Abstract
Defective cardiac mechanical activity in diabetes results from alterations in intracellular Ca2+ handling, in part, due to increased oxidative stress. Beta-blockers demonstrate marked beneficial effects in heart dysfunction with scavenging free radicals and/or acting as an antioxidant. The aim of this study was to address how β-blocker timolol-treatment of diabetic rats exerts cardioprotection. Timolol-treatment (12-week), one-week following diabetes induction, prevented diabetes-induced depressed left ventricular basal contractile activity, prolonged cellular electrical activity, and attenuated the increase in isolated-cardiomyocyte size without hyperglycemic effect. Both in vivo and in vitro timolol-treatment of diabetic cardiomyocytes prevented the altered kinetic parameters of Ca2+ transients and reduced Ca2+ loading of sarcoplasmic reticulum (SR), basal intracellular free Ca2+ and Zn2+ ([Ca2+]i and [Zn2+]i), and spatio-temporal properties of the Ca2+ sparks, significantly. Timolol also antagonized hyperphosphorylation of cardiac ryanodine receptor (RyR2), and significantly restored depleted protein levels of both RyR2 and calstabin2. Western blot analysis demonstrated that timolol-treatment also significantly normalized depressed levels of some [Ca2+]i-handling regulators, such as Na+/Ca2+ exchanger (NCX) and phospho-phospholamban (pPLN) to PLN ratio. Incubation of diabetic cardiomyocytes with 4-mM glutathione exerted similar beneficial effects on RyR2-macromolecular complex and basal levels of both [Ca2+]i and [Zn2+]i, increased intracellular Zn2+ hyperphosphorylated RyR2 in a concentration-dependent manner. Timolol also led to a balanced oxidant/antioxidant level in both heart and circulation and prevented altered cellular redox state of the heart. We thus report, for the first time, that the preventing effect of timolol, directly targeting heart, seems to be associated with a normalization of macromolecular complex of RyR2 and some Ca2+ handling regulators, and prevention of Ca2+ leak, and thereby normalization of both [Ca2+]i and [Zn2+]i homeostasis in diabetic rat heart, at least in part by controlling the cellular redox status of hyperglycemic cardiomyocytes.
Introduction
Diabetes is one of the major risk factors for the development of cardiovascular complications. A specific cardiomyopathy was first recognized by Rubler et al. [1] in diabetic patients with marked mechanical dysfunction [2]. In animal model studies with type 1 diabetic rats, the defects identified in mechanical activity of the hearts include alterations of Ca2+ signaling via changes in critical processes that regulate intracellular free Ca2+ concentration, [Ca2+]i [2], [3], [4], [5]. Recent studies demonstrated that myocardial heart failure is associated with increased oxidative stress and abnormal excitation-contraction coupling (ECC) characterized by depletion of sarcoplasmic reticulum (SR) Ca2+ stores and reduction in Ca2+-transient amplitude associated with oxidative modification of thiols in both SR Ca2+-ATPase (SERCA) and Na+/Ca2+-exchanger (NCX) [6], [7]. In addition, although there are some contradictions between the experimental results in the literature, it is pointed out that increased oxidative stress, induced by reactive oxygen and nitrogen species (ROS/RNS) derived via hyperglycemia, has important contribution, directly and/or indirectly, to the structural and functional damages in the diabetic cardiomyocytes [8], [9]. In both early and recent studies, depression in contraction and relaxation of cardiomyocytes from streptozotocin (STZ)-induced diabetic rats were found in parallel with reduced rate of rise and decline of intracellular Ca2+ transient elicited by electrical stimulation which were mostly attributed to anomalous SERCA and phospholamban (PLN) activities, hyperphosphorylation of SR Ca2+ release channel ryanodine receptors (RyR2), and in part to reduced NCX activity [3], [10], [11], [12], [13], [14].
Within the last decade, the role of RyR2 in the mammalian heart has been well-defined. Under physiological conditions, RyR2 controls Ca2+ release and regulates cardiac ECC in a manner of macromolecular complex that includes mainly protein kinase A (PKA), FK506 binding protein 12.6 (FKBP12.6 or calstabin2), and Ca2+-calmodulin kinase II (CaMKII). In heart failure, PKA-mediated hyperphosphorylation of RyR2 causes dissociation of calstabin2 from RyR2 which results in an abnormal Ca2+ leak through RyR2 leading to cardiac dysfunction [3], [15], [16], [17]. We and others showed that ventricular myocytes isolated from STZ-induced diabetic rat hearts exhibit increased frequency of spontaneous Ca2+ sparks leading to an increased basal [Ca2+]i which are related, in part, with a leaky SR associated with hyperphosphorylation of RyR2 and decreased protein level of FKBP12.6 in 4-week diabetic rat cardiomyocytes [3].
It has been also shown that intracellular basal free Zn2+ level (resting free Zn2+) can increase rapidly in cardiomyocytes due to Zn2+ release from intracellular stores by reactive, ROS/RNS [18]. Moreover, ROS/RNS have been proposed to contribute to direct and/or indirect damage to cardiomyocytes in diabetes [19], [20], providing a close relationship between both increased and deleterious effects of intracellular basal free Zn2+ level in heart.
Hyperadrenergic state is an important marker for increased risk of mortality in patients with heart failure, and therefore it is a logical basis as to why treatment with β-blockers reduces the rate of mortality of these patients, as well as restoring cardiac function in experimental animal studies [21], [22]. It is now well-documented that ligand-binding to β-adrenoreceptors (β-ARs) activates adenylyl cyclase via G-proteins, resulting in a marked elevation in cAMP and PKA activation. Indeed, β-ARs are downregulated in the diseased heart, and uncoupled from downstream signaling via G proteins [23]. Moreover, an early study by Feldman et al. [23] showed a relation between decreased cAMP production and thus PKA activity and contractile dysfunction in failing hearts, while a few studies examined the PKA phosphorylation–dependent RyR2 dysfunction in similar failing hearts [24].
Several studies have investigated the preventive role of various β-blockers on the development of heart failure by restoring RyR2 dysfunction [25], [26]. Furthermore, it was mentioned that non- selective β-blockers, aside from their β-blockage action [27], [28], [29], exert adrenoceptor-independent effects including scavenging of free radicals leading to controlled cellular redox status [30], [31]. We reported that chronic treatment with either timolol or propranolol demonstrates beneficial effects on heart function in male rats during increasing-age, whereas timolol, but not propranolol exerts similar beneficial effects in female rats [32], [33]. Additionally, our recently published data has demonstrated that chronic treatment with propranolol seems to prevent diabetes-related changes in heart function by controlling intracellular Ca2+ signaling and preventing the development of left ventricular remodeling in diabetic cardiomyopathy without any antioxidant action as systemic or targeting heart of STZ-rats [32]. Furthermore, in a cell culture study, Miyamoto et al. [34] showed that both nipradilol and timolol are potent protective agents against increased oxidative stress. Also, most important data related with direct ROS scavenging action of timolol are presented by [35] and [36] via a nice comparison with other β-blockers. Moreover, we showed previously a profound cardioprotection with timolol in a female rat model of aging-related altered left ventricular function via prevention of the antioxidant system dysfunction, including increased lipid peroxidation, decreased ratio of reduced glutathione to oxidized glutathione, and decreased activities of thioredoxin reductase and glucose-6-phosphate dehydrogenase of left ventricular heart samples [32]. All above data can provoke ones to investigate whether or not timolol action is different among the other known β-blockers in diabetic subjects.
Taken into consideration the preventive role of β-blockers on the structure and function of RyR2 macromolecular complex in various studies on both human and animal heart failure models, we aimed to investigate the mechanisms that underlie the benefits observed with β-blocker timolol treatment on diabetic cardiomyopathy. Our data showed that a long-term treatment of diabetic male rats with a β-AR blocker timolol prevented diabetes-induced depressed basal activity of the left ventricle. Moreover, we report for the first time that this important preventive effect of timolol is associated with its normalization action on the RyR2 macromolecular complex, balanced intracellular Ca2+ and Zn2+ homeostasis, and a balanced level of oxidant to antioxidant ratio in both heart and circulation. We also report that timolol-treatment significantly normalized depressed levels of some Ca2+ handling regulators, such as NCX and phospho-PLN to PLN ratio. These observations may account for some of the beneficial effects of β-ARs blockage with timolol in diabetic cardiomyopathy confirmed by severe heart dysfunction.
Materials and Methods
Induction of diabetes
Diabetes was induced by a single injection of streptozotocin (STZ, 50 mg/kg dissolved in 0.1 M citrate buffer at pH 4.5; intraperitoneal; Sigma-Aldrich) in 3-month-old male Wistar rats (weighing 200–250 g) following an overnight fast as described previously [9]. Blood glucose concentration >3-fold that of the age-matched control at both 7 days and 12 weeks post-STZ injection was the criterion for experimental diabetes. One group of diabetic rats was treated with timolol (5 mg/kg daily) for 12 weeks. All animals were handled in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH publication No. 85–23, revised 1996). The protocol is approved by the Committee on the Local Ethics of Animal Experiments of Ankara University (N°: 2007-11-38).
Langendorff-perfused cardiac function
The left ventricular developed pressure (LVDP), left ventricular end diastolic pressure (LVEDP) and the rates of changes in developed pressure (±dP/dt) of isolated hearts were measured as previously described [37].
Action potential recording
Papillary muscle strips isolated from left ventricle were used to monitor intracellular action potentials using a conventional glass microelectrode connected to a preamplifier as described previously [9]. Action potential parameters such as amplitude of action potential, membrane potential, and repolarisation phases at 75% and 90% (APD75, 90) were determined and compared between groups.
Cell isolation
Cardiomyocytes from rat hearts were isolated freshly as described previously [3]. The cells were suspended in HEPES buffer with 1 mM Ca2+ and 0.5% bovine serum albumin (pH 7.4) and were kept at 37°C prior to being used for the experiments.
Patch-clamp experiments
Whole-cell patch-clamp recordings were performed as described previously [3]. Briefly, L-type Ca2+ currents (ICa) were recorded in cardiomyocytes isolated from the left ventricle of the hearts at room temperature (22±2°C) in the presence of cesium to inhibit K+ currents. Na+ current was inhibited by a voltage ramp protocol from a holding potential of –80 mV to –50 mV. Patch pipettes (1.0–1.2 MΩ) were filled with a solution (in mM): 100 CsCl, 20 TEA-Cl, 10 EGTA, 5.4 ATP-Na2 and 10 HEPES; pH 7.3. Cells were held at –80 mV and the current amplitude was estimated as the difference between peak inward current and the current level at the end of the 200 ms pulse.
Global and local cytosolic Ca2+ measurements
Freshly isolated left ventricular myocytes were loaded with the fluorescent Ca2+ indicators either Fura-2 (4-µM Fura-2 AM) or Fluo-3 (2-µM Fluo-3 AM). Transient intracellular free Ca2+ concentration ([Ca2+]i) changes under electric-field stimulation (Ca2+ transients as fluorescence ratio changes) were measured from Fura-2 loaded cardiomyocytes at room temperature (21±2°C) as described previously [3]. The fluorescence ratio F340/380 of the emitted light (with a frequency of 10 Hz) on excitation at 340 and 380 nm was used as an indicator of intracellular free Ca2+ changes. Peak amplitude (difference between basal and peak F340/380 ratios; ΔF) time to peak fluorescence (TP) and half-decay time of fluorescence (DT50) shifts between groups were estimated by a trend fit to whole Ca2+ transients evoked by field stimulation.
Tiny local Ca2+ releases in quiescent cells, Ca2+-sparks were measured from Fluo-3 loaded freshly isolated cardiomyocytes as described previously [3]. Briefly, an X60 (numerical aperture of 1.2) water immersion objective was used for imaging cardiomyocytes (Leica, SP5). The 488 nm argon laser line was used to excite Fluo-3, and the emitted fluorescence was collected with a long-pass filter set at 505 nm. The parameters of fluorescence changes such as peak amplitude (ΔF/F0, where ΔF = F−F0; F was identified as local maximum elevation of fluorescence intensity over basal level, F0), TP, spatial width (full width at half-maximum intensity, FWHM), and full duration half maximum (FDHM) were calculated automatically by using ImageJ program.
