Abstract
Hypertension is one of the most prevalent chronic diseases among older adults, but rates of blood pressure control are low. In this paper, we explore the role of social network ties and network-based resources (e.g., information and support) in hypertension diagnosis and management. We use data from the National Social Life, Health, and Aging Project (NSHAP) to identify older adults with undiagnosed or uncontrolled hypertension. We find that network characteristics and emotional support are associated with hypertension diagnosis and control. Importantly, the risks of undiagnosed and uncontrolled hypertension are lower among those with larger social networks -- if they discuss health issues with their network members. When these lines of communication are closed, network size is associated with greater risk of undiagnosed and uncontrolled hypertension. Health care utilization partially mediates associations with diagnosis, but the benefits of network resources for hypertension control do not seem to stem from health-related behaviors.
Americans are living longer, but they are spending more years with conditions such as diabetes, heart disease, and cancer (Crimmins and Beltran-Sanchez 2010). While some older adults are able to successfully manage these conditions, many remain unaware of their disease, do not follow recommended treatments, or require complex medical regimens. Inadequate management of chronic conditions can lead to a cascade of health problems, significantly increasing hospitalization, care costs (Sokol et al. 2005), and mortality (Rasmussen, Chong, and Alter 2007).
Health care delivery is critical for diagnosis and management of chronic diseases, but its role is limited. Fewer than half of older adults who have been diagnosed with hypertension have controlled blood pressure (Ostchega et al. 2007). The vast majority of those with uncontrolled hypertension have health insurance and regular health care providers (Hyman and Pavlik 2001). And, an intervention study found that even with frequent physician follow-up and free medications, less than 70 percent of hypertensive patients achieve blood pressure control (Cushman et al. 2002). This likely reflects the fact that much of the day-to-day work of managing chronic diseases occurs outside of the clinic walls.
The social context in which disease diagnosis and management takes place may therefore be a critical factor for health trajectories. Consistent with this, a growing body of literature indicates that social connectedness promotes recovery and survival following the advent of health problems (see, e.g., Mookadam and Arthur 2004; Nausheen et al. 2009; Reifman 1995). The benefits of social relationships can be quite striking; Idler and colleagues (2012) recently demonstrated that unmarried patients are nearly twice as likely to die within five years after cardiac surgery. But the mechanisms through which social relationships improve prognosis are not yet well-understood, and the unique contributions of particular types and features of relationships for getting diagnosed and managing chronic conditions have not been fully explicated (DiMatteo 2004; Gallant 2003; Luttik et al. 2005).
This paper examines the contributions of multiple social factors including marriage/partnership, social network characteristics and communication, and instrumental and emotional support to hypertension diagnosis and control among older adults. We pay particular attention to the role of social networks and their functioning. Social networks, which include spouses but reach beyond them, may be important sources of information about disease diagnosis and management (Perry and Pescosolido 2010; Scanfeld, Scanfeld, and Larson 2010), as well as social control and support for healthy behaviors (Umberson 1992; Umberson, Crosnoe, and Reczek 2010). Accordingly, we look for evidence that behaviors associated with hypertension management such as health care utilization, physical activity, and avoidance of alcohol and tobacco serve as mechanisms through which social network resources increase the likelihood of blood pressure control.
Social Relationships and Health in Later Life
A large body of research demonstrates that social relationships are associated with better physical and mental health (see, e.g., Berkman et al. 2000; Smith and Christakis 2008; Thoits 2011; Umberson et al. 2010; York Cornwell and Waite 2009). There are several reasons for this. Having a larger or more diverse social network seems to boost self-esteem, which brings downstream benefits in the form of reduced physiological reactivity or enhanced immune function (Hawkley and Cacioppo 2010; Steptoe et al. 2003). And when network ties provide access to resources such as information and social support, they can also shape health-related behaviors and buffer responses to stress (Thoits 2011). This is particularly important in later life, which is often characterized by a number of stressful transitions such as retirement, bereavement, and the advent of health problems.
Social networks and support are also important for recovery and survival following the onset of illness or adverse health events (for reviews, see Lett et al. 2005; Luttik et al. 2005; Molloy et al. 2008a; Mookadam and Arthur 2004; Nausheen et al. 2009; Reifman 1995). But most research does not explicitly distinguish between the roles of social connectedness in processes of disease onset, diagnosis, and management. This is an important consideration because different aspects of social relationships may bring unique benefits (or liabilities) at different stages of the disease process. For example, there is some evidence that support may be more closely associated with disease prognosis than with disease incidence (Antonucci and Johnson 1994; Barth, Schneider, and von Kanel 2010).
