Abstract
Background and purpose:
Few studies have explored optimal advancement and variation in mobility and length of stay (LOS) data with critically ill patients in the intensive care unit (ICU). The purpose of this study was to analyze the outcomes and LOS of critically ill patients in the neurotrauma ICU involved in rehabilitation.
Methods:
A bidirectional case–control study of a total of 30 patients admitted to a level 1 trauma hospital in the metropolitan Chicago area with Glasgow Coma Score (GCS) of ≤12 (3-12) were studied. Functional outcomes of a structured mobility group were compared at first upright sitting and at ICU discharge using the functional independence measure (FIM). Retrospective LOS review of a group (n = 15) with unstructured activity advancement was compared.
Results:
The main outcome measures were FIM scores and LOS in number of days. In the structured mobility group, a significant increase in functional performance between first upright sitting and ICU discharge was found (P < .005). Length of stay was shorter in the structured mobility groups but the difference was not statistically significant.
Conclusions:
Results from this study revealed favorable functional outcomes for patients involved in a structured mobility program with physical therapy in the neuro/trauma ICU.
Keywords: outcomes, neurocritical care, brain hemorrhage, cerebrovascular trauma, physical therapy
Introduction
Increasingly, emphasis in health care is placed on improving functional outcomes while decreasing intensive care unit (ICU) length of stay (LOS) and costs.1–4 Of the many interventions that occur for a patient in the ICU, advancing the ability to move and function with more independence has also received attention.5,6 Transitioning from supine to upright sitting is often encouraged once a patient’s medical status allows,7 since optimization of oxygen transport with more uniform ventilation and perfusion and improvements in functional residual capacities have been found in the seated position over supine.8 Incorporating rehabilitation services, specifically physical therapy (PT), has been supported to advance the activity and function of a patient and potentially improve outcomes.9 While the goals of reducing the deleterious effects of immobility as well as overall costs of care are common, a wide variety of approaches have been found in intensity and frequency of therapy,7,10 and no universally accepted criteria for safely increasing mobility are established although recent guidelines have been published.11
In the United States, PT in the ICU is currently a service that requires consultation directly by physicians. Decisions can then be made by the multidisciplinary team to advance the mobility of an ICU patient. While structured mobility programs with early involvement of PT are becoming more common in medical ICUs, there is little data regarding the feasibility of such programs in the neurological ICU.
The purpose of this research was to describe the functional outcomes and LOS of patients in the neuro/trauma ICU involved in a structured upright sitting mobility program with PT. We hypothesized that there would be a statistically significant difference between functional outcome measures for those in the structured mobility program from PT on the first day of upright sitting to the day of ICU discharge. In addition, we identified a retrospective cohort of patients who were treated prior to the introduction of the structured mobility program yet met the program’s inclusion criteria. Our secondary hypothesis was that there would be a statistically significant reduction in ICU LOS for participants in the structured mobility programs.
Methods
Study Design and Participants
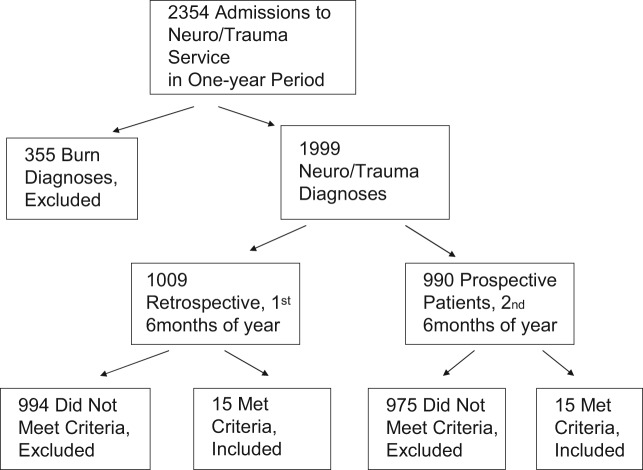
This bidirectional case–control study was conducted at a large level 1 Trauma University Hospital located in the metropolitan Chicago area (Figure 1 ), in the late 1990s. For the 6-month prospective arm of the study, a physical therapist was present at daily multidisciplinary Neuro Trauma rounds. At those team rounds, each patient was reviewed for potential inclusion in the study and activity advancement. All patients admitted to the Neuro Trauma unit were considered for inclusion. The initial inclusion criteria were 3-fold: participants were (1) admitted through the neuro/trauma services, (2) assigned a Glasgow Coma Score (GCS) of ≤12 by the admitting physician within 24 hours after injury/insult by assigning a severe (score 3-5) or moderately severe (score 6-12) injury categorization,12 and (3) a physician’s referral for PT evaluation and treatment.
