3 deletion decreased lung epithelial cell death and caspase-3 levels and a suppressed NF-κB levels compared with WT controls. Taken together, this research demonstrates for the first time that NLRP3-deficient mice have suppressed inflammatory response and blunted lung epithelial cell apoptosis to HALI.
Keywords: hyperoxia, inflammation, injury, lung, reactive oxygen species
acute lung injury (ALI) is characterized by severe alveolar damage resulting from an acute inflammatory response that leads to proinflammatory cytokine production, neutrophil, macrophage infiltration, and edema. The most severe form of ALI is acute respiratory distress syndrome (ARDS), which is a major cause for admission to critical care units. Hyperoxia therapy is a necessary part of treatment for patients with acute and chronic cardiovascular and pulmonary diseases. However, prolonged exposure to hyperoxia could deteriorate ALI (19, 47). Currently, there are several animal models available to study the mechanism of ALI. The hyperoxia-induced acute lung injury (HALI) animal model became widely used to study human ALI after Cochrane et al. (7) revealed the increase of oxidants in the lungs of patients with ARDS. It is now well established that there are clinically relevant similarities between the animal model of HALI and human lung injury (26). However, the molecular mechanisms that initiate and amplify the lung inflammation in response to inhaled oxygen are not well understood.
IL-1β is one of the most potent early cytokines found in ALI patients, and it induces the production of other cytokines (12). The proinflammatory cytokine IL-1β is also known to be one of the most biologically important inflammatory mediators in the air space of patients with early ALI (35). Interestingly, IL-1β can also act as an important activator and prosurvival cytokine for neutrophils (37). However, mechanisms that initiate IL-1β processing in ALI are not clearly defined.
Martinon et al. (25) first reported in 2002 that caspase-1-mediated processing of IL-1β is mediated by the nucleotide-binding domain and leucine-rich repeat PYD-containing protein 3 (NLRP3) inflammasome. The NLRP3 inflammasome is a multiprotein complex, which contains NLRP3, the caspase recruitment domain containing protein Cardinal, apoptosis-associated speck-like protein (ASC), and caspase-1 (33). NLRP3 inflammasome is implicated in sensing stress caused by reactive oxygen species (9, 32). Recently we showed that hyperoxia induces inflammasome activation (21, 22). However, whether inhibition or deletion of NLRP3 inflammasome is critical to confer protection against HALI has not been studied yet. Since the HALI model is thoroughly characterized in terms of reactive oxygen species involvement, assessing the effect of NLRP3 deletion on HALI will provide important information about how NLRP3 plays a role in HALI and might result in novel therapeutic strategies to treat ALI. In this study for the first time we used NLRP3-deficient mice to identify the role of inflammasomes in hyperoxia-induced lung injury.
MATERIALS AND METHODS
Mice.
The University of South Florida Institutional Animal Care and Use Committee (IACUC) approved all animal procedures. NLRP3 knockout mice (gift from Dr. Vishva Dixit, Genentech, San Francisco, CA) and C57BL/6J mice (Harlan Laboratories, Indianapolis, IN) were used to conduct in vivo experiments. NLRP3 −/− mice were derived from C57BL/6J strain.
Mice, aged 7–9 wk, were used in all experiments. Mice were placed in cages in a chamber (75×50×50 cm) and exposed to 100% O2 for 48 or 72 h. The oxygen concentration in the chamber was monitored and regulated with the proOx P100 sensor (BioSpherix). Mice were euthanized 48 or 72 h after exposure to 100% O2 for sample collection.
Lung perfusion and tissue collection.
Mice were anesthetized by an intraperitoneal injection of ketamine/xylazine mixture. Postmortem, the abdominal cavity was opened, and the inferior vena cava (IVC) was severed for blood removal. Following thoracotomy, the IVC was clamped just above the diaphragm and then the lungs were perfused through the right ventricle. The left lower lobe of the lung was removed and fixed in 10% buffered formalin for standard histological processing and paraffin embedding (FFPE). The remaining portion of the lungs was cut into several pieces and stored in an ultralow temperature freezer.
Bronchoalveolar lavage analysis.
Blood was removed from the IVC, as described previously, followed by a small transverse incision in the skin of the ventral neck. The trachea was exposed, a catheter was inserted, and a whole lung lavage was performed by using sterile PBS. Bronchoalveolar lavage (BAL) fluid, (2–3 ml), was centrifuged at 400 g for 10 min at 4°C. Cell pellets were resuspended in 1 ml of ice-cold sterile PBS. The total number of cells in the cell suspension was counted using a disposable hemocytometer. Aliquots, 200–400 μl, of cell suspension were centrifuged onto glass slides at 800 rpm for 3 min in a cytocentrifuge (Shandon Cytospin 2, Pittsburgh, PA). The cytospined cells were stained with Diff-Quik stain set (Andwin Scientific, Schaumburg, IL), and a differential white blood cell count was performed (200 cells).
ELISA.
The levels of IL-1β, monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-2 (MIP-2; eBioscience, San Diego, CA), TNF-α (RayBiotech, Norcross, GA), and IL-6 (BD Biosciences, San Diego, CA) in BAL fluid were measured using commercial ELISA kits as per the manufacturer's instructions.
Histology and evaluation of lung injury.
FFPE lung tissue sections were stained with hematoxylin and eosin, and the extent of lung injury was evaluated. Evaluation of the lung tissue pathological severity was performed in a blinded manner following the methods described previously (17, 45) by independently scoring four parameters: alveolar congestion, hemorrhage, aggregation of neutrophil or leukocyte infiltration, and thickness of the alveolar wall. 0: no lung abnormalities; 1: lesions involving <25% of the lung; 2: lesions involving 25–50% of the lung; 3: lesions involving 50–75% of the lung; and 4: lesions involving 75% or more of the lung. The total histopathological score was expressed as the sum of the scores for all parameters.
Terminal deoxynucleotidyl transferase dUTP-mediated nick-end labeling staining on lung tissue sections.