Specific attention to the role of social relationships in disease management is badly needed because later life is often marked by the onset of chronic illness (Crimmins and Beltran-Sanchez 2010). Multiple morbidities can make the management of chronic conditions particularly challenging for older adults. Depression, cognitive impairment, and functional impairments (e.g., vision loss) are common in later life and can impede medication adherence and lifestyle changes associated with disease management (Insel et al. 2006). As a result, support and assistance from close others can be critical factors in disease management among older adults.
Assessments of previous research on the role of social relationships in disease management point to two important gaps. First, inconsistent and limited measures of social relationships make it difficult to identify the distinct contributions of social network characteristics and particular types of support (Barth et al. 2010; Lett et al. 2005). For example, some studies assess support based on a single-item indicator of living alone or having a spouse/partner (Luttik et al. 2005: 167–168), but neither of these conditions necessarily indicates the availability (or lack) of support (York Cornwell and Waite 2009). And few studies consider multiple types of support. In a meta-analysis, DiMatteo (2004) found that only 5 of 122 studies examined more than one form of support in medication adherence, although practical support brings different benefits than emotional support and the two are not always strongly correlated (Wethington and Kessler 1986). Second, the mechanisms through which social relationships and support affect disease outcomes are not well-understood (Gallant 2003:188; Lett et al. 2005; Reifman 1995:128). Some aspects of relationships may play a unique role in early diagnosis, while others may enhance or impede post-diagnosis efforts to manage medications, comply with treatment regimens, and make lifestyle changes. This paper elaborates how social networks provide access to information and forms of support that may affect the diagnosis and management of chronic conditions such as hypertension.
Hypertension Diagnosis and Management as a Function of Social Relationships
We focus on hypertension for two reasons. First, about two-thirds of older adults have hypertension, yet rates of management are relatively low. Roughly a quarter of those with hypertension are unaware of their condition and more than half are uncontrolled. Rates of uncontrolled hypertension are even higher among African-American older adults (Ostchega et al. 2007). Having elevated blood pressure takes a toll on the body, putting individuals at increased risk for cardiovascular disease, as well as heart attack, heart failure, stroke, and kidney disease (NHLBI 2003). Therefore, improving hypertension management can have a substantial effect on health trajectories for a large segment of the elderly population.
Second, there are reasons to believe that social context may play a particularly important role in the diagnosis and management of hypertension. Since hypertension is commonly asymptomatic, individuals are unlikely to seek treatment because of discomfort or declining function. Therefore, factors that encourage individuals to undergo preventative screenings are critical. Once diagnosed, management of hypertension involves substantial daily effort including multiple anti-hypertensive medications, weight reduction, and changes in physical activity, diet, and alcohol and tobacco use (NHLBI 2003). Social network ties and network-based resources such as support may promote or impede these behaviors. Below we draw from previous research to describe how particular types and aspects of network ties may shape hypertension diagnosis and management.
Marriage/Partnership
Married individuals may be particularly advantaged with regard to hypertension diagnosis. First, people who are married have higher incomes, are more likely to have health insurance, and tend to use better hospitals (Iwashyna and Christakis 2003; Montez, Angel, and Angel 2009). Medicare eligibility in later life diminishes disparities in access to health care, but there is evidence that marriage promotes health care utilization such as preventative screenings (Stimpson and Wilson 2009), particularly among men (McFall and Davila 2008). Perhaps as a result, those who are married tend to get diagnosed with health problems sooner and have better prognoses after disease onset (Reyes Ortiz et al. 2007).
Close daily contact with a spouse or partner makes him or her well-positioned to influence health habits. Through direct social control -- persuading, monitoring, reminding, or threatening -- spouses can encourage each other to adopt health-promoting behaviors (Lewis and Rook 1999; Umberson 1987). Spouses can also provide assistance with things like medication management and diet changes (Gallant, Spitze, and Prohaska 2007) and encourage lifestyle changes like smoking cessation and weight loss (Gorin, Wing, and al. 2008). Women are more likely to make efforts to control their partners’ health, so married men may benefit more with respect to disease management (Umberson 1992; Westmaas, Wild, and Ferrence 2002). But spousal social control can also increase both psychological distress and physiological symptoms, particularly among men (August and Sorkin 2010; Helgeson et al. 2004). Marital stress may also have detrimental effects -- lowering medication adherence, increasing health risk behaviors, and leading to physiological dysregulation (Molloy et al. 2008c; Robles and Kiecolt-Glaser 2003), particularly among women (Kiecolt-Glaser and Newton 2001).
