Abstract
Patients with incarcerated abdominal wall hernias (AWHs) are often encountered in emergency care units. Despite advances in anesthesia, antisepsis, antibiotic therapy, and fluid therapy, the morbidity and mortality rates for these patients remain high. Between 2006 and 2011, we retrospectively analyzed the cases of 131 patients who underwent emergency surgery for incarcerated abdominal wall hernias. Of these, there were 70 women (53.4%) and 61 men (46.6%) with an average age of 63.3 ± 17.4 years (range, 17–91 years). Morbidity was observed in 28 patients (21.4%), and the mortality rate was 2.3%. Intestinal resection, presence of concomitant disease, and general anesthesia were the independent variants that affected morbidity of patients with incarcerated abdominal wall hernias.
Keywords: Hernia, Incarceration, Morbidity, Mortality
Incarcerated hernia is a hernia that is so occluded it cannot be returned to the abdomen.1 Patients with incarcerated abdominal wall hernia (AWH) (inguinal, femoral, umbilical, and incisional) are frequently encountered in the emergency care unit, and such patients commonly have painful swellings localized in the inguinal or abdominal regions.2 The small intestine, omentum, and colon are the most commonly herniated organs in incarcerated hernia.3 Among the patients with incarcerated hernia, 5% to 13% had emergency surgery, and 10% to 15% required intestinal resection as a result of necrosis.4 The objective of surgical intervention in patients with incarcerated AWH is to obtain low morbidity and mortality, as well as low relapse in the long term.5 Despite advances in anesthesia, antisepsis, antibiotic therapy, and fluid therapy, the morbidity and mortality rates for these patients remain high.4 Here, our objective is to discuss the factors affecting the morbidity and mortality of patients who underwent emergency surgery for incarcerated AWH.
Materials and Methods
In this study, we retrospectively analyzed the records of 131 patients who underwent emergency surgery for incarcerated abdominal wall hernias, between January 2006 and January 2011, at the General Surgery Department of the Dicle University Medicine Faculty. Age, gender, hernia localization, repair technique, anesthesia technique, American Society of Anesthesiology (ASA) scores, additional need of intervention, duration of hospital stay, and morbidity and mortality rates of these patients were recorded. Patients with hernias that could not be reduced and/or those who underwent emergency surgery with findings of peritoneal irritation were included in this study. Patients whose hernias were reduced and who were operated on electively after clinical follow-up were not included in the study. All patients who were admitted to the emergency service underwent routine preoperative laboratory examinations (whole blood count, blood biochemistry, coagulation tests, lung X-ray, and electrocardiography) after physical examination. Patients diagnosed with concomitant diseases by anamnesis and physical examination were held for consultation. The appropriate anesthesia technique was determined by evaluating the patient's general condition, localization of the hernia, suggestion of the anesthetist, and the patient's request. General anesthesia was administered for supraumbilical incisional and umbilical hernia surgery, whereas spinal or local anesthesia was administered for infraumbilical incisional, inguinal, and femoral hernias. The repair technique for the hernias (using a mesh) was the surgeon's choice. Prolene mesh was used to repair the hernias in all the patients. An incision was made over the hernial mass, but a midline incision was used for patients in whom resection could not be achieved through the present incision. All patients received second-generation cephalosporin prophylaxis preoperatively, and on the basis of the surgical findings, an antibiotic for the treatment of anaerobic microorganisms was added to the antibiotic therapy when necessary.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) software for Windows Version 11.5 (Company name, City, State name spelled out) was used for statistical analysis of the study results. Quantitative data were indicated as mean ± standard deviation (SD). The Kolmogorov-Smirnov test was used for the compatibility of normally distributed data. For comparison of the groups, the Mann-Whitney U test was used for analyzing nonparametric data, while the χ2 test was used for analyzing categorical data. Multivariate analyses were used to evaluate the risk factors affecting morbidity and mortality. P values less than 0.05 were accepted to be significant for all variables.
