Abstract
The benefits of laparoscopic surgery have not been available to the majority of Mongolians. Mongolian surgical leaders requested assistance in expanding laparoscopy. A capacity-building approach for teaching laparoscopic cholecystectomy throughout Mongolia is reviewed. A laparoscopic cholecystectomy training program was developed. The program included a didactic course and an intensive 2-week practical operating experience. Courses were taught in Ulaanbataar and at 3 of the 4 regional diagnostic referral and treatment centers from 2006 to 2010. During this training period, a total of 303 teaching laparoscopic cholecystectomies were performed. There was one common bile duct injury and one duodenal injury. The conversion rate was 2.0%. This program has been successful in creating a self-sustaining practice of training. The traditional surgical approach to gallbladder disease in Mongolia has been challenged and has, in turn, been a stimulus for improvement in the medical community.
Keywords: Developing countries, Specialties surgical/education, Cholecystectomy, Laparoscopic, Mongolia, Cholecystectomy laparoscopic/education, Laparoscopy/economics, Laparoscopy/standards
Cholecystectomy is one of the most common operations performed worldwide.1 Laparoscopic cholecystectomy has revolutionized the care of gallbladder disease, allowing for faster recovery, shorter hospitalizations, decreased wound infections, and decreased use of narcotic medications. In developed countries, laparoscopic cholecystectomy has now become the gold standard in the treatment of gallstones. However, open cholecystectomy with its increased morbidity remains the standard of care in developing nations owing to limitations in training, funding, and availability of equipment. The benefits of laparoscopic surgery elude much of the developing world, where people often accept several painful conditions as a fact of life.
In Mongolia, 49% of the 2.7 million people reside in rural areas and live a nomadic lifestyle.2 Mongolia covers a large geographic area equal to the combined areas of Great Britain, France, Germany, and Italy; it is the most sparsely populated country in the world. The dry deserts and wet mountains coupled with the extremes of weather are significant obstacles to adequate road building and impede transportation for patients in need. The vast rural areas of Mongolia are isolated and present a serious challenge to providing access to adequate medical and surgical care.
In 2006, expenditures for health care reached 4.6% of the gross domestic product of Mongolia; this translated into US $23.2 per capita for health care per year.2 Weiser et al3 found that surgery is almost absent in countries where less than US $100 is spent on health care per person per year. Laparoscopic cholecystectomy was first introduced into Mongolia in 1994, but by 2005 only 2% of the gallbladders were being removed laparoscopically, and no laparoscopy was performed outside of the capital city, Ulaanbataar.4,5
The epidemiology of diseases in Mongolia has dramatically changed over the last 3 decades. Where echinococcal disease was one of the leading surgical diagnoses in the early 1960s, it is now uncommon. Today, the second most common cause of hospital morbidity in Mongolia is gastrointestinal diseases, with liver diseases, appendicitis, and gallbladder disease representing the majority of these illnesses. A cohort study in Mongolia in 2006, comparing the few laparoscopic cholecystectomies to the many open cholecystectomies, found that the laparoscopic approach afforded patients lower infection rates and shorter hospitalizations, and provided hospitals cost savings.6
Mongolia is divided into 21 geographic/administrative areas called Aimags. In the early 2000s, the Ministry of Health of Mongolia, in an effort to increase access to improved medical and surgical care to the rural areas throughout Mongolia, designated 4 of the Aimag hospitals as Regional Diagnostic Referral and Treatment Centers (RDRTCs) and targeted them for improved infrastructure and human resource development.
Despite the obvious concerns of inadequate physical and human resources, difficult travel, and relatively limited financial investment in health care, the chief of surgery at the Health Sciences University of Mongolia, recognizing the need for improved treatment for gallbladder disease, requested assistance from the W.C. Swanson Family Foundation (a nonprofit, nondenominational, non-governmental organization [NGO] that had been helping to develop and improve the infrastructure of hospitals in Mongolia since 1999) to help expand laparoscopic cholecystectomy to these 4 RDRTCs. This article reviews the teaching methods and important concepts learned over the last 5 years in expanding laparoscopy in a sustainable manner throughout Mongolia.5
Methods
In collaboration with the Health Science University of Mongolia (HSUM), the Ministry of Health (MOH) of Mongolia, and the W.C. Swanson Family Foundation (SFF), a comprehensive multidisciplinary 2-week laparoscopic cholecystectomy–training course was developed. The organizational components included (1) maneuvering the local political and medical system, including importation laws and agreements, and licensing the surgeons on the teaching team; (2) developing and translating an appropriate didactic curriculum; (3) organizing a functional practical component of the course that trains all important team members and provides a continuum of training including pre-, intra-, and postoperative management; and (4) implementing methods for sustainable infrastructure development that supports laparoscopy in a resource-poor environment.
