Abstract
Background
Borderline personality disorder (BPD) often presents during adolescence. Early detection and intervention decreases its subsequent severity. However, little is known about early predictors and biological underpinnings of BPD. The observed abnormal functional connectivity among brain regions in BPD led to studies of white matter, as the neural substrate of connectivity. However, diffusion tensor imaging (DTI) studies in adult BPD have been inconclusive, and, as yet, there are no published DTI studies in borderline adolescents.
Methods
We conducted DTI tractography in 38 BPD patients (14-adolescents,24-adults) and 32 healthy controls (13-adolescents,19-adults).
Results
We found bilateral tract-specific decreased fractional anisotropy (FA) in inferior longitudinal fasciculus (ILF) in BPD adolescents compared to adolescent controls. ILF FA was significantly higher in adolescent controls compared to BPD adolescents, BPD adults and adult controls (WilksF(3,57)=3.55, p<0.02). Follow-up voxelwise TBSS analysis demonstrated lower FA in BPD adolescents compared to adolescent controls also in uncinate and occipitofrontal fasciculi.
Discussion
FA generally develops along an inverted U-shape curve, increasing through adolescence, and slowly decreasing in adulthood. Our findings suggest that, in adolescent BPD, this normal developmental “peak” in FA, which is seen in healthy controls, is not achieved. This suggests a possible neural substrate for the previously reported OFC-amygdala disconnect in adults with BPD. It raises the possibility that a white matter tract abnormality in BPD present in adolescence may not be appreciable in adulthood, but a functional abnormality in the coordination among brain regions persists. Our finding represents a possible biological marker to identify those at risk for developing BPD.
Introduction
Borderline personality disorder (BPD) is a complex and serious mental disorder characterized by emotional dysregulation, poor impulse control and impaired interpersonal relationships (New et al., 2008b) with a substantial risk for completing suicide (Leichsenring et al., 2011). The full manifestations of BPD become evident during adolescence (Goodman et al., 2010), and it is in adolescence when individuals with BPD usually seek treatment (Chanen et al., 2008a). BPD can be diagnosed in adolescents using similar diagnostic instruments to those used in adults (Chanen et al., 2008b). Early detection and intervention in BPD has been shown to decrease symptom severity and improve functioning (Chanen et al., 2008a). However, little is known about early predictors and biological underpinnings of BPD. In the present study, we aimed to fill this gap in knowledge by searching for a biomarker that could help with earlier identification of BPD in young people.
Neuroimaging findings in adult BPD
The neuroimaging literature in BPD patients is rapidly growing (Mauchnik & Schmahl, 2010; New et al., 2008a), and studies support the hypothesis of a dysfunctional frontolimbic network in BPD, which appears to involve anterior cingulate cortex (ACC), orbitofrontal cortex (OFC), dorsolateral prefrontal cortex (DLPFC), hippocampus, and amygdala. It is believed that alterations in this network are related to the diminished top-down control of affective and aggressive responses (Leichsenring et al., 2011; New et al., 2008b). The most consistent structural imaging finding in adult BPD is a decrease in gray matter volume in ACC (Hazlett et al., 2005; Minzenberg et al., 2008; Tebartz van Elst et al., 2003) and hippocampus (Brambilla et al., 2004; Irle et al., 2005; Nunes et al., 2009; Zetzsche et al., 2007). Other findings include volume reduction in the left OFC (Tebartz van Elst et al., 2003) and amygdala (Nunes et al., 2009).
One theory as to what might underlie the striking symptoms of emotional lability and hyper-reactivity which characterizes BPD is that the coordinated function among brain areas is abnormal, and in fact, we previously showed a marked functional disconnect between OFC and amygdala in adult BPD (New et al., 2007). This observation led to an examination of white matter in BPD as the neural substrate of connectivity. To date, only three diffusion-tensor imaging (DTI) studies have been published in adults with BPD (Grant et al., 2007; Rusch et al.; Rusch et al., 2007). One found decreased fractional anisotropy (FA) in the OFC in women with BPD compared to controls (Grant et al., 2007), although another showed no significant difference in DTI between adults with both BPD and attention-deficit hyperactivity disorder (ADHD) and controls, but did find a correlation between FA and lifetime depressive symptoms (Rusch et al., 2007). The same group recently found impaired inter-hemispheric structural connectivity in BPD subjects with ADHD (Rusch et al., 2010).
Neuroimaging findings in adolescent BPD patients
Structural neuroimaging data in adolescent BPD is limited. One study found volume reduction in left ACC (Whittle et al., 2009), while another found reductions in dorsolateral PFC and OFC, but not ACC (Brunner et al., 2010). Other studies reported right-sided OFC gray matter reduction in adolescent BPD, but not in amygdala or hippocampus (Chanen et al., 2008d). In a sample overlapping with the present sample, we found that adolescents with BPD and MDD had decreased ACC gray matter volume compared to healthy controls (Goodman et al., 2010). There have been no published DTI studies in borderline adolescents to date.
Developmental changes in DTI
While structural imaging provides quantitative information about brain tissue volume, DTI provides information about the white matter tracts connecting brain regions. There are profound developmental changes in white matter, reflected in the outcome measure of DTI most commonly used, Fractional Anisotropy (FA), thought to reflect both myelination and organized directionality of white matter tracts (Madler et al., 2008). The developmental trajectory exhibited in most white matter tracts includes a sharp increase in FA up to the age of 2 to 3 years, followed by a gradual increase through adolescence and into the mid-third decade (Asato et al., 2010; Bava et al., 2010; Trivedi et al., 2009; Westlye et al., 2010). While FA increases progressively through adolescence, there is a leveling off and slow decrement of FA in adulthood (Hasan et al., 2010).
Little is known to date about the developmental trajectory of either structural brain imaging or DTI in BPD. Some structural alterations in BPD are observed both in adolescents and adults, while others have only been reported either early or late in the development of the disorder. It has been suggested that volume changes in prefrontal cortex may appear early in BPD, while volume changes in limbic structures might appear later as a function of the course and/or severity of BPD (Brunner et al., 2010; Chanen et al., 2008c). Since there are no published DTI studies in borderline adolescents, the developmental trajectory of white matter tracts in BPD remains unanswered. The present study aims to address this question by comparing DTI findings in two samples of BPD patients (adolescents and adults) and two age-and sex-matched healthy control (HC) samples.
Methods
Adolescent samples
Twenty-seven adolescents (14 BPD, 13 HC matched by age and sex) underwent diagnostic and structural brain imaging with DTI. BPD patients met DSM-IV (SCID-II)(First, 1997) and Diagnostic Interview for BPD-revised (DIB-R) criteria for BPD (Zanarini et al., 2002), while controls had no current axis I or II diagnosis as assessed by the SCID-I/P (First, 2002) and SCID-II. The DIB-R was included to ensure that adolescent BPD subjects met a high threshold level for BPD diagnosis. Adolescent BPD patients were recruited from the adolescent psychiatric inpatient service at The Mount Sinai Hospital in New York City, and HC were recruited from the surrounding community by advertisements. All except one adolescent BPD subject also met criteria for current MDD. Adolescents were excluded for 1) history of serious head injury or neurological disorder; 2) schizophrenia, any other psychotic disorder, bipolar disorder type I or pervasive developmental disorder.
Adult samples
Twenty-four adult BPD patients and 19 adult HC (1 excluded due to MRI artifact) matched by sex and age completed the study. Individuals from 18-55 years of age were recruited through local newspaper advertisements and clinical referral. Subjects were excluded for: 1) history of serious head injury or neurological disorder; 2) current alcohol and/or drug abuse or dependence; 3) schizophrenia, any other psychotic disorder or bipolar disorder type I; or 4) current psychiatric medication. Axis I disorders were assessed with the SCID-I/P and Axis II with the SIDP-IV (Pfohl et al., 1996). Healthy controls had no personal history of Axis I or II diagnoses.
This study was approved by Mount Sinai’s Institutional Review Board. All adult participants provided written informed consent prior to participation. Assent was obtained for adolescents and written informed consent was obtained from each adolescent subject’s parent or guardian.
