Abstract
Context:
Vitiligo is a chronic, benign, but emotionally frustrating autoimmune disorder of depigmentation, with an incidence of 0.25-2.5% in India, the treatment of which is equally frustrating to the patient, as well as the doctor. Phototherapy is the first line treatment in many cases, which needs to be given at frequent sittings for long periods of time. As there is no satisfactory, short term treatment, many vitiligo patients, though enthusiastic in the beginning, become defaulters after a few weeks or months.
Aims:
This study was conducted to assess the compliance to phototherapy (PUVA and NB-UVB), determine the reasons for non-compliance, to calculate the overall response to phototherapy and to know about the patients’ perception about improvement of lesions.
Materials and Methods:
All files of the patients who attended phototherapy for Vitiligo in the department for a period of 4 years from January 2007 were analyzed and the patients were contacted via mail or telephone and were made to answer questionnaire regarding their disease.
Conclusions:
At the end of this retrospective questionnaire based study we concluded that only a quarter of the patients underwent regular phototherapy, among which the younger patients and those with widespread disease and facial lesions were more compliant. Educational status and sex had no impact on default status.
Keywords: Adherence, compliance, phototherapy, vitiligo
Introduction
What was known?
1. Vitiligo, though a benign disease, has great psychosocial morbidity.
2. Treatment of Vitiligo is long-drawn and usually unsatisfactory.
Vitiligo is a chronic, benign, though emotionally frustrating disorder of pigmentation with an incidence of 1-2% world-wide and 0.25-2.5% in India.[1] Vitiligo treatment is on the whole unsatisfactory as there are no known methods which lead to complete repigmentation of the depigmented lesions, though there are many modalities which may cause partial response. Out of the currently existing treatment options which include use of topical and systemic immune suppressants, phototherapy and surgery for stable lesions, phototherapy, especially narrow band ultraviolet therapy (NB-UVB) is widely used.[2] This is especially so in the case of widespread lesions, childhood, pregnancy, etc.. NB-UVB is a relatively safe and efficacious treatment, the main drawbacks being the requirement of sophisticated narrowband chamber, the repeated visits required of the patient to the place of administration, which may not be cost effective as it is prolonged and leads to loss of working hours and increases relative cost of treatment.
Settings and Design
This was a retrospective questionnaire based study involving vitiligo patients who had undergone narrow band UVB or Psoralen Ultraviolet A light therapy in the department of dermatology for the past four years.
Materials and Methods
All cases of vitiligo, who were advised phototherapy between January 2007 and December 2010 were chosen for the study. Their files were studied for details of the disease such as duration and sites affected. The patients were divided into 2 groups: One on regular phototherapy in the hospital and another group who had discontinued. Patients were contacted personally, telephonically or through post and asked a standard set of questions to evaluate their compliance to treatment, nature and effects of phototherapy. Variables compared with both groups included age, gender, education, size and extent of lesions, number of lesions, additional treatments taken, improvement of lesions and their belief regarding disease resolution. The association of the above variables was analyzed by Chi square test and the data described on the basis of frequencies and percentages.
Statistical analysis used: Chi square test
Observations and Results
Out of 101 patients who were approached for the study, 79 patients responded, of whom 21 were regular and 58 were irregular or non-compliant.
The available data was compiled and statistically analyzed. Various parameters like age, sex, education, number and extent of the lesions, area involved (whether predominantly exposed or unexposed) and occurrence of adverse effects to phototherapy, were compared in compliant and non-compliant groups and statistical significance arrived at. Reasons for discontinuation of phototherapy and alternatives used by non-compliant patients were studied. Regularity of visit, satisfaction level and the desire to continue phototherapy were recorded in the compliant group.
-
Age and regularity of phototherapy
18 out of 21 (85.7%) regular patients were less than 25 years of age, as compared to 14 out of 58 irregular patients (24.1%), which was statistically significant, according to Chi square test [Table 1]. It can be concluded that younger patients are more eager to continue phototherapy as opposed to older patients.
