Abstract
Objectives
The Saudi Project for Assessment of Coronary Events (SPACE) registry is the first in Saudi Arabia to study the clinical features, management, and in-hospital outcomes of acute coronary syndrome (ACS) patients.
Methods
We conducted a prospective registry study in 17 hospitals in Saudi Arabia between December 2005 and December 2007. ACS patients included those with ST-elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction and unstable angina; both were reported collectively as NSTEACS (non-ST elevation acute coronary syndrome).
Results
5055 patients were enrolled with mean age ± SD of 58 ± 12.9 years; 77.4% men, 82.4% Saudi nationals; 41.5% had STEMI, and 5.1% arrived at the hospital by ambulance. History of diabetes mellitus was present in 58.1%, hypertension in 55.3%, hyperlipidemia in 41.1%, and 32.8% were current smokers; all these were more common in NSTEACS patients, except for smoking (all P < 0.0001). In-hospital medications were: aspirin (97.7%), clopidogrel (83.7%), beta-blockers (81.6%), angiotensin converting enzyme inhibitors/angiotensin receptor blockers (75.1%), and statins (93.3%). Median time from symptom onset to hospital arrival for STEMI patients was 150 min (IQR: 223), 17.5% had primary percutaneous coronary intervention (PCI), 69.1% had thrombolytic therapy, and 14.8% received it at less than 30 min of hospital arrival. In-hospital outcomes included recurrent myocardial infarction (1.5%), recurrent ischemia (12.6%), cardiogenic shock (4.3%), stroke (0.9%), major bleeding (1.3%). In-hospital mortality was 3.0%.
Conclusion
ACS patients in Saudi Arabia present at a younger age, have much higher prevalence of diabetes mellitus, less access to ambulance use, delayed treatment by thrombolytic therapy, and less primary PCI compared with patients in the developed countries. This is the first national ACS registry in our country and it demonstrated knowledge-care gaps that require further improvements.
Keywords: Acute coronary syndromes, Acute myocardial infarction, Unstable angina, Registry, Saudi Arabia, Middle East
1. Introduction
Ischemic heart disease represents a global health care burden, and is expected to increase by more than 120% in developing countries by the year 2020 (Lopez et al., 2006; Yusuf et al., 2001a; Reddy, 2004; Yusuf et al., 2001b). This is related to the high prevalence of cardiovascular risk factors, such as diabetes mellitus (DM), hypertension (HTN), smoking, and hyperlipidemia; which likely resulted from significant changes in the lifestyle behaviors in the last few decades; such as reduced exercise and poor dietary habits. In addition, a knowledge-care gap has been shown by several acute coronary syndrome (ACS) registries, but scarce data are available in the Arabian populations of the Middle Eastern region (Zubaid et al., 2009). The Saudi Project for Assessment of Coronary Events (SPACE) registry was initiated to study the clinical features, management, and in-hospital outcomes of ACS patients in the Kingdom of Saudi Arabia in comparison to other worldwide ACS populations, in addition to potentially improve the quality of care.
2. Methods
The SPACE study is a prospective registry and a quality improvement initiative of all consecutive ACS patients that were admitted to the participating hospitals. Ethics committees at each hospital approved the study. The diagnosis of the different types of ACS was based on the definitions of the American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes (Cannon et al., 2001). Serum cardiac biomarkers used to assist in the diagnosis of myocardial injury were measured locally at each hospital’s laboratory using its own assays and reference ranges.
2.1. Study design and population
The study included hospitalized patients with ST-segment elevation myocardial infarction (STEMI), non ST-segment elevation myocardial infarction (NSTEMI), and unstable angina (UA). The NSTEMI and UA patient groups were combined in this report as NSTEACS (non-ST elevation acute coronary syndrome). The study extended from December 2005 until December 2007. Patients had to be 18 years of age or older and there were no exclusion criteria. The details of the pilot study design were outlined previously (AlHabib et al., 2009).
