Abstract
Objectives
Studies primarily using prevalence data suggest the relationship between body mass index (BMI) and risk factors for cardiovascular disease may vary by ethnicity. The objective of this study was to examine longitudinally the associations of BMI and ethnicity with transitions from a baseline state without evidence of chronic disease to the onset of hypertension, hyperlipidemia, or both.
Design
The study population comprised members of a large insurer in Hawaii. Individuals were eligible if continuously enrolled for at least one year without evidence of major chronic disease. Analyses used multi-state models to measure the relative rates of transitions from the baseline state to developing hypertension, hyperlipidemia, or both. All analyses were adjusted for age, sex, education, number of office visits, and island of residence.
Results
Native Hawaiians had the highest prevalence of overweight and obesity followed by Caucasians, Filipinos, Japanese, Chinese, and Koreans. Relative rates of transitions by ethnicity, however, did not parallel the prevalence of overweight and obesity. Japanese and Filipino ethnicities had significantly faster transition rates than Whites for all four study transitions, rates that ranged from 20% to more than two-fold faster. Chinese and Koreans also had significantly higher rates of many transitions compared to Whites. Native Hawaiians, by contrast, had a slower transition rate than Whites to developing hyperlipidemia without hypertension, and relatively faster transitions to the other outcome states.
Conclusions
The study offers longitudinal evidence of different patterns of risk for developing hypertension and hyperlipidemia among Asians, Whites, and Native Hawaiians.
Keywords: Ethnicity, Hypertension, Hyperlipidemia
Introduction
The World Health Organization (WHO) defines overweight and obesity as conditions in which the body accumulates fat to the extent that health and well-being are adversely affected.1 With overweight and obesity, the prevalence of hypertension, hyperlipidemia, and diabetes increases substantially and are considered to be three factors on the pathway to cardiovascular disease and mortality.2,3 Insulin resistance also becomes more common, often accompanied by higher serum insulin levels. Other consequences of obesity include musculoskeletal disorders, limitations of respiratory function, reduced physical functioning and quality of life.4
The adverse consequences of obesity are experienced by all ethnic groups. Body mass index (BMI) levels, however, differ considerably by ethnicity, and can vary among subpopulations within an ethnicity because of environmental and lifestyle factors.5 For example, compared to urban Chinese, rural Chinese have lower average BMI levels.6 The relationship of BMI and adverse health outcomes involves additional complexities. First, the strength of relationships between BMI and adverse health events can differ among ethnicities. It appears, as an example, that most Asian ethnicities experience higher risks of hypertension and cardiovascular disease, while having lower BMI levels than Whites.3,5,7–9 Underlying the differing risks are differences in the percentage of body fat for a given BMI. The relationship between BMI and percentage of body fat depends on age and sex, and differs across ethnic groups. Most Asian ethnicities have higher average body fat percentage than Whites of the same age and BMI.5 As a consequence, Asians may be predisposed to a greater risk of clinical events, despite similar BMI. In contrast to Asians, Polynesians have been reported to have lower percentages of body fat at comparable BMI.10 Among White populations, Europeans have been reported to have a higher percentage of body fat at a given BMI than Whites in the United States.5,11
This article summarizes results of an ethnic study of obesity in Hawaii. Hawaii residents include Native Hawaiians, Whites, and diverse Asian populations. Our study describes the longitudinal relationships of overweight, obesity, and ethnicity with the rates of clinical diagnosis of hypertension and hyperlipidemia.
Methods
Study Design
The study population was drawn from the membership of the largest insurer in Hawaii. Study participants had received and answered the insurer’s membership satisfaction surveys between 2002 and 2009. A sample of the membership was surveyed annually with response rates typically of 40% to 50%. To be eligible for the study, the members had to have at least one year of continuous enrollment that ended in 2002 or later, and no evidence of hypertension, hyperlipidemia, diabetes, chronic kidney disease, or heart disease prior to the end of the year of continuous enrollment. The population was followed from the date they met the enrollment criteria until having evidence of the development of both hypertension and hyperlipidemia, disenrollment with the insurer, or the end of the study period.
