Abstract
This study examined psychologists’ views and practices regarding diagnostic classification systems for mental and behavioral disorders so as to inform the development of the ICD-11 by the World Health Organization (WHO). WHO and the International Union of Psychological Science (IUPsyS) conducted a multilingual survey of 2155 psychologists from 23 countries, recruited through their national psychological associations. Sixty percent of global psychologists routinely used a formal classification system, with ICD-10 used most frequently by 51% and DSM-IV by 44%. Psychologists viewed informing treatment decisions and facilitating communication as the most important purposes of classification, and preferred flexible diagnostic guidelines to strict criteria. Clinicians favorably evaluated most diagnostic categories, but identified a number of problematic diagnoses. Substantial percentages reported problems with crosscultural applicability and cultural bias, especially among psychologists outside the USA and Europe. Findings underscore the priority of clinical utility and professional and cultural differences in international psychology. Implications for ICD-11 development and dissemination are discussed.
Keywords: International Classification of Diseases (ICD), Diagnostic and Statistical Manual of Mental Disorders (DSM), diagnostic classification system, clinical utility, psychologists
Abstract
Cette étude porte sur les points de vue et les pratiques des psychologues en matière de systèmes de classification diagnostique des troubles mentaux et du comportement, afin d'aider à l'élaboration de la CIM-11 par l'Organisation mondiale de la santé (OMS). L'OMS et l'Union internationale des sciences psychologiques (IUPsyS) ont effectué une enquête multilingue de 2 155 psychologues de 23 pays recrutés par le biais de leurs associations de psychologie nationales. Soixante pour cent des psychologues du monde utilisent systématiquement un système de classification officiel, avec la CIM-10 utilisée le plus fréquemment par 51 % d'entre eux et le DSM-IV, par 44 %. Les psychologues considèrent que les plus importants objectifs de la classification sont de prendre des décisions de traitement éclairées et de faciliter la communication. Et, aussi, ils préfèrent des orientations diagnostiques flexibles à des critères stricts. Les cliniciens évaluent favorablement la plupart des catégories diagnostiques, mais identifient un certain nombre de diagnostics problématiques. Un pourcentage substantiel d'entre eux ont signalé des problèmes avec l'applicabilité transculturelle et les biais culturels. C'est surtout le cas avec les psychologues qui ne sont ni américains ni européens. Les résultats soulignent la priorité de l'utilité clinique et les différences culturelles et professionnelles en psychologie internationale. Les auteurs discutent des implications pour le développement de la CIM-11 et de sa diffusion.
Abstract
Este estudio examina el punto de vista como también las prácticas de los psicólogos respecto de los sistemas de clasificación de diagnóstico para los trastornos mentales y conductuales, con el fin de informar el desarrollo del ICD-11 hecho por la Organización Mundial de la Salud (OMS). La OMS y la International Union of Psychological Science (IUPsyS) realizaron una encuesta multilingüística entre 2155 psicólogos provenientes de 23 países, reclutados a través de las asociaciones nacionales de psicólogos. El sesenta por ciento de los psicólogos utilizaba de rutina un sistema formal de clasificación, siendo el ICD-10 el sistema utilizado con mayor frecuencia (51 por ciento) y el DSM-IV utilizado el 44 por ciento. Según los psicólogos, el propósito más importante de la clasificación era para decidir sobre diferentes tratamientos, como también facilitar la comunicación, y preferían parámetros flexibles de diagnóstico en contraste con criterios estrictos. Los clínicos evaluaron de manera favorable a la mayor cantidad de categorías de diagnóstico, pero identificaron un número de diagnósticos problemáticos. Hubo un porcentaje substancial que dijo tener problemas con la aplicación transcultural y el sesgo cultural, especialmente entre los psicólogos fuera de los Estados Unidos y Europa. Los hallazgos enfatizan la prioridad de la utilidad clínica y las diferencias profesionales y culturales en la psicología internacional. Se analizan las implicaciones para el desarrollo y la difusión del ICD-11.
The World Health Organization (WHO) is currently revising the International Classification of Diseases and Related Health Problems (ICD-10) (WHO, 1992a), including the chapter on mental and behavioral disorders (WHO, 1992b). Publication of the ICD-11 is expected in 2015 (WHO, 2013). The revision process began several years ago and has included the formation of an International Advisory Group, systematic literature reviews, articulation of goals and priorities, and the establishment of a research agenda (International Advisory Group, 2011; Reed, 2010). Currently, WHO is concluding the ICD-11's formative research phase, revising the second (beta) draft, entering a broad review and comment process, and preparing to conduct Internet- and clinic-based field trials.
In the development of the mental and behavioral disorders classification for ICD-11, the WHO Department of Mental Health and Substance Abuse has emphasized improving the classification's clinical utility as a central goal of the current revision. This goal is directly linked to mental health service delivery and WHO's global public health mission (International Advisory Group, 2011; Reed, 2010). Problems with the clinical utility of current classification systems have been widely described (e.g., First, 2005, 2010; First & Westen, 2007; Flanagan & Blashfield, 2010; Mullins-Sweatt & Widiger, 2009; Reed, 2010). For the purposes of the current ICD revision efforts, including the present study, WHO is evaluating the clinical utility of a diagnostic classification system (DCS) in terms of three components: (a) value in communicating information; (b) implementation characteristics in clinical practice (e.g., ease of use, goodness of fit); and (c) usefulness for making clinical treatment and management decisions (Reed, 2010).
In order to assess the clinical utility of current DCSs to provide specific indications for revisions, it is important to assess the views and experiences of those who use them in routine clinical practice. Surprisingly, given the stated importance of clinical utility in both the ICD-10 (WHO, 1992b, p. 8) and the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association [APA], 2000, p. xxiii), few such efforts have been made in the past. Those studies that are available have often been limited by their sample size, methods, or geographical scope. Earlier surveys (Maser, Kaelber, & Weise, 1991; Mezzich, 2002; Müssigbrodt et al., 2000; Sechter, 1995) mostly focused on broad questions regarding clinicians’ usage of and satisfaction with the ICD and DSM, with little specific direction for revisions.
More recently, a few clinician surveys have addressed more substantive and specific issues. Mellsop and colleagues (Mellsop et al., 2007a; Mellsop, Dutu, & Robinson, 2007b) developed a survey to examine New Zealand psychiatrists’ views on the purposes, problems, and features of DCSs. Adaptations of this survey have subsequently been used to examine psychiatrists’ views across different geographical and cultural contexts, including New Zealand, Brazil, and Japan (Mellsop et al., 2007a), the USA (Bell, Sowers, & Thompson, 2008), and Japan, Korea, China, and Taiwan (Suzuki et al., 2010), and among primary care physicians, psychiatrists, psychologists, and consumers in New Zealand (Mellsop, Lutchman, Lillis, & Dutu, 2011). Similarly, Zielasek and colleagues (2010) conducted their own survey of German-speaking psychiatrists. A consistent finding from these more recent studies has been that clinicians favor a simple, reliable, and easy-to-use system with fewer disorder categories. However, there has been less agreement regarding how best to tailor a system to meet the needs of different users, and views on crosscultural applicability have varied across different countries and cultural contexts.
By far the largest, most international, and most comprehensive clinician survey to date was conducted by WHO and the World Psychiatric Association (WPA; Reed, Correia, Esparza, Saxena, & Maj, 2011). WHO and WPA surveyed 4887 psychiatrists in 44 countries around the globe in 19 languages. A large majority of respondents agreed that the most important purposes of a DCS were to facilitate interclinician communication and inform clinical decisions about treatment and management. Respondents preferred flexible diagnostic guidelines rather than strict criteria, and a simplified system with fewer diagnostic categories. There was disagreement about whether or how to incorporate dimensional classification, functional impairment, and severity into a DCS. In general, findings supported the priority of clinical utility and reflected favorably on most diagnostic categories while also indicating problems with specific diagnoses.
With few exceptions (e.g., Mellsop et al., 2011), studies of clinicians’ views on DCSs have been conducted with samples composed entirely or mostly of psychiatrists; few have included psychologists or other mental health professionals. This is an important limitation because, worldwide, psychiatrists provide only a small fraction of mental health services delivered (WHO, 2011). In light of this consideration, WHO has worked to develop a strong multidisciplinary perspective as a part of the development of the ICD-11 classification of mental and behavioral disorders, including formal involvement by organizations representing psychologists, mental health counselors, social workers, nurses, and primary care physicians, in addition to psychiatrists (International Advisory Group, 2011). Psychologists, in particular, represent a significant constituency among DCS users, and may offer a useful perspective on improving the clinical utility of the ICD-11. Accordingly, psychologists have been formally represented in the ICD revision process by the IUPsyS. WHO's collaboration with IUPsyS provided the vehicle for the present study.
