Abstract
Aims
The goal of our study is to investigate the combined contribution of 10 genetic variants to diabetes susceptibility.
Methods
Bibliographic databases were searched from 1970 to Dec 2012 for studies that reported on genetic association study of diabetes. After a comprehensive filtering procedure, 10 candidate gene variants with informative genotype information were collected for the current meta-anlayses. Using the REVMAN software, odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to evaluate the combined contribution of the selected genetic variants to diabetes.
Results
A total of 37 articles among 37,033 cases and 54,716 controls were involved in the present meta-analyses of 10 genetic variants. Three variants were found to be significantly associated with type 1 diabetes (T1D): NLRP1 rs12150220 (OR = 0.71, 95% CI = 0.55–0.92, P = 0.01), IL2RA rs11594656 (OR = 0.86, 95% CI = 0.82–0.91, P<0.00001), and CLEC16A rs725613 (OR = 0.71, 95% CI = 0.55–0.92, P = 0.01). APOA5 −1131T/C polymorphism was shown to be significantly associated with of type 2 diabetes (T2D, OR = 1.27, 95% CI = 1.03–1.57, P = 0.03). No association with diabetes was showed in the meta-analyses of other six genetic variants, including SLC2A10 rs2335491, ATF6 rs2070150, KLF11 rs35927125, CASQ1 rs2275703, GNB3 C825T, and IL12B 1188A/C.
Conclusion
Our results demonstrated that IL2RA rs11594656 and CLEC16A rs725613 are protective factors of T1D, while NLRP1 rs12150220 and APOA5 −1131T/C are risky factors of T1D and T2D, respectively.
Introduction
The prevalence of diabetes is soaring up in the recent decades. The global number of diabetes patients was 173 million in 2002 and will increase to 350 million by 2030. As a group of metabolic diseases characterized with high blood sugar, most diabetes is caused by either a lack of insulin for type 1 diabetes (T1D) or a blockage in the insulin signaling pathway for type 2 diabetes (T2D). The classical symptoms of diabetes consist of polyuria, polydipsia, polyphagia and weight loss. Diabetes also causes damages to blood vessels and capillaries that may eventually lead to coronary heart diseases and blindness, respectively.
T1D and T2D are two major types of diabetes [1]. Microbial exposures and sex hormones together with lifestyle factors have been shown to be important to the development of this complex disease [2], [3]. Besides environmental factors, twin studies have demonstrated a strong heritability for diabetes [4], [5] and insulin related phenotypes [6]–[8]. A handful of candidate genes have been found for both the risk and complex traits of the two major types of diabetes [3], [9]–[12].
T1D is an autoimmune disease. Little or no insulin is produced by pancreatic beta cells that may be mistakenly attacked after an infection or some other triggers. The present meta-analyses of T1D focus on four immunomodulatory genes including IL2RA, NLRP1, IL12B and CLEC16A. IL2RA gene encodes the α-chain of IL-2 receptor (IL-2R) complex which acts as an important modulator to regulate T-cell immune response [13]. NLRP1 gene encodes a member of the Ced-4 family of apoptosis proteins that can stimulate innate immunity [14]. IL12B gene encodes a subunit of an important immunomodulatory cytokine, IL-12. IL-12 induces production from NK and T cells of interferon γ (IFN-γ) which favors Th1 cell differentiation [15]. CLEC16A encodes C-type lectin domain family 16 (CLEC16A) protein highly expressed on B-lymphocytes, natural killer (NK) and dendritic cells [16].
The impairment of insulin signaling in T2D is complex. Insulin signaling is involved in both glucose and lipid metabolism. In the present meta-analyses of T2D, we selected 2 genes in glucose metabolism (SLC2A10 and CASQ1), 2 genes in lipid metabolism (APOA5 and KLF11), and 2 genes in signal transduction (ATF6 and GNB3). SLC2A10 gene encodes a member of the facilitative glucose transporter family with an effect on maintaining glucose homeostasis. CASQ1 gene encodes acidic glycoprotein calsequestrin 1 (CASQ1) that is a calcium storage protein and calcium is considered to regulate the expression of the insulin-responsive glucose transporter GLUT4 [17]. APOA5 is located on human chromosome 11q23, in the APOA1/APOC3/APOA4 gene cluster [18]. KLF11 encodes Kruppel-like factor 11 with the function of regulating hepatic lipid metabolism [19]. ATF6 encodes UPR transducer unfolded protein that is related to the endoplasmic reticulum stress in the β-cell pathogenesis of type 2 diabetes [20]. GNB3 encodes the β3 subunit of hetero-trimeric G proteins in insulin signaling [21].
Associations between single-nucleotide polymorphisms (SNPs) of the above 10 genes and diabetes (including T1D and T2D) have been reported in different ethnic populations [16], [22]–[57]. Here we performed a series of meta-analyses for these SNPs whose allelic frequencies are often substantially different among multiple ethnic populations. The goal of our study is to evaluate the overall contribution of these SNPs to diabetes susceptibility in combined populations using a meta-analysis approach.
Materials and Methods
Search Strategy and Study Selection
An initial search was performed through online databases including PubMed, Embase, SpingerLink, Web of Science, Chinese National Knowledge Infrastructure (CNKI), and Wanfang. The keywords comprise the terms including “diabetes” together with “SNP” or “polymorphism” or “variants” or “mutation”. The selection of studies in our meta-analysis was abided by the criteria as follows: (1) case-control studies; (2) selected studies have sufficient data to calculate ORs with the corresponding 95% CIs; (3) every polymorphism has at least 3 independent datasets from the retrieved articles; (4) selected polymorphisms have not been addressed in previous meta-analysis of diabetes. Finally, the current meta-analysis involved a total of 10 genetic variants comprising NLRP1 rs12150220, IL2RA rs11594656, CLEC16A rs725613,APOA5 −1131T/C, SLC2A10 rs2335491, ATF6 rs2070150, KLF11 rs35927125, CASQ1 rs2275703, GNB3 C825T, and IL12B 1188A/C.
