Abstract
Abnormal uterine bleeding (AUB) is a substantial cause of ill health in women worldwide. In this study, our aim was to evaluate the effectiveness of endometrial ablation using a modified urologic resectoscope along with tranexamic acid in AUB. Sixty patients were enrolled in this study. All patients underwent resectoscopic surgery. Patients were randomly divided into two groups. Group 1 (n = 30) received 500 mg of tranexamic acid. Group 2 (n = 30) served as the control group and underwent surgery without the administration of tranexamic acid. Total pictorial blood loss assessment chart (PBAC) scores were significantly lower postoperatively (152.14 ± 9.65 versus 6.6 ± 0.90; P < 0.001). When stratified by the administration of tranexamic acid, the number of patients with a postoperative day 1 PBAC score ≤15 was higher in the tranexamic group (19 versus 13), whereas the number of patients with a post operative day 1 PBAC score >15 was lower in the tranexamic group (11 versus 17), but the differences were not statistically significant (P > 0.05). AUB is a complex disease that may need repeated treatments. In expert hands, the treatment rate of resectoscopic surgery seems acceptable. However, some patients may require additional interventions, like repeated surgery, hysterectomy, or a drug therapy in the long run. Introduction of tranexamic acid as a potential adjunct to rollerball endometrial ablation may present an interesting option that requires additional well-designed studies before firm conclusions can be made.
Key words: Abnormal uterine bleeding, Endometrial ablation, Resectoscopic surgery
Abnormal uterine bleeding (AUB) is a substantial cause of ill health in women worldwide. AUB accounts for up to 20% of visits to the gynecologist.1
Studies have shown that as many as 79% of such women will have no identifiable source of such bleeding, such as polyps, myomas, hyperplasia, or carcinomas, and subsequently leave the clinician with a “diagnosis of exclusion” of dysfunctional or anovulatory bleeding.2 Reasons for such dysfunction and the actual mechanisms of bleeding are still unclear.
Once a proper diagnosis is established, there is again no consensus on the best treatment, including surgical approaches versus nonsurgical approaches with hormonal and nonhormonal drug therapies.
One common factor in patients is abnormal blood loss from the endometrial lining. Hence, if one could remove the entire endometrial lining by selective destruction of the endometrium, also known as endometrial ablation, in theory, bleeding should stop. Such a procedure can be performed without an incision and have little impact on ovarian hormone production or ovarian reserve. Therefore, it may be an attractive approach. Endometrial ablation may be indicated for the treatment of women who have either menorrhagia or menometrorrhagia due to a benign condition, have completed their childbearing, and have failed medical therapy or cannot receive medical therapy because of a health condition.
There are a number of surgical approaches that attempt treatment of AUB by endometrial ablation. Currently, there are four main techniques: endometrial desiccation with an electrosurgical rollerball or vaporizing electrode, laser endometrial desiccation, and endomyometrial resection using a wire loop. Rollerball endometrial ablation (REA) is the most commonly used resectoscopic method and can be performed with either a monopolar or bipolar resectoscope.
Tranexamic acid, a competitive inhibitor of plasminogen activation, has been used to treat AUB for decades. It is particularly useful in women who either desire immediate pregnancy or for whom hormonal treatment is inappropriate. Tranexamic acid is a well-tolerated treatment that reduces menstrual blood loss in the range of 34% to 59%.3
In this study,4 our aim was to evaluate the effectiveness of endometrial ablation using a modified urologic resectoscope along with tranexamic acid in AUB.
Patients and Methods
From June 2009 to December 2010, a total of 60 patients who attended the gynecology clinic of Istanbul University School of Medicine for uterine bleeding were enrolled in this prospective study. Approval of the ethics committee of Istanbul University and informed consent from all participants were obtained prior to the treatment.
Inclusion criteria for the study were: (1) uterine bleeding not associated with pathology, (2) pictorial blood loss assessment chart (PBAC) score >100, and (3) not responding to medical therapy (i.e., oral progesterone, combined oral contraceptive pill, nonsteroidal anti-inflammatory drugs). All patients underwent transvaginal pelvic ultrasound examination, endometrial sampling with dilatation and curettage, as well as cervical smear sampling to rule out malignancy, blood tests for blood clotting defects, hemoglobin levels, and biochemical pregnancy (β-hCG), and FSH/E2 serum sampling. The diagnosis of menorrhagia was based on assessment of menstrual blood loss using the PBAC of Higham et al.4 The PBAC itself consists of a series of diagrams representing lightly, moderately, and heavily soiled pads on which the patient marks the appropriate box at the time that each item of sanitary protection was discarded. The PBAC scoring system is as follows: 1 point for each lightly stained pad, 5 points for a moderately soiled pad, and 10 points for a pad completely saturated with blood. When added up, total scores represent: 0 points, amenorrhea, absence of menstrual flow; <15 points, spotting, hypomenorrhea; 40 to 70 points, menstrual flow; and >100 points, menorrhagia.