Terminal deoxynucleotidyl transferase dUTP-mediated nick-end labeling (TUNEL) staining was performed on FFPE lung tissue sections using the in situ apoptosis detection kit (TaKaRa Biomedicals, Tokyo, Japan) according to the manufacturer's instructions with some modifications. Briefly, the lung tissue sections were deparaffinized and then incubated with 20 μg/ml proteinase K for 40 min at 37°C to unmask antigen binding sites. After being blocked with 3% hydrogen peroxide in PBS, the sections were incubated with TdT enzyme and FITC-labeled dUTP for 90 min at 37°C. Subsequently, the sections were incubated with anti-FITC horseradish peroxidase conjugate for 60 min at 37°C. Colorimetric detection of apoptotic cells was performed using 3,3′-diaminobenzidine reagent.
Lung homogenization.
Lung tissue samples were thawed on ice and homogenized using a PowerGen 500 homogenizer (Fisher Scientific, Pittsburgh, PA). For protein extraction, lysis buffer (20 mM Tris·HCl, pH 7.4, 150 mM NaCl, and 0.5% Triton X-100) was supplemented with protease and phosphatase inhibitors (Sigma-Aldrich, St. Louis, MO). After two freeze-thaw cycles, the lung homogenates were centrifuged at 15,000 g for 10 min at 4°C. Supernatants were collected and stored at −80°C until use.
Western blotting.
Supernatants from lung homogenates were boiled in Laemmli 4× SDS sample buffer (Boston BioProducts, Worcester, MA), and equal amounts of protein were subjected to SDS-PAGE. Proteins were then transferred onto polyvinylidene difluoride membranes. The membranes were blocked in Tris-buffered saline (20 mM Tris·HCl at pH 7.5 and 150 mM NaCl) with 0.1% Tween 20 (TBS-T) containing 5% skim milk and then incubated with anti-NF-κB, anti-phosphor-NF-κB antibody, anti-cleaved casp-3 antibody (Cell Signaling Technology, Beverly, MA), or anti-caspase-1 p10 antibody (Santa Cruz Biotechnology, Dallas, TX). The membranes were washed with TBS-T and incubated with horseradish peroxidase-conjugated secondary antibody for 30 min at room temperature. Following TBS-T washes, the proteins were visualized using Pierce ECL Western blotting substrate (Thermo Fisher Scientific, Hudson, NH).
Statistical analysis.
Statistical analysis was performed with GraphPad Prism 5 (GraphPad Software, San Diego, CA). Comparison of continuous variables between two groups was performed using the Student's t-test, while total histopathological scores were compared using the Mann-Whitney U test. All tests were two-tailed, and values of P < 0.05 were considered significant.
RESULTS
Effect of hyperoxia and NLRP3 deletion on lung histology.
Hematoxylin-eosin-stained lung tissue sections obtained from wild-type (WT) and NLRP3−/− mice exposed to 100% O2 for 48 h were compared to determine if NLRP3 deletion ameliorates oxygen toxicity. Hyperoxia-exposed WT mice show diffuse pathological changes characterized by alveolar congestion and inflammatory cell infiltration into the air space. However, these changes are suppressed in NLRP3−/− mice (Fig. 1A). Evaluation of pathological severity of the lung, as performed by independently scoring four parameters, shows a significant decrease in total histopathological score in NLRP3−/− compared with WT mice (Fig. 1B). These results suggest that NLRP3−/− mice are resistant to hyperoxia-induced ALI.
Fig. 1.
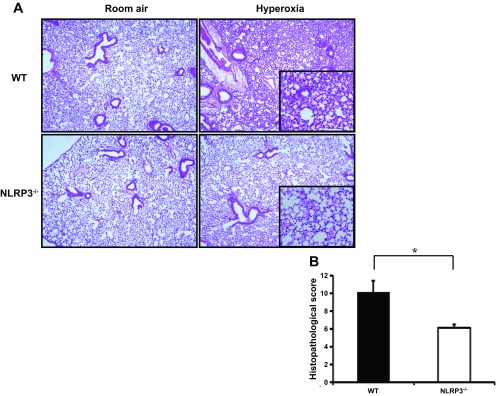
Hyperoxia-exposed Nucleotide-binding domain and leucine-rich repeat PYD-containing protein 3-deficient (NLRP3−/−) mice show attenuated lung injury. wild-type (WT) and NLRP3−/− mice were exposed to room air or 100% O2 for 48 h. Mice were euthanized and lung tissues were collected. A: representative hematoxylin-eosin (H&E)-stained lung tissue sections. Original magnifications: ×40 (insets, ×100). B: semiquantitative lung injury analysis by evaluation of H&E-stained lung tissue sections. Total histopathological score was expressed as summed scores for 4 independent parameters: alveolar congestion, hemorrhage, aggregation of neutrophil or leukocyte infiltration, and thickness of the alveolar wall. Results (means ± SE; n = 8 in each group) are cumulative data of 2 independent experiments. *P < 0.05.
Hyperoxia-induced recruitment of inflammatory cells and elevation of MCP-1 is attenuated in NLRP3−/− mice.
Quantification of total number of cells recovered from BAL fluid is useful to evaluate alveolitis in hyperoxia-induced murine models (38). Results show that the total number of cells in BAL fluid obtained from NLRP3−/− mice exposed to 100% O2 is significantly decreased compared with their WT controls (Fig. 2A). Macrophages are the most abundant immune cells in lung parenchyma (5). Activation of these alveolar macrophages in lungs is regulated by different cytokines and inflammatory mediators (13, 23). The number of macrophages present in BAL fluid was assessed by performing total and differential cell counts. The results show that total number of macrophages in BAL fluid in NLRP3−/− mice exposed to 100% O2 for 72 h is significantly lower compared with WT mice (Fig. 2B). MCP-1 is known to be a potent chemoattractant mainly acting on monocytes/macrophages (18). MCP-1 concentrations in BAL fluid obtained from WT and NLRP3−/− mice exposed to 100% O2 for 72 h were measured to determine whether suppressed macrophage recruitment in NLRP3−/− mice is related to a decrease in MCP-1 levels in BAL fluid. The results show that hyperoxia-induced elevated MCP-1 levels in WT mice (means ± SE; 189.9 ± 16.4 pg/ml) is significantly suppressed in NLRP3−/− mice (111.6 ± 8.3 pg/ml), consistent with decreased macrophage infiltration (Fig. 2C). These results suggest that hyperoxia-induced immune cell infiltration and MCP-1 secretion in lung are, at least in part, under the control of the NLRP3 inflammasome activation.
