Summary
There is pressing need to develop alternatives to annual influenza vaccines and antiviral agents licensed for mitigating influenza infection. Previous studies reported that acute lung injury (ALI) caused by chemical or microbial insults is secondary to generation of host-derived, oxidized phospholipid that potently stimulates Toll-like Receptor 4 (TLR4)-dependent inflammation1. Subsequently, we reported that TLR4−/− mice are highly refractory to influenza-induced lethality2, and hypothesized that therapeutic antagonism of TLR4 signaling would protect against influenza-induced ALI. Herein, we report that therapeutic administration of Eritoran (E5564), a potent, well-tolerated, synthetic TLR4 antagonist3,4, blocks influenza-induced lethality in mice, as well as lung pathology, clinical symptoms, cytokine and oxidized phospholipid expression, and decreases viral titers. CD14 and TLR2 are also required for Eritoran-mediated protection, and CD14 directly binds Eritoran and inhibits ligand binding to MD2. Thus, Eritoran blockade of TLR signaling represents a novel therapeutic approach for inflammation associated with influenza, and possibly other, infections.
Influenza continues to evolve, and new antigenic variants emerge annually, giving rise to seasonal outbreaks. During annual influenza epidemics, 5–15% of the population is affected with upper respiratory tract infection, with hospitalization and death occurring mainly in the elderly and chronically ill. Annual influenza epidemics are estimated to result in 3 – 5 million cases of severe illness and 250,000 – 500,000 deaths yearly worldwide5,6. In addition, strains to which humans have no prior immunity may appear suddenly, and the resulting pandemics can be catastrophic, as illustrated by the 1918 “Spanish flu” that killed millions7,8. Logistical problems related to prediction of future immunogenic epitopes and production and distribution issues, often limit efficacy and/or vaccine availability. Moreover, increasing resistance to existing antiviral therapy, coupled with the need to administer these agents within 2–3 days after infection, limits their usefulness9–11. Thus, there is a critical need for a safe and effective therapeutic adjunct and/or alternative to influenza vaccines and antiviral agents.
The prototype Toll-like receptor 4 (TLR4) agonist, Gram negative lipopolysaccharide (LPS), is a highly potent inflammatory stimulus that has been strongly implicated in Gram negative septic shock, including acute respiratory distress syndrome caused by endothelial leak12. In 2008, Imai et al.1 published a highly provocative paper in which they proposed that induction of acute lung injury (ALI), induced by acid aspiration, infection by respiratory viruses and bacteria, or exposure to their products (e.g., inactivated H5N1 influenza), was mediated by a common signaling pathway: NADPH oxidase-dependent production of reactive oxygen species generated oxidized host phospholipids, e.g., oxidized 1-palmitoyl-2-arachidonoyl-phosphaticylcholine (OxPAPC), that, in turn, potently stimulated TLR4. They proposed that the ensuing cytokine storm, and in particular, IL-6, mediated ALI. The finding of Nhu et al. that TLR4−/− mice were protected from lethality caused by mouse-adapted influenza virus (A/PR/8/34; “PR8”)2, led us to hypothesize that blocking TLR4 therapeutically would protect against influenza infection. Herein, we provide compelling data showing that Eritoran (E5564) (Eisai, Inc.), an extremely potent TLR4 antagonist3,4, is highly protective when administered therapeutically to mice infected with a lethal dose of influenza.
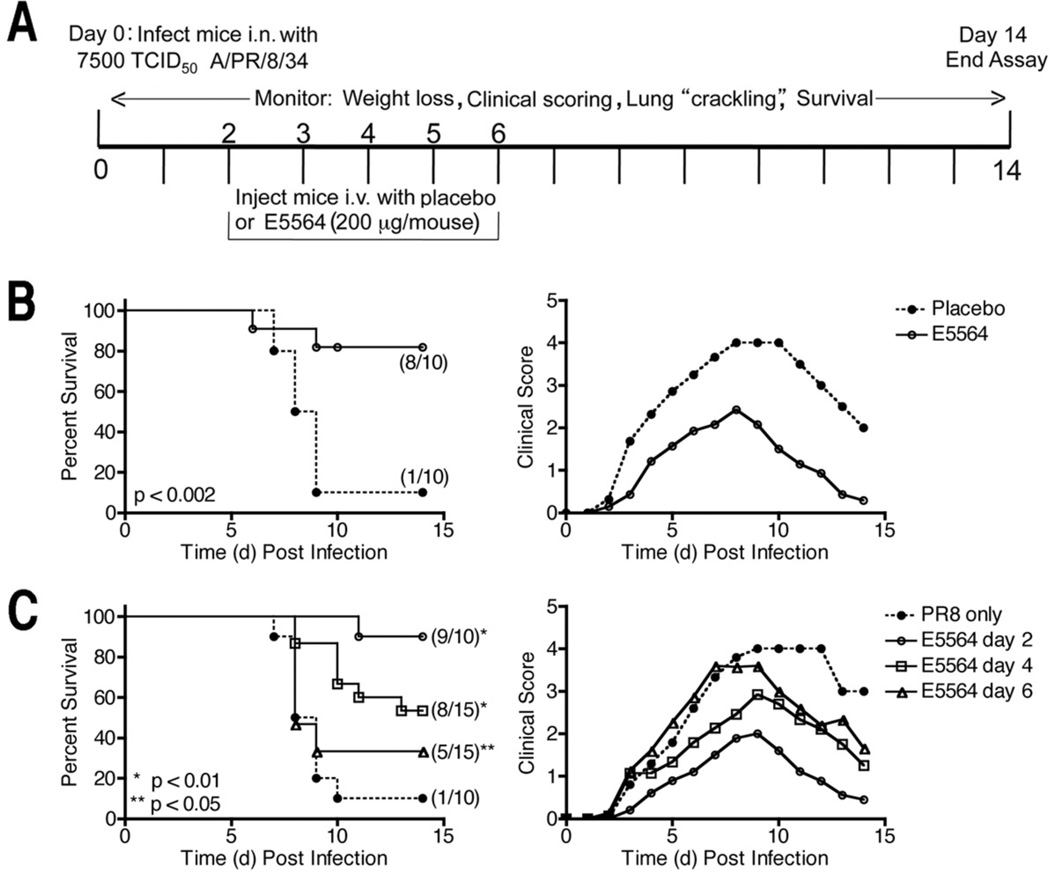
Fig. 1A illustrates our initial protocol. On “Day 0,” 6–8 wk old, female C57BL/6J mice were infected intranasally (i.n.) with a dose of PR8 that was determined to kill ~90% of mice (~LD90). Two days later, the TLR4 signaling antagonist, Eritoran (E5564), was administered daily for 5 consecutive days (200 µg/mouse; Days 2–6) intravenously (i.v.). Each mouse was weighed and clinical symptoms (e.g., lethargy, piloerection, ruffled fur, hunched posture, rapid shallow breathing, audible rattling) were scored daily for 2 weeks. Eritoran-treated mice were significantly protected from influenza-induced lethality, while 90% of mice administered placebo (vehicle only) succumbed (Fig. 1B, left panel). This was paralleled by more severe clinical scores (Fig. 1B, right panel) and weight loss (Supplementary Fig.1A) in control mice vs. Eritoran-treated mice. Treatment of mice with 10-fold less Eritoran (20 µg/mouse) decreased survival to 40% (4/10 mice survived) (data not shown). The efficacy of Eritoran treatment decreased from 90% survival in mice infected with 7500 TCID50 to 60% and 25% survival in mice infected with 10,000 and 20,000 TCID50, respectively (Supplementary Fig. 1B). Treatment with Eritoran also protected mice infected with a lethal dose of the non-adapted 2009 human pandemic influenza strain A/California/07/2009 H1N1 (Supplementary Fig. 1C).