In another group of experiments, we repeated the experiments in diabetic cardiomyocytes incubated with either timolol (10-μM) or glutathione (4-mM) for 1 hour at 37°C.
Measurement of resting levels of cytosolic Ca2+ and Zn2+
To monitor the resting (or basal) level of intracellular free Zn2+ as well as Ca2+ in quiescent cells, we used two different Zn2+ sensitive fluorescence dye-loaded cells, by using either a ratiometric Fura-2 (4-µM Fura-2 AM) for a PTI Ratiomaster microspectrofluometer (working with FELIX software; Photon Technology International) or a non-ratiometric FluoZin-3 (3-μM FluoZin-3 AM) for fluorescence spectrometer (Jasco FP-6500, Japan).
We utilized an indirect approach to monitoring intracellular free Zn2+ level in freshly isolated cardiomyocytes by which the fluorescence attributable to Zn2+ was quenched by chelating the free intracellular Zn2+ with the heavy metal chelator N,N,N’,N’-tetrakis(2-pyridylmethyl) ethylenediamine (TPEN) similiar to early studies by us and others [18], [38], [39], [40]. Our approaches were based on the assumption that chelation of Zn2+ by TPEN did not affect intracellular free Ca2+ or other heavy metal ions due to fact that TPEN has very high affinities for heavy metals, for example, Ka = 1010.27 M−1, 1014.61 M−1, and 1015.58 M−1 for Mn2+, Fe2+, and Zn2+, respectively [41], [42]. In addition, the dissociation constant for the complex Ca-TPEN is ∼40 µM, compared with 10−15.6 M for Zn-TPEN [41], indicating that only negligible amounts of intracellular Ca2+ would be bound to TPEN under normal conditions. We first performed in vitro calibrations of Fura-2 with Zn2+ and Ca2+ in a manner similar to those described at 37°C in a manner similar to those described previously [18], [38], using various Zn2+- and Ca2+-buffered solutions with EGTA and nitrilotriacetic acid, and the equation given in our previous study is used to fit the data considered competitive binding between Zn2+ and Ca2+ for Fura-2 [18], [38]. The Rmin, Rmax,Zn, and Rmax,Ca were determined directly from Fura-2 loaded cardiomyocytes exposed to calibration solutions supplemented with 1 µM digitonin to hyperpermeabilize the cell membrane. In here, we did not aim to quantitate either the Zn2+ or Ca2+, we just presented fluorescence ratio changes for both Zn2+ or Ca2+, and results are presented as % of the control.
To monitor the basal levels of intracellular free Zn2+ and Ca2+, we repeated the above measurements in FluoZin-3AM loaded quiescent cells by using a fluorescence spectrometer (Jasco FP-6500, Japan). FluoZin-3 is highly selective for Zn2+ [43] and is not perturbed by Ca2+ or Mg2+ [40]. The fluorescence level corresponding to cytosolic free Zn2+ is calculated by using [Zn2+]i = KdX(F-Fmin) /(Fmax-F) formula, where the Kd for FluoZin-3 is 15 nM. Fmax and Fmin represent the maximum fluorescence intensity (with 10 µM a zinc-ionophore of 1-hydroxypyridine-2-thione, ZnPT) and the minimum fluorescence intensity (with 50 µM TPEN) while F represents the measured basal intensity. The intrinsic fluorescence measurements were performed on fluorescence spectrophotometer (Jasco FP-6500, JAPAN) with a Cuvette and temperature-controlled water bath. Same amount of cardiomyocytes (∼3000 cells/cuvette) for every experiments, placed into a cuvette which is stirred up with a small magnet for measuring the basal level of Zn2+ by spectrophotometer. Florescence intensities were acquired at 1 Hz, 490-nm excitation wavelength and collected at 525-nm. The fluorescence emissions were derived after subtracting of auto-florescent of the cells. Results are presented as % of control.
Although most of the published data demonstrated that both Fura-2 and FluoZin-3 have very high sensitivity to free Zn2+ rather than the other heavy metal ions [18], [38], [39], [43] while a metal-chelator TPEN has very high affinity to Zn2+ [40], [41], [42], yet there is limitation to monitor intracellular free Zn2+ and it is not possible to exclude even any little contribution of other ions, including Ca2+ or Mg2+.
To asses SR Ca2+ load experiment, caffeine-induced Ca2+ transients were induced in Fura-2 loaded cardiomyocytes by a rapid application of 10-mM caffeine as described previously [3].
Western blot analysis
For preparation of tissue homogenates, frozen heart samples from left ventricle were crushed at liquid N2 temperature and then homogenized to measure the phosphorylation and protein levels of contractile machinery complex as described previously [3] (CaMKII, phospho-CaMKII-Thr286, PKA, phospho-PKA-Thr198, FKBP12.6, RyR2, phospho-RyR2-Ser2808, Na/Ca-exchanger (NCX1), sarcoplasmic reticulum Ca-ATPase (SERCA2), phospholamban (PLN), phospho-PLN-Thr17, and β-actin were identified using specific antibodies with recommended dilutions from companies of either Santa Cruz biotechnology, USA or Badrilla Ltd., UK. Density analysis of protein bands was performed using Image J programme.
The similar Western blot analysis was also performed in the diabetic rat cardiomyocytes from left ventricle incubated with either timolol (10-μM) or zinc-ionophore of 1-hydroxypyridine-2-thione (ZnPT) (1 or 10- μM) for 20–30 min at 37°C.
Determination of protein-thiols
Oxidized and free levels of protein-thiols (protein-SH) were measured in heart homogenates as described previously [20].
Measurement of β-adrenergic receptor density
Density of total β-adrenergic receptors in crude membrane preparations from ventricular parts of the hearts were measured as described previously [28]. Briefly, a single concentration of 125I-cyanopindolol was used at a concentration of 800 pmol/L (80 times of its Kd value) to saturate β-AR. Nonspecific binding was determined in the presence of 100 µmol/L of unlabeled timolol and specific binding was calculated as the difference between total and nonspecific bindings.
Measurement of total oxidant and antioxidant status
Total oxidant status (TOS) and total antioxidant status (TAS) measurements were performed in both the left ventricular heart homogenates and plasma by using commercial kits (Rel Assay Diagnostics). TOS measurement was based on the oxidation of the ferrous ion–o-dianisidine complex to ferric ion by the oxidants present in the sample. The assay was calibrated with H2O2 and the results are expressed in terms of μmol H2O2 equivalent per liter.
For the TAS assay, the reduced 2,2′-azino-bis (3-ethylbenz-thiazo-line-6-sulfonic acid) (ABTS) molecule was oxidized to ABTS.+ by using hydrogen peroxide alone in acidic medium (the acetate buffer 30 mmol/L, pH 3.6). Antioxidants present in the sample accelerate the bleaching rate to a degree proportional to their concentrations. This reaction can be monitored spectrophotometrically and the bleaching rate is inversely related with the total-antioxidant status (TAS) of the sample. The reaction rate is calibrated with Trolox standard (an analog of vitamin E) and is expressed as mmol Trolox equivalent per liter.
Direct measurements of timolol antioxidant activity and antioxidant status
Using the same principle and method mentioned in the previous section, the assay was calibrated with hydrogen peroxide (H2O2) and the results are expressed in terms of H2O2 equivalent per liter (μmol H2O2 Equiv./L). We used increasing concentrations of timolol (in μM; 10-30-100-300) and measured the absorbance changes (at 530 nm) of H2O2 induced signal and evaluated the data as antioxidant activity.
For the second part of measurement, the assay was calibrated with a stable antioxidant standard solution which is traditionally named as Trolox Equivalent. The change of absorbance at 660 nm is related with total antioxidant level of the samples (increasing timolol concentrations in μM; 10-30-100-300). We measured the capacity of the samples to reduce chromogen ABTS and evaluated the data as antioxidant status.
Data analysis
Groups were tested and compared using one-way ANOVA and Tukey post hoc test. Values of p<0.05 were taken as statistically significant. Significant levels are given in the text, and data are presented as mean ± SEM.
Results
General effects of 12-week timolol-treatment of diabetic rats
As a typical model of type 1 diabetes, STZ-injected rats displayed hyperglycemia as indicated by significant increases in water intake and plasma glucose level compared with age-matched controls starting from week 1 until week 13 after STZ-injection. Timolol-treatment had no significant effect on plasma glucose level; however, it improved diabetic symptoms by significantly reducing weight loss although the weight of the subjects remained less than that of the controls (Fig. 1A). Cardiac hypertrophy that occurred during diabetes was also prevented by timolol. The mean cell capacitance of the untreated diabetic group was significantly higher (229.7±9.8 pF, ncell = 26 and nrat = 6) than that of the control (193.5±11.3 pF, ncell = 20 and nrat = 6), but it was not significantly different in the timolol-treated diabetics compared to the controls (181.7±6.5 pF, ncell = 34 and nrat = 7).
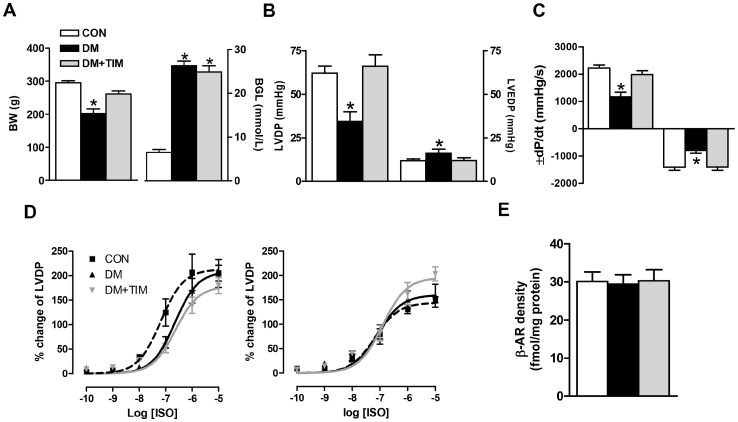
Figure 1. Timolol treatment prevents cardiac dysfunction via normalizing basal mechanical activity.
(A) Body weights (left) and blood glucose levels (right) of the rats at the end of the 12-week experimental period. Left ventricular developed pressure, LVDP (B, left) and left ventricular end diastolic pressure, LVEDP (B, right), the rates of changes in the developed pressure (±dP/dt) (C). Bar graphs in A to C represent mean ± SEM values from control, diabetic, and timolol-treated diabetic groups (number of rats in the groups; nCON = 18, nDM = 24, and nDM+TIM = 18, respectively) Effects of submaximal concentrations of a non-specific agonist, isoproterenol (ISO) on LVDP responses measured in short-term (left) and long-term (right) timolol-treated as well as untreated diabetic rats (D). Concentration–response curves for ISO represent the inotropic responses as % of their initial values and the LogEC50 value, which is equal to the concentration required to produce 50% of the maximal response induced by the agonist as determined from log-probit plots of individual response vs. concentration. LogEC50 values for ISO responses: −7.2±0.2, −6.6±0.2, −6.6±0.1 for short-term (4-week) protocol groups and −7.2±0.1, −7.1±1.2, −6.9±0.1 for long-term (12-week) protocol groups, in CON (n = 7/8 for 4-week/12-week), DM (n = 6/7 for 4-week/12-week), and DM+TIM (n = 7/7 for 4-week/12-week), respectively. The total β-AR density was measured in the crude membrane preparation from the hearts of long-term protocol groups by using saturation-binding technique with 125I-cyanopindolol (E). Bar graphs and the data points in each curve represent mean ± SEM values from CON (n = 6), DM (n = 7), DM+TIM (n = 6) groups. Significant at *p<0.05 vs. CON.