Results
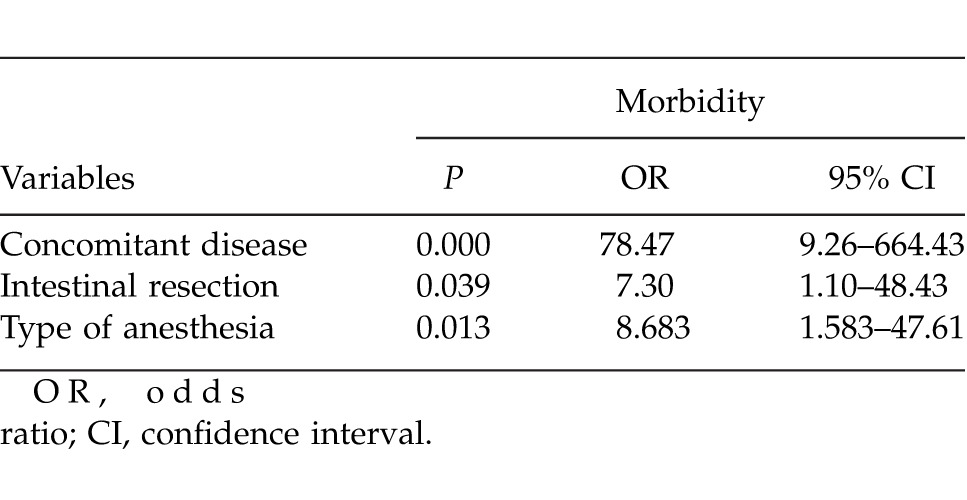
Of the 131 patients, there were 70 women (53.4%) and 61 men (46.6%) with an average age of 63.3 ± 17.4 years (range, 17–91 years). Demographic characteristics of patients are given in Table 1. While inguinal hernia was more frequent in male patients, umbilical, incisional, and femoral hernias were more commonly encountered in female patients (P < 0.001). Mostly loco-regional anesthesia was used for inguinal hernia, while general anesthesia was used for the other hernias (P < 0.001). Less additional intervention was required for patients who underwent inguinal hernia repair as compared with others (P = 0.031). The mean duration of hospital stay was 5.76 ± 2.98 days (range, 2–19 days). In terms of hernia localization, there were no significant differences in the ASA scores, presence of concomitant diseases, necessity of intestinal resection, and morbidity and mortality rates (Table 2). Postoperatively, morbidity was observed in 28 patients (21.4%): 14 (10.8%) had wound infections, 3 (2.3%) had peritonitis, 3 (2.3%) had pneumonia, 2 (1.5%) had deep vein thrombosis, 2 (1.5%) had heart failure, 2 (1.5%) had myocardial infarction, and 2 (1.5%) had urinary tract infection. Postoperatively, 3 patients (2.3%) died. Patients older than 65 years showed significantly higher morbidity rates (P = 0.026), although the mortality rates of this age group were similar to those in the other age groups. Patients who underwent intestinal resection and had both a high ASA score and concomitant disease showed significantly higher mortality and morbidity rates. Further, patients who received general anesthesia had higher morbidity rates compared with those who received loco-regional anesthesia (P < 0.001). Patients who underwent primary repair showed higher morbidity and mortality rates (P = 0.028 and P < 0.001, respectively) as compared with patients in whom prosthetic materials were used. Multivariate logistic regression analysis revealed no independent variant affecting mortality, but intestinal resection, presence of concomitant disease, and general anesthesia were found to affect morbidity (P = 0.039, P < 0.001, and P = 0.013, respectively; Table 3).