Figure 1.
Eritoran treatment protects mice from lethal influenza challenge. (A) Basic experimental protocol used to test Eritoran in mice infected with influenza. C57BL/6J mice were infected with mouse-adapted influenza, strain PR8 (~7500 TCID50, i.n.; ~LD90). Two days later, mice received placebo (vehicle only) or E5564 (Eritoran; 200 µg/mouse i.v.) once daily for 5 successive days (Days 2 to 6). (B) Mice were treated as shown in (A). In the left graph, survival was monitored daily (p <0.002). In the right graph, clinical scores (see Methods) were also measured daily. Each graph represents the combined results of 2 separate experiments, each with 5 mice/treatment/experiment. (C) Mice were infected as described in (A), but treated with Eritoran starting on Days 2, 4, or 6 post-infection. Left panel, survival (Day 2 and Day 4, p < 0.01; Day 6, p ≤ 0.05); right panel, clinical scores. Results are combined results from 2 to 3 separate experiments, with 5 mice/treatment group/experiment.
Additional experiments were performed in which Eritoran treatment was started on Day 2, Day 4, or Day 6 post-infection. Fig. 1C (left panel) illustrates that 90% of PR8-infected mice that did not receive Eritoran treatment died, while mice that received Eritoran starting at Days 2, 4, or 6 exhibited statistically significant survival rates of 90%, 53%, and 33%, respectively. The clinical scores for these same mice (Fig. 1C, right panel) illustrate that the later mice began Eritoran treatment, the more severe their clinical scores. Mice that did not receive Eritoran exhibited the most severe symptoms and highest clinical scores. Similarly, weight loss was progressively greater the later treatment was initiated after infection (data not shown). Thus, in contrast to current antivirals that must be administered early after infection, Eritoran treatment significantly enhanced survival, even when started as late as 6 days post-infection.
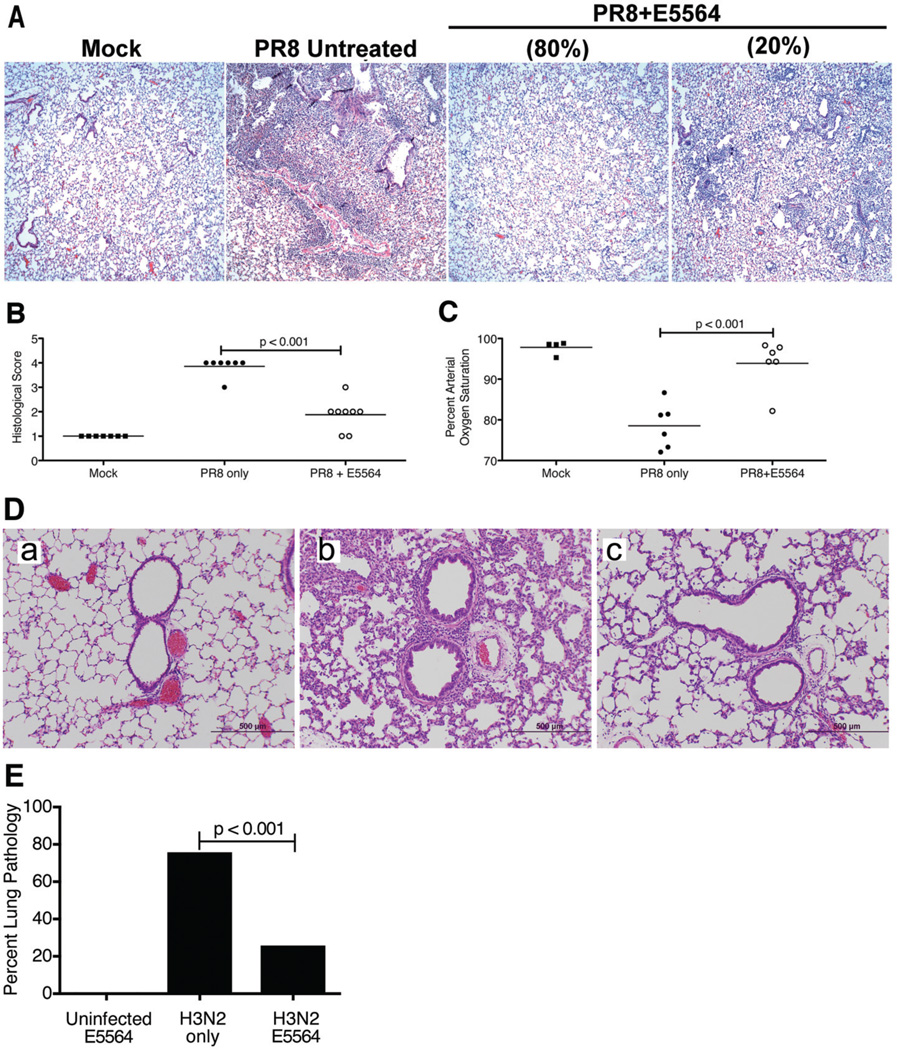
Eritoran treatment also led to a signficant reduction in influenza-induced lung pathology. Groups of mice received saline only (“Mock”), PR8 only (“PR8 Untreated”), or PR8-infected and Eritoran treated (PR8+E5564) starting 2 days post-infection (per Fig. 1A) and were euthanized 7 days post-infection. In mice infected with PR8 only, extensive lung damage (i.e., highly basophilic lining epithelium in the bronchioles, focal degenerating cells undergoing apoptosis or necrosis, and extensive cellular infiltrates (neutrophils, monocytes, and lymphocytes)) were observed; however, in infected, Eritoran-treated mice, ~80% of each lung section examined exhibited nearly normal lung architecture (similar to “Mock”), while in ~20% of each section, inflammatory infiltrates could be observed, although to a lesser extent than in lungs of mice infected with PR8 only (Fig. 2A). These observations are supported by blinded histological scoring (Fig. 2B). By Day 14 post-infection, Eritoran-treated mice showed normal lung architecture (data not shown). Previously, Verhoeven et al.13 reported a direct correlation between pulse-oximetry measurements of oxygen saturation and lung pathology that reflected the morbidity and survival of mice infected with PR8. By Day 6 post-infection, the oxygen saturation levels observed between mock-infected and PR8-infected, Eritoran treated mice was not significantly different. In contrast, PR8-infected mice demonstrated a significant oxyhemoglobin desaturation to 78%, suggesting a functional consequence of the alveolar injury demonstrated histologically (Fig. 2C).