Previous studies in this area have two further limitations: Most have surveyed clinicians in only one or a few countries; and most have been conducted with samples that generally use the same DCS, or with little to no examination of differences between DSM and ICD users. To date, Reed et al. (2011) is the only study with sufficient sample size and diversity to investigate either of these issues, and the findings posed interesting implications for psychiatry around the globe and across cultures. In anticipation of ICD-10 and DSM-5 (APA, 2013), the present study represents the next major step in this emerging body of research: a global survey of psychologists.
Specifically, the aims of this study were to examine psychologists’ views on issues concerning the clinical utility of DCSs and the extent to which these opinions differ across geographical region, country, and ICD-10 vs. DSM-IV users. These data, along with data from other investigations (e.g., Reed et al., 2011, 2013; Roberts et al., 2012), will be used to help inform revisions to the forthcoming ICD-11 chapter on mental and behavioral disorders, with a focus on improving clinical utility. To this end, an Internet-based survey for psychologists was developed by WHO and IUPsyS, and distributed in 23 countries by IUPsyS member psychological associations. Items addressed topics such as the usage, purposes, and features of a DCS; practical and conceptual issues of mental disorder classification; clinical prevalence, ease of use, and goodness of fit of particular diagnoses; and recommendations for DCS revisions.
METHODS
As described below, the survey and study procedures resembled those of the WPA-WHO global survey of psychiatrists (Reed et al., 2011), but with differences in participants, timeframe, and select items. All procedures and materials were approved by WHO Research Ethics Review Committee and the University of Kansas Human Subjects Committee – Lawrence.
Survey development
Before developing the survey, three of the investigators (PR, ADW, and GMR) composed and sent letters to the presidents of IUPsyS member national psychological associations, assessing their level of interest and ability in participating in various international ICD-11 research projects, including the present study. Those unable to participate in an English-language study were asked if they could assist with translation. In total, 47 associations expressed interest, and 23 ultimately implemented the survey to completion (see Table 1).
TABLE 1.
Sample characteristics by country and region
| REGION Country | Participating psychological association | Survey language | N | Response rate (%) | % of total sample | M age | M years of experience | % Female | % Licensed | % Seeing patients |
|---|---|---|---|---|---|---|---|---|---|---|
| AFRICA | ||||||||||
| Namibia | Psychological Association of Namibia | English | 7 | 21.9 | 0.3 | 39.9 | 8.1 | 85.7 | 100.0 | 85.7 |
| South Africa | Psychological Society of South Africa | English | 91 | 18.8 | 4.2 | 48.3 | 14.1 | 68.6 | 96.5 | 94.2 |
| Uganda | Uganda National Psychological Association | English | 20 | 50.0 | 0.9 | 41.1 | 7.9 | 40.0 | 85.0 | 90.0 |
| Zimbabwe | Zimbabwe Psychological Association | English | 3 | 21.4 | 0.1 | 40.5 | 4.0 | 0.0 | 100.0 | 100.0 |
| Unweighted M/total | – | – | 121 | 21.2 | 5.6 | 46.4 | 12.7 | 63.5 | 94.8 | 93.0 |
| Weighted M | – | – | 30.3 | 28.0 | 1.4 | 42.4 | 8.5 | 48.6 | 95.4 | 92.5 |
| ASIA | ||||||||||
| Hong Kong | Hong Kong Psychological Society | English | 72 | 23.9 | 3.3 | 41.6 | 12.3 | 82.9 | 98.6 | 92.9 |
| India | India National Academy of Psychology | English | 54 | Unknown | 2.5 | 39.3 | 12.0 | 70.2 | 97.9 | 91.5 |
| Sri Lanka | Sri Lanka Psychological Society | English | 13 | 72.2 | 0.6 | 40.5 | 6.8 | 63.6 | 90.9 | 72.7 |
| Unweighted M/total | – | – | 139 | 43.6 | 6.5 | 40.6 | 11.7 | 76.6 | 97.7 | 90.6 |
| Weighted M | – | – | 46.3 | 48.1 | 2.2 | 40.4 | 10.4 | 72.2 | 95.8 | 85.7 |
| EASTERN MEDITERRANEAN | ||||||||||
| Israel | Israel Psychological Association | English | 40 | Unknown | 1.9 | 53.2 | 19.9 | 54.8 | 96.8 | 100.0 |
| Lebanon | Lebanese Psychological Association | English & French | 10 | 33.3 | 0.5 | 40.3 | 11.7 | 90.0 | 100.0 | 100.0 |
| Turkey | Turkish Psychological Association | Turkish | 174 | 38.8 | 8.1 | 36.7 | 11.4 | 75.5 | 89.8 | 92.4 |
| Unweighted M/total | – | – | 224 | 46.9 | 10.4 | 39.6 | 12.8 | 72.9 | 91.5 | 94.0 |
| Weighted M | – | – | 74.7 | 36.1 | 3.5 | 43.4 | 14.3 | 73.4 | 95.5 | 97.5 |
| EUROPE | ||||||||||
| Denmark | Danish Psychological Association | English | 223 | 50.9 | 10.3 | 47.1 | 14.5 | 77.5 | 97.2 | 98.6 |
| Estonia | Union of Estonian Psychologists | English | 10 | 76.9 | 0.5 | 43.6 | 15.6 | 77.8 | 100.0 | 100.0 |
| Finland | Finnish Psychological Society | English | 186 | 41.3 | 8.6 | 43.6 | 15.1 | 79.8 | 98.3 | 96.6 |
| France | French National Committee of Scientific Psychology | French | 343 | 65.6 | 15.9 | 39.9 | 10.9 | 76.7 | 95.5 | 95.5 |
| Germany | Federation of German Psychologists’ Associations | German | 170 | 34.8 | 7.9 | 50.6 | 19.2 | 53.9 | 94.6 | 89.8 |
| Ireland | Psychological Society of Ireland | English | 40 | 8.0 | 1.9 | 45.7 | 16.3 | 78.4 | 94.6 | 94.6 |
| Norway | Norwegian Psychological Association | English | 239 | 48.6 | 11.1 | 42.5 | 11.5 | 67.7 | 99.6 | 97.0 |
| Sweden | Swedish Psychological Society | English | 100 | 20.0 | 4.6 | 44.3 | 10.8 | 67.7 | 100.0 | 97.8 |
| Switzerland | Swiss Psychological Association | English | 37 | 14.3 | 1.7 | 47.9 | 18.2 | 61.8 | 100.0 | 97.0 |
| United Kingdom | British Psychological Society | English | 50 | 11.4 | 2.3 | 44.0 | 13.7 | 70.2 | 100.0 | 95.7 |
| Unweighted M/total | – | – | 1398 | 15.6 | 64.8 | 44.2 | 13.7 | 71.6 | 97.4 | 95.9 |
| Weighted M | – | – | 139.8 | 37.2 | 6.5 | 44.9 | 14.6 | 71.1 | 98.0 | 96.2 |
| LATIN AMERICA | ||||||||||
| Argentina | Argentinian Association of Behavioral Science | Spanish | 26 | 60.5 | 1.2 | 41.4 | 12.3 | 68.0 | 100.0 | 84.0 |
| Mexico | Mexican Psychological Association | Spanish | 139 | 31.2 | 6.5 | 44.1 | 16.8 | 66.1 | 93.7 | 66.9 |
| Unweighted M/total | – | – | 165 | 33.8 | 7.7 | 43.7 | 16.1 | 66.4 | 94.7 | 69.7 |
| Weighted M | – | – | 82.5 | 45.9 | 3.8 | 42.8 | 14.5 | 67.1 | 96.9 | 75.5 |
| USA | American Psychological Association | English | 108 | 10.9 | 5.0 | 54.5 | 20.9 | 57.5 | 100.0 | 94.3 |
| OVERALL | ||||||||||
| Unweighted M/total | – | – | 2155 | 31.0 | 100.0 | 44.2 | 14.0 | 70.4 | 96.6 | 93.2 |
| M weighted by country | – | – | 93.7 | 35.9 | 4.3 | 43.9 | 13.2 | 66.7 | 96.9 | 92.5 |
| M weighted by region | – | – | 359.2 | 28.7 | 16.7 | 44.8 | 14.6 | 68.1 | 96.0 | 89.6 |
The questionnaire was developed by WHO's Department of Mental Health and Substance Abuse and IUPsyS to solicit psychologists’ views relevant to the development of the ICD-11 chapter on mental and behavioral disorders, and was designed to be parallel and similar to the WHO-WPA survey of psychiatrists (Reed et al., 2011). It also included items adapted from other previous surveys of clinicians (Mellsop et al., 2007a, 2007b; Zielasek et al., 2010) and the ICD-10 field trials (Sartorius et al., 1993). New questions were developed specifically to address issues relevant to psychological practice.
Surveys were programmed and administered through the Qualtrics web-based survey platform, hosted through an account licensed to the University of Kansas. Where appropriate, the survey was programmed to be adaptive to participants’ responses, such that some items were presented only if certain responses were selected for previous items. For example, participants were asked about their clinical experiences with diagnostic categories only if they had previously indicated that they were currently seeing patients. To minimize missing data, the survey was programmed to require participants to respond to all items before moving to the next screen.