Statistical Analysis
All the analyses were performed in Review Manager (version 5.0, The Cochrance Collaboration [58]). The combined ORs and the corresponding 95% CIs were calculated and demonstrated in the forest plots using the fixed or the random effects model. Heterogeneity was measured in our meta-analysis using Cochran’s Q and the inconsistency index (I2) statistic [59]. Funnel plots were used to detect whether there were obvious publication bias among the involved studies. An I2 value of equal to or greater than 50% indicates a substantial heterogeneity among the studies in the meta-analysis that used a random-effect model for the analysis. For I2 value less than 50%, a fixed-effect model will be applied for the meta-analysis. The combined ORs and the corresponding 95% CIs were calculated using the fixed-effect model or the random-effect model if I2 is less than 50%. P values less than 0.05 were considered to be significant.
Results
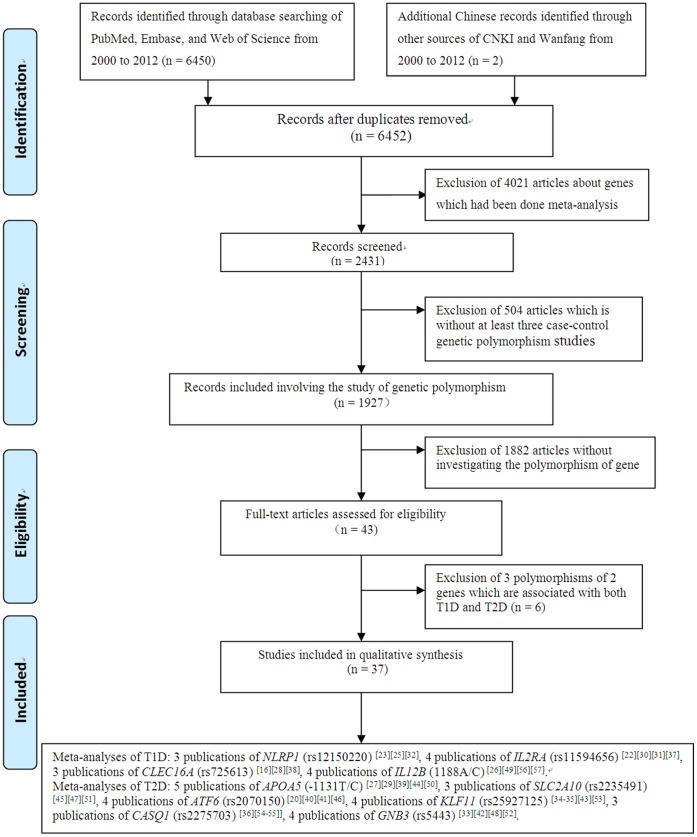
As shown in Figure 1, our initial search for the genetic studies of diabetes retrieved 6,452 articles from PubMed, Embase, Web of Science, CNKI and Wanfang from 2000 to 2012. Among them, 4,021 studies were involved with genes reported in previous meta-analyses and thus discarded for further analysis. A total of 504 articles were again filtered out because they failed to accumulate at least three independent genotypic datasets for the same genetic variants. Among the rest 1,927 studies, 1,882 studies with unconcerned SNPs were removed. At last, there were 42 case-control studies from 37 articles (including 35 articles in English and 2 in Chinese) for the current meta-analyses. There were four SNPs of T1D (Table 1) and six SNPs of T2D (Table 2) involved in our present study.
Figure 1. Flow diagram of selecting studies for meta-analysis.
Table 1. Characteristics of individual T1D studies in the meta-analyses.
| Gene | SNP | Year | Author | Ethnic Group | Case/Control (n) | Allele 1 (Case/Control) | Allele 2 (Case/Control) |
| IL2RA | rs11594656 | T | A | ||||
| 2007 | Christopher E Lowe | Caucasian | 2874/2484 | 4482/3726 | 1266/1242 | ||
| 2007 | Christopher E Lowe | Caucasian | 5259/6809 | 8199/10248 | 2319/3370 | ||
| 2008 | Deborah J Smyth | Caucasian | 8064/9339 | 12548/14083 | 3580/4595 | ||
| 2009 | Eiji Kawasaki | Japanese | 881/606 | 1715/1175 | 47/37 | ||
| 2012 | M. Fichna | Caucasian | 445/671 | 701/994 | 189/348 | ||
| NLRP1 | rs12150220 | T | A | ||||
| 2009 | NF Magitta | Caucasian | 1067/3177 | 929/2987 | 1205/3367 | ||
| 2010 | A. PONTILLO | Brazilian | 196/192 | 248/255 | 144/129 | ||
| 2011 | Magdalena Zurawek | Caucasian | 221/254 | 230/270 | 212/238 | ||
| IL12B | 1188 A/C | A | C | ||||
| 2002 | Lorenza Nistico | Caucasian | 470/544 | 662/787 | 278/301 | ||
| 2002 | RM McCormack | Caucasian | 120/330 | 194/533 | 46/127 | ||
| 2005 | José L. Santiago | Caucasian | 300/516 | 453/773 | 147/259 | ||
| 2010 | A.E.Altinova | Turks | 91/87 | 133/120 | 49/54 | ||
| CLEC16A | rs725613 | A | C | ||||
| 2007 | Hakon Hakonarson | Caucasian | 561/1143 | 785/1395 | 337/891 | ||
| 2009 | M Zoledziewska | Caucasian | 1037/1706 | 969/1473 | 1105/1939 | ||
| 2009 | Xiao pan Wu | Chinese | 205/422 | 352/643 | 58/201 |
Table 2. Characteristics of individual T2D studies in the meta-analyses.