Self report measures
Depressive symptoms were assessed with the Beck Depression Inventory (Beck et al., 1961); trait aggression was measured with the Buss Perry Aggression Questionnaire (BPAQ), a 29-item questionnaire (Buss & Perry, 1992), and the State-Trait Anger Expression Inventory (STAXI) (Spielberger et al., 1983). Affect lability was measured with the Affect Lability Scale (ALS), a 54-item self-report measure in which subjects rate their agreement with statements regarding the tendency of their mood to shift (Harvey et al., 1989). Impulsivity was measured with the Barratt impulsivity scales-11 (BIS) (Barratt, 1965), a 34-item questionnaire that assess motoric (acting without thinking), cognitive (hasty decisions) and nonplanning (failure to plan ahead) impulsiveness. Each item is rated on a 4-point scale ranging from “Rarely/Never” to “Almost always/ Always” (Patton et al., 1995).
DTI Methods
DTI was acquired on a 3T Allegra MRI scanner (Siemens, Ehrlangen, Germany) with the following parameters: a pulsed-gradient spin-echo sequence with EPI-acquisition (TR=4100ms, TE=80ms, FOV=21cm, matrix=128×128, 28 slices, thickness=3mm skip 1mm, b-factor=1250s/mm2, 12 gradient directions, 5 averages).
DTI-tractography was implemented in Matlab v2009 (The Mathworks) and used the brute-force (Huang et al., 2004), streamline (Mori & Barker, 1999) algorithm with multiple anatomical criteria for each tract to increase the validity of the tractography (Huang et al., 2004). Streamline termination criteria for FA was <0.10 and for inter-voxel deflection was (>45°). To minimize inter-subject variance and maximize reproducibility, all anatomical tracking criteria were defined on a study-specific template that was created with the tract-based spatial statistics package (TBSS) of FSL (FSL, Oxford, www.fmrib.ox.ac.uk/fsl). Tracking criteria were converted from template coordinates to each subject’s DTI image using the transformation determined by the TBSS routine. For a more detailed description of the tractography methods see Carpenter et al. (Carpenter et al., 2008). The anatomical definitions for tracking the genu and splenium of the corpus callosum, bilateral inferior longitudinal fasciculus (ILF), and bilateral cingulum bundle were established previously by Wakana et al. (Wakana et al., 2007).
The TBSS voxel-wise statistical analysis was also used to further investigate the tractography findings in the ILF in adolescents. The analysis was conducted to answer two questions: 1) Are the changes in FA that were identified using tractography localized to any portion of the ILF? 2) Are the differences in FA unique to the ILF or are they present in other tracts of the temporal lobe, not assessed in our tractography analysis, including the uncinate fasciculus and the occipitofrontal fasciculus. The JHU White-Matter Tractography Atlas provided with FSL was used to limit the TBSS analysis to the ILF, uncinate and occipitofronal fasciculus. For completeness, the results of a whole brain TBSS analysis are reported. Hypothesis testing was performed with the TFCE (Threshold-Free Cluster Enhancement) option in randomize of FSL and significance was determined by p<0.05 family-wise error corrected for multiple comparisons.
For comparison of the interaction of diagnostic group and age cohort, we performed a mixed factorial repeated measures analysis of variance on FA in an age cohort (adolescent, adult) × group (BPD, HC) × sex (male, female) × tract analysis (forceps major, forceps minor, cingulum [mean right and left], and ILF [mean right and left]), including Beck Depression Scale as a covariate since most adolescents met criteria for MDD while all but one adult subject did not.
Results
See Table 1 for clinical characteristics and self-report instruments scores. Demographic and clinical measures were compared using student’s t test for continuous and Chi-square for categorical variables. Although within age groups (adolescent and adult samples respectively) BPD patients and HCs were matched by age and sex, there were significant differences in the gender distribution of adolescent BPDs compared to adult BPDs (Yates’ chi-square= 12.5; df=1; p=0.0004). Adolescent BPDs had a higher proportion of females, while adult BPDs had a higher proportion of males. Therefore, sex was included as a factor in all of the analyses comparing outcome measures across the two age groups. Since most adolescents met criteria for MDD while all but one adult subject did not, we also included Beck Depression Scale as a covariate in the analyses across the two age groups. Because BPD adolescents also differed from BPD adults in aggression scores (BPAQ) and trait Anger (STAXI-T) (See Table 1) we repeated the analyses adding these measures as covariates.
Table 1.
Descriptive Characteristics of the adult and adolescent samples.
| Adolescents | Adults | |||
|---|---|---|---|---|
| Groups | HC (n=13) | BPD (n=14) | HC (n=18) | BPD (n=24) |
| Age (years) | 16.2 (0.8) | 15.8 (1.1) | 28.6 (6.9) | 32.0 (9.0) |
| Sex | 9F, 4M | 12F, 2M *** | 6F, 12M | 5F, 19M *** |
| ALS | 28.8 (26.1) | 92.4 (26.9) # | 19.5 (20.3) | 97.3 (23.6) # |
| BIS-11 | 74.5 (4.3) | 73.8 (5.3) | 48.2 (7.9) | 75.0 (8.8) # |
| BPAQ | 46.1 (7.6) | 52.3 (23.9)**# | 41.7 (7.3) | 76.2 (9.7)**# |
| BDI | 2.3 (4.2) | 20.8 (12.4) # | 1.1 (2.3) | 19.2 (7.3) # |
| STAXI-T | 13.9 (3.5) | 21.8 (6.5)*# | 13.1 (2.2) | 28.2 (7.4)*# |
ALS = Affective Lability Scale; BIS-11 = Barratt Impulsivity Scale; BDI = Beck Depression Inventory; STAXI-T = State-Trait Anger Expression Inventory II, trait anger; BPAQ = Buss-Perry Aggression Questionnaire. For contrast between adolescent BPD and adult BPD:
p < 0.02;
p = 0.0001;
p=0.0004.
For contrast between BPD and HC in adolescents and adults separately:
p<0.001. Uncorrected p values reported.
See Table 2 for Axis I diagnoses in adolescent and adult BPDs. See Table 3 for medication list for the adolescent subjects. Adult subjects were not on medication at the time of study. Although adult BPDs were collected in an outpatient setting and adolescent BPDs on an inpatient unit, they did not differ in severity of affective lability, impulsivity, or depression. However, adult BPDs showed more aggression and state anger. Our adolescent sample overlaps with a sample in which we reported regional brain volumes but not DTI (Goodman et al., 2010), in that 10 of the 14 BPD and all the HC subjects were included in that analysis.
Table 2.
Axis I comorbidity in BPD groups.
| Adolescents | Adults | |
|---|---|---|
| MDD now | 11/14 | 1/24 |
| MDD past | 12/14 | 23/24 |
| Dysthymia | 2/14 | 1/24 |
| OCD | 1/14 | 2/24 |
| Social phobia | 0/14 | 4/24 |
| PTSD now | 2/14 | 4/24 |
| PTSD past | 2/24 | 8/24 |
| ODD | 9/14 | N/A |
| ADHD | 4/14 | N/A |
MDD now=current major depressive disorder, MDD past, past history of major depressive disorder, OCD= obsessive compulsive disorder, PTSD now=current post traumatic stress disorder, PTSD past= past post-traumatic stress disorder, ODD= oppositional defiant disorder, ADHD= attention deficit disorder.
Table 3.
Medications for adolescent BPD sample.
| 1. methylphenidate, bupropion |
| 2. aripiperazole |
| 3. escitalopram |
| 4. aripiperazole, citalopram |
| 5. sertraline |
| 6. citalopram |
| 7. sertraline |
| 8. fluoxetine |
| 9. None |
| 10. fluoxetine, escitalopram |
| 11. escitalopram, amphetamine/dextro-amphetamine, lamotrigine, aripiperazole |
| 12. fluoxetine |
| 13. sertraline, fluoxetine, risperidone |
| 14. None |
Table 3 describes current medications for each subject in our adolescent BPD sample. Adult subjects were taking no medications at the time of study.
T-tests comparing FA between BPD and HC in the major white matter tracts (i.e. forceps major, forceps minor, left cingulum, right cingulum, left ILF, right ILF) in the adolescent sample showed a tract-specific bilateral decrease in FA in the ILF of BPD adolescents compared to HC adolescents (left ILF t=3.13 p<0.005; right ILF t=2.92 p<0.008; p>0.1 for other tracts). See Figure 1. T-tests comparing FA between adult BPD and HC in the same major white matter tracts showed no significant group differences.