2.2. Study organization
A Case Report Form (CRF) for each patient with suspected ACS was filled out upon hospital admission by assigned physicians working in each hospital using standard definitions, and completed throughout the patient’s hospital stay. All CRFs were verified by a cardiologist then sent to the principal coordinating center, where the forms were further checked for incomplete data and mistakes before submission for final analysis. To avoid double-counting patients, each patient’s national identification number was used. Thus, only the first ACS admission was included for each patient. Patients who presented directly to the emergency department (ED) were labeled as “own”, while those who were transferred from a non-registry hospital were labeled as “referral”. An independent clinical research organization (Dubai Pharmaceutical Co., Dubai, UAE) was contracted to randomly audit all data collected from 20% of the hospitals in phase-I. Data accuracy was found to be more than 99%.
2.3. Case report form data variables
Data collected included the following variables: patient’s demographics, past medical history, provisional diagnosis on admission and final discharge diagnosis, ECG findings, laboratory investigations, medical therapy, use of cardiac procedures and interventions, in-hospital outcomes, and mortality. The consistency of data collection was maintained using data collection standards, field definitions, and explanations at each participating site. The following definitions were used; body mass index (BMI): weight in kilograms divided by the square meter of the height, DM: self-reported or being on oral hypoglycemic agents and/or insulin, HTN: self-reported, on anti-hypertensive therapy, history of systolic blood pressure more than 140 mmHg or diastolic blood pressure more than 90 mmHg, current smoking: cigarette, cigar, pipe, or shisha smoking during the last 1 year of the index admission, hyperlipidemia: self-reported or being on treatment for hyperlipidemia, coronary artery disease (CAD): history of angina or myocardial infarction (MI), family history of premature CAD: history of angina, MI, or sudden cardiac death in first-degree relatives at age less than 55 years in men and less than 65 years in women, recurrent MI: two or more out of three criteria: new-onset chest pain or discomfort, new elevation in cardiac enzymes, and new ECG changes consistent with ischemia or infarction, recurrent ischemia: new-onset chest pain or discomfort with or without new ST-segment depression and/or T-wave inversion on ECG but without elevation in cardiac enzymes, congestive heart failure: shortness of breath on exertion and/or at rest, paroxysmal nocturnal dyspnea, and/or orthopnea associated with clinical signs of pulmonary and/or peripheral edema requiring treatment with diuretic therapy, cardiogenic shock: persistent hypotension (systolic blood pressure of less than 90 mmHg) unresponsive to fluid administration and requirement for intravenous inotropic therapy or insertion of intra-aortic balloon pump, stroke: clinical evidence of hemiparesis, hemiplegia, or impaired speech with or without brain CT-scan or MRI confirmation, major bleeding: a drop in hemoglobin of greater than 5 g/dl (0.5 g/l) or bleeding causing hemodynamic instability or requiring blood transfusion.
2.4. Statistical analysis
Data were summarized as means ± SD if they were normally distributed; otherwise, they were summarized as the median and interquartile range (IQR). Differences between groups were assessed using chi square or Fisher’s exact test for categorical variables, student t-test for continuous variables for normally distributed variables, and the Mann–Whitney U test for skewed variables. All analyses were considered significant at P < 0.05. The analysis was performed using SPSS software, version 17. We excluded “referral” cases from other non-registry hospitals in the analysis of “therapy-related timelines” in STEMI and new or presumed new left bundle branch block (LBBB) patients who underwent TT or primary PCI because of insufficient and/or inaccurate data, and also those who presented to the hospital at more than 12 h of symptom onset. We also excluded “referral” cases in the analysis of the ambulance use to get an accurate reporting of mode of transportation of ACS patients from the community to the hospitals.
3. Results
3.1. Study population characteristics
Over a 24-month period, 5055 ACS patients were enrolled from 17 hospitals in the Kingdom of Saudi Arabia. One third of these hospitals was non-tertiary care hospitals and had no cardiac catheterization or cardiac surgery facilities.