The study was originally developed in English, and 17 out of the 23 associations used the English version only. For the other six countries, survey materials were translated into Spanish, French, German, and Turkish (see Table 1). The Spanish and French translations were provided by WHO. The German and Turkish associations assisted with the translations into those languages. To facilitate translations, WHO provided explicit instructions that included forwardand back-translation, conceptual equivalence across cultures, semantic equivalence across languages, and agreement among multiple translators.
Procedures and participants
Participating IUPsyS member associations received a standard set of instructions for the selection of participants, initial solicitation message, reminder messages, and tracking of participation. The instructions indicated that the primary purpose of the study was to “assess the views and opinions of psychologists around the world regarding the problems with current DCSs and to provide scientific and clinical input to strengthen, broaden, and improve the revision process.” In exchange for their participation, associations received a data set and report containing the results obtained from their sample, which they could present or publish as desired (with appropriate approval from and acknowledgement of WHO and IUPsyS).
National psychological associations were instructed to select participants who met the following inclusion criteria: (a) membership in their national psychological association, (b) professional status as a psychologist in their country, (c) completion of all necessary professional training, (d) authorization or licensure to practice as a psychologist in their country, and (e) current provision of treatment or assessment services for persons with mental and behavioral disorders in their country. Further, they were instructed not to solicit members who were not psychologists, still in training, or not currently practicing. However, not all associations had the membership data necessary to implement all of these criteria in sample selection.
Large associations (≥ 1000 members) were asked to randomly select 500 individuals from their membership who satisfied the above criteria for participation. Small associations (< 1000 members) were asked to solicit all available members who met these criteria. Selected participants received an initial email and up to two follow-up emails soliciting their voluntary participation in an online survey to inform WHO's revision process for the ICD chapter on mental and behavioral disorders. Due to technological barriers, one national association (Uganda) used a paper-and-pencil version of the survey delivered by mail. Still, they were given the same directions as those using the Internet-based survey. All associations collected data for a period between December 2010 and February 2012 (median data collection period = 3 months).
Analytic plan
Data were analyzed in aggregate as well as by country, region, and which DCS participants used. National association subsamples were used as country groups. Countries were sorted a priori into six regional groups (Africa, Asia, Eastern Mediterranean, Europe, Latin America, USA) adapted from WHO's official global regions. DCS groups were formed based on participants’ selection of the ICD-10 or DSM-IV as their primary DCS in clinical practice. Descriptive results were calculated in two ways: (a) unweighted figures, based on all participants’ data combined into one group; and (b) weighted figures, based on country-level statistics. Weighted estimates overcome some of the problems associated with disparate sample sizes by giving each national sample “equal weight” in estimating results for the entire sample. However, these figures should be interpreted cautiously when sample sizes are very disproportionate. By comparing weighted and unweighted estimates, one may determine whether the total, unweighted values are disproportionately influenced by countries with large sample sizes, and thereby arrive at a more accurate interpretation (Reed et al., 2011).
To test for significant differences across regional and DCS groups, chi-square and ANOVA analyses were conducted for all multiple-choice and scale items, respectively. For ordinal multiple-choice items, chi-square tests for linearity were also examined, but revealed no significant differences that were not identified through nonlinear comparisons. To control for an inflated Type I error rate due to a large sample and numerous comparisons, Bonferroni corrections were used, maintaining a study-wise alpha of .01. Effect sizes were calculated as Cramer's V for categorical variables and Cohen's d for continuous variables. Following Cohen's (1988) recommendations, a Cramer's V > .1 is interpreted as a small effect size, > .3 as medium, and > .5 as large; and a Cohen's d > .2 is interpreted as a small, >.5 as medium, and > .8 as large.
RESULTS
The final sample consisted of 2155 participants (Mage = 44.18, SD = 12.06; 70.4% female) from 23 countries and six regions around the globe. Table 1 presents response rate, demographic, and professional characteristics of the overall, national, and regional samples. The 23 participating associations recorded a total of 6911 solicitations by email and 40 by mail.1 Overall, 2155 individuals consented to participate (response rate = 29.7%, weighted = 35.9%), including 2135 online participants (response rate = 30.9%) and 20 paper-and-pencil participants (response rate = 50.0%). Response rates for national subsamples ranged from 8.0% to 76.9%.
Professional characteristics and practices
Clinical experience
Globally, 93.2% (92.5% weighted) of participating psychologists reported that they were currently seeing patients, and 96.6% (96.9% weighted) were currently licensed or authorized to provide assessment or treatment services to persons with mental disorders, whether independently (86.7%; 84.1% weighted) or under supervision (9.9%; 12.9% weighted). As shown in Table 1, country- and region-level results varied on these items, but still indicated that psychologist practitioners constituted the large majority of each national subsample (66.9–100.0%). Clinicians reported having an average of 13.97 years of post-training clinical experience (weighted M = 13.22, SD = 10.93). Three-quarters (75.2%, 66.3% weighted) indicated that they currently spend between 10 and 40 h per week seeing patients.
Diagnostic practices
Two items asked what types of professionals typically make diagnoses in the setting where respondents worked most, and what role psychologists played with regard to diagnosis. Three-quarters of respondents (75.0%; 79.2% weighted) reported that psychologists typically assigned diagnoses in their primary work settings, followed by psychiatrists (60.4%; 56.8% weighted), and other physicians (20.0%; 17.7% weighted). This rank ordering remained consistent across each regional subgroup, but, as shown in Table 2, there were substantial differences by country. In the USA, Germany, and Mexico, for example, nearly 100% of participating psychologists indicated that in the settings where they worked, psychologists typically made diagnoses. However, in Denmark, Finland, Turkey, and the United Kingdom, psychiatrists most often made diagnoses in psychologists’ primary work settings.
TABLE 2.
Respondents’ diagnostic practices by region and country
| REGION | Item N |
Who makes diagnoses in the setting where you work? (%) |
Respondents’ diagnostic role (%) |
% Always / often use DCS |
DCS used most often (%) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Psychologists | Psychiatrists | Other physicians | Nurses | Diagnose independently | Contribute to diagnostic formulations | No active role | ICD-10 | DSM-ÍV | ||
| AFRICA | |||||||||||
| Namibia | 6 | 83.3 | 66.7 | 16.7 | 0.0 | 83.3 | 16.7 | 0.0 | 16.7 | 0.0 | 83.3 |
| South Africa | 80 | 93.8 | 28.8 | 11.3 | 5.0 | 81.3 | 12.5 | 3.8 | 72.5 | 45.6 | 49.4 |
| Uganda | 18 | 40.0 | 50.0 | 15.0 | 5.0 | 50.0 | 50.0 | 0.0 | 72.2 | 7.7 | 69.2 |
| Zimbabwe | 2 | 100.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 0.0 | 100.0 | 100.0 | 100.0 |
| Unweighted total | 106 | 84.9 | 34.9 | 12.3 | 4.7 | 76.4 | 18.9 | 2.8 | 69.8 | 37.0 | 55.0 |
