Abstract
We report on a 33-year-old female liver donor candidate who developed intraoperative latex-induced anaphylactic shock during surgery for living donor transplantation. She was the mother of the organ recipient, who was a 9-year-old boy with biliary atresia. We planned extended lateral segmentectomy for her. Although we dissected the ligament around the left lobe, the systolic blood pressure suddenly dropped and her body became flushed and warm. We administered transfusion and an ephedrine injection to recover the blood pressure. Because she recovered after the treatment, we restarted the procedure. However, she went into shock again within a few minutes. We decided to discontinue the operation. Postoperative blood tests revealed an increase in IgE-RAST and basophil activation, suggesting that the anaphylactic shock was induced by latex. Because latex allergy has become a public health problem, this allergy should be kept in mind as a potential donor operation risk.
Keywords: Latex allergy, Living donor liver transplantation, Anaphylactic reaction, Shock
Latex is derived from the Hevea brasiliensis tree indigenous to the Amazon region of South America. It can be found in many of the items used in the medical-hospital environment, such as tourniquets, catheters, urine collecting bags, tubing, and gloves. These products can be the source of reactions to latex. The first report of anaphylactic reactions linked to latex sensitivity was in 19891 and since then the number of case reports of latex-induced anaphylactic reactions has steadily grown. Here, we report a case of a living donor for liver transplantation in whom latex-induced anaphylactic shock occurred during the operation, necessitating discontinuation of both the donor and recipient operations.
Case Report
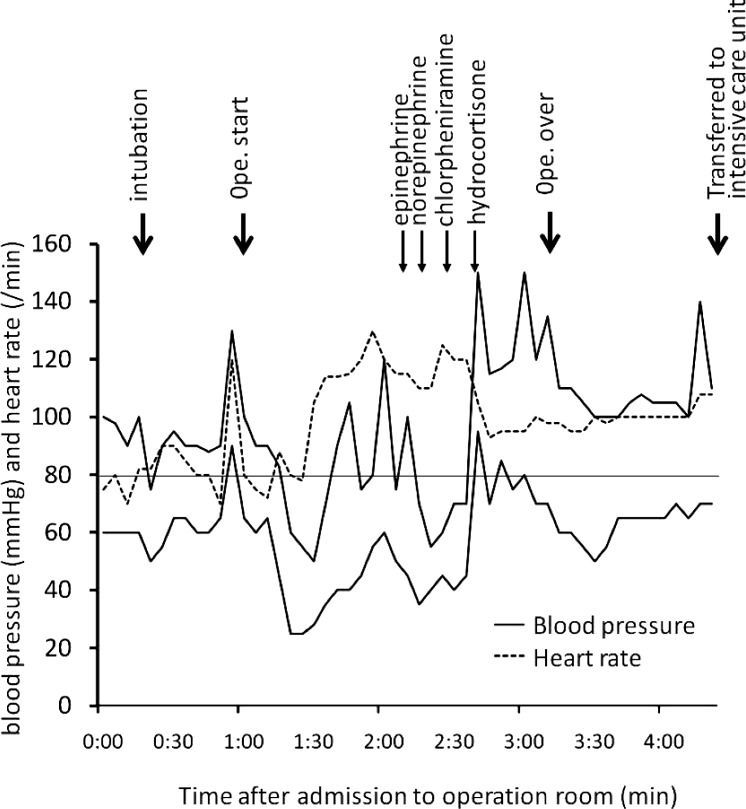
This living donor was a Japanese woman who was 153 cm tall and weighed 56 kg. She was the mother of the organ recipient, who was a 9-year-old boy with biliary atresia. She had undergone cesarean section 4 times in the past and had allergy to pollen and mackerel. Her preoperative evaluation (hemogram, biochemical markers, coagulation profile, hepatitis virus markers, tumor markers, abdominal X-ray, abdominal-enhanced computed tomography [CT], and drip infusion cholangiography CT) revealed no abnormalities, except for positivity to antinuclear antibody. At our facility, intraoperative donor liver biopsy (zero biopsy) is performed routinely at the beginning of living donor liver transplantation (LDLT) to confirm eligibility of the donor liver for LDLT in terms of steatosis and portal zone inflammation.2 We usually perform lateral segmentectomy and extended segmentectomy through a 10-cm incision using a Thompson retractor (Thompson Surgical Instruments Inc, Traverse City, Michigan). For this donor, we planned a 10-cm laparotomy operation that included zero biopsy and subsequent extended lateral segmentectomy, estimating that the graft weight-to-recipient weight ratio was 1.31%. During the operation, we initially made a 10-cm incision in the donor's upper abdomen and performed zero biopsy of the liver, which revealed no abnormal findings. Although we dissected the ligament around the left lobe through this incision, the systolic blood pressure suddenly dropped to 50 mmHg (Fig. 1) and her face and upper extremities became flushed and warm. We stopped the surgical procedure and administered treatment consisting of transfusion and an ephedrine injection to recover the blood pressure. We knew that she had multiple prior surgical procedures without a complication and did not strongly suspect latex-induced anaphylactic shock. One of the differential diagnoses was mesenteric traction syndrome because the episode occurred while we made traction on the liver. Because her systolic blood pressure recovered to more than 80 mmHg about 20 minutes later, we restarted the procedure avoiding traction on either the liver or mesentery. However, she again went into shock within a couple of minutes. After this second episode, we suspected latex-induced anaphylactic shock, because the use of gloves was a common denominater between the episodes. We switched to latex-free gloves and removed the urinary catheter from the patient's bladder (a latex-free urinary catheter was inserted immediately after the operation). Her systolic blood pressure recovered again within about 20 minutes after a second round of treatment consisting of epinephrine, norepinephrine, chlorpheniramine, and hydrocortisone by injection. Her body looked edematous and her intraoperative chest X-ray revealed mild pulmonary edema. We decided to discontinue the donor operation. Although the recipient operation had already proceeded to laparotomy and detachment of adhesion, it was also discontinued. The only procedure that