AUB patients were randomly divided into two groups. Group 1, including 30 patients, received 500 mg of tranexamic acid (250 mg during REA and 250 mg 2 hours after REA). Tranexamic acid was administered intravenously to all patients in group 1 in 100 mL normal saline. Group 2, including 30 patients, served as the control group and underwent REA without the administration of tranexamic acid.
Endometrial preparation was undertaken preoperatively with gonadotropin-releasing hormone analog. This was achieved by using 3.6 mg of goserelin acetate (Zoladex, AstraZeneca UK Ltd, London, United Kingdom) 4 weeks preoperatively in all patients.
The resectoscopic surgery was performed with a 26F resectoscope fitted with a monopolar 90° angle knife electrode and with a 0° telescope (Karl Storz GmbH & Co KG, Tuttlingen, Germany). The uterine cavity was examined after distention with a solution of 1.5% glycine irrigant. The endometrium of the cornual areas was coagulated with a 3-mm diameter ball electrode and current set at 90 W, and resection was then performed down to the isthmus with use of a loop with cutting current set at 100 W. Submucous fibroids were resected to the plane of the uterine wall. Active electrodes were powered by Valleylab generators (Boulder, Colorado) at 140 W.
Operating time, total hospital stay, recovery period, and any complications encountered were recorded for all patients.
One day after the treatment and at 12 months, the women's bleeding status was evaluated again with the measurement of hemoglobin levels and PBAC. Patients were evaluated for pain and bleeding 3 months after the treatment as well. To standardize the PBAC scores, all patients enrolled in the study were supplied with the same type and brand of sanitary pads. After their menses, patients returned the PBAC together with all of the soiled sanitary pads. Success of the procedure was defined as a posttreatment PBAC total score of 75 points or less.
All statistical calculations were performed using the Statistical Package for Social Sciences 18.0 (SPSS Inc, Chicago, Illinois). Continuous data were expressed as mean ± SD and compared using the Student t test. Categoric data were expressed as n (%) and compared using the χ2 test. P < 0.05 was considered statistically significant.
Results
Adequate endometrial samples were obtained in all of the patients, of whom 26 had a disordered proliferative endometrium, 23 had endometrial dysfunction (progesterone induced), 7 had atypical simple endometrial hyperplasia, and 4 had polypoid hyperplasia.
Twelve months after REA, 35 patients (58%) reported hypomenorrhea, whereas amenorrhea and spotting were present in 22 patients (37%) and 3 patients (5%), respectively. PBAC scores of hypomenorrhea, amenorrhea, and spotting patients were 35, 22, and 3, respectively.
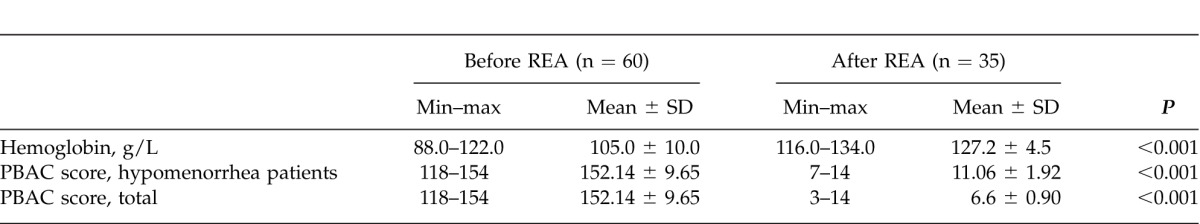
Preoperative and postoperative PBAC scores of hypomenorrhea patients, and all patients and hemoglobin levels are presented in Table 1. Total PBAC scores were significantly lower postoperatively (152.14 ± 9.65 versus 6.6 ± 0.90; P < 0.001), whereas hemoglobin levels were higher postoperatively (10.50 ± 1.00 versus 12.72 ± 0.45; P < 0.001). When hypomenorrhea patients were further analyzed, PBAC scores for this subgroup were significantly lower postoperatively as well (152.14 ± 9.65 versus 11.06 ± 1.92; P < 0.001).
Table 1 .
