Abstract
Streptococcus agalactiae (group B Streptococcus, GBS) vaginal pathogenicity is not uniformly acknowledged throughout the literature; accordingly, in women, genital itching and burning, along with leukorrhea are commonly and almost exclusively referred to bacterial vaginosis, candidiasis and trichomoniasis. Conversely, GBS virulence for vagina was recognized in the past, as the organism has been observed to potentially cause local inflammation and discharge, as well as lactobacilli rarefaction. We depict here a case where a nonhemolytic (γ-hemolytic) GBS strain was found to be the etiologic agent of vaginal infection. Such uncommon S. agalactiae phenotypes are hard to be recognized and may be therefore responsible for misdiagnosing and underestimation of GBS vaginitis prevalence; here, we had the support of the Liofilchem® Chromatic StreptoB medium, that successfully detected such an atypical variant.
Keywords: Streptococcus agalactiae, group B antigen, GBS, vaginitis, leukorrhea
Case report
Streptococcus agalactiae (group B Strep-tococcus, GBS) is responsible for serious infections in newborns, such as septicemia, meningitis, and pneumonia. Also, it may cause diverse diseases in the adult population, including skin, soft tissue, urinary tract and osteoarticular pathologies, pneumonia, peritonitis, meningitis, endocarditis, pyometra and bacteremia (without a focus). Nevertheless, GBS pathogenicity for vagina is not uniformly acknowledged; hence, the organism is not usually included, unfortunately, in the etiologic diagnosis of vaginitis. Conversely, it is mostly dismissed as a saprophyte or a transient colonizer despite the isolation as a single organism from vaginal exudates of symptomatic women [3,5].
A 23-year old patient came to our attention due to genital pruritus and burning, white discharge and mucosal erythema (the latter was documented at speculum examination). Exudate observation under a microscope showed numerous polymorphonuclear cells and Gram positive cocci (bacteria were even inside leukocytes), along with lactobacilli rarefaction, and absence of ‘clue cells’, Trichomonas vaginalis trophozoites and fungal images (blastospores, hyphae, pseudohyphae). pH value was >4.5 (that is alkaline), with a negative amine test. Both the clinical and the microbiological pictures indicated therefore an ongoing vaginal infection due to coccoid organisms, and with underlying rarefaction of the saprophyte microflora.
When cultivating the woman’s exudate, a massive growth of nonhemolytic (γ-hemolytic), Gram positive, catalase- and coagulase-negative cocci was obtained on the bioMérieux Columbia agar (plus 5% sheep blood) (Figure 1); culture was pure, as no other bacterial phenotypes could be observed on none of blood medium, mannitol salt and MacConKey agar; also, Sabouraud plates did not show any fungal growth (after concomitant incubation both at 36±1°C and 25±1°C, for 4 days). Such an isolate was unexpected, and initially labeled as belonging to the normal microflora. Nevertheless, given it was a pure culture, we carefully studied it, and surprisingly found it possessed the Lancefield group B antigen (latex test by Liofilchem®, Roseto degli Abruzzi, Italy). Also, after 24 h incubation, the Chromatic Strepto B medium (Liofilchem®) showed green-blue colonies (Figure 2) that are described (in the product package insert) to be formed by GBS (enterococci produce instead purple colonies). In agreement, the Vitek2 system (bioMérieux, Marcy l’Etoile, France) provided identification as S. agalactiae (99% certainty). The isolate was finally deposited into our laboratory collection as S. agalactiae strain Sa29.
Figure 1.

A: Strain Sa29 – B: A typical β-hemolytic GBS isolate from our bacteriology lab, Pescara (PE), Italy (Right image from ‘Savini et al., Group B Streptococcus agalactiae interspecies exchange, Vet Microbiol. 2013 [Epub ahead of print]’).
Figure 2.
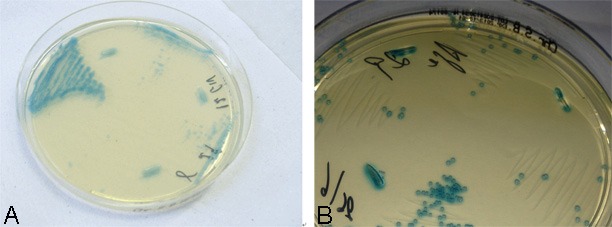
Strain Sa29 grown on the Liofilchem® Chromatic StreptoB (24 h incubation).