Table 1 .
Patient characteristics classified according to hernia types and differences between these categories
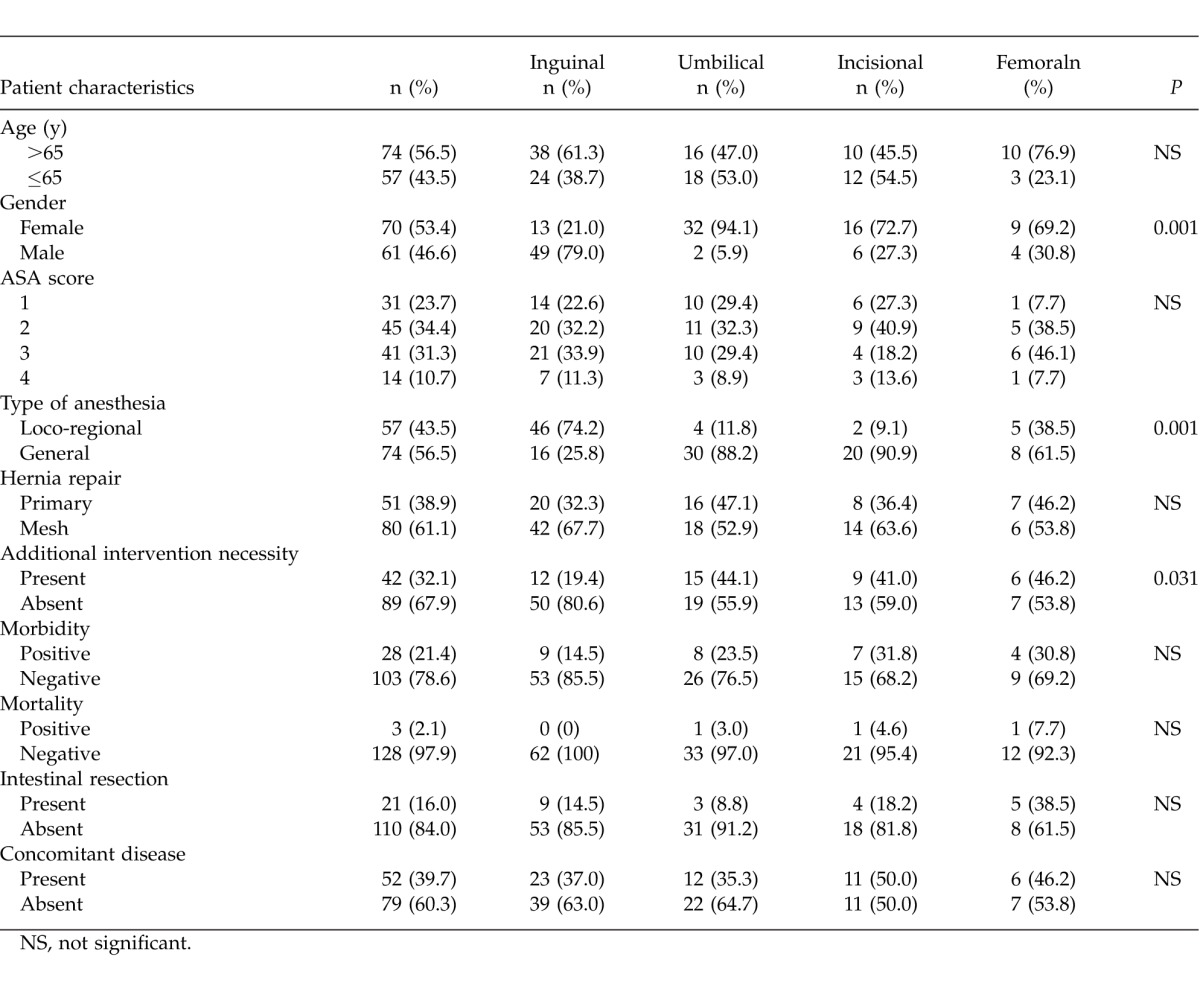
Table 2 .
Univariate analyses of the factors affecting morbidity and mortality
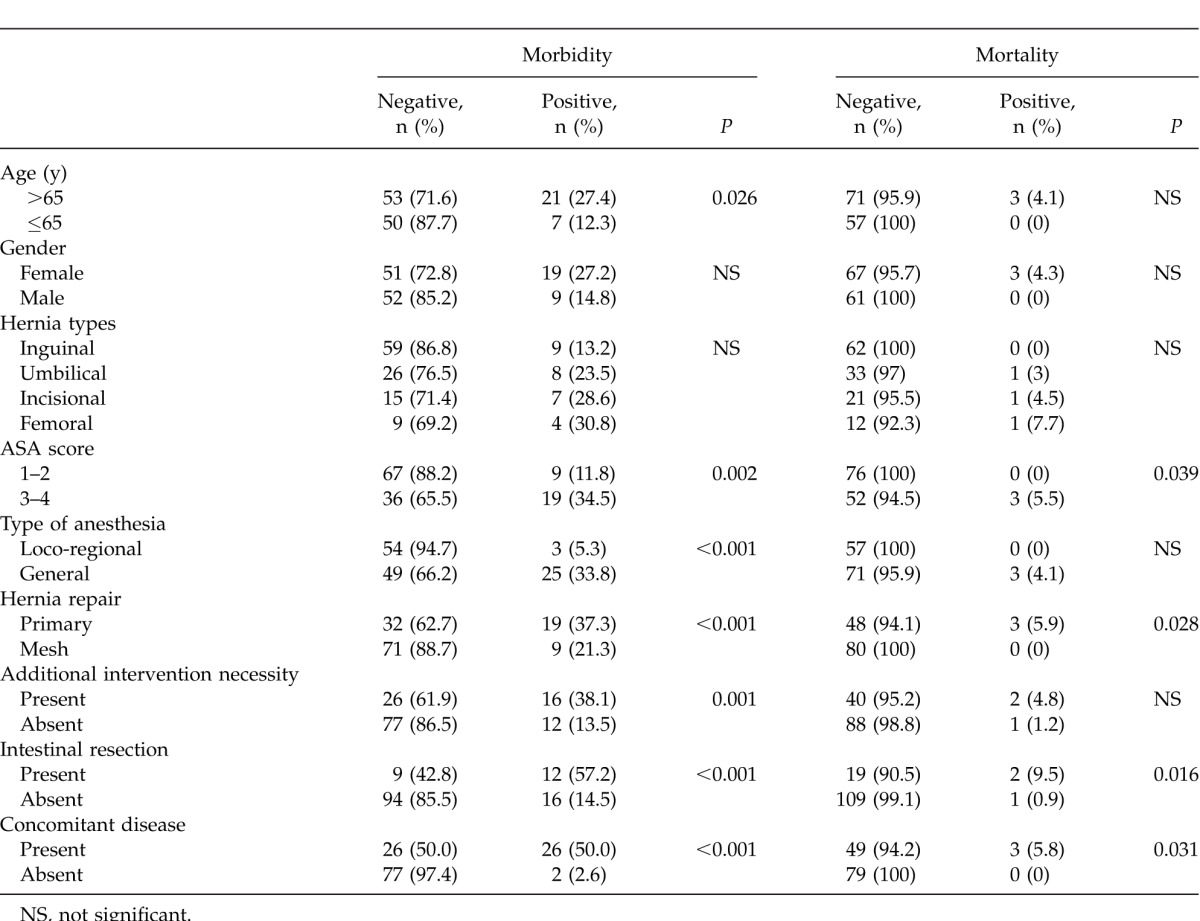
Table 3 .
Multivariate analyses of the factors affecting morbidity
Discussion
As compared with elective repairs, patients with incarcerated AWHs had higher morbidity and mortality rates3 of 19% to 30% and 1.4% to 13.4%, respectively.4,6 In our study, the morbidity rate was 21.4% and the mortality rate was 2.1%. Dunne et al7 reported that postoperative morbidity is high in elderly patients, and Alvarez et al3 noted that in the postoperative period, the incidence of cardiovascular and pulmonary complications is higher in advanced-age groups. Kulah et al8 established that elderly patients with high ASA scores have higher mortality and morbidity. Similarly, Alvarez et al3 reported that patients with concomitant diseases had higher mortality and morbidity rates. In another study, it was demonstrated that a high ASA score is a very important independent variable influencing mortality.9 Our study showed that the morbidity was high in patients older than 65 years (P = 0.026), but there were no significant differences in the mortality rates. Further, the mortality and morbidity rates of patients with high ASA scores were higher than the corresponding rates in patients with lower ASA scores (P = 0.002 and P = 0.039, respectively). Similar to the findings of Alvarez et al,3 our study established high morbidity and mortality rates (P < 0.001 and P = 0.031, respectively) in patients with concomitant disease in the univariate analysis, but high morbidity rate in multivariate analysis (P = 0.001).
