Abstract
Coronary sinus (CS) anomalies such as diverticulum, persistent left superior vena cava or CS ostium dilatation are predominantly found in patients with accessory pathway-related tachycardias. Diverticulum of the proximal CS found in 7–11% of patients with postero-septal or left posterior manifests accessory pathways. We reported a 28 year old gentleman with manifested postero-septal accessory pathway, who underwent repeat electrophysiological study (EPS) and radiofrequency ablation for previously failed ablation. Huge CS diverticulum was identified by angiography as a reason for resistant accessory pathway. Successful RF ablation was achieved at the neck of the diverticulum without complications. Other associated anomalies were ruled out by cardiac computerized tomography (CT) and trans-esophageal echocardiography.
Keywords: WPW, Cardiac CT, CS diverticulum, Ablation
1. Introduction
Radiofrequency current ablation has been used with great success in patients with Wolff–Parkinson–White syndrome (Jackman, 1991). Radiofrequency catheter ablation has become the treatment of choice for patients with symptomatic tachyarrhythmias (Morady, 2004). Target sites for ablation of accessory pathways are identified by early ventricular activation relative to the delta wave onset (for manifest accessory pathways), by the earliest atrial activation in the retrograde direction (for any accessory pathway that conducts retrogradely), and/or by the presence of high frequency electrogram consistent with an accessory pathway potential (Sethi et al., 2007). For most free-wall accessory pathways, complete bidirectional block can be achieved with a conventional 4 mm-tip ablation catheter, using a power setting of 50 W and a temperature setting of 60 °C. If the conduction block is transient, permanent accessory pathway block may be easier to achieve with an 8 mm-tip ablation catheter or with an irrigated-tip ablation catheter (ACC/AHA/ESC Guidelines, 2003; Al-Khatib et al., 1999). Accessory pathways posteroseptal in location are most often ablatable using a right-sided approach with the delivery of radiofrequency energy along the posteroseptal aspect of the tricuspid annulus (Sethi et al., 2007). The initial efficacy of catheter ablation of accessory pathways is approximately 95% in most series (Sethi et al., 2007; ACC/AHA/ESC Guidelines, 2003; Al-Khatib et al., 1999).
Coronary sinus aneurysm can be diagnosed by echocardiography, coronary sinus contrast angiography, and nuclear magnetic resonance imaging (Pedersen et al., 1992). CS diverticula associated with pre-excitation can be visualized by transesophageal echocardiography. This case study reports the assessment of coronary sinus diverticulum associated with posteroseptal accessory pathway using angiography, CT and transesophageal echocardiography.
2. Case presentation
A 28 year old male was diagnosed with Wolff–Parkinson–White syndrome with left posteroseptal accessory pathway location based on the surface electrocardiogram (Fig. 1). Radiofrequency ablation using the retrograde approach was unsuccessful. An electrophysiological study and ablation procedure were hence repeated. Assuming that accurate mapping was done previously, immediate transeptal puncture was to be performed due to the failed retrograde approach.
Figure 1.
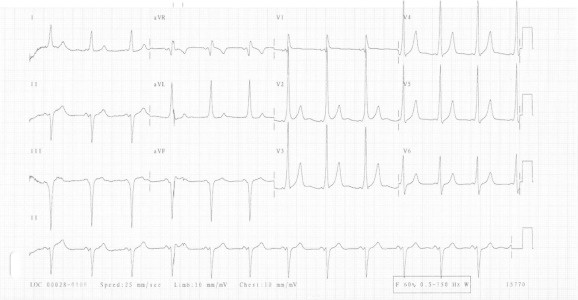
Twelve-lead surface ECG (25 mm/s): sinus rhythm with ventricular preexcitation with left postero-septal location.