Cardiovascular function was evaluated by left ventricular (LV) hemodynamic analysis. For comparison as preliminary data, we used either short-term (4-week) or long-term (12-week) timolol-treatment. The basal contractile activity of the heart (left ventricular developed pressure, LVDP) from either 4-week or 12-week diabetic rats was found to be depressed compared to that of the age-matched controls. Timolol-treatment of diabetic rats either short-term or long-term exerted a significant preventive effect on the depressed basal contractile activity of the heart. The LVDP and end diastolic pressure, LVEDP, and maximum rate of rise/fall of LVDP (±dP/dt) in 12-week timolol-treated or untreated diabetic rat heart are given in Fig. 1B and C. Timolol-treatment either short-term or long-term of diabetic rats exerted similar but significant preventive effect on the depressed basal contractile activity of the heart.
We previously reported a significant decrease in the potency of isoproterenol (ISO) on LVDP in 4-week diabetic male rats without a significant change in the maximum response [44]. As can be seen from Fig. 1D (left), a 4-week timolol-treatment of diabetic rats did not affect the ISO responses measured with LVDP changes. In a 12-week timolol-treatment of diabetic rats, the maximum ISO response measured with 10−5 M was found to be slightly but significantly increased (without any effect in LogEC50) in the treated diabetic group compared with those of both untreated diabetic and age-matched control groups (Fig. 1D, right). Besides, β-ARs densities were similar in myocardial membranes from control and diabetic rats and not modified after chronic timolol-treatment (Fig. 1E).
Timolol-treatment prevents changes in cardiac electrical activity of the diabetic rat heart
Diabetes significantly prolonged the action potential duration (APD), mainly the repolarizing phase at 75% and 90% repolarization (APD75 and APD90) in isolated left ventricular papillary muscles (Fig. 2A and B). Timolol-treatment significantly prevented the prolongation in action potential observed in the untreated diabetic rat heart. The resting membrane potential of 6-month-old diabetic rats (−70.5±0.7 mV) was significantly more depolarized than age-matched controls (−74.4±1.3 mV). Timolol-treatment of the diabetic rats maintained the resting membrane potential (−73.8±0.9 mV).
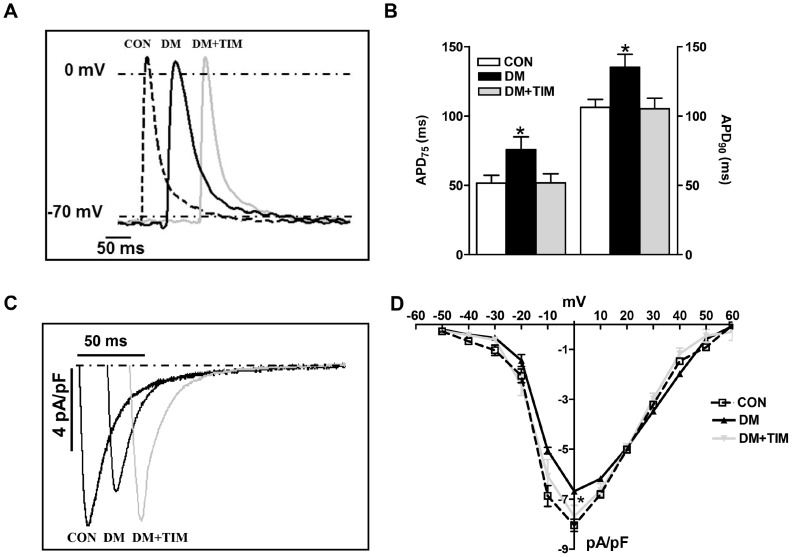
Figure 2. Timolol treatment restores prolonged action potential duration in the papillary muscle strips of the left ventricle and the depressed L-type Ca2+-channel currents in the ventricular cardiomyocytes from the diabetic rat heart.
(A) Representative intracellular action potential recordings in papillary muscle strips from left ventricle (inset). In here, traces are shifted for sake of clarify. (B) The mean changes in the action potential duration (as % repolarization at 75, 90; APD75,90) are presented as bar graphs (represents mean ± SEM from control, CON with white bars; from 8 rats, diabetic, DM with black bars; from 7 rats, and timolol treated diabetic rats, DM+TIM with gray bars; from 8 rats). (C) Representative L-type Ca2+-channel currents recorded at 0 mV depolarization (inset; time shifted for clarity), and (D) current–voltage relationship as current density (calculated by dividing their amplitude to their cell capacitance) in freshly isolated cardiomyocytes from control, diabetic and timolol-treated diabetic rats (CON; n = 20 cells from 6 rats, DM; n = 26 cells from 6 rats, and DM+TIM; n = 34 cells from 7 rats). Currents were recorded at room temperature (22±2°C) in the presence of cesium to inhibit K+ currents and Na+ current was inhibited after a voltage ramp protocol from a holding potential of –80 mV to –50 mV. Voltage pulses were applied from a holding potential of −80 mV to between −60 mV and +60 mV, with 10 mV voltage-steps. Data points on the curves represent mean ± SEM values. Significant at *p<0.05 vs. CON.
To determine whether a change in L-type Ca2+ -currents (ICaL) contributes to these changes in the electrical activity, ICaL was examined by using the whole cell patch-clamp technique. In contrast to our previous study with 4-week-old diabetic rats [3], ICaL densities recorded at various membrane potentials were significantly reduced in cardiomyocytes from 12-week diabetic rats when compared to that of age-matched controls (Fig. 2C and D). ICaL densities at 0 mV were −6.5±0.5 pA/pF and −8.1±0.5 pA/pF in the untreated diabetic and control groups, respectively while the time courses of these currents were similar among the groups (inactivation time course of ICaL was calculated by fitting the curve traces by two exponential equations as described previously, [45] (data not given). Timolol-treatment significantly prevented ICaL decrease (−7.8±0.4 pA/pF) without any effect on the time course of the currents. Although slower time constants were generally associated with smaller ICaL densities, we have similar time courses with smaller current densities in the diabetic group. In addition, we calculated the quantity of total electrical charges carried by ICaL over a 200 ms depolarizing period at 0 mV. The total electrical charges carried by ICaL at 0 mV in the untreated diabetic group was significantly less (3.0±0.7 amol/pF) than in the control group (4.0±0.7 amol/pF), while this decrease in the diabetic group was partially but significantly prevented with timolol-treatment (3.5±0.6 amol/pF).
Timolol regulation of intracellular global Ca2+ changes
To further understand the restoring effects of timolol on diabetic rats, we first performed some additional experiments to monitor [Ca2+]i transients elicited by electrical-field stimulation of cardiomyocytes. In line with our previous observations on 5-week STZ-induced diabetic cells [3], the mean peak amplitude of ΔF340/380 was significantly smaller in 12-week diabetics than in the control cells (Fig. 3A and B). Furthermore, time-to-peak amplitude (TP) and half-time for recovery (DT50) of the Ca2+ transients recorded from untreated diabetic rat cells were significantly prolonged compared with that of the control (Fig. 3C). Timolol-treatment of STZ-diabetic rats for 12-week prevented markedly both the depression in the fluorescence intensity and the prolongation in the time course of the intracellular Ca2+ transients (Fig. 3A and B). The averaged diastolic value of ΔF340/380 (basal level of intracellular free Ca2+) in cardiomyocytes from untreated diabetic rat heart was found to be significantly higher than that of age-matched control, and timolol-treatment prevented the increase in basal level of intracellular free Ca2+ (Fig. 3B; middle and left bars).
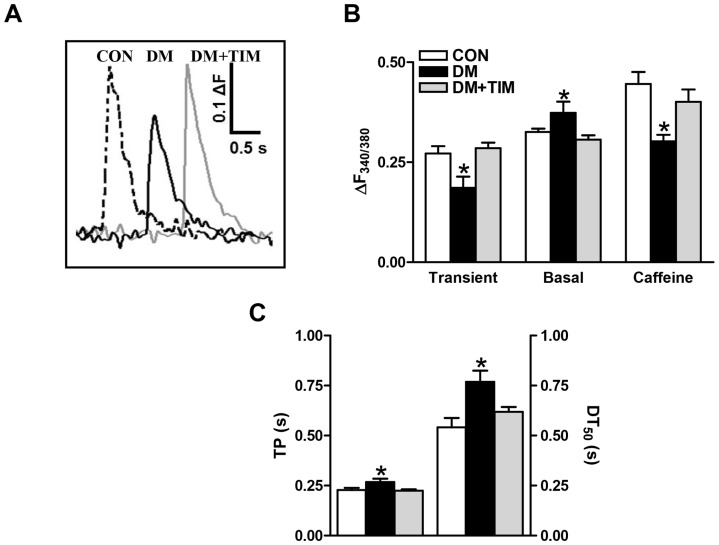
Figure 3. Effect of timolol treatment of diabetic rats on intracellular global Ca2+ changes.
(A) Representative Ca2+ transients in freshly isolated cardiomyocytes loaded with Fura-2 and field-stimulated at 0.2 Hz, (B) changes in peak amplitude of the fluorescence related with global Ca2+ transients (ΔF340/380 = F340/380Peak-F340/380Basal) (left), basal level of intracellular Ca2+ (middle), and caffeine-induced peak Ca2+ transients elicited in the cardiomyocytes (right), and the effect of timolol-treatment of diabetic rats (DM+TIM) on the time course (time to peak fluorescence, TP and half-decay time of fluorescence (left), DT50 shifts between groups were estimated by a trend-fitting to whole Ca2+ transients evoked by field stimulation of intracellular global Ca2+ changes (right) recorded from freshly isolated ventricular cardiomyocytes (C). Bar graphs represents mean ± SEM of 12–17 cells from at least 5 animals for each group protocol. Significant at *p<0.05 vs. CON.
Caffeine application on cardiomyocytes caused a sudden and transient increase in the intracellular free Ca2+ due to Ca2+ release from the sarcoplasmic reticulum, SR. The size of the caffeine-induced Ca2+ transient has been used to assess the SR-Ca2+ load of cardiomyocytes from control and diabetic rats as well as timolol-treated diabetic rats. To assure stable SR-Ca2+ load, cells were first stimulated, then caffeine (10-mM) was rapidly applied 30 s after cessation of electrical stimulation. The caffeine-induced Ca2+ transient recorded in cardiomyocytes from diabetic rats was smaller than that of the control one, while the caffeine-induced Ca2+ transient was not significantly different in timolol-treated diabetics compared to that of the control (Fig. 3B; right bars), implying that timolol-treatment maintained SR-Ca2+ load.
Timolol regulation of intracellular basal free Zn2+ level
Under both in vitro and in vivo conditions, exogenously enhanced oxidative stress or diabetes-induced oxidative stress is known to increase the basal levels of intracellular free Ca2+ and, as well, Zn2+ which is a strong indicator of the cellular level of oxidative stress in cardiomyocytes [18], [20]. For an assessment of possible antioxidant effects of timolol, first we compared the changes induced by either timolol or reduced glutathione, GSH treatment of cardiomyocytes from diabetic rats compared to age-matched controls. Incubation of diabetic cardiomyocytes with either 10-μM timolol, or with 4-mM GSH for 1 hour enhanced the intensity of fluorescence related with intracellular free Ca2+ transients under electric-field stimulation, and also significantly shortened their time courses (Fig. 4A and B). In addition, incubation for 1 hour of diabetic cardiomyocytes with either 10-μM timolol or with 4-mM GSH markedly prevented the increases in the basal levels of intracellular free Zn2+ and Ca2+ (by using either Fura-2AM or FluoZin-3AM), while these compounds did not affect the basal Zn2+ level in control cells (Fig. 4C and D, respectively).