The study outcomes consisted of five transitions from less to more complex health states. The transitions were going from the baseline state to having hypertension, hyperlipidemia, or having both diagnosed closely together in time; and from having one of the two chronic conditions to developing both. Members with claims for hypertension and hyperlipidemia submitted within 90 days of one another were considered to have had both diagnosed at about the same time. A similar definition was used in a study examining medication adherence among patients taking both anti-hypertension and lipid-lowering medications.12
Other study variables included age, sex, ethnicity, body mass index, education, the number of office visits, and living on the major Hawaii island of Oahu or on a neighboring island. Ethnicities were defined from 14 categories listed on the membership survey. Participants were asked to check all the categories that applied. Anyone checking Native Hawaiian was treated in the analyses as Native Hawaiian, even if other ethnicities were identified. This choice follows the practice used by the Hawaii State Department of Health in summarizing survey data. Eighty six percent of the other respondents selected only one ethnic category; as a consequence, to simplify interpretation of the results, analyses were limited to people selecting a single ethnicity. The study included White, Chinese, Filipino, Native Hawaiian, Japanese, and Korean ethnicities. Education was classified into three categories: less than high school, completing high school but not going further, and having some college education. BMI was categorized into five ranges: ≤18.5, >18.5 to 24, 25 to 29, 30 to 34, and 35 and higher. The BMI ranges were chosen to measure the relative transition rates of the various ethnicities using the standard WHO categories.
Data Analysis
Initial analyses included tabulating frequencies of the study variables and examining the cross-classifications such as BMI levels by ethnicity. Subsequent analyses examined transitions from less to more complex health states using multi-state regression models.13,14 The models are extensions of proportional hazard models and use times to transitions as the outcomes. People without transitions were treated as censored. The multi-state models measure the hazard ratios of transitions as a function of covariates. Results are expressed as hazard ratios with 95% CI.
Results
The study population included 54,418 people with a mean age of 44.8 ± 13.8 (SD) years; 64.6% were female. Only 3.6% had not completed high school; 49.6% had a high school degree but had not gone further; and 46.7% had some college education. The majority lived on Oahu (66.3%). The percentages by ethnicity were 31.6% White, 27.7% Japanese, 19.3% Hawaiian, 12.3% Filipino, 7.0% Chinese, and 2.1% Korean. The median length of enrollment before the start of follow-up was 5.0 years, so most participants had a relatively long interval prior to the study without evidence of chronic disease. A slight majority (54.3%) of the participants were in the normal range for BMI; most others were overweight (28.1%) or obese (13.3%) and a small percentage (4.4%) were underweight (Table 1). The prevalence of obesity by ethnicity was highest for Native Hawaiians followed by Whites, Filipinos, Japanese, Chinese, and Koreans.
Table 1.
Number and percent of people by ethnicity and range of body mass index (BMI)
| Ethnicity | n | Range of BMI and % Within Each Ethnicity
|
||||
|---|---|---|---|---|---|---|
| ≤18.5 | >18.5–24 | 25–29 | 30–34 | ≥35 | ||
| Caucasian | 14,694 | 3.46 | 57.64 | 27.44 | 8.22 | 3.25 |
| Chinese | 3,262 | 8.22 | 66.34 | 20.91 | 3.65 | 0.89 |
| Filipino | 5,731 | 3.63 | 55.98 | 30.41 | 7.56 | 2.43 |
| Hawaiian | 8,948 | 1.99 | 35.49 | 32.81 | 18.02 | 11.69 |
| Japanese | 12,849 | 6.14 | 58.35 | 27.20 | 6.76 | 1.56 |
| Korean | 980 | 8.37 | 72.65 | 15.51 | 2.65 | 0.82 |
| Total | 46,464 | 4.4 | 54.3 | 28.1 | 9.2 | 4.1 |
Table 2 summarizes the rates of transitions from the various starting and ending states. From the baseline state, people transitioned twice as rapidly to hyperlipidemia as to hypertension and twice as rapidly from having hypertension alone to having both hyperlipidemia and hypertension as from only having hyperlipidemia. The highest transition rate was among people transitioning from having hypertension alone to having both conditions.
Table 2.
