The specificity of H1N1 antibody responses can be shifted to epitopes near the HA receptor–binding domain after sequential infections with viral strains that share homology in this region.
Abstract
Human antibody responses against the 2009 pandemic H1N1 (pH1N1) virus are predominantly directed against conserved epitopes in the stalk and receptor-binding domain of the hemagglutinin (HA) protein. This is in stark contrast to pH1N1 antibody responses generated in ferrets, which are focused on the variable Sa antigenic site of HA. Here, we show that most humans born between 1983 and 1996 elicited pH1N1 antibody responses that are directed against an epitope near the HA receptor–binding domain. Importantly, most individuals born before 1983 or after 1996 did not elicit pH1N1 antibodies to this HA epitope. The HAs of most seasonal H1N1 (sH1N1) viruses that circulated between 1983 and 1996 possess a critical K133 amino acid in this HA epitope, whereas this amino acid is either mutated or deleted in most sH1N1 viruses circulating before 1983 or after 1996. We sequentially infected ferrets with a 1991 sH1N1 virus and then a pH1N1 virus. Sera isolated from these animals were directed against the HA epitope involving amino acid K133. These data suggest that the specificity of pH1N1 antibody responses can be shifted to epitopes near the HA receptor–binding domain after sequential infections with sH1N1 and pH1N1 viruses that share homology in this region.
Most influenza pandemics occur when a new subtype of virus enters the human population. Once introduced into the human population, influenza viruses typically accumulate mutations in the hemagglutinin (HA) and neuraminidase (NA) glycoproteins, a process called antigenic drift. An H1N1 influenza virus strain caused a pandemic in 2009 (Smith et al., 2009) even though H1N1 viruses have circulated in humans from 1918 to 1957 and then again from 1977 to 2009. The 2009 pandemic H1N1 (pH1N1) strain is antigenically distinct from recently circulating seasonal H1N1 (sH1N1) strains and is more closely related to older sH1N1 strains (Garten et al., 2009; Manicassamy et al., 2010; Skountzou et al., 2010).
Sera isolated from influenza-infected ferrets are currently used for surveillance of antigenically drifted influenza strains (Stöhr et al., 2012). Anti-pH1N1 antibody responses elicited in ferrets are focused on the highly variable Sa antigenic site of HA (Chen et al., 2010). Conversely, the majority of monoclonal antibodies derived from humans infected or vaccinated with pH1N1 are directed against conserved regions of the HA stalk and receptor binding domain (Li et al., 2012; O’Donnell et al., 2012; Wrammert et al., 2011). Most of these monoclonal antibodies possess many somatic mutations and bind to sH1N1 viruses efficiently, which is consistent with the idea that these antibody responses were likely originally primed by sH1N1 infection and were later recalled during pH1N1 infection/vaccination (Settembre et al., 2011; Wrammert et al., 2011; Li et al., 2012; O’Donnell et al., 2012; Qiu et al., 2012). Understanding the precise events that promote the development of these cross-reactive antibody repertoires will aid in developing a universal influenza vaccine that targets conserved areas of HA.
Here, we compared the specificity of pH1N1 antibody responses elicited in different aged humans. We find that most individuals born between 1983 and 1996 elicit pH1N1 antibody responses that are dominated against an epitope near the HA receptor–binding domain. Most sH1N1 viruses that circulated between 1983 and 1996 share homology with the pH1N1 virus in this region of HA. Antibody responses dominated against this HA epitope were induced after sequential infection of ferrets with a 1991 sH1N1 virus and a pH1N1 virus. Most humans born before 1983 or after 1996 did not mount anti-pH1N1 antibody responses against this HA region. Importantly, most sH1N1 viruses that circulated before 1983 or after 1996 have an amino acid mutation or deletion in this HA epitope.
RESULTS AND DISCUSSION
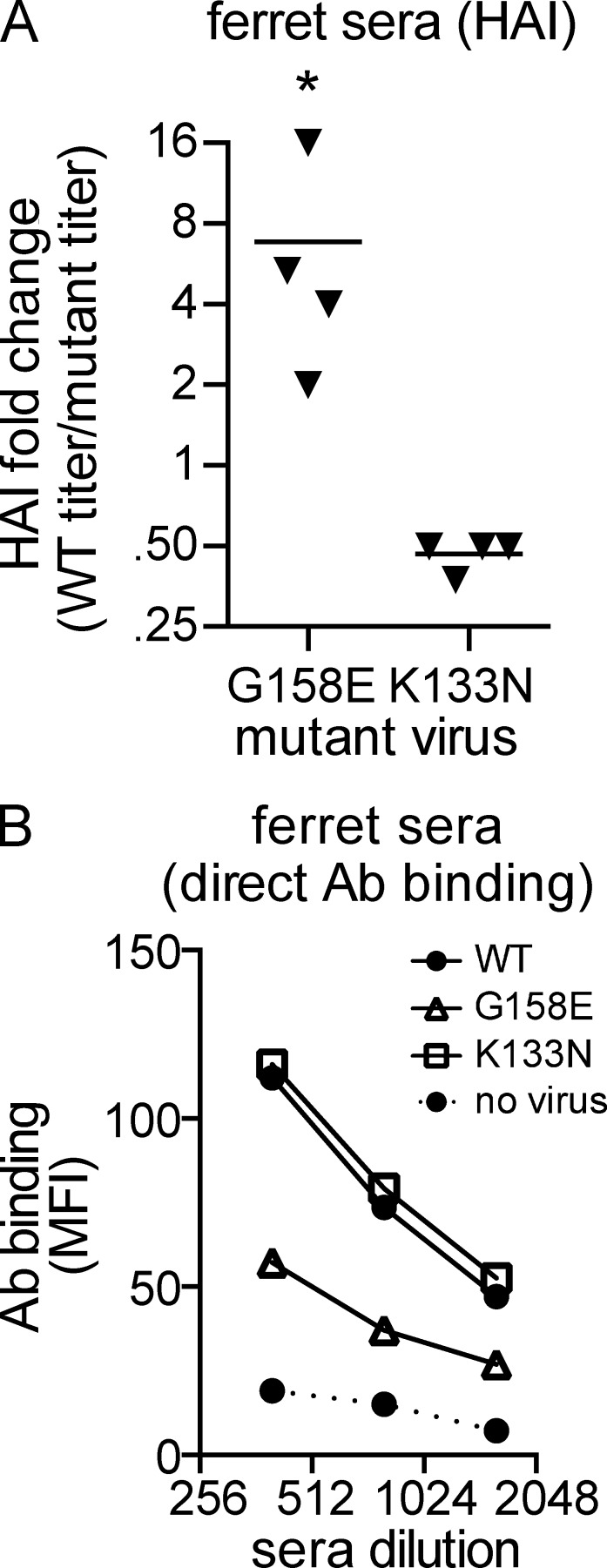
Anti-pH1N1 sera produced in previously naive ferrets are dominated against the Sa antigenic site of HA
Since entering the human population in 2009, pH1N1 viruses have remained antigenically stable, and ∼99% of pH1N1 isolates characterized by the CDC in 2012–2013 were antigenically similar to the A/California/07/2009 vaccine strain (www.cdc.gov/flu/weekly). We obtained three rare viral strains from the CDC that efficiently escape anti-pH1N1 ferret sera in hemagglutination inhibition (HAI) assays (Table S1). Each of these strains possesses a mutation at amino acid residues 158 or 159 in the Sa antigenic site of HA (Table S2). Atomistic modeling and electrostatic calculations suggest that the G158E HA mutation locally alters the electrostatic properties and shape of the Sa antigenic site (Fig. 1). Reverse-genetics experiments revealed that a single G158E HA mutation was sufficient to promote escape from sera isolated from ferrets infected with the A/California/07/2009 pH1N1 vaccine strain (Fig. 2 A; P = 0.016 using paired Student’s t test). These findings are consistent with previous studies that demonstrated that anti-pH1N1 ferret sera are dominated against an epitope involving aa 156, 157, and 158 of the Sa HA antigenic site (Chen et al., 2010).