Figure 2.
Eritoran treatment inhibits influenza-induced lung pathology and lung function. (A) Eritoran treatment improves lung pathology induced by PR8 infection. Representative H&E-stained sections were derived from mice treated as described in the text (4–5 mice/treatment group) sacrificed on Day 7 post-infection. Images are at 400× magnification. (B) Histological scoring for PR8-infected mice without or with Eritoran treatment ± s.e.m. (C) Pulse oximetry data collected on Day 6 post-infection ± s.e.m. (p < 0.001, comparing PR8 only with Mock-infected or PR8 + E5564; 4–6 mice/treatment group). (D) Eritoran treatment improves lung pathology of H3N2 infection of cotton rats. (E) Histological scoring for H3N2-infected cotton rats with or without eritoran treatment (n = 5 rats/treatment; data shown is means ± s.e.m.).
To determine whether the therapeutic effect of Eritoran extends to other animal models of human influenza infection, we performed experiments in cotton rats (Sigmodon hispidus)14,15. A/Wuhan/359/95 (H3N2), a human non-adapted strain of influenza, replicates in lungs of cotton rats on day 1 and produces peak lung pathology on day 4 post-infection (Fig. 2D, panel b; and Fig. 2E, H3N2/mock). Animals treated with Eritoran post-H3N2 challenge showed significant reduction in lung pathology on day 4 when compared to animals treated with vehicle (Fig. 2D, panel c, and Fig. 2E, H3N2/E5564).
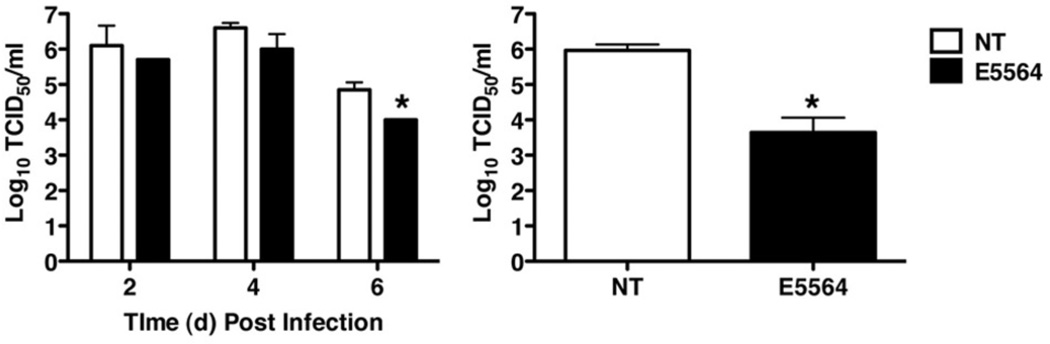
Fig. 3 (left panel) shows that by Day 6 post-infection, Eritoran treatment resulted in a statistically significant decrease in lung viral titers that was further decreased by Day 7 (Fig. 3, right panel) and Day 8 (data not shown). This was not a direct effect of Eritoran on virus replication (Supplementary Table I). By Day 14, all surviving mice had completely cleared the virus, regardless of treatment. Since the effects of influenza infection are systemic16, levels of liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were measured in sera. While PR8 infection resulted in significant increases in ALT and AST levels, these were significantly lower in Eritoran-treated mice 6 days post-infection (Supplementary Fig. 2).
Figure 3.
Treatment with Eritoran reduces lung viral titers. Mice were infected with PR8 and then either left untreated (NT) or eritoran (E5564)-treated as described in Fig. 1A and were sacrificed on Days 2, 4, 6 (A) and 7 (B) post-infection. (A, left panel). Results represent the combined results of 2 separate experiments (5 mice/treatment group/experiment) *, p < 0.05. (A, right panel). Day 7 post-infection (7 mice/treatment group); *, p < 0.001.