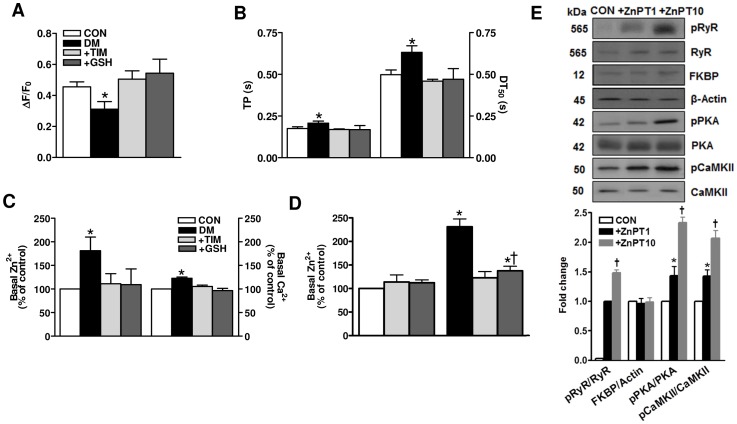
Figure 4. Acute effect of timolol on intracellular global Ca2+ changes, and the basal levels of intracellular both free Zn2+ and Ca2+ in ventricular hyperglycemic cardiomyocytes.
(A) Incubation of diabetic cardiomyocytes with either 10-μM TIM or, for comparison 4-mM GSH for 1 hour enhanced the intensity of intracellular free Ca2+ transients under electric-field stimulation at 0.2 Hz (left) and shortened their time courses as well, significantly (right) (B). Diabetic cardiomyocytes were incubated for 1 hour with either 10-μM TIM or 4-mM GSH. (C) To record basal levels of both intracellular free Zn2+ and Ca2+ in resting cells in parallel, we used a ratiometric Fura-2 (4-µM Fura-2 AM) loaded cells and 50-µM N,N,N′,N′-tetrakis (2-pyridylmethyl) ethylenediamine (TPEN) (for more information about methods, see [28]). (D) FluoZin-3 (3-μM FluoZin-3 AM) loaded cells used to measure basal level of intracellular free Zn2+. Incubation of cardiomyocytes isolated from either normal or diabetic rat hearts with either TIM or GSH did not affect FluoZin-3 intensity related with basal level of intracellular free Zn2+, while these both incubations induced significant decreases the increased FluoZin-3 intensity in the diabetics. (E) Incubation of cardiomyocytes with a zinc-ionophore of 1-hydroxypyridine-2-thione (ZnPT; 1-μM and 10-μM) at 37°C for 20–30 min did not affect total protein levels of RyR2 and its accessory protein of RyR2 macromolecular complex FKBP12.6 and two important kinases PKA and CaMKII while phosphorylation levels of RyR2 as well as PKA and CaMKII (pPKA and pCaMKII, respectively) increased markedly with ZnPT incubation in a concentration-dependent manner. Values for controls (CON; nrat = 5, ncell = 25), diabetics (DM; nrat = 5, ncell = 30), TIM- or GSH-incubated (+TIM or +GSH) diabetics (nrat = 6, ncell = 24 or ncell = 22), and ZnPT incubated controls (nrat = 5, ncell = 30 for each protocol) are expressed as mean ± SEM. Significant at *p<0.05 vs. CON.
Zinc ion is essential for numerous cellular functions although it is toxic for live cells [46]. Zinc ion homeostasis is therefore dynamically maintained by a variety of transporters, stores, and other proteins distributed in distinct cellular compartments. For assessment of the possibility of increased intracellular basal Zn2+-induced RyR2 hyperphosphorylation, which may in turn contribute to the cardiac dysfunction in diabetic subjects, we measured the phosphorylation levels of RyR2 with respect to its protein level with a zinc-ionophore of 1-hydroxypyridine-2-thione (ZnPT) under in vitro conditions. As can be seen from Fig. 4E, total protein levels of both RyR2 and accessory protein of RyR2 macromolecular complex, FKBP12.6 were not affected with either 1 µM or 10 µM ZnPT incubation (at 37°C for 20–30 min) of cardiomyocytes freshly isolated from control group rats. However, we measured significantly increased phosphorylation levels of RyR2 with these two ZnPT incubations in a concentration-dependent manner (Fig. 4E). The last data further support the hypothesis that Zn2+ disbalance results in a signaling disbalance caused by a local surplus of Zn2+ interfering with cellular signaling networks.
It is well-accepted that intracellular free Zn2+ plays critical roles in the redox signaling pathway and maintaining the normal structure and physiology of various cell types [18], [38], [47]. In addition, it has been shown that Zn2+ has multiple functional effects on Ca2+/calmodulin-dependent protein kinase II (CaMKII) [48], [49] while divalent metal ions influence catalysis and active-site accessibility in the cAMP-dependent protein kinase [50]. In order to demonstrate possibility of higher phosphorylation levels of two different kinases (PKA and CaMKII) with increased intracellular Zn2+, which are responsible from hyperphosphorylation of RyR2 under pathological conditions, rather than a direct hyperphosphorylated-RyR2 with Zn2+, in another set of experiments, we measured the phosphorylation levels of both PKA and CaMKII (with respect to their protein levels) with ZnPT exposures, under in vitro conditions. As can be seen from Fig. 4E, their phosphorylation levels are increased with ZnPT in a concentration-dependent manner while their protein levels were not changed with these exposures. Therefore, although it needs further experiments, it is tempting to supeculate a possible pathway for hyperphosphorylated-RyR2 via induction of intracellular free Zn2+-dependent PKA-/CaMKII-phosphorylation in our experimental conditions performed in freshly isolated cardiomyocytes.
Timolol regulation of intracellular local Ca2+ changes
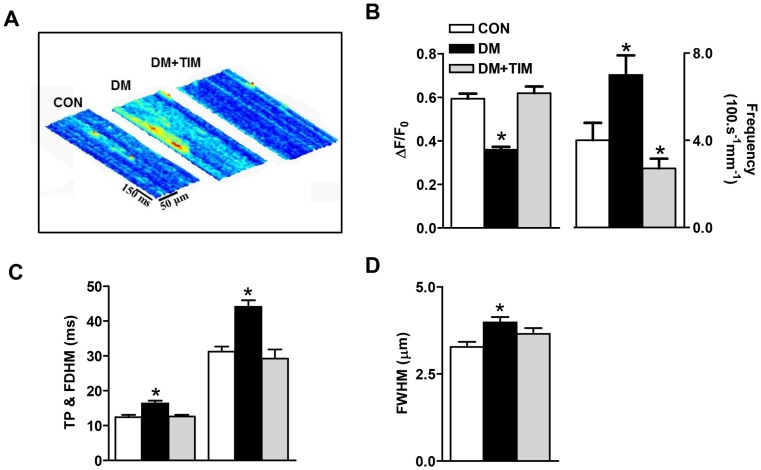
The contribution of elementary Ca2+ release, Ca2+ sparks, to decreased Ca2+ content of SR and increased basal Ca2+ level was examined in cardiomyocytes isolated from the hearts of a 6-month-old control, a 12-week STZ-induced diabetic, and a 12-week timolol-treated diabetic rats. Representative line-scan images are displayed in Fig. 5. The maximum fluorescence intensity, determined as ΔF/F0 at the peak of Ca2+ sparks and spontaneous Ca2+-spark frequency were calculated from individual gamma distribution function fits (Fig. 5A and B). The two parameters were significantly changed with respect to age-matched controls with a marked reduction in peak Ca2+ sparks and a marked increase in their occurrence frequency during diabetes. Time-to-peak (TP), full duration half maximum (FDHM) and full width at half-maximum intensity (FWHM),of the peak Ca2+ sparks were also found to be significantly enhanced in untreated diabetics (Fig. 5C and D, respectively). Timolol-treatment of the diabetic rats significantly prevented diabetes-induced changes in all Ca2+ sparks parameters.
Figure 5. Prevention of increased intracellular basal free Ca2+ with timolol in diabetic cardiomyocytes is closely correlated with restoration in Ca2+ spark parameters.
(A) Representative 3D-reconstruction of a representative line-scan recordings demonstrate the characteristic spreads of fluorescence in space and time in freshly isolated cardiomyocytes from three groups of rats. (B) Bar graphs from control (CON), diabetic (DM), and timolol treated diabetic rats (DM+TIM) are representing peak amplitude (left) and frequency (right), (C) time to peak amplitude TP (left) and full duration at half maximum, FDHM (right), and (D) full width of half maximum of Ca2+ sparks (nrat = 5, ncell = 44, nspark = 150; nrat = 5, ncell = 55, nspark = 165; nrat = 5, ncell = 38, nspark = 135 in control CON, diabetic DM, and timolol-treated diabetic DM+TIM groups, respectively). Significant at *p<0.05 vs. CON.
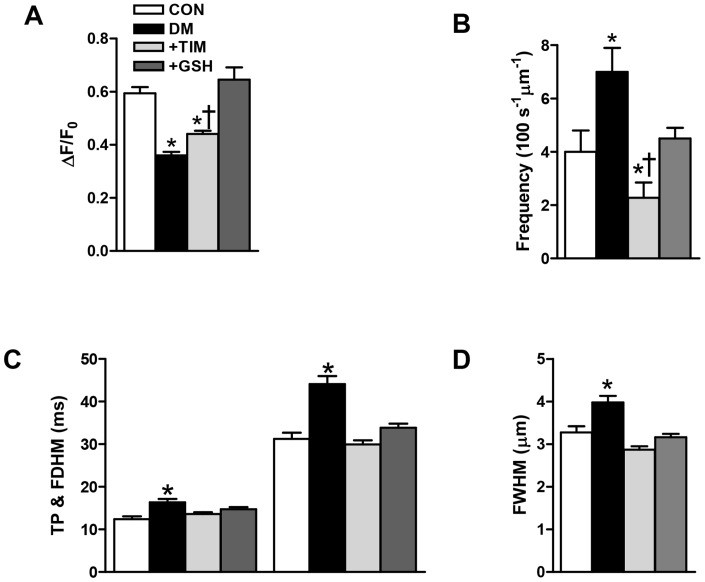
Of note, essentially similar results on Ca2+-spark intensity and frequency were obtained after 1 hour incubation with 10-µM timolol or 4-mM GSH of cardiomyocytes isolated from diabetic rats, although at these concentrations GSH appeared more potent than timolol (Fig. 6A–D, respectively).
Figure 6. In vitro experiments with either timolol or glutathione confirmed the cardioprotective effects of timolol via prevention of increased basal free Ca2+ in diabetic cardiomyocytes due to a restoration in Ca2+ spark parameters.
Effects of either 10-μM TIM or 4-mM GSH incubation of diabetic cardiomyocytes for 1 hour on the fluorescence changes related with Ca2+ sparks amplitude (A), sparks frequency (B), time to peak amplitude TP (left) and full duration half maximum, FDHM (right) (C), and full width of half maximum of the Ca2+ sparks (D). Bars represent control (CON; nrat = 5, ncell = 30, nspark = 102), diabetic (DM; nrat = 5, ncell = 35, nspark = 122) and TIM or GSH incubated (+TIM or +GSH) diabetic (nrat = 6, ncell = 38 or ncell = 32, nspark = 120 or nspark = 104) groups, respectively. Values are expressed as mean ± SEM. Significant at *p<0.05 vs. CON, †p<0.05 vs. DM.