We hypothesize that married individuals will generally be less likely to have undiagnosed or uncontrolled hypertension, due in part to greater utilization of health care and health-promoting behaviors. Previous research indicates that the net benefits of marriage may be greater for men (Goldman, Korenman, and Weinstein 1995; Lillard and Waite 1995). Thus, we expect that marriage is associated with larger reductions in the risk of undiagnosed and uncontrolled hypertension among men.
Social Networks and Network-Based Health Communication
Social networks include, but extend beyond, one’s spouse. One’s network can involve a variety of different types of linkages with a diverse set of individuals (Smith and Christakis 2008). Longitudinal studies provide strong evidence that following the onset of a health problem, individuals with larger and more diverse networks have lower rates of subsequent hospitalization (Mookadam and Arthur 2004), disease progression (Nausheen et al. 2009), and mortality (Brummett et al. 2001). One possibility is that the greater self-esteem, sense of belonging, and perceived control that are associated with larger social networks (Cohen 1988; Cornman et al. 2003) increase success with disease management. Like one’s spouse, network members may also encourage health-promoting behaviors, health care utilization, and medication adherence through social control (Kinney et al. 2005; Molloy et al. 2008c), although negative health behaviors can also be transmitted through social networks (e.g., Christakis and Fowler 2007). And some studies have found negative associations between network size and disease management (e.g., Kaplan and Hartwell 1987), which may reflect social obligations and responsibilities that take time away from self-care.
Other characteristics of one’s social network may also shape disease diagnosis and management. Stronger network ties – as measured by frequency of interaction and emotional closeness – buffer physiological responses to stress (Cohen and Williamson 1991) and reduce feelings of loneliness which can give rise to physiological dysregulation such as inflammation and elevated blood pressure (Cacioppo, Hawkley, and Berntson 2003; Steptoe et al. 2003). Stronger ties and more frequent interaction also imply greater opportunities to monitor or influence health behaviors.
Interactions with network members that involve discussions about health may be particularly efficacious for disease diagnosis and management. Network ties can serve as a conduit for information (Berkman et al. 2000), particularly regarding health-related issues (see, e.g., Kinney et al. 2005; Perry and Pescosolido 2010). Research on health communication, for example, indicates that “storytelling” about health experiences increases health knowledge within local networks (Kim et al. 2011) and families (Warren-Findlow, Seymour, and Shenk 2010). Peccioni and Sparks (2007) find that many cancer patients turn first to family members and close friends for information following diagnosis, and they report greatest satisfaction with the health information obtained through these sources -- perhaps because their relationships tend to be imbued with trust and intimacy. These types of health-related discussions may also constitute key mechanisms through which family and friends attempt to control health behaviors.
We therefore hypothesize that older adults who have larger social networks, stronger relationships with network members (as indicated by more frequent interaction), and more network-based discussions about health are less likely to have undiagnosed or uncontrolled hypertension. We expect that these associations are due in part to greater health care utilization and more health-promoting behaviors among those who have more network resources.
Social Support
Social networks can also be beneficial for disease diagnosis by providing access to social support. However, not all network ties are supportive. This distinction has led some researchers to caution against using social network connectedness as a proxy for support (Smith and Christakis 2008; Stoller and Pugliesi 1991; Wellman and Wortley 1990). Close social relationships and strong ties are most likely to bring access to various forms of support or assistance (Seeman and Berkman 1988).
We focus on two types of social support. Instrumental support involves help or material assistance with practical tasks or problems (Thoits 2011). Family and friends may help to locate a physician, make an appointment, and provide transportation (Boutin-Foster 2005) – all of which may bring earlier diagnosis. Accordingly, instrumental support is associated with better medication adherence and rehabilitation attendance (Gallant et al. 2007; Molloy et al. 2008b). The provision of healthy foods and assistance with other lifestyle changes such as increasing physical activity can create a context that promotes disease management (Boutin-Foster 2005; Rosland and Piette 2010).
But several studies suggest that emotional support may be even more important than instrumental support for individuals coping with health problems (see, e.g., Berkman, Leo-Summers, and Horwitz 1992; Luttik et al. 2005; Seeman and Chen 2002). Expressions of love, caring, concern, and affection buffer stress and enhance one’s self-esteem (Thoits 2011), which may reduce physiological reactivity, such as inflammation and blood pressure variation, and lead to better disease outcomes (Uchino 2006). Emotional support may also reduce risky health behaviors, such as smoking and drinking, as a way of coping with stress (Umberson et al. 2010).