Maneuvering the political and medical regulatory environment in Mongolia
To facilitate the constant changing laws and regulations, a local Mongolian expert was hired as an in-country facilitator and representative for the SFF. Agreements through the MOH and support from local political representatives led to critical long-term alliances that facilitated the import of the necessary laparoscopic and medical supplies. Also, appropriate medical licenses were obtained through the MOH and the National Mongolian Surgical Society for the foreign surgeons. The chief of surgery at HSUM was instrumental in obtaining the licenses as well as organizing the Mongolian doctors, nurses, and administrators for the courses at the various facilities each year.
Developing the didactic curriculum
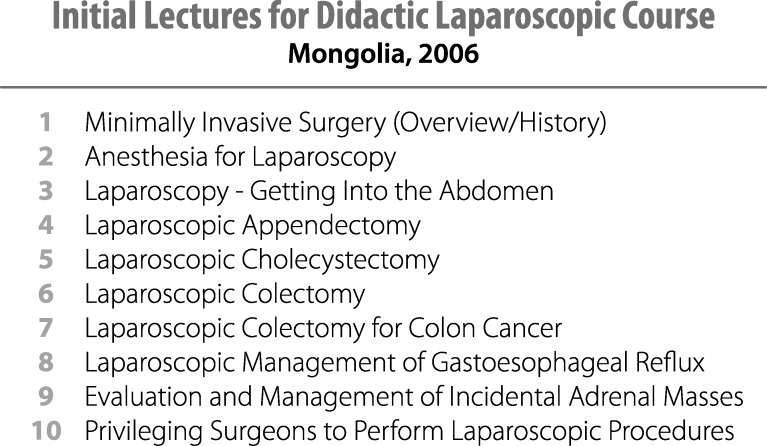
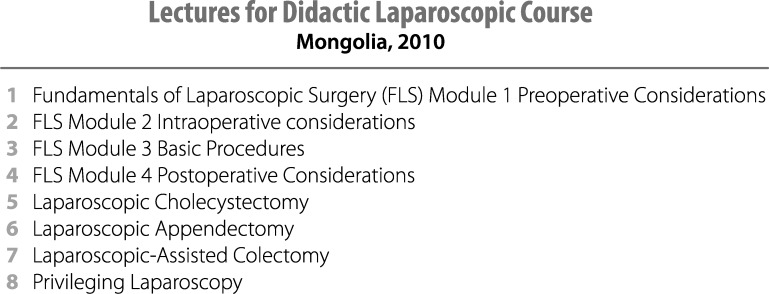
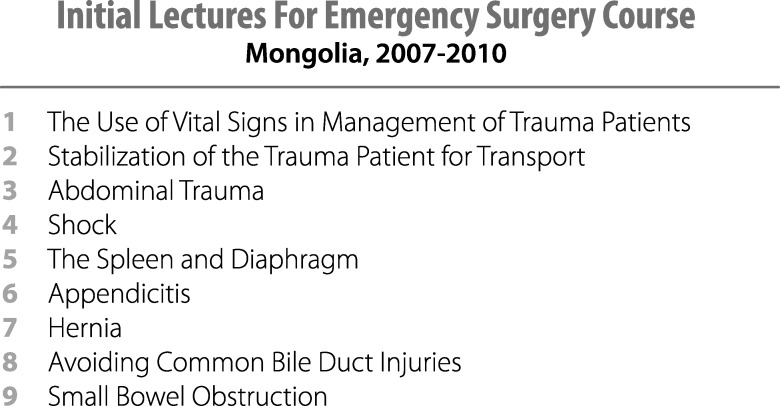
The course combined both didactic and practical sessions. The laparoscopic didactic lectures were given either the first day, or over several days in the morning. The initial topics for the laparoscopic didactic course were developed through discussions between the chief of surgery at HSUM and the medical director for the SFF. The topics included basic and advanced laparoscopic training as the first course and was scheduled for Hospital No. 1 where laparoscopy had begun in 1994 (Fig. 1). Later, with permission from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), the didactic lectures from the Fundamentals of Laparoscopic Surgery course replaced some of the initial lectures. These lectures, combined with those on basic laparoscopy skills, sterile technique, and surgical safety as outlined by the World Health Organization (WHO) surgical safety checklist, provided a total of 8 hours of didactic lectures (Fig. 2). All lectures and presentations were translated into Mongolian. Medical translation for the PowerPoint (Microsoft, Redmond, WA) slides and during the actual course proved to be a significant hurdle solved by collaborating with native surgeons and other physicians from the tertiary care centers in the capital city, who were bilingual in Mongolian and English. Following the direction of the chief of surgery at HSUM, an Emergency Surgery didactic lecture series was also develop and included during the complete 2-week training course at the RDRTCs (Fig. 3). Surgeons and nurses from different surgical specialties (orthopedics, obstetrics and gynecology, and others) attended the didactic portions of the course.