-
Sex and regularity of treatment
There were 7 males and 14 females in the regular group and 29 each males and females in the irregular group. [Table 2] There was no statistical significance.
-
Educational status and regularity of treatment
14 out of 21 regular patients (66.67%) and 18 out of 58 irregular patients (31%) were college educated. Though educated people constituted the larger chunk in the regular treatment group, Chi square test did not demonstrate statistical significance [Table 3].
-
Number of lesions and regularity
18 out of 21 (85.7%) regular patients had 4 or more lesions as compared to 22 out of 58 (37.9%) of irregular patients, which was statistically significant [Table 4]. It could be concluded that patients with a fewer number of lesions tend to stop phototherapy.
-
Occurrence of adverse effects and regularity
Adverse effects were noticed only in 4 people (19%) who were regular in treatment as compared to 46 (76.3%) who had stopped the treatment, which was statistically significant [Table 5]. Therefore, it could be concluded that most people stopped treatment due to adverse effects. These included erythema, itching, burning sensation, pigmentation, blistering and ocular side effects [Table 6].
-
Faith in treatment and general impression regarding the treatment
All 79 patients were asked their impression about the improvement of the disease with treatment. All 21 patients in the regular group firmly believed that treatment will improve the disease; whereas in the 58 patients who stopped treatment, 22 believed that disease will improve (37.9%), 7 were not sure of the effect of treatment on the disease and 27 (46.6%) believed that the disease will not improve [Table 7].
-
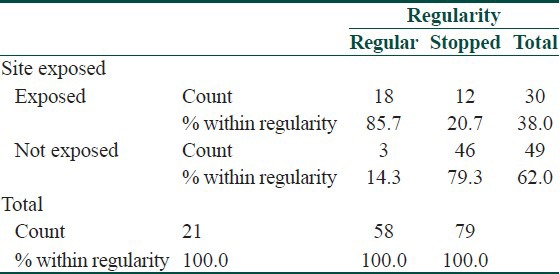
Site of involvement
18 out of 21 (85.7%) patients who completed treatment had lesions on their exposed parts of the body whereas only 12 patients who stopped treatment (20.7%) had lesions on their exposed areas. 79.3% patients who stopped had lesions in the non-exposed areas [Table 8]. Similarly, 19 out of 21 regular patients had facial involvement (90.5%) as compared to 16 patients who had stopped treatment (27.6%), which was again a significant difference according to the Chi square test. It can be concluded that patients who have lesions in exposed areas, especially over the face, tend to comply with treatment.
-
Other treatment used (PUVASOL and topical)
25 patients who had stopped follow-up (43.1%) and 5 regular patients (23.8%) were using psoralen soaks followed by solar exposure (PUVASOL) regularly. So also, 8 (38.1%) regular and 25 irregular patients (43.1%) were using topical medications for their lesions. Statistical analysis showed that though there was significant association between irregularities of hospital attended phototherapy and use of PUVASOL, there was no significant difference in the two groups as regarding to usage of topical medicine.
Table 1.
Age regularity cross tabulation
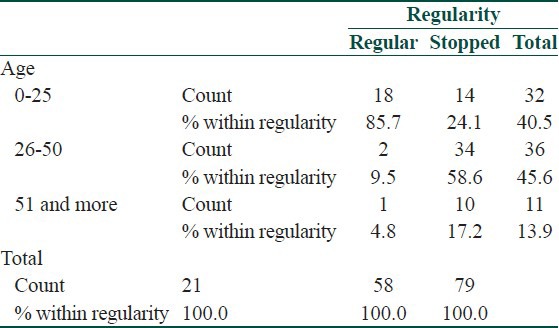
Table 2.