Figure 1.
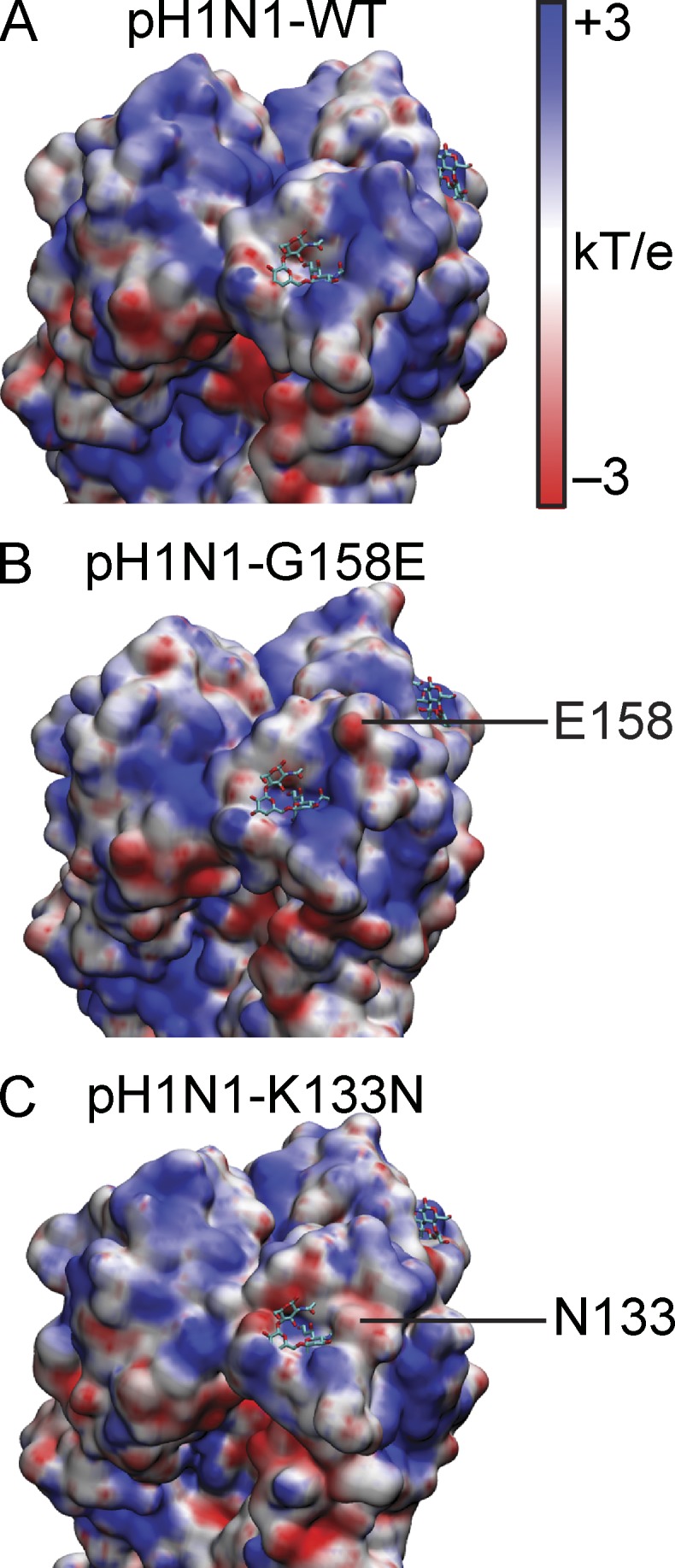
Modeling and electrostatics of pH1N1 HA mutants. The structures and electrostatic potentials of pH1N1 HAs with G158E or K133N mutants were modeled. Shown are pH1N1-WT (A) and computationally modeled pH1N1 HAs with G158E (B) or K133N (C) mutations. Sialic acid is shown as a stick structure. Surface coloring indicates electrostatic potential in units of kT/e where k is Boltzmann’s constant, T is temperature, and e is the elementary charge.
Figure 2.
pH1N1 antibody responses in previously naive ferrets are dominated against Sa antigenic site of HA. (A) HAI assays were completed using viruses possessing either wild-type A/California/07/2009 HA or A/California/07/2009 HA with G158E or K133N mutations. HAI assays were performed with sera isolated from ferrets 14 d after infection with the A/California/07/2009 pH1N1 strain. Fold change for each mutant virus (WT HAI titer/mutant HAI titer) is shown here. Each triangle represents an individual sera sample, and the mean is indicated with a line. HAI titers using the G158E mutant virus are lower compared with HAI titers using the WT virus, as determined using a paired Student’s t test on log2 transformed data (*, P = 0.016). Data are representative of three independent experiments. (B) Direct flow cytometry-based antibody (Ab) binding assays were completed using pooled anti-sera. pH1N1-infected MDCK cells were incubated with ferret anti-sera, and antibody binding was determined after addition of a FITC anti-ferret antibody. Data are representative of three independent experiments.