we completed in the donor was dissection of the ligament around the left lobe. At the end of the operation, the donor's serum albumin level and prothrombin time-international normalized ratio were 1.7 mg/dL and 1.59, respectively. She was admitted to the intensive care unit intubated until the following day. Although she was edematous and drowsy for a few days after she returned to the general ward, her overall condition and blood parameters gradually recovered and she was discharged 7 days after the operation. Postoperatively, the blood level of IgE-RAST (radio-allergosorbent test, BML Laboratories, Inc, Kawagoe, Japan) was elevated (10.0 ARU/mL versus upper limit of 0.34 ARU/mL) and a basophil activation test (CD203c up-regulation; BML Laboratories) showed a strong positive result (23.1% at 1:312.5 dilution; evaluation criteria were negative at <6%, positive in 15% to 20%, and strongly positive at >20%), suggesting that anaphylactic shock was induced by latex. Postoperatively, we asked the patient about her history again, focusing on a specific issue of latex allergy potential and found that she had experienced itching when she used kitchen rubber gloves within the past couple of months. The recipient also gradually recovered and is currently waiting to undergo deceased donor liver transplantation.
Discussion
Latex allergy was unusual until the late 1980s, but as more health care workers began using latex gloves to control infections in the 1990s, the incidence steadily increased thereafter. Anaphylactic reaction linked to latex sensitivity was first reported in 1989,1 and since there have been numerous case reports of latex-induced anaphylactic reactions in patients with various diseases.3–5 The number of LDLTs performed each year has also steadily risen since LDLT was first performed in 1988 in Brazil.6 According to the Japanese Society for Transplantation, more than 6000 patients received living donor liver transplants between 1989 and 2009 in Japan.7 The Organ Procurement and Transplantation Network in the United States (http://optn.transplant.hrsa.gov/) estimated 282 cases of LDLT in 2010. Although this is the first report of latex-induced anaphylactic shock occurring in an LDLT donor, it is increasingly likely that transplant surgeons will encounter donors or donor candidates with latex allergy potential.
This case highlighted the risk of latex-induced anaphylactic reaction during LDLT operation. Obstetric and gynecologic procedures are the most common settings for latex anaphylaxis during surgery,5,8–11 but our donor's past child deliveries were all uneventful. Because she reported a recent increasingly intense allergic reaction to kitchen gloves, we assume that she had been sensitized by the kitchen rubber gloves rather than past exposure to surgical procedures, and that sensitization might have increased her risk for latex allergy during the donor operation. Preoperatively, we simply asked the patient about her allergic history but we were not focusing on latex allergy. She answered that she had allergy only to pollen and mackerel and did not refer to her recent experience of itching from kitchen rubber gloves. Because of lack of information that was indicative of the latex anaphylaxis potential, we had not considered this patient to be at risk for latex allergy. Even during the operation we did not initially suspect latex allergy, although a protocol of diagnosis and management for latex allergy and latex-free equipment store were available as part of our standard operating room equipment. Turillazzi et al5 also highlighted difficulties in the initial diagnosis of latex allergy and reported a fatal case of anaphylactic latex reaction during anesthesia. Surgeons should be aware that latex allergy is rare but possible in both donor and recipient operations and should obtain detailed histories from the patients with respect to potential risk factors for latex allergy. Risk factors for latex allergy include work occupations and medical histories; health care or rubber industry workers, atopic individuals, spina bifida patients, multiple surgical procedures, and allergy to fresh fruits and nuts.12 If a donor or recipient has such a risk factor, or, especially, has an increasing allergic reaction to rubber as did our patient, a preoperative test, such as a prick test, is recommended to confirm hypersensitivity to latex. If circulatory collapse and respiratory failure occur during surgery due to latex allergy, the donor should be resuscitated adhering to the guideline for management of latex allergy13 and the operation should be stopped as soon as possible. Although the implications of high doses of epinephrine for the graft have not been fully elucidated, we have no alternative but to use standard resuscitative drugs and procedures, even for the living donor.