Figure 1.
Flow diagram of admissions and patients who met the criteria in a 1-year time period.
Patients meeting the initial inclusion criteria then had to pass certain further judgment criteria in order to be appropriate for advancement to an upright sitting position. These judgment criteria included the following: (1) vital signs must be stable as defined by systolic blood pressure between 90 and 200 mm Hg, heart rate between 40 and 130 beats/min at rest, respiratory rate between 5 and 40 breaths/min, and pulse oximetry oxygen saturation of >88%, (2) specific activity orders from the primary service physician to increase activity as tolerated or to sit up at the side of the bed, and (3) no other specific contraindications to activity advancement such as an unstable fracture, elevated intracranial pressure, or pharmacologically induced sedation and paralysis.
Patients with evidence of radiographic, computed tomography (CT), magnetic resonance imaging (MRI), or clinical examination of extremity, spinal or pelvic fracture that inhibited or delayed initiation of mobilization to an upright sitting position remained on bed rest. Patients requiring intracranial pressure bolt monitoring were initially not advanced to sitting due to concerns regarding interrupting the device position and elevated intracranial pressures. Patients whose monitoring equipment prevented upright sitting (eg, femoral arterial line) were initially excluded if this device was in place at the time of determination of readiness for upright sitting, and/or upright sitting would have caused harm to the patient or the equipment.
In addition, the principal investigator (PI) performed a review of all medical records from a sample of convenience of neurotrauma admissions in the 6 months prior to the prospective group. During the time of the retrospective group, a physical therapist was involved in neurotrauma rounds on a weekly basis without defined judgment criteria for consulting PT or activity advancement. The retrospective patients' charts were reviewed with the same inclusion/exclusion criteria as the prospective group. As it was a retrospective review, none had been involved in a structured mobility program yet each had received PT. Only LOS data were collected for this group as functional assessment would have been unreliable.
A total of 15 individuals were included in each of the prospective and retrospective groups. Patients who did not qualify for the study included those who were discharged from the ICU prior to achieving appropriate status to upright sit or those who expired. None of the participants was assisted to upright sitting prior to PT intervention. Description of the characteristics of the individuals can be found in Table 1 . In addition to the diagnoses listed, patients also incurred diagnoses such as traumatic amputations, liver lacerations, pneumothorax, and vein ligation. Institutional Review Board approval was obtained for this study.
Table 1.
Descriptive Characteristics of Participants Involved in Both the Retrospective Unstructured Group and the Prospective Structured Groupa
| Structured Mobility Program (n = 15) | Retrospective Review (n = 15) | |
|---|---|---|
| Gender | 3 female, 12 male | 5 female, 10 male |
| Age (ave years ± SD) | 48 ± 20.6 | 51 ± 17.7 |
| Age range | 18-79 | 24-72 |
| Diagnosis | ||
| Subdural hematoma | 10 | 10 |
| Extradural hematoma | 0 | 1 |
| Cerebral edema | 1 | 1 |
| Pneumocephalus | 0 | 1 |
| Hydrocephalus | 0 | 1 |
| Cerebellar infarct | 0 | 1 |
| Spinal cord injury | 0 | 1 |
| Spine subluxation | 0 | 1 |
| Mechanism of injury | ||
| Motor vehicle collision | 5 | 8 |
| Fall | 5 | 2 |
| Pedestrian injury | 3 | 3 |
| Gun shot wound | 1 | 1 |
| Assault | 1 | 1 |
a Participants may have had multiple diagnoses.