Unlike ferret anti-sera, most human anti-pH1N1 monoclonal antibodies are dominated against conserved regions of the HA stalk and receptor-binding domains (Wrammert et al., 2011; Li et al., 2012). HA aa 133, which is located near the receptor-binding domain, is a critical contact residue for several broadly neutralizing human monoclonal antibodies (Krause et al., 2011; Tsibane et al., 2012). Most pH1N1 strains have a lysine at HA aa 133. We completed additional HAI assays with a pH1N1 virus possessing a K133N HA mutation, which is predicted to broadly alter the electrostatic potential on the surface surrounding the receptor-binding domain (Fig. 1). Unlike pH1N1 viruses with a G158E Sa mutation, pH1N1 viruses with a K133N HA mutation were efficiently recognized by anti-pH1N1 sera produced in ferrets (Fig. 2 A). HAI titers using pH1N1 viruses with a K133N HA mutation were slightly higher compared with HAI titers using wild-type pH1N1. The K133N HA mutation decreases receptor binding avidity (unpublished data), and our previous studies demonstrated that viruses with lower receptor binding avidity can be more easily inhibited in HAI assays (Hensley et al., 2009). For this reason, we completed additional direct antibody-binding assays, which are not affected by variations in viral receptor binding avidities. These assays confirmed that anti-pH1N1 sera produced in ferrets reacts strongly to wild-type pH1N1 virus and pH1N1 virus with a K133N HA mutation, but not to pH1N1 virus with a G158E HA mutation (Fig. 2 B).
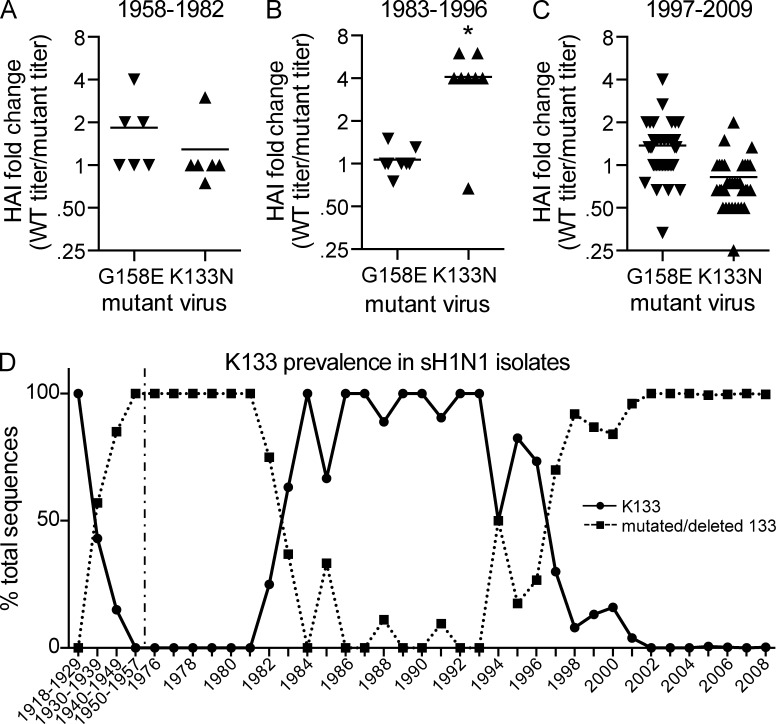
Humans of different ages mount vastly different pH1N1 antibody responses
Next, we completed HAI assays with sera isolated from pH1N1-infected humans (Fig. 3, A–C; and Table S3). Only 11 of 54 human sera samples had reduced HAI titers (at least a twofold change) to pH1N1 viruses with the G158E Sa mutation. Of these 11 Sa-specific sera samples, 8 (73%) were from individuals with no evidence of sH1N1 preexposure, as determined by HAI assays using sH1N1 strains from 1957 (A/Denver/1/1957), 1991 (A/Texas/36/1991), and 2007 (A/Brisbane/59/2007; Table S3). The three Sa-specific samples that exhibited sH1N1 cross-reactivity were from individuals born before 1971 (Table S3). Strikingly, 7 of 8 samples from individuals born between 1983 and 1996 were highly specific to the pH1N1 HA epitope involving K133 (Fig. 3 B and Table S3; Fisher’s exact test P < 0.001 comparing 1983–1996 sera to sera from other time periods). This time period is noteworthy, as the HAs of most sH1N1 strains circulating from 1983–1996 possessed a K133, whereas the HAs of most sH1N1 strains circulating before 1983 and after 1996 had a mutation or deletion at this critical amino acid (Fig. 3 D). The A/Texas/36/1991 strain possesses K133, whereas A/Denver/1/1957 and A/Brisbane/59/2007 strains have a deletion at this amino acid. Notably, eight of nine of the K133-specific sera isolated from pH1N1-infected humans had high titers against the A/Texas/36/1991 strain (Table S3). Previous studies have documented that most humans have high HAI titers against strains that circulated early in each individual’s childhood (Carter et al., 2012). Therefore, individuals born between 1983 and 1996 were likely exposed to a sH1N1 strain similar to A/Texas/36/1991. One individual born in 1979 possessed K133-specific sera (Table S3). This individual’s first H1N1 exposure likely involved a K133-possessing sH1N1, as sH1N1 did not widely circulate between 1979 and 1982 (Ferguson et al., 2003).
