Abstract
Background
HIV testing is the gateway for prevention and care. We explored factors associated with HIV testing among Chinese men who have sex with men (MSM).
Methods
In Chongqing City, we recruited 492 MSM in 2010 using respondent driven sampling in a cross-sectional study. Computer-assisted self-interviews were conducted to collect information on history of HIV testing.
Results
Only 58% of participants reported ever having taken an HIV test. MSM who had a college degree [adjusted odds ratio (AOR): 1.7; 95% confidence interval (CI): 1.2-2.6; P=0.008] were more likely to take a test; those who preferred a receptive role in anal sex were less likely to do so than those with insertive sex preference (AOR: 0.6; 95% CI: 0.35-0.94; P=0.03); those who used condoms with the recent male partner during the past 6 months were more likely to get tested (AOR: 2.87; 95%CI: 1.25-6.62; P=0.01). Principal perceived barriers to testing included: fear of knowing a positive result, fear of discrimination if tested positive, low perceived risk of HIV infection, and not knowing where to take a test. Factors reported to facilitate testing were sympathetic attitudes from health staff and guaranteed confidentiality. Prevalence was high: 11.7% HIV-positive and 4.7% syphilis positive.
Conclusion
The HIV testing rate among MSM in Chongqing is still low, though MSM prevalence is high compared to other Chinese cities. MSM preferring receptive anal sex are less likely to get testing and perceive having lower HIV risk. Along with expanded education and social marketing, a welcoming and non-judgmental environment for HIV testing is needed.
Keywords: Human immunodeficiency virus, syphilis, men who have sex with men, HIV testing, respondent driven sampling, China
Introduction
HIV testing is an entry point both for HIV prevention and care1. Early detection of HIV not only reduces the chance of transmitting the virus to uninfected individuals, but also enables timely treatment to reduce mortality and morbidity2. HIV testing is also the backbone of combination HIV prevention highlighting testing and linkage to care3. The UNAIDS strategy 2011-2015 proposed to reduce HIV sexual transmissions by half among men who have sex with men (MSM) and to offer universal access to combination antiretroviral therapy (cART) for eligible people living with HIV by 20151. These goals are achievable only if a high proportion of at-risk persons go for periodic HIV testing to know their status.
The Chinese government has implemented free HIV testing in HIV voluntary counseling and testing (VCT) clinics under the “Four Frees and One Care” policy since 20034. By the end of 2009, 7335 VCT clinics had been established with at least 1 or 2 per county, of which 43.4% were in local CDC venues, 26.1% in general hospitals (including Traditional Chinese Medicine Hospitals), 14.8% in township health centers, and 15.7% elsewhere4. Despite the efforts made by the government to facilitate universal access to HIV testing, 56% of an estimated 780,000 individuals living with HIV/AIDS in mainland China did not know their status at the end of 20115. National sentinel surveillance data have suggested that MSM have now become one of the subgroups at highest risk for HIV in China, as is the case worldwide6,7. The national average prevalence of HIV infection among MSM in the sentinel sites surpassed that among intravenous drug users for the first time in 2010 5. Moreover, approximately 17% of MSM in China are currently married and 26% of MSM had female sexual partners in the last six months; unawareness of their HIV status could increase risk of MSM to both men and women8.
Chongqing City, located in southwestern China, is among the world’s largest cities. In Chongqing, HIV incidence rate among MSM was nearly twice that in other Chinese cities (8.3% vs. 4.6%) while the average testing rate in 2009 was only 34.5% 9,10. Our study aimed to assess the history of and the barriers to HIV testing among MSM in Chongqing City, with the goal of providing guidance for design of future interventions.