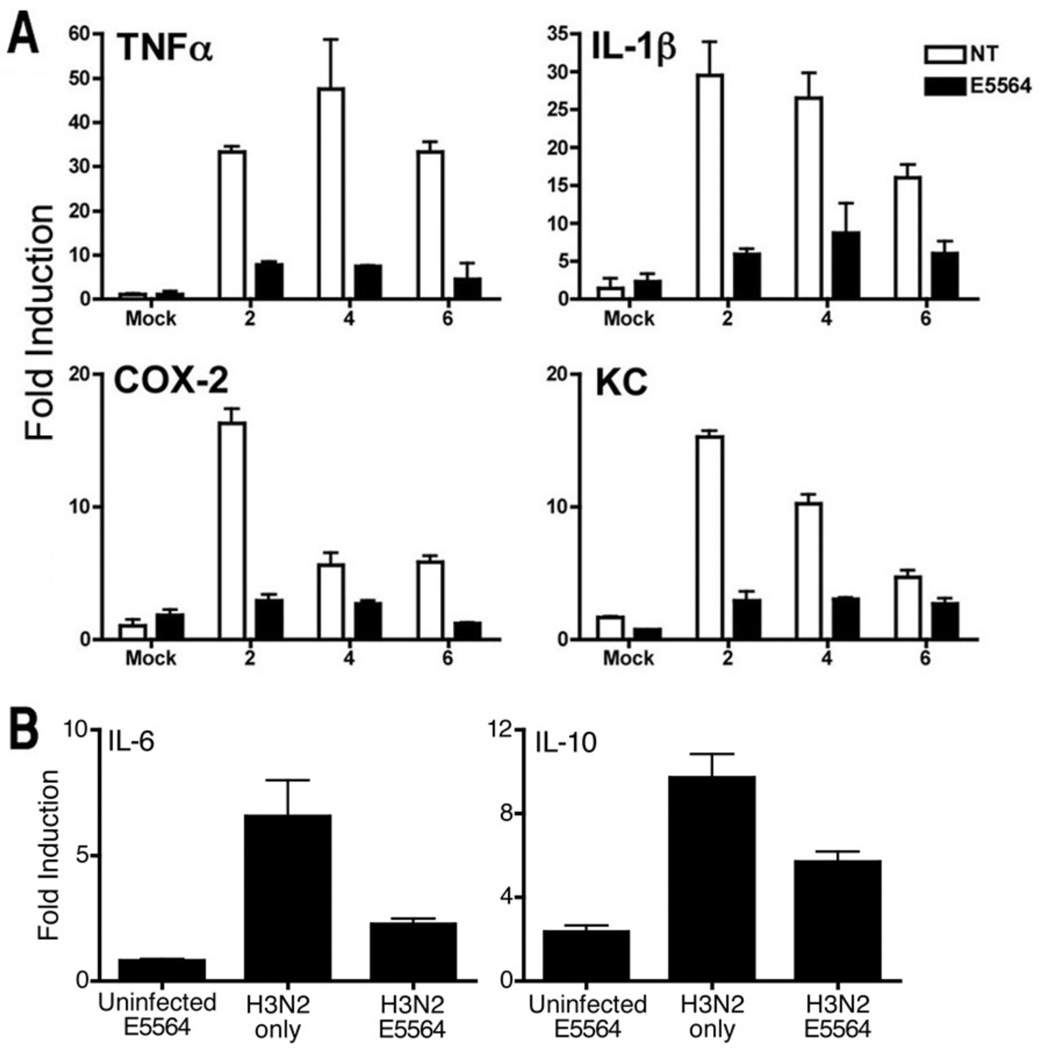
Influenza infection potently induces expression of both pro- and anti-inflammatory genes in vivo that contribute to the inflammatory response1,17. To determine if Eritoran also mitigates PR8-induced gene expression, groups of mice were infected on Day 0 and treated with Eritoran starting on Day 2 and sacrificed on Day 2 (3 h post-Eritoran treatment) and on Days 4 and 6. Total RNA was extracted from lung homogenates and gene expression measured by qRT-PCR. Eritoran-treated mice exhibited significantly blunted pro- and anti-inflammatory gene expression at each time point (Fig. 4A; Supplementary Fig. 3A; p < 0.001), as early as 3 h post-treatment on Day 2. Supplementary Fig. 3B shows that influenza induced types I, II, and III IFNs; however, only IFN-β and IFN-γ mRNA expression were blunted by Eritoran treatment. In addition, cotton rats infected with the non-adapted human Wuhan H3N2 strain and treated with Eritoran showed decreased lung expression of IL-6 and IL-10 (Fig. 4B).
Figure 4.
Eritoran treatment suppresses influenza-induced cytokine gene expression. Mice were treated as described in Fig. 1A and euthanized on Days 2 (3 h post-treatment), 4, and 6 post-infection (4 mice/treatment group/experiment; data presented are means ± s.e.m. from 2 separate experiments; p< 0.01 at each time point). Lungs were processed for total RNA and subjected to qRT-PCR for detection of specific gene expression.
IFN-β−/− mice are highly susceptible to PR8 and fail to be protected by the potent IFN-β inducer, 5,6-dimethylxanthenone-4-acetic acid18. In addition, endogenous IFN-β is required for normal basal and LPS-inducible expression of many proinflammatory cytokines in macrophages19. PR8-infected IFN-β−/− mice failed to be protected by Eritoran (Supplementary Fig. 4). This indicates that while both proinflammatory and IFN-β gene expression are blunted in PR8-infected, Eritoran-treated WT mice (Fig. 4A,B), the elaboration of some IFN-β is required for antiviral protection in the absence of significant priming.
Most potent activation of TLR4 by LPS depends on LPS binding protein (LBP)-catalyzed extraction and transfer of individual LPS molecules from aggregated LPS to CD14 and then from CD14 to MD2, followed by engagement and dimerization of TLR4. Crystallographic analysis revealed that Eritoran, like LPS monomer, binds in the deep hydrophobic pocket of MD2 and engages TLR4; however, Eritoran fails to induce TLR4 dimerization and activation, thus acting as a TLR4 antagonist20.