Figure 3.
pH1N1 antibody responses in humans born between 1983–1996 are dominated against region of HA involving K133. (A–C) HAI assays were completed using viruses possessing either wild-type A/California/07/2009 HA or A/California/07/2009 HA with G158E or K133N mutations. HAI assays were performed with sera isolated from humans 9–31 d after onset of pH1N1 symptoms. Humans were naturally infected with pH1N1 (PCR-verified). HAI titers are shown in Table S3. Fold change for each mutant virus (WT HAI titer/mutant HAI titer) is shown here. Each triangle represents an individual sera sample, and the mean is indicated with a line. Individuals are separated based on year of birth. 7 of 8 sera samples from individuals born between 1983 and 1996 had reduced titers to the K133N mutant, whereas only 2 sera samples from the other time periods (n = 46) had reduced titers to the K133N mutant (K133-specificity of sera from 1983–1996 is significantly different compared with sera from other time periods; Fisher’s exact test; *, P < 0.001). HAI data are representative of three independent experiments. (D) Timeline depicting the percentage of sH1N1 isolates possessing Lys (solid line) or a mutation/deletion (dotted line) at position 133 of HA based on sequences contained in the NCBI database. In total, 7,045 sequences resulting from unique isolates were aligned using the program MUSCLE to yield K133 prevalence on a yearly basis. Isolates from 1918–1957 were grouped due to low number of sequences from these years. sH1N1 viruses did not circulate between 1958 and 1976, and this is indicated by a dashed vertical line.
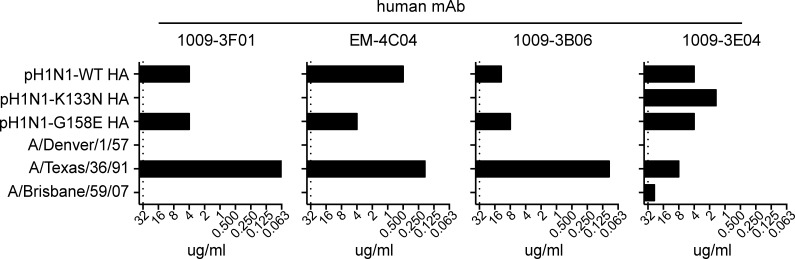
Monoclonal antibodies derived from pH1N1-infected humans bind to a sH1N1 virus possessing K133
Because our sera samples were collected from humans naturally infected with pH1N1, we were unable to obtain sera before pH1N1 infection. To determine if antibody-secreting cells specific for the K133 HA epitope were actively recruited during pH1N1 exposure, we analyzed the specificity of monoclonal antibodies derived from plasmablasts transiently expanded in the blood of human adults infected with pH1N1. We analyzed four monoclonal antibodies that were previously shown to efficiently recognize pH1N1 in HAI, ELISA, and in vitro neutralization assays (Wrammert et al., 2011).
Three of four antibodies failed to react with pH1N1 virus expressing the K133N HA mutation in HAI assays (Fig. 4). All three of the K133-specific antibodies reacted strongly with the A/Texas/36/1991 seasonal H1N1 strain, which possesses K133. Only the EM-4C04 monoclonal antibody had reduced reactivity to pH1N1 viruses expressing a G158E HA mutation in the Sa antigenic site (Fig. 4), which is consistent with previous mapping studies showing that this antibody is more strain-specific compared with other human anti-pH1N1 monoclonal antibodies (O’Donnell et al., 2012). None of the three K133-specific antibodies reacted with the A/Denver/1/1957 or A/Brisbane/59/2007 seasonal strains, which have a deletion at aa 133 of HA (Fig. 4). Based on this reactivity pattern and the observation that the immunoglobulin genes of these antibodies have many somatic mutations (Wrammert et al., 2011), it is likely that these monoclonal antibodies were derived from plasmablasts that were originally primed by sH1N1 viruses similar to A/Texas/36/1991, and then later recalled during pH1N1 infection.
Figure 4.
Human monoclonal antibodies specific for pH1N1 HA epitope involving aa 133 react strongly with a 1991 sH1N1 strain. HAI assays were completed using monoclonal antibodies derived from pH1N1-infected humans. HAI assays were completed using viruses possessing either wild-type pH1N1 HA (A/California/07/2009), pH1N1 with a G158E HA mutation, pH1N1 with a K133N HA mutation, or sH1N1 viruses from 1957 (A/Denver/1/1957), 1991 (A/Texas/36/1991), or 2007 (A/Brisbane/59/2007). Shown are minimum amounts of antibody required to inhibit agglutination of red blood cells in the HAI assay. Data are representative of three independent experiments.
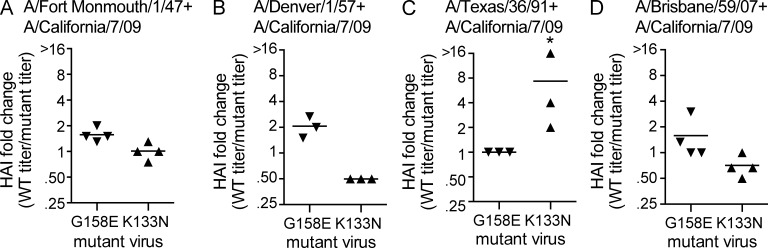
Antibodies specific for an HA epitope involving K133 can be induced in ferrets
Based on our HAI assays using sera (Fig. 3 and Table S3) and monoclonal antibodies (Fig. 4) isolated from humans, we hypothesized that K133 HA-dominated antibody responses could be induced by sequential infection with sH1N1 and pH1N1 strains that both possess K133. To address this, we preexposed ferrets with different sH1N1 strains circulating from 1947–2007, and then we infected these same ferrets with a pH1N1 strain. Remarkably, sera isolated from three different ferrets sequentially infected with the sH1N1 strain A/Texas/36/1991 (which possesses K133) and the pH1N1 strain were dominated against an HA epitope involving K133 (Fig. 5 C). Sera isolated from pH1N1-infected ferrets that were previously exposed to either A/Fort Monmouth/1/1947 (which possesses R133), A/Denver/1/1957 (which possesses a 133 deletion), or A/Brisbane/59/2007 (which possesses a 133 deletion) were not dominated against the HA epitope involving K133 (Fig. 5, A, B, and D). Differences in K133 specificity were statistically significant between the different preexposed groups (Fisher’s exact test P = 0.003 comparing HAI titers of sera isolated from A/Texas/36/1991 preexposed animals to HAI titers of sera isolated from animals preexposed to other sH1N1 viruses). Sera isolated from ferrets infected with only sH1N1 strains (and not pH1N1) did not react with pH1N1 or the pH1N1 mutant viruses.