| Gene | SNP | Year | Author | Ethnic Group | Case/Control (n) | Allele 1 (Case/Control) | Allele 2 (Case/Control) |
| APOA5 | −1131 T/C | T | C | ||||
| 2005 | Sheng kai Yan | Chinese | 172/155 | 231/224 | 113/86 | ||
| 2006 | P. J. Talmud | Caucasian | 142/2438 | 273/4401 | 11/295 | ||
| 2007 | Guang hua Zhai | Chinese | 71/152 | 81/214 | 61/90 | ||
| 2008 | Xue feng Li | Chinese | 256/340 | 322/468 | 190/212 | ||
| 2008 | Yan Qiao | Chinese | 154/206 | 222/313 | 86/99 | ||
| SLC2A10 | rs2235491 | G | A | ||||
| 2005 | Karen L. Mohlke | Caucasian | 784/401 | 1476/746 | 92/56 | ||
| 2005 | Jennifer L Bento | Caucasian | 296/305 | 568/592 | 24/18 | ||
| 2006 | W. H. Lin | Chinese | 375/377 | 691/683 | 59/71 | ||
| ATF6 | rs2070150 | C | G | ||||
| 2006 | Farook Thameem | Pima Indian | 561/399 | 913/626 | 209/172 | ||
| 2007 | Steven J. R. Meex | Caucasian | 367/377 | 670/693 | 64/61 | ||
| 2007 | Winston S. Chu | Caucasian | 191/188 | 364/350 | 18/26 | ||
| 2011 | Cheng Hu | Chinese | 1892/1808 | 1181/1088 | 2603/2528 | ||
| KLF11 | rs35927125 | A | G | ||||
| 2005 | Bernadette Neve | Caucasian | 313/313 | 562/517 | 64/109 | ||
| 2006 | Jose C. Florez | Caucasian | 469/468 | 850/854 | 88/82 | ||
| 2006 | Jose C. Florez | Caucasian | 504/503 | 906/910 | 102/96 | ||
| 2006 | Jose C. Florez | Canadian | 111/109 | 195/188 | 27/30 | ||
| 2006 | Jose C. Florez | Caucasian | 1207/1198 | 2129/2103 | 285/293 | ||
| 2006 | Jose C. Florez | Caucasian | 1000/997 | 1789/1779 | 211/215 | ||
| 2008 | T. Tanahashi | Japanese | 925/893 | 1850/1786 | 0/0 | ||
| 2008 | Lijun Ma | Pima Indian | 1455/1816 | 2780/3457 | 130/175 | ||
| CASQ1 | rs2275703 | A | C | ||||
| 2004 | Mao Fu | Caucasian | 145/358 | 90/305 | 200/411 | ||
| 2004 | Swapan Kumar Das | Caucasian | 190/119 | 205/117 | 175/121 | ||
| 2007 | Thomas Sparsø | Caucasian | 1391/4575 | 1452/4841 | 1330/4309 | ||
| GNB3 | rs5443 | C | T | ||||
| 2005 | Jawad G. Kiani | Arab | 256/254 | 178/246 | 334/262 | ||
| 2006 | G. Andersen | Caucasian | 1358/4723 | 1855/6574 | 861/2872 | ||
| 2007 | Tetsuo Hayakawa | Japanese | 427/388 | 445/338 | 409/388 | ||
| 2008 | Makoto Daimon | Japanese | 230/2576 | 259/2740 | 201/2712 |
No evidence of statistical heterogeneity was observed for 7 SNPs (Figures 2 and 3, and Table 3), including rs11594656 of IL2RA gene (I2 = 0%), rs12150220 of NLRP1 gene (I2 = 0%), 1188A/C of IL12B gene (I2 = 0%), −1131T/C of APOA5 gene (I2 = 1%), rs2335491 of SLC2A10 gene (I2 = 0%), rs2070150 of ATF6 (I2 = 0%), and rs35927125 of KLF11 gene (I2 = 7%). No visual bias was showed in the meta-analyses of these 7 SNPs (Figure 4 and Table 3). Our data also demonstrated a significant heterogeneity of the rest 3 SNPs that comprise rs725613 of CLEC16A gene (I2 = 69%), rs2275703 of CASQ1 gene (I2 = 65%), and C825T of GNB3 gene (I2 = 82%). Therefore random-effect tests were applied for the meta-analyses of the above 3 SNPs. Their funnel plots were demonstrated in Figure 4 and no visual bias was observed for the 3 meta-analyses.
Figure 2. Forest plots of the association studies between four SNPs and T1D.
Figure 3. Forest plots of the association studies between six SNPs and T2D.
Table 3. Additional characteristics of individual T1D and T2D studies in the meta-analyses.
| T1D | Gene | SNP | Model | Heterogeneity index | P values |
| IL2RA | rs11594656 | Fixed effectmodel | 0% | <0.00001 | |
| NLRP1 | rs12150220 | Fixed effectmodel | 0% | 0.04 | |
| IL12B | 1188 A/C | Fixed effectmodel | 0% | 0.86 | |
| CLEC16A | rs725613 | Random effectmodel | 69% | 0.01 | |
| T2D | Gene | SNP | Model | Heterogeneity index | P values |
| APOA5 | −1131 T/C | Fixed effectmodel | 1% | 0.03 | |
| SLC2A10 | rs2235491 | Fixed effectmodel | 0% | 0.48 | |
| ATF6 | rs2070150 | Fixed effectmodel | 0% | 0.26 | |
| KLF11 | rs35927125 | Fixed effectmodel | 7% | 0.27 | |
| CASQ1 | rs2275703 | Random effectmodel | 65% | 0.53 | |
| GNB3 | rs5443 | Random effectmodel | 82% | 0.82 |
Figure 4. Funnel plots of the studies involved in the 10 meta-analyses.
Meta-analysis of rs12150220 of NLRP1 gene was involved with 3 studies [23], [25], [32] among 833 T1D cases and 3,623 controls. As shown in Figure 2, our result indicated that rs12150220 of NLRP1 gene was significantly associated with T1D risk in the Caucasian and Brazilian populations (the overall OR = 0.71, 95% CI = 0.55–0.92, P = 0.01). Meta-analysis of rs11594656 of IL2RA gene among 17,523 T1D cases and 19,909 controls [22], [30], [31], [37] indicated that rs11594656 of IL2RA gene was significantly associated with T1D risk in the Caucasian and Japanese populations (Figure 2, the overall OR = 0.86, 95% CI = 0.82–0.91, P<0.00001). Meta-analysis of rs725613 of CLEC16A gene [16], [28], [38] included 1,803 T1D cases and 3,271 controls. As shown in the Figure 2, there was significant association between rs725613 of CLEC16A gene and T1D in Caucasian and Chinese populations (the overall OR = 0.71, 95% CI = 0.55–0.92, P = 0.01). Meta-analysis of −1131T/C of APOA5 gene [27], [29], [39], [44], [50] among 795 T2D cases and 3210 controls indicated that −1131T/C of APOA5 gene was associated with T2D in Chinese and Caucasian populations (Figure 3, the overall OR = 1.27, 95% CI = 1.03–1.57, P = 0.03). For the rest 6 SNPs, our meta-analyses were unable to find significant associations of them with T1D or T2D.
