Abstract
Context
Although the nation’s local health departments (LHDs) share a common mission, variability in administrative structures is a barrier to identifying common, optimal management strategies. There is a gap in understanding what unifying features LHDs share as organizations that could be leveraged systematically for achieving high performance.
Objective
To explore sources of commonality and variability in a range of LHDs by comparing intraorganizational networks.
Intervention
We used organizational network analysis to document relationships between employees, tasks, knowledge, and resources within LHDs, which may exist regardless of formal administrative structure.
Setting
A national sample of 11 LHDs from seven states that differed in size, geographic location, and governance.
Participants
Relational network data were collected via an on-line survey of all employees in 11 LHDs. A total of 1 062 out of 1 239 employees responded (84% response rate).
Outcome Measures
Network measurements were compared using coefficient of variation. Measurements were correlated with scores from the National Public Health Performance Assessment and with LHD demographics. Rankings of tasks, knowledge, and resources were correlated across pairs of LHDs.
Results
We found that 11 LHDs exhibited compound organizational structures in which centralized hierarchies were coupled with distributed networks at the point of service. Local health departments were distinguished from random networks by a pattern of high centralization and clustering. Network measurements were positively associated with performance for 3 of 10 essential services (r > 0.65). Patterns in the measurements suggest how LHDs adapt to the population served.
Conclusions
Shared network patterns across LHDs suggest where common organizational management strategies are feasible. This evidence supports national efforts to promote uniform standards for service delivery to diverse populations.
Keywords: complex adaptive systems, management, network analysis, organizations, performance, public health
Despite the fact that local health departments (LHDs) have consistent missions and perform essentially similar work,1 efforts to standardize, measure, and compare performance have been difficult.2 The organizational structures of LHDs have evolved nonuni-formly as entities of state and/or local government.3 Administrative and task-oriented strategies derived in any one LHD are not perceived to be applicable across all jurisdictions. A well-recognized and long-term need for consistent performance criteria is being addressed currently through a voluntary national program to accredit LHDs, and uniform standards are emerging.4 Much of the focus of standards development is on capacity and infrastructure for service delivery5–9 There is little empirical evaluation of the characteristics LHDs may share as organizations, which could be leveraged for standardization.10 An important resource for LHD performance improvement is organizational science, a mature field with well-developed theory and analytic techniques.
The aim of the study reported here was to identify common organizational features in a range of LHDs that may be useful to inform management and improve performance. To do this, we used organizational network analysis to empirically model 11 LHDs of differing size and governance to see whether common organizational network characteristics occur. We investigated whether LHDs share a similar pattern of network measurements; whether LHD networks exhibit a distinctive pattern; and whether there are similarities in essential work across LHDs. We also investigated the relationship between LHD networks and system performance.
Network Analysis
A network is a set of nodes and links that connect the nodes. Nodes can represent people such as a public health employee or things such as a public health task. Links indicate a tie or relationship between them, such as daily communication, or assignment to a task. Network analysis uses mathematical equations to calculate measurements that describe the relationships among the nodes (eg, the number of links shared between nodes). Relationships between nodes can also be graphically displayed in network visualizations.
Organizational network analysis (ONA) is an extension of social network analysis that is used to study organizational dynamics. Unlike traditional organizational evaluation methods that are concerned with value or outcome, ONA draws conclusions about an organizational behavior by examining the relationships among employees and their work and interpreting these with social and management theory.
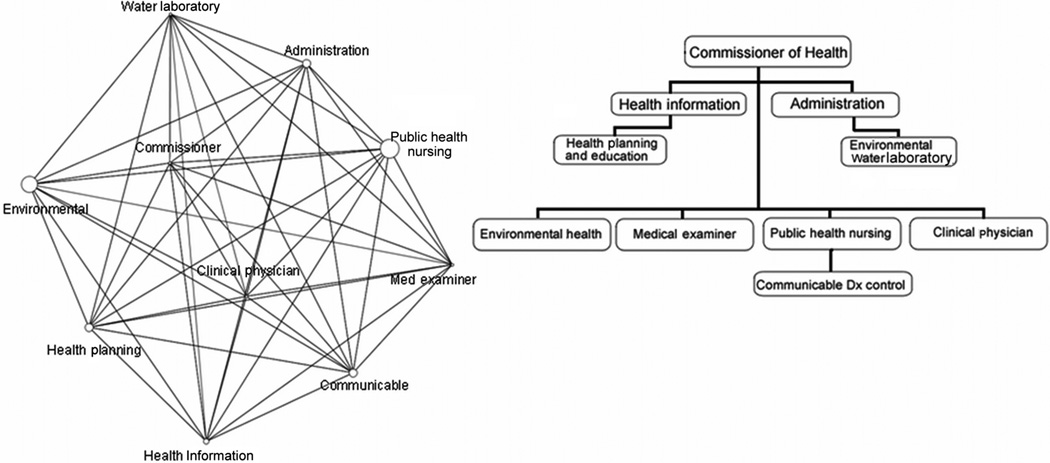
Actual LHDs are complex adaptive systems in which public health work takes place as a result of nonlinear interactions among many organizational elements. “Org” charts and process maps fail to capture these interactions. The result is that important aspects of public health work may not be fully managed. The measurements and visualizations produced through ONA reveal patterns in these interactions, which gives managers insights (often unexpected) into how the relationships between people and work are structured in the LHD and how the work actually gets done. For example, Figure 1 illustrates a health department network at the divisional level on the left, compared with a traditional organizational chart on the right. The size of the nodes in the network diagram corresponds to the number of staff in the division. The nonlinear pattern of links between divisions in the network presents a striking contrast to the directed hierarchy of the organizational chart. The insights produced by ONA are empirical evidence that manager can use to support their decision making to improve performance.
FIGURE 1. A Health Department Network at the Divisional Level on the Left Compared With a Traditional Organizational Charta.
a The size of the nodes in the network diagram is related to number of staff in the division. The nonlinear pattern of links between divisions in the network presents a striking contrast to the directed hierarchy of the organizational chart. From Merrill et al.19
Methods
In this multiagency network analysis, we move beyond a social network approach that examines relationships among people (employees) to examine relationships between employees and elements of their work within the LHD.11 We operationalized an LHD as a set of networks representing employee-to-employee relationships as well as the relationships between employees and the tasks to which they are assigned, the knowledge they possess, and the resources to which they have access.11–14
Sample
A stratified purposive sample was drawn from among LHDs that participated in the National Public Health Performance Standards (NPHPS) program. The NPHPS program, which is coordinated by the Centers for Disease Control and Prevention, measures performance of the overall public health system (ie, the combined activities of all public, private, and voluntary entities in a jurisdiction that may contribute to the public health mission). The NPHPS Local Assessment Instrument, Version 1 (NPHPS V1), is based on 10 Essential Services of Public Health and gives respondents a score for performance on each of these services.15,16
The sample LHDs werer ecruited on the basis of completion of the NPHPS V1 within the past 3 years. Local health departments containing between 30 and 200 employees were targeted to reduce survey response burden and optimize network visualizations. Local health departments of this size encompass about 32 percent of LHDs nationally.1 Eligible sites were identified by reviewing the 2005 National Profile of Local Health Departments1 and the NPHPS V1 data file.