Fig. 1.
Initial lectures for didactic laparoscopy course.
Fig. 2.
Revised lectures for didactic laparoscopy course.
Fig. 3.
Emergency surgery didactic lecture series.
Organizing the practical training component
The first laparoscopic course in 2006 included 1 week of laparoscopic cholecystectomy experience and 1 week of advanced laparoscopic surgical procedures (colectomies, an adrenalectomy, a Nissen fundoplication). From 2007 to 2010, all of the practical laparoscopic training components focused on laparoscopic cholecystectomy, with a few appendectomies. The laparoscopic cholecystectomy practical portion of the course provided general surgeons with 5 days of hands-on experience performing laparoscopic cholecystectomies in 2 different operating rooms. The experience was initially designed to provide 2 to 3 Mongolian surgeons per operating room the opportunity to gradually learn the laparoscopic skills—progressing from camera holder, then advancing to first assistant, and finally to lead surgeon. It was politically very difficult to limit the number of surgeons participating in this first practical session. Many Mongolian surgeons assisted, but few gained enough experience to allow them to act as the lead surgeon. Future courses were able to select the few surgeons who would receive the operative practical experience before the teams arrived, allowing for very intensive, focused training with the graduated approach. The numbers of teaching laparoscopic cholecystectomies were also decreased to 3 (or rarely 4) cases, from 6, per day for each operating room; as 6 cases overwhelmed local resources and staff. Relatively few course participants had received prior training in laparoscopy.
Each course included a multidisciplinary education team consisting of 2 surgeons, an anesthesiologist, an operating room nurse, an operating room scrub technician, and a bio-technician. A surgical resident frequently joined the team to facilitate research and patient improvement projects. Each team member was tasked with training his/her Mongolian counterpart about the specifics of laparoscopic surgery from their perspective. This included not only the intra-operative training, but also the pre- and postoperative management of the patients and the care and cleaning of the equipment. Bio-technicians trained their counterparts on maintenance and repair of the equipment and helped identify sustainable ways to replace and upgrade equipment. Inanimate laparoscopic skill simulator boxes were added to the practical component of the course during the last 2 years (2009–2010).
Due to the infrastructure of the health care system in Mongolia, training began first in the capitol city of Ulaanbaatar (UB), where tertiary care is provided. Training was subsequently expanded to the regional centers in 3 of the 4 regional diagnostic referral centers (Erdenet, Khovd, and Choibalsan), and the fourth (Uvukhanghai) was scheduled for training in June 2011. Each education site received an initial training course and a follow-up course the next year. (The initial course in Choibalsan was completed in 2010.) Participants were issued a certificate of completion signed by the President of the National Mongolian Surgical Society and the Medical Director of the SFF at the conclusion of the course. This did not imply any competency but supported the Mongolian national standards for required continuing medical education.
During the 2 weeks of laparoscopic training, any emergency and trauma cases at that facility were managed together with the local Mongolian surgical team and the visiting surgical education team. This included the pre-, intra-, and postoperative management, with daily combined-team rounds morning and night. Some patients with appendicitis were offered the laparoscopic approach to begin expanding the students' laparoscopic skills. Traditional open surgical procedures were done for all other emergency cases.
Infrastructure development
As laparoscopy requires a totally different set of equipment and instruments, and none of the RDRTCs had any of this equipment, each of the courses included on-site evaluations well in advance of the training sessions. Hospital infrastructure was assessed, including suitability of the power source, status of basic surgical equipment (instruments, cautery, suction, anesthesia machines, operating room lights and beds, autoclaves, and other sterilization methods), and supplies (suture, bandages, medicines). The SFF supplied the necessary infrastructure, initially using equipment obtained from US hospitals that had been refurbished to meet US standards. Working with industry, new equipment and supplies were donated. Containers were shipped months in advance of the education teams, and then installed in the hospitals working with the local Mongolian counterparts. Laparoscopic towers and equipment were installed in each facility (Hospital No. 1, Erdenet; Hospital No. 2, Khovd) prior to the training through the SFF; except in Choibalsan, where a Belgium project had installed some equipment the previous year and had begun laparoscopic training there. Additional laparoscopic equipment was installed in Choibalsan by the SFF. Operating room tables, anesthesia machines, autoclaves, electrocautery machines, open surgical instruments, and open retractors were also donated. Partnerships with industry have begun establishing local vendors in Ulaanbataar to help maintain and provide sources for continued training, supplies, and equipment.
