Abstract
Background:
Alopecia areata (AA) is considered as a T-cell mediated autoimmune disorder. The 308-nm excimer laser is thought to be capable of inducing T-cell apoptosis in vitro, suggesting that the 308-nm excimer lamp (not laser) might be effective for the treatment of AA. We examined the effectiveness of the 308-nm excimer lamp for treating AA.
Materials and Methods:
We treated 16 patients with single AA and multiple AA (MAA). The lesions were irradiated with a 308-nm excimer lamp at 2-week intervals.
Results:
Hair regrowth was observed in 14 patients. Among them, 10 patients showed more than 50% hair re-growth. Our results suggested that the 308-nm excimer lamp system is effective and safe for the treatment of single AA and MAA.
Conclusion:
Our results suggest that the 308-nm excimer lamp is a good therapeutic alternative without serious side effect for treating AA.
Keywords: 308-nm excimer lamp, alopecia areata, treatment
Introduction
What was known?
Alopecia areata (AA) is considered as a T-cell mediated autoimmune disorder. Treatment AA is often difficult.
Alopecia areata (AA) is a non-scarring, autoimmune, inflammatory, relapsing hair loss affecting the scalp and/or body.[1] It commonly manifests as a sudden loss of hair in localized areas. The lesion is usually single round or oval patch. Histologically, the early stage of AA is characterized by the presence of CD+4 and CD+8 T lymphocytic infiltration in the peribulbar region.[2,3] The late stage is characterized by numerous miniaturized hair follicles. AA has been hypothesized to be an organ-specific autoimmune disease with a genetic predisposition and an environmental triggers.[4]
Treating AA is often difficult, with corticosteroids being the most popular treatment option. Several methods of corticosteroid administration including topical, intra-lesional and systemic therapy have been used. Although systemic corticosteroids are occasionally utilized to treat severe AA, this approach is limited due to the frequent adverse effects associated with long-term administration. On the other hand, there have been several studies reporting success with psoralen plus ultraviolet A (PUVA) therapy in patients with AA[5,6,7,8,9] in addition, narrow-band ultraviolet B (NB-UVB) phototherapy with wavelengths between 311 and 313 nm is also effective and safe for treating various inflammatory skin diseases. However, one of the major disadvantages of these phototherapeutic modalities is that along with the alopecia lesions, large areas of normal skin are also exposed to irradiation, resulted in limited increment of irradiation dose.[14]
The novel non-laser 308-nm monochromatic excimer lamp, which is less costing than excimer laser, can selectively deliver high doses of ultraviolet (UV) irradiation to the limited skin sites. In this study, we utilized the 308-nm excimer lamp to treat 16 patients with localized or multiple AA (MAA).
Materials and Methods
Phototherapy sources
The 308-nm excimer lamp (VTRAC®; PhotoMedex, Inc. Montgomeryville, PA, USA) is a monochromatic non-coherent light with the spot size 18.9 cm2 (6.1 cm × 3.1 cm), which could emit power density of 150 mW/cm2. The light source is a Xenon chloride lamp.
Patients
Sixteen patients (4 male and 12 female) with single AA or MAA were enrolled in this study. Informed consent was obtained from all patients before starting the study. Patients who were pregnant or who had a history of photo-hypersensitivity were excluded. In all cases, clinical examination revealed no evidence of additional diseases with negative results of routine laboratory tests, including thyroid hormone and antinuclear antibody tests.
Treatment schedule
Alopecia lesions were treated once every two weeks. The initial irradiation doses ranged from 150 to 200 mJ/cm2. Treatments were given up to once every two weeks with dose increments of 50 mJ/cm2 until the appearance of fine erythema. When erythema appeared the dosage of irradiation was fixed. Phototherapy with the 308-nm excimer lamp was added to the baseline treatment.
Regrowth of hair was evaluated on a three-point scale: Score 0, no effect; score 1, hair re-growth involving less than 50% of scalp lesions; score 2, hair re-growth involving more than 50% of the scalp lesions.
