Abstract
Coronary artery anomalies (CAAs) are found in approximately 1% of all patients undergoing coronary angiography and in 0.3% of patients undergoing autopsy (Roberts, 1986). CAAs may be classified into those of origin and course, intrinsic coronary arterial anatomy, and coronary termination (Angelini et al. 2002). The most common malformation is abnormal origin and course, origin of a coronary artery from a wrong aortic sinus of Valsalva; either the right from the left coronary sinus or the left from the right coronary sinus; these anomalies must be excluded in young adults with typically ischemic- sounding chest pain or syncope. Anomalies coronary artery termination typically presented as coronary artery fistula, commonly the right coronary artery is affected, although, left sided coronary artery fistulae are well documented (Gandy et al. 2004). The anomalies of intrinsic coronary arterial anatomy, such as ostial stenosis, Artesia, and single, absent, or hypoplastic coronary arteries are rare but may have clinical importance.
Keywords: Coronary artery anomalies, Cardiac CT, Coronary Angiography (AC)
1. Introduction
Coronary Angiography (AC) has traditionally been indicated to detail the coronary vasculature before intervention and has remained the reference standard imaging modality (Scanlon et al. 1999). Owing to the potentially complex three-dimensional natures of these anomalies, CA cannot show reliably the relationship of aberrant vessels with the underlying cardiac structures. These limitations can be overcome by using a non-invasive diagnostic modality that acquires full three-dimensional (3D) data from both the heart cavities and the coronary arteries. Mutidetector CT (MDCT) CA allows rapid acquisition of the entire 3D cardiac volume of data in a Single scan with excellent spatial resolution (Schmitt et al, 2005). MDCT CA is considered to be appropriate indication for patient with suspicious CAA c (Kramer et al. 2007).
To date, the main diagnostic method for the detection of coronary anomalies has been selective CA. CA is invasive associated with risk of ionizing radiation and iodinated contrast. Furthermore, CA cannot delineate the spatial relation between anomalies coronary artery and cardiac structures. Although, MDCT CA is emerging as the best non-invasive test for the diagnosis of CAAs, it has several limitations such as ionizing radiation, iodinated contrast, and significant inferior spatial resolution compared to conventional CA. We report two cases referred for evaluation for suspected CAAs, these two cases will demonstrate the importance of high spatial resolution obtained by CA and 3D cardiac volume data obtained by MDCT CA.
1.1. Case number 1
A 32-year-old male with history of chest pain, mildly impaired left ventricular function. CA revealed mild irregularities of the left main (LMN), Abnormal Left anterior descending artery (LAD) demonstrating ectasia and abnormal network like and sinusoidal appearance of proximal to mid LAD (no luminal continuation to allow wire for intravascular ultrasound- IVUS) with normal caliber distally (Fig. 1A). Owing to very high resolution of CA, fine details of intrinsic lumen of LAD was clearly visualized; we categorized these anomalies as intrinsic coronary artery anomalies. To the best of our knowledge this is first reported case in literature.
Figure 1.
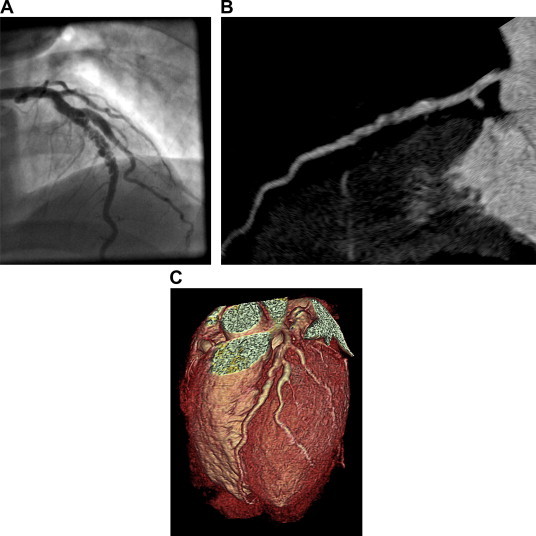
A 32-year-old man with history of chest pain. (A) Coronary angiogram demonstrating ectasia and abnormal network and sinusoidal like appearance of proximal to mid left anterior descending artery (LAD). (B) Maximum intensity projection (MIP) multidetector CT image shows luminal irregularities and noncalcified plaques in corresponding segment of LAD. (C) Three-dimensional volume-rendered (VR) image demonstrating luminal irregularities, but both MIP and VR failed to show the fine details of LAD lesion owing to inferior spatial resolution.