Evaluation
Data were prospectively collected on the numbers of students attending the courses. Patient demographics were collected prospectively on all patients during the training course. Complications were identified prospectively and confirmed with a retrospective follow-up after the courses.
Patient demographics (age and sex), ultrasound findings, procedure type (open versus laparoscopic versus conversion), surgeon (trainee versus trainer), intraoperative complications, and postoperative complications were collected. Hospital records from January 2005 to September 2010 were reviewed in 2 of the 3 regional centers (Khovd and Choibalsan) for all cholecystectomies, and the following data were collected: patient age, sex, preoperative diagnosis, type of procedure, and surgeon. Data collected from Erdenet have recently been published.5
Results
All foreign surgeons and anesthesiologists were able to obtain a medical license while in Mongolia. The study was approved by the chief of surgery at the HSUM, the chief of surgery at each hospital, the hospital administration, and the review board of the SFF.
Training courses were organized and taught in Ulaanbataar at Hospitals Nos. 1 and 2, and at 3 of the 4 RDRTCs in Erdenet, Khovd, and Choibalsan from 2006 to 2010. Erdenet, Khovd, and Choibalsan each only had 4 active general surgeons, all of whom completed the practical training. Courses taught at Hospitals Nos. 1 and 2 included students from multiple hospitals throughout Mongolia.
Mongolian surgeons conducted evaluations of patients with symptoms consistent with gallbladder pathology prior to the arrival of the teaching team. All patients underwent laboratory studies consisting of complete blood count (CBC) and comprehensive metabolic panel (CMP). Nearly all patients underwent right upper quadrant ultrasound to verify the presence of cholelithiasis. The patients selected for laparoscopic cholecystectomy had the presence of stones confirmed and symptoms consistent with symptomatic cholelithiasis. The patients were reexamined the day before the planned surgery with a combined training team of Mongolian and international surgeons. Laboratory and radiographic studies were reviewed together during these preoperative teaching rounds. Patients suspected of having choledocholithiasis or acute cholecystitis were treated by traditional open surgery.
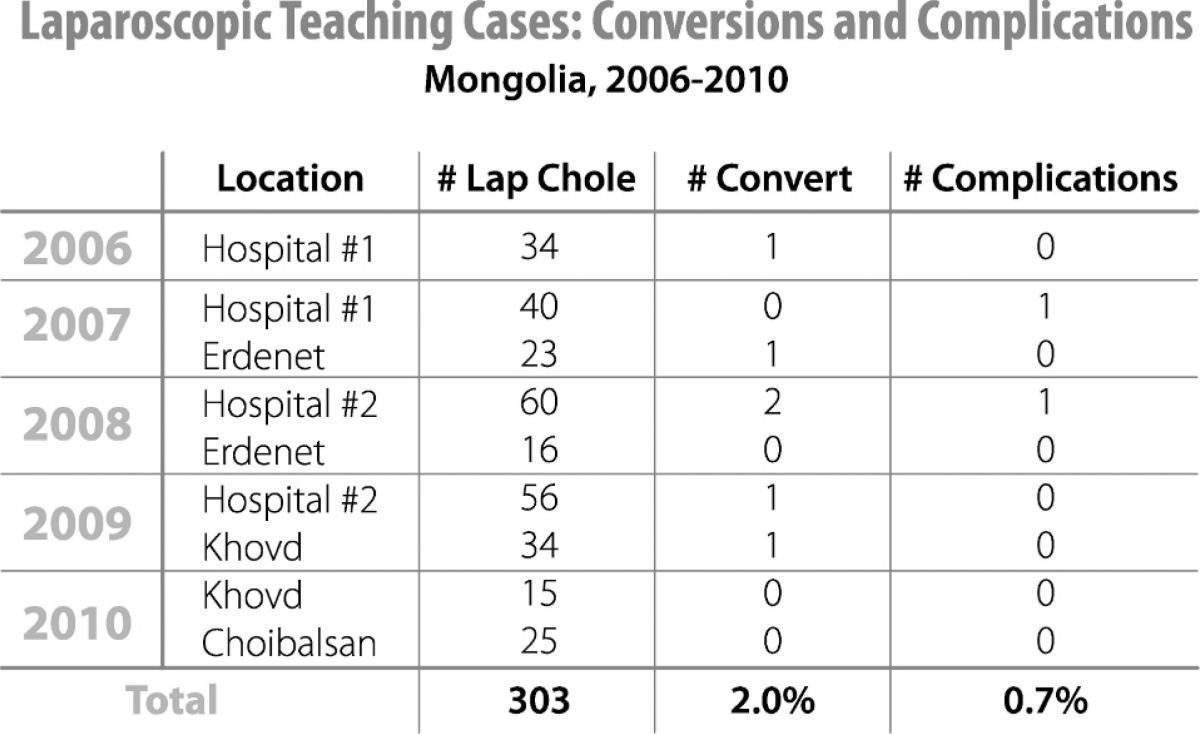
A total of 303 laparoscopic cholecystectomies were performed during the practical components of the courses from 2006 to 2010. The female to male ratio was 3.7∶1. All patients with gallstones were identified preoperatively with ultrasound. There was one common bile duct injury (0.33%) and one duodenal injury (0.33%). The conversion rate was 2.0% (Table 1). Intra-operative cholangiogram technique was taught during 3 cases in Choibalsan, as it was the first facility that had the capability for intra-operative x-ray during our training courses.