Local health departments were selected to represent four types of governance: centralized, which derive authority and command structure from the state; centralized-hybrid, which derive authority from the state but their command structure is autonomous; home rule, which derive authority from local boards of health and have an autonomous command structure; and independent, which derive authority from the county and have an autonomous command structure. Fourteen LHDs met the study criteria for geographical distribution, population served, and dispersion of scores on NPHPS V1, and these were invited to participate. Eleven LHDs within seven states volunteered. Reasons three LHDs gave for not participating were lack of interest or capacity to participate in research. Descriptive data on the sample sites are given in Table 2.
TABLE 2.
Demographics, governance, aggregate performance score, and network measurements of the 11 LHD samplesa
| LHD | State | Goveenance | Size | Population served |
Income per capita |
Population density sq mile |
NPHPS mean Score |
Density b |
Centralization b |
Complexity b |
Clustering Coefficient b |
% Divisions tending toward silo |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Strongest | All | Strongest | All | Strongest | All | Strongest | All | Strongest | ||||||||
| 1 | AR | Centralized | 35 | 35 253 | $16175 | 57.4 | 92.3 | 0.44 | 0.29 | 0.49 | 0.18 | 0.36 | 0.34 | 0.78 | 0.71 | 25 | 25 |
| 2 | AR | Centralized | 43 | 92141 | $18 631 | 130.1 | 66.2 | 0.53 | 0.21 | 0.38 | 0.34 | 0.40 | 0.33 | 0.68 | 0.57 | 0 | 33 |
| 3 | FL | Centralized hybrid |
121 | 145 207 | $18 321 | 273.6 | 82.1 | 0.32 | 0.13 | 0.53 | 0.42 | 0.37 | 0.28 | 0.53 | 0.48 | 17 | 33 |
| 4 | IL | Independent | 115 | 139 849 | $28 674 | 202.2 | 67.7 | 0.23 | 0.11 | 0.52 | 0.29 | 0.30 | 0.24 | 0.54 | 0.50 | 0 | 38 |
| 5 | FL | Centralized hybrid |
187 | 226 216 | $18 790 | 336.9 | 52.0 | 0.28 | 0.09 | 0.51 | 0.23 | 0.35 | 0.25 | 0.51 | 0.42 | 0 | 22 |
| 6 | NJ | Home rule | 139 | 423 394 | $26 339 | 526 | 61.4 | 0.15 | 0.07 | 0.48 | 0.12 | 0.25 | 0.21 | 0.57 | 0.60 | 44 | 67 |
| 7 | FL | Centralized hybrid |
115 | 179 669 | $19 708 | 180.2 | 66.8 | 0.31 | 0.13 | 0.52 | 0.53 | 0.36 | 0.28 | 0.57 | 0.45 | 0 | 14 |
| 8 | AZ | Independent | 144 | 122 754 | $40 040 | 6.2 | 54.5 | 0.17 | 0.07 | 0.56 | 0.16 | 0.29 | 0.24 | 0.51 | 0.51 | 14 | 57 |
| 9 | MT | Independent | 107 | 95 000 | $17 808 | 36.9 | 49.0 | 0.21 | 0.09 | 0.46 | 0.15 | 0.31 | 0.26 | 0.59 | 0.54 | 22 | 56 |
| 10 | NY | Independent | 118 | 235 469 | $18516 | 194.1 | 49.5 | 0.18 | 0.08 | 0.34 | 0.19 | 0.26 | 0.22 | 0.56 | 0.61 | 14 | 86 |
| 11 | NY | Independent | 122 | 200 536 | $19168 | 283.6 | c | 0.19 | 0.09 | 0.52 | 0.17 | 0.37 | 0.37 | 0.57 | 0.56 | 43 | 57 |
| Range | 35 | 35 253 | $16175 | 6.2 | 49.0 | 0.15 | 0.07 | 0.34 | 0.12 | 0.25 | 0.21 | 0.51 | 0.42 | 0 | 14 | ||
| 187 | 423 394 | $40 040 | 526 | 92.3 | 0.53 | 0.29 | 0.56 | 0.53 | 0.40 | 0.37 | 0.78 | 0.71 | 44 | 86 | |||
| Mean | 113.27 | 172317 | $22 015 | 202.47 | 64.1 | 0.27 | 0.12 | 0.48 | 0.25 | 0.33 | 0.27 | 0.58 | 0.54 | 16 | 44 | ||
| SD | 42.79 | 103 064 | $7 077 | 150.72 | 14.3 | 0.12 | 0.07 | 0.07 | 0.13 | 0.05 | 0.05 | 0.08 | 0.08 | 16 | 22 | ||
|
Coefficient of variation |
43.62 | 54.48 | 13.84 | 51.17 | 15.04 | 18.88 | 13.63 | 15.22 | 100.27 | 48.98 | |||||||
Abbreviations: LHD, local health department; NPHPS, National Public Health Performance Standards.
Network measurements are given for all ties and strongest ties networks.
Network measurements are standardized between 0 and 1.
Performance scores for LHD 11 were omitted from the analysis because of an erroneously recorded date on its NPHPS V1 assessment (not within 3 years).
Data collection procedures
An organizational network survey was developed and pilot tested prior to implementation.17 The survey was administered electronically to all employees of the sample LHDs (N = 1 267). A paper option was available for those without Internet access. The study was approved by the Columbia University Institutional Review Board.
Section I of the survey captured employee-to-employee communication, defined as giving or receiving information about public health work, including e-mail and phone calls. Employees were asked to characterize their communication with other employees as follows: routine and frequent communication (daily or weekly); routine but not frequent communication (monthly or quarterly); or nonroutine communication (communication would be unusual). These categories were developed to address the collaborative culture of public health, a suspected source of overresponse bias (overestimating communication links) identified in our pilot work.18,19 The responses to section I of the survey produced the employee-to-employee network. Responses that indicated both frequent and not frequent communication produced a network representing “all ties” between employees. Responses indicating only frequent communication produced a network representing “strongest ties” between employees. Responses regarding nonroutine communication were not analyzed.