Rates of transitions between health states by starting and ending states
| Starting State | Ending State | Transition Category | Rate per 100 years |
|---|---|---|---|
| Baseline | Hyperlipidemia only | 1 to 2 | 7.0 |
| Baseline | Hypertension only | 1 to 3 | 3.4 |
| Baseline | Hyperlipidemia & hypertension | 1 to 4 | 1.7 |
| Hyperlipidemia only | Hyperlipidemia & hypertension | 2 to 4 | 7.5 |
| Hypertension only | Hyperlipidemia & hypertension | 3 to 4 | 16.8 |
Rates are calculated as the number of transitions divided by the sum of the followup times for people in the starting state. Transitions are from a baseline state free of either condition or from states of having hyperlipidemia only or hypertension only. The ending state of hyperlipidemia and hypertension was defined as the data of detection of the second condition for people having the first, or the earliest diagnosis date of hyperlipidemia or hypertension when both conditions were first identified within 90 days of one another.
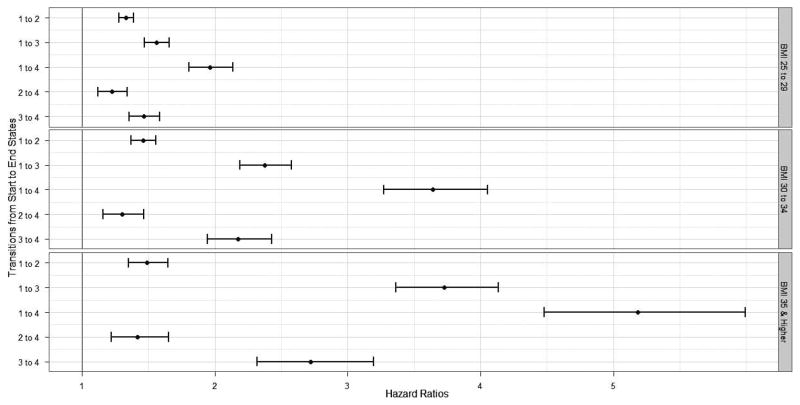
The hazard ratios for transitioning from less to more complex states, as might be expected, became greater with increasing BMI for all five transitions examined (Figure 1). The ratios were lower for transitions to having hyperlipidemia without hypertension than to developing hypertension without hyperlipidemia in the models adjusted for age, sex, ethnicity, education, number of office visits, and residence on Oahu or a neighboring island. As an example, compared to normal weight individuals people within BMI levels of 25–29, 30–34, and ≥35 had hazard ratios for developing hypertension alone of 1.6, 2.4, and 3.7, respectively. The comparable hazard ratios for transitions to hyperlipidemia alone were 1.3, 1.4, and 1.5. The relative rates of initial transitions were invariably greater going from the baseline state to the development of hypertension and hyperlipidemia close together in time. Transitions from having one of hypertension or hyperlipidemia to having both were slower than transitions to the single states.
Fig 1.
Hazard ratios with 95% CI compared to having a normal body mass index (BMI) for transitions from start to end states by heightened ranges of BMI. Start and end states are defined in Table 2. Analyses were adjusted for age, sex, ethnicity, education, number of office visits, and residence on Oahu or neighboring island
Not shown in Figure 1 are the relative rates of transitions for underweight individuals compared to people with normal BMI levels. With underweight, we were only able to fit a simplified model examining the three initial transitions because of low numbers of transitions from having one to having both conditions. Relative to people with normal BMI levels the underweight subgroup had hazard ratios (95% CIs) of 0.9 (0.8, 1.0), 0.7 (0.6, 0.8), and 0.7 (0.5, 0.8), respectively, for transitions from baseline to hypertension, hyperlipidemia, and having both diagnosed closely together.
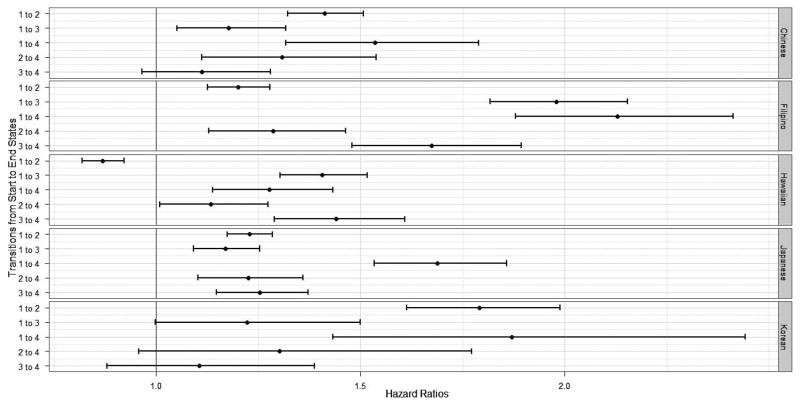
Figure 2 presents results for ethnicity from the same regression model as illustrated in Figure 1. All transitions were significantly faster for Filipinos and Japanese compared to Whites, and all transitions except the transition from baseline to hyperlipidemia had higher hazard rates for Hawaiians. Hawaiians were significantly less likely than Whites to transition to hyperlipidemia without accompanying hypertension. Although based on smaller numbers and not consistently significant, the hazard ratios for Chinese and Koreans had increased estimates compared to Whites.