This case also highlighted the issue of whether it is safe to use the same donor after recovery from the latex-induced anaphylactic reaction. We usually perform latex-free operations for patients with known latex allergy. If an episode of latex-induced anaphylactic reaction accidentally occurs during surgery, and if the disease the patient is being treated for is life threatening, the operation can be continued excluding latex items or the patient can be rescheduled for a latex-free operation at a later date. However, we must be always aware that donor safety is the golden rule. We cannot rule out the possibility that another allergen caused the anaphylactic reaction in this case, and it is not possible to test for allergy to all possible allergens. Even for the recipient, it is unknown whether the liver graft derived from donor with latex allergy has no immune reactions in the post-transplant course. Therefore, we ultimately decided that this woman was unsuitable as a living donor. We knew that this donor was the only possible living donor for the recipient, because all other relatives were medically or socially unqualified as living donors. However, no risk should be tolerated for the donor even if there are fewer alternative candidate donors. We believe that transplant surgeons should be knowledgeable about the risks of latex allergy during transplant surgery and use this knowledge to make more precise judgments when assessing donor qualifications.
Fig. 1 .
Intraoperative chart of blood pressure and heart rate.
References
- 1.Morales C, Basomba A, Carreira J, Sastre A. Anaphylaxis produced by rubber glove contact. Case reports and immunological identification of the antigens involved. Clin Exp Allergy. 1989;19(4):425. doi: 10.1111/j.1365-2222.1989.tb02409.x. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa Y, Kawachi S, Shimazu M, Hoshino K, Tanabe M, Fuchimoto Y, et al. Discontinuation of living donor liver transplantation for PSC due to histological abnormalities in intraoperative donor liver biopsy. Am J Transplant. 2007;7(9):2204. doi: 10.1111/j.1600-6143.2007.01898.x. [DOI] [PubMed] [Google Scholar]
- 3.Atanaskovic-Markovic M, Gavrovic-Jankulovic M. Cirkovic Velickovic T, Vuckovic O, Ivanovski P, Nestorivic B et al. Intraoperative anaphylactic shock in a child with no history of type I hypersensitivity. Iran J Allergy Asthma Immunol. 2008;7(2):97. [PubMed] [Google Scholar]
- 4.Poterio GM. Braga Ade F, Santos RM, Gomes Ide F, Luchetta MI. Anaphylaxis during renal transplantation of live donor graft in a child with latex allergy: case report. Rev Bras Anestesiol. 2009;59(2):210. doi: 10.1590/s0034-70942009000200009. [DOI] [PubMed] [Google Scholar]
- 5.Turillazzi E, Greco P, Neri M, Pomara C, Riezzo I, Fineschi V. Anaphylactic latex reaction during anaesthesia: the silent culprit in a fatal case. Forensic Sci Int. 2008;179(1) doi: 10.1016/j.forsciint.2008.03.021. e5. [DOI] [PubMed] [Google Scholar]
- 6.Raia S, Nery JR, Mies S. Liver transplantation from live donors. Lancet. 1989;2(8661):497. doi: 10.1016/s0140-6736(89)92101-6. [DOI] [PubMed] [Google Scholar]
- 7.The Japanese Society for Transplantation. Fact Book 2009. Tokyo: The Japanese Society for Transplantation; 2009. [Google Scholar]
- 8.Ahmed DD, Sobczak SC, Yunginger JW. Occupational allergies caused by latex. Immunol Allergy Clin North Am. 2003;23(2):205. doi: 10.1016/s0889-8561(02)00079-6. [DOI] [PubMed] [Google Scholar]
- 9.Draisci G, Nucera E, Pollastrini E, Forte E, Zanfini B, Pinto R, et al. Anaphylactic reactions during cesarean section. Int J Obstet Anesth. 2007;16(1):63. doi: 10.1016/j.ijoa.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Draisci G, Zanfini BA, Nucera E, Catarci S, Sangregorio R, Schiavino D, et al. Latex sensitization: a special risk for the obstetric population? Anesthesiology. 2011;114(3):565. doi: 10.1097/ALN.0b013e318206ff50. [DOI] [PubMed] [Google Scholar]
- 11.Lieberman P. Anaphylactic reactions during surgical and medical procedures. J Allergy Clin Immunol. 2002;110(2 Suppl):S64. doi: 10.1067/mai.2002.124970. [DOI] [PubMed] [Google Scholar]
- 12.Hepner DL, Castells MC. Latex allergy: an update. Anesth Analg. 2003;96(4):1219. doi: 10.1213/01.ANE.0000050768.04953.16. [DOI] [PubMed] [Google Scholar]
- 13.Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010;126(3):477. doi: 10.1016/j.jaci.2010.06.022. [DOI] [PubMed] [Google Scholar]