Abstract
Objective
This prospective study aimed to describe the nature and time course of HPA axis dysregulation and psychopathology among terror-bereaved spouses.
Method
Twenty-three spouses bereaved from September 11, 2001 terror attacks and 22 nonbereaved spouses were compared using a psychiatric diagnostic interview (SCID), three days of salivary cortisol collection, and a dexamethasone suppression test. Most subjects had repeated assessments at six month intervals during the two year study.
Results
After September 11, 2001, bereaved compared to nonbereaved had significantly higher rates of posttraumatic stress disorder (PTSD) (68.1% versus 0%) and major depressive disorder (MDD) (45.5% versus 9.5%). Bereaved had significantly higher morning basal cortisol and less afternoon postdexamethasone cortisol suppression than nonbereaved. Among bereaved, those with PTSD without comorbid MDD had significantly greater afternoon postdexamethasone cortisol suppression than those without psychiatric disorders.
Conclusions
Terror-related spouse death is a severe stressor associated with persistent HPA axis activation, PTSD, and MDD. However, bereaved spouses who developed PTSD and were not depressed had enhanced postdexamethasone cortisol suppression, evidence of heightened glucocorticoid receptor sensitivity.
Keywords: Bereavement, Cortisol, PTSD, MDD, September 11
Introduction
Most bereaved spouses experience moderate emotional difficulties that usually abate within two years after spouse death (1) but anxiety, depression, anger, and violent spouse death increase psychosocial impairment (2). Increased basal cortisol following loss (3) and resistance to dexamethasone suppression among bereaved adults with harm-avoidant temperament and chronic dysphoric mood or anxiety (4, 5) has been reported.
Although low basal cortisol and high cortisol suppression have been identified among adults with PTSD in numerous studies of traumatic events (6), other studies reported no differences in these HPA axis measures among war exposed adults with or without PTSD (7) and no indication that HPA axis dysregulation after acute trauma preceded PTSD onset (8). There is some evidence that prior trauma (6) and soft neurological signs and brain abnormalities (9) increase PTSD risk and reduce propensity to HPA axis dysregulation after trauma. Currently, a paucity of prospective research exists evaluating relations between HPA axis reactivity and psychopathology following trauma and bereavement.
Epidemiological studies document high Posttraumatic Stress Disorder (PTSD) rates after terrorist attacks on September 11, 2001 (9/11/01) (10). This event offered an opportunity to prospectively examine the alterations in psychopathology and HPA axis regulation in traumatically bereaved subjects. We hypothesized that after terror-related spouse death, bereaved compared to nonbereaved spouses would have 1) greater HPA axis activation, evidenced by higher basal salivary cortisol levels and less dexamethasone suppression of salivary cortisol and 2) persistent PTSD and MDD. This study explored whether HPA axis dysregulation is associated with concurrent PTSD and MDD diagnoses.
Method
Design
Individuals bereaved by terror-related spouse death and nonbereaved were compared at study entry and six month intervals for two years on HPA axis indices and psychiatric disorder rates.
Participants (Table 1)
Table 1.