Subsequently, a 4 mm-tip ablation catheter (Boston Scientific EPT) was introduced into the left atrium via a long sheath (Diag SL1, SJM). Careful mapping during sinus rhythm around the mitral valve annulus did not identify a clear site of pathway insertion, and the relatively early ventricular activation was located at the posterior septum. Although the electrogram was not completely fused, several radiofrequency lesions were applied at the posterior septum resulting in a minimal separation of atrial and ventricular signals. However, pre-excitation persisted. Further assessments of atrio-ventricular activation in the left side were unrevealing. The possibility of deep epicardial location or right posteroseptal insertion was raised, therefore, further mapping was performed from the right side. This revealed a typical fusion of the activation deep inside the middle cardiac vein. Abnormal coronary sinus anatomy was suspected during this stage. Coronary sinus angiography, using SL1 sheath and reverse Bermin angio catheter (Fig. 2a and b), identified a very large, saccular, and proximal coronary sinus diverticulum.
Figure 2.
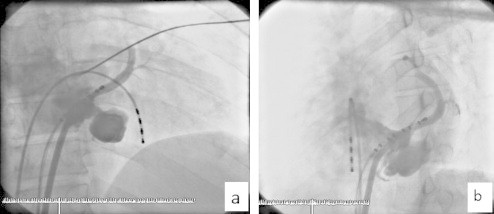
(a and b) Coronary sinus diverticulum selective contrast media injection antero- posterior and left anterior oblique view.
Old ablation catheter was used for mapping and ablation around the diverticulum neck, but the results were unsatisfactory, probably due to the distorted anatomy and the stagnant blood flow which made it difficult to generate enough power to create deep lesions. Therefore, it was replaced by an 8 mm-tip ablation catheter to ensure effective electrical current and energy. Finally, the accessory pathway was successfully ablated (Fig. 3). Additional coronary sinus and selective diverticular angiograms were obtained at the end of the procedure which revealed systolic and diastolic phases without communications with the coronary arteries (Fig. 4a–c). Post procedure, CT angiography as well as transesophageal echocardiography were performed for further assessment of the diverticulum and to rule out associated anomalies (Figs. 5 and 6).
Figure 3.
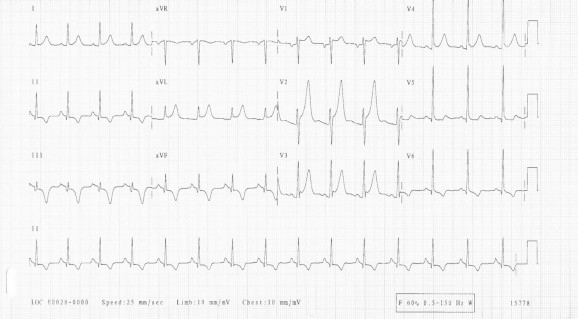
Post ablation 12 leads ECG showed complete disappearance of pre-excitation.
Figure 4.
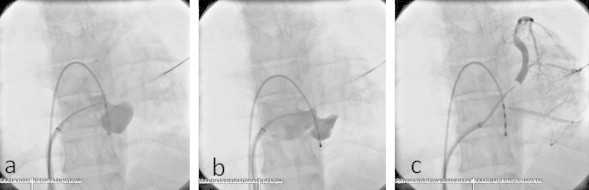
(a and b) Selective CS angiography during systole and diastole, (c) occlusive CS angiography showed no retrograde connection to the diverticulum.
Figure 5.
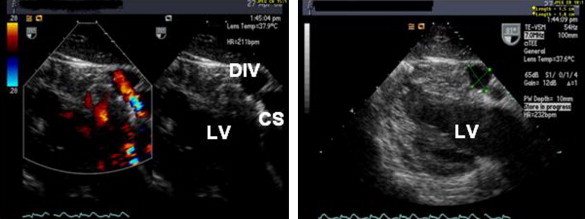
Transoesephageal echo with and without Doppler showed diverticulum communicating with the coronary sinus. (Div, diverticulum; CS, coronary sinus).
Figure 6.

Cardiac CT angiography shows the diverticulum communicating with the coronary sinus without associated anomalies.