There were 2096 (41.5%) STEMI/new LBBB, and 2959 (58.5%) NSTEACS patients. The NSTEACS patients included 1840 (62.2%) NSTEMI and 1119 (37.8%) UA patients. Table 1 shows the baseline characteristics, CAD risk factors, clinical features upon presentation, and key investigations for the overall study population and its ACS sub-types. The mean age ± SD of the overall population was 58 ± 12.9 years and over three quarters were men. The prevalence of CAD risk factors was high; three-fifths had DM, over half had HTN, one-third were current smokers, and two-fifths had hyperlipidemia. Median BMI ± SD was 27.6 ± 6.1 kg/m2. Only 5.1% of “own” patients arrived at the hospital in an ambulance (overall rate of own and referral was 20%), one-fifth had clinical evidence of congestive heart failure upon presentation, over three-fifths had positive serum troponin, and nearly two-thirds had coronary angiography. Compared with STEMI patients, those with NSTEACS were older and more likely to be Saudis, have a history of PCI, coronary artery bypass graft (CABG) surgery, DM, HTN, hyperlipidemia, stroke, and were more likely to present with ischemic chest pain and to undergo coronary angiogram during hospitalization (P < 0.0001 for all comparisons). However, STEMI patients were more likely to be men, current smokers, to have hypotension (systolic blood pressure ⩽ 90 mmHg), and positive serum troponin upon clinical presentation (P < 0.0001 for all comparisons).
Table 1.
Patients’ baseline characteristics and key investigations.
| Variables | Overall n = 5055 n (%) | STEMI/new LBBB n = 2096 (41.5%) n (%) | NSTEACS n = 2959 (58.5%) n (%) | P-value |
|---|---|---|---|---|
| Mean age (SD), years | 58 (12.9) | 55.4 (13.1) | 58.6 (12.9) | <0.0001 |
| Male sex, n (%) | 3914 (77.4) | 1767 (84.3) | 2147 (72.4) | <0.0001 |
| Saudi nationality, n (%) | 4164 (82.4) | 1583 (75.5) | 2581 (87.3) | <0.0001 |
| BMI, median (IQR) | 27.6 (6.1) | 27.4 (5.8) | 28.1 (6.5) | <0.001 |
| Diabetes mellitus, n (%) | 2937 (58.1) | 1092 (52.1) | 1845 (62.3) | <0.0001 |
| Hypertension, n (%) | 2783 (55.3) | 855 (40.9) | 1928 (65.5) | <0.0001 |
| Current smoking, n (%) | 1638 (32.4) | 903 (43.1) | 734 (24.8) | <0.0001 |
| Hyperlipidemia, n (%) | 2084 (41.4) | 559 (26.7) | 1525 (51.9) | <0.0001 |
| History of CAD, n (%) | 2145 (42.4) | 469 (22.4) | 1676 (56.6) | <0.0001 |
| History of PCI, n (%) | 698 (13.8) | 121 (5.7) | 577 (19.4) | <0.0001 |
| History of CABG, n (%) | 295 (5.8) | 31 (1.4) | 264 (8.9) | <0.0001 |
| History of CVA/TIA, n (%) | 309 (6.1) | 90 (4.3) | 219 (7.4) | <0.0001 |
| Family history of premature CAD∗ | 719 (15.4) | 281 (14.3) | 431 (16.2) | 0.078 |
| Killip class > 1, n (%) | 940 (20.4) | 344 (19.1) | 596 (21.1) | 0.02 |
| SBP < 90 mmHg, n (%) | 148 (3.2) | 89 (4.9) | 59 (2.1) | <0.0001 |
| HR > 100 beats per minute, n (%) | 678 (14.8) | 262 (14.5) | 416 (15) | 0.85 |
| Ischemic chest pain, n (%) | 3057 (87.6) | 1730 (84.5) | 1327 (92.2) | <0.0001 |
| Ambulance use⁎⁎, n (%) | 186 (5.1) | 102 (8.3) | 84 (3.5) | 0.17 |
| Positive serum troponin⁎⁎⁎, n (%) | 3148 (62.5) | 1424 (68.3) | 1724 (58.2) | <0.0001 |
| Coronary angiogram, n (%) | 3400 (67.2) | 1327 (63.4) | 2073 (69.9) | <0.0001 |
NSTEACS = non-ST elevation acute coronary syndrome; STEMI = ST-elevation myocardial infarction; LBBB: left bundle branch block; CAD = coronary artery disease; PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft; CVA/TIA = cerebrovascular accident/transient ischemic attack; SBP = systolic blood pressure; HR = heart rate. ∗Family history of premature CAD was unknown in 7% of the overall study cohort.
