Abstract
Objective
To characterize risk profile of acute coronary syndrome (ACS) patients in different age groups and compare management provided to in-hospital outcome.
Design
Prospective multi-hospital registry.
Setting
Seventeen secondary and tertiary care hospitals in Saudi Arabia.
Patients
Five thousand and fifty-five patients with ACS. They were divided into four groups: ⩽40 years, 41–55 years, 56–70 years and ⩾70 years. Main outcome measures: prevalence, utilization and mortality.
Results: Ninety-four percent of patients <40 years compared to 68% of patients >70 years were men. Diabetes was present in 70% of patients aged 56–70 years. Smoking was present in 66% of those <40 years compared to 7% of patients >70 years. Fifty-three percent of the patients >70 years and 25% of those <40 years had history of ischemic heart disease. Sixty percent of patients <40 years presented with ST elevation myocardial infarction (STEMI) while non-ST elevation myocardial infarction was the presentation in 49% of patients >70 years. Thirty-four percent of patients >70 years compared to 10% of patients <40 years presented >12 h from symptom onset with STEMI. Fifty-four percent of patients >70 compared to 64–71% of those <70 years had coronary angiography. Twenty-four percent of patients >70 compared to 34–40% of those <70 years had percutaneous coronary intervention. Reperfusion shortfall for STEMI was 16–18% in patients >56 years compared to 11% in patients <40 years. Mortality was 7% in patients >70 years compared to 1.6–3% in patients <70 years. For all comparisons (p < 0.001).
Conclusions
Young and old ACS patients have unique risk factors and present differently. Older patients have higher in-hospital mortality as they are treated less aggressively. There is an urgent need for a national prevention program as well as a systematic improvement in the care for patients with ACS including a system of care for STEMI patients. For older patients there is a need to identify medical as well as social factors that influence the therapeutic management plans.
Keywords: Age, Mortality, In-hospital outcome, Acute coronary syndrome
Age is a recognized determinant of outcome in acute coronary syndromes (ACS) [1]. In the Global Registry of Acute Coronary Events (GRACE) registry age was found to be an independent prognostic predictor of hospital mortality across the entire spectrum of ACS in general clinical practice with an odds ratio of 1.70 per 10 year increment [2]. Although age above 65 years is part of the TIMI risk score, the utilization of angiography and revascularization has been found to be less in the elderly [3]. No comparable data exist for Saudi Arabia. The Saudi Project for the Assessment of Coronary Events (SPACE) registry was designed to study ACS. By studying the characteristics of patients it would be possible to target interventions suitable for each age group in order to reduce the burden of modifiable risk factors, optimize outcome and follow evidence based practice.
Methods
Patient population and methods
SPACE was a prospective registry of all consecutive ACS patients that were admitted to 17 participating hospitals. The diagnosis of different types of ACS as well as the definitions of the terms used was based on the definitions of American College of Cardiology (ACC) [4]. Current smoking was defined as having smoked cigarettes or tobacco within the previous 12 months. The study design, population, data collection and organization have been previously described [5].
For the purpose of this analysis patients were divided into four groups: ⩽40 years, 41–55 years, 56–70 years and ⩾70 years.
Study organization
Data collected included demographics, medical history including the presence of known cardiovascular risk factors, diagnosis on admission and final discharge diagnosis, ECG findings, laboratory investigations, medical therapy, use of cardiac procedures and interventions, in-hospital outcomes, and mortality. Ethical approval was obtained in all participating centers.
Statistical analysis
Categorical data were summarized with absolute numbers and percentages. Continuous data were summarized with means and standard deviations (SD) or median and inter-quartile range (IQR). Comparisons among different groups were performed using Chi-square test for categorical variables and analysis of variance or Kruskal–Wallis test for continuous variables. Whenever needed Bonferroni correction was used to adjust for multiple comparisons. Cochran–Armitage trend test was used to test the statistical significance of the observed trend in in-hospital outcome across different age groups. Multiple logistic regression analysis was used to estimate the adjusted odds ratios. Adjustments were made for, gender, body mass index (BMI), smoking, hyperlipidaemia, diabetes, hypertension, heart rate, systolic blood pressure, past history of IHD, peripheral artery disease (PAD), diagnostic coronary angiography, PCI, CABG, and all pharmacological therapies. All analyses were performed using [SAS/STAT] software, Version [9.1.3] (SAS Institute Inc., Cary, NC, USA).