Fig. 2.

Hyperoxia-induced recruitment of inflammatory cells and elevation of monocyte chemoattractant protein-1 (MCP-1) were attenuated in NLRP3−/− mice. WT and NLRP3−/− mice were exposed to room air or 100% O2 for 72 h and euthanized, and bronchoalveolar lavage fluid (BALF) was collected. A: total cell counts. B: total number of macrophages. Results of A and B (means ± SE; n = 4 in each group) are representative of 2 independent experiments. C: levels of MCP-1 were measured by ELISA. Results (means ± SE; n = 4 in each group for normoxia; n = 8 in each group for hyperoxia) are cumulative data of 2 independent experiments. *P < 0.05 **P < 0.01.
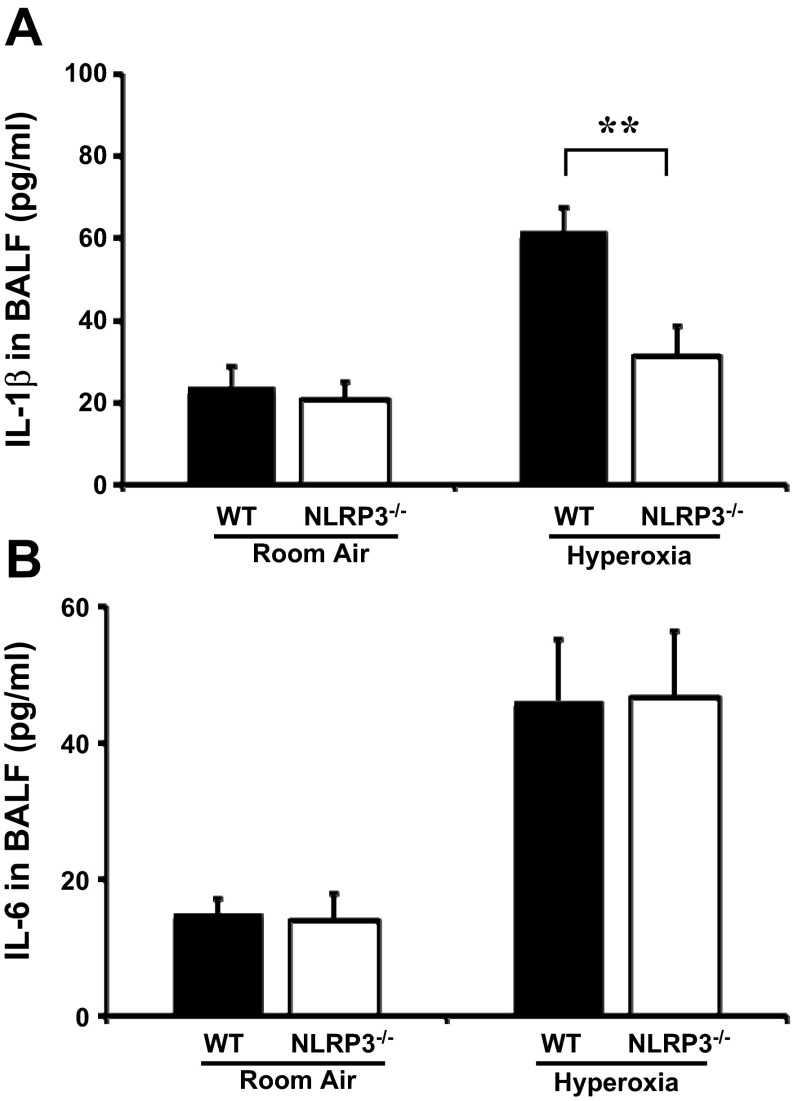
Hyperoxia-induced elevation of IL-1β is NLRP3 dependent.
IL-1β is one of the most potent cytokines in the lungs of early ALI patients (12, 50). Although inflammasome-mediated IL-1β processing is involved in a variety of inflammatory diseases, its significance in HALI has not been studied. WT and NLRP3−/− mice were exposed to hyperoxia for 72 h, and IL-1β levels in BAL fluid was measured by ELISA to determine whether IL-1β processing in HALI occurs through NLRP3 inflammasome activation. Results show that hyperoxia induces elevated IL-1β levels in WT mice (61.5 ± 5.8 pg/ml). However, this elevation was significantly suppressed in NLRP3−/− mice (31.2 ± 7.3 pg/ml; Fig. 3A). Additionally, levels of IL-6, another major proinflammatory cytokine in HALI were measured. Results show that hyperoxia-induced IL-6 elevation in BAL fluid seen in WT mice (46.1 ± 9.0 pg/ml) is not altered in NLRP3−/− mice (46.6 ± 9.8 pg/ml; Fig. 3B). These results suggest that IL-1β secretion in HALI is NLRP3 dependent.
Fig. 3.
Hyperoxia-induced elevation of IL1-β is NLRP3 dependent. WT and NLRP3−/− mice exposed to room air or 100% O2 for 72 h were euthanized and BALF was collected. IL-1β (A) and IL-6 (B) concentrations in BALF were measured by ELISA. Results (means ± SE; n = 4 in each group for normoxia; n = 7–8 in each group for hyperoxia) are cumulative data of 2 independent experiments. **P < 0.01.