Materials and Methods
Study design and procedures
We conducted the study between September and December 2010 in Chongqing City, China. This was the second round of cross-sectional surveys following the first survey in 2009. The original aim of the serial cross-sectional surveys was to evaluate the change of HIV prevalence and risk behaviors in the MSM population over time. The study procedures and sampling strategies were described in detail elsewhere11. In brief, participants were recruited using a respondent driven sampling (RDS) approach 12. Six MSM were selected as initial seeds by several local gay-friendly community-based organizations (CBO): three recruited from gay websites by Lan Yu, Hua Yang Nian Hua Tong Xin and Yang Guan Volunteer Groups; two recruited from bars by Cai Hong and Zhi Ai Volunteer Groups; and one from brothel by Lan Tian Volunteer Group. They were chosen through focus group discussion, taking into consideration their demographic characteristics and sub-group memberships, active social networks, and motivation to recruit peers. Each seed and each of his referred peers was allowed to recruit up to 3 participants. All referred participants had to be a member of the recruiter’s social network and meet the eligibility criteria for the study. Participants were compensated with 30 Chinese Yuan (≈US $4.5) for their participation in the study and an additional 20 Chinese Yuan (≈US $3.0) for those who successfully recruited eligible MSM who subsequently completed the study interview. Eligible participants (≥ 18 years old) completed a computer-assisted self-interview (CASI) on their history of receiving HIV testing, barriers and facilitators for taking a test, and, when applicable, reasons for not taking one. For the perceived barriers, all the participants were asked “In your opinion, what prevents a gay man from having an HIV test?”; To probe for reasons (barriers) for not taking a test, men who never took a test were asked “Why have you never tested for HIV?” Venous blood samples were collected to test for HIV and syphilis. All eligible persons expressing interest and providing written consent were enrolled in the study. The study protocol was reviewed and approved by the institutional review boards of the National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention (China CDC), University of California, San Francisco, and Vanderbilt University.
Laboratory tests
Venous blood specimens were first screened for HIV-1 using a rapid test (Determine HIV-1/2™, Inverness Medical Japan Co., Ltd, Tokyo, Japan) at the study site and the result was given to the participant immediately after the interview, with counseling as to its meaning. All samples were then sent to laboratories in Chongqing CDC for testing using enzyme-linked immunosorbent assay (ELISA, Vironostika HIV Uni-Form plus O™, bioMérieux Shanghai Company Ltd., Shanghai, China). Positive samples were confirmed by Western Blot for HIV-1 (HIV Blot 2.2 WBTM™, Genelabs Diagnostics, Singapore). Only the ELISA and Western blot positive tests were deemed seropositive. Syphilis antibody testing used the Treponema pallidum particle assay (TPPA, InTec Products, Inc., Xiamen, China).
Statistical methods
We examined correlates of prior HIV testing among MSM who participated in the cross-sectional survey in 2010. The six seeds were excluded in all analyses as they were not recruited by peers 13. Descriptive analyses of HIV and syphilis prevalence and characteristics of social demographics and sexual behaviors were conducted using RDSAT software (Respondent-Driven Sampling Analysis Tool V 5.6.0™; www.respondentdrivensampling.org), which adjusted for personal social network size and patterns of recruitment12. Such adjustments compensate for potential bias arising from different personal social network sizes and respondents’ homophily (recruitment of participants often occurs within certain groups)12. Univariate and multivariate logistic regression analyses were performed using RDSAT-generated individual weights for prior HIV testing (outcome variable). Variables significantly associated with prior HIV testing at the level of P<0.1 in the univariate analyses were included in the multivariate logistic regression model, calculating adjusted odds ratio (OR) and 95% confidence intervals (CI). Statistical analyses were carried out using STATA/SE V11.2™ (StataCorp LP, College Station, Texas, USA).
Results
Socio-demographic characteristics of study participants
Among the 492 respondents, 16 individuals (3.3%, 16/492) had enrolled in the 2009 survey. Of these 16, three individuals had been tested only once, all during the 2009 survey; the other 13 had been tested more than once. Since none of these 16 individuals tested HIV positive in the 2010 survey, we included them in the calculation of the HIV testing rate.
Of the 492 participants, 87% were never married and 98% were of Han ethnic origin. The median age was 24 years old [interquartile (IQR): 21-28, range: 18-65]; 78% were registered residents in Chongqing City. No income was reported by 29% and 45% were not enrolled in any health insurance plan. A quarter (25.2%) were students, of whom 88% were currently enrolled in college. The median age of having their first sex with a man was 20 years old (IQR: 18-23). More than one male sex partner in the past six months was reported by 56%, 18% of participants were currently living with a male sexual partner, and 40% had ever had sex with women. Two-thirds self-reported as preferring homosexual relations. Of 485 MSM (98.6%) who ever had anal sex, 33% preferred an insertive role, 30% preferred a receptive role, and 37% preferred both. Only half (51%) of participants perceived a high risk of getting HIV through homosexual contact. Among 477 MSM who had a recent male partner in the past six months, 94% of them (444/474) used condoms during anal sex, and 19% (89/474) always used condoms. (Table 1)
Table 1. Univariate and multivariate analysis of the association between selected characteristics and prior HIV testing behavior in 492 men who have sex with men in Chongqing City, China, 2010.