Results
Baseline patient characteristics
The SPACE registry collected data on 5055 patients from 17 participating hospitals between December 2005 and December 2007 (Table 1). Patient’s age ranged from 18 to 111 years with a mean of 58 years. Seventy-five percent were 41–70 years, 9% ⩽40 years while 16% were >70 years. Women were increasingly represented with increasing age, comprising 6% of patients ⩽40 years and reaching 32% of patients >70 years (p < 0.001). Saudi citizens predominated in all age groups, and the proportion increased with increasing age (p < 0.001). Patients ⩾56 years were more likely to have diabetes mellitus and hypertension. Hyperlipidemia varied among age groups from approximately one-third to almost one-half, peaking in those aged 56–70 years (p < 0.001). The prevalence of smoking was highest in patients aged ⩽40 years and was least in those >70 years (p < 0.001). The prevalence of history of ischemic heart disease (IHD) increased with age and was highest in those >70 years (p < 0.001).
Table 1.
Patients’ baseline characteristics.
| Variables | Overall | Age <40 years | Age 41–55 years | Age 56–70 years | Age > 70 years | p value |
|---|---|---|---|---|---|---|
| n (%) | 5055(100) | 440(9) | 1835(36) | 1951(39) | 829(16) | |
| Mean age (SD) (years) | 58.01(12.92) | 36.1(4.13) | 48.8(4.06) | 63.2(4.22) | 77.8(5.92) | |
| Male sex, n (%) | 3919(77) | 412(94) | 1538(84) | 1404(72) | 565(68) | <0.001 |
| Saudi nationality, n (%) | 4167(82) | 289(66) | 1332(73) | 1752(90) | 794(96) | <0.001 |
| Diabetes mellitus, n (%) | 2933(58) | 113(26) | 941(51) | 1373(70) | 506(61) | <0.001 |
| Hypertension, n (%) | 2785(55) | 121(28) | 839(46) | 1283(66) | 542(66) | <0.001 |
| Current smoker, n (%) | 1636(32) | 291(66) | 875(48) | 413(21) | 57(7) | <0.001 |
| Hyperlipidemia, n (%) | 2086(41) | 138(32) | 704(39) | 933(48) | 311(38) | <0.001 |
| History of IHD, n (%) | 1568(45) | 111(25) | 682(37) | 915(47) | 438(53) | <0.001 |
| History of PCI, n (%) | 700(13) | 40(9) | 247(13) | 304(16) | 109(13) | <0.001 |
| History of CABG, n (%) | 296(6) | 7(2) | 70(4) | 131(7) | 88(11) | <0.001 |
| History of CVA/TIA, n (%) | 309(6) | 5(1) | 54(3) | 152(8) | 98(12) | <0.001 |
| History of PAD, n (%) | 364(7) | 10(2) | 94(5) | 152(8) | 108(13) | <0.001 |
| Ambulance use, n (%) | 186(5) | 14(4) | 78(6) | 62(5) | 32(5) | 0.168 |
| Ischemic chest pain, n (%) | 3057(88) | 284(93) | 1173(91) | 1142(86) | 458(80) | <0.023 |
| SBP ⩽ 90 mmHg, n (%) | 148(3) | 13(3) | 53(3) | 57(3) | 25(3) | 0.999 |
| HR ⩾ 100 beats per minute, n (%) | 679(15) | 53(13) | 238(14) | 262(15) | 126(16) | 0.491 |
| Presenting with KILLIP class > 1, n (%) | 937(21) | 54(13) | 249(15) | 394(23) | 240(31) | <0.001 |
| STEMI, n (%) | 2096(41) | 263(60) | 883(48) | 691(35) | 259(31) | <0.001 |
| STEMI presenting first to a registry hospital within 12 h from symptom onset, n (%) | 912(74) | 159(87) | 413(79) | 248(67) | 92(59) | <0.001 |
| STEMI presenting first to a registry hospital beyond 12 h from symptom onset, n (%) | 260(21) | 18(10) | 89(17) | 100(27) | 53(34) | <0.001 |
| NSTEMI, n (%) | 1841(36) | 112(25) | 526(29) | 801(41) | 402(49) | <0.001 |
| Unstable angina, n (%) | 1118(22) | 65(15) | 426(23) | 459(24) | 168(20) | <0.001 |
NSTEMI = non-ST elevation acute myocardial infarction; STEMI = ST elevation myocardial infarction; IHD = ischemic heart disease; PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft; CVA/TIA = cerebrovascular accident/transient ischemic attack; SBP = systolic blood pressure; HR = heart rate. PAD = peripheral arterial disease.