Comparison of PBAC scores and hemoglobin levels before and after REA
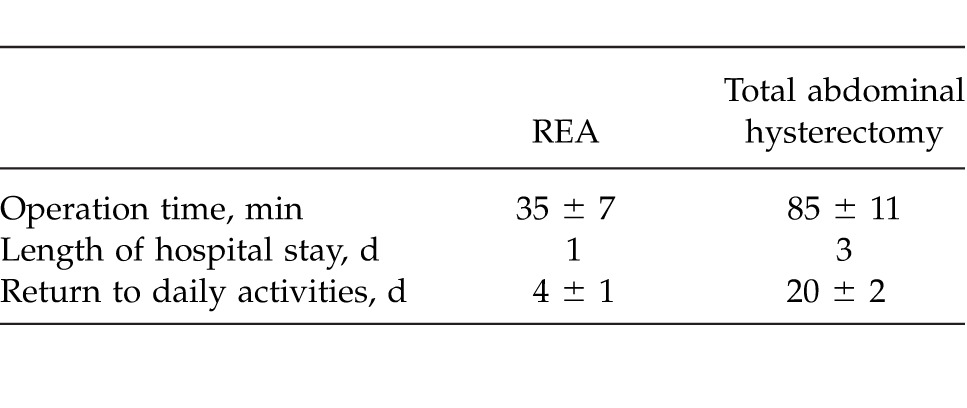
Average length of hospital stay was 1 day, operation length was 35 ± 7 minutes, and return to daily activities was 4 ± 1 days. Table 2 presents the comparison of operation time, length of hospital stay, and time to return to daily activities between REA and our gynecology clinic's abdominal hysterectomy surgeries.
Table 2 .
Comparison of operation time, length of hospital stay, and time to return to daily activities between REA and clinic's abdominal hysterectomy surgeries
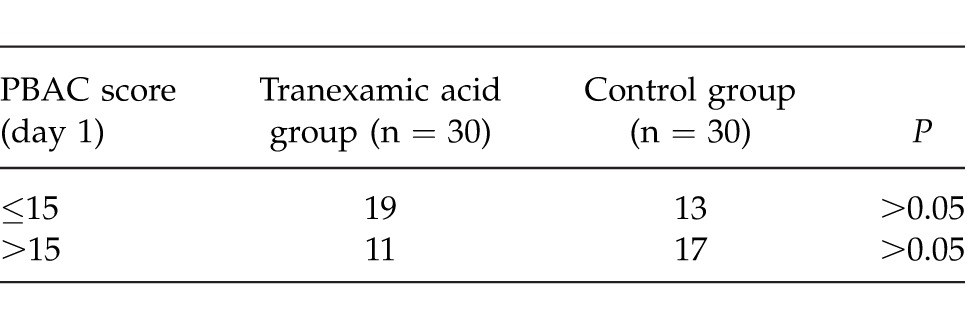
When stratified by the administration of tranexamic acid, the number of patients with a postoperative day 1 PBAC score ≤15 was higher in the tranexamic group (19 versus 13), whereas the number of patients with a postoperative day 1 PBAC score >15 was lower in the tranexamic group (11 versus 17), but the differences were not statistically significant (P > 0.05; Table 3). PBAC score of 15 was chosen as a benchmark because patients who had a PBAC score below 15 were either spotting or with hypomenorrhea.
Table 3 .
Comparison of PBAC scores when stratified by tranexamic acid administration
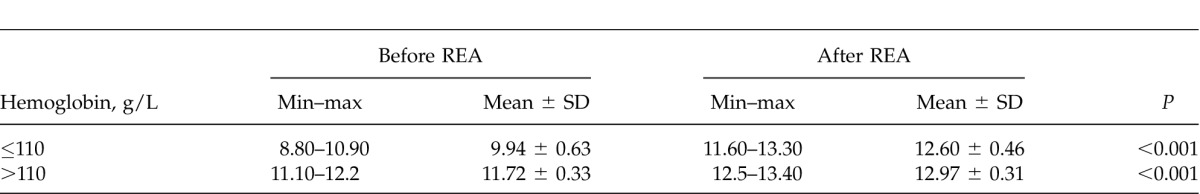
In hemoglobin level measurements, having a score of ≤110 g/L was regarded as anemic, whereas a score of >110 g/L was regarded in the normal range. When preoperative and postoperative hemoglobin levels were compared at the 12-month evaluation, anemic patients had a significant increase in their levels postoperatively (9.94 ± 0.63 versus 12.60 ± 0.46; P < 0.001). A similar finding was observed in normal-range patients (11.72 ± 0.33 versus 12.97 ± 0.31; P < 0.001; Table 4).
Table 4 .