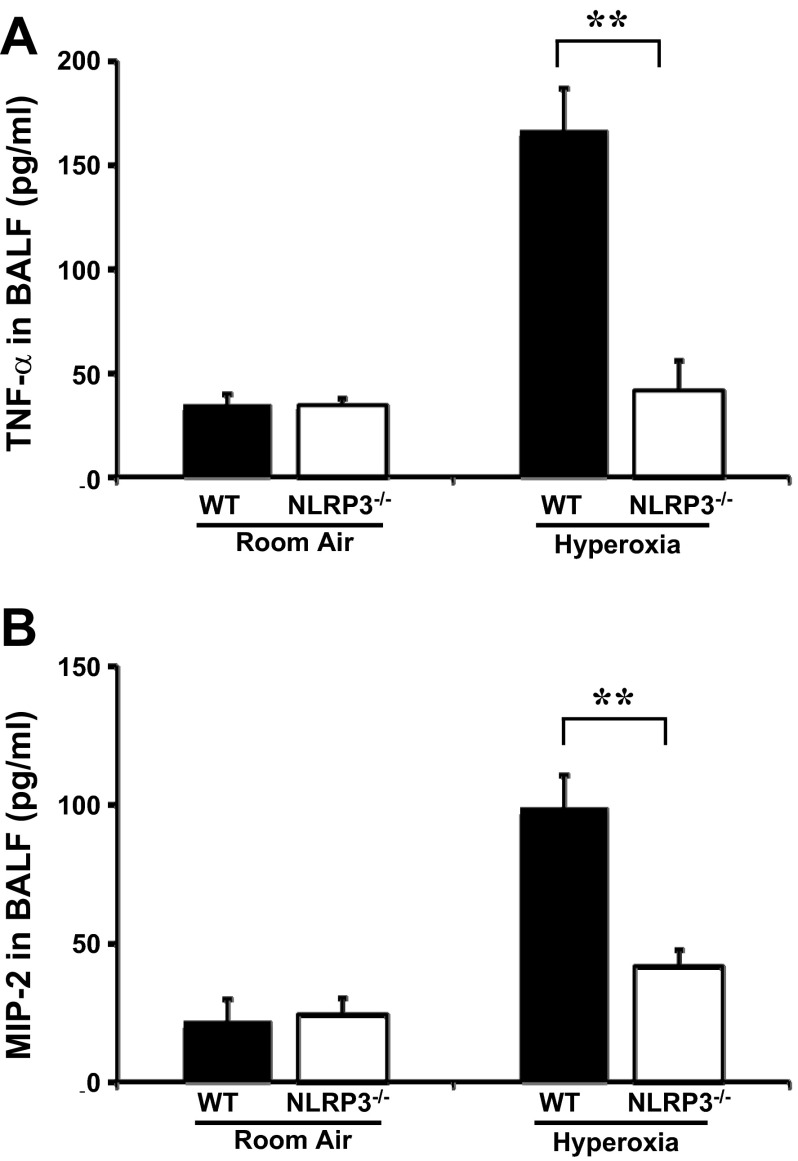
Hyperoxia-induced expression of TNF-α and MIP-2 is suppressed in NLRP3−/− mice.
TNF-α is the most widely studied proinflammatory cytokine member of the TNF super family and is recognized as a mediator of the pulmonary inflammatory response (30). TNF-α concentrations in BAL fluid obtained from WT and NLRP3−/− mice exposed to 100% O2 for 72 h were measured. Results show that hyperoxia-induced TNF-α elevation in BAL fluid is significantly suppressed in NLRP3−/− mice (41.0 ± 14.9 pg/ml) compared with WT mice (166.4 ± 20.3 pg/ml; Fig. 4A). MIP-2, a functional homologue of human IL-8, is known to be chemotactic for neutrophils in ALI (41, 46). MIP-2 levels in BAL fluid obtained from mice exposed to 100% O2 for 72 h were measured to check whether protection of NLRP3−/− mice is accompanied by modulation of MIP-2. Results show that MIP-2 levels in hyperoxia-induced WT mice (98.7 ± 11.9 pg/ml) were significantly higher compared with NLRP3−/− mice (41.5 ± 5.9 pg/ml; Fig. 4B).
Fig. 4.
Hyperoxia-induced elevation of TNF-α and macrophage inflammatory protein-2 (MIP-2) is suppressed in NLRP3−/− mice. WT and NLRP3−/− mice exposed to room air or 100% O2 for 72 h were euthanized and BALF was collected. TNF-α (A) and MIP-2 (B) concentrations were measured by ELISA. Results (means ± SE; n = 4 in each group for normoxia, n = 8 in each group for hyperoxia) are cumulative data of 2 independent experiments. **P < 0.01.
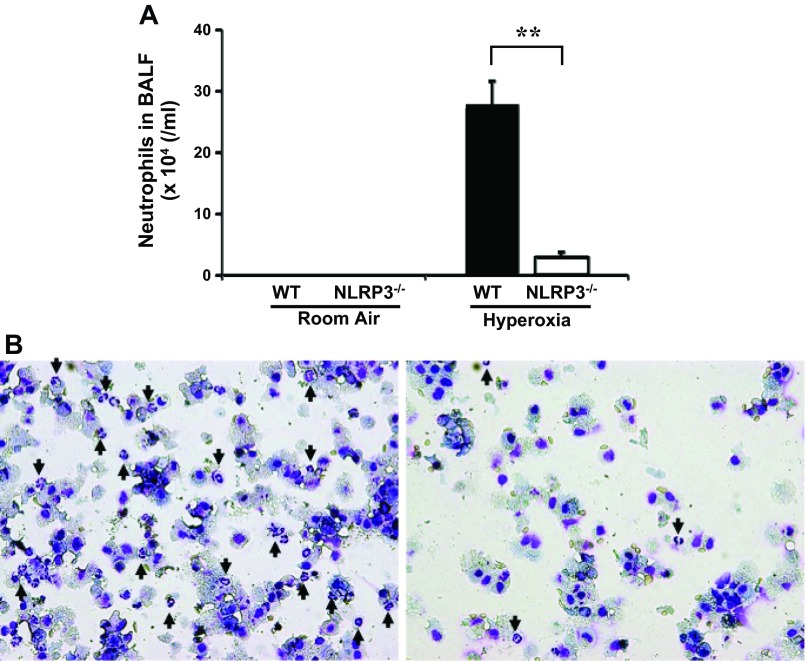
Hyperoxia-induced neutrophil accumulation is suppressed in NLRP3−/− mice.