Characteristics of 23 Bereaved and 22 Nonbereaved Spouses
| Bereaved (N=23) | Nonbereaved (N=22) | Statistical Analyses | |
|---|---|---|---|
| Age (years) at 9/11/01 | 41.79 ± 6.52 | 41.12 ± 6.46 | t(43)=0.35, P=0.73a |
| Gender (Female) | 91.30% | 100% | P=0.49b |
| Ethnicity/Race | X2(3)=5.03, P=0.17c | ||
| White | 86.95% | 68.18% | |
| Black | 0% | 13.64% | |
| Hispanic | 4.35% | 13.64% | |
| Asian | 8.70% | 4.54% | |
| Socioeconomic Status | X2(2)=0.79, P=0.67c | ||
| High | 69.57% | 72.73% | |
| Middle | 13.04% | 18.18% | |
| Low | 17.39% | 9.09% | |
| Lifetime Psychiatric Disorders before 9/11/01 | |||
| Anxiety Disorder | 31.82% | 42.86% | P=0.54b |
| MDD | 0% | 14.29% | P=0.11b |
| Simple Phobia | 13.64% | 19.05% | P=0.70b |
| PTSD | 0% | 0% | |
| Lifetime Stressful Events before 9/11/01 | 30.43% | 36.36% | P=0.76b |
| Study Entry months after 9/11/01 | 19.00 ± 9.82 | 19.93 ± 8.19 | X2(1)=0.03, P=0.86d |
| Last Assessment months after 9/11/01 | 27.24 ± 10.76 | 28.51 ± .27 | X2(1)=2.35, P=0.13d |
| Number of Assessments | 2.13(range 1-8) | 1.82 (range 1-4) | t(43)=0.86, P=0.40a |
Note: No significant differences between bereaved and nonbereaved spouses at entry after 9/11/01
Tests:
Student”s T
Fisher's Exact
Chi-Square
Log Rank
Twenty-three spouses bereaved by 9/11/01 terror-related spouse deaths in New York City and 22 nonbereaved spouses participated. All were parents of 6 to 12 year old children in a concurrent study (11). Bereaved spouses were recruited from advertisements in schools, police and fire departments, and corporations where the terror-related decedents worked (11). Nonbereaved were recruited from advertisements in schools (11) and excluded if they lived or worked at or near the World Trade Center preceding or after 9/11/01, had a relative who died from these terror attacks, or were rescue workers or first responders. Bereaved and nonbereaved with trauma histories before 9/11/01 were excluded. Nonbereaved were recruited to match bereaved on distributions at 9/11/01 of age, gender, ethnicity/race, social status (12) a month before 9/11/01, and lifetime psychiatric disorder rates before 9/11/01. All participants were physically healthy nonsmokers. Female predominance concurs with data that over 80% of 9/11/01 decedents were males (13). Two (8.70%) bereaved were menopausal. Bereaved and nonbereaved had similar types of lifetime stresses before 9/11/01. Bereaved and nonbereaved had similar numbers of assessments and times of study entry (earliest at four months, latest at three years) and final assessments.
Weill Cornell Medical College Institutional Review Board-approved written informed consent was obtained.
Psychiatric Disorder and Stressful Life Events Assessments
All current psychiatric disorders were evaluated at entry and six month intervals thereafter in subject interviews using full Structured Clinical Interview for DSM IV (SCID) (14) administered by trained research assistants blind to subjects’ bereavement status. All lifetime psychiatric disorders before 9/11/01 and psychiatric disorders with onset after 9/11/01 but before entry were SCID evaluated at entry. Lifetime stressors including family deaths, serious illness, and marital and financial problems before 9/11/01 were evaluated at entry and post-9/11/01 current stressors were identified at each assessment using a brief self-report checklist.
Cortisol Measurements
Basal and postdexamethasone salivary cortisol samples were collected at home at each assessment using the Salivette device (Sarstedt, Inc., Newton, North Carolina) on four consecutive days starting Monday morning (AM) (day 1) and ending Thursday evening (PM) (day 4). On day three, 1.0 mg dexamethasone was ingested orally immediately after collecting evening cortisol; a dose chosen because it was more sensitive than 0.5 mg (15) for detecting differences among stressed and non-stressed subjects. To increase compliance in collecting cortisol and dexamethasone administration, research staff telephoned participants daily to discuss these activities. Participants collected basal and postdexamethasone cortisol 30 minutes after awakening at 7AM and at 4PM and 9PM.
Three days of basal cortisol were utilized to minimize impact of day-to-day cortisol secretion variability and influences of stressors or activity. There were good compliance rates for all three AM (>86%) and PM (>86%) and 4PM (> 93%) basal and postdexamethasone AM (>78%), 4PM (>76%), and PM (>75%) cortisol samples. Dexamethasone blood concentrations were not obtained to confirm dexamethasone ingestion and control for differences in subjects’ dexamethasone levels.
A psychiatrist (CRP), who was not blind to subjects’ bereavement status, interviewed subjects to identify health problems, medications or intense physical exercise that may affect HPA axis function. No participants were excluded for these issues. Five (21.74%) bereaved and 4 (18.18%) nonbereaved refused dexamethasone and were not included in postdexamethasone suppression analyses. If a subject took short-term medication, such as an antibiotic, or had acute cold symptoms or injury, assessment was delayed three weeks to avoid cortisol measurement distortion.