Section II was based on the taxonomy of essential public health work (ie, work likely to be performed in any LHD), identified from documents describing public health practice.17 Each employee was asked to indicate from a list containing the following:
44 tasks, those assigned to him or her as part of normal work;
53 knowledge items, those for which he or she possessed better than average knowledge; and
54 resources, those readily available when needed for daily work.
Responses to section II produced the employee-to-task network (tasks assigned), employee-to-knowledge network (better than average knowledge), and employee-to-resource network (resources available). The Organizational Risk Analyzer (ORA) computer program was used for the analysis.20
Structured interviews with health officers of each LHD documented their best estimate of change (if any) in their NPHPS V1 scores between the time the local public health system completed the instrument and the time of the network survey. Scores were updated accordingly.
Network measurement procedures
We calculated four network measurements that reflect organizational cohesion and integration, and we developed one measure to assess interdivisional communication. The network measurements consist of ratios of different links between employees. These measurements have been normalized between 0 and 1 to allow comparisons between networks of different size. The network measurements are described in detail in Table 1.
TABLE 1.
Network measures reported in this study with definitions and interpretations
| Network measure | Definition | Interpretation a |
|---|---|---|
| Density | Ratio of the number of links present between employees vs the maximum number of possible links. The measurement is normalized between 0 and 1 to account for network size. |
Measurements closer to 1 signify that there are relatively many communication links between employees, suggesting inefficient or repetitive information exchange. Measurements closer to 0 signify relatively few communication links, suggesting that information is not flowing. |
| Centralization | Centralization of the employee communication network is calculated from the total number of direct links each employee has divided by the maximum possible sum of differences, normalized between 0 and 1. |
Measurements closer to 1 signify that many links are concentrated around a few nodes, suggesting more centralized information flow with hierarchical “command and control” decision making. Measurements closer to 0 signify little variation in the number of links each employee has, suggesting more decentralized information flow with decisions made closer to point of service. |
| If every employee in the network were linked only to a single “leader” at the center, the network would look like a star (*) and centralization would be 1. In a decentralized network, the links are more dispersed. | ||
| Complexity | A composite measure to approximate interdependencies and integration. It represents the ratio of links present in all four matrices vs the maximum number of possible links (ie, employee × employee; employee × knowledge; employee × task; and employee × resource), normalized between 0 and 1. |
Measurements that are closer to 0 signify that interdependency and integration are low, suggesting duplication of effort and inefficiency. Measurements closer to 1 signify that interdependency and integration are high, suggesting that error “cascades” are more likely (ie, one error leads to subsequent errors in all dependent areas). |
| Clustering coefficient | The average of the proportion of links between each employee and other employees to which he or she is directly linked divided by the number of links that could possibly exist between them, normalized between 0 and 1 (eg, three employees can communicate directly with each other, but in fact only two of them may do so). |
The clustering coefficient measures of degree to which employees tend to cluster together in terms of communication. It gives a sense of the local characteristics of the network—how information flows among small groups of employees. An optimal level of clustering supports local information sharing and a decentralized infrastructure. |
| Percentage divisions tending toward silo | The percentage of an LHD’s divisions or programs with an SI ≥ 0.5. The SI is the proportion of communication links that are between two members of the same division vs communication links that are between members of different divisions. |
In an information silo, communication between employees is internal and vertical within a division or program. Information silos can make overall organizational coordination and communication difficult to achieve, with a deleterious effect on performance. |
Abbreviations: LHD, local health department; SI, silo index.
Network measurements must be interpreted in the context of the organization’s size and the type of work being done. Network measurements, depending on the circumstances, tend to be less advantageous both when they are very high or very low. For example, optimal performance in a small shoelace factory may be achieved with relatively few communication links between employees (low density), whereas the opposite may be true in a small research laboratory. Table 2 gives the range for each measurement in the 11 LHDS studied, which can serve as benchmarks for LHDs.
Measurements of cohesion and integration
The first measure is density in the employee-to-employee network. We calculated the ratio of links present versus the total number of possible links. Density is an indicator for how effectively communication is flowing between all employees in the network.
The second measure is centralization of the employee-to-employee network. Centralization is equal to the difference between the total number of links to and from all pairs of employees divided by the maximum possible sum of differences for all employees. Centralization is an indicator for hierarchical versus distributed decision making.
The third measure, organizational complexity, is a composite measure. Complexity is equal to the ratio of links present versus the total number of possible links in the employee-to-employee networks, plus the employee-to-task, employee-to-knowledge, and employee-to-resource networks. Complexity is an indicator for integration and cohesion among the organization’s components.21,22
The fourth measure, clustering coefficient, is equal to the average proportion of links between each employee and his or her direct neighbors divided by the number of links that could possibly exist between them.23 A direct neighbor is a person with whom an individual employee communicates directly. The clustering coefficient is an indicator for how effectively communication flows between small groups in the network.
Measurement of interdivisional communication
We calculated the percentage of LHD divisions tending toward information silos, using the employee-to-employee network, to create a silo index (SI). In an information silo, there is tight communication between employees who work together in a division or program but interaction with other parts of the organization (other silos) tends to be limited or only initiated through management.24
Silo index is equal to the proportion of communication links that are internal(between two members of the same division) versus communication links that are external (between members of different divisions). It is computed as follows:
where d is the division or program, I is number of internal links, and E is the number of external links. The division SI is between −1 and 1. A score of 1 indicates all links are internal (ie, a perfect silo structure), whereas a score of negative −1 indicates all external links. The LHDs in our sample had between four and nine divisions. To compare how “silo-ed” the LHDs were, we transformed this measure from the divisional level to the LHD level of analysis by computing the percentage of divisions with SI ≥ 0.5.
Data analysis procedures
We compared network measurements for 11 LHDs by using descriptive statistics and graphic visualizations. To investigate whether LHDs share a similar pattern of network measurements, we compared the variability of measurements with the coefficient of variation (CV). CV is a relative scale that indicates the dispersion of a measurement as the ratio of the standard deviation to the mean.25
To determine whether LHDs networks have a distinctive pattern, we used the CV to compare the centralization and clustering of LHD networks with random networks. To make this comparison, we produced a set of five random networks for each LHD by starting with the same number of nodes and adding links between them at random until the density of the real LHD networks was reached. To test randomization, we preformed pairwise correlations for measurements of centralization and clustering coefficient between each LHD and its set of random networks. No correlations were more than 0.5, indicating randomization was sufficient. The random networks contained no silos. Thus, the CV was not calculated for the silo measure. We did not include network complexity in this comparison because this measure is calculated using density.