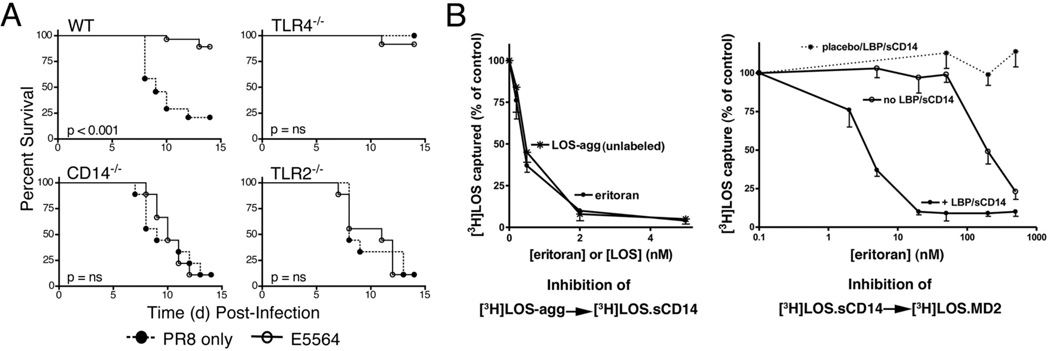
We confirmed the finding of Nhu et al.2 that the PR8-induced lethality in mice was TLR4-dependent (Fig. 5A), but also found, surprisingly, that influenza mortality was not CD14-dependent as indicated by the similar mortality of PR8 infection in WT and CD14−/− mice vs. the resistance of TLR4−/− mice (Fig. 5A). These findings suggest that TLR4-dependent influenza mortality is mediated by influenza-induced TLR4 agonists that, unlike LPS, do not depend on CD14 for engagement and activation of TLR4/MD2. In contrast, the protection induced in WT mice when Eritoran treatment is started on Day 2 post-infection is absent in CD14−/− mice, indicating that the protective effect of Eritoran in this influenza infection model is CD14-dependent (Fig. 5A).
Figure 5.
Molecular requirements of Eritoran-induced protection. (A) WT, TLR4−/−, CD14−/−, TLR2−/− mice were either untreated (closed circles), or treated with E5564 (open circles) or 2 days post-infection, for 5 successive days. WT data were combined from 5 separate experiments (5–6 mice/treatment/experiment), TLR4−/− data from 3 separate experiments (5–6 mice/treatment/experiment), CD14−/− mice (2 separate experiments; 5 mice/treatment group/experiment, and TLR2−/− mice (2 separate experiments; 4–5 mice/treatment group/experiment). WT: untreated vs. E5564 treatment (p < 0.0001); TLR4−/−: untreated vs. E5564 treatment (p = ns); CD14−/−: untreated vs. E5564 treatment (p = ns); TLR2−/−: untreated vs. E5564 treatment (p = ns). (B) Dose-dependent Eritoran inhibition of the transfer and binding of monomeric [3H]LOS from aggregated [3H]LOS to sCD14 and from [3H]LOS.sCD14 to MD2. Samples containing [3H]LOS aggregates (0.2 nM), His6-sCD14 (~0.5 nM), and increasing concentrations as indicated of Eritoran or unlabeled LOS (left panel) or 2 nM [3H]LOS.sCD14, ca. 2 nM His6-MD2, and increasing concentrations of Eritoran (or placebo) ± LBP (50 pM) and sCD14 (2 nM) (right panel) were incubated for 30 min at 37° C, followed by addition and incubation with NiFF Sepharose beads to capture His-tagged proteins. Formation of complexes of [3H]LOS with His6-sCD14 (left) or MD2 (right) was assayed by measuring co-capture of [3H]LOS by NiFF Sepharose as previously described25. Data are expressed as percent of co-capture of [3H]LOS observed in the absence of added Eritoran. Results shown represent the mean ± s.e.m. of 3 separate experiments with duplicate samples for each dose.
One possible explanation for the CD14-dependence of Eritoran-mediated protection is that engagement by Eritoran of MD2 and antagonism of TLR4 depends on CD14. To test this possibility, we assayed in vitro the capacity of Eritoran to bind CD14 and MD2 by measuring inhibition by Eritoran of LBP-dependent transfer of tritiated lipooligosaccharide (3H-LOS; the LPS of Neisseria) to CD14 (Fig. 5B, left panel), as well as the transfer of 3H-LOS from CD14 to MD2 (Fig. 5B, right panel). Since the inhibitory effect of Eritoran on the transfer of 3H-LOS to MD2 is 100x more potent when LBP and sCD14 are present, this strongly suggests that interaction of Eritoran with MD2 occurs most efficiently following LBP-dependent interaction of Eritoran with CD14.
While MD1, a homolog of MD2 that also binds lipid A21, was considered as an alternative target for Eritoran, this possibility was dismissed since MD1 failed to substitute for MD2 to enable TLR4 signaling (Supplementary Fig. 5).
Diacylated lipids can act as TLR2 agonists. Hence, if oxidized host phospholipids (e.g., OxPAPC) play a role in TLR4-dependent influenza, it is conceivable these diacylated lipids could also engage TLR2-containing receptor complexes and that influenza-induced mortality might also be TLR2-dependent. However, TLR2−/− mice showed similar susceptibility to PR8 infection as WT mice (Fig. 5A), arguing against an important role for TLR2 in influenza-induced mortality. Remarkably, however, protection induced by Eritoran treatment beginning at Day 2 post-infection was absent in TLR2−/− mice, suggesting a novel role for TLR2 in Eritoran action.
If PR8-induced ALI and mortality we have observed is due substantially to influenza-induced oxidized host phospholipids (OxPL), as proposed by Imai et al.1, these compounds should show preferential activation of TLR4 (vs. TLR2) and be inhibited by Eritoran. Commercially obtained OxPAPC comparably activated IL-6 gene expression in WT and TLR2−/− peritoneal macrophages, but was inhibited by ~84% in TLR4−/− macrophages when compared to the WT response. Cellular activation by OxPAPC was also significantly inhibited by Eritoran, including the low level of TLR4-independent production of IL-6 mRNA observed in TLR4−/− macrophages (Supplementary Fig. 6). This indicates that the response to OxPAPC is predominantly TLR4-dependent and Eritoran-sensitive.
To assess the effect of Eritoran on production of oxidized phospholipids during infection, matrix-assisted laser desorption ionization-imaging mass spectrometry (MALDI-IMS) was used to identify alterations in the lipid composition of mouse lungs after PR8 infection, without or with Eritoran treatment. Predicted oxidation products (m/z 650, 830) of 1-palmitoyl-2-arachidonayl-sn-glycero-3-phosphocholine (PAPC), or other polyunsaturated phosphatidylcholines (PCs), as described by Imai et al.1 were detected in greater abundance in PR8-infected vs. mock-infected or infected and Eritoran-treated lungs (Supplementary Fig. 7). These results were confirmed by electrospray ionization-mass spectrometry (data not shown). Together, these results indicate that oxidized phosphatidylcholines are present in influenza-infected lungs and show that treatment with Eritoran reduces the relative abundance of these characteristic ions. Thus, Eritoran treatment of influenza-infected mice not only blocks the cytokine storm exacerbated by influenza-induced endogenous TLR4 agonists, but also inhibits the production and accumulation of certain oxidized phospholipids in infected lungs, including OxPAPC and possibly others.