Subjects were instructed to abstain from eating at least 15 minutes before cortisol collection and during collection to gently chew on a cotton swab for approximately one minute to saturate it with saliva before inserting it in a collection tube. Samples were refrigerated during collection at home and then frozen at − 80 ° C until assay with an ELISA kit optimized for salivary samples (Salimetrics, State College, Pa). The laboratory director (MA) and technicians were blind to subjects’ bereavement status. Cortisol samples were run in duplicate and mean value was calculated for each sample. Two percent of postdexamethasone cortisol values were below assay detection limit and were assigned the detection limit value (0.01 ug/dl). Intra-assay and inter-assay variability was less than 4% and 9%, respectively.
Statistical Analyses
Descriptive statistics are provided as means and standard deviations. Cross-sectional comparisons used chi-square or Fisher exact tests for categorical and Student's t tests for continuous variables. McNemar tests measured within-subject psychiatric disorder rate changes from before to after 9/11/01.
Mixed effects models for repeated measures (16) included linear models, yielding Wald t test statistics, for cortisol measures and mixed effects logistic regression for categorical psychiatric disorder variables. Both intercept and regression coefficients of time from 9/11/01 to each assessment were modeled as random to account for within-family correlations and varying outcome trajectories. Bereavement status was modeled as fixed. Testing hypotheses was based on analyses of log-transformed cortisol levels. Untransformed cortisol values are shown in figures. Log-odds based on estimated regression lines were converted to probability of having diagnoses during follow-up. Statistical analyses were preformed using SAS (SAS Institute Inc, Cary North Carolina) vol 8.2, PROC MIXED, and NLMIXED for continuous and dichotomous outcomes, respectively. Statistical significance was declared as two-sided p-values < 0.05. Degrees of freedom (df) varied depending on number of observations appropriate for specific variables.
There were no significant differences in AM or PM cortisol across the three basal cortisol measurement days. Averages of three basal cortisol levels at AM and PM are presented. Postdexamethasone cortisol suppression was calculated as difference between basal and postdexamethasone cortisol at AM, afternoon, and PM, while controlling for basal cortisol at these times. The resulting estimated log-scale difference was converted to percent cortisol suppression. Psychiatric disorder effects on basal cortisol and cortisol suppression were modeled as a four-level variable including current PTSD without (N=5) versus with (N=10) comorbid MDD versus bereaved (N=7) versus nonbereaved (N=16) without psychiatric disorders and as time-varying independent variables, i.e., considering psychiatric disorders present at cortisol collection time. Age, gender, ethnicity/race, and stressful life events before 9/11/01 were not included as covariates because they were not significantly associated with basal cortisol, cortisol suppression, or psychiatric disorders after 9/11/01. Low psychiatric disorder rates before 9/11/01 and low stressful life events post-9/11/01 precluded statistical evaluation of their effects on cortisol.
After 9/11/01, more bereaved received psychotherapy (bereaved: 76.19%, nonbereaved: 25%, p = 0.002) and were treated with antidepressant/antianxiety medications (bereaved: 33.33%, nonbereaved: 10%, p = 0.13). Psychotherapy or antidepressant/antianxiety medications were not included as covariates because mixed effects models evaluating time by treatment interactions identified no significant psychotherapy or medication effects on basal cortisol or cortisol suppression or psychotherapy effects on psychiatric disorders.
Results
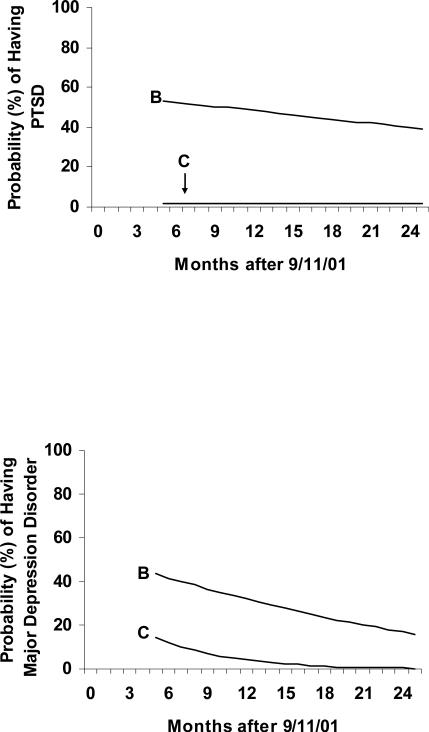
Psychiatric Disorders (Figure 1)
Figure 1.