ACS type, clinical presentation and extent of disease by age
Of the 5055 patients, 2096 (41%) presented with STEMI, 1841 (36%) with NSTEMI, and 1118 (22%) with UA. NSTEMI increased with age from 25% of patients aged ⩽40 years to 49% of patients aged >70 years (p < 0.001). Conversely, STEMI decreased with increasing age from 60% of patients aged ⩽ 40 years to 31% of patients aged >70 years (p < 0.001). As age increased, patients with STEMI were less likely to present to a registry hospital within 12 h from symptom onset (p < 0.001). UA was of lesser frequency (15%) in patients aged ⩽40 years than in the other age groups (20–24%; p < 0.001). Of the two-thirds of patients with an angiogram, single vessel disease was less prevalent with increasing age, while three-vessel or left main disease was more common in older patients (p < 0.001). A presentation in Killip class >1 increased with age (p < 0.001). Admission creatinine was higher with increasing age (p < 0.001).
In-hospital treatment
The use of aspirin, clopidogrel and statins was similar among age groups (Table 2). There was a trend for less use of beta blockers (BB) with increasing age (p = 0.003). Patients aged ⩽40 years were less likely to be treated with either an angiotensin converting enzyme inhibitor (ACEI) and or angiotensin receptor blocker (ARB) (p < 0.001).
Table 2.
In-hospital treatment.
| Therapies used | Overall | Age <40 years | Age 41–55 years | Age 56–70 years | Age >70 years | p Value |
|---|---|---|---|---|---|---|
| n (%) | 5055(100) | 440(9) | 1835(36) | 1951(39) | 829(16) | |
| Aspirin, n (%) | 4935(97) | 432(98) | 1795(98) | 1903(97) | 805(97) | 0.321 |
| Clopidogrel, n (%) | 4232(84) | 357(81) | 1543(84) | 1630(83) | 702(85) | 0.542 |
| Beta-blockers, n (%) | 4121(81) | 375(85) | 1518(83) | 1583(81) | 645(78) | 0.003 |
| ACEI/ARB, n (%) | 3805(75) | 292(66) | 1345(73) | 1524(78) | 644(78) | <0.001 |
| STATIN, n (%) | 4711(93) | 408(93) | 1725(94) | 1814(93) | 764(92) | 0.429 |
| Thrombolytic therapy for STEMI within 12 h from symptom onset, n (%) | 627(69) | 116(73) | 305(74) | 151(61) | 55(60) | <0.001 |
| Primary PCI within 12 h from symptom onset, n (%) | 158(17) | 25(16) | 58(14) | 53(21) | 22(24) | <0.001 |
| Reperfusion shortfall in STEMI patients initially presenting within 12 h to a registry hospital, n (%) | 127(14) | 18(11) | 50(12) | 44(18) | 15(16) | <0.001 |
| Coronary angiogram, n (%) | 3403(67) | 282(64) | 1280(70) | 1390(71) | 451(54) | <0.001 |
| Non critical disease, n (%) | 58(2) | 19(7) | 27(2) | 9(1) | 3(1) | <0.001 |
| Single vessel CAD, n (%) | 1074(32) | 131(47) | 464(37) | 393(29) | 86(20) | <0.001 |
| Two vessel CAD, n (%) | 745(22) | 50(18) | 280(22) | 316(23) | 99(22) | 0.345 |
| Triple Vessel CAD, n (%) | 1144(34) | 44(16) | 361(28) | 531(38) | 208(46) | <0.001 |
| Left Main CAD, n (%) | 162(5) | 5(2) | 42(3) | 71(5) | 44(10) | <0.001 |