Thus, we hypothesize that both instrumental and emotional support are associated with lower risk of undiagnosed and unmanaged hypertension. We will examine support from family and friends separately, since family members are more likely to provide instrumental support for older adults, but emotional support from friends is particularly beneficial for well-being in later life (Adams and Blieszner 1995; Fiori, Antonucci, and Cortina 2006). Previous work also suggests that the relationship between support and disease management may be more pronounced among women (Jackson 2006), so we test for gender differences in these associations. We also expect that health care utilization and other health-related behaviors partially mediate the association between support and hypertension.
Data and Methods
We use data from the National Social Life, Health, and Aging Project (NSHAP), a nationally representative population-based study of community-residing older adults. From summer 2005 to spring 2006, NSHAP interviewed 3,005 individuals, ages 57–85, achieving a final weighted response rate of 75.5 percent (O’Muircheartaigh, Eckman, and Smith 2009).
Most of the data for the NSHAP study were collected during a two-hour in-home interview. Respondents were also given a leave-behind questionnaire (LBQ) to return by mail. The return rate for the LBQ was 84 percent. The NSHAP study was modularized, so that some questionnaire items were always included in the in-person questionnaire, while other items were included in either the in-person interview or the LBQ for a randomly-selected subset of respondents (see Smith et al. 2009). All of our measures are drawn from the in-person interview except as noted below.
Dependent Variable: Hypertension Awareness and Management
We combine self-reported and biological measures to assess hypertension diagnosis and control. Respondents reported whether a medical doctor had ever told them that they have high blood pressure or hypertension. In addition, each respondent completed two seated blood pressure measures on the left arm, using a Lifesource digital blood pressure monitor (Model UA-767PVL). If the two readings differed by more than 20 mmHg systolic or 14 mmHg diastolic, interviewers collected a third blood pressure reading. Respondents whose mean blood pressure (based on all readings taken) exceeded either 140 mmHg systolic or 90 mmHg diastolic are considered hypertensive. We use lower cutoffs of either 130 mmHg systolic or 90 mmHg diastolic for respondents who reported that they have been diagnosed with diabetes (NHLBI 2003).
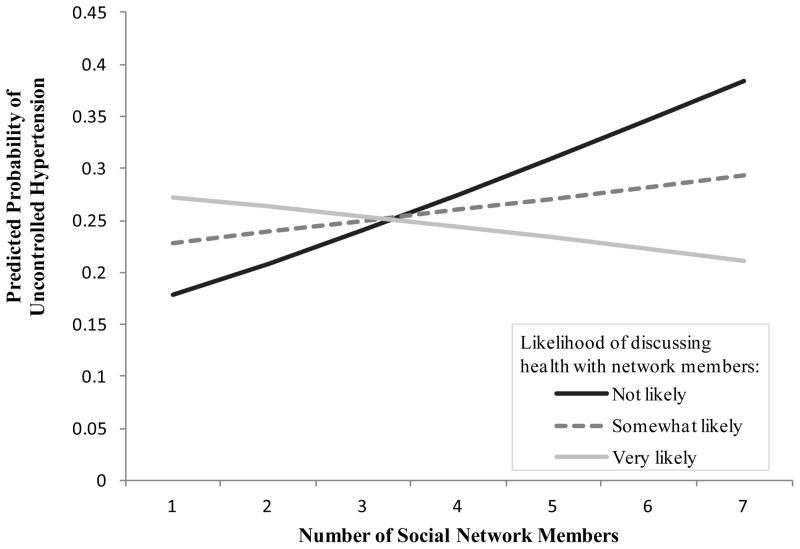
Based on self-reported hypertension and blood pressure, we place each respondent into one of four categories. The distribution is shown in Figure 1. Note that the modal category is uncontrolled hypertension and about half of the older adults in our sample have undiagnosed or uncontrolled hypertension.
Figure 1. Hypertension Categories Derived from Self-Report and Blood Pressure.
a Individuals who had been diagnosed with diabetes or suffered kidney problems were considered to have high blood pressure if their pressure exceeded 130/80.
Social Network Resources
NSHAP collected egocentric network data by asking respondents to list people with whom they most often discussed things that were important to them over the last 12 months (see Cornwell et al. 2009). Each respondent was permitted to name up to five network members. Then, the respondent’s spouse or romantic partner was added to the network if he/she was not already identified. Finally, respondents were asked if they wanted to add anyone else who is very important or especially close. The maximum network size is therefore 7.
Follow-up questions assessed the respondent’s frequency of interaction and likelihood of discussing health matters with network members. We aggregate both of these measures across all network members to gain a general sense of the strength of the respondent’s relationships with his or her network members and the potential for the respondent’s network to assist with disease management or provide health-relevant information. Table 1 provides further details on the construction of these measures and other key variables used in our analyses.