Prospective Structured Mobility Group Procedures
After having met the inclusion and judgment criteria, participants were evaluated by the PI, a physical therapist, and assigned an initial FIM score.13 The FIM allows assessment of 7 levels of dependence on assistance required for individuals involved in rehabilitation.
Appropriateness for upright sitting was determined from aforementioned judgment criteria. If the participants were deemed unstable by not meeting the judgment criteria, they awaited advancement of upright sitting activity. During this interim period, the participants continued to be treated by PT daily with progression of active involvement in range of motion and strengthening exercises as well as bed mobility training. If they met the judgment criteria, the participant was considered stable and their activity was advanced to upright sitting. To achieve upright sitting, participants were assisted from supine to an upright sitting position with a trunk and hip angle of approximately 90°. The lower extremities were placed in a dependent position off the side of bed with foot support from the floor or supportive platform surface. Data regarding the amount of assistance required, the duration of tolerance to upright sitting and vital signs were recorded.
Ongoing activity was progressed according to physician’s orders, participant tolerance, vital signs, and the physical therapist’s determination of appropriateness. The FIM scores were recorded within 24 hours of the participant’s discharge from the ICU. The FIM scores were also recorded on the date of hospital discharge if the participant had been admitted to a hospital unit. Length of stay data were recorded for ICU stay and hospital stay.
Data Analysis
Statistical Analysis, Functional Outcomes, and Prospective Structured Mobility Group
The FIM scores were collected for the structured mobility group and analyzed to determine whether there was a difference in FIM scores in the same participant from upright sitting to ICU discharge. This data was analyzed using Rasch analysis, descriptive statistics, and paired t test analysis.
Rasch analysis allows statistical analysis of ordinal data such as the GCS and the FIM.14–16 Each item on the FIM was calibrated and averaged according to the 7 levels of dependency. Using logits, paired t test analysis was performed between the 2 groups of data on the same participants. The FIM scores were compared from the first upright sitting to participant discharge from the ICU setting.
Statistical Analysis, LOS, and Prospective and Retrospective Groups
Length of stay in number of days was calculated and was descriptively analyzed for those participants in the prospective structured mobility group. The LOS data were also collected from 15 patients in a retrospective review. These patients also met the inclusion criteria yet were not subjected to the structured mobility program nor FIM scoring. The levels of activity of these patients were not progressed according to specific structured guidelines. In this manner, the determination of readiness for mobility for the retrospective groups varied between therapists and patients. Independent “t” test analysis was performed to determine whether there was a statistically significant difference between the 2 groups on LOS measured at the .05 level of significance.
Results
Both groups had 53% moderately severely GCS-rated participants with a score of between 9 and 12 and 47% severely GCS-rated patients with a score of ≤8.
Functional Outcomes—Prospective Structured Mobility Group
For the participants in the structured mobility program, we compared FIM scores from first day of upright sitting and the day of ICU discharge. Table 2 displays the item difficulties from the Rasch analysis compared between those 2 time points. Rasch analysis allows statistical analysis of ordinal data, data that are ranked in a specific order yet not necessarily in equal intervals, to be converted into interval, or equidistant, data. The units, or logits, are assigned to each item on the FIM and the 7 levels of dependency ratings were then transferred to a linear scale.
Table 2.
Functional Independence Measure Item Difficulty in Rasch Logits With Standard Errora
| Items Listed Most Difficult to Least Difficult | Measure (Logits) | Error |
|---|---|---|
| Stairs | 1.87 | 0.39 |
| Walking | 1.38 | 0.32 |
| Bladder | 0.39 | 0.25 |
| Tub transfer | 0.20 | 0.25 |
| Bowel | 0.20 | 0.25 |
| Dressing—upper extremity | 0.14 | 0.25 |
| Dressing—lower extremity | 0.14 | 0.25 |
| Toileting | 0.14 | 0.25 |
| Toilet transfers | 0.07 | 0.25 |
| Bathing | −0.11 | 0.25 |
| Eating | −0.18 | 0.25 |
| Grooming | −0.24 | 0.25 |
| Bed transfer | −0.36 | 0.25 |
| Memory | −0.42 | 0.25 |
| Problem solving | −0.49 | 0.25 |
| Social interaction | −0.79 | 0.24 |
| Comprehension | −0.85 | 0.24 |
| Expression | −1.09 | 0.24 |
a Stair climbing was found to be the most difficult item and expression of the least difficult item.