In summary, our findings provide further support for a prominent role of influenza-induced oxidized host phospholipids in TLR4-dependent ALI and mortality and demonstrate a novel therapeutic potential of Eritoran toward this and, potentially, other respiratory infections. In the hypothetical model shown in Supplementary Figure 8, we would predict, based on our data, that Eritoran blocks oxidized phospholipid-induced TLR4 signaling, thereby mitigating the cytokine storm and subsequent potentiation of ROS-induced oxidation of phospholipids. Our failure to detect commensal bacteria or LPS in lung homogenates from PR8-infected mice suggests that the disease manifestations are not the result of secondary bacterial infection (data not shown). The TLR2- and CD14-independence of influenza mortality is consistent with the selective agonist properties of at least certain OxPLs that we have observed and suggests that these compounds, unlike most LPS species, can engage MD2/TLR4 in the absence of CD14, perhaps by interacting with an alternative lipid acceptor/donor such as albumin22,23. In contrast, the CD14- and TLR2-dependence of the therapeutic action of Eritoran may reflect both CD14-dependent engagement by Eritoran of MD2/TLR4 by Eritoran, precluding action of endogenous TLR4 agonists generated after initiation of infection and early tissue alterations, as well as, as yet, uncharacterized interactions of Eritoran with TLR2-containing receptors. This possibility is supported by the observation that mycobacterial lipoarabinomannan requires CD14 for TLR2 activation24. That influenza infection modulates TLR2 expression in many cell types25,26 and synthetic TLR2 ligands provide prophylaxis against lethal influenza infection27 strengthen the notion that TLR2-containing receptors may provide another target for Eritoran. These findings underscore the novel therapeutic potential of Eritoran, either used as a monotherapy or, more likely, as an adjunct to antiviral agents. The potential utility of Eritoran is further enhanced by its well-documented safety profile28.
Many drugs targeting endotoxin or the endotoxin-induced cytokine storm were originally developed for use in sepsis, yet none have emerged as effective therapeutics for sepsis. Moreover, while many of these drugs failed to protect therapeutically in animal models of endotoxicity or in clinical trials in septic humans, they were found to be of great benefit in other, more localized models of inflammation (e.g., rheumatoid arthritis, IBD, etc.). The data provided in this report suggest that Eritoran might follow a similar development pathway. Eritoran demonstrated remarkable activity in vitro and in vivo4,28 in endotoxin challenge studies when administered prophylactically or very early in the “sepsis cascade.” A non-statistically significant improvement in mortality was also observed in a small Phase 2 severe sepsis study29. The Phase 2 study design and statistical power calculations were expanded to perform a single dose, placebo-controlled Phase 3 severe sepsis study (the ACCESS study) in which 1,984 patients were treated in a 2:1 ratio of drug:placebo. Results of this study demonstrated that newly-employed treatment regimens including aggressive fluid resuscitation and early goal-directed therapy dramatically reduced mortality in the placebo group; however, further benefit to septic patients was not observed with Eritoran treatment30. Thus, it is of significance that in the study described herein, Eritoran prevented mortality when administered up to 6 days after influenza infection of mice. This more practical timing of treatment may enable effective clinical treatment of influenza and, perhaps, other infectious agents.
Full Methods
Reagents
Eritoran (E5564) and its corresponding placebo (vehicle only) were kindly provided by Eisai Inc. (Japan). Eritoran was prepared at 2.33 mg/ml in sterile, endotoxin-free water and diluted for injection in sodium bicarbonate-buffered 5% dextrose water. Oxidized 1-palmitoyl-2-arachidonayl-sn-glycero-3-phosphocholine (OxPAPC) was purchased from Hycult biotech (Plymouth Meeting, PA). Escherichia coli K235 LPS was prepared as previously described1. Pam3Cys was purchased from EMC Microcollections (Germany).
Mice and cotton rats
Six to 8-week old, WT C57BL/6J, TLR2−/−, and CD14−/− mice were purchased (The Jackson Laboratory, Bar Harbor, ME). TLR4−/− mice (provided by Shizuo Akira, Osaka, Japan) on a C57BL/6 background, were bred in UMB’s accredited facility. Inbred young adult (4–8 weeks old) cotton rats (Sigmodon hispidus) were bred at Sigmovir Biosystems, Inc. (Rockville, MD). All animal experiments were conducted with institutional IACUC approval from University of Maryland, Baltimore and Sigmovir Biosystems, Inc.
Virus
Mouse-adapted H1N1 influenza A/PR/8/34 virus (“PR8”) (ATCC, Manassas, VA) was grown in the allantoic fluid of 10-day old embryonated chicken eggs as described2 and was kindly provided by Dr. Donna Farber (Columbia University). Non-adapted human influenza virus strain A/Wuhan/359/95 (H3N2), and A/Brisbane/59/07 (H1N1) was obtained and grown as previous described3,4. Non-adapted human influenza strain A/California/07/2009 strain (human pandemic H1N1) was kindly provided by Ted Ross (U. Pittsburgh).
Virus challenge and treatments
C57BL/6J WT, TLR4−/−, TLR2−/−, and CD14−/− mice were infected with mouse-adapted influenza virus, strain A/PR/8/34 (PR8; ~7500 TCID50, i.n., 25 µl/nares) or the non-adapted human pandemic H1N1 strain, A/California/07/2009 (~107 TCID50, i.n.). This dose was found in preliminary experiments to kill ~90% (PR8) or ~75% (human H1N1) of infected mice. Two days after infection, mice received either placebo or E5564 (Eritoran; 200 µg/mouse in 100 µl, i.v.) daily (Day 2 to Day 6). In some experiments, some groups of mice were treated with eritoran starting at day 4 or day 6 post-infection and treated for 5 or 3 consecutive days, respectively. In some experiments, some mice were infected with ~10,000 or 20,000 TCID50 PR8. Mice were monitored daily for survival, weight loss, and clinical signs of illness (e.g., lethargy, piloerection, ruffled fur, hunched posture, rapid shallow breathing, audible crackling) for 14 days. A clinical score ranging from 0 (no symptoms) – 5 (moribund) was ascribed to each mouse daily5. In some experiments, mice were euthanized at the indicated times post-infection to harvest serum for liver enzyme levels or lungs for analysis of gene expression, lung pathology, or viral titers.