Neutrophil infiltration into the pulmonary interstitium and alveoli is one of the key features of ALI. Suppression of neutrophils infiltration reduces hemorrhage- or endotoxemia-induced lung injury (1). The number of neutrophils in BAL fluid in mice exposed to 100% O2 for 72 h was assessed to determine whether protection of NLRP3−/− mice against HALI is related to suppression of neutrophil infiltration. There is a significantly lower number of neutrophils in BAL fluid in hyperoxia-exposed NLRP3−/− mice compared with WT mice (Fig. 5A). Consistently, microscopic observation of BAL fluid cells stained with Diff-Quik shows decreased neutrophil infiltration in the BAL fluid of NLRP3−/− mice (Fig. 5B).
Fig. 5.
Hyperoxia-induced neutrophil recruitment was decreased in NLRP3−/− mice. WT and NLRP3−/− mice exposed to room air or 100% O2 were euthanized and BALF was collected. A: means ± SE of total number of neutrophils (n = 4 in each group) from 1 of the 2 independent experiments is shown. B: mixture of equal amount of BALF from 4 different mice per each group was cytospined and stained with Diff-Quik. Infiltrating neutrophils are indicated by arrows. Magnification: ×200. **P < 0.01.
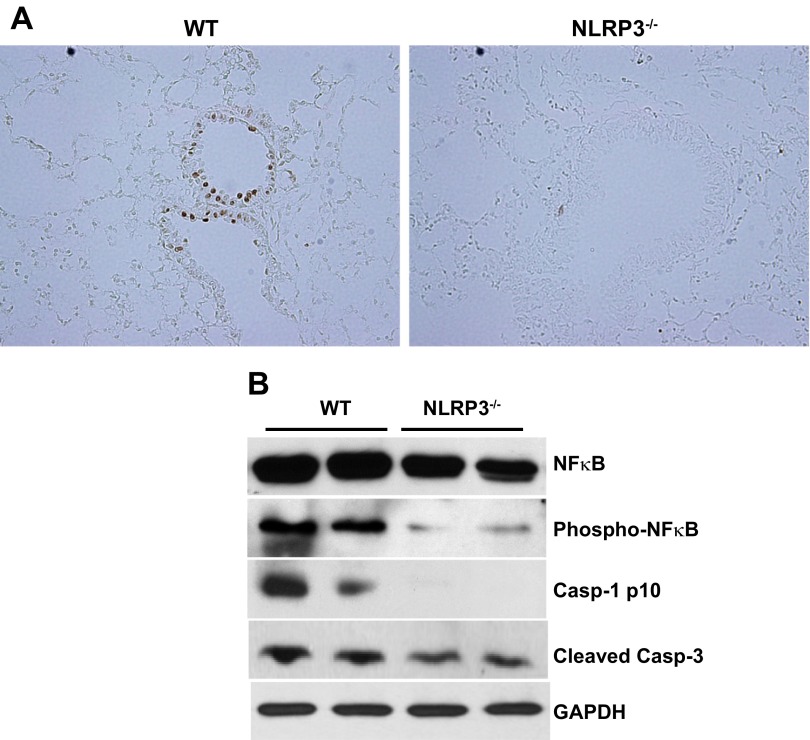
Hyperoxia-induced DNA fragmentation in lung epithelium is ameliorated in NLRP3−/− mice.
Hyperoxia-induced lung injury is characterized by lung epithelial cell death that features apoptosis and necrosis (51). Since both can be associated with DNA fragmentation, TUNEL assay to assess the extent of epithelial cell death was performed on lung tissue sections obtained from WT and NLRP3−/− mice exposed to hyperoxia for 48 h. TUNEL-positive lung epithelial cells are detectable in a patchy distribution in WT mice whereas they are barely detectable in NLRP3−/− mice (Fig. 6A). To quantitatively characterize and compare the extent of apoptosis, inflammasome activation, and inflammation, Western blot was performed on the whole lung protein extract for cleaved caspase-3, an apoptotic marker; caspase-1 p10, an NLRP3 inflammasome activation marker; and NF-κB, phospho-NF-κB, markers for inflammatory activation. Consistent with the results from TUNEL staining, the expression of cleaved caspase-3 in the lung after 48-h exposure to hyperoxia was decreased in NLRP3−/− mice compared with WT controls. Likewise, the expression of caspase-1 p10, NF-κB, and phospho-NF-κB was decreased in NLRP3−/− mice compared with WT controls (Fig. 6B). Our results showed that NLRP3 deletion decreased lung epithelial cell death, caspase-3 levels and suppressed NF-κB pathway compared with WT controls. These results suggest that hyperoxia-induced epithelial cell death is ameliorated in NLRP3-deficient mice.
Fig. 6.
Hyperoxia-induced lung epithelial cell death is attenuated in NLRP3−/− mice. A: WT and NLRP3−/− mice (n = 8 in each group) exposed to 100% O2 for 48 h were euthanized and lung tissues were collected. Lung tissue sections were stained using terminal deoxynucleotidyl transferase dUTP-mediated nick-end labeling (TUNEL) assay. Shown are representative images of 2 independent experiments. TUNEL-positive apoptotic cells are observed in lung epithelium in WT mice, but they are hardly detectable in NLRP3−/− mice. Magnification: ×200. B: Western blot analysis of NF-κB, phosphor-NF-κB, caspase-1 p10, and cleaved caspase-3 in whole lung lysates after 48-h hyperoxic exposure. Results are representative of 2 independent experiments.
DISCUSSION
The NLRP3 inflammasome is a multiprotein complex responsible for IL-1β processing in various inflammatory diseases (28, 50). In this study to determine whether inflammasome activation is critical in hyperoxia-induced lung injury we used NLRP3 homozygous knockout mice. IL-1β induces the production of other proinflammatory cytokines such as TNF-α and IL-8 (a human homologue of MIP-2; Refs. 4, 6, 20, 43, 49). IL-1β also causes surfactant abnormalities (16). Elevated TNF-α concentrations are associated with morbidity and mortality in patients with ARDS (2).