There is limited knowledge concerning mesh use to treat incarcerated hernia in emergency surgery.10–12 Prosthetic materials are not used routinely in these patients. Derici et al13 reported that in incarcerated inguinal hernia repair, the risk of recurrence is lower with the usage of prosthetic materials. However, use of prosthetic materials in surgery for patients with acute incarcerated AWH may result in an increased tendency for wound infection.2 In our study, prosthetic materials were used in 61.1% of patients, and this group had lower morbidity and mortality rates than the primary repair group (P < 0.001 and P = 0.028, respectively). However, to avoid bacterial contamination, particularly in patients in whom additional intervention for the intestines was required, prosthetic materials were not used. Therefore, the mortality and morbidity rates were higher in primary repair because of a lack of bacterial contamination. In those patients with incarcerated AWH who required intestinal resection due to necrosis, the duration of hospital stay was longer, resulting in increased morbidity.14 In some studies, it has been shown that intestinal activity directly affects the morbidity and mortality rates.15 In our study, we determined that patients who underwent intestinal resection had higher morbidity and mortality rates. However, in multivariate analysis, intestinal resection was found to be an independent risk factor affecting only morbidity (P = 0.039). For acute cases in which different anesthesia techniques (general and loco-regional) were performed, there was no significant difference in morbidity and mortality. However, patients with concomitant disease and who had general anesthesia were found to have higher morbidity rates.3,8 In our study, patients who underwent general anesthesia had higher morbidity and multivariate analysis, suggesting that general anesthesia is an independent risk factor affecting morbidity (P = 0.013). We consider that this difference is related to the use of different anesthetic techniques in different types of hernia surgery.
One limitation of this study is that there are some differences between the different types of hernias and the techniques for repairing them; in this study, these different types have been grouped together.