Discussion
In the present study, a comprehensive systematic overview of genetic association studies was performed for the susceptibility of T1D and T2D. We scrutinized all the candidate case-control studies to identify the eligible SNPs with at least three independent datasets. Our meta-analyses of 10 polymorphisms showed significant evidence for 3 T1D-associated SNPs (NLRP1 rs12150220, IL2RA rs11594656, and CLEC16A rs725613) and 1 T2D-associated SNP (APOA5 −1131T/C). Our meta-analyses were unable to find significant associations of the rest 6 SNPs with T1D or T2D. Moreover, power analysis showed that there might be a lack of power for the meta- analysis of SLC2A10 rs2335491 (1,455 cases and 1,083 controls, 39%) under a moderate risk of diabetes (OR = 1.2). These might partly explain our failure to observe significant results for the meta-analyses of some polymorphisms.
After Bonferroni correction, only the association of SNP rs11594656 with T2D remains significant. However, false discovery rate (FDR) test, a less conservative correction for multiple hypothesis testing, shows that the q values are 5.11E-5 for IL2RA rs11594656, 0.051 for NLRP1 rs12150220, 0.026 for CLEC16A rs725613, and 0.051 for APOA5 −1131T/C. This suggests the robustness of our positive results in the meta-analyses, although we can’t exclude a chance of false positive results for NLRP1 rs12150220, CLEC16A rs725613 and APOA5 −1131T/C. Sensitivity analysis demonstrated there were no significant differences of four significant genetic variants after exclusion, suggesting that the results of our meta-analyses was robust. In addition, we have performed a comprehensive analysis for the Fst values of the involved SNPs. Our results show there are moderate ethnic differences for ATF6 rs2070150 (Fst = 0.13), although there are minimal heterogeneity among the involved studies from different ethnic groups (I2 = 0). And KLF11A rs35927125 is monomorphic in Asians, however, its minor allele frequency in Caucasian populations ranges from 8.8–12.2% (Fst = 0.0232). On the contrary, there were little ethnic difference for CLEC16A rs725613 and GNB3 rs5443 (Fst <0.1), although there exist large heterogeneity in the involved studies (I2>60%). For CASQ1 rs2275703, the heterogeneity might come from the discrepancies of the samples in the case-control studies.
Pancreatic β-cell inflammation and apoptosis plays a pivotal role in the pathogenesis of T1D [60]. As a member of the Ced-4 family of apoptosis proteins, NLRP1 is an important mediator of programmed cell death [61]. NLRP1 plays a pivotal role in the pathogenesis of some inflammatory diseases [62], [63]. In the present research, we combined three independent datasets and performed a meta-analysis to evaluate the association between NLRP1 rs12150220 polymorphism and T1D susceptibility. Although large ethnic differences of allele frequency were found for NLRP1 rs12150220 (T allele frequency: 47–53.1% in Caucasians versus 66.4% in Brazilians), minimal heterogeneity was observed in the meta-analysis of this polymorphism (I2 = 0%). Our results support NLRP1 rs12150220 as a protective genetic factor of T1D and provide hints to clarify the mechanistic role of NLRP1 gene in the pathogenesis of T1D.
Evidence from both genetic and animal model studies has shown a crucial role of IL-2/IL-2RA in the pathogenesis of T1D [37], [64]–[67]. IL-2/IL-2RA regulates CD4+CD25+ regulatory T cells so as to maintain immune homeostasis [67]. IL-2RA rs12722495 was shown to contribute to the risk of T1D by lowering IL-2 signaling and diminishing the function of CD4+CD25+ regulatory T cells [64]. Interestingly, there is a significant association of IL-2RA rs11594656 as a protective factor with the risk of T1D in Polish population [22]. These two SNPs were 24.726 kb away and not in the same linkage disequilibrium block. Expansion of CD4+CD25+FOXP3+ regulatory T cells through maternal insulin treatment was shown to reduce the risk of T1D in children [68]. Increased resistance to CD4+CD25hi regulatory T cell-mediated suppression was showed in T1D patients [69]. Our meta-analysis established a significant association between IL-2RA rs11594656 polymorphism and T1D, although the influence of rs11594656 polymorphism on the regulation of IL-2RA gene remains to be unveiled in the future.
CLEC16A gene is located in the major histocompatibility complex class II region (16p13), and it encodes a member of the C-type lectin domain containing family. CLEC16A gene variants were associated with multiple autoimmune diseases such as T1D [38], [70]–[72]. CLEC16A gene variants were shown to be associated with the alternative splicing event in the CLEC16A transcription [73]. Our results suggested a significant association between CLEC16A rs725613 and T1D among 5,074 samples from Caucasian and Chinese populations (P = 0.01). A significant heterogeneity (I2 = 69%) among these ethnic samples warranted a replication in additional populations.
High level of glucose was shown to induce expression of APOA5 [74], [75] that is an efficient regulator of plasma triglycerides (TGs) by enhancing the catabolism of TG-rich lipoproteins [76] and prohibiting the transportation of TGs [77]. APOA5 could probably play a role in the pathogenesis of T2D by regulating the cholesterol homeostasis [44], [76]. APOA5 gene variants were also reported to be associated with the lipid levels [50], [78], [79] and the risk of coronary heart disease [80], [81] in T2D patients. Since both environmental factors [82], [83] and other genes [84] interact with APOA5 gene, our significant observation for APOA5 −1131T/C polymorphism may only partly explain the risk of T2D. Minimal heterogeneity among the involved studies in our meta-analysis (I2 = 1%), however, along with previous results [85], [86], in which ethnic differences were observed for the T allele frequency of APOA5 −1131T/C among the studies in our meta-analysis (68.8–76% in Chinese versus 93.7% in Caucasians).