Fig 2.
Hazard ratios with 95% CI compared to Whites for transitions among Filipinos, Hawaiians, and Japanese as examined in separate regression models adjusted and unadjusted for body mass index. Start and end states are defined in Table 2. Analyses were adjusted for age, sex, education, number of office visits, and residence on Oahu or neighboring island
Discussion
Within our modeling framework, the paths to developing hypertension and hyperlipidemia involve five distinct steps. Transitions across all of the steps increased with increasing BMI. By accelerating the development of both hypertension and hyperlipidemia, heightened BMI compounds the risk of subsequent heart disease. Strong relationships between BMI and the development of hypertension and hyperlipidemia have been previously shown in national surveys and other large studies.2,15 Using longitudinal data, our results emphasize the increased rates of transitions associated with increasing BMI levels.
The transition rates also varied in our study by ethnicity, but the rates did not parallel ethnic differences in the prevalence of overweight and obesity. All five of the transitions tended to occur faster for Asians compared to Whites. Filipinos had notably high rates of development of hypertension. Native Hawaiians, the ethnicity with highest percentages of overweight and obese individuals, developed conditions involving hypertension at greater relative rates than Whites. Native Hawaiians, however, developed hyperlipidemia without accompanying hypertension relatively more slowly. Rates of development of hypertension and hyperlipidemia among Asian ethnicities generally equaled or exceeded those among Native Hawaiians despite lower BMI levels. The study results suggest distinct patterns of transition rates among Asians, Whites, and Native Hawaiians.
A number of studies have reported greater risks of hypertension and hyperlipidemia among Asians than Whites at similar BMI levels.5,15,16 For example, one study observed a greater cross-sectional prevalence of hypertension among Chinese men and women and Filipino women compared to non-Hispanic Whites.17 The study did not observe a difference for Filipino men. A recent study using a large clinical database reported a higher prevalence of hypertension and hyperlipidemia among Whites than among Asians.18 Asians have also been shown to have a greater prevalence of the metabolic syndrome despite having a lower average BMI than Whites, and in one study Filipinos had the highest prevalence among Asian ethnicities.19,20 The Nurses’ Health Study reported a greater risk of developing diabetes by Asian women compared to White women.21
Whether Asians should have lower cut-points for defining overweight and obesity has received considerable discussion.3,5,8,9,11,22,23 One cut-off may not apply for all Asians; especially for some rural or malnourished populations, recommendations for Asians as a broad category may not suffice. The World Health Organization (WHO) has recommended having public health action points that may be specific to each country.5 A comparison of one set of action points for hypertension in a rural population of Asians and Native Hawaiians in Hawaii reported improvement in sensitivity and specificity compared with traditional cut-offs for Asians but not for Native Hawaiians.24 Our results present further evidence that the risks associated with heightened BMI may differ between Asians and Native Hawaiians.
Among Native Hawaiians a greater degree of Hawaiian ancestry has been associated with a higher prevalence of hypertension.25 Native Hawaiians as a group face elevated risks of obesity, cancer, cardiovascular disease, and mortality.26–29 Compared to Whites, for example, all-cause mortality among Native Hawaiians was 30% higher in 1990, and increased to 40% higher by 2000.28 Native Hawaiians are overrepresented in lower education and socioeconomic strata relative to most ethnicities in the United States, and more marginalized from the larger society.27 One study found that differences between the percentage of Hawaiian or other Pacific Islander ancestry and anthropometric outcomes was explained in part by differences in education, suggesting socioeconomic influences.30
The results in this article should be interpreted with respect to a number of limitations. First, the data are derived from one insurer and only include its members that answered member satisfaction surveys. In addition, a single measure of BMI was available per participant to study the development of hypertension and hyperlipidemia, and BMI was based on self-reported height and weight. At the beginning of followup, participants were considered to not have chronic conditions based on a minimum of one year without claims evidence of existing conditions. Some participants, however, could have had conditions not identified in the administrative data. Outcomes were identified from submitted claims, requiring health care utilization, but the use of health care was variable, although all participants were insured. Some important issues could not be studied with the available data, such as the influence of acculturation on the processes of transition from one health state to another.