| Weighted M | 26.5 | 79.3 | 36.4 | 10.7 | 2.5 | 78.6 | 19.8 | 0.9 | 65.3 | 38.3 | 75.5 |
| ASIA | |||||||||||
| Hong Kong | 64 | 87.5 | 45.3 | 20.3 | 1.6 | 79.7 | 17.2 | 3.1 | 79.7 | 3.1 | 96.9 |
| India | 41 | 90.2 | 75.6 | 14.6 | 0.0 | 73.2 | 22.0 | 0.0 | 78.0 | 75.0 | 12.5 |
| Sri Lanka | 8 | 62.5 | 87.5 | 50.0 | 0.0 | 25.0 | 62.5 | 0.0 | 12.5 | 37.5 | 62.5 |
| Unweighted total | 113 | 86.7 | 59.3 | 20.4 | 0.9 | 73.5 | 22.1 | 1.8 | 74.3 | 31.3 | 64.3 |
| Weighted M | 37.7 | 80.1 | 69.5 | 28.3 | 0.5 | 59.3 | 33.9 | 1.0 | 56.7 | 38.5 | 57.3 |
| EASTERN MEDITERRANEAN | |||||||||||
| Israel | 25 | 96.0 | 40.0 | 8.0 | 0.0 | 76.0 | 20.0 | 4.0 | 24.0 | 9.2 | 85.0 |
| Lebanon | 9 | 88.9 | 55.6 | 0.0 | 0.0 | 66.7 | 33.3 | 0.0 | 77.8 | 11.1 | 77.8 |
| Turkey | 126 | 64.3 | 67.5 | 9.5 | 0.8 | 46.8 | 41.3 | 9.5 | 54.0 | 7.4 | 87.6 |
| Unweighted total | 160 | 70.6 | 62.5 | 8.8 | 0.6 | 52.5 | 37.5 | 8.1 | 50.6 | 9.2 | 85.0 |
| Weighted M | 53.3 | 83.1 | 54.3 | 5.8 | 0.3 | 63.2 | 31.5 | 4.5 | 51.9 | 12.0 | 79.8 |
| EUROPE | |||||||||||
| Denmark | 207 | 57.5 | 73.4 | 7.2 | 5.3 | 37.2 | 51.2 | 4.3 | 71.0 | 94.0 | 3.5 |
| Estonia | 9 | 55.6 | 88.9 | 33.3 | 0.0 | 0.0 | 100.0 | 0.0 | 55.6 | 100.0 | 0.0 |
| Finland | 172 | 11.0 | 79.7 | 28.5 | 1.7 | 3.5 | 72.1 | 18.0 | 19.8 | 76.3 | 21.1 |
| France | 285 | 68.1 | 67.0 | 36.8 | 3.9 | 34.0 | 44.2 | 15.1 | 22.8 | 19.2 | 69.5 |
| Germany | 147 | 98.6 | 21.8 | 12.2 | 0.7 | 93.9 | 4.8 | 0.7 | 93.2 | 93.2 | 5.4 |
| Ireland | 33 | 84.8 | 48.5 | 6.1 | 3.0 | 48.5 | 42.4 | 6.1 | 69.7 | 6.1 | 90.9 |
| Norway | 220 | 99.1 | 75.9 | 19.1 | 6.4 | 87.7 | 8.6 | 1.4 | 86.4 | 98.2 | 1.4 |
| Sweden | 89 | 87.6 | 69.7 | 31.5 | 13.5 | 56.2 | 31.5 | 6.7 | 71.9 | 34.1 | 61.4 |
| Switzerland | 32 | 100.0 | 59.4 | 9.4 | 0.0 | 96.9 | 3.1 | 0.0 | 78.1 | 71.0 | 19.4 |
| UK | 43 | 69.8 | 83.7 | 16.3 | 11.6 | 41.9 | 53.5 | 0.0 | 34.9 | 36.6 | 61.0 |
| Unweighted total | 1237 | 70.2 | 66.3 | 22.0 | 4.7 | 50.6 | 36.9 | 7.7 | 57.0 | 68.4 | 27.6 |
| Weighted M | 123.7 | 73.2 | 66.8 | 20.0 | 4.6 | 50.0 | 41.1 | 5.2 | 60.3 | 62.9 | 33.3 |
| LATIN AMERICA | |||||||||||
| Argentina | 21 | 90.5 | 52.4 | 19.0 | 0.0 | 57.1 | 23.8 | 4.8 | 61.9 | 0.0 | 85.7 |
| Mexico | 80 | 93.8 | 35.0 | 27.5 | 1.3 | 76.3 | 16.3 | 2.5 | 51.3 | 10.8 | 81.1 |
| Unweighted total | 101 | 93.1 | 38.6 | 25.7 | 1.0 | 72.3 | 17.8 | 3.0 | 53.5 | 8.4 | 82.1 |
| Weighted M | 50.5 | 92.1 | 43.7 | 23.3 | 0.6 | 66.7 | 20.0 | 3.6 | 56.6 | 5.4 | 83.4 |
| USA | 100 | 99.0 | 34.0 | 15.0 | 3.0 | 96.0 | 3.0 | 0.0 | 86.0 | 1.0 | 93.9 |
| OVERALL | |||||||||||
| Unweighted total | 1817 | 75.0 | 60.4 | 20.0 | 3.8 | 57.4 | 32.1 | 6.4 | 59.7 | 51.4 | 43.8 |
| M weighted by country | 80.4 | 79.9 | 56.0 | 17.7 | 2.4 | 62.2 | 30.6 | 3.6 | 60.2 | 37.7 | 59.6 |
| M weighted by region | 302.8 | 84.1 | 49.3 | 17.4 | 2.5 | 70.2 | 22.7 | 3.9 | 65.2 | 25.9 | 68.0 |
Table does not display percentages of respondents who selected “other” in response to “Who makes diagnoses … ?,” or who selected “ICD-9” or “other” as the DCS used most often. Item N refers to the number of participants who responded to the majority of these items.
A modest majority (57.4%; 61.4% weighted) reported that they “make diagnoses independently,” compared to 32.1% (31.7% weighted) who “contribute to diagnostic formulations made by other health professionals,” and 6.4% (3.5% weighted) who said they had “no role” in assigning diagnoses. As shown in Table 2, there was substantial variability across countries in the role that psychologists played in diagnosis.
Usage of diagnostic classification systems
Respondents were asked, “As part of your day-today clinical work, how much of the time do you use a formal diagnostic classification system … ?” The majority selected “always or almost always” (35.7%; 34.7% weighted) or “often” (24.0%; 25.7% weighted), followed by “sometimes” (18.1%; 22.2% weighted), “rarely” (16.1%; 14.4% weighted), and “never” (6.1%; 3.0 % weighted). Distinct variations were found across countries and between ICD-10 and DSM-IV users, χ2 (3,N = 1611) = 53.58, p < .0001, V = .182. Among respondents who used any DCS, frequency of use was greater among ICD-10 users (71.8% always/often) than DSM-IV users (56.5% always/often). Over 80% of respondents in USA, Germany, and Norway reported using a DCS regularly, compared to less than 35% in Finland, France, the United Kingdom, Israel, Sri Lanka, and Namibia (see Table 2).
Regarding particular DCSs, 51.4% (36.8% weighted) of all respondents indicated that they most often used ICD-10, followed by DSM-IV (43.8%; 56.8% weighted), “other” (4.1%; 5.7% weighted), and ICD-9 (0.7%; 0.7% weighted). As shown in Table 2, there was a great deal of regional variability related to ICD-10 vs. DSM-IV usage, χ2 (5, N = 1611) = 445.49, p < .0001, V = .526. Respondents in most European countries and in India tended to use the ICD-10 most often, whereas others reportedly used the DSM-IV more often. Among clinicians who use a DCS other than the ICD-10, 36.2% (44.3% weighted) were at least somewhat familiar with it.
General aspects of diagnostic classification systems
Most important purpose
Participants were asked, “From your perspective, which is the single most important purpose of a diagnostic classification system?” As presented in Figure 1, the three most popular responses were directly related to clinical utility—(a) informing decisions about treatment and management, (b) communication with other clinicians, and (c) communication with patients—which together comprised a large majority of respondents (87.6%; 89.1% weighted). No significant differences were found between ICD-10 and DSM-IV users in their views of the purpose of a classification.
Figure 1.
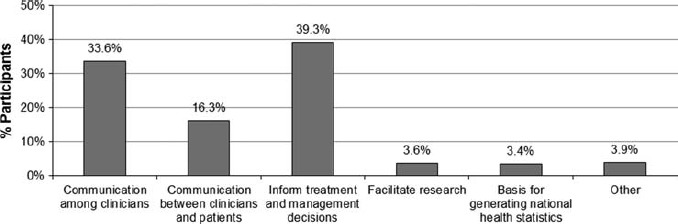
Respondents’ views on “what is the single, most important purpose of diagnostic classification system.” Percentages are equally weighted by country. Unweighted percentages were relatively similar (from left to right: 38.7%, 15.5%, 33.4%, 3.3%, 4.6%, and 4.5%).
Optimal number of diagnostic categories
When asked, “In clinical settings, how many diagnostic categories should a classification system contain to be most useful for mental health professionals?” the great majority (85.1%; 86.9% weighted) indicated that the classification should contain fewer than 100 categories. More specifically, 34.8% (38.3% weighted) selected 10–31 categories, and 50.3% (48.6% weighted) selected 31–100 categories as the optimal number. Few selected 101–200 (10.6%; 9.0% weighted) or more than 200 (4.4%; 4.1% weighted) as the preferred number of categories. No DCS-related differences were found.
Strict criteria vs. flexible guidance
Diagnostic categories can be operationalized through strict, specified diagnostic criteria or more flexible diagnostic guidelines. When asked which format would allow for “maximum utility in clinical settings,” the large majority preferred “diagnostic guidance that is flexible enough to allow for cultural variation and clinical judgment” (78.3%; 74.8% weighted) to “clear and strict (specified) diagnostic criteria for all disorders” (21.7%; 25.2% weighted). This was consistent across users of ICD-10 and DSM-IV.
Severity
When asked what would be the best way to incorporate the concept of severity in the diagnostic system, respondents showed very little consensus beyond the general agreement that it should be included somehow (88.1%; 89.8% weighted). That is, there were three evenly split opinions regarding how to incorporate severity: (a) subtypes based on severity and/or symptom count (29.7%; 32.4% weighted); (b) subtypes based on degree of functional impairment (29.5%; 31.9% weighted); or (c) on a separate, “cross-cutting” axis used for all diagnoses (28.9; 25.5% weighted). No significant differences were found for DCS.
Functional impairment
Similar to the above item on severity, respondents were asked whether and how considerations of functional status should be conceptualized in a DCS. As shown in Figure 2, 76.9% (81.6% weighted) of participants provided responses indicating that it should be included somehow—most commonly, “for some disorders” when necessary (the middle choice between two opposite extremes). No significant differences were found for DCS.