There are some limitations in the present study. Firstly, publishing bias might exist in this meta-analysis. Case-control studies with a lack of significant results were much harder to be published than those with positive findings. In addition, only publications in English and Chinese were included in the current meta-analyses. All these may distort the results in our meta-analyses. Secondly, some of the involved case-control studies [22]–[24], [26], [28], [31], [34], [35], [37]–[39], [41], [43]–[46], [49], [51]–[57] didn’t provide information on the exclusion of other diseases (such as coronary artery diseases, hypertension, and etc.) during recruitment. Thirdly, the effects of genetic factors on diabetes risk were confounded by other phenotypic parameters such as body mass index. Therefore, case-control studies with better design are warranted to avoid these confounding factors and replicate our findings in future. Fourthly, due to a lack of enough independent datasets, subgroup analysis and meta-regression were not applied to identify differences in effect and sources of heterogeneity. Lastly, our meta-analysis focused on gene loci with at least three independent studies, and this might prevent those gene loci in two large scale case-control studies from being included in the current meta-analysis.
In conclusion, we identify significant associations between 4 SNPs (NLRP1 rs12150220, IL2RA rs11594656, CLEC16A rs725613 and APOA5 −1131T/C) and diabetes. Meta-analysis among 4,456 samples has confirmed that rs12150220 of NLRP1 gene is a risk factor of T1D in Caucasian and Brazilian populations. Meta-analysis among 37,432 samples has confirmed that rs11594656 of IL2RA gene is a risk factor of T1D in Caucasian and Japanese populations. Meta-analysis among 5,074 samples has confirmed that rs725613 of CLEC16A gene is a risk factor of T1D in Caucasian and Chinese populations. Another meta-analysis among 4,005 samples indicates that −1131T/C of APOA5 gene is a risk factor of T1D/T2D in Chinese and Caucasian populations.
Funding Statement
The research was supported by the grants from National Natural Science Foundation of China (No. 31100919), Ningbo social development research projects(2012C50032), K.C. Wong Magna Fund in Ningbo University, Natural Science Foundation of Ningbo (2007A610077), and Program for Innovative Research Team in Zhejiang Province (2010R50046). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO (2011) Burden: mortality, morbidity and risk factors - Chapter 1 of the latest WHO report “Global status report on NCDs 2010”.
- 2. Markle JG, Frank DN, Mortin-Toth S, Robertson CE, Feazel LM, et al. (2013) Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 339: 1084–1088. [DOI] [PubMed] [Google Scholar]
- 3. Ashcroft FM, Rorsman P (2012) Diabetes mellitus and the beta cell: the last ten years. Cell 148: 1160–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hyttinen V, Kaprio J, Kinnunen L, Koskenvuo M, Tuomilehto J (2003) Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: a nationwide follow-up study. Diabetes 52: 1052–1055. [DOI] [PubMed] [Google Scholar]
- 5. Jenkins AB, Samaras K, Carey DG, Kelly P, Campbell LV (2000) Improved indices of insulin resistance and insulin secretion for use in genetic and population studies of type 2 diabetes mellitus. Twin Res 3: 148–151. [DOI] [PubMed] [Google Scholar]
- 6. Wang X, Ding X, Su S, Spector TD, Mangino M, et al. (2009) Heritability of insulin sensitivity and lipid profile depend on BMI: evidence for gene-obesity interaction. Diabetologia 52: 2578–2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Poulsen P, Levin K, Petersen I, Christensen K, Beck-Nielsen H, et al. (2005) Heritability of insulin secretion, peripheral and hepatic insulin action, and intracellular glucose partitioning in young and old Danish twins. Diabetes 54: 275–283. [DOI] [PubMed] [Google Scholar]
- 8.Beck-Nielsen H (1999) General characteristics of the insulin resistance syndrome: prevalence and heritability. European Group for the study of Insulin Resistance (EGIR). Drugs 58 Suppl 1: 7–10; discussion 75–82. [DOI] [PubMed]
- 9. Huyghe JR, Jackson AU, Fogarty MP, Buchkovich ML, Stancakova A, et al. (2013) Exome array analysis identifies new loci and low-frequency variants influencing insulin processing and secretion. Nat Genet 45: 197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morris AP, Voight BF, Teslovich TM, Ferreira T, Segre AV, et al. (2012) Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet 44: 981–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Manning AK, Hivert MF, Scott RA, Grimsby JL, Bouatia-Naji N, et al. (2012) A genome-wide approach accounting for body mass index identifies genetic variants influencing fasting glycemic traits and insulin resistance. Nat Genet 44: 659–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cho YS, Chen CH, Hu C, Long J, Ong RT, et al. (2012) Meta-analysis of genome-wide association studies identifies eight new loci for type 2 diabetes in east Asians. Nat Genet 44: 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim HP, Imbert J, Leonard WJ (2006) Both integrated and differential regulation of components of the IL-2/IL-2 receptor system. Cytokine Growth Factor Rev 17: 349–366. [DOI] [PubMed] [Google Scholar]
- 14. Tschopp J, Martinon F, Burns K (2003) NALPs: a novel protein family involved in inflammation. Nat Rev Mol Cell Biol 4: 95–104. [DOI] [PubMed] [Google Scholar]
- 15. Trinchieri G (1995) Interleukin-12: a proinflammatory cytokine with immunoregulatory functions that bridge innate resistance and antigen-specific adaptive immunity. Annu Rev Immunol 13: 251–276. [DOI] [PubMed] [Google Scholar]