The patient made a full recovery after 10-day topic lactobacilli (1 capsule/die) plus 6-day oral amoxicillin (1 gr, twice a day). Post-therapy cultures performed after two weeks from stopping treatment showed restoration of a normal microflora as well as GBS eradication. Particularly, it was also suggested that the β-lactam be assumed by her partner, too.
We believe readers may capture a few interesting messages from this brief communication. First, S. agalactiae pathogenicity for vagina is poorly acknowledged, then the organism is mostly labeled as an innocent by-stander despite the isolation as a pure culture from leukorrhea patients [1,3,5,6]. Nevertheless, GBS has been observed to provoke cytokine release in the vaginal tissue, genital inflammation as well as decrease of the lactobacillary microflora; it is therefore a potential cause of vulvovaginal burning, discharge (usually clear/white-coloured), and fiery red labia, even with fissures [1].
Secondly, nonhemolytic GBS isolates are presumed to be uncommon (5-8% of all isolates) [6]; indeed, we believe their prevalence might be underestimated due to misdiagnosing. The case we presented, moreover, further highlights that such phenotypical variants may show the same pathogenicity as the more commonly encountered β-hemolytic S. agalactiae strains. Particularly, then, when γ-hemolytic streptococci are found to massively grow from symptomatic women, and in the absence of any other detectable vaginal pathogen, they should always be screened for the group B antigen. Otherwise, their recognition on a visual basis is exceedingly hard and, unfortunately, chromogenic media may fail in identifying such phenotypes [6]. We achieved a good result with the Liofilchem® Chromatic Strepto B. However, no further observation has been published to our knowledge about this medium performance, so a wider number of β- and γ-hemolytic GBS strains must be tested in order to define this product’s properties and limits.
Nowadays, vaginal inflammation is mostly considered to be related to Candida and T. vaginalis[2,4]; nonetheless, we would like to finally emphasize that GBS may represent an underestimated agent of vaginitis. Recognition of γ-hemolytic variants may shed more light on S. agalactiae genital infection prevalence; in this context, a reliable etiologic diagnosis, achieved through both standard and chromogenic media (provided that these may detect nonhemolytic phenotypes), is indispensable to avoid improper treatments and chronification of female discomfort.
Disclosure of conflict of interest
None to declare.
References
- 1.Cohain JS. Long-term symptomatic group B streptococcal vulvovaginitis: eight cases resolved with freshly cut garlic. Eur J Obstet Gynecol Reprod Biol. 2009;146:110–111. doi: 10.1016/j.ejogrb.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 2.Derbent AU, Ulukanlıgil M, Keskin EA, Soylu G, Kafalı H. Does vaginal irrigation with saline solution in women with infectious vaginitis contribute to the clinical and microbiological results of antibiotic therapy? Gynecol Obstet Invest. 2012;73:195–200. doi: 10.1159/000332396. [DOI] [PubMed] [Google Scholar]
- 3.Farley MM, Harvey RC, Stull T, Smith JD, Schuchat A, Wenger JD, Stephen DS. A population-based assessment of invasive disease due to group B Streptococcus in nonpregnant adults. N Engl J Med. 1993;328:1807–1811. doi: 10.1056/NEJM199306243282503. [DOI] [PubMed] [Google Scholar]
- 4.Fule SR, Fule RP, Tankhiwale NS. Clinical and laboratory evidence of Trichomonas vaginalis infection among women of reproductive age in rural area. Indian J Med Microbiol. 2012;30:314–316. doi: 10.4103/0255-0857.99493. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R, Das A, Krishna PS. Streptococcus agalactiae causing pyometra in an elderly female with cervical cancer. J Infect Dev Ctries. 2012;6:891–894. doi: 10.3855/jidc.2159. [DOI] [PubMed] [Google Scholar]
- 6.Nickmans S, Verhoye E, Boel A, Van Vaerenbergh K, De Beenhouwer H. Possible solution to the problem of nonhemolytic group B Streptococcus on Granada medium. J Clin Microbiol. 2012;50:1132–1133. doi: 10.1128/JCM.05372-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