Figure 2.
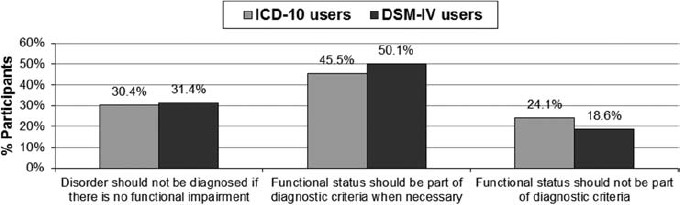
Clinicians’ opinions about what would be “the best way for a diagnostic system to conceptualize the relationship between diagnosis and functional status.” From left to right, the results for the overall sample are as follows: 28.7% (34.9% weighted), 48.2 % (46.8% weighted) 23.1% (18.4% weighted). Differences between ICD-10 and DSM-IV users are nonsignificant.
Dimensional component
As Figure 3 illustrates, when asked whether a DCS should include a dimensional component, the majority of participants (78.9%; 83.2% weighted) favored dimensional classification, whether for a “more accurate representation of psychopathology” or a “more detailed and personalized diagnosis.” The remainder responded that dimensional classification might be “too complicated for clinical settings” or there was “insufficient research on reliability.” No significant differences were found relating to DCS.
Figure 3.
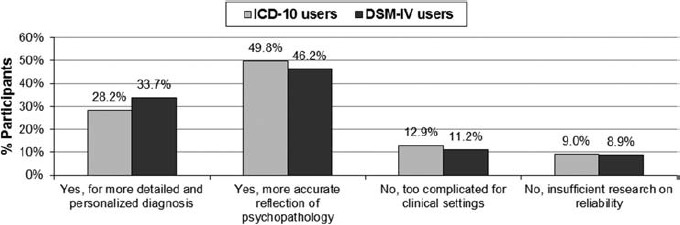
Clinicians’ views on whether to incorporate a dimensional component into a diagnostic classification system and why. From left to right, the results for the overall sample are as follows: 31.2% (34.1% weighted), 47.7% (49.1% weighted), 11.9% (9.6% weighted), 9.1% (7.2% weighted). Differences between ICD-10 and DSM-IV users are nonsignificant.
Depression and proportionality to adverse life events
Participants were asked whether a diagnosis should be “assigned if the symptoms are a proportionate response to adverse life events.” Responses were nearly evenly split: 51.2% (52.0% weighted) selected “Yes, if the full depressive syndrome is present, the diagnosis of depression should be made regardless …” and 48.8% (48.0% weighted) disagreed, responding, “No, a proportionate response to an adverse life event should not be considered a mental disorder.” No DCS-related differences were found.
Cultural concerns
Three items addressed concerns about the application of a DCS across different cultural backgrounds and contexts. Country-level results for these items are presented in Figure 4.
Figure 4.
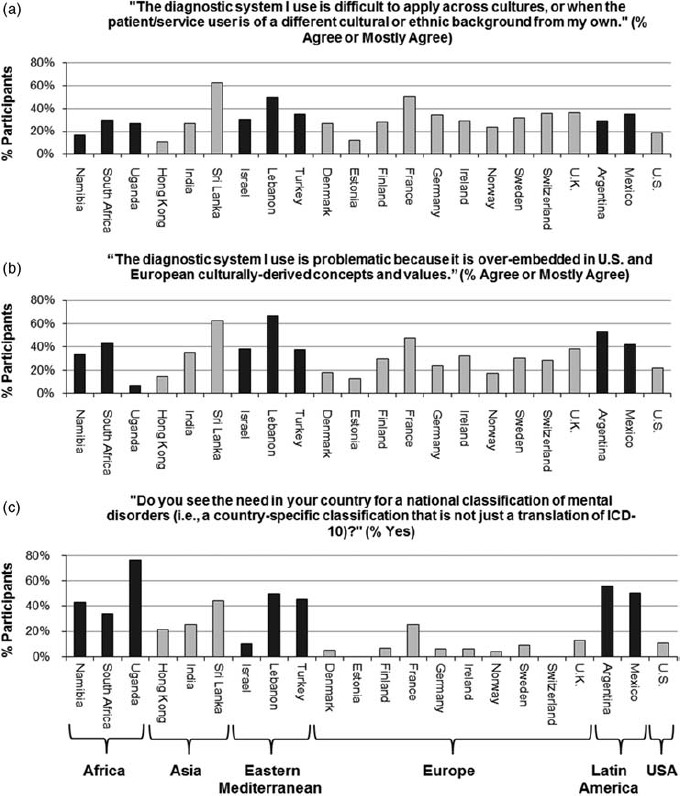
Percentages of respondents in each national subsample who indicated that they mostly/completely agreed with or responded yes to the above statements and question about (a) crosscultural problems, (b) US/European bias, and (c) the need for a national classification. Data from the Zimbabwean sample are not presented due to very low response on these items.
Crosscultural applicability
First, 30.8% (33.9% weighted) of clinicians completely or mostly agreed that “The diagnostic system I use is difficult to apply across cultures, or when the patient/service user is of a different cultural or ethnic background from my own.” About half (51.9%; 50.2% weighted) agreed somewhat. ICD-10 users and DSM-IV users did not differ in the extent to which they reported problems with crosscultural applicability; however, there were significant differences across regions, χ2 (15, N = 1513) = 43.68, p < .0001, V = .098. Psychologists from the Eastern Mediterranean, Latin America, Europe, and Africa (29–35% unweighted; 31–43% weighted) more often agreed that their DCS was crossculturally problematic compared to those from USA (18.4%) and Asia (20.0%; 33.4% weighted).
US and European bias
Similar to the previous item, 29.7% (36.3% weighted) of clinicians agreed (“mostly” or “completely”) that “The diagnostic system I use is problematic because it is over-embedded in US and European culturally-derived concepts and values,” and about half (48.7%; 42.3% weighted) agreed “somewhat.” Again, ICD-10 users and DSM-IV users did not differ in their views of cultural bias in their DCS, but there were regional differences, χ2 (15, N = 1512) = 45.91, p < .0001, V = .101. Respondents from Africa, the Eastern Mediterranean, and Latin America (38–45% unweighted; 46–48% weighted) more often agreed that US/European bias was a problem, compared to relatively fewer in Asia, the USA, and Europe (22–28% unweighted; 22–37% weighted).
Need for a national classification
When asked, “Do you see a need in your country for a national classification of mental disorders (i.e., a country-specific classification that is not just a translation of ICD-10)?”, 18.3% (28.0% weighted) of the overall sample responded “yes.” Unlike the previous two items, regional differences were larger and more consistent for this item (5, N = 1575) = 229.05, p < .0001, V = .381, and there were also significant differences for DCS, χ2 (1, N = 1,321) = 71.68, p < .0001, V = .233. Slightly more than half of the respondents from Latin America (51.3%; 53.0% weighted) indicated that they saw a need for a national DCS, as did large minorities of respondents from Africa (42.9%; 63.4% weighted), the Eastern Mediterranean (42.7%; 35.2% weighted), and Asia (24.8%; 30.5% weighted). By contrast, very few European (9.7%; 7.6% weighted) and American (10.5%) psychologists saw a need for a DCS specific to their country. Approximately one-quarter (26.5%) of DSM-IV users indicated a need for a national classification in their country, compared to only 9.0% of ICD-10 users. Those who endorsed a national classification system were asked to explain why. Open-ended responses commonly cited cultural differences about what constitutes psychopathology, culturebound syndromes, and differences in mental health service delivery.
Usage and evaluation of ICD-10 and DSM-IV diagnostic categories
Usage of diagnostic categories
Respondents who reported that they regularly see patients and use either the ICD-10 (N = 797) or the DSM-IV (N = 629) were asked to first select from a list of 44 (ICD-10) or 45 (DSM-IV) diagnostic categories which ones they use regularly (i.e., they see a patient or client with that diagnosis once a week or more), then evaluate those categories on two dimensions discussed below.2 Figures 5 and 6 present the percentages of clinicians who reported that they regularly use particular diagnostic categories from the ICD-10 and DSM-IV, respectively. Patterns of frequency were generally similar between ICD-10 and DSM-IV users and categories. Mood and anxiety disorders were by far the most commonly seen categories, and stress-related and childhood disorders were also seen relatively regularly. Less frequently seen were substance-related disorders, psychotic disorders, and eating disorders. Interestingly, individual clinicians saw an average of only 8.85 categories (SD = 5.69; weighted M = 9.77) regularly, with no significant difference between ICD-10 users and DSM-IV users. However, the average number of categories seen regularly varied greatly across countries, from 6.07 (SD = 4.92) in Argentina and 6.19 (SD = 4.12) in Hong Kong to 14.41 (SD = 6.57) in India.
Figure 5.