Figure 5.
sH1N1 preexposure alters the specificity of pH1N1 antibody responses in ferrets. (A–D) HAI assays were completed using viruses possessing either wild-type A/California/07/2009 HA, or A/California/07/2009 HA with G158E or K133N mutations. Sera were isolated from ferrets sequentially infected with a sH1N1 strain, and then the A/California/07/2009 pH1N1 strain. Infections were completed 84 d apart and sera were isolated 14 d after infection with the pH1N1 virus. Fold change for each mutant virus (WT HAI titer/mutant HAI titer) is shown here. Each triangle represents an individual sera sample, and the mean is indicated with a line. Differences in K133 specificity were statistically significant between the different preexposed groups (Fisher’s exact test; *, P = 0.003 comparing HAI titers of sera isolated from A/Texas/36/1991 preexposed animals to HAI titers of sera isolated from animals preexposed with other sH1N1 viruses). Data are representative of two independent experiments.
Unlike sera obtained from ferrets infected with pH1N1 virus only (Fig. 2), most sera samples obtained from ferrets sequentially infected with sH1N1 and pH1N1 strains did not mount a dominant response to the Sa antigenic site of HA (Fig. 5). Notably, zero of three animals sequentially infected with A/Texas/36/1991 and pH1N1 virus mounted responses that were dominated against the Sa antigenic site (Fig. 5 C).
To determine if sequential influenza infections induce antibodies that are capable of reacting to conserved epitopes on antigenically distinct influenza strains, we completed additional HAI assays using two different A/Puerto Rico/8/1934 sH1N1 strains (Table S4), which were originally isolated in 1934. The HA of the A/Puerto Rico/8/1934-Mt. Sinai strain and the HA of the A/Puerto Rico/8/1934-Cambridge strain share ∼98% amino acid homology with each other, but notably, the Cambridge HA possesses K133 and the Mt. Sinai HA has a deletion at this amino acid (Caton et al., 1982). The HAs of the 1934 sH1N1 strains share poor homology to the HA of the pH1N1 strain (between 82–83% amino acid homology). Consistent with this, sera obtained from ferrets infected with only pH1N1 virus did not react to either 1934 strain (Table S4). Sera obtained from ferrets infected with only A/Denver/1/1957 reacted weakly with both 1934 strains (HAI titers 80–160), but antibody titers were not boosted greatly after subsequent infection with pH1N1 virus (HAI titers 120–160). Sera obtained from ferrets infected with A/Fort Monmouth/1/1947 or A/Brisbane/59/2007 did not react to either 1934 strain, even after a subsequent pH1N1 infection. Sera obtained from ferrets infected with only the A/Texas/36/1991 strain reacted weakly to the 1934 strain possessing K133 (HAI titer 60); however, these antibody titers were dramatically boosted after subsequent infection with pH1N1 virus (HAI titer 5120). Consistent with the hypothesis that sequential infection with A/Texas/36/1991 and pH1N1 induces an antibody response that is dominated against an HA epitope involving K133, sera from animals sequentially infected with these viruses did not react to the 1934 virus with a 133 deletion (HAI titer <40).
Collectively, these data suggest that the specificity of pH1N1 antibody responses can be shifted to conserved epitopes in individuals that are preexposed to sH1N1 strains. Previous studies have demonstrated that the Sa antigenic site of pH1N1 viruses is similar to the Sa antigenic site of some sH1N1 viruses that circulated before 1957 (Krause et al., 2010; Manicassamy et al., 2010; Wei et al., 2010; Xu et al., 2010). H1N1 viruses did not circulate in humans between 1957 and 1977, and most H1N1 strains that circulated after 1977 have an additional glycosylation site that shields the Sa antigenic site (Wei et al., 2010). The addition of this glycosylation site in more recently circulating sH1N1 strains offers an explanation of why younger individuals were more susceptible compared with their elders during the 2009 pandemic. Here, we have identified a very unique antibody profile in individuals born between 1983 and 1996. pH1N1 antibody responses in these individuals are not focused on the Sa antigenic site, but instead on an HA epitope near the receptor–binding domain involving aa 133.
As early as the 1960s, it was noted that the immune system preferentially mounts antibody responses to previously circulating influenza strains, as opposed to new antibody responses that exclusively target newer viral strains (Francis, 1960). Studies in the 1960s used elegant absorption methods to demonstrate that antibodies induced in this manner bind to epitopes that are conserved between heterologous viruses (Fazekas de St. Groth and Webster, 1966). We propose that cross-reactive antibodies are developed in this manner after infection with heterologous sH1N1 and pH1N1 viruses. Humans generally have high HAI titers against strains that circulated early in each individual’s childhood (Carter et al., 2012), indicating that most humans are infected with influenza viruses early in childhood. Most humans born between 1983 and 1996 were likely exposed to sH1N1 strains possessing K133, leading to the development of antibodies against the HA epitope involving K133. We propose that these K133-specific antibody responses were boosted upon exposure with pH1N1 virus.
In this study, we focused on antibody responses that prevent HA binding to cell surfaces (HAI antibodies). Previous studies have shown that stalk-specific antibodies are elicited in pH1N1-infected adult humans born between 1964 and 1988 (Wrammert et al., 2011; Pica et al., 2012). It is likely that stalk-specific antibodies were also elicited in sequentially infected ferrets in our study. Future studies will address if different amounts of stalk-specific antibodies are elicited in ferrets sequentially infected with different sH1N1 and pH1N1 viruses. Because a large proportion of antibodies are elicited against the K133-HA epitope in ferrets infected with A/Texas/36/1991 and pH1N1, it is reasonable to speculate that a higher overall proportion of antibodies would be elicited against the HA stalk in ferrets infected with sH1N1 and pH1N1 viruses that do not share homology at aa 133 of HA.
We simplified our studies by focusing on two amino acids. Anti-HA antibody–binding footprints involve several amino acids of HA, and there are most definitely other amino acids involved in the binding of the cross-reactive antibodies in our studies. For example, the broadly neutralizing 5J8 monoclonal antibody recognizes an epitope near the receptor-binding domain of HA involving aa 133, 137, and 222 (Krause et al., 2011). A recent crystal structure of the 1F1 broadly neutralizing monoclonal antibody with HA demonstrated that this antibody contacts many amino acids that influence binding with sialic acid, including aa 133 (Tsibane et al., 2012). Other broadly neutralizing antibodies, such as CH65, bind to the receptor-binding domain of viruses that have the K133 deletion (Whittle et al., 2011). Interestingly, these antibodies do not bind to pH1N1, and this appears to be due to the presence of K133 (Whittle et al., 2011). Strategically designed sequential vaccination approaches could elicit mixtures of broadly neutralizing antibodies with specificities such as those of 1F1 and CH65. This type of universal vaccination approach would presumably protect against a large range of antigenically distinct influenza viruses that do and do not possess K133.