To investigate whether there are similarities in essential public health work across LHDs, we used Kendall’s τ, a nonparametric test of correspondence between two rankings.26 We calculated pairwise correlations for the rankings of task, knowledge, and resources produced by the employees in each LHD. We correlated ranked lists of (a) tasks to which employees were assigned to as part of normal work; (b) items for which they possessed better than average knowledge; and (c) resources readily available when needed for daily work. A detailed description of the results of this analysis is reported elsewhere.17
Finally, we correlated LHDs’ network measurements with their NPHPS V1 performance scores and demographic variables using Pearson r, a parametric test of the magnitude and direction of association between two variables measured as intervals or ratios.27 These correlations were calculated for LHD 1 through LHD 10. LHD 11 was excluded because of an erroneous date recorded on its NPHPS V1 assessment (not within 3 years).
Results
Of 1 239 employees in 11 LHDs, 1 062 completed the survey, with a response rate of 84 percent. Individual LHD response rates ranged between 80 percent and 95 percent, sufficient to produce a reliable description of the networks.28–30 Table 2 provides descriptive data for the sample LHDs, mean NPHPS performance scores, and network measurements.
Common organizational features
The responses from section I of the survey revealed that LHDs share a compound two-mode communication structure in which centralized hierarchies are coupled with distributed networks at the point of service.31 The all ties networks for 11 LHDs have a mean density measurement of 0.27 and mean centralization of 0.48. In contrast, the strongest ties networks had lower mean density at 0.12 and lower mean centralization at 0.25. In Table 2, LHD 7 is an outlier with high centralization in both all ties and strongest ties networks (0.52 and 0.53). At the time of the study, LHD 7 was assembling documentation for the Baldridge process,32 a type of performance assessment that produced intensive day-to-day communication between central office and program staff. The high/low pattern of density and centralization does not extend to clustering coefficient (mean 0.58 all ties and 0.54 strongest ties) and complexity (mean 0.33 all ties and 0.27 strongest ties).
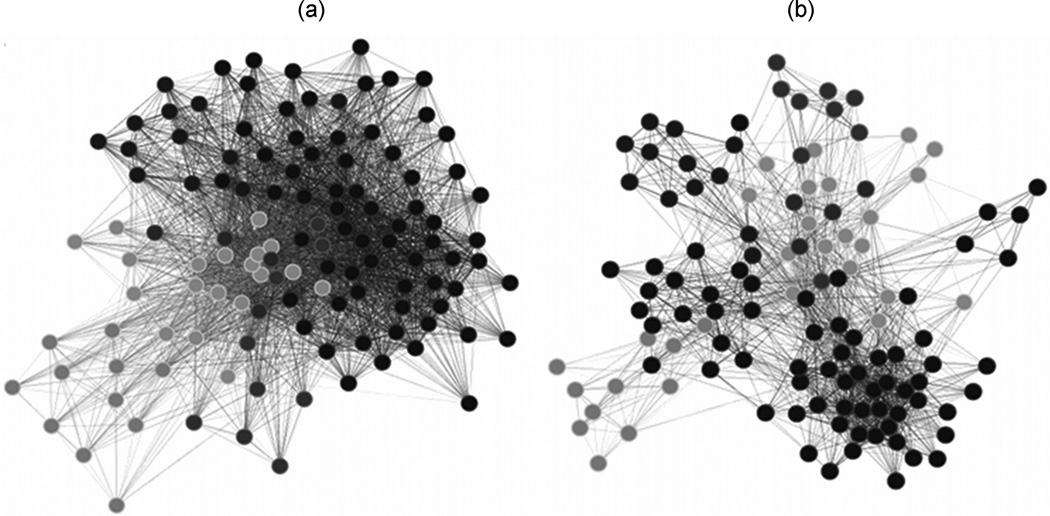
Figure 2 gives an example of the two-mode structure. Figure 2a showing all ties between employees who represents communication for both control and maintenance, such as routine progress reports, staff meetings, and status updates, plus more frequent daily and weekly communication. It has a density of 0.23, centralization of 0.52, and complexity of 0.30. Figure 2b shows the communication structure of strongest ties between employees representing frequent communication such as daily and weekly assignments and reports on active cases, closer to the point of service. It has a much lower density of 0.11, much lower centralization of 0.29, and similar complexity of 0.24.
FIGURE 2. An Example of the Two-Mode Communication Structure in a Local Health Department (LHD): (a) All Ties Showing a More Centralized Network; (b) Strongest Ties Showing a More Decentralized Networka.
a Nodes represent employees, and links represent a relationship between employees (in this case, communication). Gray tones represent programmatic division within the LHD.
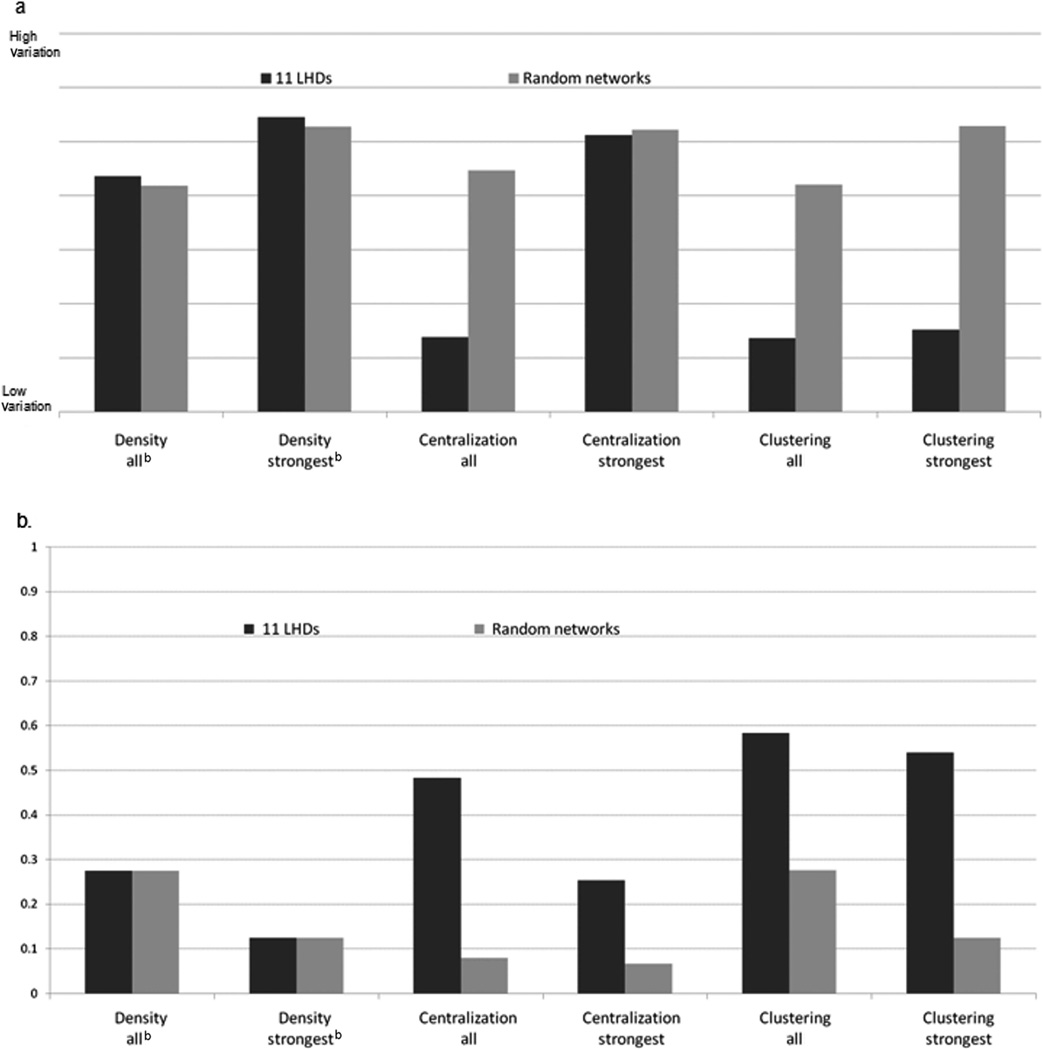
Local health departments also share a distinct pattern of high centralization and clustering. When we compared CVs, we found low variability across LHDs on centralization of the all ties networks and low variability on clustering coefficients of both all ties and strongest ties networks. Low variability on these measures is different from what would be expected in a random network. We found higher, more random variability in centralization of the LHD strongest ties networks. We suspected that finding was driven by LHD 7,a high outlier that we ha veexplained.However,when we removed LHD 7 from the CV calculation, variability for centralization in the strongest ties networks was minimally reduced (<10 units) and remained close to random variability. When we compared the means of the network measurements, we found that 11 LHD networks had higher centralization and clustering coefficients than expected in random networks. Taken together, the comparison of CVs and mean network measurements suggests that these 11 LHDs are distinguished from random networks by a pattern of high centralization in the all ties network and high clustering coefficients. Centralization in the strongest ties networks is variable. Figure 3 illustrates the CVs and the mean network measurements.