Table 1.
Descriptions and Summary Statistics for Key Variables (n = 2,658)
| Variable | Weighted Mean or Proportiona | SD | |
|---|---|---|---|
| Social Connectedness and Support | |||
| Co-resident partner | Whether R has a spouse or co-resident partner (yes = 1, no = 0) | .721 | .449 |
| Social network size | Number of people listed in the R’s network roster (range = 1, 7)b | 4.192 | 1.588 |
| Network interaction | Rs were asked how often they talk with each network member, from “less than once a year” to “every day.” We recode these to represent the number of times per year that interaction occurs, and then average the values across all network members (range = 0, 365) | 205.346 | 86.295 |
| Network-based health discussion | Rs were asked how likely they are to discuss a health problem or medical medical treatment with each network member: “not likely” (1), “somewhat likely” (2), or “very likely” (3). We average these values across all network members (range = 1, 3) | 2.567 | .442 |
| Instrumental support | R can “sometimes” or “often” rely on… | ||
| Family members (yes = 1, no = 0) | .907 | --- | |
| Friends (yes = 1, no = 0) | .820 | --- | |
| Emotional support | R can “sometimes” or “often” open up to… | ||
| Family members (yes = 1, no = 0) | .854 | --- | |
| Friends (yes = 1, no = 0) | .717 | --- | |
| Health-Related Behaviors | |||
| Anti-hypertensive medication use | R takes a cardiovascular agent such as an ACE inhibitor, beta-blocker, diuretic, calcium channel blocker, or peripheral vasodilator (yes = 1, no = 0) | .625 | --- |
| Alcoholic drinks | Rs were asked how many days per week they drank alcohol during the past 3 months, and how many drinks they typically consumed. We calculate drinks per week as days*drinks (range = 0, 140) | 3.307 | 6.992 |
| Cigarette use | R currently smokes cigarettes (yes = 1, no = 0) | .146 | --- |
| Body Mass Index (BMI) | Set of variables representing R’s body mass index (BMI): | ||
| Normal or underweight (BMI < 25) | .253 | ||
| Overweight (25 ≤ BMI < 30) | .371 | ||
| Obese (30 ≤ BMI < 40) | .322 | ||
| Morbidly obese (BMI ≥ 40) | .054 | ||
| Physical activity | Whether R participates in physical activities such as walking, dancing, gardening, exercise, or sports ≥ 3 times per week (yes = 1, no = 0) | .618 | --- |
Means are survey-adjusted and weighted to account for probability of selection, with post-stratification adjustments for non-response. Proportions are unadjusted and unweighted.
NSHAP assessed respondents’ instrumental social support by asking how often, if they have a problem, they can rely on family members for help and how often they can rely on friends for help. To capture emotional support, respondents were asked how often they can open up to family members and how often they can open up to friends they need to talk about their worries. Responses for all four questions ranged from “hardly ever (or never)” to “some of the time” and “often.” In supplemental analyses, we have examined the relevance of the availability, frequency, and diversity of sources of support. Of these, only the availability of support was associated with our dependent variable. Because it provides the most parsimonious representation of the relationship between support and hypertension, we utilize indicators of whether the respondent can access instrumental or emotional support from friends or family members “some of the time” or “often” (= 1, else = 0). These support questions were modularized so that a randomly-selected subset of NSHAP respondents (763 of the respondents included in our analyses) answered these questions on the LBQ.
Health-Related Behaviors and Covariates
We consider four indicators of health-related behaviors. The respondent’s use of anti-hypertensive medications comes from the NSHAP medication log, in which respondents listed all of the medications that they take regularly (Qato et al. 2009). We are unable to assess whether respondents are taking their medications on schedule, so this serves only as an indicator of health care utilization.
We consider three health-related behaviors that are typically included in recommended lifestyle changes for individuals diagnosed with hypertension: cigarette use, alcohol consumption, and physical activity. In addition, we consider body mass index (BMI) since being overweight is a risk factor for hypertension, and weight loss may be included in physicians’ recommendations for hypertension management. BMI was calculated from the respondent’s measured height and weight. For 134 respondents who had missing data, we impute BMI based on interviewer assessments of obesity. Results from analyses excluding respondents who had missing data on BMI do not appreciably differ from those presented here.
We account for aspects of respondents’ health that may impact the likelihood of hypertension diagnosis and management, including an indicator of whether the respondent has diabetes and a count of other co-morbidities. We also control for sociodemographic characteristics, including age, gender, race/ethnicity, educational attainment, and health insurance. Descriptive statistics for these variables are provided in Table A1 in the online appendix.