Table 1.
Complications and conversion rates in laparoscopic teaching courses (2006–2010)
Operative time, expressed in minutes, was defined as the time of the operation from skin to skin. In Erdenet, the mean operative time for teaching cases was 78 minutes. The average operative times for teaching cases in UB, Khovd, and Choibalsan were 64.3, 82.2, and 92.9 minutes, respectively.
Trainees progressed from camera holders to first assistant once they were able to demonstrate the ability to orient and move the camera appropriately. They did not progress to primary surgeon until they were able to consistently place the instruments safely into the abdomen, handle tissue, retract appropriately, and dissect the gallbladder from the gallbladder fossa. Once these skills were obtained, they were allowed to perform the dissection of the triangle of Calot. Acquisition of all of these skills was the benchmark for successful training.
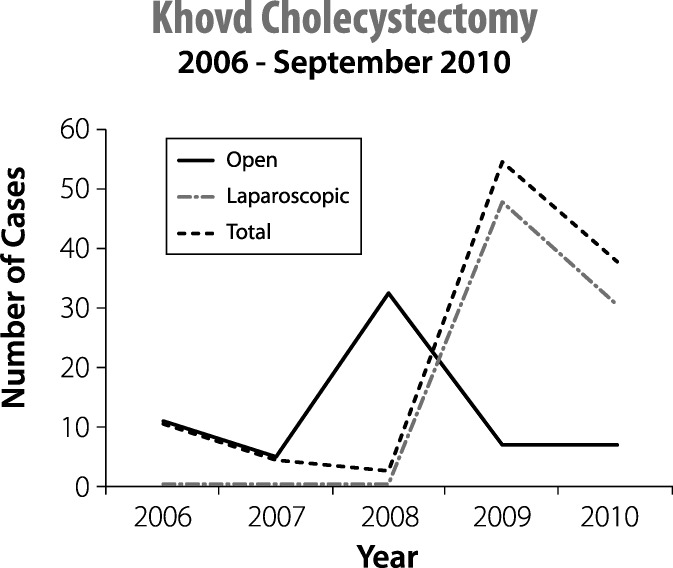
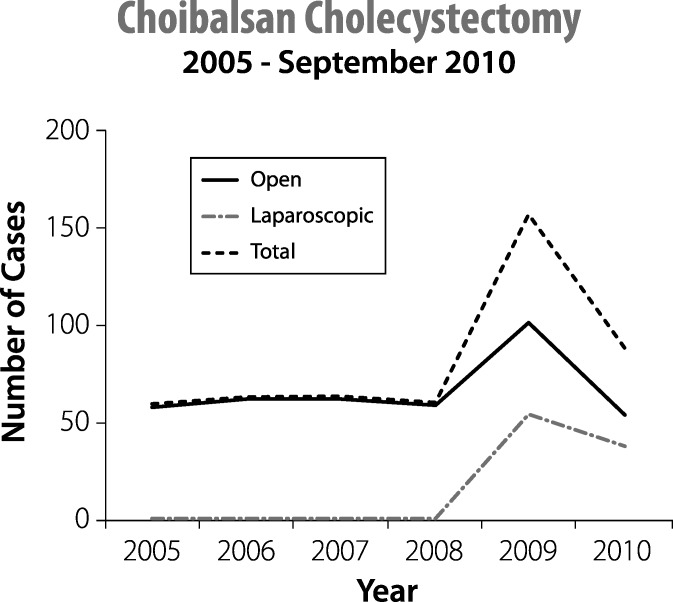
From 2005 to 2008 in Khovd and Choibalsan, all gallbladders were removed by the open technique. The overall frequency of cholecystectomy as well as the number performed laparoscopically has increased in these facilities since training began in 2009 (Figs. 4 and 5).
Fig. 4.
Incidence of cholecystectomy in Khovd.
Fig. 5.
Incidence of cholecystectomy in Choibalsan.