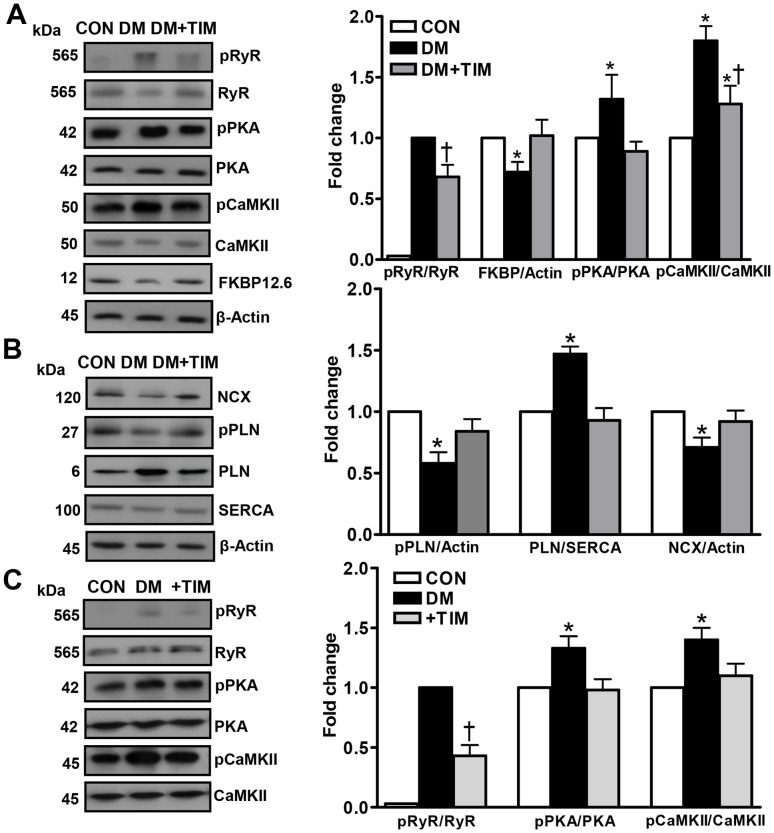
Timolol-treatment of diabetic rats affects biochemical properties of RyR2 macromolecular-complex
Under most pathological conditions including diabetes, alterations in the characteristics of intracellular basal free Ca2+ transients occur in combination with altered phosphorylated levels of RyR2 (pRyR2; 565 kDa phospho-RyR2-Ser2808). The pRyR2 level in heart homogenates of 6-month-old control, diabetic and timolol-treated diabetic rats was thus evaluated by using specific antibodies directed against RyR2 and its phosphorylated form. Similar to our previous studies [3], [51], diabetic group showed a significant decrease in protein level of RyR2 compared to the age-matched controls. Treatment with timolol reversed the depressed protein levels of RyR2 in the diabetic rats compared to the untreated diabetic rats (data not shown). Furthermore, in line with the previous studies, a marked hyperphosphorylation of RyR2 occurred in diabetic rats compared to the age-matched controls, while timolol-treatment of the diabetic rats significantly repressed this enhancement (Fig. 7A). The amount of FK506-binding protein (FKBP12.6) that stabilizes RyR2, thus preventing aberrant activation of the channel during the resting phase of the cardiac cycle, is decreased in the diabetic heart [3]. Similarly, timolol-treatment restored the FKBP12.6 protein level in diabetic rat heart (Fig. 7A).
Figure 7. Effects of timolol on phosphorylation and protein levels of both SR Ca2+ release channel (RyR2) and some Ca2+ handling regulators.
Data presented in (A) and (B) are obtained from homogenates from control (CON), diabetic (DM), and timolol treated diabetic (DM+TIM) rat hearts. (A) Left: representative Western blotting for 565 kDa phospho-RyR2-Ser2808 (pRyR2) and total RyR2, 42 kDa phospho-PKA-Thr198 (pPKA) and PKA, 50 kDa phospho-CaMKII-Thr286 (pCaMKII) and CaMKII, 12 kDA FKBP12.6, and 45 kDa β-actin, respectively. Right: quantification for the ratio of pRyR2 to RyR2, FKBP12.6 to β-actin pPKA to PKA, and pCaMKII to CaMKII, respectively. (B) Left: Western blotting for 120 kDa sarcolemmal NCX, 27 kDa phopho-PLN (Thr-17) and 6 kDa total PLN (L-15), 100 kDa SERCA2 (N-19), and 45 kDa β-actin, respectively. Right: quantification for the ratio of pPLN/actin, PLN/SERCA, and NCX/actin, respectively. The parameters given in section (C) are presented for ratio of 565 kDa pRyR2 to total RyR2, pPKA/PKA, and pCaMKII/CaMKII, respectively (right) in the isolated cardiomyocytes from the diabetic (DM) rats incubated with either 10-μM TIM (+TIM) or 4-mM glutathione, GSH (+GSH) (1 hour). Left: representative Western blotting for 565 kDa pRyR2 and total RyR2, 42 kDa pPKA (Thr198) and PKA, and 50 kDa pCaMKII-Thr286 and CaMKII, respectively. Bars represent mean ± SEM, n = 5–6 for hearts/group/protocol (double assays in each sample from each group for each type of measurement). Significant at *p<0.05 vs. CON and †p<0.05 vs. DM.
The phospho-PKA level, pPKA (42 kDa phospho-PKA-Thr198), known to activate RyR2 and induce Ca2+ release, was estimated in the heart homogenates from three groups of animals. There was no difference in PKA protein level between the treated and the untreated diabetic groups (data not shown), while there is a significant increase in the pPKA level of untreated diabetic group that was prevented significantly with timolol treatment (Fig. 7A). There were no significant differences in the protein levels of CaMKII (an important protein regulating of intracellular Ca2+ level among the treated diabetics) untreated diabetics, and the controls while there was a significant increase in phospho-CaMKII, pCaMKII (50 kDa phospho-CaMKII-Thr286) level of the diabetic group compared to that of the control. Timolol-treatment also significantly prevented this increase.
Effects of timolol-treatment of diabetic rats on total amount of SR Ca2+-ATPase (SERCA), sarcolemmal Na+/Ca2+-exchanger (NCX), phospholamban (PLN), and phospho-PLN
To test whether the depression in SR function was associated, in part, with any other Ca2+-handling regulators besides RyR2-macromolecular complex proteins, we analyzed the changes in total expression levels of SR Ca2+-ATPase (SERCA2; N-19 at 100 kDa) and total phospholamban (PLN; L-15 at 6 kDa), and the phosphorylated level of PLN (Thr-17 at 27 kDa) among the groups. Western blot analysis demonstrated that, compared with the control group, the level of PLN (129±10%) with respect to the β-actin and the ratio of PLN to SERCA (147±6%) were significantly different in the diabetic group and these were normalized significantly with timolol-treatment (Fig. 7B). On the other hand, either diabetes or timolol-treatment of diabetics did not affect significantly the SERCA levels (88±10% and 102±4%, respectively) with respect to that of the control. However, the phospho-PLN (relative to that of β-actin) in the diabetic group was found to be significantly depressed (50±9%) compared to that of the control, while it was normalized with timolol-treatment. Therefore, the calculated ratio of phospho-PLN to total PLN indicates a marked decrease in the diabetic group in comparison with the control group (39±9%), while again it was significantly prevented with timolol-treatment (73±13%).
The diabetic rats also displayed abnormal cardiac sarcolemmal Na+/Ca2+-exchanger (NCX1 at 120 kDa) protein level. NCX level was decreased significantly (71±12%) in the diabetic rats compared with that of the control, while timolol-treatment presented a significant preservation (92±11%) (Fig. 7B).
Acute effect of timolol in hyperglycemic cardiomyocytes under in vitro conditions
To assess further the antioxidant effect of timolol on diabetic cardiomyocytes, diabetic cardiomyocytes were incubated with timolol and then the RyR2 phosphorylation level was measured. Incubation of diabetic cardiomyocytes with 10-μM timolol for 1 hour significantly prevented the hyperphosphorylation level of RyR2 without any significant effect of its protein level (Fig. 7C). Timolol also significantly reduced the phosphorylated states of PKA and CaMKII in diabetic cardiomyocytes without any significant effect of their protein levels (Fig. 7C).
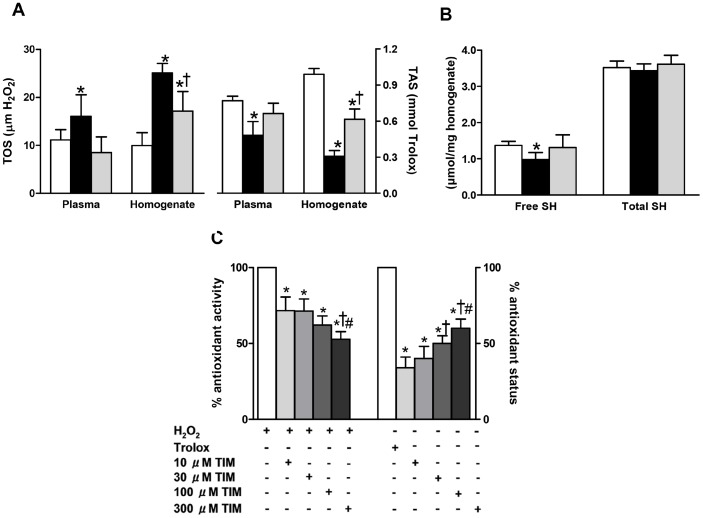
Timolol has antioxidant action in both circulatory system and myocardium of diabetic rats
To be well-known circulating plasma markers of oxidative stress in STZ-diabetic rats, increased total oxidant status (TOS) and decreased total antioxidant status (TAS) measured in plasma were significantly antagonized after timolol treatment of diabetic rats (Fig. 8A). To further explore whether the increased oxidative stress and decreased antioxidative defence system in chronic diabetic rats can also induce similar changes in the myocardium, we also analyzed the TOS and TAS levels in the heart homogenates. The TOS level was higher, while the TAS level was found to be lower in untreated diabetic rat heart homogenates compared with those of the controls. Significantly, timolol-treatment of diabetic rats for a 12-week period prevented these changes (Fig. 8A). The relative contents of free and total protein thiols were also analyzed in the heart homogenates of these three groups of rats. Free protein thiol content was markedly decreased in untreated diabetics compared to age-matched controls, and was restored with timolol-treatment, while the total protein thiols were found to be similar in these three groups (Fig. 8B).
Figure 8. Confirmation of antioxidant effect of timolol on the contractile activity of diabetic rat heart via using different biochemical approaches.
The total oxidant status measured with respect to H2O2 and the total antioxidant status measured with respect to trolox (A) in both plasma and heart homogenate of control rats (CON group; white bar) and diabetic rats without treatment (DM group; black bar) or with TIM treatment (DM+TIM group; gray bar) for 4-week following the one week of diabetic status confirmation. (B) The total and free protein thiol levels measured in heart homogenate of the groups. Bars represent mean ± SEM. The number of rats is 12–17 for rats/group/protocol. Significant at *p<0.05 vs. CON group, †p<0.05 vs. DM group. (C) In vitro antioxidant activity and antioxidant status of TIM was measured with colorimetric methods. Antioxidant activity of increasing concentration of TIM is evaluated with absorbance changes in H2O2-induced signal. Bar graphs represent mean ± SEM values for 10-30-100-300 μM TIM applications on H2O2 included samples for expressing antioxidant activity. Bar graphs represent mean ± SEM values from Trolox or 10-30-100-300 μM TIM applications on ABTS chromogen solution for expressing antioxidant status (triple assays in each sample for each type of measurement). Significant at *p<0.05 vs. H2O2 or Trolox, and †p<0.05 vs. 10-μM TIM, #p vs. 30-μM TIM.
To assess further the antioxidant effect of timolol in diabetic rat heart, in part due to its action on some modification of sulfhydryl groups in diabetic heart, as presented previously by an early study [52], the relative levels of both free and total protein thiols were also analyzed in the heart homogenates. The free protein thiol content was markedly decreased in the untreated diabetic rats compared with the age-matched controls, and they were restored with timolol-treatment, whereas the total protein thiols were found to be similar among these three groups (Fig. 8B).