The most difficult item for participants to accomplish was stairs, defined as the “ability to ascend and descend 12 to 14 stairs indoors safely.”17,18 This was followed by walking. The motor item the participants found easiest was bed transfers. The easiest of the cognitive components was expression, defined as the “clear expression of language within the cognitive components.” The easiest motor item, bed transfers, fell at the same level of difficulty as memory and problem solving. Testing the fit of the items by the manner in which they separate from each other, the item separation was good, indicated by a separation index of 2.47, where a value of greater than 2.0 is desirable. The item with the highest outfit or unexpected response was expression followed by the remaining cognitive items such as social interaction, memory, comprehension, and problem solving.
Using the logit values obtained, it was found that 6 of the 15 participants in the structured mobility group did not show improvement in functional performance as measured by the FIM. All of the logit values were compared between first upright sitting to ICU discharge. Of the 6 participants, 4 presented with a cluster at the same low level of functioning from first dangling and ICU discharge. Of the 6, 2 clustered again at a higher level of functioning. The remaining 9 participants all improved in functional performance on their FIM score items from first dangling to ICU discharge. A person separation of 2.64 and a reliability score of .87 were good, indicating a more heterogeneous group of participants studied. The mean ordinal FIM score was less at first upright sitting versus ICU discharge. The t test indicated that a significant difference occurred between functional performance from first upright sitting to ICU discharge for those participants in the structured mobility program (P < .005).
Length of Stay
All LOS scores were reduced in the structured mobility group, however the results on independent t tests were not significantly different (Table 3 ).
Table 3.
Comparison of Length of Stay Between Structured Prospective and Unstructured Retrospective Groups in Number of Days
| Period of Length of Stay Measured | Retrospective Group Mean in Days (n = 15) | Structured Group Mean in Days (n = 15) | P Value |
|---|---|---|---|
| Admission to ICU discharge | 21.9 | 16.4 | .445 |
| PT evaluation to ICU discharge | 16.9 | 11.5 | .355 |
| Admission to first upright sitting | 13.3 | 12.7 | .471 |
| First upright sitting to ICU discharge | 8.6 | 4.1 | .300 |
| Admission to hospital discharge | 26.4 | 20.5 | .460 |
| First upright sitting to hospital discharge | 13.5 | 9.0 | .391 |
Abbreviation: ICU, intensive care unit.
Discussion
During a structured mobility program in a neurotrauma unit, we found a significant difference in functional performance from first upright sitting to ICU discharge (P < .005). The improvements found may have occurred due to the comprehensive ICU treatment which included the PT-structured mobility program, the interaction of multiple disciplines, and the intensive focus on sitting and mobility. Indeed, other studies have found that the implementation of a structured mobility program utilizing a mobility protocol compared to usual care has shown decreased LOS in the medical ICU.4 Such a study also found that PT services were more likely to be utilized during the ICU stay when a structured mobility program was in place. Hospital costs were also lower for those in such a program.
According to the scores from the GCS, the participants in this study were severely and moderately/severely injured. Because of this, it was anticipated that the participants would not be able to perform the more difficult items on the FIM. In a study of functional outcomes of 328 patients with traumatic brain injury, only 2 participants (0.6%) were found to be independent in all 18 of the FIM functional items, upon discharge.17 In our study, advanced endurance and strength activities such as stairs and walking were found, as anticipated, to be most difficult if at all able to be performed. Of the 15 participants in the structured mobility group, 6 (40%) did not improve on the FIM scale. Of these 6 participants, 4 scored at the lowest level of functioning on the scale and were admitted with GCS scores all within the severely impaired category. Although the FIM was not originally intended to measure functional changes in the ICU and may lack sensitivity in this population, we found it the most reliable, valid, and easy to utilize tool to study functional outcomes.18–29
Comparing patients in the retrospective unstructured and prospective structured groups, the mean LOS from first upright sitting to ICU discharge was 8.6 days and 4.1 days, respectively. This difference in LOS did not reach statistical significance. Foremost, the study was underpowered with a small sample. Other contributing factors could include priority medical needs, early stress on the system of a participant, and severity of injury. However, the difference in mean values may indicate a potential cost-saving benefit from a structured mobility program in the neurological ICU to the patient and the hospital in terms of LOS. The decreased LOS was anticipated as intervention in mobility in the ICU has long been thought to be beneficial toward the functional outcomes of the patient and to expedite recovery.7,11,30,31 The integration of PT as a requisite discipline in the progression of activity and a contributor to decreasing LOS supports the use of this profession in the ICU setting.