| GP IIb/IIIa inhibitor, n (%) | 1387(27) | 121(28) | 542(30) | 541(28) | 183(22) | <0.001 |
| PCI, n (%) | 1778(35) | 172(39) | 735(40) | 671(34) | 200(24) | <0.001 |
| CABG, n (%) | 425(8) | 17(4) | 146(8) | 201(10) | 61(7) | <0.001 |
PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft surgery. STEMI = ST elevation acute myocardial infarction. ACE-I/ARB = angiotensin converting enzyme inhibitor and/or angiotensin receptor blocker; GP IIb/IIIa inhibitor = glycoprotein IIb/IIIa inhibitors.
Among STEMI patients arriving to a registry hospital within 12 h from symptom onset those aged 56 or more were less likely to receive thrombolytic therapy but were more likely to be treated with primary PCI (p < 0.001). Patients older than 56 years had the highest reperfusion shortfall with between 16% and 18% not receiving any reperfusion therapy (p < 0.001). The median door-to-needle time for STEMI patients receiving thrombolytic therapy was 53 min for the entire cohort, and increased with increasing age, from a median of 50 min in patients aged ⩽56 years to 84 min in those aged >70 years (p = 0.009). Patients >70 years were less likely to get an angiogram, receive a glycoprotein IIb/IIIa inhibitor or be treated by PCI (p < 0.001). Patients in the age group 56–70 years were more likely than other age groups to be treated by coronary artery bypass graft surgery (CABG).
In-hospital outcome
Recurrent myocardial infarction occurred in 77 patients (1.5%), and did not vary among age groups (p = 0.108) (Table 3). Older patients were more likely to develop heart failure, cardiogenic shock or have a major non-surgical bleed (p < 0.001). Overall, 155 patients (3%) died. In-hospital mortality increased from <2% of patients aged <56 years to 7% of patients aged >70 years (p < 0.001). Following adjustment for several variables the adjusted odds ratio for mortality was 0.25 for patients 41–55 years and 0.33 for patients 56–70 years in comparison to those >70 years and 0.45 for heart failure development in patients aged 41–55 years in comparison to those >70 years (both p < 0.001) (Table 4).
Table 3.
In-hospital outcome.
| Variables | Overall, n (%) | Age below 40 years | Age 41–55 years | Age 56–70 years | Age more than 70 years | p Value using Chi-square test | p Value using Cochran–Armitage trend test |
|---|---|---|---|---|---|---|---|
| Death, n (%) | 155(3.0) | 8(1.8) | 30(1.6) | 58(3) | 59(7) | <0.001 | <0.001 |
| Recurrent myocardial infarction, n (%) | 77(1.5) | 4(1) | 24(1.3) | 29(1.5) | 20(2.4) | 0.108 | 0.0127 |
| Non-surgical major bleeding, n (%) | 68(1.3) | 4(1) | 6(0.3) | 42(2) | 16(1.9) | <0.001 | <0.001 |
| Stroke, n (%) | 48(0.9) | 3(0.6) | 13(0.7) | 20(1) | 12(1.5) | 0.29 | 0.033 |
| Heart failure during hospitalization, n (%) | 520(10.2) | 19(4.3) | 115(6.2) | 258(13) | 128(15) | <0.001 | <0.001 |
| Cardiogenic shock, n (%) | 222(4.4) | 17(3.8) | 58(3) | 92(4.7) | 55(6.6) | <0.001 | <0.001 |
Table 4.