Our results show that hyperoxia-induced TNF-α and IL-1β elevation in BAL fluid is significantly suppressed in NLRP3−/− mice compared with WT controls, suggesting that hyperoxia-induced TNF-α elevation in lung is NLRP3 dependent. Previously, IL-1β was reported to induce IL-6 elevation (40). However, in the present study, there is no significant difference in IL-6 level in BAL fluid between hyperoxic WT and NLRP3−/− mice, suggesting that hyperoxia-induced IL-6 elevation is NLRP3 independent.
Macrophages are the most abundant immune cells in lung parenchyma, and different cytokines and inflammatory mediators activate these cells (5, 13, 23, 38). Recruitment of macrophages or monocytes to inflammatory sites in HALI is mainly controlled by MCP-1 (34), and a significant correlation exists between the BAL fluid MCP-1 level and severity of ARDS (39). The accumulation of macrophages in the lungs as seen in HALI should reflect enhanced recruitment of macrophages and/or their resistance to apoptosis. To investigate the role of NLRP3 inflammasome in macrophage accumulation in HALI, we assessed the number of macrophages and levels of MCP-1 in BAL fluid obtained from WT and NLRP3−/− mice exposed to hyperoxia. NLRP3−/− mice showed a significant decrease in the number of total cells and macrophages in BAL fluid under hyperoxic condition compared with WT mice. The levels of MCP-1 in BAL fluid were also significantly decreased in NLRP3−/− mice under hyperoxic conditions compared with WT mice. Neutrophil infiltration in the lung is a key event that correlates well with the severity of ALI/ARDS (14). The elimination of neutrophils markedly decreases the severity of ALI in experimental models (1). MIP-2 and IL-8 (a human homologue of MIP-2) are well-known neutrophil-attracting CXC chemokines and were reported to be elevated in ALI/ARDS (3, 29, 38, 42). In terms of the relationship between the inflammasome and neutrophil recruitment, it was recently reported that neutrophil recruitment to the thermally injured local site of the liver surface was blunted in NLRP3- or ASC-deficient mice compared with WT controls (27). Similarly, we show that the accumulation of neutrophils seen in HALI was diminished in NLRP3−/− mice. This suppression of neutrophil infiltration may be due to complete deletion of NLRP3 in all cell types. However, cell-specific knockout studies are further warranted in the future.
Both IL-1β and MIP-2 are also decreased in BAL fluid obtained from NLRP3−/− mice compared with WT controls. These results suggest that neutrophil accumulation in HALI is NLRP3 dependent through suppression of MIP-2 (as a neutrophil chemoattractant). Enhanced and sustained neutrophil accumulation in the lung would further facilitate the secretion of abundant proinflammatory cytokines or elastase from neutrophils. Several lines of evidence support the idea that oxidant stress directly injures lung epithelium (11, 24, 36, 44). In HALI, it is well known that inhaled oxygen toxicity induces oxidative damage and DNA fragmentation, an apoptotic marker, in lung epithelium (15, 48). Our results show that DNA fragmentation and cleaved caspase-3 expression are decreased in NLRP3−/− mice compared with WT controls. Although we also found decreased NF-κB activity in whole lungs obtained from NLRP3−/− mice compared with WT controls, additional studies are required to confirm how NF-κB pathway is directly involved in NLRP3-mediated HALI protection.
Taken together, this research demonstrates for the first time that NLRP3-deficient mice have suppressed inflammatory response to HALI. Based on our current results, we believe that a cytokine burst that follows cytokine-dependent inflammation and epithelial cell apoptosis in HALI is dependent on the NLRP3 inflammasome. The cytokine burst will facilitate epithelial permeability, epithelial barrier dysfunction, and epithelial cell death (8, 10, 31), key features of ALI.
From a clinical perspective, targeting inflammasome by a pharmacological approach that disrupts inflammasome activation may provide a novel therapeutic strategy for the protection of lung tissue from cellular injury during acute or chronic illness associated with ALI syndromes. However, one major limitation of our study is using a single insult (hyperoxia) as a trigger to study the inflammasome. In many clinical conditions, hyperoxia is currently being used to treat critically ill adults who may already have vigorous inflammasome activation. Further, it is also totally possible that inflammasome-independent mechanisms of transcription and release of IL-1β and IL-18 may coexist and represent a fundamental consideration for future therapeutics. Future investigation is needed to gain mechanistic insights into the regulation of NLRP3 inflammasome in ALI. Understanding the mechanisms of NLRP3-mediated HALI may lead to the development of clinical interventions for the protection of patients requiring supplemental oxygen.
GRANTS
N. Kolliputi was funded by the American Heart Association National Scientist Development Grant 09SDG2260957 and National Heart, Lung, and Blood Institute Grant R01-HL-105932 and the Joy McCann Culverhouse Endowment to the Division of Allergy and Immunology.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: J.F., I.F., P.T.P., R.C., and B.H. performed experiments; J.F. analyzed data; J.F. prepared figures; J.F. drafted manuscript; P.T.P., D.S.A.-G., R.F.L., and N.K. edited and revised manuscript; G.K.R., R.B.V., and N.K. interpreted results of experiments; N.K. approved final version of manuscript.
ACKNOWLEDGMENTS
We thank Dr. Brenda Flam for critical reading of the manuscript.