Results
All 16 patients completed the treatment schedule. Four (57%) of those with single AA showed re-growth involving more than 50% of lesional areas, while 2 (29%) showed regrowth involving less than 50% of lesional areas. Hair regrowth was documented in 86% of single AA patients [Table 1]. On the other hand, only six patients (67%) with MAA showed re-growth involving more than 50% of lesional areas while two (22%) showed regrowth involving less than 50% of lesional areas. In total, 89% of MAA patients experienced hair regrowth [Tables 1 and 2].
Table 1.
Numbers of patients with single AA and MAA showing responses to the treatment (according to the 3-point scale)
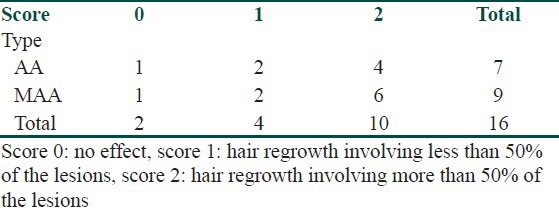
Table 2.
Demographics and phototherapy data
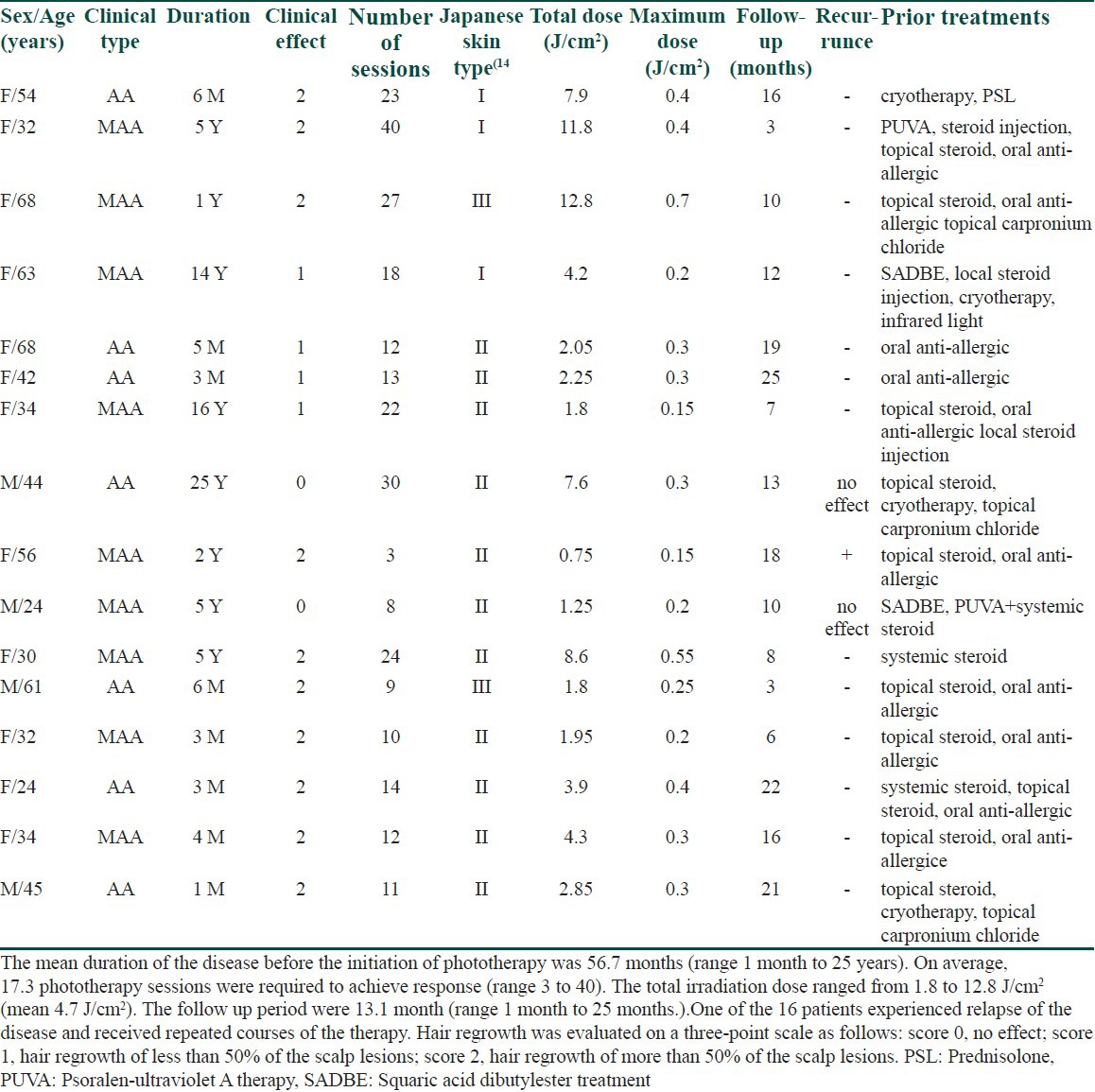
Side-effects observed in different patients were limited to mild erythema, hyperpigmentation and mild itching. The excimer lamp therapy was tolerable to all the patients tested.
Comment
Our results demonstrated that phototherapy with the 308-nm excimer lamp is effective and safe for treating AA. It was previously reported that UV induces not only DNA damage in T-cells but also emigration of T-cells from the skin.[10,11,12] However, clinical trials of PUVA and NBUVB treatments for AA have been conducted with variable results.[5,6,7,8] These therapies are thought to be disadvantageous because large unaffected areas are irradiated along with the AA lesions, resulting in insufficient increment of irradiation dose at lesional skin sites. On the other hand, the 308-nm excimer lamp allows selective irradiation of the affected areas while sparing the surrounding unaffected skin. With the excimer lamp, the UVB can be applied to only one or a few individual patches, with adequate protection of the surrounding healthy skin. The 308-nm excimer laser, which is not a monochromatic excimer lamp, can reportedly induce T-cell apoptosis in vitro.[13] In addition, we experienced favorable effect of the monochromatic excimer lamp, which is less costing than the laser system, on AA patients in this study.