Two of the surgeons who received training during the advanced laparoscopic portion of the 2006 course became part of the SFF education team in Erdenet. Two other surgeons from the 2006 laparoscopic cholecystectomy course also joined the SFF teams to teach in Khovd and Choibalsan. These surgeons have facilitated follow-up on-site proctoring and provided short-term fellowships at their facilities to continue the training of the surgeons from these regional hospitals.
In addition, one of these surgeons has become the medical director of Songdo Hospital, a new private Korean hospital in Ulaanbataar, where he performed nearly 100 laparoscopic colectomies in 2010.
Discussion
The introduction of laparoscopy in resource-poor areas has been a topic of some debate. Some have argued that the introduction of laparoscopy in developing countries does not contribute to the improvement of quality and effectiveness of surgical care unless basic and essential surgical and anesthetic services are strengthened in parallel and that perhaps the drive for laparoscopy is driven by industry or academia and not public demand.7 Others suggest that the benefits of laparoscopy—faster return to work, less pain, and fewer infections—may actually be more important in the developing world, leading to improved productivity in an already fragile economic environment.8
Laparoscopy had previously been introduced into Mongolia in 1994, but 10 years later, very few laparoscopic cholecystectomies were being performed. Barriers to the expansion of laparoscopy included the lack of adequate training and significantly limited resources, especially in the rural regions. In Mongolia, the impetus for the expansion of a laparoscopic program resulted from a concerted campaign from the local surgical community to address a critical need for their country. The partnership created between the Health Sciences University of Mongolia and the W.C. Swanson Family Foundation as well as the continued support of the entire surgical community has been an extremely important concept for the successful and sustainable introduction of laparoscopy in Mongolia.
Many lessons were learned from the initial course taught in 2006, as the teams had to carefully navigate the cultural and political nuances. In Mongolia, physicians are trained in a system where they learn by watching and only sometimes assisting. Despite the predesigned curriculum, this led to many surgeons each assisting during the practical component of the laparoscopic cholecystectomy training without providing anyone with enough experience to competently perform a laparoscopic cholecystectomy independently. In order for the training to be effective, local leaders had to be convinced that a different method of teaching was required; training 2 surgeons in one operating room over several days as they progressed through a graduated experience would allow the surgeons to become somewhat proficient in the technique. The chief of surgery, Dr Sergelen, commented in 2009 that one of the most important aspects of the training program had been the introduction of a new way to teach surgery in Mongolia—a “hands-on” approach that allows the surgeons to “do” rather than just “watch”—leading to a more rapid acquisition of new surgical skills. It was much easier to consolidate the practical training in Erdenet, Khovd, and Choibalsan, as each facility had only 4 general surgeons and had selected 2 for the majority of the operative experience. One of the most important aspects of this training course is the training of surgeons in their native operative environment. They are able to learn on their own equipment and are involved in troubleshooting and problem solving when issues with the existing infrastructure arise. All trainees continue to practice at the RDRTC where they received their training.
Understanding the limitations imposed by the medical system's infrastructure was another lesson learned during the 2006 course. Sterilization of instruments to allow rapid turnover of the operating room was a limiting factor. Lack of adequate human resources and time, as well as the concern of inadequate sterilization and transmission of infectious diseases if the system was strained, forced us to reevaluate the feasibility of performing a large volume of cases. To overcome this problem, the number of procedures being done per day was decreased by nearly half, and enough scopes and instruments are now taken to each site to allow adequate sterilization to safely facilitate 3 to 4 laparoscopic cases per day.
Combining emergency and essential surgical training in parallel with the laparoscopic training for the RDRTCs indeed has allowed for culturally acceptable methods to improve surgical care in general. Teaching laparoscopic surgery not only led to the expansion of more modern surgical techniques to rural Mongolia, but it also enabled improved reception for basic surgical training. In addition to improved decision making and technical abilities of the surgical team, teaching laparoscopy has facilitated the acceptance of sterile technique courses and the implementation of surgical safety measures, such as incorporating the surgical safety checklist and implementing a “time out” at the beginning of the cases. By providing the surgeons in Mongolia with the training they requested, trust has been gained, allowing for the introduction of training in trauma surgery, emergency surgery, and pediatric surgery and anesthesia, in addition to laparoscopy.
