Abstract
Caseous mitral annular calcification (CMAC) is a variant of mitral annular calcification (MAC) with a central liquefaction necrosis. The echocardiographic prevalence of CMAC is approximately 0.6% in patients with MAC and 0.06–0.07% in large series of patients of all ages. However, the prevalence in necropsy series has been reported to be 2.7%, which indicates that this condition is yet under-recognized. Furthermore CMAC is probably underappreciated as a source of potentially serious conditions. We report a case of recent stroke associated with CMAC diagnosed by trans-thoracic and confirmed by trans-esophageal echocardiogram (TEE). The importance of correct diagnosis of CMAC extends beyond the possible complications; since several misdiagnoses of CMAC as abscesses and cardiac tumors have been reported leading to inappropriate interventions.
Keywords: Caseous mitral annular calcification (CMAC), Mitral annular calcification (MAC), Trans-esophageal echocardiography (TEE), Stroke
Introduction
Mitral annular calcification (MAC) is a common finding especially among the elderly. However, caseous mitral annular calcification (CMAC), alternatively termed liquefaction necrosis of MAC, is a rare echocardiographic finding, which may be mistaken for an intra-cardiac tumor or abscess. CMAC has an appearance of a large echogenic mass with a central echo-lucent area and no acoustic shadowing artifacts [9]. It is a degenerative abnormality of the fibrous skeleton of the heart that usually involves the posterior annulus of the mitral valve. The lesion is typically composed of an admixture of calcium, fatty acids, and cholesterol and has “toothpaste like” texture. This pasty material is composed of amorphous acellular basophilic substance with scattered calcifications and sparse histiocytes [11].
CMAC is usually considered as a benign condition; however, it may cause mitral stenosis, mitral regurgitation, left ventricular outflow obstruction or systemic embolization [2,12,13].
We report a case of CMAC presenting with stroke, aiming to reconsider the clinical significance of this condition.
1. Case study
A 59-year-old female with end-stage renal disease (ESRD) was admitted with left-side weakness. She had a known history of hypertension, coronary artery disease and bronchial asthma. Her CT brain scan showed lacunar infarcts in the posterior limb of the internal capsule. Laboratory investigations revealed high blood urea (23 mmol/L) and serum creatinine (473 μmol/L), normal serum calcium, high serum phosphate (1.65 mmol/L), high ESR (82 mm/h) and high eosinophilic count (14.8%). Blood cultures were negative.
Trans-thoracic echocardiogram showed a rounded mass located in the posterior mitral annulus with faint central echo-lucent area without acoustic shadowing (Fig. 1). This prompted the need for trans-esophageal echocardiography (TEE) which revealed round to oval echo-bright mass with central echo-lucent area and no acoustic shadowing artifacts. No communication with any cardiac chamber could be detected (Fig. 2). Otherwise, there was no cardiac source of systemic embolism on this TEE study.
Figure 1.
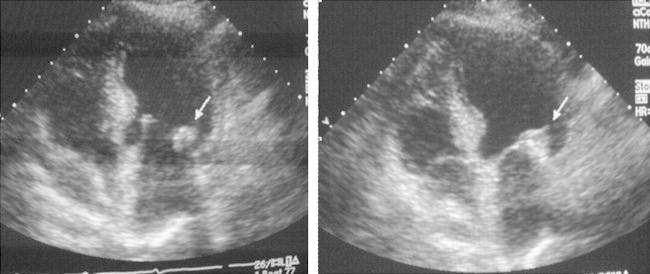
Two trans-thoracic echocardiography views showing “2.5 × 2.8 cm echo-dens mass”.
Figure 2.
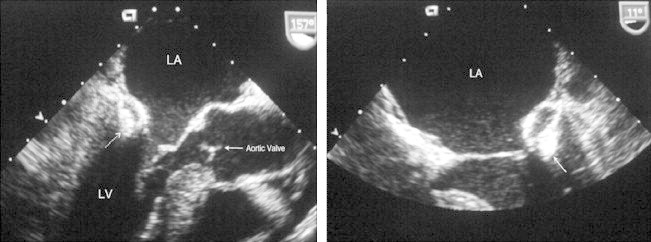
Two trans-esophageal echocardiography views showing “echo-dens mass with central lucent area”.
Despite the high ESR, valvular endocarditis was unlikely in the absence of vegetation on any of the heart valves, valve dysfunction, fever or positive blood cultures. The specific echocardiographic features favored the diagnosis of CMAC.
Although some authors advise operative intervention in case of CMAC with evidence of embolic phenomena [6], surgical removal of CMAC was not considered in our case due to the absence of mitral valve dysfunction and the lack of randomized trials to support the operative intervention.