Probability of Current Posttraumatic Stress Disorder (PTSD) or Major Depressive Disorder (MDD) among 23 Bereaved (B) and 22 Nonbereaved (C) after 9/11/01
Note: Probability of current PTSD or MDD among bereaved did not decline significantly but was persistently low among nonbereaved.
Bereaved (p < 0.0009) but not nonbereaved (p = 0.32) had significantly increased psychiatric disorder rates from pre-to-post 9/11/01. After 9/11/01, bereaved versus nonbereaved had significantly higher PTSD (68.18% versus 0%, p = 0. 0001) and MDD (45.45% versus 9.52%, p = 0.02) rates. Bereaved PTSD (t [42] = −0.36, p = 0.72) or MDD (t [21] = −0.58, p = 0.57) probability did not decline significantly and was persistently low for nonbereaved (PTSD: t [37] = 0.00, p = 1.00, MDD: t [20] = −1.42, p = 0.17). A significant medication by time interaction (F [1, 19.3] = 26.04, p < 0.0001) for the four (40%) bereaved with MDD comorbid with PTSD suggested that declines in these disorders’ probabilities may be related to antidepressant/antianxiety medications.
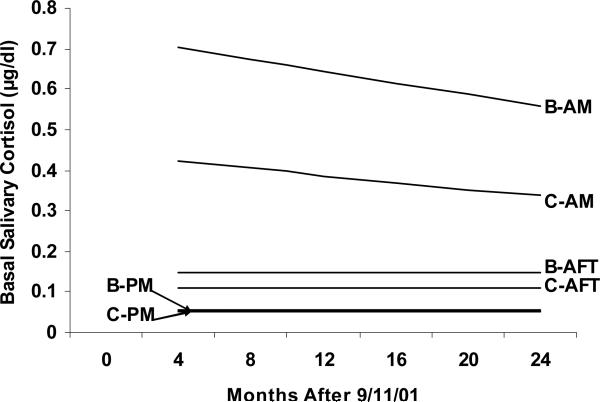
Basal Cortisol (Figure 2)
Figure 2.
AM, Afternoon (AFT), and PM Basal Salivary Cortisol Levels among 23 Bereaved (B) and 22 Nonbereaved (C) after 9/11/01
Note: Bereaved compared to nonbereaved had significantly higher AM and tendency for higher AFT basal cortisol. Only bereaved and nonbereaved AFT basal cortisol decreased significantly.
AM bereaved cortisol was significantly higher than nonbereaved (t [42.5] = 3.67, p < 0.0007) without a significant decline for the combined bereaved-nonbereaved sample (t [44.8] = −1.65, p = 0.11) or time by group interaction (F [1, 54.3] = 0.12, p = 0.73).
Afternoon bereaved cortisol tended to be higher than nonbereaved (t [27.2] = 1.81, p = 0.08) and decreased significantly for the combined bereaved-nonbereaved sample (t [77.1] = −2.03, p < 0.05) without time by group interaction (F [1, 52.6] = 2.54, p = 0.12). There was no significant bereavement effect on PM cortisol (t [46.7] = 0.75, p = 0.46).
Diurnal cortisol variation was preserved for bereaved (F [2, 115] = 175.8, p < 0.0001) and nonbereaved (F [2, 120] = 118.74, p < 0.0001).