Figure 1. DTI Tractography Comparing Adolescent Borderline Personality Disorder and Adolescent Healthy Controls.
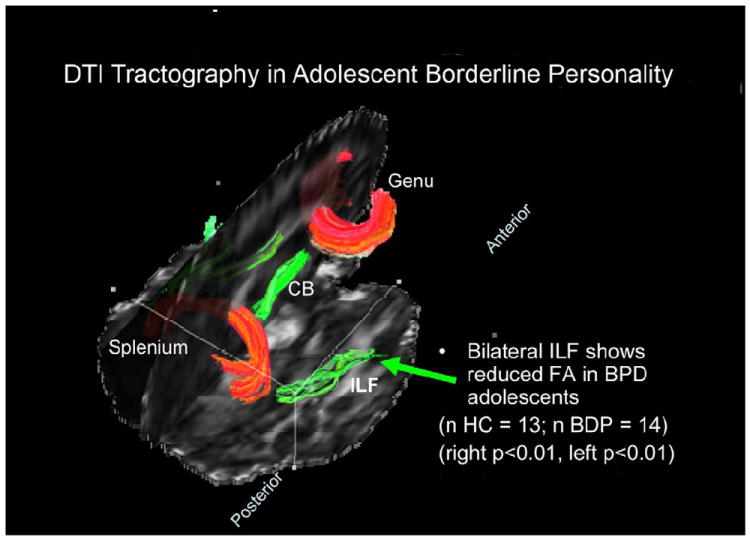
Adolescents with BPD showed reduced FA in Inferior Longitudinal Fasciculus (in green) in both hemispheres compared to normally developing controls. No differences were seen in forceps major or forceps minor (in red), nor in the left or right cingulum bundle (CB, in green).
The mixed factorial repeated measures analysis of variance on FA in an age cohort (adolescent, adult) × group (BPD, HC) × sex (male, female) × tract analysis (forceps major, forceps minor, cingulum [mean right and left], and ILF [mean right and left]) including Beck Depression Scale as a covariate showed that HC adolescents had significantly higher FA in the ILF compared to adolescent BPD and compared to adult BPD and adult HCs (Wilks F(3,52)=4.74, p<0.001; post-hoc Fisher LSD: adolescent HC>adult HC (p<0.001), adolescent HC> adolescent BPD (p<0.02), adolescent HC> adult BPD (p<0.05)). There was no significant effect involving sex. See Figure 2. Because BPD adolescents also differed from BPD adults in aggression scores (BPAQ) and trait Anger (STAXI-T) (See Table 1) we repeated the analysis above adding these measures as covariates. The results were similar with HC adolescents showing significantly higher FA in the ILF compared to adolescent BPD, as well as adult BPD and adult HCs (Wilks F(3,52)=2.86, p<0.05; post-hoc Fisher LSD: adolescent HC>adult HC (p<0.001), adolescent HC> adolescent BPD (p<0.02), adolescent HC> adult BPD (p<0.05)).
Figure 2. DTI Tractography Comparing Adolescent and Adult Borderline Personality Disorder Patients.
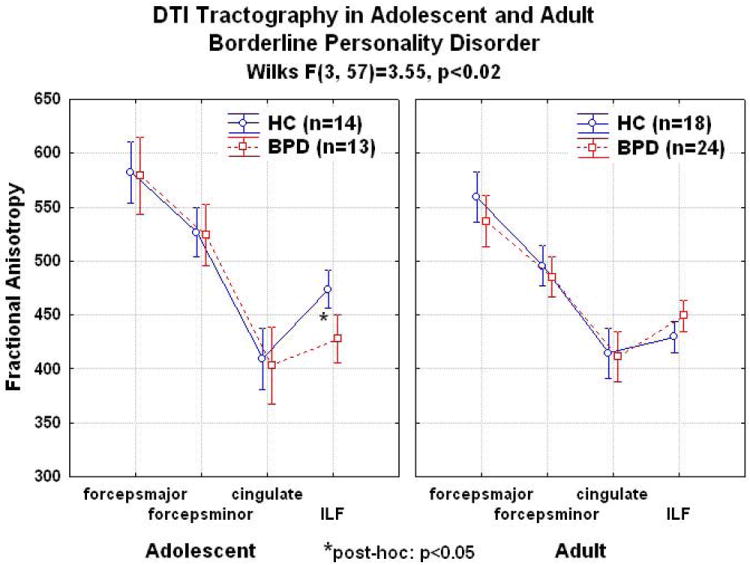
Adolescent patients with BPD showed reduced FA in tractography analysis compared to normally developing adolescents specifically in Inferior Longitudinal Fasciculus in both hemispheres, but no differences in other tracts. Healthy adolescent controls had higher FA in ILF compared to adolescents with BPD, adults with BPD and adult healthy controls (Wilks F(3,52)=4.74, p<0.001; post-hoc Fisher LSD: adolescent HC>adult HC (p<0.001), adolescent HC> adolescent BPD (p<0.02), adolescent HC> adult BPD (p<0.05)).
We used TBSS analysis within these regions to investigate more thoroughly the localization of the FA reduction in adolescent BPD. The ILF traverses the length of the temporal lobe in parallel with the arms of the occipitofrontal fasciculus, while the uncinate fasciculus runs perpendicularly to the ILF and more directly connects OFC to limbic regions such as amygdala (Wakana et al., 2004). FA reductions were found in portions of all these three tracts, predominantly in the medial temporal lobe as opposed to the frontal lobe (Figure 3; p<0.05 FWE corrected for multiple comparisons). FA reductions were abundant in the left hemisphere and only a small significant cluster was found in the right hemisphere (Figure 3). These tracts are tortuous and the location of the FA differences can be better understood in a three-dimensional rendering (Figure 4). The whole brain TBSS analysis did not reveal group differences that survived corrections for multiple comparisons.
Figure 3. TBSS statistical analysis.
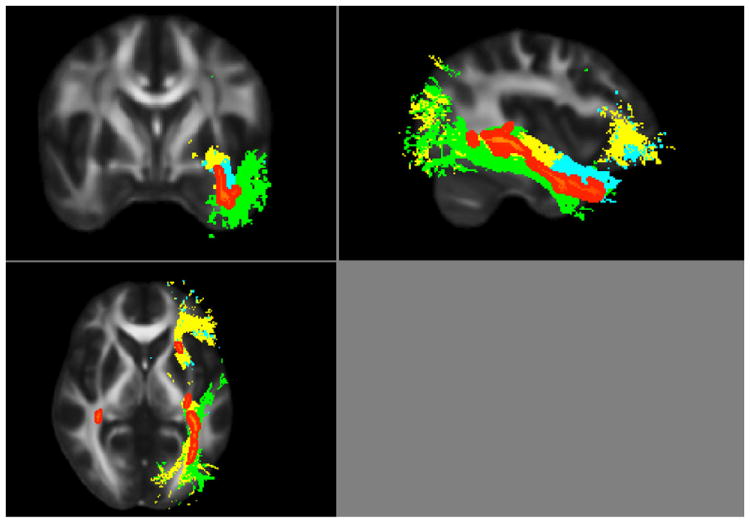
Adolescent BPD patients showed a reduced FA throughout the temporal lobe (shown in red; p < 0.05, family wise error corrected for multiple comparisons). FA differences are projected onto the white matter tracts for reference: the uncinate fasciculus in blue, occipitofronal fasciculus in yellow, and the inferior longitudinal fasciculus in green.
Figure 4. Three-dimensional rendering of TBSS statistical analysis.