Conclusions
Patients with incarcerated AWHs require emergency surgery and have high mortality and morbidity rates. Multivariate logistic regression analysis performed in this study showed that intestinal resection, presence of concomitant disease, and general anesthesia are the factors that affect the morbidity rate of patients who undergo emergency surgery for incarcerated AWHs.
References
- 1.Eveney KE. Hernias and other lesions of the abdominal wall. In: Doherty GM, editor. Current Diagnosis and Treatment: Surgery. New York, N. Y.: McGraw Hill; 2010. pp. 724–736.http://www.accessmedicine.com/content.aspx? In. ed. [Google Scholar]
- 2.Nieuwenhuizen J, van Ramshorst GH, ten Brinke JG, de Wit T, van der Harst E, Hop WC, et al. The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia. 2011;15(3):297–00. doi: 10.1007/s10029-010-0779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvarez JA, Baldonedo RF, Bear IG, Solís JA, Alvarez P, Jorge JI. Incarcerated groin hernias in adults: presentation and outcome. Hernia. 2004;8(2):121–126. doi: 10.1007/s10029-003-0186-1. [DOI] [PubMed] [Google Scholar]
- 4.Derici H, Unalp HR, Bozdag AD, Nazli O, Tansug T, Kamer E. Factors affecting morbidity and mortality in incarcerated abdominal wall hernias. Hernia. 2007;11(4):341–346. doi: 10.1007/s10029-007-0226-3. [DOI] [PubMed] [Google Scholar]
- 5.Ezer A, Calışkan K, Colakoğlu T, Parlakgümüş A, Belli S, Tarım A. Factors affecting morbidity in urgent repair of abdominal wall hernia with intestinal incarceration in adults. Ulus Travma Acil Cerrahi Derg. 2011;17(4):344–348. doi: 10.5505/tjtes.2011.28009. [DOI] [PubMed] [Google Scholar]
- 6.Kulah B, Kulacoglu IH, Oruc MT, Duzgun AP, Moran M, Ozmen MM, et al. Presentation and outcome of incarcerated external hernias in adults. Am J Surg. 2001;181(2):101–104. doi: 10.1016/s0002-9610(00)00563-8. [DOI] [PubMed] [Google Scholar]
- 7.Dunne JR, Malone DL, Tracy JK, Napolitano LM. Abdominal wall hernias: risk factors for infection and resource utilization. J Surg Res. 2003;111(1):78–84. doi: 10.1016/s0022-4804(03)00077-5. [DOI] [PubMed] [Google Scholar]
- 8.Kulah B, Duzgun AP, Moran M, Kulacoglu IH, Ozmen MM, Coskun F. Emergency hernia repairs in elderly patients. Am J Surg. 2001;182(5):455–459. doi: 10.1016/s0002-9610(01)00765-6. [DOI] [PubMed] [Google Scholar]
- 9.Golub R, Cantu R. Incarcerated anterior abdominal wall hernias in a community hospital. Hernia. 1998;2(4):157–161. [Google Scholar]
- 10.Wysocki A, Kulawik J, Pozniczek M, Strzalka M. Is the Lichtenstein operation of strangulated groin hernia a safe procedure? World J Surg. 2006;30(11):2065–2070. doi: 10.1007/s00268-005-0416-z. [DOI] [PubMed] [Google Scholar]
- 11.Pans A, Desaive C, Jacquet N. Use of a preperitoneal prosthesis for strangulated groin hernia. Br J Surg. 1997;84(3):310–312. [PubMed] [Google Scholar]
- 12.Papaziogas B. Lazaridis Ch, Makris J, Koutelidakis J, Patsas A, Grigoriou M et al. Tension-free repair versus modified Bassini technique (Andrews technique) for strangulated inguinal hernia: a comparative study. Hernia. 2005;9(2):156–159. doi: 10.1007/s10029-004-0311-9. [DOI] [PubMed] [Google Scholar]
- 13.Derici H, Unalp HR, Nazli O, Kamer E, Coskun M, Tansug T, et al. Prosthetic repair of incarcerated inguinal hernias: is it a reliable method? Langenbecks Arch Surg. 2010;395(5):575–579. doi: 10.1007/s00423-008-0326-2. [DOI] [PubMed] [Google Scholar]
- 14.Rai S, Chandra SS, Smile SR. A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg. 1998;68(9):650–654. doi: 10.1111/j.1445-2197.1998.tb04837.x. [DOI] [PubMed] [Google Scholar]
- 15.Oishi SN, Page CP, Schwesinger WH. Complicated presentations of groin hernias. Am J Surg. 1991;162(6):568–571. doi: 10.1016/0002-9610(91)90110-y. [DOI] [PubMed] [Google Scholar]