Sex regularity crosstabulation
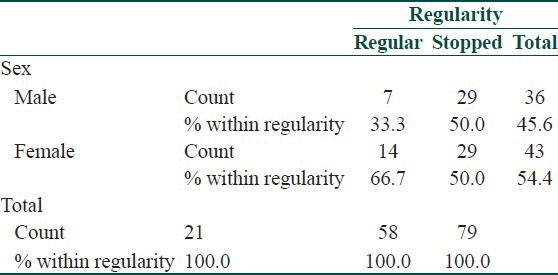
Table 3.
Education and regularity cross tabulation
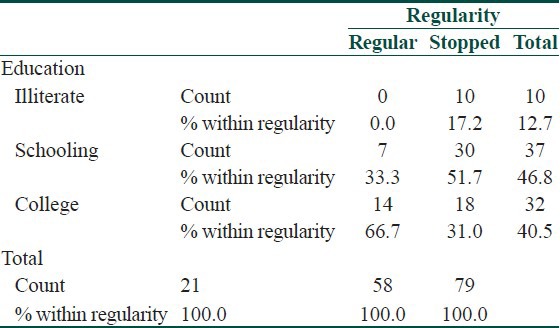
Table 4.
Number of lesions and regularity cross tabulation
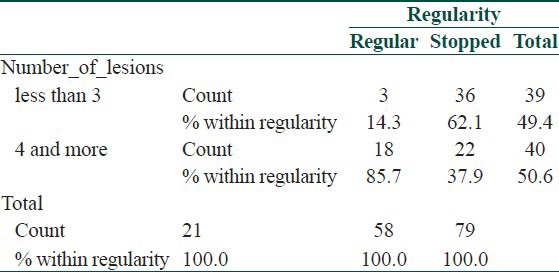
Table 5.
Adverse effects* regularity crosstabulation
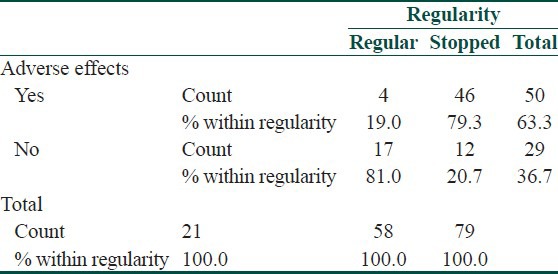
Table 6.
Adverse effects noted in patients
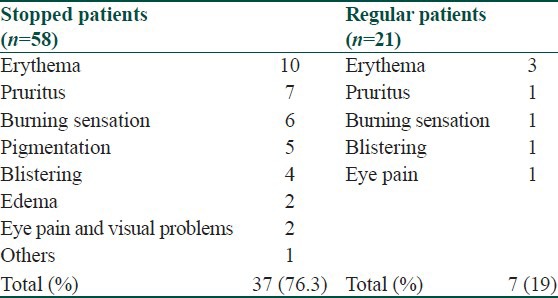
Table 7.
Faith and regularity cross tabulation
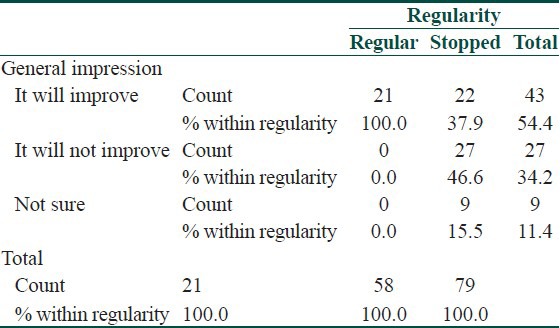
Table 8.
Site exposed and regularity cross tabulation
Reasons for non-compliance
The patients who had stopped treatment were asked further questions to ascertain the cause for irregularity and non-compliance to treatment. It was found that nearly half the patients stopped treatment in the first 4 weeks of initiation and 10 people stopped after one year of regular treatment [Table 9]. The predominant factor for non-compliance was occurrence of adverse effects (22.8%), followed by the distance they had to travel at least 2-3 times per week for a prolonged period (14.4%). The other factors included a busy schedule, loss of faith in the treatment, and even resolution of the lesions [Figure 1].