Multivariate analysis for in-hospital outcome.
| Outcomes | Age in years | OR(95% CI) | p Value | Adjusted OR | p Value |
|---|---|---|---|---|---|
| Death | ⩽40 | 0.24(0.11–0.51) | <0.001 | 0.30(0.06–1.44) | 0.1345 |
| 41–55 | 0.21(0.13–0.33) | <0.001 | 0.25(0.11–0.56) | <0.001 | |
| 56–70 | 0.39(0.27–0.57) | <0.001 | 0.33(0.18–0.62) | <0.001 | |
| Recurrent myocardial infarction | ⩽40 | 0.37(0.12–1.09) | 0.0720 | 1.72(0.29–10.25) | 0.5487 |
| 41–55 | 0.53(0.29–0.97) | 0.0414 | 1.65(0.53–5.13) | 0.3831 | |
| 56–70 | 0.60(0.34–1.08) | 0.0913 | 0.79(0.25–2.46) | 0.6915 | |
| Non-surgical major bleeding | ⩽40 | 0.46(0.15–1.40) | 0.1746 | 3.68(0.75–18.09) | 0.1079 |
| 41–55 | 0.16(0.06–0.42) | <0.001 | 0.79(0.21–2.98) | 0.7376 | |
| 56–70 | 1.11(0.62–1.99) | 0.7124 | 2.42(0.88–6.65) | 0.0863 | |
| Stroke | ⩽40 | 0.47(0.13–1.67) | 0.2435 | 1.27(0.22–7.35) | 0.7837 |
| 41–55 | 0.48(0.22–1.07) | 0.0733 | 0.72(0.23–2.22) | 0.5683 | |
| 56–70 | 0.70(0.34–1.44) | 0.3397 | 0.65(0.24–1.71) | 0.3846 | |
| Heart failure during hospitalization | ⩽40 | 0.24(0.15–0.40) | <0.001 | 0.42(0.18–0.97) | 0.0443 |
| 41–55 | 0.36(0.28–0.47) | <0.001 | 0.45(0.29–0.72) | <0.001 | |
| 56–70 | 0.83(0.66–1.04) | 0.1188 | 0.90(0.62–1.29) | 0.5715 | |
| Cardiogenic shock | ⩽40 | 0.56(0.32–0.98) | 0.0448 | 1.08(0.42–2.76) | 0.8593 |
| 41–55 | 0.45(0.31–0.67) | <0.001 | 0.53(0.28–1.03) | 0.0629 | |
| 56–70 | 0.69(0.49–0.98) | 0.0387 | 0.94(0.55–1.60) | 0.8205 | |
Discussion
The SPACE registry which is the first of its kind in Saudi Arabia documented characteristics of patients, measured quality indicators including in-hospital outcome and allowed comparison with other published registries and studies worldwide.
Age and risk factors
SPACE registry patients, with a mean age of 58 years, were eight years younger than the mean age of 66 years in (GRACE) registry, and six years younger than the median of 64 years for ACC National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network (ACTION) registry [6,7]. ACS patients of similar age to SPACE registry patients include Gulf RACE ACS registry patients from six Gulf countries with a mean age of 55 years [8] and the CREATE registry from India with a mean age of 57 years [9]. In a 2000–2001 Euro Heart survey only 23% of the patients were aged <55 years while 25% were >75 years of age [10]. It is likely that younger age in this registry reflects higher prevalence of risk factors in the population in addition to the fact that there is currently considerably fewer persons aged >65 years in Saudi Arabia compared with most Western countries. In 2011, 3% of Saudis were aged ⩾65 years, which is much less than the 13.1% in the US or 16% or more in most of the European countries [11].