Denominator is “own” patients only. The overall ambulance use (own and referral) was 20%.
Serum troponin was not done or unavailable in 17.8% of the overall study cohort.
3.2. STEMI presentation and management
Fig. 1 shows the flow sheet of the acute revascularization treatments for STEMI/ new LBBB patients. Of 1232 STEMI/new LBBB “own” patients, 905 (73.5%) presented at less than 12 h of symptom onset. Only 102 (8.3%) patients arrived at the hospital in an ambulance, and the median time from symptom onset to hospital arrival was 150 min (IQR: 223). 625 (69.1%) patients were treated with thrombolytic therapy (TT), 93 (14.8%) received TT at less than 30 min of hospital arrival, and the median door-to-needle time (DNT) was 52 min (IQR 55). The most commonly used TT was streptokinase (46%), followed by retaplase (32.2%). 158 (17.5%) patients had primary PCI. 114 (12.6%) patients did not receive TT or primary PCI, and did not have a contraindication to either strategy, i.e. reperfusion shortfall.
Figure 1.
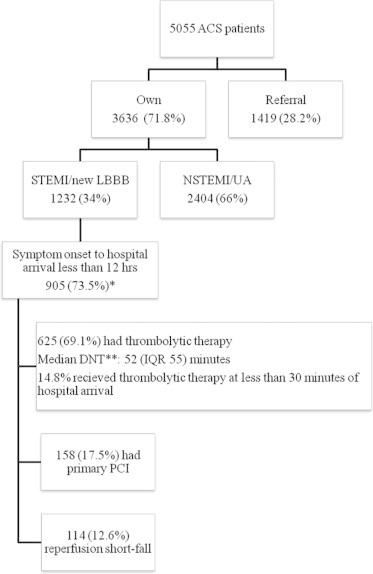
Acute revascularization treatments for SPACE-own STEMI/ new LBBB patients who presented to the hospital at less than 12 h from symptom onset. ∗Eight patients had missing data about revascularization therapies. ∗∗DNT: door-to-needle time.
3.3. In-hospital medications, procedures, and outcomes
Table 2 shows the high use of in-hospital evidence-based medications. Most of the patients received aspirin and statins, over four-fifths received clopidogrel and beta-blockers, and three-quarters received angiotensin converting enzyme inhibitors and/or angiotensin receptor blockers (ACE-I/ARBs). Over one-third received glycoprotein IIb/IIIa inhibitors (GP IIb/IIIa-I), over one-third had PCI, and 8.4% had CABG surgery. The NSTEACS patients were more likely to receive clopidogrel, beta-blockers, statins, GP IIb/IIIa-I, and undergo CABG surgery, while STEMI patients were more likely to receive aspirin, anticoagulants (unfractionated or low molecular weight heparin), and undergo PCI (P < 0.05 for all comparisons).
Table 2.
In-hospital treatments of the overall, STEMI/LBBB, and NSTEACS patients.