Direct antioxidant action of timolol
To test whether the observed timolol effects in diabetic cardiomyocytes as well as diabetic rats are due to its putative scavenging activity for ROS (O2 −, H2O2, OH.), we investigated its direct antioxidant effect in H2O2-induced oxidant medium (Fig. 8C). Timolol exerted a clear antioxidant effect in this fully oxidized medium in a concentration-dependent manner. Also dose-dependently, antioxidant status of timolol was increased, respect to Trolox (well known antioxidant) solution. We repeated similar experiments with another β-blocker propranolol. Propranolol, at any concentration (from 10 to 1500 µM), did not show any antioxidant effect in the presence of H2O2, in the oxidized medium, as earlier reported by Gomes et al. [35] who suggested that timolol was more effective on ROS scavengers whereas an antioxidant role of propranolol was on the reactive nitrogen species (RNS) scavengers.
Discussion
The present data, in male rats with 12-week diabetes following streptozotocin injection, showed that simultaneous chronic treatment with timolol, a β-AR blocker, markedly prevented diabetes-associated cardiac alteration as evidenced by preserved left ventricular function and cellular electrical activity. The main finding of this study is to demonstrate an association of timolol effect in diabetic rat heart with normalization of the sarcoplasmic reticulum (SR) Ca2+ release channel ryanodine receptors (RyR2) macromolecular complex together with normalization of intracellular free Ca2+ ([Ca2+]i) homeostasis, including also the [Zn2+]i homeostasis. Our present study indicates that a treatment of the diabetic rats with a β-blocker, timolol prevented the depressed maximal contractile responses to isoproterenol, ISO stimulation slightly but significantly in a time-dependent manner similar to that of propranolol effect in the similar animal model [53], without affecting the total β-AR density. Our present data are in line with the previous data carried out with different β-blockers such as carvedilol, metroprolol, or atenolol, of which reduced left ventricular volume and improved cardiac function in diabetic rats [25], [26]. Beta-blockers are widely used for the treatment of cardiovascular and noncardiovascular diseases. Indeed, in even an early review article, it had been mentioned that severe heart failure due to idiopathic dilated cardiomyopathy could be improved in patients receiving beta-blocker therapy starting at a very low dose and followed by a stepwise increase depending on the treatment duration [54]. Nevertheless, although many patients were treated with metoprolol, carvedilol or bucindolol for periods of 2 to 12 months, their mechanism of action is not fully known. Furthermore, in here, timolol, itself demonstrates antioxidant activity and antagonizes the increased oxidative stress while some of its effects on [Ca2+]i and [Zn2+]i homeostasis were mimicked by reduced glutathione. Accordingly, we proposed that the beneficial effects of timolol-treatment on the cardiac activity in diabetic rats results, in most part, from its antioxidant properties.
Defective intracellular Ca2+ signaling contributes to cardiomyopathy in type 1 diabetic rats. In the previous studies, we and others have demonstrated that depression in both contraction and relaxation activities of Langendorff-perfused whole heart, reduced amplitude and prolonged time course of the Ca2+ transients, as well as increase in intracellular basal free Ca2+ level, are associated with anomalous Ca2+ pumping, Na+/Ca2+ exchange, and more recently to altered RyR2 behaviour as well as some Ca2+ handling regulators such as phospholamban (PLN) [3], [10], [11], [12], [13], [14]. In their study, Yaras et al. [3] reported that Ca2+-spark frequency of cardiomyocytes isolated from 5-week STZ-induced diabetic rats significantly increased with respect to aged-matched control rats while their amplitude is reduced. In this group of diabetic rats, spatio-temporal properties of the Ca2+ sparks were also significantly altered to being almost parallel to the changes of Ca2+ transients. In addition, RyR2 from diabetic rat hearts were hyperphosphorylated and protein levels of both RyR2 and calstabin2, FKBP12.6 depleted [3]. Here, our present data in cardiomyocytes from rats with 12-week diabetes reinforced the observations from 5-week diabetic rats. More importantly, in here, our data showed also a marked increase in the fluorescence ratio of basal [Zn2+]i besides that of the [Ca2+]i. Notably, it has been previously shown that exogenously applied oxidants caused about a 30-fold increase in the resting level of [Zn2+]i but only doubled in the [Ca2+]i in freshly isolated cardiomyocytes [18]. Furthermore, previous reports have shown that the basal free [Zn2+]i is increased by 70% in cardiomyocytes from male diabetic rats being parallel to an unbalanced oxidant-status/antioxidant capacity in the same heart preparations [20], and by over 200% in aldosteronism [55]. Coordinated changes in the basal [Ca2+]i and [Zn2+]i levels have recently been reported under experimental conditions (intracellular Zn2+ overload or intracellular Ca2+ decrease), as well as during a single beat (transients or elementary events) [28].
Zinc ion and redox status demonstrate a complex interplay in cells. The [Zn2+]i level is modulated by the redox state and the level of reactive oxygen species, ROS in cells [56] while Zn2+ increases the antioxidant capacity of the cells or leads to the release of toxic ROS [57]. Indeed, the [Zn2+]i distribution is linked to redox metabolism despite Zn2+ itself not being redox active and generally Zn2+-proteins being redox-inert. Therefore, it has been long viewed as a component of the antioxidant network, and growing evidence points to its involvement in redox-regulated signaling. Zinc-coordination environments with cysteine ligands have the remarkable property that the sulfur-ligands can be oxidized and then reduced with concomitant release and binding of Zn2+ [57]. About 30% of the Zn2+-buffering capacity emanates from sulfur donors (thiols) and thus serves as redox (oxidant) buffer capacity at the same time [56]. Moreover, Zn2+ elevates ROS, in living cells by inhibiting mitochondria [58] and activating NADPH oxidase [59] although it has been shown in an early study that oxidative phosphorylation rate and Mg2+-dependent ATPase activities were depressed in mitochondria from left ventricle of diabetic rat heart contributing into development of cardiomyopathy at late stages of diabetes [60]. However, in a recent work, it has been shown that both extra-and intracellular Zn2+ modulates L-type Ca2+ channel properties, as well as its regulation by β-adrenergic agonists independently of altering the cellular redox status [61]. The reduced Ca2+-current density that we observed in diabetic cardiomyocytes (Fig. 2D) might be attributable to the alteration in the intracellular basal free Zn2+, despite the fact that we were using the whole-cell perforated patch-clamp in which the cytolosic medium is in most part substituted by the intracellular pipette solution. In addition, our present work demonstrated, for the first time, that an increase in [Zn2+]i is associated with hyperphosphorylation of the RyR2 in a concentration-dependent manner, at most via phosphorylation of both PKA and CamKII under acute zinc-inophore ZnPT exposure rather than a direct hyperphosphorylaion of RyR2 with increased [Zn2+]i. This hypothesis depending on our observations is further supported with the data on multiple functional effects of [Zn2+]i on CaMKII and modulation of RyR1 binding to SR vesicles in skeletal muscle biphasically [48], [49]. Indeed, it is well-accepted that [Zn2+]i level plays critical roles in the redox signaling pathway and maintaining the normal structure and physiology of various cell types [62]. Therefore, it can be hypothetized that Zn2+ may compete with or substitute for metal ions crucial for the activity of signaling proteins. Accordingly, supporting this last statement, Zn2+ is also known to induce CaMKII autophosphorylation, inhibit protein tyrosine phosphatases [48] while divalent metal ions influence catalysis and active-site accessibility in the cAMP-dependent protein kinase [50]. In here, although a likely role for such [Zn2+]i signals is the modulation of protein phosphorylation, it is a strong possibility that both activated/phosphorylated CaMKII and PKA due to increased [Zn2+]i, turn into a hyperphosphorylated RyR2 under high extracellular Zn2+ exposure. Therefore, increased [Zn2+]i, most probably a contribution of increased [Ca2+]i, under increased oxidative stress together with depressed antioxidant-defence in the cells via hyperglycemia induces important defects in excitation-contraction coupling of cardiomyocytes. The Zn2+ -dependent RyR2 hyperphosphorylation thereby correlates a possible indirect contribution of increased level of [Zn2+]i into RyR2-dependent dysregulation of diastolic Ca2+ in diabetic cardiomyocytes. There are several Zn2+ signaling pathways involved in intracellular Zn2+ homeostasis. Possibly, Zn2+ disbalance results in a signaling disbalance caused by a local surplus of Zn2+ interfering with cellular signaling networks. Therefore, it can be clearly seen that the [Zn2+]i signaling can easily interfere with the the [Ca2+]i signaling of cardiomyocytes, particularly under pathological conditions, underlying, in part, cardiac dysfunction.
Therapeutic effects of β-adrenergic antagonists are generally explained by their capacity to block β-adrenoceptors (β-ARs), and β1-AR blockage has become the chosen therapy in the treatment of congestive heart failure [63]. It is one of general textbook information that any major injury that reduces cardiac pumping capacity activates neurohumoral mechanisms, including the sympathetic system. Under pathophysiological conditions, acute increase in norepinephrine serves as a fast and powerful mechanism that stabilizes perfusion of crucial organs by redirecting blood flow away from muscles, kidney, etc., and stimulating heart rate and developed force. However in pathological situations such as hyperglycemia or diabetes, if the primary pumping defect of the heart continues, the sustained increase in sympathetic tone turns from friend to foe, primarily for two reasons: first, peripheral vasoconstriction and increased load lead to reduced cardiac output; second, sustained stimulation of cardiomyocytes leads to an overproportional increase in cell death, fibrosis, and hypertrophy in cardiomyocytes. Collectively, these changes accelerate the decline of the heart function. In heart failure, the signaling cascade is normally desensitized in response to chronic norepinephrine stimulation. The diabetic heart is more susceptible to hypertensive or ischemic injury as a result of a number of pathological changes including cell death, increased oxidative stress, impaired Ca2+ handling, and alterations in second messenger signaling pathways. As summarized in the introduction, some of the beneficial cardiovascular effects of β-ARs blockage have already been shown to be associated with their antioxidant properties by scavenging endogenous oxidants [30], [31]. Indeed, oxidative stress plays several critical roles in the development of diabetic cardiovascular complications, including myocardial hypertrophy. Diabetes-induced heart dysfunction is associated with a very low plasma insulin level, and an unbalanced level of oxidative stress to antioxidant defense ratio, while oxidative stress in diabetic animals is reversed with antioxidants [20], [64]. To date, molecular mechanisms underlying the dysregulation of SR-Ca2+ release channel ryanodine receptors (RyR2) during chronic diabetes remains incompletely understood. However, alterations in the sensitivity of RyR2 to Ca2+ activation could result from oxidation of RyR2 by ROS and/or reactive carbonyl species (RCS) [17], [65], besides increases in phosphorylation by PKA at Ser2808 and by CaMKII at Ser2808 and Ser2814 sites [66]. In the present study, long-term timolol treatment maintains normal intracellular Ca2+ signaling in cardiomyocytes via preventing RyR2 hyperphosphorylation in STZ-injected rat hearts. A similar preserved channel regulation in RyR2 with improved cardiac function was previously shown by Doi et al. in tachycardia-induced canine heart failure [25] and by Tuncay et al. with propranolol treatment of diabetic rats [28]. In these studies, propranolol had no effect on the protein level of SERCA as opposed to a previous report describing an enhancement of SERCA expression and activity with β-blockers in human heart failure [67]. This discrepancy might be attributed to the different experimental dose of β-blockers used or a different regulation of β-ARs antagonism. Beta-blockers are widely used for the treatment of cardiovascular and non-cardiovascular diseases. Nevertheless, their mechanism of action is not fully known, and is significantly different from other agents in this class. Nonselective β-blockers such as propranolol, metoprolol, or carvedilol can exert adrenoceptor-independent effects including scavenging of free radicals and inhibition of PKC leading to controlled cellular redox status and consequently functional recovery in organs including the heart [36], [68]. Indeed, a direct radical scavenging effect of the β-blockers has also been previously [36]. In a cell-line study, Miyamoto et al. [34] put forward that both nipradilol and timolol maintained potent protective action against increased oxidative stress. In other studies carvedilol demonstrated a marked beneficial effect in heart failure via scavenging free radicals, preventing Ca2+ leak due to stabilization of RyR2 in hearts with a marked failure [68]. Further, in a recent study, we demonstrated a beneficial action with the chronic timolol treatment on age-related alterations in heart function of 12-month-old female rats via regulation of cellular redox status [32].