Another implication of our studies is that ferret anti-sera (currently used for influenza surveillance) might not be fully representative of human population immunity. Vaccine strains for H1N1, H3N2, and influenza B viruses are all selected based on HAI assays using sera collected from ferrets recovering from a primary infection. Future studies should address if influenza viruses have evolved in response to antibodies that are elicited by sequential heterologous infections, as most (if not all) evolutionary influenza studies have only used sera isolated from ferrets recovering from primary influenza infections.
MATERIALS AND METHODS
Viruses.
A/California/07/2009, A/England/195/2009, A/Utah/42/2009, A/Utah/20/2009, A/Philippines/2810/2009, and A/South Carolina/18/2009 were gifts from N. Cox (Centers for Disease Control [CDC], Atlanta, GA). A/Brisbane/59/2007 and A/Denver/1/1957 were obtained through the National Institutes of Health (NIH) Biodefense and Emerging Infectious Research Resources Repository, National Institute of Allergy and Infectious Disease (NIAID; NR-3223 and NR-4229). A/Fort Monmouth/1/1947 and A/Puerto Rico/8/1934 viruses were obtained from the Wistar Institute Gerhard collection. A/Texas/36/1991 and A/California/07/2009 viruses with mutant HAs were created via reverse genetics. Single amino acid changes to the HA gene were made using the QuikChange site-directed mutagenesis kit (Stratagene) and confirmed by sequence analysis. All reverse-genetics viruses with A/California/07/2009 HA and NA were created using six A/Puerto Rico/8/1934 internal genes to enhance virus growth. Reverse-genetics plasmids were gifts from J. Bloom (Fred Hutchinson Cancer Center, Seattle, WA). All viruses possessing A/California/07/2009 HA and NA were propagated in MDCK-SIAT1 cells, and the supernatant was harvested through a 0.45-µm filter (Millipore). The HA genes of these viruses were sequenced to verify that mutations did not arise during propagation.
Ferret sera.
The following pooled ferret sera (6–9 animals/batch) were obtained through the NIH Biodefense and Emerging Infectious Research Resources Repository: anti-A/California/07/09 (NR-15429), anti-A/Nanchang/8008/2009 (NR-19265), and anti-Mexico/4108/2009 (NR-19264). Ferret antisera against A/Fort Monmouth/1/1947 (FR-952) were obtained from Influenza Reagent Resource (Influenza Division, WHO Collaborating Center for Surveillance, Epidemiology, and Control of Influenza, CDC, Atlanta, GA). Additional ferret anti-sera were produced at the University of Pittsburgh (Carter et al., 2013) using procedures in accordance with the NRC Guide for the Care and Use of Laboratory Animals, the Animal Welfare Act, and the CDC/NIH Biosafety in Microbiological and Biomedical Laboratories handbook. Fitch ferrets (female, 6–12 mo of age) that were seronegative for circulating H1N1, H3N2, and influenza B viruses were purchased from Marshall Farms. Ferrets were infected with 106 PFU of sH1N1 virus (A/Denver/1/1957, A/Texas/36/1991, or A/Brisbane/ 59/2007) or pH1N1 virus (A/California/07/2009) and bled 14 d later. Other ferrets were sequentially infected with a sH1N1 virus (A/Fort Monmouth/1/1947, A/Denver/1/1957, A/Texas/36/1991, or A/Brisbane/ 59/2007), and then pH1N1 virus. For these experiments, ferrets were infected with 106 PFU of sH1N1, and then infected again with 106 PFU of pH1N1 virus 84 d later. These animals were bled 14 d later, and sera were isolated after centrifugation.
Human sera.
Studies involving human adults were approved by Emory University and the University of Chicago, and studies involving pediatric samples were approved by the Institutional Review Board of the Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy. These sera were collected in 2009 for previous studies (Esposito et al., 2011; Wrammert et al., 2011), and leftover sera were used for this study. Sera were collected at Emory between 10 and 31 d after onset of influenza symptoms (Wrammert et al., 2011) and at Milan 28 d after diagnosis of pH1N1 infection (Esposito et al., 2011). Diagnosis of pH1N1 influenza infection was determined by PCR.
Human monoclonal antibodies.
Monoclonal antibodies were generated from antibody-secreting cells isolated from the peripheral blood mononuclear cells of patients infected with pH1N1 in 2009 as previously described (Wrammert et al., 2011). Antibody-secreting cells were sorted, VH and VK genes were amplified, sequenced, and cloned into IgG1 cloning vectors, and recombinant antibodies were purified from cell supernatant after co-transfecting heavy and light chain plasmids into 293A cells.
HAI assay.
As previously described (Hensley et al., 2009), HAI titrations were performed in 96-well round plates (BD). All sera samples were pretreated with receptor-destroying enzyme (Sigma-Aldrich). Sera or monoclonal antibodies were serially diluted twofold and added to 4 agglutinating doses of virus in a total volume of 100 μl. Next, 12.5 μl of a 2% (vol/vol) turkey erythrocyte solution was added. The sera, virus, and erythrocytes were gently mixed and the assay was read out after incubating for 60 min at room temperature. HAI titers were recorded as the inverse of the highest dilution that inhibited hemagglutination of turkey erythrocytes.
Flow cytometry-based sera binding assay.
MDCK cells were seeded in 6-well plates at 1.5 × 106 cells per well. The cells were infected with pH1N1 viruses the next day and 15–18 h later the infected cells were harvested. Serial dilutions of sera were added to the cells for 30 min at 4 C. Cells were washed and then anti-ferret FITC antibody (Abcam) was added for 30 min at 4°C. Levels of total HA cell surface expression was monitored by incubating cells with the anti-HA stalk monoclonal antibody, 70-1F02. Flow cytometry was performed and data are expressed as mean fluorescent intensity.
Sequencing.
RNA was extracted from virus using QiAmp viral RNA mini kit (QIAGEN). The HA gene was amplified using the One-Step RT-PCR kit (Invitrogen), and sequencing was performed at the University of Pennsylvania Sequencing Facility.