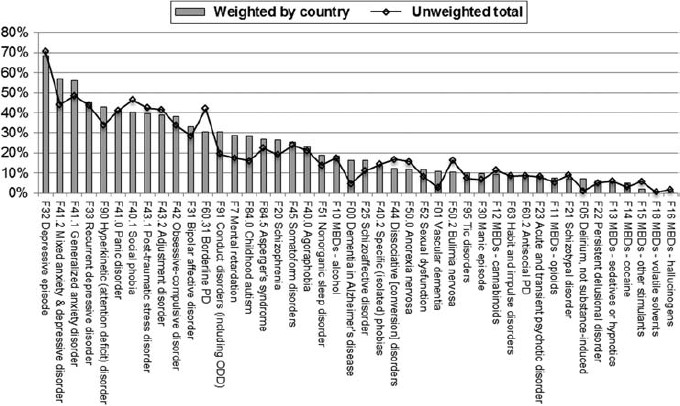
Percentages of clinicians who reported seeing persons with select ICD-10 diagnostic categories at least once a week. MBDs = mental and behavioral disorders (due to the use of a substance). PD = personality disorder.
Figure 6.
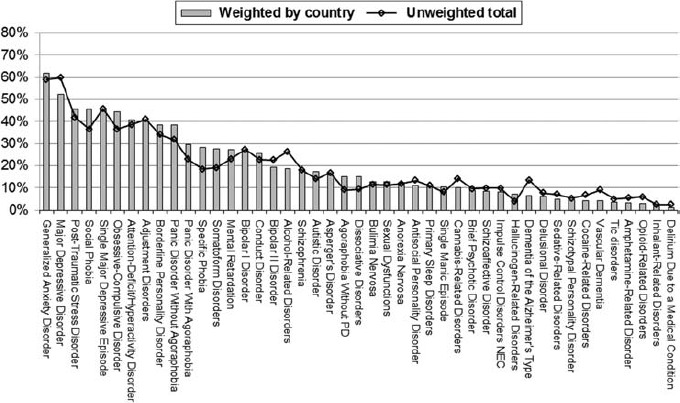
Percentages of clinicians who reported seeing persons with select DSM-IV diagnostic categories at least once a week. PD — panic disorder. NEC — not elsewhere classified.
Ease of use and goodness of fit of diagnostic categories
Next, clinicians were asked to evaluate each diagnostic category they reported using at least once per week in terms of two dimensions of clinical utility: ease of use and goodness of fit or accuracy in describing patients or clients (Reed, 2010). Note that this procedure was used to ensure that ease of use and goodness of fit ratings for each category were informed by clinical experience with patients with those particular diagnoses. Ease of use and goodness of fit ratings were made on the following four-point Likert scale: 0 = not at all (easy to use or accurate); 1 = somewhat; 2 = quite; and 3 = extremely. To facilitate comparisons, the original 0–3 scales were transformed to 0–1 scales (such that 0.00 = not at all, 0.33 = somewhat, 0.67 = quite, and 1.00 = extremely).
As presented in Figures 7 (ICD-10) and 8 (DSM-IV), clinicians’ ease of use and goodness of fit ratings were relatively favorable for diagnostic categories in both ICD-10 (ease of use: M = .641, SD = .076; goodness of fit: M = .600, SD = .072) and DSM-IV (ease of use: M = .657, SD = .076; goodness of fit: M = .597, SD = .075), with no differences between the two systems. Interestingly, nearly all diagnostic categories received higher mean ratings for ease of use than for goodness of fit. Participants’ ratings in these two dimensions were highly, but not perfectly correlated (ICD-10: M Pearson's r = .662, SD = .105; DSM-IV: M Pearson's r = .680, SD = .101). Table 3 lists the ICD-10 and DSM-IV categories with low mean ratings for ease of use and goodness of fit, i.e., those that fell at least one-half standard deviation below the overall mean.
Figure 7.
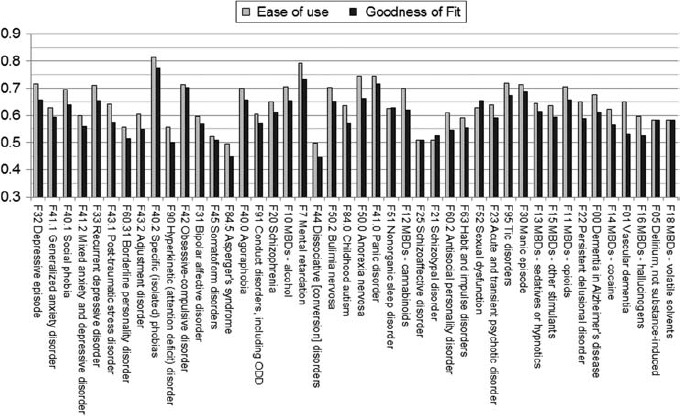
Clinicians’ unweighted mean ratings for the ease of use and goodness of fit of the ICD-10 diagnostic categories they see regularly. Categories are in order from most to least frequently seen, such that those toward the left were seen more often and therefore received more ratings, leading to more reliable estimates, than those near the right. MBDs — mental and behavioral disorders (due to the use of a substance).
Figure 8.
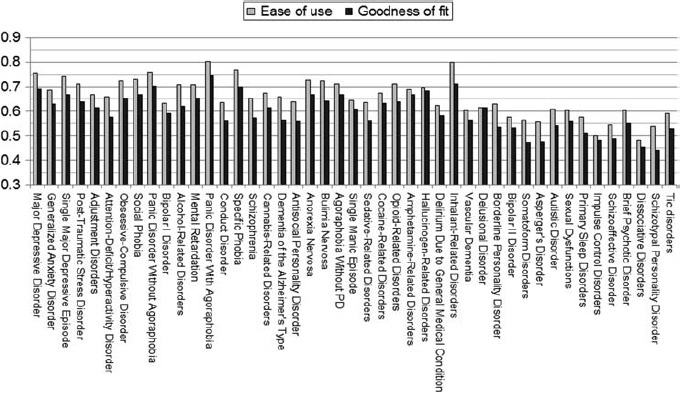
Clinicians’ unweighted mean ratings for the ease of use and goodness of fit of the DSM-IV diagnostic categories they see regularly. Categories are in order from most to least frequently seen, such that those toward the left were seen more often and therefore received more ratings, leading to more reliable estimates, than those near the right.
TABLE 3.
ICD-10 and DSM-IVdiagnostic categories with low ease of use and/or goodness of fit ratings
| ICD-10 Categories | EOU | GOF | DSM-IV Categories | EOU | GOF |
|---|---|---|---|---|---|
| Adjustment disorder | .603 | .550 | Asperger's disorder | .557 | .477 |
| Antisocial PD | .609 | .547 | Autistic disorder | .608 | .541 |
| Asperger's syndrome | .495 | .451 | Bipolar II disorder | .577 | .534 |
| Bipolar affective disorder | .596 | .570 | Borderline PD | .629 | .535 |
| Borderline PD | .556 | .514 | Brief psychotic disorder | .602 | .550 |
| Delirium, not substance induced | .583 | .583 | Delusional disorder | .615 | .615 |
| Dissociative [conversion] disorders | .497 | .447 | Dissociative disorders | .483 | .454 |
| Habit and impulse disorders | .591 | .554 | Impulse control disorders | .500 | .483 |
| Hyperkinetic (attention deficit) disorder | .556 | .500 | Primary sleep disorders | .576 | .510 |
| MBDs – hallucinogens | .595 | .524 | Schizoaffective disorder | .544 | .489 |
| MBDs – volatile solvents | .583 | .583 | Schizotypal PD | .538 | .441 |
| Mixed anxiety and depressive disorder | .599 | .560 | Sexual dysfunctions | .603 | .559 |
| Schizoaffective disorder | .508 | .508 | Somatoform disorders | .564 | .474 |
| Schizotypal disorder | .510 | .525 | Tic disorders | .593 | .531 |
| Somatoform disorders | .523 | .510 | Vascular dementia | .603 | .564 |
| Vascular dementia | .650 | .533 |
EOU — ease of use; GOF — goodness of fit; MBDs — mental and behavioral disorders (due to the use of substances). PD — personality disorder. Categories are considered to have a low ease of use or goodness of fit if the mean rating fell at least one-half standard deviation below the mean for all categories. Boldface type denotes these low ratings. All mean ratings are unweighted.
DISCUSSION
This study examined psychologists’ views on diagnostic classification systems in mental health care, with attention to differences across countries, regions, and ICD-10 users compared to DSM-IV users. Consistent with these objectives, the sample consisted largely of experienced, practicing clinicians from 23 countries around the globe. Despite differences in subsample size and representativeness, relatively large numbers of participants were obtained from each of the global regions examined, allowing for preliminary examinations of regional and DCS-related differences. In line with previous research, primary findings include: a preference for clinical utility, simplification, and flexibility in a DCS; disagreement regarding broad, conceptual questions of classification; relative satisfaction with most ICD-10 and DSM diagnoses, as well as areas for improvement; and many variations across countries and regions, but few differences between ICD-10 and DSM-IV users. These findings are discussed in greater detail below.