| Variables | Overall n = 5055 n (%) | STEM I/new LBBB n = 2096 (41.5%) n (%) | NSTEACS n = 2959 (58.5%) n (%) | P-value |
|---|---|---|---|---|
| Aspirin | 4932 (97.7) | 2057 (98.4) | 2875 (97.2) | 0.001 |
| Clopidogrel | 4227 (83.7) | 1676 (80.1) | 2551 (86.3) | <0.0001 |
| Beta-blocker | 4118 (81.6) | 1625 (77.7) | 2493 (84.1) | <0.0001 |
| ACE inhibitors/ARB | 3801 (75.1) | 1600 (76.4) | 2201 (74.3) | <0.10 |
| Statins | 4707 (93.3) | 1932 (92.4) | 2775 (93.9) | 0.03 |
| Anticoagulants | 4178 (86.2) | 1687 (85.2) | 2491 (86.9) | 0.04 |
| GPIIb/IIIa-I | 1746 (34.5) | 778 (37.1) | 986 (33.3) | 0.001 |
| PCI | 1775 (35.3) | 888 (42.6) | 887 (30.0) | <0.0001 |
| CABG | 424 (8.4) | 105 (5.0) | 319 (10.8) | <0.0001 |
NSTEACS = non-ST elevation acute coronary syndrome; STEMI = ST-elevation myocardial infarction; LBBB: left bundle branch block; PCI = percutanous coronary intervention; CABG = coronary artery bypass graft. ACE-I/ARB = angiotensin converting enzyme inhibitor and/or angiotensin receptor blocker; GP IIb/IIIa-I = Glycoprotein IIb/IIIa Inhibitors.
Table 3 shows the in-hospital mortality and outcomes. The overall in-hospital mortality was low (154 patients, 3.0%). The most frequent complications were recurrent ischemia (638 patients, 12.6%) and congestive heart failure (519 patients, 10.2%), whereas rates of stroke (48 patients, 0.9%) and major bleeding (68 patients, 1.3%) were very low. STEMI patients had higher in-hospital mortality and cardiovascular complications (P < 0.05 for all comparisons) but similar major bleeding rates compared with NSTEACS patients. There was no difference in outcomes between “own” and “referral” patients (data not shown).
Table 3.
In-hospital outcomes of the overall, STEMI/LBBB, and NSTEACS patients.
| Variables | Overall n = 5055 n (%) | STEM I/new LBBB n = 2096 (41.5%) n (%) | NSTEACS n = 2959 (58.5%) n (%) | P-value |
|---|---|---|---|---|
| Death | 154 (3.0) | 94 (4.5) | 60 (2.0) | <0.0001 |
| Recurrent myocardial infarction | 77 (1.5) | 49 (2.3) | 28 (0.9) | <0.0001 |
| Recurrent ischemia | 638 (12.6) | 317 (15.1) | 321 (10.8) | <0.0001 |
| Congestive heart failure | 519 (10.2) | 239 (11.4) | 280 (9.4) | 0.02 |
| Cardiogenic shock | 220 (4.3) | 156 (7.4) | 64 (2.1) | <0.0001 |
| Stroke | 48 (0.9) | 30 (1.4) | 18 (0.6) | <0.0001 |
| Major bleeding | 68 (1.3) | 27 (1.2) | 41 (1.3) | NS |
NSTEACS = non-ST elevation acute coronary syndrome; STEMI = ST-elevation myocardial infarction; LBBB: left bundle branch block; NS: non-significant.
4. Discussion
SPACE is the first registry for ACS patients in the Kingdom of Saudi Arabia. It provides a good representation of the clinical management of ACS patients, since several hospitals (secondary and tertiary) from all geographic regions of Saudi Arabia and most health care providers were involved.
