Abstract
Wound dehiscence is a postoperative complication encountered following abdominal surgery. A prospective randomized study was conducted to compare the incidence of wound dehiscence with a delayed absorbable and a nonabsorbable suture material in the mass closure of vertical laparotomy wounds. In one group, 100 patients were analyzed after closure with Prolene®, and in another group, 100 patients were analyzed after closure with Vicryl®. The incision was closed by continuous far and near suture technique using polypropylene (Prolene) suture in one group and a synthetic delayed absorbable polyglactin 910 (Vicryl) suture in the other group. There was significant difference in the incidence of wound dehiscence between the two groups: 6 % with Prolene and 17 % with Vicryl, (χ2 = 5.944, 1 DF, P value = 0.0148). The overall incidence of wound dehiscence was 11.5 % in this study. The incidence of wound dehiscence in both the study groups was higher than expected as compared to previous literature. There was a significant difference between the two suture materials. In our study, Prolene is a better suture material for closure of vertical laparotomy wounds.
Keywords: Wound dehiscence, Mass closure, Vertical laparotomy wounds, Polypropylene, Polyglactin
Introduction
Postoperative complete wound dehiscence is an unfortunate condition, and serious complication is associated with a high morbidity and mortality rate [1–3]. Surgeons have been continuously striving to overcome postoperative complications associated with laparotomy wound closure using newer techniques and newer suture materials. Several reviews have studied the optimal suture repair for closing the abdominal fascia [4–9], but no consensus has been reached. In the present study, two types of suture materials were compared: Prolene®, a nonabsorbable polypropylene monofilament suture material, and Vicryl®, a synthetic delayed absorbable polyglactin 910 polyfilament suture material.
Material and Methods
All patients undergoing an elective or emergency midline laparotomy for various indications in the department of surgery at Rajindra Hospital, Patiala, Punjab, India, from September 1, 2009, to August 30, 2011, were included in this prospective study. Exclusion criteria were pregnancy, presence of an abdominal hernia, lack of informed consent, age less than 18 years, and previous laparotomy.
The patients were allocated to either of the two groups, namely group A or Group B, randomly using randomization tables. In study group A, patients underwent mass closure of abdominal wound using polypropylene (Prolene), whereas in study group B, mass closure of abdominal wound was done using polyglactin 910 (Vicryl). Comorbid factors such as anemia, hypertension, and diabetes mellitus were corrected where possible. Detailed clinical history and physical examination with special reference to the presence of known risk factors for wound disruption such as malignancy, malnutrition, anemia, obesity, diabetes, chemotherapy, cardiovascular status, pulmonary disease, renal failure, and previous history, if any, regarding surgical intervention were recorded.
The investigations done preoperatively were complete blood profile, routine urine examination, random blood sugar, urea, creatinine, X-ray chest, X-ray plain abdomen (erect), and serum electrolytes. Liver function tests, electrocardiography, ultrasonography, and CT scan abdomen were done where required.
The closure of the fascia of the abdominal wall was performed after surgery had been completed using one of the two suture materials (Prolene or Vicryl) as prescribed by randomization. For both the suture materials, a similar strength of suture material was used (No. 1) and the fascia was closed in single layer using continuous far and near suture technique with wide bites through the rectus sheath. The suture length to laparotomy wound length was at least 4:1. No tension sutures were used. Any bleeding vessel in the abdominal wall was either coagulated using thermal cautery or tied with catgut 3-0, and skin closure was carried out with nylon 2-0. The operative and postoperative management was identical in both the groups. The wound was inspected on the third, fifth, seventh, and ninth postoperative days for evidence of any redness, infection, or dehiscence. Other details which were recorded include duration of patient stay in the hospital, drain used or not, approximate length of incision, antibiotics used, and complications if any. Follow-up was conducted at 7th, 30th, and 90th days to assess the wound. The results were recorded and the observations obtained were analyzed using appropriate statistical methods.
Results
A total of 287 consecutive patients were eligible for participation in this study, out of which 211 patients were enrolled and randomized. Of the 76 excluded patients, 46 failed to meet the inclusion criteria, 17 refused to participate in the study, and 13 were not eligible for other reasons (a different suture material was used in them). Eleven randomized patients were excluded from the study since vertical laparotomy incision was not employed (Fig. 1). Baseline characteristics of 200 patients finally analyzed in the study (Table 1).