- 16. Zoledziewska M, Costa G, Pitzalis M, Cocco E, Melis C, et al. (2009) Variation within the CLEC16A gene shows consistent disease association with both multiple sclerosis and type 1 diabetes in Sardinia. Genes Immun 10: 15–17. [DOI] [PubMed] [Google Scholar]
- 17. Lanner JT, Katz A, Tavi P, Sandstrom ME, Zhang SJ, et al. (2006) The role of Ca2+ influx for insulin-mediated glucose uptake in skeletal muscle. Diabetes 55: 2077–2083. [DOI] [PubMed] [Google Scholar]
- 18. Pennacchio LA, Olivier M, Hubacek JA, Cohen JC, Cox DR, et al. (2001) An apolipoprotein influencing triglycerides in humans and mice revealed by comparative sequencing. Science 294: 169–173. [DOI] [PubMed] [Google Scholar]
- 19.Zhang H, Chen Q, Yang M, Zhu B, Cui Y, et al.. (2012) Mouse KLF11 regulates hepatic lipid metabolism. J Hepatol. [DOI] [PubMed]
- 20. Back SH, Kang SW, Han J, Chung HT (2012) Endoplasmic reticulum stress in the beta-cell pathogenesis of type 2 diabetes. Exp Diabetes Res 2012: 618396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chang L, Chiang SH, Saltiel AR (2004) Insulin signaling and the regulation of glucose transport. Mol Med 10: 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fichna M, Zurawek M, Fichna P, Januszkiewicz D, Nowak J (2012) Polymorphic variants of the IL2RA gene and susceptibility to type 1 diabetes in the Polish population. Tissue Antigens 79: 198–203. [DOI] [PubMed] [Google Scholar]
- 23. Zurawek M, Fichna M, Fichna P, Januszkiewicz D, Nowak J (2011) No evidence for association of the polymorphisms in NLRP1 gene with type 1 diabetes in Poland. Diabetes Res Clin Pract 92: e49–51. [DOI] [PubMed] [Google Scholar]
- 24. Hu C, Zhang R, Wang C, Ma X, Wang J, et al. (2011) Lack of association between genetic polymorphisms within DUSP12 - ATF6 locus and glucose metabolism related traits in a Chinese population. BMC Med Genet 12: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pontillo A, Brandao L, Guimaraes R, Segat L, Araujo J, et al. (2010) Two SNPs in NLRP3 gene are involved in the predisposition to type-1 diabetes and celiac disease in a pediatric population from northeast Brazil. Autoimmunity 43: 583–589. [DOI] [PubMed] [Google Scholar]
- 26. Altinova AE, Engin D, Akbay E, Akturk M, Toruner F, et al. (2010) Association of polymorphisms in the IL-18 and IL-12 genes with susceptibility to Type 1 diabetes in Turkish patients. J Endocrinol Invest 33: 451–454. [DOI] [PubMed] [Google Scholar]
- 27.Qiao Y, Liu R, Tian HM, Liu Y, Qiang O, et al.. (2008) [Association of apolipoprotein A5 gene -1131T/C polymorphism with serum lipids and carotid intima-media thickness in patients with type 2 diabetes mellitus]. Sichuan Da Xue Xue Bao Yi Xue Ban 39: 965–968, 999. [PubMed]
- 28. Wu X, Zhu X, Wang X, Ma J, Zhu S, et al. (2009) Intron polymorphism in the KIAA0350 gene is reproducibly associated with susceptibility to type 1 diabetes (T1D) in the Han Chinese population. Clin Endocrinol (Oxf) 71: 46–49. [DOI] [PubMed] [Google Scholar]
- 29. Li X, Xu Y, Ding Y, Qin C, Dai Z, et al. (2008) Polymorphism of apolipoprotein A5 is a risk factor for cerebral infarction in type 2 diabetes. J Huazhong Univ Sci Technolog Med Sci 28: 653–656. [DOI] [PubMed] [Google Scholar]
- 30. Kawasaki E, Awata T, Ikegami H, Kobayashi T, Maruyama T, et al. (2009) Genetic association between the interleukin-2 receptor-alpha gene and mode of onset of type 1 diabetes in the Japanese population. J Clin Endocrinol Metab 94: 947–952. [DOI] [PubMed] [Google Scholar]
- 31. Smyth DJ, Plagnol V, Walker NM, Cooper JD, Downes K, et al. (2008) Shared and distinct genetic variants in type 1 diabetes and celiac disease. N Engl J Med 359: 2767–2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Magitta NF, Boe Wolff AS, Johansson S, Skinningsrud B, Lie BA, et al. (2009) A coding polymorphism in NALP1 confers risk for autoimmune Addison’s disease and type 1 diabetes. Genes Immun 10: 120–124. [DOI] [PubMed] [Google Scholar]
- 33. Daimon M, Sato H, Sasaki S, Toriyama S, Emi M, et al. (2008) Salt consumption-dependent association of the GNB3 gene polymorphism with type 2 DM. Biochem Biophys Res Commun 374: 576–580. [DOI] [PubMed] [Google Scholar]
- 34. Ma L, Hanson RL, Que LN, Mack JL, Franks PW, et al. (2008) Association analysis of Kruppel-like factor 11 variants with type 2 diabetes in Pima Indians. J Clin Endocrinol Metab 93: 3644–3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tanahashi T, Shinohara K, Keshavarz P, Yamaguchi Y, Miyawaki K, et al. (2008) The association of genetic variants in Kruppel-like factor 11 and Type 2 diabetes in the Japanese population. Diabet Med 25: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sparso T, Hussain MS, Borch-Johnsen K, Jorgensen T, Madsbad S, et al. (2007) Studies of association of the CASQ1 rs2275703 polymorphism in relation to type 2 diabetes and related quantitative metabolic traits among 7,088 Danish whites. Mol Genet Metab 92: 278–282. [DOI] [PubMed] [Google Scholar]
- 37. Lowe CE, Cooper JD, Brusko T, Walker NM, Smyth DJ, et al. (2007) Large-scale genetic fine mapping and genotype-phenotype associations implicate polymorphism in the IL2RA region in type 1 diabetes. Nat Genet 39: 1074–1082. [DOI] [PubMed] [Google Scholar]
- 38. Hakonarson H, Grant SF, Bradfield JP, Marchand L, Kim CE, et al. (2007) A genome-wide association study identifies KIAA0350 as a type 1 diabetes gene. Nature 448: 591–594. [DOI] [PubMed] [Google Scholar]