One alarming finding from this registry is that 66% of those below the age of 40 years were current smokers while the overall rate of current smokers was 32%. This is less than the 36.6% seen in the Gulf RACE registry. The prevalence of current smokers in a 1995–2000 nationwide Saudi epidemiological health survey of 17,350 Saudi adults was 18.1% for men aged 30–39 years and 4.5% for women in the same age group [12]. Results of other surveys suggest that the pool of smokers is being fed by Saudis who begin smoking at younger ages. A recent survey of Riyadh Health Sciences College students revealed current smoking (within the past month) to be 32.7% among male and 6% among female students aged 19–25 years [13]. These results emphasize the urgent need for national policies for primary and secondary prevention of smoking particularly amongst young people.
The rate of DM in our youngest patients (26%) was similar to that of the entire cohorts in the CREATE, ACTION, and GRACE registries (30%, 30%, and 23%). DM prevalence was 23.7% in a Saudi national survey in 1995–2000 [14]. Similarly, hypertension affected 28% of our youngest patients, compared with 26% national prevalence in Saudi Arabia in the 1995–2000 survey [15].
What is disturbing is that 25% of those ⩽40 years had history of IHD and for those aged >70 years the proportion was 53%. That a quarter of the youngest group of patients are presenting with ACS with that past history suggests ongoing progression of disease either due to non compliance with lifestyle changes or medical therapy or inadequate past revascularization. Increasing age was also associated with greater probability for all forms of vascular disease and being on evidence based treatment for vascular disease. Increasing age was also more likely to be associated with worse baseline renal function which is a predictor of worse outcome in patients with ACS [16]. The constellation of high prevalence of all these risk factors therefore demands policymakers to target primary and secondary prevention of IHD with a high degree of urgency.
Clinical presentation and treatment
Eighty-nine percent of STEMI patients <40 years received reperfusion therapy. This was the highest rate achieved in any STEMI age group but was lower than what was achieved by the middle 10% performing hospitals of the ACTION registry at 94% [7]. Only 76% of STEMI patients >56 years received any form of reperfusion therapy even when they presented within 12 h from symptom onset. We did not study the factors that led to this shortfall but this requires careful consideration in order to reduce this therapeutic missed opportunity. In addition increasing age was associated with delayed presentation. Almost one-third of patients >70 patients arrived more than 12 h from symptom onset as can be seen in Graph 1. Even when patients came in time TT was often given late and the delay was more obvious with increasing age. What was also disappointing that almost half of patients >56 had prior history of IHD and therefore should have been able to recognize symptoms and seek help early. Patients were either not sufficiently educated to seek early help or had barriers that prevented them from seeking early help. Financial considerations are not relevant since medical care is entirely free to Saudi nationals. Only 5% of patients utilized an ambulance to come to hospital while the rest were usually transported by a relative. It is not also clear whether any delay was related to the distance needed to travel to hospitals or to congestion in cities. Unfortunately even when these patients presented late they were not offered primary PCI to make up for not receiving TT. The overall rate of primary PCI was very low but similar to that reported by the CREATE registry [9]. This was extremely low in comparison to the rates achieved in ACTION (81%) or GRACE (58%) registries [7,6]. The underuse of primary PCI in spite of the fact that we have more patients presenting with STEMI and at younger age calls for major efforts to change current practice by improving the entire care process of managing such patients. The public require better education in order to shorten the time of symptom onset to presentation. Primary PCI service needs to be made more available in all areas and made accessible for people of all ages. The obstacles that lead to the very low use of the ambulance service in all age groups need to be explored since early diagnosis of STEMI before hospital arrival could influence direct transfer of patients to PCI facilities thereby reducing delays and improving adoption of such evidenced based therapy. Initiatives such as that proposed by the American Heart Association [17] or the European Society of Cardiology Stent 4 Life [18,19] or that proposed by others can be used or modified to suit local needs [20]. It has been shown that it is safe to return immediately almost two-thirds of patients to their local hospital after primary PCI [21].