Our study showed that ACS patients in Saudi Arabia have several unique features compared with their counterparts in other populations. Nearly two-fifths of our patients had STEMI compared with one-third in other ACS populations reported worldwide (Goodman et al., 2009; Yan et al., 2007; Mehta, 2006; Rosengren et al., 2006; Steg et al., 2002). This is probably due to the relatively young average age of ACS presentation (58 years), which is almost a decade younger than those of developed countries. However, the rate of STEMI is very similar to that of ACS patients from other Arabian Gulf countries and Malaysia (Zubaid et al., 2009; Cannon et al., 2001; Goodman et al., 2009; Yan et al., 2007; Mehta et al., 2006; Rosengren et al., 2006; Steg et al., 2002; Chin, 2008), but less than the 60.6% rate reported in India (Xavier et al., 2008). This is likely because of the overall younger age of the population in developing countries (The International Bank for Reconstruction and Development/The World Bank: World Development Report 2007), in addition to the extremely high prevalence of uncontrolled CAD risk factors in the general population (Al-Elq, 2009; Eledrisi et al., 2007), and particularly supported by the staggeringly high prevalence of DM, involving 58% of our patients. To our knowledge, this is the highest-ever reported rate of DM in an ACS population, which is double – and sometimes triple – the DM rate reported in other registries (Zubaid et al., 2009; Goodman et al., 2009; Yan et al., 2007; Mehta et al., 2006; Rosengren et al., 2006; Steg et al., 2002; Chin et al., 2008; Xavier et al., 2008). The rate of DM was 40% in ACS patients from other Arabian Gulf countries (Zubaid et al., 2009), which is lower than in our study; this may be because of the higher ratio of “expatriates to nationals” living in some of these countries relative to those in Saudi Arabia, who are usually younger and otherwise apparently healthy manual workers. Plausible explanations for this high rate of DM include lack of regular exercise and adopting the “western” diet (Yusuf et al., 2004). These changes in the Arabian culture of Saudi Arabia are probably the result of oil wealth-induced “obesogenic urbanization” that has occurred at a particularly rapid pace over only few generations (Guy et al., 2009).
Our STEMI patients took an average of 150 min before presenting to the ED compared with 140–170 min in developed countries (Steg et al., 2002; Hasdai et al., 2002; Mandelzweig et al., 2006). The infrequent use of ambulance services (5.1% in “own” patients) is one of the major reasons for delayed presentations. Other factors include the underestimation of the importance of symptoms, traffic congestion in major cities, and the absence of a universal health care system provider. Moreover, only 14.8% of our STEMI patients received TT within the standard 30 min, likely because they were awaiting approval of administration of care by the cardiology service, transfer of patients to intensive care units to receive care, and lack of the immediate availability of such care in the ED of many hospitals. Primary PCI was done only in 17.5% of patients, a rate much lower than in developed countries (Goodman et al., 2009). In addition, the “reperfusion shortfall” rate was also high (12.6%) but less than the 33% reported in international registries, and similar to other Arabian Gulf countries (9.3%) (Zubaid et al., 2009; Steg et al., 2002; Al-Mallah et al., 2010).
Similar to recent trends reported by other ACS registries (Goodman et al., 2009; Amsterdam et al., 2009; Fox et al., 2007) our study showed high use of guidelines-recommended medications and invasive procedures. The high rates of coronary angiography, PCI, and GP IIb/IIIa-I are similar to those in developed countries, but more than double the rates in many other Middle Eastern and Asian countries (Goodman et al., 2009; Yan et al., 2007; Mehta et al., 2006; Rosengren et al., 2006; Steg et al., 2002; Chin et al., 2008; Xavier et al., 2008; Amsterdam et al., 2009; Fox et al., 2007). These findings reflect the wide availability of tertiary care hospitals in Saudi Arabia that managed to establish high-caliber technical and human resources in the past few decades. However, in our study, it remains to be shown whether coronary revascularization was done for those ACS patients with high-risk coronary artery disease (Cohen et al., 2009).
The overall low in-hospital mortality of 3% is similar to contemporary data from developed countries and some Arabian Gulf countries, but lower than those reported in Yemen and poor communities in India (Goodman et al., 2009; Yan et al., 2007; Mehta et al., 2006; Rosengren et al., 2006; Steg et al., 2002; Chin et al., 2008; Xavier et al., 2008; Amsterdam et al., 2009). Low-socioeconomic strata correlate with poor access to health care and high mortality (Xavier et al., 2008; Salomaa et al., 2001; Alter et al., 1999). Improved overall socioeconomic strata and high use of guidelines-based therapies in addition to the relatively young age of ACS presentation are probably the main reasons for the low mortality in our study. STEMI patients had higher in-hospital complications (except for major bleeding) than those with NSTEACS. This is similar to other ACS registries (Zubaid et al., 2009; Xavier et al., 2008) and is most likely related to the longer times from symptom onset to hospital arrival, and below-standard DNT.