A strength of the study is the relatively large sample size, sufficient to investigate transitions across multiple health states. The results provide longitudinal evidence of associations between BMI and ethnicity at early steps on the pathway to major chronic disease. Previous studies have often been cross-sectional or examined late stages such as the development of cardiovascular disease or mortality. The results affirm increasing rates of transition with increasing BMI, and for all five transitions investigated. The results further show that four Asian populations within a shared geographical setting and comparable BMI levels generally developed hypertension and hyperlipidemia at faster rates than Whites with similar BMI levels. Future studies might examine the comparative effectiveness of reducing BMI on the ethnic-specific risks of developing hypertension and hyperlipidemia as concurrent conditions as well as individually. The relative rates of transitions of Filipinos were especially high, a poorly understood observation as there has been very little research on this group. The study results emphasize the higher risks of Asians than Whites at comparable BMI levels and the high rates of hypertension development among Native Hawaiians.
Acknowledgments
The study was supported by Awards No. U54MD007584, G12MD007601, and 8P20GM103466-11 from the National Center for Research Resources (NCRR), National Institutes of Health NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCRR or NIH.
Footnotes
Author Contributions
Design and concept of study: Davis, Hodges
Acquisition of data: Davis, Hodges
Data analysis and interpretation: Davis, Juarez
Manuscript draft: Davis, Juarez
Administrative: Hodges
References
- 1.World Health Organization. Report on a WHO consultation on obesity. WHO; Geneva: 1997. Obesity: Preventing and Managing the Global Epidemic, 1997. [PubMed] [Google Scholar]
- 2.Bays HE, Chapman RH, Grandy S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidemia: comparison of data from two national surveys. Int J Clin Pract. 2007;61:737–747. doi: 10.1111/j.1742-1241.2007.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin WY, Chen CY, Hsia HH, et al. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obesity. 2002;26:1232–1238. doi: 10.1038/sj.ijo.0802040. [DOI] [PubMed] [Google Scholar]
- 4.Seidell JC, Kahn HS, Williamson DF, Lissner L, Valdez R. Report from a Centers for Disease Control and Prevention Workshop on use of adult anthropometry for public health and primary care. Am J Clin Nutr. 2001;73:123–126. doi: 10.1093/ajcn/73.1.123. [DOI] [PubMed] [Google Scholar]
- 5.WHO expert consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 6.Hu FB, Wang B, Chen C, et al. Body mass index and cardiovascular risk factors in rural Chinese population. Am J Epidemiol. 2000;151:88–97. doi: 10.1093/oxfordjournals.aje.a010127. [DOI] [PubMed] [Google Scholar]
- 7.Deurenberg-Yap M, Chew SK, Deurenberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obesity Reviews. 2002;3:209–215. doi: 10.1046/j.1467-789x.2002.00069.x. [DOI] [PubMed] [Google Scholar]
- 8.Wen CP, Cheng TYD, Tsai SP, et al. Are Asians at greater mortality risk for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2008;12:497–506. doi: 10.1017/S1368980008002802. [DOI] [PubMed] [Google Scholar]
- 9.Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas. 2010;65:315–319. doi: 10.1016/j.maturitas.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Swinburn BA, Ley SJ, Carmichael HE, Plank LD. Body size and composition in Polynesians. Int J Obes. 1999;2:1178–1183. doi: 10.1038/sj.ijo.0801053. [DOI] [PubMed] [Google Scholar]
- 11.Deurenberg P, Yap M, Staveren van WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obesity. 1998;22:1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 12.Chapman RH, Petrilla AA, Benner JS, Schwartz S, Tang SSK. Predictors of adherence to concomitant antihypertensive and lipid-lowering medications in older adults. Drugs Aging. 2008;25:885–892. doi: 10.2165/00002512-200825100-00008. [DOI] [PubMed] [Google Scholar]