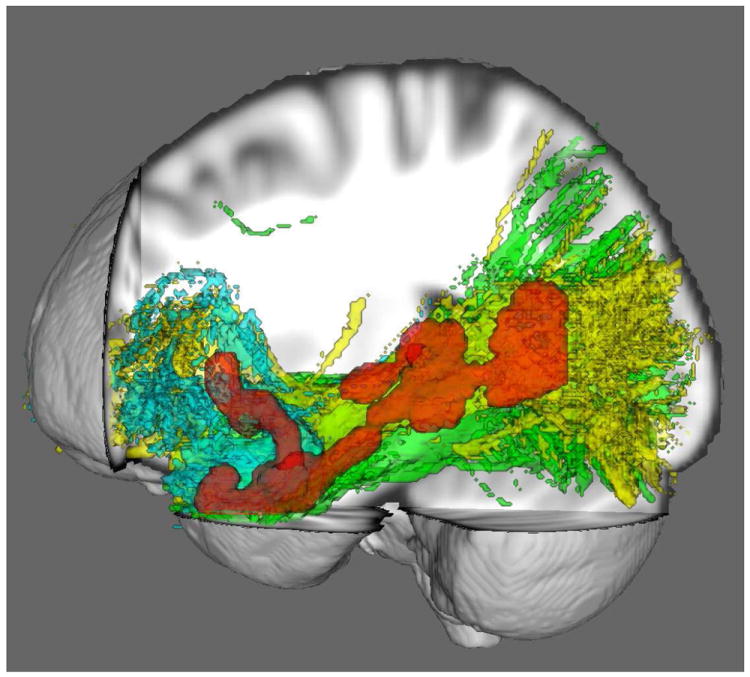
Adolescent BPD patients showed a reduced FA throughout the temporal lobe (shown in red; p < 0.05, family wise error corrected for multiple comparisons). FA differences are projected onto the white matter tracts for reference: the uncinate fasciculus in blue, occipitofronal fasciculus in yellow, and the inferior longitudinal fasciculus in green.
We examined correlations between FA in forceps major, forceps minor, left and right cingulum, left and right ILF with depression, affective lability, impulsive aggression and trait anger in the adolescent and adult samples separately. No correlations between clinical symptoms and FA in any tract survived correction for multiple comparisons.
Discussion
Our principal finding is decreased FA in temporal white matter tracts in adolescents, but not adults, with BPD. Specifically, tractography revealed a robust tract-specific bilateral decrease in ILF FA in BPD adolescents compared to HC adolescents, but no differences between adult BPDs and adult HCs. This finding led us to explore more thoroughly the white matter tracts within temporal lobe in BPD adolescents; voxelwise TBSS analysis demonstrated FA reductions throughout temporal white matter tracts, especially on the left. This analysis revealed FA decreases not only in ILF but also in both uncinate and occipitofrontal fasciculi. Consistent with other studies of BPD adults (Rusch et al., 2007), we found no effect of BPD diagnosis on FA in our adult cohort.
ILF FA was significantly higher in adolescent controls compared to BPD adolescents, BPD adults and adult controls. When comparing FA cross-sectionally across the entire lifespan, most white matter tracts demonstrate an inverted U-shaped curve, with FA increasing progressively through adolescence, and leveling off and slowly decreasing in adulthood (Hasan et al., 2010). In parallel to this developmental process, normal brain maturation from childhood to adolescence shows a pattern of increasing synaptogenesis and prefrontal myelination, with subsequent synapse pruning and remodeling (Giedd et al., 2010). Our findings suggest that, in adolescent BPD patients, this normal developmental “peak” in FA, which is seen in healthy controls, is not achieved.
This finding may represent a biological marker for those at risk for the development of BPD. During this developmental window, early intervention preventive and treatment strategies may improve future clinical outcome. Although fronto-temporal white matter connections appear to develop late (Supekar et al., 2010), the ILF normally demonstrates among the earliest and most rapid changes in FA with age, and these changes appear to be consistent with a process of increasing myelination of pre-existing fibers (Lebel et al., 2008).
The consequences of a developmental delay in ILF maturation are not clear. The ILF is a ventral associative bundle connecting visual areas to the amygdala and hippocampus (Catani et al., 2003). Individuals with brain lesions in this area show poor object naming ability (Mandonnet et al., 2007; Shinoura et al., 2010) and difficulty in recognition of facial affect (Philippi et al., 2009), a basic element of social cognition. A profound deficit in the ability to describe feelings and high levels of alexithymia have been reported in adult BPD (Guttman & Laporte, 2002; New et al., 2012). Our finding of low FA in the ILF, a brain region implicated in object naming and emotion recognition, provides an interesting potential neural substrate for this difficulty in naming and describing affect in BPD. We theorize that impaired connectivity in this region during adolescence may be associated with an inability to learn how to adaptively implement basic semantic processing and integrate these functions into higher-order social cognitive processes, a developmental milestone that typically reaches its pinnacle during adolescence. Abnormalities in the ILF may therefore lie at the core of the dysfunctional mentalizing (Fonagy & Luyten, 2009) and representational disturbances (Bender & Skodol, 2007) seen in BPD. ILF connectivity is required for semantic processing (Mandonnet et al., 2007), and the development of semantic processing may thus be a necessary first step for higher-order social cognitive and affective neural processing, which is disturbed in BPD.
Our follow up TBSS analysis revealed decreased FA in other tracts within the temporal lobe, including uncinate and occipitofrontal fasciculi. This is especially interesting because it provides evidence for a possible neural substrate for the previously reported OFC-amygdala disconnect seen in adults with BPD (New et al., 2007). This raises the possibility that the structural abnormality in BPD apparently present in adolescence may not be appreciable in adult BPD, but that there remains a functional abnormality in the coordination among brain regions that remains into adulthood. This point is speculative and would require a longitudinal study to adolescent BPD for better empirical grounding, but a similar perspective on volume changes has previously been considered (Brunner et al., 2010; Chanen et al., 2008c).
We note that our tractography finding in ILF is bilateral, whereas the TBSS finding is predominantly in the left hemisphere. Our interpretation of this is that, by nature, voxel-wise statistics have more noise that DTI-tractography (the latter takes the average of many voxels thus smoothing the inter-voxel noise). DTI tractography has been shown to be more sensitive to tract-specific white matter changes, and so we believe that the TBSS may not be as sensitive as tractography, and thus miss the less robust decrease in FA in right temporal regions (Kanaan et al., 2006).
The Axis I diagnostic comorbidities seen in our sample (and seen ubiquitously in BPD) (Zanarini et al., 2004), prompted us to compare our findings in adolescent BPD with DTI findings in adolescent samples with the Axis I disorders represented in our sample as well as certain prototypic Axis I disorders exemplifying some of the symptoms domains of BPD. Of note, our finding of decreased FA bilaterally in ILF in BPD adolescents is not reported in adolescents with the Axis I disorders most represented in our sample: MDD and ADHD. In adolescent MDD, broad changes in FA have been shown throughout many areas of the brain, including subgenual and supragenual ACC, right and left uncinate, but not ILF (Cullen et al., 2010). Similarly, adolescents at familial risk for MDD showed widespread decreases in FA in cingulum, the splenium of the corpus callosum, the superior longitudinal fasciculi, uncinate and fronto-occipital fasciculi (Huang et al., 2011). DTI studies in ADHD adolescents have been inconsistent. Most, like in MDD, have shown broad decreases in FA, in regions including superior longitudinal fasciculus (including arcuate fasciculus) (Hamilton et al., 2008), frontoparietal and frontolimbic, and temporoparietal areas (Nagel et al., 2011), anterior limb and superior regions of the internal capsule and anterior corona radiata (Pavuluri et al., 2009). Other studies have shown increased FA in ADHD, in tracts including parts of the cingulum, uncinate, superior and inferior longitudinal fasciculi (Silk et al., 2009) and anterior corona radiata (Davenport et al.). While there are inconsistencies in DTI findings in ADHD, it seems unlikely that our findings are the result of comorbid ADHD because we have only few subjects with co-morbid ADHD and FA in ILF in ADHD adolescents, if different from healthy controls, appears to be increased (Silk et al., 2009).
One disorder in which decreased FA in ILF has been reported is schizophrenia. Adult schizophrenic patients and their first-degree relatives show decreased FA in the ILF (Cheung et al., 2008; Clark et al.), with negative correlations between FA and positive psychotic symptoms (Mitelman et al., 2007). Similarly, children and adolescents with schizophrenia (Ashtari et al., 2007) and subclinical psychosis (Jacobson et al., 2010) demonstrate a similar association between ILF FA and positive psychotic symptoms, with one study indicating the prognostic significance of this white matter abnormality for future social functioning (Karlsgodt et al., 2009). Another diagnosis associated with decreased white matter integrity in ILF is autism, both in adults (Thomas et al., 2011) and adolescents (Jou et al., 2011; Pugliese et al., 2009). Of note, none of our adolescent subjects had a diagnosis of schizophrenia, current psychosis or autism.