Several limitations exist in our study. Firstly, as with most other registries, hospital enrollment was voluntary; thus, the study results may not be representative of clinical practice in all hospitals in the country. In addition, hospitals that participated in the registry might be more enthusiastic about adherence to guidelines and quality improvement initiatives. However, the wide geographic distribution of several hospitals from different health care sectors in our study provides a reasonable overall representation of ACS care. Secondly, there is an inherent selection bias because of the observational nature of the study design. Thirdly, the mortality rate might have been underestimated because of missing major adverse events, particularly ACS-related mortalities that happened prior to admission to the cardiology service. We tried to mitigate this issue by requiring all hospitals to enroll consecutive patients. Fourthly, absence of accurate acute reperfusion treatments data for STEMI patients in the “referral” hospitals might have resulted in underestimation of the rate of use of such therapies. Fifthly, serum troponin was not done routinely in all our patients, but the treating physicians believed that the ACS diagnosis was correct based on the clinical presentation, ECG changes, and elevated serum CK-MB. Lastly, long-term outcomes were unavailable.
In conclusion, SPACE is the first ACS registry in Kingdom of Saudi Arabia. It showed that our ACS patients present at a relatively young age and have extremely high rates of DM. STEMI- “own” patients rarely arrived to the hospital by an ambulance, and only a few received either thrombolytic therapy or primary PCI within the recommended time-line. Guidelines-based medications and coronary revascularization rates were high, and in-hospital outcomes were low.
Financial disclosure
The SPACE registry was financially sponsored by sanofi-aventis, which had no role in data extraction or analyses, the writing of the manuscript, or the decision to submit the manuscript for publication. The College of Medicine Research Center at King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia, provided ethical approval and partial funding. None of the authors has any conflict of interest to report.
Case reports data collection
Kazi Nur Asfina, Ali Al-Shahrani, Nawaf Al-Majed, Rayan Al-Hazmi, Osama Al-Mogbel, Waleed Al-Harbi, Aws Al-Herbish, Ayman Al-Saleh, Eman Shisha, Adel Maria, Syed Asghar Hussain, Huda Abdullah Al-Mefarih, Ola Abdelmajeed, Asif Malik, Hassan Khalaf, Khalid Koumi, Hamad Fayez AlHabib, Ambreen Gul, Yahia Al Hossni, Shaima Al-Omani, Hind Kamar, Attiea Saleh, Hesham Hassoun, Mohamed Maghrabi, Ali Mohamed Elkeliei, Raed Salim Abu Tuaima, Sohil Elfar, Sharif El-Bardisy, Sajid Naeem Choudary, Ali Yousef, Mohamed Atteiah, Abdulaziz Sabry, Masood Ghori, Najeeb Ullah Bugti, Riffat Ahmad Bukhari, Yousif Noor Sahib, Mahmoud Hazaimeh, Mohamed Munir Baig, Hassan Mohamed Darwish, Ahmad Aftab, Adel Mahmoud Hasanin, Ayman Hassan Elshiekh, Hafez Mohammed Omer, Mohammed Salih Aziz, Ali khames, Mohammad raja, Murad alswaiti, Ahmad sababha.