Mutant modeling and electrostatics.
The construction of mutant HA structural models and their associated surface electrostatic potential calculations are fully described in the Supplemental text. In brief, mutant structures were homology modeled based on the crystal structure of pandemic H1N1 (Xu et al., 2010), and were thoroughly equilibrated at a temperature of 300 K and pressure of 1 atm using rigorous molecular dynamics simulation in explicit KCl electrolyte using the GROMACS package (version 4.5) with the AMBER03 force field (Essman et al., 1995; Dolinsky et al., 2007; Hess et al., 2008). Continuum solvent electrostatic potential calculations at the molecular surface of each mutant were performed with the Adaptive Poisson Boltzmann Solver (version 1.3; Baker et al., 2001).
Statistical analysis.
Paired Student’s t tests were used to evaluate differences between WT and mutant viruses based on log2-transformed titer data. Fisher’s exact tests were used to compare the proportions of samples with at least a twofold lower titer to mutant virus than WT virus between specified infection groups. Data were graphed using MS Excel and GraphPad Prism software.
Online supplemental material.
Table S1 shows HAI data using pH1N1 mutant strains obtained from the CDC and Table S2 shows HA amino acid differences of these strains. Table S3 show primary HAI data that were used to derive Fig. 3 of the main manuscript. Table S4 shows HAI data using PR8 strains. Finally, there is additional information on mutant modeling in the online materials. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20130212/DC1.
Supplementary Material
Acknowledgments
S.E. Hensley is supported by the NIH (NIAID K22AI091651), the state of PA CURE funds, the Wistar Institute Cancer Center Core grant, and a University of Pennsylvania Institute for Translational Medicine and Therapeutics grant. J.B. Plotkin and D.L. Bostick are supported by the Burroughs Wellcome Fund, the David and Lucile Packard Foundation, the James S. McDonnell Foundation, the Alfred P. Sloan Foundation, and a University of Pennsylvania Institute for Translational Medicine and Therapeutics grant. D.L. Bostick is also supported by the NIH (NIH T32A1055400). J. Madara is supported by the Penn Genome Frontiers Institute. T.M. Ross is supported by the NIH (NIAID GM083602-01). D.M. Carter is supported by an Oak Ridge Visiting Scientist training program award. Computational support from the San Diego Supercomputing Center is gratefully acknowledged. We acknowledge support from Jeffrey Faust and the Wistar Institute Flow Cytometry Facility. This work used the Extreme Science and Engineering Discovery Environment (XSEDE), which is supported by National Science Foundation grant number OCI-1053575.
R. Ahmed., J. Wrammert, and P.C. Wilson have a licensing agreement with MedImmune on the influenza virus-specific human monoclonal antibodies. There are no further conflicting financial interests.
Author contributions: S.E. Hensley, P.C. Wilson, R. Ahmed, T.M. Ross, S. Esposito, N. Principi, and J. Wrammert designed and supervised experiments. Y. Li, J.L. Myers, C.B. Sullivan., J. Madara, S.L. Linderman, D.M. Carter, and J. Wrammert performed experiments. D.L. Bostick and J.B. Plotkin completed computational modeling. Q. Liu and Y. Li completed statistical analyses. S.E. Hensley and Y. Li wrote the paper with input from all authors.
Footnotes
Abbreviations used:
- HA
- hemagglutinin
- HAI
- hemagglutination inhibition
- NA
- neuraminidase
- pH1N1
- pandemic H1N1
- sH1N1
- seasonal H1N1
References
- Baker N.A., Sept D., Joseph S., Holst M.J., McCammon J.A. 2001. Electrostatics of nanosystems: application to microtubules and the ribosome. Proc. Natl. Acad. Sci. USA. 98:10037–10041 10.1073/pnas.181342398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter D.M., Lu H.R., Bloom C.E., Crevar C.J., Cherry J.L., Lipman D.J., Ross T.M. 2012. Complex patterns of human antisera reactivity to novel 2009 H1N1 and historical H1N1 influenza strains. PLoS ONE. 7:e39435 10.1371/journal.pone.0039435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter D.M., Bloom C.E., Nascimento E.J., Marques E.T., Craigo J.K., Cherry J.L., Lipman D.J., Ross T.M. 2013. Sequential seasonal H1N1 influenza virus infections protect ferrets against novel 2009 H1N1 influenza virus. J. Virol. 87:1400–1410 10.1128/JVI.02257-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caton A.J., Brownlee G.G., Yewdell J.W., Gerhard W. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell. 31:417–427 10.1016/0092-8674(82)90135-0 [DOI] [PubMed] [Google Scholar]
- Chen Z., Wang W., Zhou H., Suguitan A.L., Jr, Shambaugh C., Kim L., Zhao J., Kemble G., Jin H. 2010. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J. Virol. 84:44–51 10.1128/JVI.02106-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolinsky T.J., Czodrowski P., Li H., Nielsen J.E., Jensen J.H., Klebe G., Baker N.A. 2007. PDB2PQR: expanding and upgrading automated preparation of biomolecular structures for molecular simulations. Nucleic Acids Res. 35:W522–W525 10.1093/nar/gkm276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito S., Daleno C., Tagliabue C., Scala A., Picciolli I., Taroni F., Galeone C., Baldanti F., Principi N. 2011. Antibody response of healthy children to pandemic A/H1N1/2009 influenza virus. Virol. J. 8:563 10.1186/1743-422X-8-563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essman U., Perera L., Berkowitz M.L., Darden T., Lee H., Pedersen L.G. 1995. A smooth particle mesh Ewald method. J. Chem. Phys. 103:8577–8593 10.1063/1.470117 [DOI] [Google Scholar]
- Fazekas de St. Groth S., Webster R.G. 1966. Disquisitions of original antigenic sin. I. Evidence in man. J. Exp. Med. 124:331–345 10.1084/jem.124.3.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N.M., Galvani A.P., Bush R.M. 2003. Ecological and immunological determinants of influenza evolution. Nature. 422:428–433 10.1038/nature01509 [DOI] [PubMed] [Google Scholar]