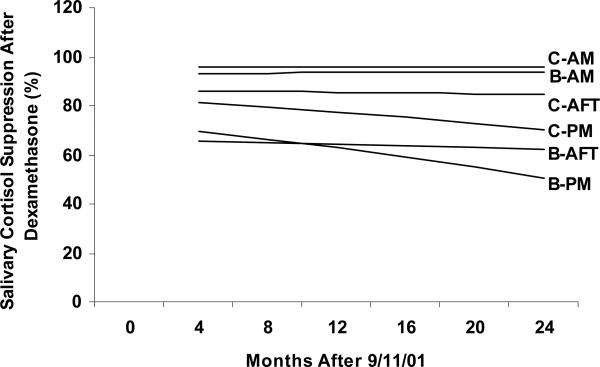
Cortisol Suppression (Figure 3)
Figure 3.
AM, Afternoon (AFT), and PM Percent Postdexamethasone Cortisol Suppression among 18 Bereaved (B) and 18 Nonbereaved (C) after 9/11/01.
Note: Only bereaved AFT cortisol suppression was significantly less than nonbereaved.
Bereaved had significantly less afternoon cortisol suppression than nonbereaved (t [22.1] = −2.61, p < 0.02) without changes for the combined bereaved-nonbereaved sample (t [18.4] = −0.28, p = 0.79) and no time by group interaction (F [1, 66.8] = 2.01, p = 0.16). Bereaved and nonbereaved cortisol suppression was not significantly different at AM (t [23.5] = −1.19, p = 0.25) or PM (t [31.9] = −1.22, p = 0.23).
Cortisol and Psychiatric Disorders
Afternoon cortisol suppression, affected by PTSD (F [3, 35.2] = 3.64, p < 0.02), was significantly greater for bereaved with PTSD without comorbid MDD than bereaved without psychiatric disorders (t [36.2] = 2.43, p < 0.02) and tended to be greater for bereaved with comorbid PTSD and MDD than bereaved without psychiatric disorders (t [32.4] = 1.76, p < 0.09). There was no time by group interaction (F [3, 37.7] = 0.94, p < 0.43).
Discussion
This prospective study identified persistent HPA axis dysregulation and psychopathology among 9/11/01 terrorist-related decedents’ spouses. As hypothesized, persistently high AM basal cortisol and less afternoon cortisol suppression was observed among the bereaved group. In contrast, bereaved with PTSD without comorbid MDD had significantly greater afternoon cortisol suppression than bereaved without psychiatric disorders. This finding is consistent with other research on PTSD and provides further support for glucocorticoid receptor sensitization as a component of PTSD (6). As time passed after 9/11/01, nonbereaved cortisol levels decreased, which may be related to reduced fears of threat and less disruption in daily routines.
PTSD rates were higher among bereaved (68.18%) and similar among nonbereaved (0%) to those in the New York City area within six months post-9/11/01, comparing participants not directly affected (3.7%) or directly affected by loss of relatives, home or job or being on-site during the attacks (12%) (10).
Generalizability is limited by a small sample of predominantly female Caucasians. In addition, 33% bereaved were using psychotropic medications and 76% received psychotherapy, which may have led to underestimation of psychiatric and HPA axis sequellae of traumatic bereavement. No statistical correction was made for multiple analyses’ p-values and findings should be interpreted cautiously.
Clinical and Research Implications
Long-term studies are needed to determine when, if ever, bereaved recover from persistent HPA axis activation, PTSD and MDD and whether persistent HPA axis dysregulation associated with traumatic bereavement affects cognitive function. Medical monitoring of bereaved may identify impaired immunity, obesity, atherosclerosis, and bone demineralization associated with persistent HPA axis hyperactivity (17).
High PTSD and MDD rates among terror-bereaved emphasize importance of psychiatric evaluation and treatment shortly after violent spouse death. Further work is needed to determine whether early treatment (18) could prevent development of PTSD in traumatically bereaved. While uncontrolled psychotherapy or medication had no effect on reducing salivary cortisol levels in this study, treatments specific to complicated grief (19) should be studied for efficacy in preventing or ameliorating HPA axis hyperactivity.
Acknowledgements
This study, funded by National Institute of Mental Health Grant RO1MH-066367 to Cynthia R. Pfeffer, M.D, is indebted to bereaved and nonbereaved participants and to Ruth Yang M.A. for assaying cortisol.