Table 9.
Treatment duration
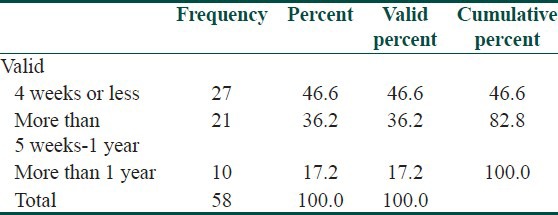
Figure 1.
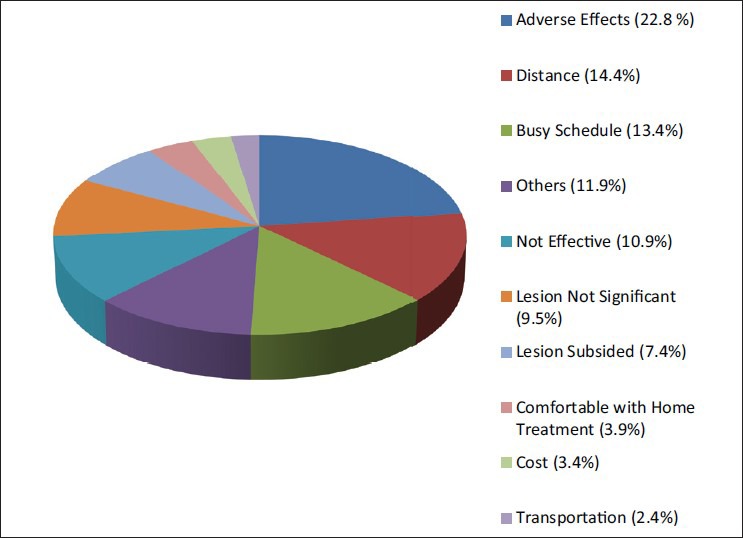
Reasons for discontinuation of phototherapy
35 out of 58 were not ready to restart the treatment and 5 had not decided upon whether to restart treatment.
The frequencies of visits were calculated in the compliant group and it was found that the majority (15 patients - 71.4%) were attending the hospital at twice weekly intervals.
Discussion
Vitiligo is a chronic disorder of pigmentation which is not easily amenable to treatment as evidenced by the current literature. Treatment of vitiligo is based on various factors like age and sex of patient, psychosocial conditions, site of the lesions, availability of a particular modality of treatment, financial status and expectations of the patient. Overall, phototherapy is a well-established modality in the treatment of vitiligo, especially for widespread lesions occurring in adults.[3] Both Psoralen intake followed by ultraviolet. A light exposure (PUVA) and narrow band ultraviolet B rays (NBUVB) are widely used in phototherapy of vitiligo, though these are not free of drawbacks like cost and frequency of treatment, exposure to ultraviolet rays in specialized chambers in hospital or clinic setup and the uncertainty of repigmentation. NBUVB is found to be superior to PUVA due to various reasons[4,5] including better repigmentation and color match with natural skin, a better safety profile as it maximizes the delivery of narrow-band UVB radiation in the range of 312-313 nm which is the most beneficial of the UV spectrum, while minimizing exposure to superfluous UV radiation thereby considerably decreasing the risk of severe burning or pathogenic exposure to UV in harmful ranges. It also avoids the adverse side effects of the psoralens used in conventional PUVA therapy. As UVB treatment requires no supplemental drugs and is considered to be effective and safe in children and pregnant women. There is no need for post treatment eye protection and it is easier and less expensive. PUVASOL is widely used still but with inherent drawbacks like inability to undergo exposure at the time of maximum UVA incidence in people who are studying or working, inability to expose covered areas in females and interference of UVA incidence by atmospheric conditions like rain, smog and cloud.