Fig. 1.
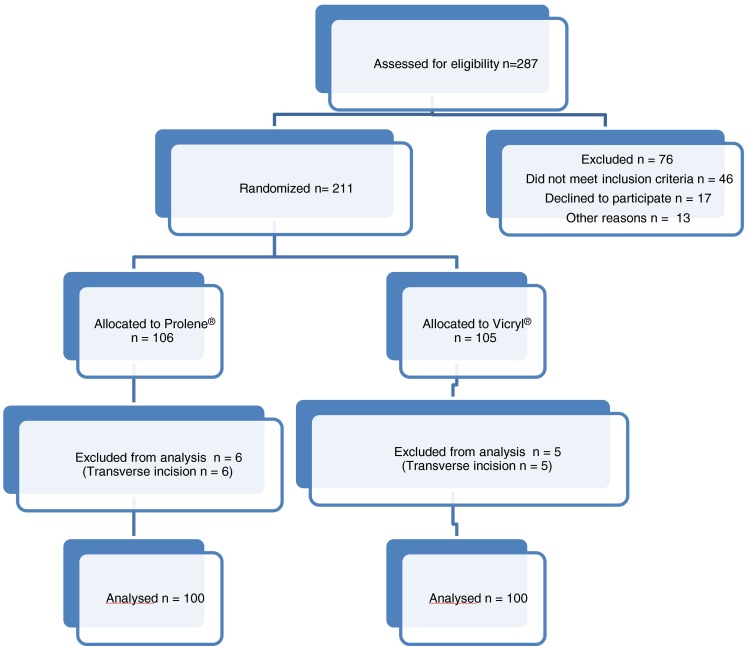
CONSORT diagram for the study
Table 1.
Baseline characteristics in randomized study of vertical laparotomy wound closure
| Prolene® (n = 100) | Vicryl®(n = 100) | |
|---|---|---|
| Age (years) | 54* | 56* |
| Sex ratio (Male: Female) | 2.84 | 3.54 |
| Anaemia | 7 | 6 |
| Body Mass Index(kg/m2) | 28.4* | 27.6* |
| Smoker (Yes/No) | 26/74 | 24/76 |
| Diabetes Mellitus | 7 | 9 |
| Diagnosis | ||
| Intestinal perforation | 48 | 42 |
| Intestinal obstruction | 16 | 18 |
| Haemoperitoneum | 10 | 12 |
| Blunt trauma abdomen | 11 | 9 |
| Mass abdomen | 10 | 14 |
| Gut gangrene | 2 | 3 |
| Obstructed umblical hernia | 3 | 2 |
| Settings | ||
| Elective | 22 | 19 |
| Emergency | 78 | 81 |
*Mean value
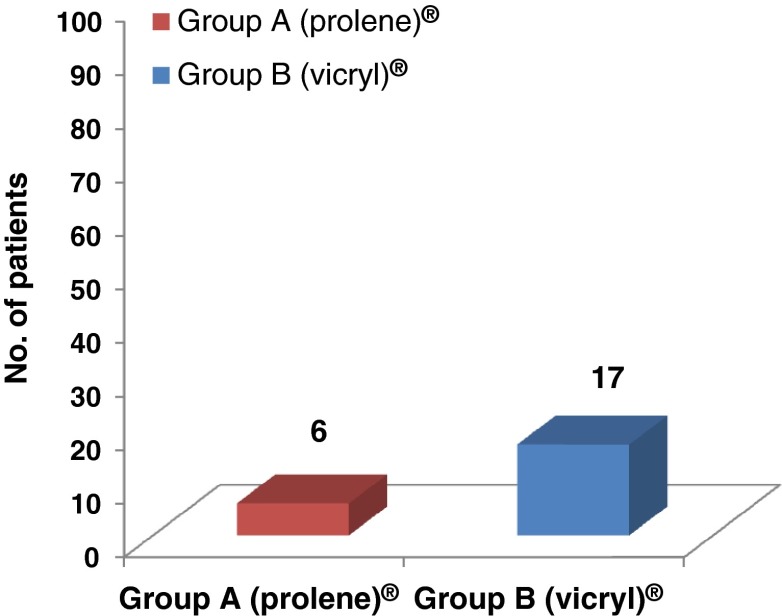
We observed in our study that wound dehiscence occurred in 6 % cases in whom Prolene was used whereas 17 % had wound dehiscence with the use of Vicryl suture (Fig. 2, Table 2). The incidence of wound dehiscence in both the study groups was higher than expected as compared to the previous literature. Wound dehiscence was fairly high with the use of absorbable suture material in our study. Abdominal closure with the use of delayed absorbable suture material (Vicryl) was followed by significantly higher incidence of wound dehiscence than closure by nonabsorbable suture material (Prolene) (χ2 = 5.944, 1 DF, P value = 0.0148).