Comparison of hemoglobin levels before and after REA at 12-month evaluation
No complications arose during REA. At the 3-month evaluation, 14 patients (24%) reported mild pelvic pain and received analgesics as a treatment, whereas 12 patients (20%) reported spotting. A total of 4 patients (7%) had pelvic inflammation and received antibiotics as a treatment. A total of 9 patients (15%) complained of heavy bleeding at the 3-month evaluation; 3 of these patients underwent REA again, 1 patient received hormonal therapy (500 mg/d medroxyprogesterone acetate), and 3 patients received tranexamic acid (dosage: 500 mg/d) again. Bleeding stopped spontaneously in 1 patient, and 1 patient had to undergo hysteroscopic adhesiolysis because of adhesions in the uterine cavity. At the 12-month evaluation, 4 patients (7%) presented with persisting pain, and 3 patients (5%) reported spotting. None of the patients required hysterectomy at the 12-month evaluation.
Discussion
Although there are a number of trials for REA, to our limited knowledge, ours is the only study that combines REA with the administration of tranexamic acid to evaluate its effectiveness on AUB.
The highest quality evidence evaluating REA comes from randomized clinical trials and systemic reviews. At this time there are 8 comprehensive randomized studies comparing REA to hysterectomy: 4 from the United Kingdom,5–8 1 from Italy,9 and 3 from the United States.10–12 In addition, these trials have resulted in a number of important additional publications, because the first 5 studies comprise the core of the Cochrane systematic review.13,14 Findings of these studies indicate that women who underwent REA had shorter hospital stays and fewer postoperative complications, and resumed daily activities earlier than those with hysterectomy, which is in line with our findings. However, according to the literature, reoperation rates increased steadily over time—up to about 30% to 40% at 4 years of follow-up in the 2 studies with such a long follow-up interval.10,15 In our study, the follow-up was shorter (up to 1 year), but at 3 months of follow-up, 3 patients had to undergo REA again (5% reoperation rate). In addition, postoperative recurrence was treated with nonsurgical approaches (hormonal treatment or tranexamic acid) in 4 patients. Because none of the patients responded to the drug treatment before REA, one can argue that REA may increase the drug response.
Tranexamic acid is an antifibrinolytic that prevents activation of plasminogen and has been approved by the US Food and Drug Administration for the treatment of menorrhagia. In previous studies, it was used to treat heavy menstrual bleeding. Lukes et al16 administered tranexamic acid to 115 patients with heavy menstrual bleeding. There was a significantly greater reduction in menstrual blood loss of −69.6 mL (40.4%) compared with −12.6 mL (8.2%) in the 72 women who received placebo (P < 0.001); reduction of menstrual blood loss exceeding a prespecified 50 mL; and, lastly, reduction of menstrual blood loss considered meaningful to women. A very recent systemic review by Naoulou and Tsai17 analyzed 10 studies to evaluate the efficacy of tranexamic acid in the treatment of idiopathic and nonfunctional heavy menstrual bleeding. Available evidence indicated that tranexamic acid treatment is effective and safe and could potentially the improve quality of life of patients presenting with heavy menstrual bleeding. In our study, the administration of tranexamic acid during REA lowered the postoperative day 1 PBAC scores, but the difference was not statistically significant. Timing and administration dosage of tranexamic acid may need further studies to improve the treatment outcome in REA, because our study was the first to try administration of this drug during REA. We believe it is worthwhile to carry out additional studies because tranexamic acid has established properties in reducing blood loss and may present an interesting adjunct to REA.
Conclusion
AUB is a complex disease that may need repeated treatments. In expert hands, the treatment rate of REA seems acceptable. However, as established in long-term trials, although a number of women are initially satisfied, some may require additional interventions, such as repeated REA, hysterectomy, or drug therapy. The reasons for these treatment failures are still not clear and deserve further study. Introduction of tranexamic acid as a potential adjunct to REA may present an interesting option that requires additional well-designed studies before firm conclusions can be made.