2. Discussion
2.1. Prevalence
The echocardiographic prevalence of CMAC is 0.64% of patients with MAC and 0.068% of all studies in large series of patients of all ages [7]. However, the prevalence in necropsy series has been reported to be 2.7% [14], which indicates that this condition is yet under-recognized. The prevalence tends to be higher in elderly women, hypertensive patients and patients with chronic renal failure or altered calcium-phosphate metabolism.
2.2. Echocardiographic findings
The CMAC is defined echocardiographically as a round or semilunar bright echogenic mass in the peri-annular region of the mitral valve, typically in the posterior mitral annulus [9]. Characteristically, it contains a central echo-lucent area resembling liquefaction, but with no acoustic shadowing artifacts unlike the mitral annular calcification that presents with a posterior echo shadow.
Transthoracic echocardiography provides a good diagnostic tool for detection of CMAC. However, in some patients, limited acoustic viewing restricts its diagnostic accuracy. The trans-esophageal approach has additional value since it improves visualization of cardiac structures and in assessing its consistency, mobility and intra-cardiac origin, particularly if posteriorly located.
The best visualization of the mass and its characteristic central area of echoluency is obtained by trans-esophageal echocardiography (TEE) in the mid-esophageal 4-chamber, the mid-esophageal 2-chamber and the mid-esophageal long axis views.
2.3. Pathogenesis
The true pathogenesis of caseous calcification is unknown; it might be an atheroma-like lesion. MAC, in general, might be a part of multiple atherosclerotic lesions, since recent reports note that calcification of the mitral annulus is related to atherosclerosis in other vascular beds including atherosclerotic coronary artery disease [1,3]. However, the higher prevalence of CMAC in patients with end-stage renal disease particularly those on hemodialysis and the observed association with hypercalcemic states suggest a relationship to altered calcium-phosphate metabolism.
CMAC may represent a reversible stage of MAC. In a large series of 20,468 consecutive patients referred for trans-thoracic echocardiography, 3 patients (out of 2169 patients diagnosed with MAC) progressed to CMAC. In the same series, 3 patients (out of 14 patients diagnosed with CMAC) reverted back to MAC. The authors concluded that CMAC may be a dynamic process [7]. Few other reports described cases of caseous calcification with spontaneous resolution, supporting the theory of dynamic nature of CMAC [8,5].
2.4. Clinical significance
In three different case reports, CMAC was linked to cerebral stroke in elderly women (72, 74 and 76 year old) [4,13,10]. In our case, CMAC is associated with cerebral stroke in a 59-year-old female. The earlier presentation may be related to end-stage renal disease.
Possible mechanisms for cerebral embolism in CMAC include embolization of small calcified parts, thrombus formation or fistulization of a caseous necrosis in the lumen of the left ventricle [4]. The increased incidence of cerebral stroke may be related to factors such as the size, the mobility and the location of the CMAC; however, such factors are not yet studied in the literature.
CMAC may also present with mitral regurgitation or less likely mitral stenosis [12,15,13]. Furthermore, the CMAC may push the mitral leaflet apparatus more anteriorly towards the left ventricular outflow tract resulting in systolic anterior motion (SAM) of the mitral valve leaflets and left ventricular outflow obstruction.
Since mitral annulus is close to the AV node and the His-Purkinje system, a high frequency of conduction abnormalities was observed in patients with CMAC.
The clinical significance of CMAC extends beyond the potential complications to include the importance of the correct diagnosis to avoid inappropriate intervention as it may be misdiagnosed as intra-cardiac tumor, abscess, vegetation or thrombus.
Despite the high ESR noted in our case, the possibility of vegetation was ruled out by the characteristic echocardiographic features of CMAC and the absence of clinical criteria of infective endocarditis.
2.5. Treatment
Optimal treatment of CMAC remains to be established. Although the presence of asymptomatic caseous calcification might be followed-up echocardiographically, any evidence of significant valve dysfunction or embolic phenomena may encourage operative intervention. Uncertain diagnosis may be another indication for surgery.
In a series of 18 patients with CMAC, 3 patients have undergone mitral valve replacement [9].
In a reported case of CMAC and end-stage renal disease on regular hemodialysis, treatment with low calcium hemodialysis was associated with regression of the CMAC. The authors concluded that acute change in the serum calcium level may contribute to the resolution of the mass [16].
3. Conclusion
A calcified mass connected to the posterior mitral annulus should raise suspicion of CMAC. Despite being a rare echocardiographic finding, CMAC may be a potentially serious condition. The clinical significance of CMAC, particularly the increased incidence of stroke should be reviewed and factors such as size, mobility and location of the mass and its relation to the increased incidence of embolization should be evaluated. Echocardiographic follow-up seems to be sufficient in asymptomatic cases; however, surgery should be considered whenever there is an evidence of embolic phenomenon or valve dysfunction. TEE should be considered in all cases of suspected embolic stroke; this may help in the decision of surgical vs. medical treatment.