Graph 1.
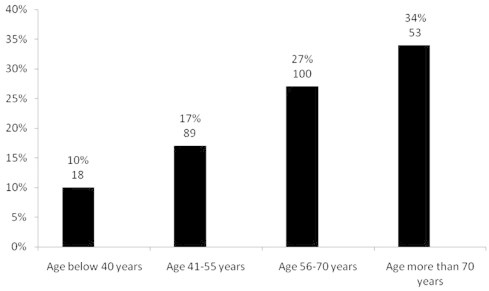
The % and number of patients presenting initially to a hospital participating in the registry beyond 12 h from symptom onset with acute ST segment elevation myocardial infarction in different age groups in the SPACE registry (p < 0.001).
The use of evidence based medical therapies upon discharge was observed to be good in all age groups. In particular the use of aspirin was 97% overall and was not significantly influenced by age. This was lower than 99% achieved by the top 10% performing hospitals in ACTION registry. Overall use of statins upon discharge was 93% and was not influenced by age. This compares with 94% achieved by the top 10% performing hospitals in ACTION registry. The overall use of clopidogrel was 84% and was not influenced by age. This compares with 86% achieved by the top 10% performing hospitals in ACTION registry. The use of beta blockers decreased with increasing age and was highest in patients <40 at 85%. This was lower than that achieved by the bottom 10% performing hospitals in the ACTION registry (92%). The use of ACEI or ARB increased with age but did not exceed 78% in those >56 years. This was similar to what was achieved by the bottom 10% performing hospitals of the ACTION registry [7].
In-hospital outcome
The lowest in-hospital mortality was seen in patients aged 41–70 years while it was highest in patients >70 years. This undoubtedly reflected not only the high prevalence of cardiovascular risk factors and greater delays in presentation, but also the sub-optimal care given to older patients. Older STEMI patients were less likely to receive reperfusion therapy or receive it very late. Even though more patients ⩾56 with all types of ACS were being admitted with prior history of IHD the proportion of past revascularization procedures with PCI or CABG was not more than 24%. It is possible that this may have also contributed to greater morbidity and mortality amongst older patients since these patients were receiving appropriate evidence based therapies on admission. Recurrent myocardial infarction, stroke, cardiogenic shock or major non-surgical bleeding were not influenced by age after multivariate adjustments for multiple risk factors and variables. Finally the lowest risk for heart failure development during hospitalization was seen in the age group 41–55 years. This perhaps reflects better myocardial function and further explains the lowest observed mortality in this age group. It is interesting to note that this group had the highest rate of thrombolytic therapy being administered within 12 h from the symptom onset in STEMI patients, the highest rate of GP IIb/IIIa inhibitor use, 70% rate of coronary angiography, the highest rate of PCI and the second highest rate of CABG. The observed higher rate of revascularization and the lower in-hospital mortality require further study to see whether this apparent early benefit is maintained over the long term or not?
Strengths and limitations
The hospitals that participated geographically represented the whole country and included general as well as tertiary care hospitals. Patient selection was avoided by requiring each hospital to maintain a log of all possible ACS patients. The use of the patient’s unique nationality or visitor identity number did not allow double counting of any patient even when being transferred between hospitals participating in the registry. Twenty percent of the entire data were audited independently by an outside auditor visiting sites and found no major concerns in the originally submitted data. Limitations include lack of long term follow-up and in-depth enquiry of factors that affected care or caused delayed presentation. In particular, we did not obtain any information from patients about their own expectation or satisfaction with the care provided. Also we did not obtain data from attending physicians regarding why a course of treatment was followed or not.
Conclusions
Young ACS patients were more likely to be smokers and to present with STEMI. Older patients were more likely to have DM, HTN, present with NSTEMI or UA, have delayed presentation, have multi-vessel CAD and were apparently treated less aggressively. They suffer from higher in-hospital mortality. There is an urgent need for a national prevention program as well as a systematic improvement in the care for patients with ACS including a system of care for STEMI patients. For older patients there is a need to identify medical as well as social factors that influence the therapeutic management plans.