However, in practice, it is seen that many patients, especially those who reside in villages have to travel long distance thereby losing productive time and money for 2 days a week or even more for a prolonged period of time, which cannot be established at the outset of treatment. Moreover, phototherapy has its inherent side-effects like occurrence of erythema, pigmentation, and sometimes even irritant reaction of the exposed site. Due to these factors, it is seen that the patients do not undertake optimum treatment. They usually compromise on the frequency of treatment and many a time discontinue treatment on their own.
Hence, we undertook this study involving vitiligo patients who had been recruited for phototherapy in the past 4 years. Our aim was to assess the compliance to phototherapy, determine the reasons for non-compliance, find the overall response to phototherapy and know about the patient's perception about improvement of lesion.
Though 101 patients were approached for the study, only 79 conceded for the same. After detailed analysis of all the data provided we came to some interesting deductions:
Out of the 79 respondents, only 21 were undergoing regular phototherapy, which accounted to 26.58%.
Majority of patients were between 2nd and 4th decade which is the most productive period in one's life. Most of the patients coming for phototherapy were less than 25 years indicating the eagerness of the younger population in receiving this treatment.
Younger patients (< 25 years) were more regular and compliant.
Interestingly, educational status and sex of the patient did not show any statistical correlation with compliance to treatment.
All patients in the regular group firmly believed that phototherapy will improve their disease, whereas only 37.9% of irregular group had faith in the treatment. This can be construed in either ways, there was a higher percentage of believers in the regular group because the disease had started responding to treatment and hence they were regular, or that the regular group responded better due to their increased faith and compliance to treatment.
People with widespread disease and with lesions on exposed areas were more regular (85.7% vs. 20.7%) perhaps because they were more psychosocially affected and were more determined to cure the disease. More than 76% of the irregular group developed adverse effects like erythema, itching, burning sensation, pigmentation, blistering and ocular side effects as compared to 19% of the regular group.
Those who were non-compliant to hospital based phototherapy were more frequently using other modalities like PUVASOL (psoralen intake and sunlight exposure at home) and topical medications.
In the irregular group, the attrition rate was maximum (50%) in the first 4 weeks. The majority of patients gave the reason for discontinuation as occurrence of side-effects. Hence, patient should be properly counseled at each visit regarding effects and side-effects and simple ways to avoid side-effects like protecting uninvolved body parts with sunscreens/clothing to avoid erythema and pigmentation, use of non steroidal anti-inflammatory drugs for mild burning sensation, avoidance of sun exposure immediately after treatment.
Another major cause for patient attrition was the time, loss of pay involved and cost of travel from distant areas to come to the hospital. Hence, home treatment with handheld NBUVB light should be popularized and made cost effective.
Majority of people who were regular attended the hospital at twice weekly frequencies. Hence, lesser frequency of weekly treatment (2 times as compared to 3-4 times) is more advisable in out patient phototherapy treatment.