FIGURE 3. Bar Graphs Showing the Coefficients of Variation (a) and the Means (b) for 11 Local Health Departments (LHDs) Compared With a Set of Randomly Generated Networks*.
*Comparisons are illustrated for employee communication networks. A set of five random networks was generated for each LHD on the basis of the same density. The y-axis in (a) represents a scale for the coefficient of variation, which is a relative term, in which a higher value indicates more variability. LHD networks exhibit much less variability in centralization of their all ties networks and in clustering than random networks. The y-axis in (b) represents mean network measurements (normalized between 0 and 1). LHD networks are more centralized and exhibit more clustering than expected in random networks.
Essential tasks and knowledge rank similarly across LHDs
We correlated ranked lists of responses to the questions in section II of the survey. About 70 percent of the correlations between LHD pairs on rankings of 44 tasks and 53 knowledge items were very strong (>0.7). For 54 resources, only 16 percent of LHD pairs were strongly correlated (>0.7) and 43 percent were moderately correlated (>0.6). Detailed findings on the task, knowledge, and resource networks are reported elsewhere.17
LHDs networks are correlated with performance of Essential Services of Public Health
Local health departments with higher density and complexity in both the all ties and strongest ties networks were strongly positively associated (r ≥ 0.65, P ≤ .05) with better performance on 3 of the 10 Essential Services of Public Health (ES): ES 4 (mobilizing community partnerships), ES 7 (linking people to health services), and ES 9 (evaluating health services). Higher centralization of the strongest ties network was associated with better performance of these services, but the association did not hold for the all ties network.
A higher SI, indicating lower cross-divisional communication among employees within an LHD, was significantly, negatively correlated with performance on 8 of 10 essential services (r ≥ −0.65, P ≤ .05). These results are displayed in Table 3.
TABLE 3.
Pearson correlation coefficients between four network measurements a and local health department performance scores on each Essential Service of Public Health (ES)
| Density |
Centralization |
Complexity |
Clustering coefficient |
% Divisions tending toward silo |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ES | All | Strongest | All | Strongest | All | Strongest | All | Strongest | All | Strongest | |
| 1 | Monitor health status to identify and solve community health problems |
−0.01 | 0.08 | 0.79b | 0.40 | 0.29 | 0.14 | 0.07 | −0.05 | 0.44 | −0.69c |
| 2 | Diagnose and investigate health problems and health hazards in the community |
0.63 | 0.62 | 0.26 | 0.43 | 0.75b | 0.75b | 0.47 | 0.41 | 0.51 | −0.73c |
| 3 | Inform, educate, and empower people about health issues |
0.57 | 0.62 | 0.39 | 0.62 | 0.57 | 0.63b | 0.43 | 0.40 | 0.52 | −0.63 |
| 4 |
Mobilize community partnerships and action to identify and solve health problems |
0.79b | 0.75b | 0.25 | 0.68b | 0.83b | 0.82b | 0.74b | 0.47 | 0.65b | −0.85c |
| 5 | Develop policies and plans that support individual and community health efforts |
0.46 | 0.51 | 0.49 | 0.59 | 0.57 | 0.58 | 0.45 | 0.32 | 0.64b | −0.65c |
| 6 | Enforce laws and regulations that protect health and ensure safety |
0.02 | 0.18 | 0.61 | 0.25 | 0.14 | 0.22 | 0.37 | 0.29 | 0.42 | −0.45 |
| 7 |
Link people to needed personal health services and ensure provision of care when otherwise unavailable |
0.71b | 0.75b | 0.18 | 0.69b | 0.67b | 0.74b | 0.53 | 0.33 | 0.66b | −0.68c |
| 8 | Ensure competent public and personal health workforce |
0.42 | 0.49 | 0.71b | 0.54 | 0.62 | 0.55 | 0.34 | −0.03 | 0.45 | −0.85c |
| 9 |
Evaluate effectiveness accessibility, and quality of personal and population-based health services |
0.60 | 0.64b | 0.44 | 0.67b | 0.75b | 0.72b | 0.60 | 0.47 | 0.61 | −0.87c |
| 10 | Research for new insights and innovative solutions to health problems |
0.12 | 0.29 | 0.65b | 0.27 | 0.33 | 0.31 | 0.15 | −0.11 | 0.32 | −0.72c |
Correlations are displayed for all ties and strongest ties networks. Significant correlations >0.60 are given in boldface. There is a pattern of correlations for ES 4, 7, and 9 (bolded).