Fig. 2.
Bar diagram showing percentage of wound dehiscence
Table 2.
Incidence of postoperative wound dehiscence in the present study
| Suture material | No. of patients included (n) | Wound dehiscence | % |
|---|---|---|---|
| Group A(Prolene®) | 100 | 6 | 6 |
| Group B (Vicryl®) | 100 | 17 | 17 |
Chi square equals 5.994. P value equals 0.0148 which is statistically significant
We reviewed the literature and found the incidence of postoperative wound dehiscence ranging from 0 to 24.9 % in various studies using various suture materials (Table 3). The overall incidence of wound dehiscence in this study was 11.5 %. No other study has reported such a higher incidence of postoperative wound dehiscence with the use of Prolene and Vicryl except one study conducted by Brolin [18] comparing Ethibond and PDS® (P = 0.04) in midline fascial closure in gastric bariatric operations and another by Bloemen et al. [20] comparing Prolene and PDS (polydioxanone) for midline abdominal wound closure (P = 0.229).
Table 3.
Post operative wound dehiscence in various studies comparing different suture materials
| Study conducted by | Year | % age of wound Dehiscence | Suture material |
|---|---|---|---|
| Mann et al. [10] | 1962 | 2.73 | Conventional |
| Bentley et al. [11] | 1978 | 0.5 | Dexon |
| White et al. [12] | 1977 | 1.5 | Catgut, steel, nylon |
| Murray and Blaisdell [13] | 1978 | <1 | PGA and Vicryl® |
| Cameron et al. [14] | 1980 | 0.60 | Prolene® & Dexon |
| Mathur SK [15] | 1983 | 0 | Nylon |
| Chowdhury et al. [16] | 1994 | 0, 3.75 | Nylon, chromic catgut |
| Shittu et al. [17] | 1995 | 9.7 | Nylon |
| Brolin et al. [18] | 1996 | 18, 10 | Ethibond®, PDS® |
| Sahlin et al. [19] | 2005 | 1, 1 | Polyglyconate (Maxon), Vicryl® |
| Bloemen et al. [20] | 2011 | 20.2, 24.9 | Prolene®, PDS® |
| Present study | 2011 | 6,17 | Prolene®, Vicryl® |
Discussion
Wound dehiscence is a multifactorial problem, conditioned by local and systemic, as well as pre-, per-, and postoperative factors [1–3, 21, 22]. Wound dehiscence occurs because of the distracting forces in a wound which exceed the holding forces. It is also important to acknowledge that the failures after abdominal wound closure (early dehiscence and late incisional hernia) are due to poor closure technique, deep wound infection, postoperative vomiting, persistent postoperative cough, postoperative abdominal distension, and poor general condition of the patient which includes obesity, jaundice, malignant disease, hypoproteinemia, and anemia [23]. Each suture should be tied loosely with a measured tension sufficient to hold the wound together while avoiding pressure necrosis. It is important for the surgeons to know that wound healing demands oxygen consumption, normoglycemia, and absence of toxic or septic factors, which reduces collagen synthesis and oxidative killing mechanisms of neutrophils [24, 25]. Spiliotis et al. commented, “During the surgical procedures, measure to reduce the risk of infections and hypoxia in the tissue are the two most important factors for the postoperative wound healing process” [26].
In our study, the incidence of wound dehiscence was higher than expected. This could be attributed to various factors which we tried to sum up as either patient-related factors or health care setting associated factors. The patient-related clinical factors which contributed to the high rate of wound dehiscence include poor general condition of the patient at presentation, prior mismanagement by the health care providers, and presence of complications such as septicemia and fluid, and electrolyte derangements. Other patient-related socioeconomic factors included lack of knowledge, negligence of health, and poverty.