In the medical literature so far, there are only limited studies on patient compliance in phototherapy in vitiligo, though studies assessing efficacy and safety of NBUVB and PUVA in vitiligo state that the more compliant the patient, better the results. Al-Aboosi et al. studies 29 patients with vitiligo who were on PUVA and found that only 18 completed treatment.[6] A study by Kishan Kumar et al. assessing the efficacy and safety of NBUVB in 150 vitiligo patients found that almost complete repigmentation is associated with good compliance. In this study, 18 people (25%) had abruptly stopped treatment before results were achieved.[2]
Indian perspectives
Rai and Srinivas have written an excellent review article on Indian scenario in phototherapy in general, with special attention to methodologies of PUVASOL, Bath PUVA and Narrow band UVB.[7]
Lahiri and Malakar have comprehensively reviewed the concept of stability in vitiligo and have confirmed that phototherapy, especially NB-UVB may play a role in stabilizing vitiligo lesions by inducing apoptosis of melanocyte specific CD8 T cells, which have a pivotal role in induction and perpetuation of the lesions.[8]
Norlund has reviewed extensive reports on side effects of phototherapy in vitiligo, especially in caucasian skin and has come to the conclusion that phototherapy does not significantly increase the risk of melanoma and other skin cancers, in contrast to albinoid skin. He also hypothesizes that melanocytes may have some role in inflammation and carcinogenesis, and vitiliginous area does not undergo cancerous changes due to absence of melanocytes.[9]
Conclusions
This study was undergone for the purpose of assessing the compliance to treatment, response and patient perception of disease cure in vitiligo patients undergoing phototherapy at the department. In our study, side effects were cited as the main reason for non compliance. Hence, time should be spent counseling patients and explaining about necessity for prolonged treatment and strict adherence to schedule. The incidence, nature and benignity of the side effects should be explained to the patients. They may also be taught ways to avoid and manage minor, but frequent side effects like erythema, burning sensation and pigmentation by simple measures like application of sunscreen on the normal skin, use of emollients and topical steroids immediately after phototherapy, regular and judicious use of sunscreens etc., Distance to be travelled and monetary and time loss in attending the hospital at least twice weekly for prolonged time were cited as the second common cause for attrition. This clearly underscores the need for popularizing hand held UVB units which are commercially available and are easy to operate turn out to be economically viable in the long run, so also the development of easy to operate, economically viable home units for people with generalized vitiligo. An interaction with phototherapy unit manufacturers in this regard is essential.
What is new?
1. The major reason for non compliance to phototherapy is the loss of time and expense involved.
2. People with extensive lesions and lesions on face are more compliant to treatment.
3. Easy to operate, economically viable home units may considerably improve patient compliance to phototherapy in vitiligo.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Das SK, Majumder PP, Chakraborty R, Majumdar TK, Haldar B. Studies on vitiligo: Epidemiological profile in Calcutta, India. Genet Epidemiol. 1985;2:71–8. doi: 10.1002/gepi.1370020107. [DOI] [PubMed] [Google Scholar]
- 2.Kishan Kumar YH, Rao GR, Gopal KV, Shanti G, Rao KV. Evaluation of narrow-band UVB phototherapy in 150 patients with vitiligo. Indian J Dermatol Venereol Leprol. 2009;75:162–6. doi: 10.4103/0378-6323.48662. [DOI] [PubMed] [Google Scholar]
- 3.Rai R. Phototherapy: An update. Indian J Dermatol Venereol Leprol. 2009;75:634–7. doi: 10.4103/0378-6323.57741. [DOI] [PubMed] [Google Scholar]
- 4.Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized Double Blind Trial of Treatment of Vitiligo: Efficacy of Psoralen-UV-A Therapy vs Narrowband-UV-B Therapy. Arch Dermatol. 2007;143:578–84. doi: 10.1001/archderm.143.5.578. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar A, Kanwar AJ, Parsad D, De D. Comparison of systemic PUVA and NB-UVB in the treatment of vitiligo: An open prospective study. J Eur Acad Dermatol Venereol. 2007;21:638–42. doi: 10.1111/j.1468-3083.2006.02035.x. [DOI] [PubMed] [Google Scholar]
- 6.al-Aboosi MM, Ajam ZA. Oral photochemotherapy in vitiligo: Follow-up, patient compliance. Int J Dermatol. 1995;34:206–8. doi: 10.1111/j.1365-4362.1995.tb01571.x. [DOI] [PubMed] [Google Scholar]
- 7.Rai R, Srinivas CR. Phototherapy: An Indian perceptive. Indian J Dermatol. 2007;52:169–75. [Google Scholar]
- 8.Lahiri K, Malakar S. The concept of stability of vitiligo: A reappraisal. Indian J Dermatol. 2012;57:83–9. doi: 10.4103/0019-5154.94271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norlund JJ. Vitiligo: A review of some facts lesser known about depigmentation. Indian J Dermatol. 2011;56:180–9. doi: 10.4103/0019-5154.80413. [DOI] [PMC free article] [PubMed] [Google Scholar]