Analytic Strategy
We use multinomial logistic regression models to simultaneously estimate binary comparisons among the categories of the dependent variable: normal (non-hypertensive), controlled hypertensive, undiagnosed hypertensive, and uncontrolled hypertensive. Because we are most interested in the role of social network resources in disease diagnosis and management, we use controlled hypertensive as our base category. This allows us to directly compare respondents who are undiagnosed vs. controlled hypertensive, and to compare respondents who are uncontrolled vs. controlled hypertensive. We present results in terms of relative risk ratios (i.e., exponentiated coefficients). These are estimates of the change in the relative risk of being in a particular hypertensive category rather than the base category (controlled) that is associated with a unit change in the predictor variable, net of other variables in the model.
Our analyses exclude 71 respondents who refused or were unable to have their blood pressure taken. Listwise deletion leads us to drop an additional 158 respondents who were randomly assigned to be asked about social support on the LBQ but did not return the questionnaire. We also exclude 15 respondents who did not name any social network members and thus have no data on network characteristics. Other respondents drop out due to item-level missing data on social support (n = 65), medications (n = 17), race/ethnicity (n = 11), alcohol use (n = 5), physical activity (n = 3), obesity (n = 1), and network interaction (n = 1). Therefore, our analyses include 2,658 respondents.
All models are adjusted for design effects resulting from NSHAP’s multi-stage sampling procedure. Variance estimates are adjusted for strata and Primary Sampling Units. Our models incorporate person-level weights that account for differential probabilities of selection into the study (with post-stratification adjustments for non-response). We adjust these using a complete-case weighting procedure to attenuate selection effects that may be caused by the exclusion of respondents who had missing data (Morgan and Todd 2008). This affords disproportionate weight to cases that are least likely to be included in the models.
Results
Below we present results from multinomial logistic regression models predicting the relative likelihood of being non-hypertensive, undiagnosed hypertensive, or uncontrolled hypertensive (compared to the base category of controlled hypertensive). Because we are most concerned with the role of social network resources following disease onset, we focus on the risks of undiagnosed and uncontrolled hypertension. Risk ratios for non-hypertension (vs. controlled hypertension) are not included in the tables presented here, but they can be found in Table A2 in the online appendix.
The first model in Table 2 presents the relative risks of undiagnosed and uncontrolled hypertension according to marriage/partnership and social network characteristics. Contrary to our hypothesis, having a co-resident partner is not associated with lower risk of undiagnosed (compared to controlled) hypertension or uncontrolled (compared to controlled) hypertension. However, it is worth noting that partnered older adults are more likely to be non-hypertensive than unpartnered adults. As shown in the online appendix (Table A2, Model 1), partnered individuals are 78 percent more likely to be non-hypertensive compared to controlled hypertensive (RR = 1.780, p < .001). Supplemental analyses indicate that they are also more likely to be non-hypertensive compared to undiagnosed (RR = 1.680, p < .01) or uncontrolled hypertensive (RR = 1.886, p < .001). We also find no evidence that marriage brings greater health benefits for men. When added to the first model presented in Table 1, an interaction term crossing female gender with marriage/partnership was non-significant for non-hypertensive (RR = 1.102; p = .581), undiagnosed hypertension (RR = .865; p = .440), and uncontrolled hypertension (RR = 1.001; p = .994).
Table 2.
Multinomial Logistic Models Predicting Undiagnosed and Uncontrolled Hypertension
| Model 1
|
Model 2
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Undiagnosed
|
Uncontrolled
|
Undiagnosed
|
Uncontrolled
|
|||||
| RRR | (SE) | RRR | (SE) | RRR | (SE) | RRR | (SE) | |
| Co-resident partner | 1.059 | (.167) | .944 | (.125) | 1.028 | (.164) | .930 | (.123) |
| Social network size | 1.471* | (.247) | 1.588* | (.292) | 1.500* | (.258) | 1.634* | (.303) |
| Frequency of network interaction | .997** | (.001) | 1.000 | (.001) | .998** | (.001) | 1.001 | (.001) |
| Network-based health discussion | 1.916* | (.597) | 1.712 | (.480) | 2.074* | (.657) | 1.832* | (.530) |
| Network size * Health discussion | .844* | (.055) | .833** | (.055) | .851* | (.056) | .835** | (.055) |
| Instrumental support from family | 1.430 | (.358) | .927 | (.261) | ||||
| Instrumental support from friends | 1.119 | (.278) | 1.027 | (.191) | ||||
| Emotional support from family | .524* | (.133) | .898 | (.190) | ||||
| Emotional support from friends | .690 | (.145) | .670* | (.130) | ||||
| Change in −2 log-likelihood (df) | 103.690*** (18) | 36.314*** (12) | ||||||
| Unweighted N | 2,658 | 2,658 | ||||||
Note: Controlled hypertensive is the base category for all models. The number of blood pressure readings is included but not shown. Estimates presented are survey-adjusted and weighted for the possibility of selection, with post-stratification adjustments for non-response.