Positive correlation, P ≤ .05.
Negative correlation, P ≤ .05
LHD networks are correlated with specific demographics
Larger LHDs with more employees serving larger populations were negatively associated with network density and complexity (ie, as the number of employees increase, there is less density [communication] and complexity [integration]) and positively associated with silos in programs or divisions. Local health departments serving younger populations were less centralized, whereas those serving more elderly populations were more dense and complex. Local health departments serving more vulnerable populations, such as those below the poverty line and American Indians, were associated with increased task redundancy (ie, more employees performing the same tasks) and information silos specifically in their administrative divisions. These results are displayed in Table 4.
TABLE 4.
Pearson correlation coefficients showing association between network measurements and LHD demographicsa
| Density |
Centralization |
Complexity |
Clustering coefficient |
Admin division silo index |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All | Strongest | All | Strongest | All | Strongest | All | Strongest | All | Strongest | |
| LHD size | −0.58 | −0.70 | 0.41 | −0.15 | −0.47 | −0.65 | −0.86 | −0.48 | 0.59 | 0.65 |
| Size of population served | −0.61 | −0.58 | −0.04 | −0.10 | −0.64 | −0.82 | −0.53 | −0.19 | 0.76 | 0.70 |
| % Age <18 y | −0.52 | −0.51 | −0.18 | −0.76 | −0.57 | −0.37 | 0.09 | 0.53 | 0.24 | 0.32 |
| % Age >65 y | 0.72 | 0.60 | −0.22 | 0.52 | 0.70 | 0.55 | 0.10 | −0.05 | 0.01 | −0.28 |
| Number persons below poverty Line |
0.10 | −0.03 | −0.15 | −0.24 | 0.11 | 0.24 | 0.18 | 0.33 | 0.59 | 0.58 |
| % American Indian/Native Alaskan |
0.08 | −0.05 | 0.02 | −0.36 | 0.12 | 0.29 | 0.13 | 0.28 | −0.76 | 0.65 |
Abbreviation: LHD, local health department.
Correlations are displayed for both the all ties and the strongest ties networks. The silo index is shown for the administrative divisions in the 11 LHDs in this study. Significant correlations are given in boldface.
Discussion
In this study, we compared 11 LHD intraorganizational networks. We found that LHDs have compound organizational forms with high network centralization and clustering. We found high correlation between LHDs in terms of the tasks and knowledge that constitute public health work but variability in correlation of resources. We found a pattern of positive associations between LHD network measurements and performance of ES 4, 7 and 9.We found strong negative associations between information silos and performance. We also found associations between LHD networks and characteristics of the population served. With these findings, we can make several observations that not only give insight into how LHDs are organized but may also inform management and performance.
Common organizational structure
The task environment for any organization consists of physical, technological, cultural, and social contexts to which the organization must adapt.33 Our findings show that LHDs in the sample respond to the public health task environment with a two-mode network structure.31 In the all ties networks, we found a pattern between LHDs of centralization close to or more than 0.50. This suggests an inherent hierarchical, or “command and control,” decision-making structure in these LHDs, in which most employee communication is directed to and from a central core group. Under this type of arrangement, there is a risk that individual employees are inhibited from exercising discretion needed for daily work.34 Local health departments appear to counter this risk with a pattern of markedly lower centralization and density in the strongest ties networks (except for the outlier LHD 7, for which we have an explanation). Fewer employee links with the core for day-to-day communication suggest distributed allocation of decision authority, which can optimize performance in complex multiple-task environments, such as LHDs.35
The compound structure allows for overall tight control coupled with some flexibility for distributed decision making in response to day-to-day contingencies.36 The compound structure makes sense for LHDs because daily decisions are often made in geographically separate locations (eg, in homes, licensed businesses, scattered clinics) by professionals with specialized training and ability, whereas tighter hierarchical control is essential given the need for public accountability regarding use of tax funds and exercise of public health authority.37 Formal structured decision making ensures that an LHD pursues a given population health focus; specialized program staff then has autonomy in carrying out these decisions.
Centralization in the strongest ties networks is variable to the degree that it is close to random. There was no correlation between centralization and LHD demographics to explain this variability. Less centralized communication (and lower density) coupled with high clustering in day-to-day work means that while employees may communicate adequately for their immediate work, they risk not being aware of what else is going on in the LHD that affects their work (ie, information silos). High clustering is particularly significant because knowledge and work strategies tend to be more similar within than between groups. Employees connected across groups are more likely to bring new information, knowledge, and alternative approaches.38 Since the strongest ties network is analogous to day-today operations, this suggests an opportunity for targeted organizational management strategies that might achieve some optimal level of day-to-day centralized communication that is not random. In particular, this suggests that standard set of management strategies to increase between-group communication and collaboration might be of value across public health systems.
Complexity measurements are less variable and appear to be a source of strength for LHDs. Complexity is associated with efficiency in dynamic work environments such a public health that require adaptation to changing conditions.36 Relatively similar levels of complexity between the all ties and strongest ties networks suggest that employees may use the most effective tasks, knowledge, or resources for a particular goal without limiting options that might be used elsewhere in the system.31 For example, an individual employee might manage a policy decision to reduce tobacco use by communicating with several colleagues and performing a range of tasks, using a variety of knowledge and resources, for reaching out to different venues, such as schools, workplaces, or recreational facilities. However, when individual employees take on different roles in response to different organizational demands, they must have sufficient competency to act efficiently and asynchronously in all these roles. These findings have implications for cross-programmatic training.
Comparable on tasks and knowledge but not resources
We found that employees across 11 LHDs were assigned to tasks similarly and possessed similar knowledge, suggesting systemic commonalities. Recognition of commonalities may support systemwide workforce development and uniform job descriptions. Somewhat lower correlations in how employees ranked their access to resources hint that this may be a source of variability between LHDs. Efforts to standardize, measure, and compare performance should take this into account. Attempts to understand public health infrastructure over the longer term should pay particular attention to LHDs that are most prone to variability, what predicts variability, and the effects of adequate or inadequate resources. Aspects of variability may include external or political influences on management and administration, but may also include management choices that can be more readily adjusted, such as how data and other resources are made available to staff.