- 39. Zhai GH, Wen P, Guo LF, Chen L (2007) [Association of apolipoprotein A5 gene -1131T/C polymorphism with lipid metabolism and insulin resistance in patients with type II diabetes mellitus]. Yi Chuan 29: 541–546. [DOI] [PubMed] [Google Scholar]
- 40. Meex SJ, van Greevenbroek MM, Ayoubi TA, Vlietinck R, van Vliet-Ostaptchouk JV, et al. (2007) Activating transcription factor 6 polymorphisms and haplotypes are associated with impaired glucose homeostasis and type 2 diabetes in Dutch Caucasians. J Clin Endocrinol Metab 92: 2720–2725. [DOI] [PubMed] [Google Scholar]
- 41. Chu WS, Das SK, Wang H, Chan JC, Deloukas P, et al. (2007) Activating transcription factor 6 (ATF6) sequence polymorphisms in type 2 diabetes and pre-diabetic traits. Diabetes 56: 856–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hayakawa T, Takamura T, Abe T, Kaneko S (2007) Association of the C825T polymorphism of the G-protein beta3 subunit gene with hypertension, obesity, hyperlipidemia, insulin resistance, diabetes, diabetic complications, and diabetic therapies among Japanese. Metabolism 56: 44–48. [DOI] [PubMed] [Google Scholar]
- 43. Florez JC, Saxena R, Winckler W, Burtt NP, Almgren P, et al. (2006) The Kruppel-like factor 11 (KLF11) Q62R polymorphism is not associated with type 2 diabetes in 8,676 people. Diabetes 55: 3620–3624. [DOI] [PubMed] [Google Scholar]
- 44. Talmud PJ, Cooper JA, Hattori H, Miller IP, Miller GJ, et al. (2006) The apolipoprotein A-V genotype and plasma apolipoprotein A-V and triglyceride levels: prospective risk of type 2 diabetes. Results from the Northwick Park Heart Study II. Diabetologia 49: 2337–2340. [DOI] [PubMed] [Google Scholar]
- 45. Lin WH, Chuang LM, Chen CH, Yeh JI, Hsieh PS, et al. (2006) Association study of genetic polymorphisms of SLC2A10 gene and type 2 diabetes in the Taiwanese population. Diabetologia 49: 1214–1221. [DOI] [PubMed] [Google Scholar]
- 46. Thameem F, Farook VS, Bogardus C, Prochazka M (2006) Association of amino acid variants in the activating transcription factor 6 gene (ATF6) on 1q21-q23 with type 2 diabetes in Pima Indians. Diabetes 55: 839–842. [DOI] [PubMed] [Google Scholar]
- 47. Bento JL, Bowden DW, Mychaleckyj JC, Hirakawa S, Rich SS, et al. (2005) Genetic analysis of the GLUT10 glucose transporter (SLC2A10) polymorphisms in Caucasian American type 2 diabetes. BMC Med Genet 6: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Andersen G, Overgaard J, Albrechtsen A, Glumer C, Borch-Johnsen K, et al. (2006) Studies of the association of the GNB3 825C>T polymorphism with components of the metabolic syndrome in white Danes. Diabetologia 49: 75–82. [DOI] [PubMed] [Google Scholar]
- 49. Santiago JL, Martinez A, de La Calle H, Fernandez-Arquero M, de La Concha EG, et al. (2005) Th1 cytokine polymorphisms in spanish patients with type 1 diabetes. Hum Immunol 66: 897–902. [DOI] [PubMed] [Google Scholar]
- 50. Yan SK, Cheng XQ, Song YH, Xiao XH, Bi N, et al. (2005) Apolipoprotein A5 gene polymorphism -1131T–>C: association with plasma lipids and type 2 diabetes mellitus with coronary heart disease in Chinese. Clin Chem Lab Med 43: 607–612. [DOI] [PubMed] [Google Scholar]
- 51. Mohlke KL, Skol AD, Scott LJ, Valle TT, Bergman RN, et al. (2005) Evaluation of SLC2A10 (GLUT10) as a candidate gene for type 2 diabetes and related traits in Finns. Mol Genet Metab 85: 323–327. [DOI] [PubMed] [Google Scholar]
- 52. Kiani JG, Saeed M, Parvez SH, Frossard PM (2005) Association of G-protein beta-3 subunit gene (GNB3) T825 allele with Type II diabetes. Neuro Endocrinol Lett 26: 87–88. [PubMed] [Google Scholar]
- 53. Neve B, Fernandez-Zapico ME, Ashkenazi-Katalan V, Dina C, Hamid YH, et al. (2005) Role of transcription factor KLF11 and its diabetes-associated gene variants in pancreatic beta cell function. Proc Natl Acad Sci U S A 102: 4807–4812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Das SK, Chu W, Zhang Z, Hasstedt SJ, Elbein SC (2004) Calsquestrin 1 (CASQ1) gene polymorphisms under chromosome 1q21 linkage peak are associated with type 2 diabetes in Northern European Caucasians. Diabetes 53: 3300–3306. [DOI] [PubMed] [Google Scholar]
- 55. Fu M, Damcott CM, Sabra M, Pollin TI, Ott SH, et al. (2004) Polymorphism in the calsequestrin 1 (CASQ1) gene on chromosome 1q21 is associated with type 2 diabetes in the old order Amish. Diabetes 53: 3292–3299. [DOI] [PubMed] [Google Scholar]
- 56. McCormack RM, Maxwell AP, Carson DJ, Patterson CC, Middleton D, et al. (2002) The IL12B 3′ untranslated region DNA polymorphism is not associated with early-onset type 1 diabetes. Genes Immun 3: 433–435. [DOI] [PubMed] [Google Scholar]
- 57. Nistico L, Giorgi G, Giordano M, Galgani A, Petrone A, et al. (2002) IL12B polymorphism and type 1 diabetes in the Italian population: a case-control study. Diabetes 51: 1649–1650. [DOI] [PubMed] [Google Scholar]
- 58. Jiang H, Sun MW, Hefright B, Chen W, Lu CD, et al. (2011) Efficacy of hypocaloric parenteral nutrition for surgical patients: a systematic review and meta-analysis. Clin Nutr 30: 730–737. [DOI] [PubMed] [Google Scholar]
- 59.Coory MD (2010) Comment on: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 39: 932; author reply 933. [DOI] [PubMed]
- 60. Ritvo RA (1987) Coordinating in-patient and out-patient services: the need for action. Soc Work Health Care 13: 39–56. [DOI] [PubMed] [Google Scholar]
- 61. Dowling JK, O’Neill LA (2012) Biochemical regulation of the inflammasome. Crit Rev Biochem Mol Biol 47: 424–443. [DOI] [PubMed] [Google Scholar]
- 62. Schroder K, Tschopp J (2010) The inflammasomes. Cell 140: 821–832. [DOI] [PubMed] [Google Scholar]