REFERENCES
- 1. Abraham E, Carmody A, Shenkar R, Arcaroli J. Neutrophils as early immunologic effectors in hemorrhage- or endotoxemia-induced acute lung injury. Am J Physiol Lung Cell Mol Physiol 279: L1137–L1145, 2000 [DOI] [PubMed] [Google Scholar]
- 2. Agouridakis P, Kyriakou D, Alexandrakis MG, Prekates A, Perisinakis K, Karkavitsas N, Bouros D. The predictive role of serum and bronchoalveolar lavage cytokines and adhesion molecules for acute respiratory distress syndrome development and outcome. Respir Res 3: 25, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ayala A, Chung CS, Lomas JL, Song GY, Doughty LA, Gregory SH, Cioffi WG, LeBlanc BW, Reichner J, Simms HH, Grutkoski PS. Shock-induced neutrophil mediated priming for acute lung injury in mice: divergent effects of TLR-4 and TLR-4/FasL deficiency. Am J Pathol 161: 2283–2294, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bethea JR, Chung IY, Sparacio SM, Gillespie GY, Benveniste EN. Interleukin-1 beta induction of tumor necrosis factor-alpha gene expression in human astroglioma cells. J Neuroimmunol 36: 179–191, 1992 [DOI] [PubMed] [Google Scholar]
- 5. Byers DE, Holtzman MJ. Alternatively activated macrophages and airway disease. Chest 140: 768–774, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chaudhary LR, Avioli LV. Regulation of interleukin-8 gene expression by interleukin-1beta, osteotropic hormones, and protein kinase inhibitors in normal human bone marrow stromal cells. J Biol Chem 271: 16591–16596, 1996 [DOI] [PubMed] [Google Scholar]
- 7. Cochrane CG, Spragg R, Revak SD. Pathogenesis of the adult respiratory distress syndrome. Evidence of oxidant activity in bronchoalveolar lavage fluid. J Clin Invest 71: 754–761, 1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coyne CB, Vanhook MK, Gambling TM, Carson JL, Boucher RC, Johnson LG. Regulation of airway tight junctions by proinflammatory cytokines. Mol Biol Cell 13: 3218–3234, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dostert C, Petrilli V, Van Bruggen R, Steele C, Mossman BT, Tschopp J. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science 320: 674–677, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Finigan JH, Faress JA, Wilkinson E, Mishra RS, Nethery DE, Wyler D, Shatat M, Ware LB, Matthay MA, Mason R, Silver RF, Kern JA. Neuregulin-1-human epidermal receptor-2 signaling is a central regulator of pulmonary epithelial permeability and acute lung injury. J Biol Chem 286: 10660–10670, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Freeman BA, Panus PC, Matalon S, Buckley BJ, Baker RR. Oxidant injury to the alveolar epithelium: biochemical and pharmacologic studies. Res Rep Health Eff Inst 54: 1–30; discussion 31–39, 1993 [PubMed] [Google Scholar]
- 12. Ganter MT, Roux J, Miyazawa B, Howard M, Frank JA, Su G, Sheppard D, Violette SM, Weinreb PH, Horan GS, Matthay MA, Pittet JF. Interleukin-1beta causes acute lung injury via alphavbeta5 and alphavbeta6 integrin-dependent mechanisms. Circ Res 102: 804–812, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity 32: 593–604, 2010 [DOI] [PubMed] [Google Scholar]
- 14. Grommes J, Soehnlein O. Contribution of neutrophils to acute lung injury. Mol Med 17: 293–307, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. He CH, Waxman AB, Lee CG, Link H, Rabach ME, Ma B, Chen Q, Zhu Z, Zhong M, Nakayama K, Nakayama KI, Homer R, Elias JA. Bcl-2-related protein A1 is an endogenous and cytokine-stimulated mediator of cytoprotection in hyperoxic acute lung injury. J Clin Invest 115: 1039–1048, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hybertson BM, Lee YM, Cho HG, Cho OJ, Repine JE. Alveolar type II cell abnormalities and peroxide formation in lungs of rats given IL-1 intratracheally. Inflammation 24: 289–303, 2000 [DOI] [PubMed] [Google Scholar]
- 17. Jain D, Atochina-Vasserman EN, Tomer Y, Kadire H, Beers MF. Surfactant protein D protects against acute hyperoxic lung injury. Am J Respir Crit Care Med 178: 805–813, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jiang Y, Beller DI, Frendl G, Graves DT. Monocyte chemoattractant protein-1 regulates adhesion molecule expression and cytokine production in human monocytes. J Immunol 148: 2423–2428, 1992 [PubMed] [Google Scholar]
- 19. Kallet RH, Matthay MA. Hyperoxic acute lung injury. Respir Care 58: 123–141, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Knofler M, Kiss H, Mosl B, Egarter C, Husslein P. Interleukin-1 stimulates tumor necrosis factor-alpha (TNF-alpha) release from cytotrophoblastic BeWo cells independently of induction of the TNF-alpha mRNA. FEBS Lett 405: 213–218, 1997 [DOI] [PubMed] [Google Scholar]
- 21. Kolliputi N, Galam L, Parthasarathy PT, Tipparaju SM, Lockey RF. NALP-3 inflammasome silencing attenuates ceramide-induced transepithelial permeability. J Cell Physiol 227: 3310–3316, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kolliputi N, Shaik RS, Waxman AB. The inflammasome mediates hyperoxia-induced alveolar cell permeability. J Immunol 184: 5819–5826, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lei D, Lancaster JR, Jr, Joshi MS, Nelson S, Stoltz D, Bagby GJ, Odom G, Shellito JE, Kolls JK. Activation of alveolar macrophages and lung host defenses using transfer of the interferon-gamma gene. Am J Physiol Lung Cell Mol Physiol 272: L852–L859, 1997 [DOI] [PubMed] [Google Scholar]
- 24. Martin WJ, 2nd, Gadek JE, Hunninghake GW, Crystal RG. Oxidant injury of lung parenchymal cells. J Clin Invest 68: 1277–1288, 1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell 10: 417–426, 2002 [DOI] [PubMed] [Google Scholar]