p < .05;
p < .01;
p < .001 (two-tailed tests)
We do find evidence consistent with our hypothesis that aspects of social networks are associated with hypertension diagnosis and management. As shown in Model 1, older adults who spend more days per year with their network members have lower risk of undiagnosed hypertension. However, frequency of network interaction is not associated with lower risk of uncontrolled hypertension.
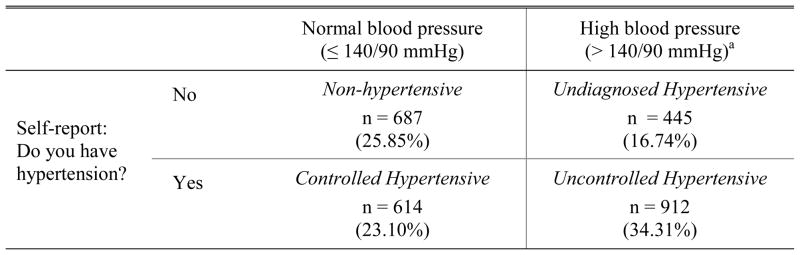
We also find that social networks are particularly beneficial for disease management when they provide access to health-relevant information. The significant interaction term crossing network size with network-based health communication indicates that the association between network size and undiagnosed hypertension varies according to the likelihood of health discussions. A similar pattern is observed with respect to uncontrolled hypertension.
Figure 2 depicts this pattern by showing predicted probabilities of uncontrolled hypertension calculated from Model 1. We allow network size to vary from 1 to 7 and utilize values for network-based health discussions that correspond with the original question: 1 indicates that the respondent is “very unlikely” to discuss health with his network members; 2 indicates that he is “somewhat likely” to discuss health; and 3 indicates that he is “very likely” to discuss health. Frequency of network interaction is fixed at its mean and co-resident partner is fixed at the modal response (i.e., respondent has a co-resident partner). The predicted probabilities illustrate that those who have larger networks have lower risk of uncontrolled hypertension – provided that they are very likely to discuss health problems with their network members. For those who are less likely to talk about health problems with their family and friends, the risk of unmanaged hypertension increases as network size increases.
Figure 2.
Predicted Probability of Uncontrolled Hypertension, According to Network Size and Discussion of Health
Results for social support are mixed. As shown in Model 2, instrumental support is not associated with hypertension diagnosis or control. However, emotional support is associated with lower risk of undiagnosed and uncontrolled hypertension. Specifically, older adults who can open up to family members are nearly 50% less likely to have undiagnosed (compared to controlled) hypertension. And those who can open up to friends are about a third less likely to have uncontrolled (compared to controlled) hypertension. There is also some evidence that emotional support from friends may play a role in hypertension diagnosis; the relative risk ratio for undiagnosed hypertension is nearly significant (RR = .690; p = .084). We expected that support may be particularly beneficial for women, but interaction terms crossing gender with instrumental and emotional support (in supplemental analyses) are not significant.
Note that relative risk ratios for network size, frequency of interaction, health discussion, and the interaction term crossing network size with health discussion do not significantly change with the inclusion of the social support variables. Further, network-based discussions of health are associated with lower risk of undiagnosed and uncontrolled hypertension, regardless of access to instrumental or emotional support. This highlights the fact that network characteristics and support play distinct roles in the process of disease management.
Table 3 introduces several additional variables to account for respondent characteristics and test whether health behaviors may be a mechanism through which social network resources are associated with hypertension diagnosis and management. The first model incorporates sociodemographic characteristics and health status. We find that the risk of undiagnosed hypertension decreases with age, but gender, education, and health insurance are not associated with undiagnosed or uncontrolled hypertension. Blacks are less likely than whites to be undiagnosed hypertensive, while Hispanics are less likely than whites to be uncontrolled hypertensive. The findings with respect to race/ethnicity run contrary to epidemiological research which has indicated that African-Americans face disproportionately high risk of uncontrolled hypertension (Hertz, Unger, et al. 2005). However, we find evidence that blacks are significantly less likely than whites to be non-hypertensive (RR = .466, p < .001 in online appendix Table A2, Model 4).