Conflict of Interest
Authors have no conflict of interest to declare.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Allison M.A., Cheung P., Criqui M.H., Langer R.D., Wright C.M. Mitral and aortic annular calcification are highly associated with systemic calcified atherosclerosis. Circulation. 2006;113:861. doi: 10.1161/CIRCULATIONAHA.105.552844. [DOI] [PubMed] [Google Scholar]
- 2.Alkadhi H., Leschka S., Prêtre R., Perren A., Marincek B., Wildermuth S. Caseous calcification of the mitral annulus. J Thorac Cardiovasc Surg. 2005;129:1438–1440. doi: 10.1016/j.jtcvs.2004.11.051. [DOI] [PubMed] [Google Scholar]
- 3.Atar S., Jeon D.S., Luo H., Siegel R.J. Mitral annular calcification: a marker of severe coronary artery disease in patients under 65 years old. Heart. 2003;89:161–164. doi: 10.1136/heart.89.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chevalier B., Reant P., Laffite S., Barandon L. Spontaneous fistulization of a caseous calcification of the mitral annulus: an exceptional cause of stroke. Eur J Cardiothorac Surg. 2011;39(6):e184–e185. doi: 10.1016/j.ejcts.2011.01.038. [Epub March 3, 2011] [DOI] [PubMed] [Google Scholar]
- 5.Correale M., Deluca G., Ieva R., Di Biase M. Spontaneous resolution of a caseous calcification of the mitral annulus. Clinics. 2009;64(11):1130–1132. doi: 10.1590/S1807-59322009001100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davidson M.J., Cohn L.H. Surgical treatment of caseous mitral valve annulus calcification. J Thorac Cardiovasc Surg. 2006;131:738–739. doi: 10.1016/j.jtcvs.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Deluca G., Correale M., Leva R., Del Salvatore B., Gramenzi S., Di Biase M. The incidence and clinical course of caseous calcification of the mitral annulus. J Am Soc Echocardiogr. 2008;21:828–833. doi: 10.1016/j.echo.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Gramenzi S., Mazzola A.A., Tagliaferri B., Protasoni G., Brusoni D., d’Aloya G. Caseous calcification of the mitral annulus: unusual case of spontaneous resolution. Echocardiography. 2005;22(6):510–513. doi: 10.1111/j.1540-8175.2005.04056.x. [DOI] [PubMed] [Google Scholar]
- 9.Harpaz D., Auerbach I., Vered Z., Motro M., Tobar A., Rosenblatt S. Caseous calcification of the mitral annulus: a neglected, unrecognized diagnosis. J Am Soc Echocardiogr. 2001;14(8):825–831. doi: 10.1067/mje.2001.111877. [DOI] [PubMed] [Google Scholar]
- 10.Higashi H., Ohara T., Nakatani S., Hashimoto S., Torii T., Miyashita K. A case of caseous calcification of the mitral annulus: a potential source of embolic stroke. J Cardiol Cases. 2010;2(3):e141–e143. doi: 10.1016/j.jccase.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronzon I., Winer H.E., Cohen M.L. Sterile, caseous mitral anular abscess. J Am Coll Cardiol. 1983;2:186–190. doi: 10.1016/s0735-1097(83)80391-x. [DOI] [PubMed] [Google Scholar]
- 12.Marcì M., Lo Jacono F. Mitral regurgitation due to caseous calcification of the mitral annulus: two case reports. Cases J. 2009;2:95. doi: 10.1186/1757-1626-2-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poh K.K., Wood M.J., Cury R.C. Prominent posterior mitral annular calcification causing embolic stroke and mimicking left atrial fibroma. Eur Heart J. 2007;28(18):2216. doi: 10.1093/eurheartj/ehm052. [DOI] [PubMed] [Google Scholar]
- 14.Pomerance A. Pathological and clinical study of calcification of the mitral valve ring. J Clin Pathol. 1970;23:354–361. doi: 10.1136/jcp.23.4.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pozsonyi Z., Tóth A., Vágó H., Adám Z., Apor A., Alotti N. Severe mitral regurgitation and heart failure due to caseous calcification of the mitral annulus. Cardiology. 2011;118(2):79–82. doi: 10.1159/000326850. [DOI] [PubMed] [Google Scholar]
- 16.Koito H., Nakamura C., Suzuki J., Takahashi H., Iwasaka T. Reduced size of liquefaction necrosis of mitral annular calcification in chronic renal failure by using low calcium concentration hemodialysis. Jpn Circ J. 1999;63(6):490–492. doi: 10.1253/jcj.63.490. [DOI] [PubMed] [Google Scholar]