Several studies in developing nations have documented both the feasibility and safety of performing laparoscopic cholecystectomies.9–11 With careful patient selection, the safety of same-day laparoscopic cholecystectomy has also been established.1,12,13 The majority of this experience has been carried out in tertiary care centers and has not been well studied in rural centers. As with the experience in developed countries, there is a learning curve for the mastery of laparoscopic skills. Complication and conversion rates in Mongolia are consistent with those seen at the inception of laparoscopy in the 1990s.5
One might expect the complication rate to be elevated during the practical portion of the training period where surgeons learning laparoscopy have not had previous experience. However, the common bile duct injury rate and bowel injury rate thus far has been extremely low during the 303 laparoscopic cholecystectomy cases performed. Although converting to an open procedure is taught as good clinical judgment and not a complication, the conversion rate as well has been extremely low during the training courses. An initial report of complication and conversion rates in Ulaanbataar and Erdenet indicated acceptable rates following the trainings.5
The multidisciplinary team approach, teaching comprehensive surgical care (pre-, intra-, and postoperative care), and introducing twice daily team rounds with surgery, anesthesia, and nursing was one of the features most appreciated by our hosts. A significant amount of time was spent discussing and reviewing the appropriate work-up and selection of patients for surgery. Teaching appropriate patient selection and criteria for the safe administration of anesthesia provided excellent opportunities to improve perioperative care. The notion that a patient scheduled for surgery should be cancelled if not medically optimized has been an important concept taught during all of the courses. The postoperative management training has been facilitated by improving monitoring capabilities of each facility. An important aspect of this course includes training for each person involved in laparoscopy, including the central processing staff sterilizing the equipment, operating room personnel cleaning the instruments, administrators who provide financial and leadership support to replace and repair the equipment, and the bio-technical support personnel who maintain and troubleshoot the equipment in the operating room.
Laparoscopy has been a gateway to improve the infrastructure of tertiary and regional care centers. In a recent update from Erdenet, the improved infrastructure has allowed the hospital there to increase the volume of surgeries performed and to do a larger variety of cases. Subsequently, they report that wait lists for surgery have dropped dramatically, and infection rates have improved. In Khovd and Choibalsan, the overall number of cholecystectomies has been increasing as well as the number performed laparoscopically. It is hard to imagine that the incidence of gallbladder disease is increasing this dramatically. The increase in cholecystectomy may reflect the improved infrastructure that lends itself to increased capability. It may also represent the increased skills of the surgeons and their willingness to perform the surgery.
Prior to our training courses in 2006, many of the Mongolian people, especially those in the rural areas, were very skeptical about laparoscopic surgery. Just as the support of the medical community is necessary for a program of this type to thrive, the public must also be educated about the new technology and its benefits. A task of this magnitude would not succeed in an environment where the community was distrustful of the technology or apprehensive of its benefits. Therefore, a component of this project included public education utilizing the local media to dispel myths and to clarify the purpose and intent of the mission. The rise in gallbladder surgery may also reflect the general population's increasing acceptance of laparoscopy. The training has led to many patients commenting that their trust in their surgeons has increased dramatically, leading to their willingness to undergo surgery in these facilities. The surgeons in Erdenet expressed that by educating the general population on the benefits of laparoscopy, the public will begin to demand increased access to laparoscopy and initiate lobbying efforts to increase funding from the government to support and sustain this technology.
The ultimate goal of this program has been to provide Mongolian surgeons with the tools and skills necessary to advance the medical and surgical care of their country. Professors from the university were recruited to translate and assist in the training of their rural colleagues. This was a vital component of the program as it helped foster a mentoring relationship between academic and rural surgeons. The program was designed to accommodate two visits to each training site in consecutive years. Some of the course participants had received laparoscopic training from other visiting foreign medical teams prior to participating in one of our courses. Moreover, many surgeons sought additional training opportunities abroad after participation in this course. Laparoscopic training in Mongolia has been an enabling process that has provided the local surgeons with an improved confidence and self-satisfaction; they can now provide modern surgical care for their people similar to the care available in other parts of the world.
A multidisciplinary team approach, including representatives from industry, is essential in creating a sustainable and practical program. While equipment can be donated, it is critical to supply these nations with technological back-up and training in maintenance of the equipment, so that they may evolve their medical centers at their own pace.14 In order to avoid the so-called “brain drain,” it is important to train surgeons in their own environment, and the training must be adapted to meet the needs of the population.15 While the medical infrastructure of most developing countries is in need of improvement in several areas, this should not be viewed as a contraindication to the introduction of new techniques. Laparoscopy should be viewed as an extension of general surgery and not a different type of surgery.16
With the ubiquitous access to information available on the Internet and other media sources, the global community is beginning to understand possibilities for improving their access to quality surgical care and is demanding the benefits from minimally invasive surgery. Overcoming barriers of limited resources and human capital to develop laparoscopy can be achieved in communities where they feel the benefits are significant and they have the motivation to maintain it. This education model has provided direct training to surgical teams in the capital and the Regional Diagnostic Referral and Treatment Centers in Mongolia as requested by the Mongolian surgical leaders; subsequently, this has provided improved access to modern surgical care in rural Mongolia. The focused training on laparoscopic cholecystectomy in a country that has a high prevalence of the disease has allowed for adequate practical experience during short-term training expeditions. Team training, infrastructure development, integration of laparoscopic training with essential and emergency surgical care, and partnering with local laparoscopic leaders have been key to the successful and sustained laparoscopic development in Mongolia.