- 13.Andersen PK, Keiding N. Multistate models for event history analysis. Stat Methods Med Res. 2002;11:91–115. doi: 10.1191/0962280202SM276ra. [DOI] [PubMed] [Google Scholar]
- 14.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26:2389–2430. doi: 10.1002/sim.2712. [DOI] [PubMed] [Google Scholar]
- 15.Stommel M, Schoenborn CA. Variations in BMI and prevalence of health risks in diverse racial and ethnic populations. Obesity. 2010;18:1821–1826. doi: 10.1038/oby.2009.472. [DOI] [PubMed] [Google Scholar]
- 16.Razak F, Sonia SS, Shannon H, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–2118. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 17.Bell AC, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol. 2002;155:346–353. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 18.Crawford AG, Cote C, Couto J, et al. Prevalence of obesity, Type II diabetes mellitus, hyperlipidemia, and hypertension in the United States: finding from the GE centricity electronic medical record database. Population Health Manag. 2010;13:151–61. doi: 10.1089/pop.2009.0039. [DOI] [PubMed] [Google Scholar]
- 19.Palaniappan LP, Wong EC, Shin JJ, Fortmann SP, Lauderdale DS. Asian Americans have greater prevalence of metabolic syndrome despite lower body mass index. Int J Obesity. doi: 10.1038/ijo.2010.152. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grandinetti A, Chang HK, Theriault A, Mor J. Metabolic syndrome in a multiethnic population in rural Hawaii. Ethn Dis. 2005;23:237. [PubMed] [Google Scholar]
- 21.Shai I, Jang R, Manson JE, et al. Ethnicity, obesity, and risk of type 2 diabetes in women. Diabetes Care. 2006;29:1585–1590. doi: 10.2337/dc06-0057. [DOI] [PubMed] [Google Scholar]
- 22.Gurrici S, Hartriyanti Y, Hautvast JGAJ, Deurenberg P. Relationship between body fat and body mass index: differences between Indonesians and Dutch Caucasians. Eur J Clin Nutr. 1998;52:779–783. doi: 10.1038/sj.ejcn.1600637. [DOI] [PubMed] [Google Scholar]
- 23.Ko GTC, Tang J, Chan JCN, et al. Lower BMI cut-off value to define obesity in Hong Kong Chinese: an analysis based on body fat assessment by bioelectrical impedance. Br J Nutr. 2001;85:239–242. doi: 10.1079/bjn2000251. [DOI] [PubMed] [Google Scholar]
- 24.Grandinetti A, Chen R, Koholokula JK, et al. Relationship of blood pressure with degree of Hawaiian ancestry. Ethn Dis. 2002;12:221–228. [PubMed] [Google Scholar]
- 25.Grandinetti A, Koholokua JK, Mau MK, Chow DC. Detecting cardiometabolic syndrome using World Health Organization public health action points for Asians and Pacific Islanders. Ethn Dis. 2010;20:123–128. [PMC free article] [PubMed] [Google Scholar]
- 26.Aluli NE, Reyes PW, Brady, et al. All-cause and CVD mortality in Native Hawaiians. Diabetes Res Clin Pr. 2010;89:65–71. doi: 10.1016/j.diabres.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mau MK, Sinclair K, Saito EP, Baumhofer KN, Keawe’aimoku J. Cardiometabolic health disparities in Native Hawaiians and other Pacific Islanders. Epidemiol Rev. 2009;31:113–129. doi: 10.1093/ajerev/mxp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panapasa SV, Mau MK, Williams DR, McNally JW. Mortality patterns of Native Hawaiians across their lifespan: 1990–2000. Am J Public Health. 2010;23:e1–e7. doi: 10.2105/AJPH.2009.183541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moy KL, Sallis JF, Davis KJ. Health indicators of Native Hawaiian and Pacific Islanders in the United States. J Commun Health. 2010;35:81–92. doi: 10.1007/s10900-009-9194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown DE, Hampson SE, Dubanoski JP, Murai AS, Hillier TA. Effects of ethnicity and socioeconomic status on body composition in an admixed, multiethnic population in Hawaii. Am J Hum Biol. 2009;21:83–388. doi: 10.1002/ajhb.20889. [DOI] [PMC free article] [PubMed] [Google Scholar]