Health care setting associated factors responsible for this high incidence of wound dehiscence especially in emergency cases could be the lack of proper sterilization in an emergency setup. Another factor could be the lack of experience on the part of the surgeon as most of the emergency laparotomies were performed by surgical residents. Most of the subjects in our study underwent emergency surgery. Our study was in accordance with other reports by Niggebrugge et al. [27], Penninckx et al. [28], and McGinn et al. [29], demonstrating significantly higher incidence of postoperative wound dehiscence in emergency than in elective surgery.
Many causes of wound dehiscence are avoidable. Good and active resuscitation of patients before surgery with emphasis on fluid and electrolyte balance, antibiotic cover, nasogastric tube aspiration, and proper intake and output monitoring do influence the outcome positively. Strict postoperative care with stress on prevention of wound infection, chest complications, and paralytic ileus can avoid a tragic outcome.
In the present study, results showed Prolene to be better as compared to Vicryl although both the study groups had a higher than expected incidence of wound dehiscence. In a developing country like ours, Prolene is economically more acceptable as compared to the Vicryl which is more costly. And lesser incidence of the complications with use of Prolene will further reduce the burden on the health care facilities as it has a significant impact on health care cost, both for the patients and hospitals.
Conclusion
The incidence of wound dehiscence was higher as compared to the previous literature in both the study groups. Wound dehiscence was significantly higher in the group where Vicryl sutures were used than in the group where Prolene sutures were used. Thus, in the present study, we found Prolene to be a better and more economical suture material for closure of vertical laparotomy wounds.
Conflict of interest
None.
References
- 1.Guiney EJ, Morris PJ, Donaldson GA. Wound dehiscence. A continuing problem in abdominal surgery. Arch Surg. 1966;92:47–51. doi: 10.1001/archsurg.1966.01320190049011. [DOI] [PubMed] [Google Scholar]
- 2.Efron G. Abdominal wound disruption. Lancet. 1965;1(7399):1287–1290. doi: 10.1016/S0140-6736(65)92777-7. [DOI] [PubMed] [Google Scholar]
- 3.Mayo Ch W, Lee MJ. Separations of abdominal wounds. A M A Arch Surg. 1951;62(6):883–894. doi: 10.1001/archsurg.1951.01250030894016. [DOI] [PubMed] [Google Scholar]
- 4.Hodgson NCF, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure. A meta analysis. Ann Surg. 2000;231(3):436–442. doi: 10.1097/00000658-200003000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ceydeli A, Wise L. Finding the best abdominal closure an evidence based review of the literature. Curr Surg. 2005;62:220–225. doi: 10.1016/j.cursur.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Rucinski J, Margolis M, Panagopoulos G, Wise L. Closure of the abdominal midline fascia: meta-analysis delineates the optimal technique. Am Surg. 2001;67(5):421–426. [PubMed] [Google Scholar]
- 7.Van’t Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta analysis of techniques for closure of mid-line abdominal incisions. Br J Surg. 2002;89(11):1350–1356. doi: 10.1046/j.1365-2168.2002.02258.x. [DOI] [PubMed] [Google Scholar]
- 8.Weiland DE, Bay RC, Del Sordi S. Choosing the best abdominal closure by meta-analysis. Am J Surg. 1998;176(6):666–670. doi: 10.1016/S0002-9610(98)00277-3. [DOI] [PubMed] [Google Scholar]
- 9.Diener MK, Voss S, Jensen K, Buchler MW, Seller CM. Elective midline laparatomy closure: the INLINE systematic review and meta-analysis. Ann Surg. 2010;251:843–856. doi: 10.1097/SLA.0b013e3181d973e4. [DOI] [PubMed] [Google Scholar]
- 10.Mann LS, Spinazzola AJ, Lindesmith GG, Levine MJ, Kuczerepa W. Disruption of abdominal wounds. JAMA. 1962;180(12):1021–1023. doi: 10.1001/jama.1962.03050250027006. [DOI] [PubMed] [Google Scholar]