Networks influence on performance
Increased density and complexity, and increased centralization in the strongest ties networks, were associated with increased performance of three Essential Services of Public Health: mobilizing the community, linking people to services, and evaluating population services (ES 4, 7, and 9, respectively). Delivery of ES 4, 7, and 9 are involved with outreach. All require partnerships external to the LHD that are sophisticated to execute at the population-health level. They likely call for more integration of tasks, knowledge, and resources (complexity) and quicker circulation of information (density). However, centralization in the all ties network appears to be less significant to ES 4, 7, and 9 than in the day-to-day strongest ties network. In contrast, more centralization in the all ties network is associated with better performance monitoring health status, ensuring a competent workforce, and research (ES 1, 8, and 10, respectively). This may reflect the administrative aspects of those services that are achieved through more hierarchical communication.
How LHDs adapt to the population served
Our correlations show that larger health departments that serve larger populations tend to have networks that exhibit problems of bureaucratic organizations such as lower communication density and a higher proportion of information silos. The specialization possible in larger LHDs has been associated with better performance of certain Essential Services.39 The compound structure we found may be a response to specialized public health work, but there is a trade-off in lower between-division communication (information silos) particularly on a day-to-day basis.40 Our results suggest that the bureaucracy to coordinate specialized activities may degrade organizational efficiency. The larger LHDs in our sample exhibited lower network density and complexity, which can mean less efficient communication and integration. In the strongest ties networks, a higher SI was negatively associated with performance for all but two Essential Services of Public Health. Silos signify absence of communication relationships between departments, which can be a byproduct of specialization barriers between groups.41 Although information silos are a problem for many organizations, for LHDs, the problem is compounded by categorical programmatic funding streams focused on narrowly defined goals.7,42 Management techniques aimed at developing organizational integration, such as cross-program teams, could be useful for LHDs systemwide.
Correlations between network measures and characteristics of the populations served suggest that LHDs do adapt to their external task environment.14 Local health departments may adapt to serving younger populations with less bureaucratic hierarchy, perhaps because these healthier groups require less services, which makes tightly centralized hierarchy less necessary. Local health departments may adapt to elderly populations with more communication and integration, perhaps because these groups need more coordinated services such as home care. Local health departments may adapt to vulnerable populations with administrative silos and redundant staff assignments, perhaps because these groups require more overlapping entitlements and services. Further research with a larger sample size will help us determine why LHDs adapt as they do and increase the generalizability of these findings.
Limitations
The small sample size limits this analysis to describing associations within the data. Although we can infer several interesting and logical tendencies, a larger dataset is needed to test these inferences and to model hierarchical relationships between factors such as LHD governance and network structure. Our analysis of networks in relation to performance raises two areas of concern. First is the reliability of NPHPS V1 performance scores. Second, LHD networks were associated with system performance under the assumption that the LHD influences performance of the system. Although the NPHPS V1 assessment instrument has been tested for validity,43 scores are self-reported and may be unreliable. To address reliability, we reviewed NPHPS scores in detail with health officials in each LHD and adjusted scores to correspond to the time of the study. The reviews and any adjustments health officials made to their scores were well reasoned and credible. Health officials made adjustments in both positive and negative directions and the LHD network findings were consistent with the public health system scores. Until a better alternative becomes available, NPHPS instruments are the only standard tools in use nationally that have produced a consistent, comparative dataset for study.44
Implications and future work
LHD networks are worth studying because they represent the true functioning of the organization41 and shed light on factors that give rise to variation in local public health. This study has shown that patterns in network structure occur across LHDs. Although each agency may have a unique configuration, LHDs share core programs and appear to have similar needs for intraorganizational communication and integration.
Organizational theorists have long argued that structure is related to performance; however, studies defining structure in terms of people-to-people interactions have found mixed results.45,46 We extended the notion of structure beyond personnel to include analysis of task, knowledge, and resource differentiation among LHDs, in effect comparing organizational structure in the context of the work performed.47 This expanded approach revealed that performance is associated with particular common structures. Network analysis can help LHD managers to make evidence-based decisions to improve performance.48 The variability we found between LHDs suggests that LHDs might benefit from a standard set of management strategies to improve day-to-day integration.
Identification of consistent organizational network features has the potential to allow LHDs to optimize common elements across systems and supports national standardization efforts to promote uniformly high performance in service delivery to all populations. This research establishes baseline network parameters that can serve as a comparative basis for local management decisions on communication, integration, and resource allocation. In the future, we will apply network analysis as an intervention to support management decisions regarding specific performance outcomes.
Acknowledgments
The Robert Wood Johnson Foundation supported this research through an HCFO PHSSR grant. J. K. is supported by National Library of Medicine grant T15-LM007079.
The authors thank Kristine Gebbie, DrPH, RN, for her insightful comments.
Contributor Information
Jacqueline Merrill, Public Health Nurse and Associate Research Scientist, Department of Biomedical Informatics, College of Physicians and Surgeons, Columbia University, New York..
Jonathan W. Keeling, Doctoral Candidate, Department of Biomedical Informatics, Columbia University, New York..
Kathleen M. Carley, Professor, School of Computer Science, Institute for Software Research, and Director, Center for Computational Analysis of Social and Organizational Systems, Carnegie Mellon University, Pittsburgh, Pennsylvania..
REFERENCES
- 1.National Association of County & City Health Officials. 2005 National Profile of Local Health Departments. Washington, DC: National Association of County&City Health Officials; 2006. [Google Scholar]
- 2.Scutchfield FD, Bhandari MW, Lawhorn NA, Lamberth CD, Ingram RC. Public health performance. Am J Prev Med. 2009;36(3):266–272. doi: 10.1016/j.amepre.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Turnock BJ. Public Health: What It Is and How It Works. 4th ed. Boston, MA: Jones & Bartlett; 2009. [Google Scholar]
- 4.Russo P. Accreditation of public health agencies: a means, not an end. J Public Health Manag Pract. 2007;13(4):329–331. doi: 10.1097/01.PHH.0000278022.18702.22. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. National Public Health Performance Standards program. [Accessed May, 2009]; http://www.cdc.gov/od/ocphp/nphpsp.
- 6.Public Health Accreditation Board. [Accessed August 2008]; Web site. http://www.exploringaccreditation.org.
- 7.Turning Point Performance Management National Excellence Collaborative. From Silos to Systems: Using Performance Management to Improve the Public’s Health. Washington, DC: Public Health Foundation; 2004. [Google Scholar]
- 8.US Department of Health and Human Services. Healthy People 2010. Washington, DC: Government Printing Office; 2000. [Google Scholar]
- 9.Centers for Disease Control and Prevention. Advancing the Nation’s Health: A Guide to Public Health Research Needs, 2006–2015. Washington, DC: US Department of Health and Human Services; 2006. [Google Scholar]
- 10.Public Health Informatics Institute. [Accessed July 2008];Taking care of business: A collaboration to define local health department business processes. http://www.phii.org/resources/doc_details.asp?id=104.