In general, UVB is thought hardly to reach deep into the dermis, where hair bulbs with inflammatory cells are located in AA. However, according to the Beer-Lambert law, which relates the absorption of light to the substances, higher fluences may reach deeper with higher intensity. We hypothesize, together with our results, that UVB could reach to the dermis of alopecia lesions and showed the effects. These results imprecated the advantage of the use of high intensity UVB than lower fluences of UVB in the treatment of AA.
We successfully treated 14 AA cases in this study, in which generally administering four sessions of 308 nm excimer lamp treatment were needed. The short duration of each session, the cycle durations, and the selective UVB exposure of only affected areas have significant benefits for patients in terms of both safety and efficacy. The results indicated that this therapy induces effective hair regrowth especially in patients with a single AA lesion. Although one of our patients reported recurrent hair loss during the follow-up period of more than six months, these recurrent lesions were also re-treated by the lamp. Therefore, this therapy machinery will be appears more useful than conventional narrow-band phototherapy for both single AA and MAA.
Excimer lamps irradiate with high energy in a short time, raising the possibility of erythema, blistering and crust formation. However, during the course of our study, erythema was the only adverse effect was detected in any patient. Our results suggest the excimer 308 nm lamp to be a good therapeutic alternative for treating AA. Additional study by recruiting more patients will be needed to achieve final conclusion for this therapy.
What is new?