- 26. Matute-Bello G, Frevert CW, Martin TR. Animal models of acute lung injury. Am J Physiol Lung Cell Mol Physiol 295: L379–L399, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McDonald B, Pittman K, Menezes GB, Hirota SA, Slaba I, Waterhouse CC, Beck PL, Muruve DA, Kubes P. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science 330: 362–366, 2010 [DOI] [PubMed] [Google Scholar]
- 28. Menu P, Vince JE. The NLRP3 inflammasome in health and disease: the good, the bad and the ugly. Clin Exp Immunol 166: 1–15, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miller EJ, Cohen AB, Nagao S, Griffith D, Maunder RJ, Martin TR, Weiner-Kronish JP, Sticherling M, Christophers E, Matthay MA. Elevated levels of NAP-1/interleukin-8 are present in the airspaces of patients with the adult respiratory distress syndrome and are associated with increased mortality. Am Rev Respir Dis 146: 427–432, 1992 [DOI] [PubMed] [Google Scholar]
- 30. Mukhopadhyay S, Hoidal JR, Mukherjee TK. Role of TNFalpha in pulmonary pathophysiology. Respir Res 7: 125, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nakamura M, Matute-Bello G, Liles WC, Hayashi S, Kajikawa O, Lin SM, Frevert CW, Martin TR. Differential response of human lung epithelial cells to fas-induced apoptosis. Am J Pathol 164: 1949–1958, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. O'Neill LA. Immunology How frustration leads to inflammation. Science 320: 619–620, 2008 [DOI] [PubMed] [Google Scholar]
- 33. Ogura Y, Sutterwala FS, Flavell RA. The inflammasome: first line of the immune response to cell stress. Cell 126: 659–662, 2006 [DOI] [PubMed] [Google Scholar]
- 34. Okuma T, Terasaki Y, Sakashita N, Kaikita K, Kobayashi H, Hayasaki T, Kuziel WA, Baba H, Takeya M. MCP-1/CCR2 signalling pathway regulates hyperoxia-induced acute lung injury via nitric oxide production. Int J Exp Pathol 87: 475–483, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Olman MA, White KE, Ware LB, Simmons WL, Benveniste EN, Zhu S, Pugin J, Matthay MA. Pulmonary edema fluid from patients with early lung injury stimulates fibroblast proliferation through IL-1 beta-induced IL-6 expression. J Immunol 172: 2668–2677, 2004 [DOI] [PubMed] [Google Scholar]
- 36. Piotrowski WJ, Marczak J, Kurmanowska Z, Gorski P. Concentration of TBA-reactive substances in type II pneumocytes exposed to oxidative stress. Arch Immunol Ther Exp (Warsz) 52: 435–440, 2004 [PubMed] [Google Scholar]
- 37. Prince LR, Allen L, Jones EC, Hellewell PG, Dower SK, Whyte MK, Sabroe I. The role of interleukin-1beta in direct and toll-like receptor 4-mediated neutrophil activation and survival. Am J Pathol 165: 1819–1826, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Reddy NM, Kleeberger SR, Kensler TW, Yamamoto M, Hassoun PM, Reddy SP. Disruption of Nrf2 impairs the resolution of hyperoxia-induced acute lung injury and inflammation in mice. J Immunol 182: 7264–7271, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rosseau S, Hammerl P, Maus U, Walmrath HD, Schutte H, Grimminger F, Seeger W, Lohmeyer J. Phenotypic characterization of alveolar monocyte recruitment in acute respiratory distress syndrome. Am J Physiol Lung Cell Mol Physiol 279: L25–L35, 2000 [DOI] [PubMed] [Google Scholar]
- 40. Cahill CM, Rogers JT. Interleukin (IL) 1beta induction of IL-6 is mediated by a novel phosphatidylinositol 3-kinase-dependent AKT/IkappaB kinase alpha pathway targeting activator protein-1. J Biol Chem 283: 25900–25912, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schmal H, Shanley TP, Jones ML, Friedl HP, Ward PA. Role for macrophage inflammatory protein-2 in lipopolysaccharide-induced lung injury in rats. J Immunol 156: 1963–1972, 1996 [PubMed] [Google Scholar]
- 42. Shanley TP, Davidson BA, Nader ND, Bless N, Vasi N, Ward PA, Johnson KJ, Knight PR. Role of macrophage inflammatory protein-2 in aspiration-induced lung injury. Crit Care Med 28: 2437–2444, 2000 [DOI] [PubMed] [Google Scholar]
- 43. Sica A, Matsushima K, Van Damme J, Wang JM, Polentarutti N, Dejana E, Colotta F, Mantovani A. IL-1 transcriptionally activates the neutrophil chemotactic factor/IL-8 gene in endothelial cells. Immunology 69: 548–553, 1990 [PMC free article] [PubMed] [Google Scholar]
- 44. Simon LM, Raffin TA, Douglas WH, Theodore J, Robin ED. Effects of high oxygen exposure on bioenergetics in isolated type II pneumocytes. J Appl Physiol 47: 98–103, 1979 [DOI] [PubMed] [Google Scholar]
- 45. Sue RD, Belperio JA, Burdick MD, Murray LA, Xue YY, Dy MC, Kwon JJ, Keane MP, Strieter RM. CXCR2 is critical to hyperoxia-induced lung injury. J Immunol 172: 3860–3868, 2004 [DOI] [PubMed] [Google Scholar]
- 46. Tsujimoto H, Ono S, Mochizuki H, Aosasa S, Majima T, Ueno C, Matsumoto A. Role of macrophage inflammatory protein 2 in acute lung injury in murine peritonitis. J Surg Res 103: 61–67, 2002 [DOI] [PubMed] [Google Scholar]
- 47. Ward NS, Waxman AB, Homer RJ, Mantell LL, Einarsson O, Du Y, Elias JA. Interleukin-6-induced protection in hyperoxic acute lung injury. Am J Respir Cell Mol Biol 22: 535–542, 2000 [DOI] [PubMed] [Google Scholar]
- 48. Waxman AB, Einarsson O, Seres T, Knickelbein RG, Warshaw JB, Johnston R, Homer RJ, Elias JA. Targeted lung expression of interleukin-11 enhances murine tolerance of 100% oxygen and diminishes hyperoxia-induced DNA fragmentation. J Clin Invest 101: 1970–1982, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Weber A, Wasiliew P, Kracht M. Interleukin-1 (IL1) pathway. Sci Signal 3: cm1, 2010 [DOI] [PubMed] [Google Scholar]
- 50. Xiang M, Shi X, Li Y, Xu J, Yin L, Xiao G, Scott MJ, Billiar TR, Wilson MA, Fan J. Hemorrhagic shock activation of NLRP3 inflammasome in lung endothelial cells. J Immunol 187: 4809–4817, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zaher TE, Miller EJ, Morrow DM, Javdan M, Mantell LL. Hyperoxia-induced signal transduction pathways in pulmonary epithelial cells. Free Radic Biol Med 42: 897–908, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]