- 11.Carley KM. Companion to Organizations. Malden, MA: Blackwell; 2002. Intra-organizational computation and complexity; pp. 208–232. [Google Scholar]
- 12.Krackhardt D, Carley KM. A PCANS model of structure in organizations; Monterey, CA. Paper presented at: International Symposium on Command and Control Research and Technology.1998. [Google Scholar]
- 13.Thompson JD. Organizations in Action Social Science Bases of Administrative Theory. New York, NY: McGraw Hill; 1967. [Google Scholar]
- 14.Nadler DA, Tushman ML. Strategic Organization Design: Concepts, Tools, and Processes. Saddle River, NJ: Scott Foresman; 1988. [Google Scholar]
- 15.Public Health Functions Steering Committee. Public Health in America: Vision, Mission, and Essential Services. Washington, DC: US Public Health Service; 1994. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Local Public Health Performance Assessment Instrument, Version 1.0. [Published March 19. Accessed November 2008]; http://www.cdc.gov/od/ocphp/nphpsp/TheInstruments.htm.
- 17.Merrill J, Keeling J, Gebbie KM. Toward standardized, comparable workforce data: a taxonomic description of essential public health work. Health Serv Res. 2009;45(5, pt II):1818–1841. doi: 10.1111/j.1475-6773.2009.01015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merrill J, Bakken S, Rockoff M, Gebbie K, Carley K. Description of a method to support public health information management: organizational network analysis. J Biomed Inf. 2007;40(4):422–428. doi: 10.1016/j.jbi.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merrill J, Caldwell M, Rockoff M, Gebbie K, Carley K, Bakken S. Findings from an organizational network analysis to support local public health management. J Urban Health. 2008;85(4):572–584. doi: 10.1007/s11524-008-9277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ORA: Organizational Risk Analyzer. Pittsburgh, PA: Center for Analysis of Social and Organizational Systems, Carnegie Mellon University; 2008. [computer program]. Version 1.3. [Google Scholar]
- 21.March JG. Exploration and exploitation in organizational learning. Org Sci. 1991;2(1):71–87. [Google Scholar]
- 22.Sorenson O. Interdependence and adaptability: organizational learning and the long-term effect of integration. Manag Sci. 2003;49(4):446–463. [Google Scholar]
- 23.Watts D, Strogatz S. Collective dynamics of “small-world” networks. Nature. 1998;393(6684):409–410. doi: 10.1038/30918. [DOI] [PubMed] [Google Scholar]
- 24.Doerscher T. [Accessed November 2005];Teamwork design for success. http://www.chiefprojectofficer.com.
- 25.UCLA: Academic Technology Services Statistical Consulting Group. [Accessed November 24, 2009];Introduction to SAS. http://www.ats.ucla.edu/stat/mult_pkg/faq/general/coefficientofvariation.htm.
- 26.Kendall M. Rank Correlation Methods. London, England: Charles Griffin & Co Ltd; 1948. [Google Scholar]
- 27.Rodgers JL, Nicewander WA. Thirteen ways to look at the correlation coefficient. Am Statistician. 1988;42(1):59–66. [Google Scholar]
- 28.Borgatti SP, Carley KM, Krackhardt D. On the robustness of centrality measures under conditions of imperfect data. Soc Netw. 2006;28:124–136. [Google Scholar]
- 29.Carley KM. Dynamic network analysis; Washington, DC. Paper presented at: Dynamic Social Network Modeling and Analysis: Workshop Summary and Papers.2002. [Google Scholar]
- 30.Kossinets G. Effects of missing data in social networks. Soc Netw. 2006;28(3):247–268. [Google Scholar]
- 31.Horling B, Lesser V. A survey of multi-agent organizational paradigms. Knowl Eng Rev. 2005;19(4):281–316. [Google Scholar]
- 32.National Institute of Standards and Technology. [Accessed May 1, 2009];Baldridge National Quality Program. http://www.quality.nist.gov.
- 33.Horner SB. Munificence, dynamism, and complexity: task environment effects on attributes of boards of directors; Indianapolis, IN. Paper presented at: the 25th Annual Meeting of the Midwest Academy of Management.2002. [Google Scholar]
- 34.Hansen M. Collaboration. Boston, MA: Harvard Business Press; 2009. [Google Scholar]
- 35.Colombo MG, Delmastro M, Rabbiosi L. “Highp erformance” work practices, decentralization, and profitability: evidence from panel data. Ind Corp Change. 2007;16(6):1037–1067. [Google Scholar]
- 36.Woodward J. Industrial Organization: Theory and Practice. London, England: Oxford University Press; 1965. [Google Scholar]
- 37.Rainey HG. Understanding and Managing Public Organizations. 3rd ed. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 38.Burt R. Structural holes and good ideas. Am J Sociol. 2004;110(2):349–399. [Google Scholar]
- 39.Mays GP, McHugh MC, Shim K, et al. Institutional and economic determinants of public health system performance. Am J Public Health. 2006;96(3):523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsai W. Social structure of “coopetition” within a multiunit organization: coordination, competition, and intraorganizational knowledge sharing. Organ Sci. 2002;13(2):179–190. [Google Scholar]
- 41.Monge PR, Contractor NS. Theories of Communication Networks. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 42.O’Carroll PW, Yasnoff W, Ward M, editors. Public Health Informatics and Information Systems. New York, NY: Springer; 2003. [Google Scholar]
- 43.Beaulieu J, Scutchfield FD, Kelly AV. Content and criterion validity evaluation of National Public Health Performance Standards measurement instruments. Public Health Rep. 2003;118(6):508–517. doi: 10.1093/phr/118.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mays GP, Smith SA, Ingram RC, Racster LJ, Lamberth CD, Lovely ES. Public health delivery systems: evidence, uncertainty, and emerging research needs. Am J Prev Med. 2009;36(3):256–265. doi: 10.1016/j.amepre.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 45.Ashworth MJ, Carey KM. Who you know vs. what you know: the impact of social position and knowledge on team performance. J Math Sociol. 2006;30(1):43–75. [Google Scholar]
- 46.Prietula M, Simon HA. The experts in your midst. Harv Bus Rev. 1989;89(1):120–124. [Google Scholar]
- 47.Perrow C. A framework for the comparative analysis of organization. Am Sociol Rev. 1967;32(2):144–208. [Google Scholar]
- 48.Johns G. The essential impact of context on organizational behavior. Acad Manag Rev. 2006;31(2):386–408. [Google Scholar]