3. Discussion
Coronary sinus aneurysms or diverticulae are rare congenital anomalies, and diverticulae associated with a posteroseptal accessory atrioventricular connection were first described in 1985. They have been identified at necropsy in patients with Wolff–Parkinson–White syndrome or sudden death, during surgical ablation of posteroseptal pathways, and during angiographic and electrophysiological studies (Bennett and Hall, 2001). Coronary sinus aneurysm can be diagnosed by echocardiography, coronary sinus contrast angiography, coronary angiography, and nuclear magnetic resonance imaging (Pedersen et al., 1992).
Electrophysiological studies can confirm the presence of posteroseptal accessory pathways, however, in the clinical environment where a patient might have grossly altered cardiac physiology under similar disease settings, it might become difficult if not impossible to determine the location of the diverticulum and thus to deliver radiofrequency ablation treatment, which is the preferred course of treatment. Echocardiographically, diverticulae appear as echo-lucent, contractile pouches on the epicardial surface of the posteroseptal or posterior left ventricle that connects to the coronary sinus by an isthmus (Hamiton et al., 1996). Previous reports have suggested that accessory pathways associated with coronary sinus aneurysms have rapid conduction times and may be associated with an increased risk of rapid ventricular response during atrial fibrillation and sudden death (Weiss et al., 2009). In the present case ablation was successful at the neck of the diverticulum only after delineation of the CS-associated anomaly.
4. Conclusion
In case of resistant posterior or postero-septal accessory pathway, further delineation of the coronary sinus anatomy might be necessary to rule out associated anomalies. CCT and trans-esophageal assessment to visualize CS anatomy associated with pre-excitation may prevent complications and enhance the success rate.
References
- ACC/AHA/ESC Guidelines for the management of patients with supraventricular arrhythmias – executive summary. Eur. Heart J. 2003. 24, 1857–1897.
- Al-Khatib Sana M., Edward L.C., Pritchett Clinical features of Wolff–Parkinson–White syndrome. Am. Heart J. 1999;138:403–413. doi: 10.1016/s0002-8703(99)70140-7. [DOI] [PubMed] [Google Scholar]
- Bennett D.H., Hall M.C.S. Coronary sinus diverticulum containing posteroseptal accessory pathway. Heart. 2001;86:539. doi: 10.1136/heart.86.5.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamiton K., Castillo M., Arruda M., Jackman W. Echocardiographic demonstration of coronary sinus diverticula in patients with Wolff–Parkinson–White syndrome. J. Am. Soc. Echocardiogr. 1996;9:337–343. doi: 10.1016/s0894-7317(96)90149-2. [DOI] [PubMed] [Google Scholar]
- Jackman W.M. Catheter ablation of accessory atrioventricular pathways (Wolff–Parkinson–White syndrome) by radiofrequency current. N. Engl. J. Med. 1991;324:1605–1611. doi: 10.1056/NEJM199106063242301. [DOI] [PubMed] [Google Scholar]
- Morady F. Cather ablation of supraventricular arrhythmias: state of the art. PACE. 2004;27:125–142. doi: 10.1111/j.1540-8159.2004.00401.x. [DOI] [PubMed] [Google Scholar]
- Pedersen A.K., Benetis R., Thomsen P.E.B. A posteroseptal accessory pathway located in a coronary sinus aneurysm: diagnosis and radiofrequency catheter ablation. Br. Heart J. 1992;68:414–416. doi: 10.1136/hrt.68.10.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi K.K., Dhall A., Chadha D.S., Garg S., Malani S.K., Mathew O.P. WPW and preexcitation syndromes. JAPI. 2007;55:10–15. [PubMed] [Google Scholar]
- Weiss C., Willems S., Meinertz T., Kuck Kh., Cappato R. Prospective evaluation of the coronary sinus anatomy in patients undergoing electrophysiologic study. Clin. Cardiol. 2009;22:537–543. doi: 10.1002/clc.4960220810. [DOI] [PMC free article] [PubMed] [Google Scholar]