| Variables | Number of participants N=492 |
Never tested N=205 (%) |
Ever tested N=287 (%) |
Crude Odds Ratio (95%CI) |
P-value | Adjusted Odds Ratio (95%CI) |
P-value |
|---|---|---|---|---|---|---|---|
| Median age in years | 24 (21-28) | 23 | 24 | 1.03 (0.99-1.06) | 0.1 | ||
| (Interquartile range) | (20-28) | (22-28) | |||||
| Ethnicity | 0.2 | ||||||
| Han majority | 480 | 198 (41.2) | 282 (58.8) | 1.00 | |||
| Minorities | 12 | 7 (58.3) | 5 (41.7) | 0.45 (0.14-1.48) | |||
| Education | 0.004 | 0.008 | |||||
| High school or below | 168 | 85(50.6) | 83 (49.4) | 1.00 | 1.00 | ||
| College or above | 324 | 120(37.0) | 204 (63.0) | 1.76(1.19-2.59) | 1.74 (1.16-2.62) | ||
| Marital status | 0.8 | ||||||
| Single | 429 | 176 (41.0) | 253 (59.0) | 1.00 | |||
| Ever Married | 63 | 29 (46.0) | 34 (54.0) | 1.07 (0.62-1.86) | |||
| Having a cohabiting… | 0.03 | 0.06 | |||||
| male sexual partner | 90 | 28 (31.1) | 62 (68.9) | 1.00 | |||
|
female sexual partner or
living alone |
402 | 177 (44.0) | 225 (56.0) | 0.57 (0.35-0.94) | 0.61 (0.36-1.01) | ||
| Occupation | 0.2 | ||||||
| Student | 124 | 57 (46.0) | 67 (54.0) | 1.00 | |||
| Non-student | 368 | 148 (40.2) | 220 (59.8) | 1.36 (0.90-2.05) | |||
| Chongqing Hu Kou or registered residence | 0.8 | ||||||
| No | 107 | 47 (43.9) | 60 (56.1) | 1.00 | |||
| Yes | 385 | 158 (41.0) | 227 (59.0) | 1.06 (0.68-1.65) | |||
|
Having a health insurance
plan |
0.8 | ||||||
| No | 224 | 96 (42.9) | 128 (57.1) | 1.00 | |||
| Yes | 268 | 109 (40.7) | 159 (59.3) | 1.05 (0.72-1.51) | |||
| Ever having sex with a woman | |||||||
| No | 294 | 122 (41.5) | 172 (58.5) | 1.00 | |||
| Yes | 198 | 83 (41.9) | 20 (18-22) | 115(58.1) | 1.10 (0.76-1.60) | ||
|
Age at first sex with a man
(median, IQR) (year) |
20 | 20 (18-23) | 0.98 (0.94-1.02) | 0.2 | |||
| Self-reported sexual orientation | 0.2 | ||||||
| Homosexual | 331 | 130 (39.3) | 201 (60.7) | 1.00 | |||
| Bisexual | 161 | 75 (46.6) | 86 (53.4) | 0.78 (0.53-1.15) | |||
| Preferred role in anal sex* | |||||||
| Insertive | 162 | 55 (34.0) | 107 (66.0) | 1.00 | 1.00 | ||
| Almost equally | 180 | 79 (43.9) | 101 (56.1) | 0.62 (0.40-0.97) | 0.04 | 0.78 (0.49-1.26) | 0.3 |
| Receptive | 143 | 67 (46.9) | 76 (53.1) | 0.55 (0.34-0.88) | 0.01 | 0.58 (0.35-0.94) | 0.03 |
| Number of male partners in the past 6 months | 0.1 | ||||||
| ≤1 | 219 | 82 (37.4) | 137(62.6) | 1.00 | |||
| >1 | 273 | 123 (45.1) | 150 (54.9) | 0.74 (0.51-1.07) | |||
| Ever exchanging sex for money with a male partner in the past 6 months | 0.1 | ||||||
| No | 479 | 197 (41.1) | 282 (58.9) | 1.00 | |||
| Yes | 13 | 8 (61.5) | 5 (38.5) | 0.38 (0.12-1.23) | |||
| Number of female partners in the past 6 months | 0.8 | ||||||