- 63. Martinon F, Mayor A, Tschopp J (2009) The inflammasomes: guardians of the body. Annu Rev Immunol 27: 229–265. [DOI] [PubMed] [Google Scholar]
- 64. Garg G, Tyler JR, Yang JH, Cutler AJ, Downes K, et al. (2012) Type 1 diabetes-associated IL2RA variation lowers IL-2 signaling and contributes to diminished CD4+CD25+ regulatory T cell function. J Immunol 188: 4644–4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Aminkeng F, Weets I, Van Autreve JE, Koeleman BP, Quartier E, et al. (2010) Association of IL-2RA/CD25 with type 1 diabetes in the Belgian population. Hum Immunol 71: 1233–1237. [DOI] [PubMed] [Google Scholar]
- 66. Dendrou CA, Wicker LS (2008) The IL-2/CD25 pathway determines susceptibility to T1D in humans and NOD mice. J Clin Immunol 28: 685–696. [DOI] [PubMed] [Google Scholar]
- 67. Chistiakov DA, Voronova NV, Chistiakov PA (2008) The crucial role of IL-2/IL-2RA-mediated immune regulation in the pathogenesis of type 1 diabetes, an evidence coming from genetic and animal model studies. Immunol Lett 118: 1–5. [DOI] [PubMed] [Google Scholar]
- 68. Luopajarvi K, Nieminen JK, Ilonen J, Akerblom HK, Knip M, et al. (2012) Expansion of CD4+CD25+FOXP3+ regulatory T cells in infants of mothers with type 1 diabetes. Pediatr Diabetes 13: 400–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lawson JM, Tremble J, Dayan C, Beyan H, Leslie RD, et al. (2008) Increased resistance to CD4+CD25hi regulatory T cell-mediated suppression in patients with type 1 diabetes. Clin Exp Immunol 154: 353–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wang N, Shen N, Vyse TJ, Anand V, Gunnarson I, et al. (2011) Selective IgA deficiency in autoimmune diseases. Mol Med 17: 1383–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Martinez A, Perdigones N, Cenit MC, Espino L, Varade J, et al. (2010) Chromosomal region 16p13: further evidence of increased predisposition to immune diseases. Ann Rheum Dis 69: 309–311. [DOI] [PubMed] [Google Scholar]
- 72. Banos R, Botella C, Garcia-Palacios A, Villa H, Perpina C, et al. (1999) Psychological variables and reality judgment in virtual environments: the roles of absorption and dissociation. Cyberpsychol Behav 2: 143–148. [DOI] [PubMed] [Google Scholar]
- 73. Mero IL, Ban M, Lorentzen AR, Smestad C, Celius EG, et al. (2011) Exploring the CLEC16A gene reveals a MS-associated variant with correlation to the relative expression of CLEC16A isoforms in thymus. Genes Immun 12: 191–198. [DOI] [PubMed] [Google Scholar]
- 74. Nowak M, Helleboid-Chapman A, Jakel H, Moitrot E, Rommens C, et al. (2008) Glucose regulates the expression of the apolipoprotein A5 gene. J Mol Biol 380: 789–798. [DOI] [PubMed] [Google Scholar]
- 75. Pruneta-Deloche V, Ponsin G, Groisne L, Fruchart-Najib J, Lagarde M, et al. (2005) Postprandial increase of plasma apoAV concentrations in Type 2 diabetic patients. Atherosclerosis 181: 403–405. [DOI] [PubMed] [Google Scholar]
- 76. Jakel H, Nowak M, Helleboid-Chapman A, Fruchart-Najib J, Fruchart JC (2006) Is apolipoprotein A5 a novel regulator of triglyceride-rich lipoproteins? Ann Med 38: 2–10. [DOI] [PubMed] [Google Scholar]
- 77. Garelnabi M, Lor K, Jin J, Chai F, Santanam N (2013) The paradox of ApoA5 modulation of triglycerides: evidence from clinical and basic research. Clin Biochem 46: 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Soter MO, Gomes KB, Fernandes AP, Carvalho M, Pinheiro PS, et al. (2012) −1131T>C and SW19 polymorphisms in APOA5 gene and lipid levels in type 2 diabetic patients. Mol Biol Rep 39: 7541–7548. [DOI] [PubMed] [Google Scholar]
- 79. Esteve E, Faure E, Calvo F, Aguillo E, Blasco C, et al. (2004) SNP3 polymorphism in apo A-V gene is associated with small dense LDL particles in Type 2 diabetes. Diabetologia 47: 355–356. [DOI] [PubMed] [Google Scholar]
- 80. Bhaskar S, Ganesan M, Chandak GR, Mani R, Idris MM, et al. (2011) Association of PON1 and APOA5 gene polymorphisms in a cohort of Indian patients having coronary artery disease with and without type 2 diabetes. Genet Test Mol Biomarkers 15: 507–512. [DOI] [PubMed] [Google Scholar]
- 81. Charriere S, Bernard S, Aqallal M, Merlin M, Billon S, et al. (2008) Association of APOA5–1131T>C and S19W gene polymorphisms with both mild hypertriglyceridemia and hyperchylomicronemia in type 2 diabetic patients. Clin Chim Acta 394: 99–103. [DOI] [PubMed] [Google Scholar]
- 82. Grarup N, Andersen G (2007) Gene-environment interactions in the pathogenesis of type 2 diabetes and metabolism. Curr Opin Clin Nutr Metab Care 10: 420–426. [DOI] [PubMed] [Google Scholar]
- 83. Jiang YD, Yen CJ, Chou WL, Kuo SS, Lee KC, et al. (2005) Interaction of the G182C polymorphism in the APOA5 gene and fasting plasma glucose on plasma triglycerides in Type 2 diabetic subjects. Diabet Med 22: 1690–1695. [DOI] [PubMed] [Google Scholar]
- 84. Hiramatsu M, Oguri M, Kato K, Horibe H, Fujimaki T, et al. (2012) Synergistic effects of genetic variants of APOA5 and BTN2A1 on dyslipidemia or metabolic syndrome. Int J Mol Med 30: 185–192. [DOI] [PubMed] [Google Scholar]
- 85. Dorfmeister B, Cooper JA, Stephens JW, Ireland H, Hurel SJ, et al. (2007) The effect of APOA5 and APOC3 variants on lipid parameters in European Whites, Indian Asians and Afro-Caribbeans with type 2 diabetes. Biochim Biophys Acta 1772: 355–363. [DOI] [PubMed] [Google Scholar]
- 86. Chandak GR, Ward KJ, Yajnik CS, Pandit AN, Bavdekar A, et al. (2006) Triglyceride associated polymorphisms of the APOA5 gene have very different allele frequencies in Pune, India compared to Europeans. BMC Med Genet 7: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]