Comparing our DTI results to those found in bipolar affective disorder (BD), a disorder like BPD of severe mood instability, showed some similarities but also some differences. Adults with BD (Bruno et al., 2008) and those considered genetically “at-risk” (Chaddock et al., 2009) demonstrated lower FA in the ILF, although others failed to demonstrate any ILF abnormality in bipolar children (Barnea-Goraly et al., 2009; Pavuluri et al., 2009). In a cross-sectional study, healthy offspring of bipolar patients showed lower ILF FA than healthy offspring of healthy individuals (Versace et al., 2010). There is a shared familial risk for BD and BPD (Gunderson et al., 2006) although our current sample excludes those with bipolar I. Thus, similar changes in ILF have been found in schizophrenia, BD, and autism; however, DTI findings in children and adolescents have usually been similar to those seen in adults. By contrast, in BPD, differences in ILF connectivity appear to be evident in borderline adolescents and not adults. Future studies following subjects longitudinally would be helpful to track the course of illness of individuals with affective instability and their white matter FA over time to explore emergent diagnoses.
The primary limitation of this study is its cross-sectional nature. Because we are comparing two separate adult and adolescent populations, the possibility remains for an inadvertent sampling bias between the two age cohorts. Specifically, the sample of adolescents included mostly subjects on psychotropic medication at the time of the DTI imaging while the adult sample was unmedicated. While it remains possible that the differences in FA in the ILF that we find between adolescents with BPD and healthy adolescents may be accounted for by medication and this is a limitation of our study, we believe this to be unlikely. Somewhat surprisingly, evidence suggests that psychotropic medication may have a larger effect on structural MRI than on functional MRI or on DTI outcomes (Hafeman et al., 2012). Indeed, this recent review on the effect of psychotropic medication on brain imaging in bipolar disorder found a minimal effect on DTI results. Furthermore, the effect of medication on structural imaging was to normalize the abnormal structural findings in bipolar disorder to resemble unaffected controls (Hafeman et al., 2012). The implication of this for our data would tend to suggest that, if anything, the presence of current psychotropic medications in our BPD adolescents might diminish the differences compared to healthy adolescents; in contrast, we would expect the unmedicated BPD adults to retain any abnormal brain imaging finding. Our data show just the opposite, perhaps suggesting that the differences between BPD adolescents and healthy controls would be even larger if BPD adolescents had been unmedicated. While we acknowledge that we cannot definitively comment on this in our sample, we do note that recent DTI research in schizophrenia, autism, bipolar disorder, and non-clinical samples has utilized a similar cross-sectional strategy, likely in an effort to identify regions of interest for future, prospective developmental research.
A similar and important limitation involves differences between our adolescent and adult samples: adolescents were recruited from an inpatient population and met criteria for MDD, whereas the adult population was recruited from the community. Although each adolescent may have been recruited during a period of greater clinical acuity, the only significant differences in symptoms between adults and adolescents was in the domain of anger and aggression, with adults reporting significantly worse severity. It bears comment that even though many of the adolescent subjects met criteria for MDD, there was no difference in BDI scores between the adult and adolescent BPD groups (See Table 1). The BDI scores of patients with BPD are often in the mild to low moderate range of depression as patients with this disorder have a great deal of intrapsychic pain even when not in a clear major depressive episode. This range of mild to moderate depression is where the BDI scores lie for both our adult and adolescent cohorts. Another factor that might account for the similarity in depressive symptoms in the face of difference in MDE diagnosis is that the diagnosis of a major depressive episode is made when the symptoms “represent a change from previous functioning” (DSM-IV criteria). While the same criteria pertain for an MDE in adolescents, perhaps there is a different threshold for giving the diagnosis as there is a shorter track record of what represents baseline functioning. Nevertheless, it remains true that the adolescents we included did meet criteria for major depressive disorder (MDD), and so the question remains whether differences between the two groups may be secondary to depression. Our analysis controlled for BDI scores, which argues against that hypothesis. Further evidence against this interpretation is that FA did not correlate with depressive symptoms. In addition, prior DTI research in adults and adolescents with MDD has shown decreased FA broadly in white matter tracts (Cullen et al., 2010; Kieseppa et al., 2010; Li et al., 2007), but not in the ILF. Nevertheless, the direct comparison between BPD adults and adolescents requires replication. Although it remains possible that FA differences were secondary to clinical differences between the two age cohorts (rather than an effect of BPD across development), the fact that adults reported, if anything, worse symptoms makes this somewhat less likely. Another limitation is that adolescents were diagnosed using the SCID-II and the DIB-R, while adults were diagnosed using the SIDP-IV. This was done as the SCID-II with DIB-R is more accepted approach to diagnosing BPD in adolescents. However, we find high inter-rater reliability in adults for BPD between the SCID-II and SIDP-IV (kappa= 0.91).
We acknowledge some limitations in our DTI parameters. Although 0mm gap would have been ideal, we used a 1mm gap due to hardware limitation. However, in satisfying the hardware requirements, we gained some improvement in DTI image quality through 1) the decreased acquisition time minimized potential motion artifact, and 2) the space between slices decreased cross-talk artifacts. In this way, we minimized the effect of subject movement on our data, which in this population was a major concern and would have rendered the data unusable. Other studies have successful employed DTI tractography with gaps leading to important results. For example, elucidating complex pathways such as Meyer’s loop(White & Zhang, 2010); abnormal diffusion in normal appearing pyramidal tracts of patients with relapsing-remitting multiple sclerosis(Lin et al., 2007); language-related subcortical connections (Kamada et al., 2007); or white matter changes during stroke (Pannek et al., 2009). In addition, DTI data that include a gap have been used to development novel tractography algorithms (Kim et al., 2003; Liu et al., 2009; Patel et al., 2010). DTI tractography validation studies are few in number and utilize long acquisition schemes with higher resolution that are not feasible in clinical studies, and would be especially difficult in patient populations for which motion is a concern like ours (Behrens et al., 2007; Ciccarelli et al., 2003; Dyrby et al., 2007; Heiervang et al., 2006). Moreover, simulations show that even with more limited resolution, akin to the interpolation done when there is a gap, tractography is still highly robust when multiple anatomical criteria are stipulated (Huang et al., 2004; Wakana et al., 2007).