Footnotes
Reprint requests: Raymond R. Price, MD, Intermountain Surgical Specialists, 5169 South Cottonwood Street, Suite 410, Salt Lake City, Utah 84107.
References
- 1.Thomas S, Singh J, Bishnoi PK, Kumar A. Feasibility of day-care open cholecystectomy: evaluation in an inpatient model. ANZ J Surg. 2001;71(2):93–97. doi: 10.1046/j.1440-1622.2001.02046.x. [DOI] [PubMed] [Google Scholar]
- 2.Gunsentsoodol B, Nachin B, Dashzeveg T. Surgery in Mongolia. Arch Surg. 2006;141(12):1254–1257. doi: 10.1001/archsurg.141.12.1254. [DOI] [PubMed] [Google Scholar]
- 3.Weiser TG. et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–144. doi: 10.1016/S0140-6736(08)60878-8. Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR. [DOI] [PubMed] [Google Scholar]
- 4.Rusher AH. Outreach surgery: surgical technology arrives in Mongolia. Bull Am Coll Surg. 1999;84(3):21–25. [Google Scholar]
- 5.Straub CM. Expanding laparoscopic cholecystectomy to rural Mongolia. World J Surg. 2011;35(4):751–759. doi: 10.1007/s00268-011-0965-2. Price RR, Matthews D, Handrahan DL, Sergelen D. [DOI] [PubMed] [Google Scholar]
- 6.Sergelen O. Development of laparoscopic surgery in Mongolia. Available at: http://www.gfmer.ch/Medical_education_En/PGC_RH_2006/Reviews/pdf/Orgoi_laparoscopy_2006.pdf. Accessed March 13, 2010. [Google Scholar]
- 7.Contini S, Taqdeer A, Gosselin RA. Should laparoscopic cholecystectomy be practiced in the developing world? The experience of the first training program in Afghanistan. Letter. Ann Surg. 2010 doi: 10.1097/SLA.0b013e3181d13ff8. 251(3):574–575. [DOI] [PubMed] [Google Scholar]
- 8.Alfa-Wali M, Antoniou A. Should laparoscopic cholecystectomy be practiced in the developing world. doi: 10.1097/SLA.0b013e3181cb8b1c. Letter. Ann Surg 2010;251(2):387–388. [DOI] [PubMed] [Google Scholar]
- 9.al Hadi FH. Comparison of laparoscopic and open cholecystectomy at Prince Abdulrahman Al Sudairy Hospital, Saudi Arabia. East Afr Med J. 1998;75(9):536–539. Chiedozi LC, Salem MM, George TV, Desouky M, Pasha SM. [PubMed] [Google Scholar]
- 10.Brekalo Z. Ten years of laparoscopic cholecystectomy: a comparison between a developed and a less developed country. Wien Klin Wochenschr. 2007;119(23–24):722–728. doi: 10.1007/s00508-007-0906-0. Innocenti P, Duzel G, Liddo G, Ballone E, Simunovic VJ. [DOI] [PubMed] [Google Scholar]
- 11.Udwadia TE. Laparoscopic cholecystectomy in India. Int Surg. 1992;77(3):149–153. Patil SU, Udwadia RT, Bhandarkar DS. [PubMed] [Google Scholar]
- 12.Bal S. Feasibility and safety of day care laparoscopic cholecystectomy in a developing country. Postgrad Med J. 2003;79(931):284–288. doi: 10.1136/pmj.79.931.284. Reddy LG, Parshad R, Guleria R, Kashyap L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chauhan A. Day care laparoscopic cholecystectomy: a feasibility study in a public health service hospital in a developing country. World J Surg. 2006;30(9):1690–1695. doi: 10.1007/s00268-006-0023-7. Mehrotra M, Bhatia PK, Baj B, Gupta AK. [DOI] [PubMed] [Google Scholar]
- 14.Gandhi N, Johari P, Naliyawala H. Overseas training for doctors from developing countries. Letter. Lancet. 1992;339(8792):556. doi: 10.1016/0140-6736(92)90379-h. [DOI] [PubMed] [Google Scholar]
- 15.Friedell MT. Training surgeons in developing countries. Int Surg. 1972;57(8):615–616. [PubMed] [Google Scholar]
- 16.Udwadia TE. Navigating laparoscopic surgery into the next decade in developing countries—a personal perspective. Langenbecks Arch Surg. 2006;392(1):99–104. doi: 10.1007/s00423-006-0093-x. [DOI] [PubMed] [Google Scholar]