| 0 | 436 | 181 (41.3) | 256 (58.7) | 1.00 | |||
| ≥1 | 56 | 25 (44.6) | 31 (55.4) | 0.94 (0.53-1.68) | |||
| Condom use with the recent male partner during the past 6 months § | 0.01 | ||||||
| No | 30 | 20 (66.7) | 10 (33.3) | 1.00 | 1.00 | ||
| Yes | 444 | 176 (39.6) | 268 (60.4) | 3.05 (1.37-6.81) | 0.007 | 2.87 (1.25-6.62) | |
| Self-perceived HIV risk via homosexual contacts | 0.07 | 0.08 | |||||
| Moderate or none | 243 | 92 (37.9) | 151 (62.1) | 1.00 | 1.00 | ||
| Great | 248 | 112 (45.2) | 136 (54.8) | 0.71 (0.49-1.03) | 0.71 (0.48-1.04) |
7 men reported oral sex or masturbation only
474 men reported having anal sex with the recent male partner during the past 6 months
The adjusted HIV and syphilis prevalence rates were 11.7% (95% CI: 8.6%-11.6%) and 4.7% (95% CI: 2.6%-7.3%), respectively.
Barriers and facilitators for HIV testing
Perceived barriers for taking an HIV test were assessed in 492 participants regardless of whether or not they had a history of HIV testing. The top four reasons for perceived barriers to HIV testing were psychological, including fear of knowing a positive result (78.7%), fear of discrimination with HIV positivity (76.7%), unwillingness of going to an HIV clinic (67.5%), and concern about meeting acquaintances at testing (67.1%). The response rates were similar between those who had and those who did not have a prior HIV testing for these four barriers. A structural barrier often mentioned was that persons did not know where to get tested; those who had not had prior testing (63%) were more likely to mention this reason than those who had (49%, P=0.001). (Figure 1)
Figure 1.
Perceived barriers for taking an HIV test by prior HIV testing experience among 492 MSM, Chongqing, China, 2010 (■ MSM who never took HIV testing;□ MSM who ever took HIV testing; *P<0.05)
Facilitating factors for HIV testing in the 492 MSM were a more sympathetic attitude from health staff (98.8%), guaranteed confidentiality (98.8%), a free or low cost test (98.2%), higher HIV/AIDS knowledge (98.0%), advice from a doctor/nurse (97.8%), anonymity (96.3%), including testing in a standard public health or medical visit (95.5%), availability of medicine for AIDS treatment (94.3%), no discrimination against AIDS in the community (94.1%), and the fact that other MSM had gone for testing (87.8%).
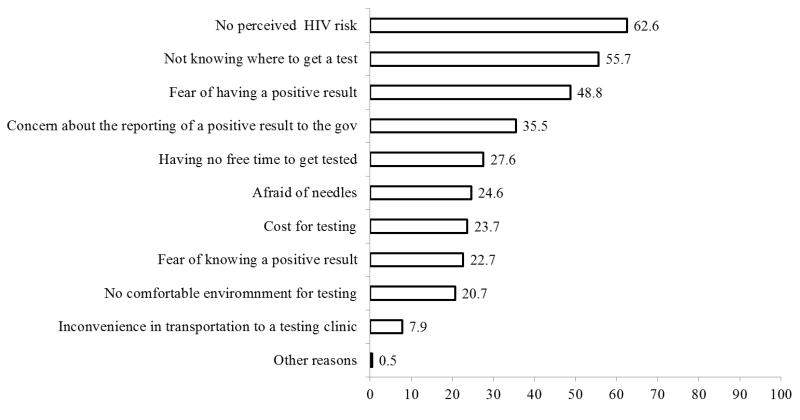
Never having had an HIV test was reported by 205 participants (42%), of whom 203 (99%) reported the actual reasons why they did not do so. The top five reasons were: no perceived HIV risk, not knowing where to get a test, fear of having a positive result, concern about the reporting of a positive result to the government, and having no free time to get tested (Figure 2).
Figure 2.