Cotton rats were infected with non-adapted human influenza strain A/Wuhan/359/95 (H3N2; ~ 107 TCID50 or pfu, i.n., 50 µl/nares). Two h post-infection, animals received E5564 (200 µg/rat in volume, retro-orbital) daily for 5 days (days 0–4). Animals were sacrificed at day 4 post-infection for lung pathology and total RNA to measure gene expression by real time PCR.
Histopathology
Lungs were inflated and perfused and fixed with 4% PFA. Fixed sections (8 µm) of paraffin-embedded lungs were stained with hematoxylin and eosin (H&E). Slides were randomized, read blindly, and examined for tissue damage, necrosis, apoptosis, and inflammatory cellular infiltration.
Pulse Oximetry Measurements
At 6 days post-infection, percent arterial oxygen saturation was measured on individual mice that were lightly anesthetized with nebutol. An extra small collar sensor and a Small Animal Oximetry Restraint Device (Starr-Gate, Oakmont, PA) was used per the manufacturer’s instructions.
Viral titration
Virus titers were obtained from supernatants of lung homogenates of PR8-infected mice that were either left untreated (NT) or treated with Eritoran and harvested on days 2, 4, 6, and 7 post-infection and expressed at TCID50/ml as described previously6.
Quantitative real-time PCR (qRT-PCR)
Total RNA isolation and qRT-PCR were performed as previously described7. Levels of mRNA for specific genes are reported as relative gene expression normalized to mock-infected lungs.
Liver enzyme levels
Serum was collected on day 7 from C57BL/6J WT mice that were either mock-infected with saline or PR8-infected and were either left untreated or treated with Eritoran (E5564) starting on day 2 post-infection. ALT and AST levels were measured using a Dimension Vista System Flex Reagent cartridge (Siemens Healthcare Diagnostics, Ltd.).
Macrophage cell cultures and treatment
Thioglycollate-elicited peritoneal macrophages from WT, TLR4−/−, and TLR2−/− mice were enriched as described8 after plating in 12-well (2x106 cells/well) tissue culture plates. Macrophages were pre-treated with E5564 (10 ng/ml) for 1 h and then stimulated with LPS (10 ng/ml), P3C (300 ng/ml), or OxPAPC (20 µg/ml) for 8 h.
Matrix-Assisted Laser Desorption Ionization-Imaging Mass Spectrometry (MALDI-IMS)
Mouse lung tissue was snap frozen by floating in an aluminum foil raft on liquid nitrogen. Tissues were cryosectioned (unfixed and unembedded) in 12 µm sections, each section was transferred to a conductive MALDI-IMS glass slide, heat-fixed until visibly dry (approximately 30–60 s), and desiccated for at least 1 hour. A 12.5 mg/mL solution of norharman MALDI matrix solvated in chloroform:methanol:water (1:2:0.8, v:v:v) was spray coated onto slides using the Bruker ImagePrep device. MS data was collected in positive mode (detection range: m/z 400–900), raster width 150 µm, 500 shots per raster, on a Bruker Daltonics AutoFlex Speed Matrix-Assisted Laser Desorption Ionization Time-of-Flight/Time-of-Flight Mass Spectrometer (MALDI-TOF/TOF MS; source) using flexControl software. Subsequently, the data was analyzed using flexImaging software. After IMS analysis, the matrix was stripped in 70% methanol and tissue sections were restained by H&E for gross histological reference using standard protocols. All MALDI-IMS specific materials, equipment, instruments, and software were obtained from Bruker Daltonics (Billerica, MA). Unless otherwise specified, all reagents were purchased from Sigma-Aldrich (St. Louis, MO).
Statistics
Statistical differences between two groups were determined using an unpaired, two-tailed Student’s t test with significance set at p <0.05. For comparisons between ≥3 groups, analysis was done by one-way ANOVA followed by a Tukey’s multiple comparison test with significance determined at p < 0.05. For survival studies, a Log-Rank (Mantel-Cox) test was used.
Supplementary Material
Acknowledgments
This work was supported by NIH grants AI057575 (J.C.G.B.), AI018797 (S.N.V.), AI059372 (J.W.), and NCRR K12-RR-023250 (W.H.C.), VA Merit Award 1I01BX0000949-01A1 (T.L.G.), and Cystic Fibrosis Foundation RDP Center Grant (C.L.K.).
Footnotes
Supplementary Information is provided with the online version of the paper at www.nature.com/nature.
Author Contributions
K.A.S. and S.N.V. carried out the study design, with advice from J.C.G.B., D.P.R., J.W., R.K.E. and C.L.K. K.A.S., W.L., J.C.G.B., L.M.P., A.J.S., T.L.G., J.M., and P.M. performed experiments. M.L. performed histological analysis. F.G., W.H.C., and D.P.R. provided crucial reagents and advice for study. K.A.S. and S.N.V. prepared the manuscript, with input and approval of all other co-authors.
With the exception of F.G., none of the authors have a competing interest. F.G. is an employee of Eisai Inc.