Acknowledgments
The SPACE registry was managed under the auspices of the Saudi Heart Association. We thank Zenaida Ramoso for secretarial assistance. Dr. Khalid F. AlHabib (principal investigator) had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Al-Elq AH. Current practice in the management of patients with type 2 diabetes mellitus in Saudi Arabia. Saudi Med. J. 2009;30:1551–1556. [PubMed] [Google Scholar]
- AlHabib K.F., Hersi A., AlFaleh H. The Saudi project for assessment of coronary events (SPACE) registry: design and results of a phase I pilot study. Can. J. Cardiol. 2009;25:e255–e258. doi: 10.1016/s0828-282x(09)70513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mallah M.H., Alsheikh-Ali A.A., Almahmeed W. Missed opportunities in the management of ST-segment elevation myocardial infarction in the Arab Middle East: patient and physician impediments. Clin. Cardiol. 2010;33(9):565–571. doi: 10.1002/clc.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alter D.A., Naylor C.D., Austin P., Tu J.V. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N. Engl. J. Med. 1999;341:1359–1367. doi: 10.1056/NEJM199910283411806. [DOI] [PubMed] [Google Scholar]
- Amsterdam E.A., Peterson E.D., Ou F.S. Comparative trends in guidelines adherence among patients with non-ST-segment elevation acute coronary syndromes treated with invasive versus conservative management strategies: results from the CRUSADE quality improvement initiative. Am. Heart J. 2009;158:748–754. doi: 10.1016/j.ahj.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Cannon C.P., Battler A., Brindis R.G. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee) J. Am. Coll. Cardiol. 2001;38:2114–2130. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- Chin S.P., Jeyaindran S., Azhari R. Acute coronary syndrome (ACS) registry – leading the charge for national cardiovascular disease (NCVD) database. Med. J. Malaysia. 2008;63(Suppl. C):29–36. [PubMed] [Google Scholar]
- Cohen M.G., Filby S.J., Roe M.T. The paradoxical use of cardiac catheterization in patients with non-ST-elevation acute coronary syndromes: lessons from the Can Rapid Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines (CRUSADE) Quality Improvement Initiative. Am. Heart J. 2009;158:263–270. doi: 10.1016/j.ahj.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Eledrisi M. Quality of diabetes care in Saudi Arabia. Diabetes Res. Clin. Pract. 2007;78:145–146. doi: 10.1016/j.diabres.2007.02.017. [DOI] [PubMed] [Google Scholar]
- Fox K.A., Steg P.G., Eagle K.A. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- Goodman S.G., Huang W., Yan A.T. The expanded global registry of acute coronary events: baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am. Heart J. 2009;158:193–201. doi: 10.1016/j.ahj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Guy G.W., Nunn A.V.W., Thomas L.E., Bell J.D. Obesity, diabetes and longevity in the Gulf: Is there a Gulf Metabolic Syndrome? IJDM. 2009;1:43–54. [Google Scholar]
- Hasdai D., Behar S., Wallentin L. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur. Heart J. 2002;23:1190–1201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- Lopez A.D., Mathers C.D., Ezzati M. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- Mandelzweig L., Battler A., Boyko V. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur. Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- Mehta R.H., Roe M.T., Chen A.Y. Recent trends in the care of patients with non-ST segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch. Intern. Med. 2006;166:2027–2034. doi: 10.1001/archinte.166.18.2027. [DOI] [PubMed] [Google Scholar]
- Reddy K.S. Cardiovascular disease in non-Western countries. N. Engl. J. Med. 2004;350:2438–2440. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- Rosengren A., Wallentin L., Simoons M. Age, clinical presentation, and outcome of acute coronary syndromes in the Euro heart acute coronary syndrome survey. Eur. Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- Salomaa V., Miettinen H., Niemela M. Relation of socioeconomic position to the case fatality, prognosis and treatment of myocardial infarction events; the FINMONICA MI Register Study. J. Epidemiol. Commun. Health. 2001;55:475–482. doi: 10.1136/jech.55.7.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steg P.G., Goldberg R.J., Gore J.M. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am. J. Cardiol. 2002;90:358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- The International Bank for Reconstruction and Development/The World Bank: World Development Report; 2007, pp. 288–289.
- Xavier D., Pais P., Devereaux P.J. CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- Yan A.T., Yan R.T., Tan M. Management patterns in relation to risk stratification among patients with non-ST elevation acute coronary syndromes. Arch. Intern. Med. 2007;167:1009–1016. doi: 10.1001/archinte.167.10.1009. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Reddy S., Ounpuu S. Global burden of cardiovascular diseases: Part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Reddy S., Ounpuu S. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Hawken S., Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- Zubaid M., Rashed W.A., Almahmeed W. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf registry of acute coronary events (Gulf RACE) Acta Cardiol. 2009;64:439–446. doi: 10.2143/AC.64.4.2041607. [DOI] [PubMed] [Google Scholar]