Future prospective research in adolescents will clarify whether abnormalities in temporal lobe white matter are a measurable biomarker of risk for BPD. If so, future research will also assist in determining the nature of early intervention to prevent future onset of BPD or mitigate its severity. Our results suggest that the course of BPD across the lifespan may involve a specific neurobiological abnormality in ILF, perhaps related to semantic processing of affect, during a specific developmental window. Our findings call for attention to developmental changes in affective and social cognitive neurobiology in BPD. By identifying individuals at-risk with a neurobiological marker, we can increase our understanding of the fundamental psychopathology of BPD, as well as develop psychotherapeutic and psychopharmacologic strategies for prevention and clinical improvement.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asato MR, Terwilliger R, Woo J, Luna B. White matter development in adolescence: a DTI study. Cereb Cortex. 2010;20:2122–31. doi: 10.1093/cercor/bhp282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashtari M, Cottone J, Ardekani BA, Cervellione K, Szeszko PR, Wu J, Chen S, Kumra S. Disruption of white matter integrity in the inferior longitudinal fasciculus in adolescents with schizophrenia as revealed by fiber tractography. Arch Gen Psychiatry. 2007;64:1270–80. doi: 10.1001/archpsyc.64.11.1270. [DOI] [PubMed] [Google Scholar]
- Barnea-Goraly N, Chang KD, Karchemskiy A, Howe ME, Reiss AL. Limbic and corpus callosum aberrations in adolescents with bipolar disorder: a tract-based spatial statistics analysis. Biol Psychiatry. 2009;66:238–44. doi: 10.1016/j.biopsych.2009.02.025. [DOI] [PubMed] [Google Scholar]
- Barratt ES. Factor Analysis of Some Psychometric Measures of Impulsiveness and Anxiety. Psychol Rep. 1965;16:547–54. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- Bava S, Thayer R, Jacobus J, Ward M, Jernigan TL, Tapert SF. Longitudinal characterization of white matter maturation during adolescence. Brain Res. 2010;1327:38–46. doi: 10.1016/j.brainres.2010.02.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Behrens TE, Berg HJ, Jbabdi S, Rushworth MF, Woolrich MW. Probabilistic diffusion tractography with multiple fibre orientations: What can we gain? Neuroimage. 2007;34:144–55. doi: 10.1016/j.neuroimage.2006.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender DS, Skodol AE. Borderline personality as a self-other representational disturbance. J Personal Disord. 2007;21:500–17. doi: 10.1521/pedi.2007.21.5.500. [DOI] [PubMed] [Google Scholar]
- Brambilla P, Soloff PH, Sala M, Nicoletti MA, Keshavan MS, Soares JC. Anatomical MRI study of borderline personality disorder patients. Psychiatry Res. 2004;131:125–33. doi: 10.1016/j.pscychresns.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Brunner R, Henze R, Parzer P, Kramer J, Feigl N, Lutz K, Essig M, Resch F, Stieltjes B. Reduced prefrontal and orbitofrontal gray matter in female adolescents with borderline personality disorder: is it disorder specific? Neuroimage. 2010;49:114–20. doi: 10.1016/j.neuroimage.2009.07.070. [DOI] [PubMed] [Google Scholar]
- Bruno S, Cercignani M, Ron MA. White matter abnormalities in bipolar disorder: a voxel-based diffusion tensor imaging study. Bipolar Disord. 2008;10:460–8. doi: 10.1111/j.1399-5618.2007.00552.x. [DOI] [PubMed] [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. J Pers Soc Psychol. 1992;63:452–9. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Carpenter DM, Tang CY, Friedman JI, Hof PR, Stewart DG, Buchsbaum MS, Harvey PD, Gorman JG, Davis KL. Temporal characteristics of tract-specific anisotropy abnormalities in schizophrenia. Neuroreport. 2008;19:1369–72. doi: 10.1097/WNR.0b013e32830abc35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catani M, Jones DK, Donato R, Ffytche DH. Occipito-temporal connections in the human brain. Brain. 2003;126:2093–107. doi: 10.1093/brain/awg203. [DOI] [PubMed] [Google Scholar]
- Chaddock CA, Barker GJ, Marshall N, Schulze K, Hall MH, Fern A, Walshe M, Bramon E, Chitnis XA, Murray R, McDonald C. White matter microstructural impairments and genetic liability to familial bipolar I disorder. Br J Psychiatry. 2009;194:527–34. doi: 10.1192/bjp.bp.107.047498. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jackson HJ, McCutcheon LK, Jovev M, Dudgeon P, Yuen HP, Germano D, Nistico H, McDougall E, Weinstein C, Clarkson V, McGorry PD. Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: randomised controlled trial. Br J Psychiatry. 2008a;193:477–84. doi: 10.1192/bjp.bp.107.048934. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, Djaja D, McDougall E, Yuen HP, Rawlings D, Jackson HJ. Screening for borderline personality disorder in outpatient youth. J Pers Disord. 2008b;22:353–64. doi: 10.1521/pedi.2008.22.4.353. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Velakoulis D, Carison K, Gaunson K, Wood SJ, Yuen HP, Yucel M, Jackson HJ, McGorry PD, Pantelis C. Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiatry Res. 2008c;163:116–25. doi: 10.1016/j.pscychresns.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Velakoulis D, Carison K, Gaunson K, Wood SJ, Yuen HP, Yucel M, Jackson HJ, McGorry PD, Pantelis C. Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiatry Res. 2008d doi: 10.1016/j.pscychresns.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Cheung V, Cheung C, McAlonan GM, Deng Y, Wong JG, Yip L, Tai KS, Khong PL, Sham P, Chua SE. A diffusion tensor imaging study of structural dysconnectivity in never-medicated, first-episode schizophrenia. Psychol Med. 2008;38:877–85. doi: 10.1017/S0033291707001808. [DOI] [PubMed] [Google Scholar]
- Ciccarelli O, Parker GJ, Toosy AT, Wheeler-Kingshott CA, Barker GJ, Boulby PA, Miller DH, Thompson AJ. From diffusion tractography to quantitative white matter tract measures: a reproducibility study. Neuroimage. 2003;18:348–59. doi: 10.1016/s1053-8119(02)00042-3. [DOI] [PubMed] [Google Scholar]
- Clark KA, Nuechterlein KH, Asarnow RF, Hamilton LS, Phillips OR, Hageman NS, Woods RP, Alger JR, Toga AW, Narr KL. Mean diffusivity and fractional anisotropy as indicators of disease and genetic liability to schizophrenia. J Psychiatr Res. 45:980–8. doi: 10.1016/j.jpsychires.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen KR, Klimes-Dougan B, Muetzel R, Mueller BA, Camchong J, Houri A, Kurma S, Lim KO. Altered white matter microstructure in adolescents with major depression: a preliminary study. J Am Acad Child Adolesc Psychiatry. 2010;49:173–83 e1. doi: 10.1097/00004583-201002000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport ND, Karatekin C, White T, Lim KO. Differential fractional anisotropy abnormalities in adolescents with ADHD or schizophrenia. Psychiatry Res. 181:193–8. doi: 10.1016/j.pscychresns.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrby TB, Sogaard LV, Parker GJ, Alexander DC, Lind NM, Baare WF, Hay-Schmidt A, Eriksen N, Pakkenberg B, Paulson OB, Jelsing J. Validation of in vitro probabilistic tractography. Neuroimage. 2007;37:1267–77. doi: 10.1016/j.neuroimage.2007.06.022. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) Washington, D.C.: American Psychiatric Press, Inc.; 1997. [Google Scholar]
- First MB, Spitzer Robert L, Gibbon Miriam, Williams Janet BW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol. 2009;21:1355–81. doi: 10.1017/S0954579409990198. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Stockman M, Weddle C, Liverpool M, Alexander-Bloch A, Wallace GL, Lee NR, Lalonde F, Lenroot RK. Anatomic magnetic resonance imaging of the developing child and adolescent brain and effects of genetic variation. Neuropsychol Rev. 2010;20:349–61. doi: 10.1007/s11065-010-9151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman M, Hazlett EA, Avedon JB, Siever DR, Chu KW, New AS. Anterior cingulate volume reduction in adolescents with borderline personality disorder and co-morbid major depression. J Psychiatr Res. 2010 doi: 10.1016/j.jpsychires.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Grant JE, Correia S, Brennan-Krohn T, Malloy PF, Laidlaw DH, Schulz SC. Frontal white matter integrity in borderline personality disorder with self-injurious behavior. J Neuropsychiatry Clin Neurosci. 2007;19:383–90. doi: 10.1176/jnp.2007.19.4.383. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Weinberg I, Daversa MT, Kueppenbender KD, Zanarini MC, Shea MT, Skodol AE, Sanislow CA, Yen S, Morey LC, Grilo CM, McGlashan TH, Stout RL, Dyck I. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163:1173–8. doi: 10.1176/ajp.2006.163.7.1173. [DOI] [PubMed] [Google Scholar]