- Francis T. 1960. On the Doctrine of Original Antigenic Sin. Proc. Am. Philos. Soc. 104:572 [Google Scholar]
- Garten R.J., Davis C.T., Russell C.A., Shu B., Lindstrom S., Balish A., Sessions W.M., Xu X., Skepner E., Deyde V., et al. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 325:197–201 10.1126/science.1176225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley S.E., Das S.R., Bailey A.L., Schmidt L.M., Hickman H.D., Jayaraman A., Viswanathan K., Raman R., Sasisekharan R., Bennink J.R., Yewdell J.W. 2009. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science. 326:734–736 10.1126/science.1178258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess B., Kutzner C., van der Spoel D., Lindahl E. 2008. GROMACS 4: Algorithms for Highly Efficient, Load-Balanced, and Scalable Molecular Simulation. J. Chem. Theory Comput. 4:435–447 10.1021/ct700301q [DOI] [PubMed] [Google Scholar]
- Krause J.C., Tumpey T.M., Huffman C.J., McGraw P.A., Pearce M.B., Tsibane T., Hai R., Basler C.F., Crowe J.E., Jr 2010. Naturally occurring human monoclonal antibodies neutralize both 1918 and 2009 pandemic influenza A (H1N1) viruses. J. Virol. 84:3127–3130 10.1128/JVI.02184-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause J.C., Tsibane T., Tumpey T.M., Huffman C.J., Basler C.F., Crowe J.E., Jr 2011. A broadly neutralizing human monoclonal antibody that recognizes a conserved, novel epitope on the globular head of the influenza H1N1 virus hemagglutinin. J. Virol. 85:10905–10908 10.1128/JVI.00700-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G.M., Chiu C., Wrammert J., McCausland M., Andrews S.F., Zheng N.Y., Lee J.H., Huang M., Qu X., Edupuganti S., et al. 2012. Pandemic H1N1 influenza vaccine induces a recall response in humans that favors broadly cross-reactive memory B cells. Proc. Natl. Acad. Sci. USA. 109:9047–9052 10.1073/pnas.1118979109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manicassamy B., Medina R.A., Hai R., Tsibane T., Stertz S., Nistal-Villán E., Palese P., Basler C.F., García-Sastre A. 2010. Protection of mice against lethal challenge with 2009 H1N1 influenza A virus by 1918-like and classical swine H1N1 based vaccines. PLoS Pathog. 6:e1000745 10.1371/journal.ppat.1000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell C.D., Vogel L., Wright A., Das S.R., Wrammert J., Li G.M., McCausland M., Zheng N.Y., Yewdell J.W., Ahmed R., Wilson P.C., Subbarao K. 2012. Antibody pressure by a human monoclonal antibody targeting the 2009 pandemic H1N1 virus hemagglutinin drives the emergence of a virus with increased virulence in mice. MBio 3(3): e00120-12 10.1128/mBio.00120-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pica N., Hai R., Krammer F., Wang T.T., Maamary J., Eggink D., Tan G.S., Krause J.C., Moran T., Stein C.R., et al. 2012. Hemagglutinin stalk antibodies elicited by the 2009 pandemic influenza virus as a mechanism for the extinction of seasonal H1N1 viruses. Proc. Natl. Acad. Sci. USA. 109:2573–2578 10.1073/pnas.1200039109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu C., Huang Y., Wang Q., Tian D., Zhang W., Hu Y., Yuan Z., Zhang X., Xu J. 2012. Boosting heterosubtypic neutralization antibodies in recipients of 2009 pandemic H1N1 influenza vaccine. Clin. Infect. Dis. 54:17–24 10.1093/cid/cir753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settembre E.C., Dormitzer P.R., Rappuoli R. 2011. Learning from the 2009 H1N1 pandemic: prospects for more broadly effective influenza vaccines. J Mol Cell Biol. 3:144–146 10.1093/jmcb/mjq046 [DOI] [PubMed] [Google Scholar]
- Skountzou I., Koutsonanos D.G., Kim J.H., Powers R., Satyabhama L., Masseoud F., Weldon W.C., Martin Mdel.P., Mittler R.S., Compans R., Jacob J. 2010. Immunity to pre-1950 H1N1 influenza viruses confers cross-protection against the pandemic swine-origin 2009 A (H1N1) influenza virus. J. Immunol. 185:1642–1649 10.4049/jimmunol.1000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G.J., Vijaykrishna D., Bahl J., Lycett S.J., Worobey M., Pybus O.G., Ma S.K., Cheung C.L., Raghwani J., Bhatt S., et al. 2009. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 459:1122–1125 10.1038/nature08182 [DOI] [PubMed] [Google Scholar]
- Stöhr K., Bucher D., Colgate T., Wood J. 2012. Influenza virus surveillance, vaccine strain selection, and manufacture. Methods Mol. Biol. 865:147–162 10.1007/978-1-61779-621-0_9 [DOI] [PubMed] [Google Scholar]
- Tsibane T., Ekiert D.C., Krause J.C., Martinez O., Crowe J.E., Jr, Wilson I.A., Basler C.F. 2012. Influenza human monoclonal antibody 1F1 interacts with three major antigenic sites and residues mediating human receptor specificity in H1N1 viruses. PLoS Pathog. 8:e1003067 10.1371/journal.ppat.1003067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei C.J., Boyington J.C., Dai K., Houser K.V., Pearce M.B., Kong W.P., Yang Z.Y., Tumpey T.M., Nabel G.J. 2010. Cross-neutralization of 1918 and 2009 influenza viruses: role of glycans in viral evolution and vaccine design. Sci. Transl. Med. 2:ra21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle J.R., Zhang R., Khurana S., King L.R., Manischewitz J., Golding H., Dormitzer P.R., Haynes B.F., Walter E.B., Moody M.A., et al. 2011. Broadly neutralizing human antibody that recognizes the receptor-binding pocket of influenza virus hemagglutinin. Proc. Natl. Acad. Sci. USA. 108:14216–14221 10.1073/pnas.1111497108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrammert J., Koutsonanos D., Li G.M., Edupuganti S., Sui J., Morrissey M., McCausland M., Skountzou I., Hornig M., Lipkin W.I., et al. 2011. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 208:181–193 10.1084/jem.20101352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Ekiert D.C., Krause J.C., Hai R., Crowe J.E., Jr, Wilson I.A. 2010. Structural basis of preexisting immunity to the 2009 H1N1 pandemic influenza virus. Science. 328:357–360 10.1126/science.1186430 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.