An elective MDCT CA was performed to define the complete anatomy and the morphology of LAD but fails to show fine details of LAD due to inferior spatial resolution compared to CA. The maximum intensity projection (MIP) and Volume rendering (VR) images showed mild non-obstructive plaque in proximal LAD, severe luminal irregularities and positive remodeling of large segment of LAD (Fig. 2B and C).
Figure 2.

A 44-year-old male with history of hypertension, atypical chest pain and nondiagnostic nuclear myocardial perfusion imaging. (A) Three-dimensional volume-rendered (VR) image, and (B) Cardiac transparency multidetector CT image show the left anterior descending artery (LAD), left circumflex artery (LCX), and right coronary artery (RCA) arising from right coronary sinus. LAD coursing anterior to the aortic root, LCX coursing below and behind the aortic root. Both LAD and LCX are not compressed between the aorta and pulmonary artery consistent with benign course RCA course and origin are normal.
1.2. Case number 2
A 44-year-old male with history of hypertension and atypical chest pain underwent nuclear myocardial perfusion imaging (MPI), but was equivocal owing to significant extra cardiac activity adjacent to the inferior wall interfering was perfusion assessment in most of the inferior and inferolateral wall. Subsequently, he was referred to CA. CA revealed the total anomalies of coronary system, and all coronary artery originate from right sinus of Valsalva (CA images not shown). To delineate the coronary artery system course and the relation with cardiac structures MDCT CA was performed. MDCT CA shows that all coronary artery originate from the right sinus of Valsalva and show the entire coronary course in relation to other cardiac structures (Fig. 2A and B).
2. Conclusion
CAAs are a major diagnostic challenge and currently there is no single diagnostic test that could evaluate all anomalies. Although, CA is the most commonly utilized test in patients with suspect CAAs it cannot show reliably the relationship of aberrant vessels with the underlying cardiac structures. ECG-gated MDCT is a non-invasive 3D-imaging technique that provides an excellent overview of the CAAs and complex vascular anatomy in three-dimensional view. We believe that MDCT CA should be the preferred initial diagnostic test for CAAs and CA may be needed in subgroups of patients with suspected intrinsic and luminal abnormalities.
References
- Angelini P., Velasco J., Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation. 2002;105:2449–2454. doi: 10.1161/01.cir.0000016175.49835.57. [DOI] [PubMed] [Google Scholar]
- Gandy K., Rebeiz A., Wang A. Left main coronary artery to pulmonary artery fistula with severe aneurysmal dilatation. Ann. Thorac. Surg. 2004;77:1081–1083. doi: 10.1016/j.athoracsur.2003.05.006. [DOI] [PubMed] [Google Scholar]
- Kramer C.M., Budoff M.J., Fayad Z.A. ACCF/AHA 2007 clinical competence statement on vascular imaging with computed tomography and magnetic resonance. A report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. J. Am. Coll. Cardiol. 2007;50(11):1097–1114. doi: 10.1016/j.jacc.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Roberts W.C. Major anomalies of coronary arterial origin seen in adulthood. Am. Heart J. 1986;111:941–963. doi: 10.1016/0002-8703(86)90646-0. [DOI] [PubMed] [Google Scholar]
- Scanlon P.J., Faxon D.P., Audet A.M. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J. Am. Coll. Cardiol. 1999;33:1756–1824. doi: 10.1016/s0735-1097(99)00126-6. [DOI] [PubMed] [Google Scholar]
- Schmitt R., Froehner S., Brunn J. Congenital anomalies of the coronary arteries: imaging with contrast-enhanced, multidetector computed tomography. Eur. J. Radiol. 2005;15:1110–1121. doi: 10.1007/s00330-005-2707-z. [DOI] [PubMed] [Google Scholar]