Barriers for HIV testing among 205 MSM who never took HIV testing, Chongqing, China, 2010
Factors associated with prior HIV testing
Of the 58% (287/492) of participants who had ever taken an HIV test, 29% had taken the test once, 29% twice, and 42% three times or more. Forty-five percent reported that their recent test was taken thanks to involvement in government or NGO projects. More persons (47%) were willing to go to a local CDC VCT clinic compared to a VCT clinic in a hospital (8%). Nearly three-quarters (73%) of ever tested MSM had taken their tests in the past 12 months prior to this 2010 survey. Higher educational level, cohabitation with a male partner, preferred insertive role in anal sex, condom use with a recent male sexual partner during the past six months, and self-perceived HIV risk were positively associated with prior HIV testing in the univariate analysis. A multivariable analysis model showed that those who had ever attended a college were more likely to take an HIV test than those who had not [adjusted odds ratio (AOR), 1.74; 95% CI, 1.16-2.62; P=0.008], as were MSM who used condoms with the recent male partner during the past six months were more likely to get tested (AOR: 2.87; 95%CI, 1.25-6.62; P=0.01).Those who preferred a receptive role in the anal intercourse were less likely to take an HIV test compared with those who preferred an insertive role (AOR, 0.58; 95%CI, 0.35-0.94; P=0.03), as were men cohabitating with female sexual partners or living alone, compared to those living with a male sexual partner (AOR, 0.62; 95%CI, 0.38-1.28; P=0.06) (Table 1).
Discussion
Our study found that 58% of MSM had a history of HIV testing in Chongqing City in southwestern China with an HIV prevalence rate in MSM of >11.7%. This testing frequency was higher than the national average of 44% in all risk groups estimated in 2011, and was also a bit higher than the estimated testing rate of 51% among MSM in 20095,14. China seems to be doing better than many other nations; a weighted average testing rate of 33% was reported from 34 low and middle-income countries in 200815. While the continuously increasing HIV testing rates among MSM in Chongqing City since 2006 suggest progress14, the rates are still disappointing compared with MSM in some metropolitans in high income countries, e.g., 90% in 21 cities in the United States16and 80.5% in Australia17.
Higher education, insertive roles in anal sex, and condom use were associated with prior HIV testing. Men with a college education were more likely to have been tested, perhaps due to their higher awareness of HIV risk. Well-educated MSM may have been oversampled with our respondent driving sampling, as the study sample included a significant proportion of college students and college students may be more likely to bring their fellow students to take a test.
Those who preferred receptive anal sex were less likely to have had an HIV test and we think it is important to study why men preferring receptive anal intercourse are less likely to test. That MSM who preferred receptive anal sex perceived themselves to have lower risk of HIV infection than those who preferred insertive anal sex (OR: 2.0, 95% CI:1.3-3.2; P=0.003) is especially worrisome18.
Those who used condoms during anal sex with their recent male sexual partner in the past 6 months were more likely to take a test. Condom use was measured within a timeframe of the last six months while testing experience was a lifetime measurement in our study. It is possible that those who used condoms more often may have gotten information about safe sex in their prior testing and counseling experience and thus increased their condom use.
Chongqing is one of the large cities in China where MSM are more visible and HIV prevalence is much higher than middle and small cities19. MSM prefer to seek sexual partners in large cities, often hiding their sexual identities from their families and friends in their hometowns20. HIV prevalence in the 2010 survey was 11.7%, higher than syphilis (4.7%). This difference was also seen in the 2009 survey (15.7% HIV vs.6.6% syphilis)11. This may reflect local public health interventions targeting at HIV/STD prevention and care among MSM9.
We found that fear of finding out about a positive result was the No.1 perceived barrier for taking an HIV test, followed by fear of discrimination, a closely related fear. These testing barrier findings have been seen worldwide, from Beijing migrant workers21to Peruvian MSM22 to high-income country MSM23. Such universal reported barriers suggested that psychological support, modifying general social attitudes, and education about the benefits of early therapy are essential to motivate MSM for HIV testing. Unwillingness to go to an HIV clinic and concern about meeting acquaintances at the testing clinic were additional barriers to testing. Rapid oral testing has become available in recent years in the Chinese market, and could be considered an alternative for a clinic-based ELISA testing strategy24. Its advantages include less invasiveness, easy access and application, ease of maintaining confidentiality, and elimination of anxiety associated with the waiting period for results24. However, linkage to counseling and care may be more difficult if self-testing becomes a norm. For persons getting clinic-based testing, high quality counseling and non-judgmental staff attitudes can help the clients to reduce their fear and concerns and can facilitate the linkage of seropositive persons to care.