- Guttman H, Laporte L. Alexithymia, empathy, and psychological symptoms in a family context. Compr Psychiatry. 2002;43:448–55. doi: 10.1053/comp.2002.35905. [DOI] [PubMed] [Google Scholar]
- Hafeman DM, Chang KD, Garrett AS, Sanders EM, Phillips ML. Effects of medication on neuroimaging findings in bipolar disorder: an updated review. Bipolar Disord. 2012;14:375–410. doi: 10.1111/j.1399-5618.2012.01023.x. [DOI] [PubMed] [Google Scholar]
- Hamilton LS, Levitt JG, O’Neill J, Alger JR, Luders E, Phillips OR, Caplan R, Toga AW, McCracken J, Narr KL. Reduced white matter integrity in attention-deficit hyperactivity disorder. Neuroreport. 2008;19:1705–8. doi: 10.1097/WNR.0b013e3283174415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey P, Greenberg B, Serper M. The affective lability scales: development reliability and validity. J Clin Psychol. 1989;45:786–93. doi: 10.1002/1097-4679(198909)45:5<786::aid-jclp2270450515>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Hasan KM, Kamali A, Abid H, Kramer LA, Fletcher JM, Ewing-Cobbs L. Quantification of the spatiotemporal microstructural organization of the human brain association, projection and commissural pathways across the lifespan using diffusion tensor tractography. Brain Struct Funct. 2010;214:361–73. doi: 10.1007/s00429-009-0238-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlett EA, New AS, Newmark R, Haznedar MM, Lo JN, Speiser LJ, Chen AD, Mitropoulou V, Minzenberg M, Siever LJ, Buchsbaum MS. Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol Psychiatry. 2005;58:614–23. doi: 10.1016/j.biopsych.2005.04.029. [DOI] [PubMed] [Google Scholar]
- Heiervang E, Behrens TE, Mackay CE, Robson MD, Johansen-Berg H. Between session reproducibility and between subject variability of diffusion MR and tractography measures. Neuroimage. 2006;33:867–77. doi: 10.1016/j.neuroimage.2006.07.037. [DOI] [PubMed] [Google Scholar]
- Huang H, Fan X, Williamson DE, Rao U. White matter changes in healthy adolescents at familial risk for unipolar depression: a diffusion tensor imaging study. Neuropsychopharmacology. 2011;36:684–91. doi: 10.1038/npp.2010.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H, Zhang J, van Zijl PC, Mori S. Analysis of noise effects on DTI-based tractography using the brute-force and multi-ROI approach. Magn Reson Med. 2004;52:559–65. doi: 10.1002/mrm.20147. [DOI] [PubMed] [Google Scholar]
- Irle E, Lange C, Sachsse U. Reduced size and abnormal asymmetry of parietal cortex in women with borderline personality disorder. Biol Psychiatry. 2005;57:173–82. doi: 10.1016/j.biopsych.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Jacobson S, Kelleher I, Harley M, Murtagh A, Clarke M, Blanchard M, Connolly C, O’Hanlon E, Garavan H, Cannon M. Structural and functional brain correlates of subclinical psychotic symptoms in 11-13 year old schoolchildren. Neuroimage. 2010;49:1875–85. doi: 10.1016/j.neuroimage.2009.09.015. [DOI] [PubMed] [Google Scholar]
- Jou RJ, Mateljevic N, Kaiser MD, Sugrue DR, Volkmar FR, Pelphrey KA. Structural neural phenotype of autism: preliminary evidence from a diffusion tensor imaging study using tract-based spatial statistics. AJNR Am J Neuroradiol. 2011;32:1607–13. doi: 10.3174/ajnr.A2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamada K, Todo T, Masutani Y, Aoki S, Ino K, Morita A, Saito N. Visualization of the frontotemporal language fibers by tractography combined with functional magnetic resonance imaging and magnetoencephalography. J Neurosurg. 2007;106:90–8. doi: 10.3171/jns.2007.106.1.90. [DOI] [PubMed] [Google Scholar]
- Kanaan RA, Shergill SS, Barker GJ, Catani M, Ng VW, Howard R, McGuire PK, Jones DK. Tract-specific anisotropy measurements in diffusion tensor imaging. Psychiatry Res. 2006;146:73–82. doi: 10.1016/j.pscychresns.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Karlsgodt KH, Niendam TA, Bearden CE, Cannon TD. White matter integrity and prediction of social and role functioning in subjects at ultra-high risk for psychosis. Biol Psychiatry. 2009;66:562–9. doi: 10.1016/j.biopsych.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieseppa T, Eerola M, Mantyla R, Neuvonen T, Poutanen VP, Luoma K, Tuulio-Henriksson A, Jylha P, Mantere O, Melartin T, Rytsala H, Vuorilehto M, Isometsa E. Major depressive disorder and white matter abnormalities: a diffusion tensor imaging study with tract-based spatial statistics. J Affect Disord. 2010;120:240–4. doi: 10.1016/j.jad.2009.04.023. [DOI] [PubMed] [Google Scholar]
- Kim DS, Kim M, Ronen I, Formisano E, Kim KH, Ugurbil K, Mori S, Goebel R. In vivo mapping of functional domains and axonal connectivity in cat visual cortex using magnetic resonance imaging. Magn Reson Imaging. 2003;21:1131–40. doi: 10.1016/j.mri.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Lebel C, Walker L, Leemans A, Phillips L, Beaulieu C. Microstructural maturation of the human brain from childhood to adulthood. Neuroimage. 2008;40:1044–55. doi: 10.1016/j.neuroimage.2007.12.053. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. 2011;377:74–84. doi: 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- Li L, Ma N, Li Z, Tan L, Liu J, Gong G, Shu N, He Z, Jiang T, Xu L. Prefrontal white matter abnormalities in young adult with major depressive disorder: a diffusion tensor imaging study. Brain Res. 2007;1168:124–8. doi: 10.1016/j.brainres.2007.06.094. [DOI] [PubMed] [Google Scholar]
- Lin F, Yu C, Jiang T, Li K, Chan P. Diffusion tensor tractography-based group mapping of the pyramidal tract in relapsing-remitting multiple sclerosis patients. AJNR Am J Neuroradiol. 2007;28:278–82. [PMC free article] [PubMed] [Google Scholar]
- Liu X, Zhu T, Gu T, Zhong J. A practical approach to in vivo high-resolution diffusion tensor imaging of rhesus monkeys on a 3-T human scanner. Magn Reson Imaging. 2009;27:335–46. doi: 10.1016/j.mri.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Madler B, Drabycz SA, Kolind SH, Whittall KP, MacKay AL. Is diffusion anisotropy an accurate monitor of myelination? Correlation of multicomponent T2 relaxation and diffusion tensor anisotropy in human brain. Magn Reson Imaging. 2008;26:874–88. doi: 10.1016/j.mri.2008.01.047. [DOI] [PubMed] [Google Scholar]
- Mandonnet E, Nouet A, Gatignol P, Capelle L, Duffau H. Does the left inferior longitudinal fasciculus play a role in language? A brain stimulation study. Brain. 2007;130:623–9. doi: 10.1093/brain/awl361. [DOI] [PubMed] [Google Scholar]
- Mauchnik J, Schmahl C. The latest neuroimaging findings in borderline personality disorder. Curr Psychiatry Rep. 2010;12:46–55. doi: 10.1007/s11920-009-0089-7. [DOI] [PubMed] [Google Scholar]
- Minzenberg MJ, Fan J, New AS, Tang CY, Siever LJ. Frontolimbic structural changes in borderline personality disorder. J Psychiatr Res. 2008;42:727–33. doi: 10.1016/j.jpsychires.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitelman SA, Torosjan Y, Newmark RE, Schneiderman JS, Chu KW, Brickman AM, Haznedar MM, Hazlett EA, Tang CY, Shihabuddin L, Buchsbaum MS. Internal capsule, corpus callosum and long associative fibers in good and poor outcome schizophrenia: a diffusion tensor imaging survey. Schizophr Res. 2007;92:211–24. doi: 10.1016/j.schres.2006.12.029. [DOI] [PubMed] [Google Scholar]
- Mori S, Barker PB. Diffusion magnetic resonance imaging: its principle and applications. Anat Rec. 1999;257:102–9. doi: 10.1002/(SICI)1097-0185(19990615)257:3<102::AID-AR7>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Nagel BJ, Bathula D, Herting M, Schmitt C, Kroenke CD, Fair D, Nigg JT. Altered white matter microstructure in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:283–92. doi: 10.1016/j.jaac.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New AS, aan het Rot M, Ripoll LH, Perez-Rodriguez MM, Lazarus S, Zipursky E, Weinstein SR, Koenigsberg HW, Hazlett EA, Goodman M, Siever LJ. Empathy and alexithymia in borderline personality disorder: clinical and laboratory measures. J Pers Disord. 2012;26:660–75. doi: 10.1521/pedi.2012.26.5.660. [DOI] [PubMed] [Google Scholar]