Professional practices of psychologists around the globe
This study offered interesting findings regarding the professional and diagnostic practices of psychologists around the world (Tables 1 and 2). Internationally, psychologists play a significant role—both individually and collaboratively with other professionals—in assessing and diagnosing persons with mental health problems. Although the majority of psychologists appear to use a DCS with some regularity in their clinical practice, a significant proportion rarely or never do so. Regarding usage of particular DCSs, results of this survey suggest that both the ICD-10 and DSM-IV are in widespread use by global psychologists, with European and Indian clinicians more likely to use the ICD-10 in their day-to-day clinical practice. There was a great deal of international variability in respondents’ diagnostic practices, which is likely related to international differences in the professional roles, experiences, and training backgrounds of psychologists (see Stevens & Wedding, 2004, for a review). External factors, such as service availability and healthcare policy, are also important to consider. For example, ICD diagnostic codes are a requirement for public or private health care reimbursement in some countries, but may not be obligatory for the provision of care in other countries where the rate of DCS usage among psychologists was found to be lower.
Findings on psychologists’ practice patterns and use of DCSs differed considerably from those of psychiatrists in the WPA-WHO survey (Reed et al., 2011). Compared to psychiatrists, psychologists reported fewer patient contact hours; seeing patients with a narrower range of diagnoses on a regular basis; using DCSs less frequently overall, with greater variability of DCS use among countries; with a lower proportion reporting the use of the ICD-10 in daily clinical practice and a higher proportion using the DSM-IV. These differences, and others discussed below, may be explained by differences in training, services delivered, professional activities, patient populations, and theoretical perspectives. They are also likely influenced by health system policies and characteristics. For example, across countries psychiatrists may be more likely than psychologists to be required to report diagnoses for routine encounters in clinical settings. Of course, the present sample and the WPA-WHO survey sample are not equivalent in terms of global representation, so comparisons between the results of the two studies should be made with caution and viewed primarily as a source of hypotheses for further investigation.
Views on diagnostic classification in mental health care
Participants’ views on general features of diagnostic systems were surprisingly consistent across countries, regions, DCSs, and with previous research; however, consistency should not be interpreted as consensus. That is, distributions of responses were similar across subsamples, but there were few cases in which a clear majority of the overall sample preferred one view to another. In line with previous research (Bell et al., 2008; Mellsop et al., 2007a, 2007b, 2011; Reed et al., 2011; Suzuki et al., 2010), a large majority (87.6%) of psychologists indicated that the most important purposes of a DCS were related to clinical care and communication (i.e., treatment/management decisions, interclinician communication, and communication with patients), as opposed to nonclinical purposes, such as research and health statistics (Figure 1). Interestingly, within those clinically oriented responses were differences between psychologists, who endorsed clinical treatment/management as the top priority, and psychiatrists, who in previous research consistently emphasized interclinician communication as paramount (Bell et al., 2008; Mellsop et al., 2007a, 2007b, 2011; Reed et al., 2011; Suzuki et al., 2010).
Across all regions, DCSs, and consistent with findings among psychiatrists (Bell et al., 2008; Mellsop et al., 2007a, 2007b, 2011; Reed et al., 2011; Suzuki et al., 2010), psychologists decidedly preferred a DCS with fewer diagnostic categories (i.e., less than 100 categories). These findings stand in contrast to the actual contents of the DSM-IV and ICD-10, which both contain well over 200 categories, depending on how they are counted. Psychologists, like psychiatrists, also overwhelmingly preferred flexible diagnostic guidelines rather than strict criteria, and this was equally true of ICD-10 and DSM-IV users. This finding is interesting because the provision of flexible guidance that allows for clinical judgment and cultural variation has been characteristic of WHO's approach (WHO, 1992b), in contrast to the rigid criterion counting that characterizes the DSM-IV. Thus, the results of this survey lend additional support to calls for nosological simplification (e.g., Flanagan & Blashfield, 2010) and suggest that a “symptom checklist” (e.g., DSM-IV) approach may be less clinically useful than more flexible and conceptual guidelines. Consistent with previous findings among psychiatrists (Reed et al., 2011), most psychologists agreed that concepts of functional impairment, severity, and dimensional classification were essential to include in a DCS, but with little agreement as to how or why (Figures 2 and 3). Differences between regional and DCS groups were often nonsignificant or of a very small effect size, suggesting that the differences of opinion on these items are common and widespread, even among clinicians in the same countries and regions.
Psychologists’ opinions were also divided on the question of diagnoses and proportionality to adverse life events. However, these results reveal interesting disciplinary differences: Nearly two-thirds of global psychiatrists supported the practice of making a diagnosis of depression regardless of whether symptoms can be seen as a proportionate response to adverse life events (Reed et al., 2011), but only half of psychologists shared this opinion. One explanation may be that, globally, psychologists are more often able to provide psychotherapy services in the absence of a formal diagnosis, while psychiatrists may be more frequently required to assign a diagnosis before treatment, particularly in the case of pharmacotherapy.
Results show that psychologists in the Eastern Mediterranean, Africa, and Latin America experience significant problems relating to the crosscultural applicability of DCSs. Compared to those in the USA and Europe, respondents from these regions were approximately twice as likely to report problems relating to US/European bias and four to five times as likely to endorse the need for a national DCS. These results provide empirical support for the notion that the clinicians who have the greatest degree of culture-related difficulties in applying the DSM-IV and ICD-10 are those who live and work outside of the USA and Europe. But even in Western, developed nations, relatively large percentages of participants reported culturally relevant problems with their DCS. These findings represent significant challenges to be addressed by future research and clinical endeavors in global mental health.
Identifying and improving upon problematic diagnoses
Although the average number of categories seen regularly varies greatly across countries, psychologists encounter relatively few diagnoses on a regular basis, especially when compared to psychiatrists (Reed et al., 2011). The practices of global psychologists appear to focus more on anxiety disorders, depressive disorders, and disorders specifically associated with stress such as PTSD and adjustment disorder (see Figures 5 and 6). In comparison with psychiatrists (Reed et al., 2011), psychologists’ practices focus less on schizophrenia and other psychotic disorders, bipolar disorders, and substance use disorders. This makes sense considering that psychosocial interventions are generally regarded as first-line treatments for the former group of disorders, while the latter group of disorders is more likely to be treated with medication.
Most diagnostic categories were evaluated relatively favorably in terms of their ease of use and goodness of fit, regardless of whether the ratings referred to ICD-10 or DSM-IV categories (Figures 7 and 8). So it appears that while individual psychologists may hold mixed opinions toward the ICD-10 or DSM-IV overall, this may be due to a small number of diagnoses viewed as problematic. This interpretation offers a more encouraging picture than the literature offering criticisms and recommendations for the DSM-5 and the ICD-11. Interestingly, nearly all diagnoses received higher ratings for their ease of use than for their accuracy in describing patients, suggesting relatively more problems with descriptive utility/validity, even when diagnostic descriptions are easy to apply.
Specific problems were identified with the utility and accuracy of a number of diagnoses (Table 3). Many of these “problematic” ICD-10 and DSM-IV categories are not surprising given the volume of recent literature questioning their validity and utility as they are currently formulated (e.g., Asperger's disorder, borderline personality disorder, schizoaffective disorder). But results also point to diagnostic entities (e.g., dissociative and somatoform disorders) that have seen less critical discussion within the literature, but nevertheless appear to be clinically problematic and therefore may warrant a greater degree of attention and reformulation during the ICD revision process, as well as greater emphasis in ICD-11 training efforts.
Notably, there were no significant differences between ratings of ICD-10 and DSM-IV categories overall. However, there were some differences for specific categories, suggesting relative strengths and weaknesses in both DCSs. For example, hyperkinetic (attention-deficit/hyperactivity) disorder and antisocial personality disorder were rated as more problematic in ICD-10 than in DSM-IV. Conversely, DSM-IV autistic disorder and brief psychotic disorder appear to be more clinically problematic than their ICD-10 counterparts. Present and future DCS revision efforts should draw upon the relative strengths and weaknesses among different diagnostic formulations in the ICD, DSM, and other systems.
Limitations
This study's main limitations are related to participant selection and representativeness. Because participants were solicited through their membership in national psychological associations, they may not be representative of the larger professional populations within each country, and countries without associations could not be represented. Additionally, the majority of participants were from high-income, European countries, and the number of participants from non-Western and developing nations was relatively low. On the other hand, there are many times fewer psychologists in developing countries (WHO, 2011), and the degree of their inclusion in the present survey is extremely favorable compared to past efforts. These findings may not be interpreted as representative of all countries within a region or all users of a particular DCS. Rather, generalizability may be limited to the 23 countries represented, and results for very low-N countries (e.g., Zimbabwe) should be interpreted with particular caution.