The current version of Chinese HIV testing guidelines requires two ELISAs for screening and Western Blot for confirmatory testing; Chinese policy makers realized the limitations of this expensive and time consuming strategy, and a new version of HIV testing guidelines is being developed .Naturally, MSM who had no history of prior HIV testing were less likely to know where to get a test than those who had been tested before. Educating MSM about access to HIV service is important, particularly among male migrants (i.e., non-residents of Chongqing) who are unfamiliar with available services in their new environment.
More than half of the participants perceived themselves not at risk of HIV infection, particularly those who had never tested. About 90% (176/196) of those who never tested used condom during anal sex with their recent male partner in the past six month and 18% (36/196) reported always using a condom. Those men using condoms during sex might have considered themselves at lower risk of infection. Equally likely, men taking preventive precautions might not seek HIV testing due to their lower perception of HIV risk.
Education about HIV/AIDS and safer sex can motivate HIV testing. A study from Shenyang, China demonstrated that recently acquired knowledge about HIV might be a trigger for HIV testing25. In comparison, the two main reasons for not taking an HIV test in our study were low perceived risk of HIV infection and not knowing where to get tested. According to the Health Belief model, perceived susceptibility (potential risk to contract HIV) and perceived severity (understanding risk of AIDS and death) are positive predictors for behavioral change26. This emphasizes that both HIV education and counseling are top priorities to improve HIV testing in Chinese MSM; education can increase risk awareness and counseling can help reduce fear of taking HIV testing. Future intervention strategies should encourage MSM to go for HIV testing (cues to action) while helping establish confidence to achieve a long-term goal of reduced risk (self-efficacy). A study from Hong Kong found that cognitive variables such as attitudes, subjective norms, perceived control and behavioral intentions that were derived from the Theory of Planned Behaviors (TPB) were independently associated with lifetime and 12-month uptake of VCT27.
In China, VCT clinics offer free HIV testing while health care settings provide paid testing28. The coverage of the testing clinics has been extended to all 31 provinces, autonomous regions and municipalities, though many Chinese live far from testing centers4. In addition, the Chinese government has implemented guidelines for provider-initiated testing and counseling in medical facilities to further expand VCT to routine medical services4. The percentage of MSM who had been tested for HIV increased from 32.7% in 2007 to 44.9% in 2009, but has not risen markedly since4,5. The Chinese government has launched a “Five Year Plan” to strengthen the prevention and control for new HIV infections in most at-risk groups. In addition, the government also collaborated with international organizations to develop large-scale public health programs for HIV/AIDS prevention and care. For example, achieving universal access to prevention, treatment and care for HIV infected people is the goal of Chinese engagement with the Global Fund to Fight HIV, Tuberculosis and Malaria (Dr. Shaodong Ye, personal communication). Despite efforts to date, the MSM testing rate lags that of higher income nations, though VCT for MSM in China is highly cost-effective29. Several limitations existed in our study. First, self-reported information about the prior HIV testing experience may be subject to recall bias and social desirability bias, especially for sensitive questions that challenge social norms. CASI likely reduced, but did not eliminate these biases. Second, we could not disaggregate the motivations for taking an HIV test in our survey. Nearly half of the participants took a test due to enrollment in a public health project and may not do so of their own initiative.
Innovative interventions for improving uptake of HIV testing are needed among Chinese MSM. Multimedia social marketing campaigns can be effective intervention approaches to increase HIV testing30. Internet-delivered interventions via chat room, websites or short message service could be further developed for their acceptability and feasibility to promote testing in Chinese MSM31. Additionally, mobile vans for HIV testing in communities may provide easier access to testing32.
In summary, the HIV testing rate in the MSM population of Chongqing is still low. Mental and psychological support from health providers, family and friends, and the society as a whole are critical to encourage MSM to get tested. Education and social marketing need to be emphasized and expanded33. Structural interventions such as oral testing, and expanded, convenient test sites are important strategies to increase HIV testing, as are behavioral, contingency management, and social marketing interventions.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (81161120428), the National Institutes of Health (R01AI078933, D43TW001035 and R01AI094562), the Ministry of Science and Technology of China (2012ZX10001-002) and Chinese State Key Laboratory for Infectious Disease Develop Grant (2011SKLID102).