References
- 1.Goldstein SR. Sonohysterography. In: Timor-Tritsch IE, Goldstein SR, editors. Ultrasound in Gynecology. 2nd ed. Philadelphia, PA: Churchill Livingston Elsevier; 2007. pp. 197–211. In. eds. [Google Scholar]
- 2.Goldstein SR, Zeltser I, Horan CK, Snyder JR, Schwartz LB. Ultrasonography-based triage for perimenopausal patients with abnormal uterine bleeding. Am J Obstet Gynecol. 1997;177(1):102–108. doi: 10.1016/s0002-9378(97)70446-0. [DOI] [PubMed] [Google Scholar]
- 3.Lumsden MA, Wedisinghe L. Tranexamic acid therapy for heavy menstrual bleeding. Expert Opin Pharmacother. 2011;12(13):2089–2095. doi: 10.1517/14656566.2011.598857. [DOI] [PubMed] [Google Scholar]
- 4.Higham JM, O'Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. Br J Obstet Gynaecol. 1990;97(8):734–739. doi: 10.1111/j.1471-0528.1990.tb16249.x. [DOI] [PubMed] [Google Scholar]
- 5.Gannon MJ, Holt EM, Fairbank J, Fitzgerald M, Milne MA, Crystal AM, et al. A randomised trial comparing endometrial resection and abdominal hysterectomy for the treatment of menorrhagia. BMJ. 1991;303(6814):1362–1364. doi: 10.1136/bmj.303.6814.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dwyer N, Hutton J, Stirrat GM. Randomised controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. Br J Obstet Gynaecol. 1993;100(3):237–243. doi: 10.1111/j.1471-0528.1993.tb15237.x. [DOI] [PubMed] [Google Scholar]
- 7.Pinion SB, Parkin DE, Abramovich DR, Naji A, Alexander DA, Russell IT, et al. Randomised trial of hysterectomy, endometrial laser ablation, and transcervical endometrial resection for dysfunctional uterine bleeding. BMJ. 1994;309(6960):979–983. doi: 10.1136/bmj.309.6960.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Connor H, Broadbent JA, Magos AL, McPherson K. Medical Research Council randomised trial of endometrial resection versus hysterectomy in management of menorrhagia. Lancet. 1997;349(9056):897–901. doi: 10.1016/S0140-6736(96)07285-6. [DOI] [PubMed] [Google Scholar]
- 9.Crosignani PG, Vercellini P, Apolone G, De Giorgi O, Cortesi I, Meschia M. Endometrial resection versus vaginal hysterectomy for menorrhagia: long-term clinical and quality-of-life outcomes. Am J Obstet Gynecol. 1997;177(1):95–101. doi: 10.1016/s0002-9378(97)70445-9. [DOI] [PubMed] [Google Scholar]
- 10.Dickersin K, Munro MG, Langenberg P, Scherer R, Frick KD, Weber AM, Johns A, Peipert JF, Clark M. Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding Research Group. Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding (STOP-DUB): design and methods. Control Clin Trials. 2003;24(5):591–609. doi: 10.1016/s0197-2456(03)00023-0. [DOI] [PubMed] [Google Scholar]
- 11.Dickersin K, Munro MG, Clark M, Langenberg P, Scherer R, Frick K. Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding (STOP-DUB) Research Group et al. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding: a randomized controlled trial. Obstet Gynecol. 2007;110(6):1279–1289. doi: 10.1097/01.AOG.0000292083.97478.38. [DOI] [PubMed] [Google Scholar]
- 12.Munro MG, Dickersin K, Clark MA, Langenberg P, Scherer RW, Frick KD. Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding Group et al. The Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding: summary of an Agency for Health Research and Quality-sponsored randomized trial of endometrial ablation versus hysterectomy for women with heavy menstrual bleeding. Menopause. 2011;18(4):445–452. doi: 10.1097/gme.0b013e31820786f1. [DOI] [PubMed] [Google Scholar]
- 13.Lethaby A, Shepperd S, Cooke I, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000 doi: 10.1002/14651858.CD000329. (2):CD000329. [DOI] [PubMed] [Google Scholar]
- 14.Lethaby A, Hickey M. Endometrial destruction techniques for heavy menstrual bleeding: a Cochrane review. Hum Reprod. 2002;17(11):2795–2806. doi: 10.1093/humrep/17.11.2795. [DOI] [PubMed] [Google Scholar]
- 15.Aberdeen Endometrial Ablation Trials Group. A randomised trial of endometrial ablation versus hysterectomy for the treatment of dysfunctional uterine bleeding: outcome at four years. Br J Obstet Gynaecol. 1999;106(4):360–366. doi: 10.1111/j.1471-0528.1999.tb08275.x. [DOI] [PubMed] [Google Scholar]
- 16.Lukes AS, Moore KA, Muse KN, Gersten JK, Hecht BR, Edlund M, et al. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol. 2010;116(4):865–875. doi: 10.1097/AOG.0b013e3181f20177. [DOI] [PubMed] [Google Scholar]
- 17.Naoulou B, Tsai MC. Efficacy of tranexamic acid in the treatment of idiopathic and non-functional heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2012;91(5):529–537. doi: 10.1111/j.1600-0412.2012.01361.x. [DOI] [PubMed] [Google Scholar]