Conflict of interest
None declared.
Footnotes
The SPACE registry was managed under the auspices of the Saudi Heart Association. Dr. Khalid AlHabib (principal investigator) had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
On behalf of SPACE co-investigators.
References
- 1.Alexannder K.P. Acute coronary care in the elderly, part I: non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2549–2569. doi: 10.1161/CIRCULATIONAHA.107.182615. [DOI] [PubMed] [Google Scholar]
- 2.Alexannder K.P. Acute coronary care in the elderly, part II: ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2570–2589. doi: 10.1161/CIRCULATIONAHA.107.182616. [DOI] [PubMed] [Google Scholar]
- 3.Antman E.M. The TIMI risk score for unstable angina/non-ST elevation MI. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 4.Cannon C.P. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee) J Am Coll Cardiol. 2001;38:2114–2130. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- 5.AlHabib KF, Hersi A, AlFaleh H, AlNemer K, AlSaif S, Taraben A, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients with acute coronary syndromes: results of the Saudi Project for Assessment of Coronary Events (SPACE) registry. J Saudi Heart Assoc 2011; doi:10.1016/j.jsha.2011.05.004. [DOI] [PMC free article] [PubMed]
- 6.Granger C.B. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 7.Peterson E.D. The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 2010;96:1798–1802. doi: 10.1136/hrt.2010.200261. [DOI] [PubMed] [Google Scholar]
- 8.Zubaid M. Clinical presentation and outcomes of acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE) Saudi Med J. 2008;29(2):251–255. [PubMed] [Google Scholar]
- 9.Xavier D. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 10.Rosengren A. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 11.<http://www.cia.gov/library/publications/the-world-factbook/geos/>.
- 12.Al-Nozha M.M. Smoking in Saudi Arabia and its relation to coronary artery disease. J Saudi Heart Assoc. 2009;21:169–176. doi: 10.1016/j.jsha.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Almutairi K.M. Tobacco prevalence among health sciences college students: Riyadh, Saudi Arabia. Middle East J Family Med. 2010;8(7) [Google Scholar]
- 14.Al-Nozha M.M. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25(11):1603–1610. [PubMed] [Google Scholar]
- 15.Al-Nozha M.M. Hypertension in Saudi Arabia. Saudi Med J. 2007;28(1):77–84. [PubMed] [Google Scholar]
- 16.Al-Faleh HF, Alsuwaida AO, Anhar Ullah, Hersi A, AlHabib KF, AlShahrani A, et al. Glomerular filtration rate estimated by the CKD-EPI formula is a powerful predictor of in-hospital adverse clinical outcomes after an acute coronary syndrome. Angiology 2011; doi:10.1177/0003319711409565. [DOI] [PubMed]
- 17.Jacobs A.K. Development of systems of care for ST-elevation myocardial infarction patients. Circulation. 2007;116:217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 18.Widimsky P. “Stent 4 Life” targeting PCI at all who will benefit the most. A joint project between EAPCI, Euro-PCR, EUCOMED and the ESC Working Group on Acute Cardiac Care. EuroIntervention. 2009;4:555–557. [PubMed] [Google Scholar]
- 19.Knot J. How to set up an effective national primary angioplasty network: lessons learned from five European countries. EuroIntervention. 2009;5:299–309. [PubMed] [Google Scholar]
- 20.Terkelsen C.J. Primary PCI as the preferred reperfusion therapy in STEMI: it is a matter of time. Heart. 2009;95:362–369. doi: 10.1136/hrt.2007.139493. [DOI] [PubMed] [Google Scholar]
- 21.Matteau A. The safety and feasibility of immediately returning patients transferred for primary percutaneous coronary intervention with ST-elevation myocardial infarction. EuroIntervention. 2009;5:599–603. doi: 10.4244/eijv5i5a96. [DOI] [PubMed] [Google Scholar]