Footnotes
We declare no conflicts of interests.
References
- 1.UNAIDS [Accessed 12/1/2011];Getting to Zero: 2011-2015 Strategy. 2010 Dec 21; UNAIDS Resources Documents. Available at http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2010/JC 2034_UNAIDS_Strategy_en.pdf.
- 2.Thompson MA, Aberg JA, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2010 recommendations of the International AIDS Society-USA panel. JAMA. 2010;304:321–33. doi: 10.1001/jama.2010.1004. [DOI] [PubMed] [Google Scholar]
- 3.Kurth AE, Celum C, Baeten JM, et al. Combination HIV prevention: significance, challenges, and opportunities. Curr HIV/AIDS Rep. 2011;8:62–72. doi: 10.1007/s11904-010-0063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Health of the People’s Republic of China [Accessed 12/5/2011];China 2010 UNGASS Country Progress Report. 2010 UNAIDS China. Available at http://www.unaids.org/en/dataanalysis/monitoringcountryprogress/2010progressreportssub mittedbycountries/china_2010_country_progress_report_en.pdf.
- 5.Ministry of Health of the People’s Republic of China [Accessed 4/15/2012];China AIDS Response Progress Report. 2012 UNAIDS 2012 Progress reports submitted by countries]. March 31,2012.Available at http://www.unaids.org/en/dataanalysis/monitoringcountryprogress/progressreports/2012cou ntries/ce_CN_Narrative_Report%5B1%5D.pdf.
- 6.Beyrer C, Wirtz AL, Walker D, et al. [Accessed 10/15/2012];The Global HIV Epidemics among Men Who Have Sex with Men. 2011 May 27; The World Bank Documents & Reports. Available at http://siteresources.worldbank.org/INTHIVAIDS/Resources/375798-1103037153392/MSMReport.pdf.
- 7.Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chow EP, Wilson DP, Zhang L. What is the potential for bisexual men in China to act as a bridge of HIV transmission to the female population? Behavioral evidence from a systematic review and meta-analysis. BMC Infect Dis. 2011;11:242. doi: 10.1186/1471-2334-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y, Chen P, Lu R, et al. Prevalence of HIV among men who have sex with men in Chongqing, China, 2006-2009: cross-sectional biological and behavioural surveys. Sex Transm Infect. 2012;88:444–50. doi: 10.1136/sextrans-2011-050295. [DOI] [PubMed] [Google Scholar]
- 10.Li HM, Peng RR, Li J, et al. HIV Incidence among Men Who Have Sex with Men in China: A Meta-Analysis of Published Studies. PLoS One. 2011;6:e23431. doi: 10.1371/journal.pone.0023431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L, Ding X, Lu R, et al. Predictors of HIV and Syphilis among Men Who Have Sex with Men in a Chinese Metropolitan City: Comparison of Risks among Students and Non-Students. PLoS One. 2012;7:e37211. doi: 10.1371/journal.pone.0037211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 13.Volz E, Heckathorn DD. Probability Based Estimation Theory for Respondent Driven Sampling. Journal of Official Statistics. 2008;24:79–97. [Google Scholar]
- 14.Chow E, Wilson D, Zhang L. The rate of HIV testing is increasing among men who have sex with men in China. HIV Med. 2012;13:255–63. doi: 10.1111/j.1468-1293.2011.00974.x. [DOI] [PubMed] [Google Scholar]
- 15.Adam PC, de Wit JB, Toskin I, et al. Estimating levels of HIV testing, HIV prevention coverage, HIV knowledge, and condom use among men who have sex with men (MSM) in low-income and middle-income countries. J Acquir Immune Defic Syndr. 2009;52(Suppl 2):S143–51. doi: 10.1097/QAI.0b013e3181baf111. [DOI] [PubMed] [Google Scholar]
- 16.Finlayson TJ, Le B, Smith A, et al. HIV risk, prevention, and testing behaviors among men who have sex with men--National HIV Behavioral Surveillance System, 21 U.S. cities, United States, 2008. MMWR Surveill Summ. 2011;60:1–34. [PubMed] [Google Scholar]