308 nm excimer lamp is effective and safe for treatment AA.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Olsen EA. Hair, in Fitzpatrick's Dermatology in General Medicine. In: Feedberg IM, editor. 5th edition. New York: McGraw-Hill; 2003. pp. 641–3. [Google Scholar]
- 2.Ghersetich I, Campanile G, Loti T. Alopecia areata: Immunohistochemistry and ultrastructure of infiltrate and identification of adhesion molecule receptors. Int J Dermatol. 1996;35:28–33. doi: 10.1111/j.1365-4362.1996.tb01611.x. [DOI] [PubMed] [Google Scholar]
- 3.Todes-Taylor N, Turner R, Woods GS, Stratte PT, Morhenn VB. T cell subpopulations in alopecia areata. J Am Acad Dermatol. 1984;11:216–23. doi: 10.1016/s0190-9622(84)70152-6. [DOI] [PubMed] [Google Scholar]
- 4.McDonagh AJ, Tazi-Ahnini R. Epidemiology and genetics of alopecia areata. Clin Exp Dermatol. 2002;27:405–9. doi: 10.1046/j.1365-2230.2002.01077.x. [DOI] [PubMed] [Google Scholar]
- 5.Weissmann I, Hofmann C, Wagner G, Plewig G, Braun-Falco O. PUVA-therapy for alopecia areata: An invest study. Arch Dermatol Res. 1978;262:333–6. doi: 10.1007/BF00447370. [DOI] [PubMed] [Google Scholar]
- 6.Lassus A, Kitano U, Johansson E, Juvakoski T. PUVA treatment for alopecia areata. Dermatologica. 1980;161:298–304. doi: 10.1159/000250381. [DOI] [PubMed] [Google Scholar]
- 7.Claudy AL, Gagnaire D. PUVA treatment alopecia areata. Arch Dermatol. 1983;119:975–8. [PubMed] [Google Scholar]
- 8.Healy E, Rogers S. PUVA treatment for alopecia areata – does it work? A retrospective review of 102 cases. Br J Dermatol. 1993;129:42–4. doi: 10.1111/j.1365-2133.1993.tb03309.x. [DOI] [PubMed] [Google Scholar]
- 9.Behrens-Williams SC, Leiter U, Schiener R, Weidmann M, Peter RU, Kerscher M. The PUVA-turban as a new option of applying a dilute psoralen solution selectively to the scalp of patients with alopecia areata. J Am Acad Dermatol. 2001;44:248–52. doi: 10.1067/mjd.2001.110060. [DOI] [PubMed] [Google Scholar]
- 10.Kölgen W, Both H, van Weelden H, Guikers KL, Bruijnzeel-Koomen CA, Knol EF, et al. Epidermal langerhans cell depletion after artificial ultraviolet B irradiation of human skin in vivo: Apotosis versus migration. J Invest Dermatol. 2002;118:812–7. doi: 10.1046/j.1523-1747.2002.01742.x. [DOI] [PubMed] [Google Scholar]
- 11.Happle R. Topical immunotherapy in alopecia areata. J Invest Dermatol. 1991;96:71S–2S. doi: 10.1111/1523-1747.ep12471884. [DOI] [PubMed] [Google Scholar]
- 12.Ree K. Reduction of Langerhans cells in human epidermis during PUVA therapy: A morphometric study. J Invest Dermatol. 1982;78:488–92. doi: 10.1111/1523-1747.ep12510257. [DOI] [PubMed] [Google Scholar]
- 13.Novak Z, Bonis B, Baltas E, Ocsovszki I, Ignacz F, Dobozy A, et al. Xenon chloride ultraviolet B laser is more effective in treating psoriasis and in inducing T cell apoptosis than narrow-band ultraviolet B. J Photochem Photobiol B. 2002;67:32–8. doi: 10.1016/s1011-1344(02)00280-4. [DOI] [PubMed] [Google Scholar]
- 14.Satho Y, Kawada A. Action spectrum for melanin pigmentation to ultraviolet light, and Japanese skin typing. In: Fitzpatrick TB, Wick MM, Toda K, editors. Brown melanoderma. Biology and disease of epidermal Pigmentation. Tokyo: University of Tokyo Press; 1986. pp. 87–95. [Google Scholar]