References
- 1.Imai Y, et al. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133:235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nhu QM, et al. Novel signaling interactions between proteinase-activated receptor 2 and Toll-like receptors in vitro and in vivo. Mucosal Immunol. 2010;3:29–39. doi: 10.1038/mi.2009.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalil AC, et al. Influence of severity of illness on the effects of eritoran tetrasodium (E5564) and on other therapies for severe sepsis. Shock. 2011;36:327–331. doi: 10.1097/SHK.0b013e318227980e. [DOI] [PubMed] [Google Scholar]
- 4.Mullarkey M, et al. Inhibition of endotoxin response by E5564, a novel Toll-like receptor 4-directed endotoxin antagonist. J Pharmacol Exp Ther. 2003;304:1093–1102. doi: 10.1124/jpet.102.044487. [DOI] [PubMed] [Google Scholar]
- 5.Thompson WW, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 6.Thompson WW, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 7.Reid AH, Taubenberger JK, Fanning TG. The 1918 Spanish influenza: integrating history and biology. Microbes Infect. 2001;3:81–87. doi: 10.1016/s1286-4579(00)01351-4. [DOI] [PubMed] [Google Scholar]
- 8.Taubenberger JK, Reid AH, Janczewski TA, Fanning TG. Integrating historical, clinical and molecular genetic data in order to explain the origin and virulence of the 1918 Spanish influenza virus. Philos Trans R Soc Lond B Biol Sci. 2001;356:1829–1839. doi: 10.1098/rstb.2001.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurt AC, Holien JK, Parker M, Kelso A, Barr IG. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J Virol. 2009;83:10366–10373. doi: 10.1128/JVI.01200-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKimm-Breschkin JL, et al. Mutations in a conserved residue in the influenza virus neuraminidase active site decreases sensitivity to Neu5Ac2en-derived inhibitors. J Virol. 1998;72:2456–2462. doi: 10.1128/jvi.72.3.2456-2462.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishin VP, Hayden FG, Gubareva LV. Susceptibilities of antiviral-resistant influenza viruses to novel neuraminidase inhibitors. Antimicrob Agents Chemother. 2005;49:4515–4520. doi: 10.1128/AAC.49.11.4515-4520.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldblum SE, Ding X, Brann TW, Campbell-Washington J. Bacterial lipopolysaccharide induces actin reorganization, intercellular gap formation, and endothelial barrier dysfunction in pulmonary vascular endothelial cells: concurrent F-actin depolymerization and new actin synthesis. J Cell Physiol. 1993;157:13–23. doi: 10.1002/jcp.1041570103. [DOI] [PubMed] [Google Scholar]
- 13.Verhoeven D, Teijaro JT, Farber DL. Pulse-oximetry accurately predicts lung pathology and the immune response during influenza infection. Virology. 2009;390:151–156. doi: 10.1016/j.virol.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blanco JCG, et al. Receptor characterization and suceptibility of cotton rats to avian and 2009 pandemic influenza virus strains. J. Virol. 2013;87 doi: 10.1128/JVI.00638-12. 4 PMID 2319287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ottolini MG, et al. The cotton rat provides a useful small-animal model for the study of influenza virus pathogenesis. J Gen Virol. 2005;86:2823–2830. doi: 10.1099/vir.0.81145-0. [DOI] [PubMed] [Google Scholar]
- 16.Polakos NK, et al. Kupffer cell-dependent hepatitis occurs during influenza infection. Am J Path. 2006;168:1169–1178. doi: 10.2353/ajpath.2006.050875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taubenberger JK, Morens DM. The pathology of influenza virus infections. Annu Rev Pathol. 2008;3:499–522. doi: 10.1146/annurev.pathmechdis.3.121806.154316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shirey KA, et al. The anti-tumor agent, 5,6-dimethylxanthenone-4-acetic acid (DMXAA), induces IFN-beta-mediated antiviral activity in vitro and in vivo. J Leukoc Biol. 2011;89:351–357. doi: 10.1189/jlb.0410216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas KE, Galligan CL, Newman RD, Fish EN, Vogel SN. Contribution of interferon-beta to the murine macrophage response to the toll-like receptor 4 agonist, lipopolysaccharide. J Biol Chem. 2006;13:31119–31130. doi: 10.1074/jbc.M604958200. [DOI] [PubMed] [Google Scholar]
- 20.Kim HM, et al. Crystal structure of the TLR4-MD-2 complex with bound endotoxin antagonist Eritoran. Cell. 2007;130:906–917. doi: 10.1016/j.cell.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Yoon SI, Hong M, Han GW, Wilson IA. Crystal structure of soluble MD-1 and its interaction with lipid Iva. Proc Natl Acad Sci USA. 2010;15:10990–10995. doi: 10.1073/pnas.1004153107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Esparza GA, Teghanemt A, Zhang D, Gioannini TL, Weiss JP. Endotoxin-albumin complexes transfer endotoxin monomers to MD-2 resulting in activation of TLR4. Innate Immun. 2012;18:478–491. doi: 10.1177/1753425911422723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gioannini TL, Zhang D, Teghanemt A, Weiss JP. An essential role for albumin in the interaction of endotoxin with lipopolysaccharide-binding protein and sCD14 and resultant cell activation. J Biol Chem. 2002;277:47818–47825. doi: 10.1074/jbc.M206404200. [DOI] [PubMed] [Google Scholar]
- 24.Means TK, et al. The CD14 ligands lipoarabinomannan and lipopolysaccharide differ in their requirement for Toll-like receptors. J Immunol. 1999;163:6748–6755. [PubMed] [Google Scholar]
- 25.Pauligk C, Nain M, Reiling N, Gemsa D, Kaufmann A. CD14 is required for influenza A virus-induced cytokine and chemokine production. Immunobiology. 2004;209:3–10. doi: 10.1016/j.imbio.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Lee RM, White MR, Hartshorn KL. Influenza a viruses upregulate neutrophil toll-like receptor 2 expression and function. Scand J Immunol. 2006;63:81–89. doi: 10.1111/j.1365-3083.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- 27.Shinya K, et al. Toll-like receptor pre-stimulation protects mice against lethal infection with high pathogenic influenza viruses. Virology Journal. 2011;8:97–101. doi: 10.1186/1743-422X-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong YN, et al. Safety, pharmacokinetics, and pharmacodynamics of E5564, a lipid A antagonist, during an ascending single-dose clinical study. J Clin Pharmacol. 2003;43:735–742. [PubMed] [Google Scholar]
- 29.Tidswell M, et al. Phase 2 trial of eritoran tetrasodium (E5564), a toll-like receptor 4 antagonist, in patients with severe sepsis. Crit Care Med. 2010;38:72–83. doi: 10.1097/CCM.0b013e3181b07b78. [DOI] [PubMed] [Google Scholar]
- 30.Cohen J, Opal S, Calandra T. Sepsis studies need new direction. Lancet Infect Dis. 2012;12:503–505. doi: 10.1016/S1473-3099(12)70136-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.