- 17.Lyons A, Pitts M, Grierson J, et al. Sexual Behavior and HIV Testing Among Bisexual Men: A Nationwide Comparison of Australian Bisexual-Identifying and Gay-Identifying Men. AIDS Behav. 2012 doi: 10.1007/s10461-012-0148-7. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 18.Dosekun O, Fox J. An overview of the relative risks of different sexual behaviours on HIV transmission. Curr Opin HIV AIDS. 2010;5:291–7. doi: 10.1097/COH.0b013e32833a88a3. [DOI] [PubMed] [Google Scholar]
- 19.Xiao Y, Ding X, Li C, et al. Prevalence and correlates of HIV and syphilis infections among men who have sex with men in Chongqing Municipality, China. Sex Transm Dis. 2009;36:647–56. doi: 10.1097/OLQ.0b013e3181aac23d. [DOI] [PubMed] [Google Scholar]
- 20.Lau JT, Lin C, Hao C, et al. Public health challenges of the emerging HIV epidemic among men who have sex with men in China. Public Health. 2011;125:260–5. doi: 10.1016/j.puhe.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Song Y, Li X, Zhang L, et al. HIV-testing behavior among young migrant men who have sex with men (MSM) in Beijing, China. AIDS Care. 2011;23:179–86. doi: 10.1080/09540121.2010.487088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blas MM, Alva IE, Cabello R, et al. Risk Behaviors and Reasons for not Getting Tested for HIV among Men Who Have Sex with Men: An Online Survey in Peru. PLoS One. 2011;6:e27334. doi: 10.1371/journal.pone.0027334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lorenc T, Marrero-Guillamon I, Aggleton P, et al. Promoting the uptake of HIV testing among men who have sex with men: systematic review of effectiveness and cost-effectiveness. Sex Transm Infect. 2011;87:272–8. doi: 10.1136/sti.2010.048280. [DOI] [PubMed] [Google Scholar]
- 24.Chen MY, Bilardi JE, Lee D, et al. Australian men who have sex with men prefer rapid oral HIV testing over conventional blood testing for HIV. Int J STD AIDS. 2010;21:428–30. doi: 10.1258/ijsa.2010.009552. [DOI] [PubMed] [Google Scholar]
- 25.Zhou L, Guo J, Fan L, et al. Survey of motivation for use of voluntary counseling and testing services for HIV in a high risk area of Shenyang, China. BMC Health Serv Res. 2009;9:23. doi: 10.1186/1472-6963-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glanz K, Rimer BK. Theory at a Glance: A Guide for Health Promotion Practice. National Cancer Institute, National Institutes of Health; Bethesda, MD: 2005. [Google Scholar]
- 27.Gu J, Lau JT, Tsui H. Psychological factors in association with uptake of voluntary counselling and testing for HIV among men who have sex with men in Hong Kong. Public Health. 2011;125:275–82. doi: 10.1016/j.puhe.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 28.Wei C, Ruan S, Zhao J, et al. Which Chinese men who have sex with men miss out on HIV testing? Sex Transm Infect. 2011;87:225–8. doi: 10.1136/sti.2010.047407. [DOI] [PubMed] [Google Scholar]
- 29.Wang S, Moss JR, Hiller JE. The cost-effectiveness of HIV voluntary counseling and testing in China. Asia Pac J Public Health. 2011;23:620–33. doi: 10.1177/1010539511412576. [DOI] [PubMed] [Google Scholar]
- 30.Wei C, Herrick A, Raymond HF, et al. Social marketing interventions to increase HIV/STI testing uptake among men who have sex with men and male-to-female transgender women. Cochrane Database Syst Rev. 2011;9:CD009337. doi: 10.1002/14651858.CD009337. [DOI] [PubMed] [Google Scholar]
- 31.Noar SM. Computer technology-based interventions in HIV prevention: state of the evidence and future directions for research. AIDS Care. 2011;23:525–33. doi: 10.1080/09540121.2010.516349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lahuerta M, Sabido M, Giardina F, et al. Comparison of users of an HIV/syphilis screening community-based mobile van and traditional voluntary counselling and testing sites in Guatemala. Sexually Transmitted Infections. 2011;87:136–40. doi: 10.1136/sti.2010.043067. [DOI] [PubMed] [Google Scholar]
- 33.Hong Y, Li X. HIV/AIDS behavioral interventions in China: a literature review and recommendation for future research. AIDS Behav. 2009;13:603–13. doi: 10.1007/s10461-008-9483-0. [DOI] [PMC free article] [PubMed] [Google Scholar]