Variations in patient background, diagnosis, and interaction with different medical disciplines may have all had influence on the functional outcomes and LOS of the patients within this study. Due to ethical considerations of withholding treatment, this study also utilized a small convenience sample of patients seen in the ICU.32 In attempts to create a homogenous sample, a large percentage of patients who were admitted were excluded from the study. This may have created an underpowered study with a small sample size.
The results from this study suggest favorable functional outcomes for participants involved in a structured mobility program with PT in the neuro/trauma ICU. There was a significant difference between functional performance from first upright sitting to ICU discharge for those patients in the structured mobility program (P < .005). While the data for LOS suggest a trend toward a decreased LOS for the structured mobility group, we did not find a significant difference.
The differences in functional outcomes after the implementation of a structured mobility program cannot be assumed to be due solely to PT intervention. It is important to note that although this study focused on PT intervention for the patient in the ICU, many services were involved with the patients. Therefore, the combination of treatments may beneficially affect the patient outcomes.9 Furthermore, discussions regarding the optimal dosage of PT and advancement of activity in the ICU are widely variable.14–16 Future studies concerning the applicability of more sensitive functional tools and the combined benefits of disciplines integral to the functional advancement of the patient in the ICU may further support PT as an important intervention within the acute ICU population.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Norris C, Jacobs P, Rapoport J, Hamilton S. ICU and non-ICU cost per day. Can J Anaesth. 1995;42(3):192–196 [DOI] [PubMed] [Google Scholar]
- 2. Engleman RM. Mechanisms to reduce hospital stays. Ann Thorac Surg. 1996;61(2 suppl):26–29 [DOI] [PubMed] [Google Scholar]
- 3. Kalra L. The influence of stroke unit rehabilitation on functional recovery from stroke. Stroke. 1994;25(4):821–825 [DOI] [PubMed] [Google Scholar]
- 4. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243 [DOI] [PubMed] [Google Scholar]
- 5. Patman S, Jenkins S. Physiotherapy does not prevent, or hasten recovery from, ventilator-associated pneumonia in patients with acquired brain injury. Intensive Care Med. 2009;35(2):258–265 [DOI] [PubMed] [Google Scholar]
- 6. Hodgin KE, Nordon-Craft A, McFann KK, Mealer ML, Moss M. Physical therapy utilization in intensive care units: results from a national survey. Crit Care Med. 2009;37(2):561–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sciaky A. Mobilizing the intensive care unit patient: pathophysiology and treatment. Phys Ther Practice. 1994;3(2):69–80 [Google Scholar]
- 8. Sjostrand T. Determination of changes in the intrathoracic blood volume in man. Acta Physiol Scand. 1951;22(2-3):114–128 [DOI] [PubMed] [Google Scholar]
- 9. Perme C, Chandrashekar R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am J Crit Care. 2009;18(3):212–221 [DOI] [PubMed] [Google Scholar]
- 10. Spencer WA, Vallbona C, Carter RE. Physiologic concepts of immobilization. Arch Phys Med Rehabil. 1965;46:89–100 [PubMed] [Google Scholar]
- 11. Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European respiratory society and European society of intensive care medicine task force on physiotherapy for critically ill patients. Intensive Care Med. 2008;34(7):1188–1199 doi: 10.1007/s00134-008-1026-7 [DOI] [PubMed] [Google Scholar]
- 12. Marion DW, Carlier PM. Problems with initial Glasgow Coma Scale assessment caused by prehospital treatment of patients with head injuries: results of a national survey. J Trauma. 1994;36(1):89–95 [DOI] [PubMed] [Google Scholar]
- 13. Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993;74(6):566–573 [DOI] [PubMed] [Google Scholar]
- 14. Merbitz C, Morris J, Grip J. Ordinal scales and foundations of misinference. Arch Phys Med Rehabil. 1989;70(4):308–312 [PubMed] [Google Scholar]
- 15. Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the functional independence measure. Arch Phys Med Rehabil. 1994;75(2):127–132 [PubMed] [Google Scholar]
- 16. Bigsteps (version 2.71). 1998. 58355 Kimbark Avenue Chicago, IL: Mesa Press; 60637–1609 [Google Scholar]
- 17. Whitlock JA, Hamilton BB. Functional outcome after rehabilitation for severe traumatic brain injury. Arch Phys Med Rehabil. 1995;76(12):1103–1112 [DOI] [PubMed] [Google Scholar]
- 18. Functional Independence Measure, Copyright c 1993. Uniform Data System for Medical Rehabilitation (UDSMRSM). All rights reserved. Reprinted with permission of the UDSMR, University at Buffalo, 232 Parker Hall, 3435 Main Street, Buffalo, NY 14214.