Cardiac dysfunction in diabetes arises from a number of alterations in Ca2+ handling in cardiomyocytes. These usually lead to depressed cardiac Ca2+ transients and to decreased contractile function. Typically, these defects in Ca2+ handling include depressed SERCA function and/or increased NCX activity [10], [11], [13], [14] that lead to decreased SR [Ca2+]. In addition, cardiomyocytes from diabetic hearts typically exhibit an increase in the diastolic leak of Ca2+ from the SR [3]. This increase is also primarily due to increased RyR2 hyperphosphorylation, while a possible contribution of NCX activity cannot be excluded. Indeed in diabetic hearts, associated with a decreased RyR2 protein level, there is a marked reduction of NCX protein. The latter, despite a reduced influx of Ca2+ ions through the L-Type Ca2+ channels may contribute to diastolic Ca2+ overload since total NCX activity should be reduced as there is no change in [Na+]i of diabetic cardiomyocytes [69].
Besides, compromised Ca2+ removal, one of the hallmarks of cardiac dysfunction including in diabetic cardiomyopathy [11], [13], [14] depends upon SERCA activity. Our classical knowledge emphasizes the importance of the fact that the amount of Ca2+ stored in SR depends, in part, on its balancing action, restoring the Ca2+ released during each cycle. SERCA is able to modulate this uptake under changing circumstances because it is regulated via an inhibitory protein, PLN which can be phosphorylated by both PKA and CaMKII at different sites of PLN [70], [71]. The molar ratio of PLN to SERCA can be conceived as a critical determinant of the contractile force and its regulation. This fact is also tested in this study: Diabetes induced a markedly increased phosphorylation level of PLN with unchanged levels of both PLN and SERCA, which are in line partially but not fully with previously published data [11], [13], [14]. The decreased PLN phosphorylation is consistent with not only the decreased function of SR but also with the absence of a hyperadrenergic state that is indicated by the slower heart rate in diabetic rats data [13]. Moreover, an early report by Kadambi et al. on targeted overexpression of PLN protein could cause cardiac contractile dysfunction is further supporting our present results [72].
Intracellular concentrations of redox-active molecules can significantly increase in the heart as a result of activation of specific signal transduction pathways or the development of certain pathophysiological conditions. Changes in the intracellular redox environment can affect many cellular processes, including the gating properties of ion channels and the activity of ion transporters [73]. Redox-mediated alterations of [Zn2+]i and [Ca2+]i homeostasis is directly involved in cardiac pathologies such as diabetes [18], [57]. Therefore, it can be suggested that redox modulation of biochemical pathways and signaling cascades related with either [Ca2+]i, [Zn2+]i, or both with any antioxidant can extend to normalize cardiac dysfunctions and other pathologies in diabetic subjects. On top of the marked antioxidant properties of timolol to scavenge ROS that might account, for the most part, for the prevention of the cardiac alterations in STZ-induced diabetic rats without affecting hyperglycemia, the regulation of [Zn2+]i should have a major importance despite of the fact that elevated [Zn2+]i might be helpful in offering protection from redox unbalance. In an early report from a study performed on a rodent heart with hereditary muscular dystrophy, [Ca2+]i overloading and oxidative stress are also accompanied by increased [Zn2+]i [74]. Besides, Kamalov et al [55] suggested that an optimal range of [Zn2+]i/[Ca2+]i ratio in cardiomyocytes and mitochondria must be preserved to combat oxidative stress. Thus, the increased cytosolic and mitochondrial free Ca2+ level are coupled to the induction of oxidative stress, while antioxidant effects result from the rise in cytosolic and mitochondrial [Zn2+] levels accompanied by a simultaneous activation of metal response element transcription factor-1, and its induction of such antioxidants as metallothionein-1 and glutathione peroxidase. However, with a long-term treatment, by maintaining both a cellular redox-status and [Zn2+]i level near to control level, timolol prevents the subsequent alterations in [Ca2+]i homeostasis including Ca2+ release by RyR2, which leads to major defects in cardiac activity.
Funding Statement
This work has been supported partially by grant from TUBITAK SBAG-111S042. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding received for this study.
References
- 1. Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, et al. (1972) New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol 30: 595–602. [DOI] [PubMed] [Google Scholar]
- 2. Fein FS, Kornstein LB, Strobeck JE, Capasso JM, Sonnenblick EH (1980) Altered myocardial mechanics in diabetic rats. Circ Res 47: 922–933. [DOI] [PubMed] [Google Scholar]
- 3. Yaras N, Ugur M, Ozdemir S, Gurdal H, Purali N, et al. (2005) Effects of diabetes on ryanodine receptor Ca release channel (RyR2) and Ca2+ homeostasis in rat heart. Diabetes 54: 3082–3088. [DOI] [PubMed] [Google Scholar]
- 4. Ganguly PK, Pierce GN, Dhalla KS, Dhalla NS (1983) Defective sarcoplasmic reticular calcium transport in diabetic cardiomyopathy. Am J Physiol 244: E528–535. [DOI] [PubMed] [Google Scholar]
- 5. Pierce GN, Kutryk MJ, Dhalla NS (1983) Alterations in Ca2+ binding by and composition of the cardiac sarcolemmal membrane in chronic diabetes. Proc Natl Acad Sci U S A 80: 5412–5416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Luo J, Xuan YT, Gu Y, Prabhu SD (2006) Prolonged oxidative stress inverts the cardiac force-frequency relation: role of altered calcium handling and myofilament calcium responsiveness. J Mol Cell Cardiol 40: 64–75. [DOI] [PubMed] [Google Scholar]
- 7. Kuster GM, Lancel S, Zhang J, Communal C, Trucillo MP, et al. (2010) Redox-mediated reciprocal regulation of SERCA and Na+-Ca2+ exchanger contributes to sarcoplasmic reticulum Ca2+ depletion in cardiac myocytes. Free Radic Biol Med 48: 1182–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cai L, Kang YJ (2001) Oxidative stress and diabetic cardiomyopathy: a brief review. Cardiovasc Toxicol 1: 181–193. [DOI] [PubMed] [Google Scholar]
- 9. Ayaz M, Ozdemir S, Ugur M, Vassort G, Turan B (2004) Effects of selenium on altered mechanical and electrical cardiac activities of diabetic rat. Arch Biochem Biophys 426: 83–90. [DOI] [PubMed] [Google Scholar]
- 10. Hattori Y, Matsuda N, Kimura J, Ishitani T, Tamada A, et al. (2000) Diminished function and expression of the cardiac Na+-Ca2+ exchanger in diabetic rats: implication in Ca2+ overload. J Physiol 527 Pt 1: 85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim HW, Ch YS, Lee HR, Park SY, Kim YH (2001) Diabetic alterations in cardiac sarcoplasmic reticulum Ca2+-ATPase and phospholamban protein expression. Life Sci 70: 367–379. [DOI] [PubMed] [Google Scholar]
- 12. Bidasee KR, Nallani K, Henry B, Dincer UD, Besch HR Jr (2003) Chronic diabetes alters function and expression of ryanodine receptor calcium-release channels in rat hearts. Mol Cell Biochem 249: 113–123. [PubMed] [Google Scholar]
- 13. Choi KM, Zhong Y, Hoit BD, Grupp IL, Hahn H, et al. (2002) Defective intracellular Ca(2+) signaling contributes to cardiomyopathy in Type 1 diabetic rats. Am J Physiol Heart Circ Physiol 283: H1398–1408. [DOI] [PubMed] [Google Scholar]
- 14. Bai SZ, Sun J, Wu H, Zhang N, Li HX, et al. (2012) Decrease in calcium-sensing receptor in the progress of diabetic cardiomyopathy. Diabetes Res Clin Pract 95: 378–385. [DOI] [PubMed] [Google Scholar]
- 15. Hasenfuss G (1998) Alterations of calcium-regulatory proteins in heart failure. Cardiovasc Res 37: 279–289. [DOI] [PubMed] [Google Scholar]
- 16. Marks AR (2000) Cardiac intracellular calcium release channels: role in heart failure. Circ Res 87: 8–11. [DOI] [PubMed] [Google Scholar]
- 17. Bidasee KR, Nallani K, Besch HR Jr, Dincer UD (2003) Streptozotocin-induced diabetes increases disulfide bond formation on cardiac ryanodine receptor (RyR2). J Pharmacol Exp Ther 305: 989–998. [DOI] [PubMed] [Google Scholar]
- 18. Turan B, Fliss H, Desilets M (1997) Oxidants increase intracellular free Zn2+ concentration in rabbit ventricular myocytes. Am J Physiol 272: H2095–2106. [DOI] [PubMed] [Google Scholar]
- 19. Malaiyandi LM, Dineley KE, Reynolds IJ (2004) Divergent consequences arise from metallothionein overexpression in astrocytes: zinc buffering and oxidant-induced zinc release. Glia 45: 346–353. [DOI] [PubMed] [Google Scholar]
- 20. Ayaz M, Turan B (2006) Selenium prevents diabetes-induced alterations in [Zn2+]i and metallothionein level of rat heart via restoration of cell redox cycle. Am J Physiol Heart Circ Physiol 290: H1071–1080. [DOI] [PubMed] [Google Scholar]
- 21. Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, et al. (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311: 819–823. [DOI] [PubMed] [Google Scholar]
- 22. Tsutsui H, Spinale FG, Nagatsu M, Schmid PG, Ishihara K, et al. (1994) Effects of chronic beta-adrenergic blockade on the left ventricular and cardiocyte abnormalities of chronic canine mitral regurgitation. J Clin Invest 93: 2639–2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Feldman MD, Copelas L, Gwathmey JK, Phillips P, Warren SE, et al. (1987) Deficient production of cyclic AMP: pharmacologic evidence of an important cause of contractile dysfunction in patients with end-stage heart failure. Circulation 75: 331–339. [DOI] [PubMed] [Google Scholar]
- 24. Marx SO, Reiken S, Hisamatsu Y, Jayaraman T, Burkhoff D, et al. (2000) PKA phosphorylation dissociates FKBP12.6 from the calcium release channel (ryanodine receptor): defective regulation in failing hearts. Cell 101: 365–376. [DOI] [PubMed] [Google Scholar]
- 25. Doi M, Yano M, Kobayashi S, Kohno M, Tokuhisa T, et al. (2002) Propranolol prevents the development of heart failure by restoring FKBP12.6-mediated stabilization of ryanodine receptor. Circulation 105: 1374–1379. [DOI] [PubMed] [Google Scholar]
- 26. Reiken S, Wehrens XH, Vest JA, Barbone A, Klotz S, et al. (2003) Beta-blockers restore calcium release channel function and improve cardiac muscle performance in human heart failure. Circulation 107: 2459–2466. [DOI] [PubMed] [Google Scholar]
- 27. Toblli JE, DiGennaro F, Giani JF, Dominici FP (2012) Nebivolol: impact on cardiac and endothelial function and clinical utility. Vasc Health Risk Manag 8: 151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tuncay E, Zeydanli EN, Turan B (2011) Cardioprotective effect of propranolol on diabetes-induced altered intracellular Ca2+ signaling in rat. J Bioenerg Biomembr 43: 747–756. [DOI] [PubMed] [Google Scholar]