In addition, diagnostic categories were evaluated only by clinicians who saw them regularly, so evaluations based on data from fewer respondents (e. g., inhalant-related disorders) should be interpreted as less reliable than those based on more ratings (e.g., major depressive disorder). Further, data were not collected on participants’ training and countries’ regulatory practices, factors that are likely to influence psychologists’ experiences and views regarding classification and diagnosis. Finally, these findings should not be interpreted as realities of global mental health, but as the experiences and opinions of psychologists in diverse contexts.
Implications and future directions
To date, this investigation represents the second largest clinician survey on the diagnostic classification of mental disorders, and the first study of its kind to be conducted among a global sample of psychologists, a largely unexamined professional population within global mental health. The Internet-based format allowed for greater participation from professionals in developing regions. Given the ubiquity of Internet access among health professionals and the increasing collaboration among national and international organizations, studies such as this provide examples of how global practitioner research can be conducted quite feasibly and successfully, even in relatively low-resource settings.
These findings have several implications for the development of the ICD-11, including revisions for specific diagnostic categories and broad, crosscutting features. For example, results suggest that the ICD-11 should be designed for utility in clinical treatment, management, and communication purposes, with flexible diagnostic guidelines and fewer categories. This is not to say that the revisions are democratically determined; rather, findings offer insight into the views of psychologists, which will be used, along with other sources of data (e.g., Reed et al., 2011, 2013; Roberts et al., 2012) and available research to inform decision-making by the relevant groups charged with the development of the ICD-11 classification of mental and behavioral disorders. Additionally, these results will serve as baseline data for future research on the clinical utility, reliability, and validity of ICD-11 categories, with immediate relevance for the ICD-11 field trials. Lastly, beyond diagnostic revisions and field trials, findings will help inform future efforts aimed at ICD-11 adaptation, translation, dissemination, and training.
The present study also suggests some directions for further international research among clinicians. More research is needed to better understand the unique sociocultural and medical factors (e.g., stigma, treatment access) operating within specific countries and in mental health service delivery around the globe. Toward that end, WHO's Department of Mental Health and Substance Use is preparing for the next phase of ICD-11 research. Incorporating the findings of the present study, these efforts will be aimed at the development of a diagnostic system that, compared to its predecessors, is more valid, reliable, and clinically useful within the challenging context of global mental health care.
Footnotes
For two associations, India and Israel, solicitation data were not recorded but response data were collected from 54 and 40 participants, respectively. Thus, the true total number of solicitations was at least 7045; however, response rates could only be calculated with available data from the 6911 recorded solicitations in 21 countries.
Because the conditional administration of these items was not reliably implemented in the paper-and-pencil version of this survey, responses from the Ugandan sample were excluded from these analyses.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text rev.) Washington, DC: APA; 2000. [Google Scholar]
- American Psychiatric Association. DSM-5 Development. 2013. Retrieved from www.dsm5.org. [Google Scholar]
- Bell C. C., Sowers W., Thompson K. S. American Association of Community Psychiatrists’ views on general features of DSM-IV. Psychiatric Services. 2008;59:687–689. doi: 10.1176/ps.2008.59.6.687. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power and analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- First M. B. Clinical utility: A prerequisite for the adoption of a dimensional approach in DSM. Journal of Abnormal Psychology. 2005;114:560–564. doi: 10.1037/0021-843X.114.4.560. [DOI] [PubMed] [Google Scholar]
- First M. B. Clinical utility in the revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM) Professional Psychology: Research and Practice. 2010;41:465–473. [Google Scholar]
- First M. B., Westen D. Classification for clinical practice: How to make ICD and DSM better able to serve clinicians. International Review of Psychiatry. 2007;19:473–481. doi: 10.1080/09540260701563429. [DOI] [PubMed] [Google Scholar]
- Flanagan E. H., Blashfield R. K. Increasing clinical utility by aligning the DSM and ICD with clinicians’ conceptualizations. Professional Psychology: Research and Practice. 2010;41:474–481. [Google Scholar]
- International Advisory Group for the Revision of the ICD-10 Mental and Behavioural Disorders. A conceptual framework for the revision of the ICD-10 classification of mental and behavioural disorders. World Psychiatry. 2011;10:86–92. doi: 10.1002/j.2051-5545.2011.tb00022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maser J. D., Kaelber C., Weise R. E. International use and attitudes toward DSM-III and DSM-III-R: Growing consensus in psychiatric classification. Journal of Abnormal Psychology. 1991;100:271–279. doi: 10.1037//0021-843x.100.3.271. [DOI] [PubMed] [Google Scholar]
- Mellsop G., Dutu G., Pereira M., Nagamine M., Shinfuku N., Banzato C. An international study of the views of psychiatrists on present and preferred characteristics of classifications of psychiatric disorders. International Journal of Mental Health. 2007a;36:17–25. [Google Scholar]
- Mellsop G., Dutu G., Robinson G. New Zealand psychiatrists’ views on global features of ICD-10 and DSM-IV. Australian and New Zealand Journal of Psychiatry. 2007b;41:157–165. doi: 10.1080/00048670601109931. [DOI] [PubMed] [Google Scholar]
- Mellsop G., Lutchman R., Lillis S., Dutu G. European Psychiatry, 26, 61–63. 2011. The views of psychiatrists, general practitioners, psychologists, and consumers on aspects of present and preferred classification systems. [Google Scholar]
- Mezzich J. E. International surveys on the use of ICD-10 and related diagnostic systems. Psychopathology. 2002;35:72–75. doi: 10.1159/000065122. [DOI] [PubMed] [Google Scholar]
- Mullins-Sweatt S. N., Widiger T. A. Clinical utility and DSM-V. Psychological Assessment. 2009;21:302–312. doi: 10.1037/a0016607. [DOI] [PubMed] [Google Scholar]
- Müssigbrodt H., Michels R., Malchow C. P., Dilling H., Munk-Jørgensen P., Bertelsen A. Use of the ICD-10 classification in psychiatry: An international survey. Psychopathology. 2000;33:94–99. doi: 10.1159/000029127. [DOI] [PubMed] [Google Scholar]
- Reed G. M. Toward ICD-11: Improving the clinical utility of WHO's international classification of mental disorders. Professional Psychology: Research and Practice. 2010;41:457–464. [Google Scholar]
- Reed G. M., Correia J. M., Esparza P., Saxena S., Maj M. The WP A-WHO global survey of psychiatrists’ attitudes toward mental disorders classification. World Psychiatry. 2011;10:118–131. doi: 10.1002/j.2051-5545.2011.tb00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed G. M., Roberts M. C., Keeley J. W., Hooppell C., Matsumoto C., Sharan P., et al. Mental health professionals’ natural taxonomies of mental disorders: Implications for clinical utility of ICD-11 and DSM-5. 2013. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Roberts M. C., Reed G. M., Medina-Mora M. E., Keeley J. W., Sharan P., Johnson D. K., et al. A global clinicians’ map of mental disorders to improve ICD-11: Analyzing meta-structure to enhance clinical utility. International Review of Psychiatry. 2012;24:578–590. doi: 10.3109/09540261.2012.736368. [DOI] [PubMed] [Google Scholar]
- Sartorius N., Kaelber C. T., Cooper J. E., Roper M. T., Rae D. S., Gulbinai W., et al. Progress toward achieving a common language in psychiatry: Results from the field trial of the clinical guidelines accompanying the WHO classification of mental and behavioral disorders in ICD-10. Archives of General Psychiatry. 1993;50:115–124. doi: 10.1001/archpsyc.1993.01820140037004. [DOI] [PubMed] [Google Scholar]
- Sechter D. Survey of the use of international classification (DSM III-R, ICD-10) in France, in private and public psychiatry. Encephale. 1995;21:35–38. [PubMed] [Google Scholar]
- Stevens M. J., Wedding D., editors. The handbook of international psychology. New York: Brunner-Routledge; 2004. [Google Scholar]
- Suzuki Y., Takahashi T., Nagamine M., Zou Y., Cui J., Han B., et al. Comparison of psychiatrists’ views on classification of mental disorders in four east Asian countries/area. Asian Journal of Psychiatry. 2010;3:20–25. doi: 10.1016/j.ajp.2009.12.004. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International classification of diseases and related health problems. 10th rev. Geneva, Switzerland: WHO; 1992a. [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: WHO; 1992b. [Google Scholar]
- World Health Organization. Mental health atlas 2011. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- World Health Organization. Classifications: Revision of the International Classification of Disease (ICD) 2013. Retrieved April 1, 2013, from www.who.int/classifications/icd/ICDRevision. [Google Scholar]
- Zielasek J., Freyberger H. J., Janner M., Kapfhammer H. P., Sartorius N., Stieglitz R. D., et al. Assessing the opinions and experiences of German-speaking psychiatrists regarding necessary changes for the 11th revision of the mental disorders chapter of the International Classification of Disorders (ICD-11) European Psychiatry. 2010;25:437–442. doi: 10.1016/j.eurpsy.2009.12.023. [DOI] [PubMed] [Google Scholar]