- 19. Fiedler RC, Granger CV, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of first admissions for 1994. Am J Phys Med Rehabil. 1996;75(2):125–129 [DOI] [PubMed] [Google Scholar]
- 20. Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin FS. Advances in functional assessment for medical rehabilitation. Topic Geriatr Rehabil. 1986;1(3):59–74 [Google Scholar]
- 21. Emhoff TA, McCarthy M, Chushman M, Garb JL, Valenziano C. Functional scoring of multi-trauma patients: who ends up where? J Trauma. 1991;31(9):1227–1232 [DOI] [PubMed] [Google Scholar]
- 22. Marciniak CM, Sliwa JA, Spill G, Heinemann AW, Semik PE. Functional outcome following rehabilitation of the cancer patient. Arch Phys Med Rehabil. 1996;77(1):54–57 [DOI] [PubMed] [Google Scholar]
- 23. Mortifee PRS, Busser J, Anton HA. The Performance of a limited set of items from the functional independence measure for use in acute trauma care and rehabilitation. Arch Phys Med Rehabil. 1996;77(5):436–439 [DOI] [PubMed] [Google Scholar]
- 24. Segal ME, Ditunno JF, Staas WE. Interinstitutional agreement of individual Functional Independence Measure (FIM) items measured at two sites on one sample of SCI Patients. Paraplegia. 1993;31(10):622–631 [DOI] [PubMed] [Google Scholar]
- 25. Whitlock JA, Hamilton BB. Functional outcome after rehabilitation for severe traumatic brain injury. Arch Phys Med Rehabil. 1995;76(12):1103–1112 [DOI] [PubMed] [Google Scholar]
- 26. George ER, Scholten DJ, Buechler CM, Jordan-Tibbs J, Mattice C, Albrecht RM. Failure of methylprednisolone to improve the outcome of spinal cord injuries. Am Surg. 1995;61(8):659–664 [PubMed] [Google Scholar]
- 27. Granger CV, Cotter AC, Hamilton BB, Fiedler RC, Hens MM. Functional assessment scales: a study of persons with multiple sclerosis. Arch Phys Med Rehabil. 1990;71(11):870–875 [PubMed] [Google Scholar]
- 28. Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-Level Functional Independence Measure (FIM). Scand J Rehabil Med. 1994;26(3):115–119 [PubMed] [Google Scholar]
- 29. Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993;74(6):566–573 [DOI] [PubMed] [Google Scholar]
- 30. Baggerly J. Rehabilitation of the adult with head trauma. Nurs Clin North Am. 1986;21(4):577–587 [PubMed] [Google Scholar]
- 31. Gordon DL, Reinstein L. Rehabilitation of the trauma patient. Am Surg. 1979;45(4):223–227 [PubMed] [Google Scholar]
- 32. Elliott D, Mudaliar Y, Kim C. Examining discharge outcomes and health status of critically ill patients: some practical considerations. Intensive Crit Care Nurs. 2004;20(6):366–377 [DOI] [PubMed] [Google Scholar]