- 29. Wai B, Kearney LG, Hare DL, Ord M, Burrell LM, et al. (2012) Beta blocker use in subjects with type 2 diabetes mellitus and systolic heart failure does not worsen glycaemic control. Cardiovasc Diabetol 11: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sgobbo P, Pacelli C, Grattagliano I, Villani G, Cocco T (2007) Carvedilol inhibits mitochondrial complex I and induces resistance to H2O2 -mediated oxidative insult in H9C2 myocardial cells. Biochim Biophys Acta 1767: 222–232. [DOI] [PubMed] [Google Scholar]
- 31. Zhuang XF, Yin CQ, Wang HY, Sun NL (2009) Distinctive effects of carvedilol in the non-infarct zone: remodelling of the ligated rat heart linked to oxidative stress. J Int Med Res 37: 1354–1364. [DOI] [PubMed] [Google Scholar]
- 32. Sozmen NN, Tuncay E, Bilginoglu A, Turan B (2011) Profound cardioprotection with timolol in a female rat model of aging-related altered left ventricular function. Can J Physiol Pharmacol 89: 277–288. [DOI] [PubMed] [Google Scholar]
- 33. Tuncay E, Seymen AA, Sam P, Gurdal H, Turan B (2009) Effects of beta-adrenergic receptor blockers on cardiac function: a comparative study in male versus female rats. Can J Physiol Pharmacol 87: 310–317. [DOI] [PubMed] [Google Scholar]
- 34. Miyamoto N, Izumi H, Miyamoto R, Kubota T, Tawara A, et al. (2009) Nipradilol and timolol induce Foxo3a and peroxiredoxin 2 expression and protect trabecular meshwork cells from oxidative stress. Invest Ophthalmol Vis Sci 50: 2777–2784. [DOI] [PubMed] [Google Scholar]
- 35. Gomes A, Costa D, Lima JL, Fernandes E (2006) Antioxidant activity of beta-blockers: an effect mediated by scavenging reactive oxygen and nitrogen species? Bioorg Med Chem 14: 4568–4577. [DOI] [PubMed] [Google Scholar]
- 36. Djanani A, Kaneider NC, Meierhofer C, Sturn D, Dunzendorfer S, et al. (2003) Inhibition of neutrophil migration and oxygen free radical release by metipranolol and timolol. Pharmacology 68: 198–203. [DOI] [PubMed] [Google Scholar]
- 37. Tuncay E, Seymen AA, Tanriverdi E, Yaras N, Tandogan B, et al. (2007) Gender related differential effects of Omega-3E treatment on diabetes-induced left ventricular dysfunction. Mol Cell Biochem 304: 255–263. [DOI] [PubMed] [Google Scholar]
- 38. Atar D, Backx PH, Appel MM, Gao WD, Marban E (1995) Excitation-transcription coupling mediated by zinc influx through voltage-dependent calcium channels. J Biol Chem 270: 2473–2477. [DOI] [PubMed] [Google Scholar]
- 39. Matias CM, Sousa JM, Quinta-Ferreira ME, Arif M, Burrows HD (2010) Validation of TPEN as a zinc chelator in fluorescence probing of calcium in cells with the indicator Fura-2. J Fluoresc 20: 377–380. [DOI] [PubMed] [Google Scholar]
- 40. Zhao J, Bertoglio BA, Gee KR, Kay AR (2008) The zinc indicator FluoZin-3 is not perturbed significantly by physiological levels of calcium or magnesium. Cell Calcium 44: 422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Arslan P, Di Virgilio F, Beltrame M, Tsien RY, Pozzan T (1985) Cytosolic Ca2+ homeostasis in Ehrlich and Yoshida carcinomas. A new, membrane-permeant chelator of heavy metals reveals that these ascites tumor cell lines have normal cytosolic free Ca2+. J Biol Chem 260: 2719–2727. [PubMed] [Google Scholar]
- 42. Yamasaki S, Sakata-Sogawa K, Hasegawa A, Suzuki T, Kabu K, et al. (2007) Zinc is a novel intracellular second messenger. J Cell Biol 177: 637–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gee KR, Zhou ZL, Ton-That D, Sensi SL, Weiss JH (2002) Measuring zinc in living cells. A new generation of sensitive and selective fluorescent probes. Cell Calcium 31: 245–251. [DOI] [PubMed] [Google Scholar]
- 44. Bilginoglu A, Cicek FA, Ugur M, Gurdal H, Turan B (2007) The role of gender differences in beta-adrenergic receptor responsiveness of diabetic rat heart. Mol Cell Biochem 305: 63–69. [DOI] [PubMed] [Google Scholar]
- 45. Ayaz M, Ozdemir S, Yaras N, Vassort G, Turan B (2005) Selenium-induced alterations in ionic currents of rat cardiomyocytes. Biochem Biophys Res Commun 327: 163–173. [DOI] [PubMed] [Google Scholar]
- 46. Vallee BL, Falchuk KH (1993) The biochemical basis of zinc physiology. Physiol Rev 73: 79–118. [DOI] [PubMed] [Google Scholar]
- 47. Qin Y, Thomas D, Fontaine CP, Colvin RA (2008) Mechanisms of Zn2+ efflux in cultured cortical neurons. J Neurochem 107: 1304–1313. [DOI] [PubMed] [Google Scholar]
- 48. Lengyel I, Fieuw-Makaroff S, Hall AL, Sim AT, Rostas JA, et al. (2000) Modulation of the phosphorylation and activity of calcium/calmodulin-dependent protein kinase II by zinc. J Neurochem 75: 594–605. [DOI] [PubMed] [Google Scholar]
- 49. Xia RH, Cheng XY, Wang H, Chen KY, Wei QQ, et al. (2000) Biphasic modulation of ryanodine binding to sarcoplasmic reticulum vesicles of skeletal muscle by Zn2+ ions. Biochem J 345 Pt 2: 279–286. [PMC free article] [PubMed] [Google Scholar]
- 50. Adams JA, Taylor SS (1993) Phosphorylation of peptide substrates for the catalytic subunit of cAMP-dependent protein kinase. J Biol Chem 268: 7747–7752. [PubMed] [Google Scholar]
- 51. Yaras N, Bilginoglu A, Vassort G, Turan B (2007) Restoration of diabetes-induced abnormal local Ca2+ release in cardiomyocytes by angiotensin II receptor blockade. Am J Physiol Heart Circ Physiol 292: H912–920. [DOI] [PubMed] [Google Scholar]
- 52. Pierce GN, Dhalla NS (1985) Mechanisms of the defect in cardiac myofibrillar function during diabetes. Am J Physiol 248: E170–175. [DOI] [PubMed] [Google Scholar]
- 53. Tuncay E, Bilginoglu A, Sozmen NN, Zeydanli EN, Ugur M, et al. (2011) Intracellular free zinc during cardiac excitation-contraction cycle: calcium and redox dependencies. Cardiovasc Res 89: 634–642. [DOI] [PubMed] [Google Scholar]
- 54.Hjalmarson A, Waagstein F (1994) The role of beta-blockers in the treatment of cardiomyopathy and ischaemic heart failure. Drugs 47 Suppl 4: 31–39; discussion 39–40. [DOI] [PubMed]
- 55. Kamalov G, Ahokas RA, Zhao W, Shahbaz AU, Bhattacharya SK, et al. (2010) Temporal responses to intrinsically coupled calcium and zinc dyshomeostasis in cardiac myocytes and mitochondria during aldosteronism. Am J Physiol Heart Circ Physiol 298: H385–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Maret W (2000) The function of zinc metallothionein: a link between cellular zinc and redox state. J Nutr 130: 1455S–1458S. [DOI] [PubMed] [Google Scholar]
- 57. Maret W (2009) Molecular aspects of human cellular zinc homeostasis: redox control of zinc potentials and zinc signals. Biometals 22: 149–157. [DOI] [PubMed] [Google Scholar]
- 58. Dineley KE, Richards LL, Votyakova TV, Reynolds IJ (2005) Zinc causes loss of membrane potential and elevates reactive oxygen species in rat brain mitochondria. Mitochondrion 5: 55–65. [DOI] [PubMed] [Google Scholar]
- 59. Noh KM, Kim YH, Koh JY (1999) Mediation by membrane protein kinase C of zinc-induced oxidative neuronal injury in mouse cortical cultures. J Neurochem 72: 1609–1616. [DOI] [PubMed] [Google Scholar]
- 60. Pierce GN, Dhalla NS (1985) Heart mitochondrial function in chronic experimental diabetes in rats. Can J Cardiol 1: 48–54. [PubMed] [Google Scholar]
- 61. Alvarez-Collazo J, Diaz-Garcia CM, Lopez-Medina AI, Vassort G, Alvarez JL (2012) Zinc modulation of basal and beta-adrenergically stimulated L-type Ca(2+) current in rat ventricular cardiomyocytes: consequences in cardiac diseases. Pflugers Arch 464: 459–470. [DOI] [PubMed] [Google Scholar]
- 62. Aras MA, Aizenman E (2011) Redox regulation of intracellular zinc: molecular signaling in the life and death of neurons. Antioxid Redox Signal 15: 2249–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hjalmarson A, Goldstein S, Fagerberg B, Wedel H, Waagstein F, et al. (2000) Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group. JAMA 283: 1295–1302. [DOI] [PubMed] [Google Scholar]
- 64. Aydemir-Koksoy A, Bilginoglu A, Sariahmetoglu M, Schulz R, Turan B (2010) Antioxidant treatment protects diabetic rats from cardiac dysfunction by preserving contractile protein targets of oxidative stress. J Nutr Biochem 21: 827–833. [DOI] [PubMed] [Google Scholar]
- 65. Eager KR, Roden LD, Dulhunty AF (1997) Actions of sulfhydryl reagents on single ryanodine receptor Ca(2+)-release channels from sheep myocardium. Am J Physiol 272: C1908–1918. [DOI] [PubMed] [Google Scholar]
- 66. Wehrens XH, Lehnart SE, Reiken SR, Marks AR (2004) Ca2+/calmodulin-dependent protein kinase II phosphorylation regulates the cardiac ryanodine receptor. Circ Res 94: e61–70. [DOI] [PubMed] [Google Scholar]
- 67. Kubo H, Margulies KB, Piacentino V 3rd, Gaughan JP, Houser SR (2001) Patients with end-stage congestive heart failure treated with beta-adrenergic receptor antagonists have improved ventricular myocyte calcium regulatory protein abundance. Circulation 104: 1012–1018. [DOI] [PubMed] [Google Scholar]
- 68. Mochizuki M, Yano M, Oda T, Tateishi H, Kobayashi S, et al. (2007) Scavenging free radicals by low-dose carvedilol prevents redox-dependent Ca2+ leak via stabilization of ryanodine receptor in heart failure. J Am Coll Cardiol 49: 1722–1732. [DOI] [PubMed] [Google Scholar]
- 69. Bilginoglu A, Kandilci HB, Turan B (2013) Intracellular Levels of Na(+) and TTX-sensitive Na (+) Channel Current in Diabetic Rat Ventricular Cardiomyocytes. Cardiovasc Toxicol 13: 138–147. [DOI] [PubMed] [Google Scholar]
- 70. Chu G, Lester JW, Young KB, Luo W, Zhai J, et al. (2000) A single site (Ser16) phosphorylation in phospholamban is sufficient in mediating its maximal cardiac responses to beta -agonists. J Biol Chem 275: 38938–38943. [DOI] [PubMed] [Google Scholar]
- 71. Hagemann D, Kuschel M, Kuramochi T, Zhu W, Cheng H, et al. (2000) Frequency-encoding Thr17 phospholamban phosphorylation is independent of Ser16 phosphorylation in cardiac myocytes. J Biol Chem 275: 22532–22536. [DOI] [PubMed] [Google Scholar]
- 72. Kadambi VJ, Ponniah S, Harrer JM, Hoit BD, Dorn GW 2nd, et al (1996) Cardiac-specific overexpression of phospholamban alters calcium kinetics and resultant cardiomyocyte mechanics in transgenic mice. J Clin Invest 97: 533–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Zima AV, Blatter LA (2006) Redox regulation of cardiac calcium channels and transporters. Cardiovasc Res 71: 310–321. [DOI] [PubMed] [Google Scholar]
- 74. Crawford AJ, Bhattacharya SK (1987) Excessive intracellular zinc accumulation in cardiac and skeletal muscles of dystrophic hamsters. Exp Neurol 95: 265–276. [DOI] [PubMed] [Google Scholar]