- 11.Bentley PG, Owen WJ, Girolami PL, Dawson JL. Wound closure with Dexon (polyglycolic acid) Ann R Coll Surg Eng. 1978;60:125–127. [PMC free article] [PubMed] [Google Scholar]
- 12.White WC. Disruption of abdominal wounds. Ann of Surg. 1934;99(1):34–38. doi: 10.1097/00000658-193401000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray DH, Blaisdell FW. Use of synthetic absorbable sutures for abdominal and chest wound closure. Experience with 650 consecutive cases. Arch Surg. 1978;113(4):477–480. doi: 10.1001/archsurg.1978.01370160135023. [DOI] [PubMed] [Google Scholar]
- 14.Cameron AEP, Gray RCF, Talbot RW, Wyatt AP. Abdominal wound closure: a trial of Prolene and Dexon. Br J Surg. 1980;67:487–488. doi: 10.1002/bjs.1800670712. [DOI] [PubMed] [Google Scholar]
- 15.Mathur SK. Burst abdomen. A preventable complication, monolayer closure of the abdominal incision with monofilament nylon. J Postgrad Med. 1983;29(4):223–229. [PubMed] [Google Scholar]
- 16.Chowdhury SK, Choudhury SD. Mass closure versus layered closure of abdominal wound: a prospective clinical study. J Indian Med Assoc. 1994;92(7):229–232. [PubMed] [Google Scholar]
- 17.Shittu OS, Ifenne DI, Ekwempu CC. A simple mass closure technique compared with layered technique in the closure of high-risk abdominal wounds. West Afr J Med. 1995;14(1):11–14. [PubMed] [Google Scholar]
- 18.Brolin RE. Prospective, randomized evaluation of midline fascial closure in gastric bariatric operations. Am J Surg. 1996;172:328–231. doi: 10.1016/S0002-9610(96)00194-8. [DOI] [PubMed] [Google Scholar]
- 19.Sahlin S, Ahlberg J, Granstrom L, Ljungstrom KG. Monofilament versus multifilament absorbable sutures for abdominal closure. Br J Surg. 2005;80(3):322–324. doi: 10.1002/bjs.1800800318. [DOI] [PubMed] [Google Scholar]
- 20.Bloemen A, Van Dooren P, Huizinga BF, Hoofwijk AGM. Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg. 2011;98:633–639. doi: 10.1002/bjs.7398. [DOI] [PubMed] [Google Scholar]
- 21.Halasz NA. Dehiscence of Laparotomy wounds. Am J Surg. 1968;116(2):210–214. doi: 10.1016/0002-9610(68)90495-9. [DOI] [PubMed] [Google Scholar]
- 22.Raahave D. Aseptic barriers of plastic to prevent bacterial contamination of operation wounds. Acta Chir Scan. 1974;140:603. [PubMed] [Google Scholar]
- 23.Williams NS, Christopher JK, Bulstrode, O’Connell PR (2008) Hernia, umbilicus and abdominal wall. In: Bailey and Love’s Short Practice of Surgery, 25th ed. Arnold, pp 1272–1293
- 24.Black F, Vibe-Petersen J, Jorgensen JN, et al. Decrease of collagen deposition in wound repair in type I diabetes independent of glycemic control. Arch Surg. 2003;138:34–40. doi: 10.1001/archsurg.138.1.34. [DOI] [PubMed] [Google Scholar]
- 25.Allen DB, Maguire JJ, Mahdavian M, Wicke C, Marcocci L, Scheuenstuhl H, et al. Wound hypoxia and acidosis limit neutrophil bacterial killing mechanisms. Arch Surg. 1997;132:991–996. doi: 10.1001/archsurg.1997.01430330057009. [DOI] [PubMed] [Google Scholar]
- 26.Spiliotis J, Tsiveriotis K, Datsis AD, Vaxevanidou A, Zacharis G, Giafis K, et al. Wound dehiscence: is still a problem in the 21th century: a retrospective study. World J Emerg Surg. 2009;4:12. doi: 10.1186/1749-7922-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niggebrugge AH, Hansen BE, Trimbos JB. Mechanical factors influencing the incidence of burst abdomen. Eur J Surg. 1995;161:655–661. [PubMed] [Google Scholar]
- 28.Penninckx FM, Poelmans SV, Kerremens RP, Beckers JP. Abdominal wound dehiscence in gastroenterological surgery. Ann Surg. 1979;189(3):345–352. doi: 10.1097/00000658-197903000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGinn FP. Effects of hemorrhage upon surgical operations. Br J Surg. 1976;63:742–745. doi: 10.1002/bjs.1800631005. [DOI] [PubMed] [Google Scholar]