- New AS, Goodman M, Triebwasser J, Siever LJ. Recent advances in the biological study of personality disorders. Psychiatr Clin North Am. 2008a;31:441–61. vii. doi: 10.1016/j.psc.2008.03.011. [DOI] [PubMed] [Google Scholar]
- New AS, Hazlett EA, Buchsbaum MS, Goodman M, Mitelman SA, Newmark R, Trisdorfer R, Haznedar MM, Koenigsberg HW, Flory J, Siever LJ. Amygdala-prefrontal disconnection in borderline personality disorder. Neuropsychopharmacology. 2007;32:1629–40. doi: 10.1038/sj.npp.1301283. [DOI] [PubMed] [Google Scholar]
- New AS, Triebwasser J, Charney DS. The case for shifting borderline personality disorder to Axis I. Biol Psychiatry. 2008b;64:653–9. doi: 10.1016/j.biopsych.2008.04.020. [DOI] [PubMed] [Google Scholar]
- Nunes PM, Wenzel A, Borges KT, Porto CR, Caminha RM, de Oliveira IR. Volumes of the hippocampus and amygdala in patients with borderline personality disorder: a meta-analysis. J Pers Disord. 2009;23:333–45. doi: 10.1521/pedi.2009.23.4.333. [DOI] [PubMed] [Google Scholar]
- Pannek K, Chalk JB, Finnigan S, Rose SE. Dynamic corticospinal white matter connectivity changes during stroke recovery: a diffusion tensor probabilistic tractography study. J Magn Reson Imaging. 2009;29:529–36. doi: 10.1002/jmri.21627. [DOI] [PubMed] [Google Scholar]
- Patel V, Chiang M-C, Thompson PM, McMahon KL, de Zubicaray GI, Martin NG, Wright MJ, Toga AW. Scalar connectivity measures from fast-marching tractography reveal heritability of white matter architecture. Biomedical Imaging: From Nano to Macro, 2010 IEEE International Symposium on IEEE. 2010:1109–1112. [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Yang S, Kamineni K, Passarotti AM, Srinivasan G, Harral EM, Sweeney JA, Zhou XJ. Diffusion tensor imaging study of white matter fiber tracts in pediatric bipolar disorder and attention-deficit/hyperactivity disorder. Biol Psychiatry. 2009;65:586–93. doi: 10.1016/j.biopsych.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Clinical Interview for DSM-IV. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Philippi CL, Mehta S, Grabowski T, Adolphs R, Rudrauf D. Damage to association fiber tracts impairs recognition of the facial expression of emotion. J Neurosci. 2009;29:15089–99. doi: 10.1523/JNEUROSCI.0796-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugliese L, Catani M, Ameis S, Dell’Acqua F, Thiebaut de Schotten M, Murphy C, Robertson D, Deeley Q, Daly E, Murphy DG. The anatomy of extended limbic pathways in Asperger syndrome: a preliminary diffusion tensor imaging tractography study. Neuroimage. 2009;47:427–34. doi: 10.1016/j.neuroimage.2009.05.014. [DOI] [PubMed] [Google Scholar]
- Rusch N, Bracht T, Kreher BW, Schnell S, Glauche V, Il’yasov KA, Ebert D, Lieb K, Hennig J, Saur D, van Elst LT. Reduced interhemispheric structural connectivity between anterior cingulate cortices in borderline personality disorder. Psychiatry Res. 181:151–4. doi: 10.1016/j.pscychresns.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Rusch N, Bracht T, Kreher BW, Schnell S, Glauche V, Il’yasov KA, Ebert D, Lieb K, Hennig J, Saur D, van Elst LT. Reduced interhemispheric structural connectivity between anterior cingulate cortices in borderline personality disorder. Psychiatry Res. 2010;181:151–4. doi: 10.1016/j.pscychresns.2009.08.004. [DOI] [PubMed] [Google Scholar]
- Rusch N, Weber M, Il’yasov KA, Lieb K, Ebert D, Hennig J, van Elst LT. Inferior frontal white matter microstructure and patterns of psychopathology in women with borderline personality disorder and comorbid attention-deficit hyperactivity disorder. Neuroimage. 2007;35:738–47. doi: 10.1016/j.neuroimage.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Shinoura N, Suzuki Y, Tsukada M, Yoshida M, Yamada R, Tabei Y, Saito K, Koizumi T, Yagi K. Deficits in the left inferior longitudinal fasciculus results in impairments in object naming. Neurocase. 2010;16:135–9. doi: 10.1080/13554790903329174. [DOI] [PubMed] [Google Scholar]
- Silk TJ, Vance A, Rinehart N, Bradshaw JL, Cunnington R. White-matter abnormalities in attention deficit hyperactivity disorder: a diffusion tensor imaging study. Hum Brain Mapp. 2009;30:2757–65. doi: 10.1002/hbm.20703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, Lushene P, Vagg P, Jacobs A. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto: Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- Supekar K, Uddin LQ, Prater K, Amin H, Greicius MD, Menon V. Development of functional and structural connectivity within the default mode network in young children. Neuroimage. 2010;52:290–301. doi: 10.1016/j.neuroimage.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebartz van Elst L, Hesslinger B, Thiel T, Geiger E, Haegele K, Lemieux L, Lieb K, Bohus M, Hennig J, Ebert D. Frontolimbic brain abnormalities in patients with borderline personality disorder: a volumetric magnetic resonance imaging study. Biol Psychiatry. 2003;54:163–71. doi: 10.1016/s0006-3223(02)01743-2. [DOI] [PubMed] [Google Scholar]
- Thomas C, Humphreys K, Jung KJ, Minshew N, Behrmann M. The anatomy of the callosal and visual-association pathways in high-functioning autism: a DTI tractography study. Cortex. 2011;47:863–73. doi: 10.1016/j.cortex.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi R, Agarwal S, Rathore RK, Saksena S, Tripathi RP, Malik GK, Pandey CM, Gupta RK. Understanding development and lateralization of major cerebral fiber bundles in pediatric population through quantitative diffusion tensor tractography. Pediatr Res. 2009;66:636–41. doi: 10.1203/PDR.0b013e3181bbc6b5. [DOI] [PubMed] [Google Scholar]
- Versace A, Ladouceur CD, Romero S, Birmaher B, Axelson DA, Kupfer DJ, Phillips ML. Altered development of white matter in youth at high familial risk for bipolar disorder: a diffusion tensor imaging study. J Am Acad Child Adolesc Psychiatry. 2010;49:1249–59. 1259 e1. doi: 10.1016/j.jaac.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakana S, Caprihan A, Panzenboeck MM, Fallon JH, Perry M, Gollub RL, Hua K, Zhang J, Jiang H, Dubey P, Blitz A, van Zijl P, Mori S. Reproducibility of quantitative tractography methods applied to cerebral white matter. Neuroimage. 2007;36:630–44. doi: 10.1016/j.neuroimage.2007.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakana S, Jiang H, Nagae-Poetscher LM, van Zijl PC, Mori S. Fiber tract-based atlas of human white matter anatomy. Radiology. 2004;230:77–87. doi: 10.1148/radiol.2301021640. [DOI] [PubMed] [Google Scholar]
- Westlye LT, Walhovd KB, Dale AM, Bjornerud A, Due-Tonnessen P, Engvig A, Grydeland H, Tamnes CK, Ostby Y, Fjell AM. Life-span changes of the human brain white matter: diffusion tensor imaging (DTI) and volumetry. Cereb Cortex. 2010;20:2055–68. doi: 10.1093/cercor/bhp280. [DOI] [PubMed] [Google Scholar]
- White ML, Zhang Y. Three-tesla diffusion tensor imaging of Meyer’s loop by tractography, color-coded fractional anisotropy maps, and eigenvectors. Clin Imaging. 2010;34:413–7. doi: 10.1016/j.clinimag.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Whittle S, Chanen AM, Fornito A, McGorry PD, Pantelis C, Yucel M. Anterior cingulate volume in adolescents with first-presentation borderline personality disorder. Psychiatry Res. 2009;172:155–60. doi: 10.1016/j.pscychresns.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161:2108–14. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA. Inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines. J Pers Disord. 2002;16:270–6. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- Zetzsche T, Preuss UW, Frodl T, Schmitt G, Seifert D, Munchhausen E, Tabrizi S, Leinsinger G, Born C, Reiser M, Moller HJ, Meisenzahl EM. Hippocampal volume reduction and history of aggressive behaviour in patients with borderline personality disorder. Psychiatry Res. 2007;154:157–70. doi: 10.1016/j.pscychresns.2006.05.010. [DOI] [PubMed] [Google Scholar]