References
- 1.Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 2.Kaltman S, Bonanno GA. Trauma and bereavement: examining the impact of sudden and violent deaths. Journal Anxiety Disorders. 2003;17:131–147. doi: 10.1016/s0887-6185(02)00184-6. [DOI] [PubMed] [Google Scholar]
- 3.Petitto JM, Quade D, Evans DL. Relationship of object loss during development to hypothalamic pituitary-adrenal axis function during major affective illness later in life. Psychiatry Research. 1992;44:227–236. doi: 10.1016/0165-1781(92)90026-y. [DOI] [PubMed] [Google Scholar]
- 4.Gerra G, Monti D, Paneral AE, Sacerdote P, Anderlini R, Avanzini P, Zaimovic A, Brambila F, Franceschi C. Long-term immune-endocrine effects of bereavement: relationships with anxiety levels and mood. Psychiatric Research. 2003;121:145–158. doi: 10.1016/s0165-1781(03)00255-5. [DOI] [PubMed] [Google Scholar]
- 5.Shuchter SR, Zisook S, Kirkorowicz C, Risch C. The dexamethasone suppression test in acute grief. American Journal Psychiatry. 1986;143:879–881. doi: 10.1176/ajp.143.7.879. [DOI] [PubMed] [Google Scholar]
- 6.Yehuda R. Current status of cortisol findings in post-traumatic stress disorder. Psychiatric Clinics of North America. 2002;25:341–368. doi: 10.1016/s0193-953x(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 7.Metzger LJ, Carson MA, Lasko NB, Paulus LA, Orr SP, Pitman RK, Yehuda R. Basal and suppressed salivary cortisol in female Vietnam nurse veterans with and without PTSD. Psychiatry Research. 2008;161:330–335. doi: 10.1016/j.psychres.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shalev AY, Videlock EJ, Peleg T, Segman R, Pitman RK, Yehuda R. Stress hormones and post-traumatic stress disorder in civilian trauma victims: a longitudinal study. Part I: HPA axis responses. International Journal of Neruopsychopharmacology. 2008;11:365–372. doi: 10.1017/S1461145707008127. [DOI] [PubMed] [Google Scholar]
- 9.Pitman RK, Gilbertson MW, Gurvits TV, May FS, Lasko NB, Netzger LJ, Shenton ME, Yehuda R, Orr SP. Clarifying the origin of biological abnormalities in PTSD though the study of identical twins discordant from combat exposure. Annals of the New York Academy Science. 2006;1071:242–254. doi: 10.1196/annals.1364.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galea S, Resnick H. Posttraumatic stress disorder in the general population after mass terrorist incidents: Considerations about the nature of exposure. CNS Spectrums. 2005;10:107–115. doi: 10.1017/s1092852900019441. [DOI] [PubMed] [Google Scholar]
- 11.Pfeffer CR, Altemus M, Heo M, Jiang H. Salivary cortisol and psychopathology in children bereaved by the 9/11/01 terror attacks. Biological Psychiatry. 2007;61:957–965. doi: 10.1016/j.biopsych.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Hollingshead AB, Redlich P. Social Class and Mental Illness. Wiley; New York: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MMWR Deaths in World Trade Center Terrorist Attacks-New York City, 2001. 2002;51:18. [PubMed] [Google Scholar]
- 14.Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG. The Collaborative Longitudinal Personality Disorders Study. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 15.Young EA, Vazquez D, Jiang H, Pfeffer CR. Saliva cortisol and response to dexamethasone in children of depressed parents. Biological Psychiatry. 2006;60:831–836. doi: 10.1016/j.biopsych.2006.03.077. [DOI] [PubMed] [Google Scholar]
- 16.Laird NM, Ware JH. Random effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 17.McEwen BS. Mood disorders and allostatic load. Biological Psychiatry. 2003;54:200–207. doi: 10.1016/s0006-3223(03)00177-x. [DOI] [PubMed] [Google Scholar]
- 18.Pitman RK, Delahanty DL. Conceptually driven pharmacologic approaches to acute trauma. CNS Spectrum. 2005;10:99–106. doi: 10.1017/s109285290001943x. [DOI] [PubMed] [Google Scholar]
- 19.Shear K, Frank E, Houck PR, Reynolds CF. Treatment of complicated grief: a randomized controlled trial. Journal of the American Medical Association. 2005;293:2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]