Table 3.
Multinomial Logistic Models Predicting Undiagnosed and Uncontrolled Hypertension, adjusted for Sociodemographic Characteristics, Health Status, and Health-Related Behaviors
| Model 1
|
Model 2
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Undiagnosed
|
Uncontrolled
|
Undiagnosed
|
Uncontrolled
|
|||||
| RRR | (SE) | RRR | (SE) | RRR | (SE) | RRR | (SE) | |
| Co-resident partner | .849 | (.129) | .913 | (.127) | .930 | (.169) | .905 | (.123) |
| Social network size | 1.476* | (.249) | 1.667* | (.344) | 1.227 | (.254) | 1.697* | (.362) |
| Frequency of network interaction | .998** | (.001) | 1.000 | (.001) | .999 | (.001) | 1.000 | (.001) |
| Network-based health discussion | 2.080* | (.648) | 1.885* | (.559) | 1.304 | (.520) | 1.901* | (.574) |
| Network size * Health discussion | .855* | (.056) | .826* | (.062) | .935 | (.075) | .823* | (.823) |
| Instrumental support from family | 1.519 | (.408) | .995 | (.279) | 1.490 | (.572) | .961 | (.274) |
| Instrumental support from friends | .984 | (.249) | 1.040 | (.208) | .972 | (.274) | 1.027 | (.205) |
| Emotional support from family | .511* | (.132) | .889 | (.193) | .578 | (.174) | .937 | (.205) |
| Emotional support from friends | .659* | (.136) | .656* | (.129) | .642 | (.171) | .644* | (.126) |
| Age (in decades) | .735** | (.067) | .898 | (.074) | 1.235 | (.145) | .960 | (.087) |
| Female | 1.093 | (.186) | 1.116 | (.138) | 1.121 | (.229) | 1.184 | (.155) |
| Race/ethnicity | ||||||||
| Black | .506** | (.110) | .841 | (.167) | .524* | (.143) | .908 | (.168) |
| Hispanic, non-black | .614 | (.172) | .603* | (.141) | .431* | (.169) | .579* | (.146) |
| White or Other (ref. ) | --- | --- | --- | --- | ||||
| Education | ||||||||
| Less than high school | .999 | (.218) | 1.061 | (.205) | .966 | (.222) | 1.074 | (.215) |
| High school diploma | 1.025 | (.228) | 1.015 | (.120) | 1.038 | (.290) | 1.039 | (.203) |
| Some college | 1.092 | (.220) | .905 | (.167) | .989 | (.262) | .884 | (.166) |
| Bachelor’s degree or higher (ref. ) | --- | --- | --- | --- | ||||
| Health insurance | 1.147 | (.280) | .757 | (.124) | 1.390 | (.389) | .759 | (.129) |
| Diabetes | 1.006 | (.186) | 2.462*** | (.393) | 2.866*** | (.629) | 2.864*** | (.462) |
| Other co-morbidities | .732*** | (.057) | .919 | (.039) | .843 | (.079) | .928 | (.042) |
| Anti-hypertensive medication use | .012*** | (.003) | .378*** | (.072) | ||||
| Alcoholic drinks | 1.023 | (.014) | 1.028* | (.013) | ||||
| Cigarette use | 1.356 | (.440) | .798 | (.151) | ||||
| Body Mass Index | ||||||||
| Normal or underweight (ref. ) | --- | --- | ||||||
| Overweight | .954 | (.234) | 1.108 | (.182) | ||||
| Obese | 1.178 | (.270) | 1.062 | (.179) | ||||
| Morbidly obese | .894 | (.336) | .835 | (.218) | ||||
| Physical activity | 1.211 | (.264) | .900 | (.119) | ||||
| Change in −2 log-likelihood (df) | 371.109*** (30) | 1,381.049*** (21) | ||||||
| Unweighted N | 2,658 | 2,658 | ||||||
Note: Controlled hypertensive is the base category for all models. The number of blood pressure readings is included but not shown. Estimates presented are survey-adjusted and weighted for the possibility of selection, with post-stratification adjustments for non-response.
p < .05;
p < .01;
p < .001 (two-tailed tests)
With respect to health status, diabetics are more likely to have uncontrolled hypertension. But those who have other conditions are less likely to be undiagnosed hypertensive and they may also be less likely to have uncontrolled hypertension (RR = .919, p = .053), perhaps because they see a health provider more frequently. The associations between network characteristics, social support and hypertension are largely unchanged with the inclusion of these control variables.
Health Care Utilization and Health-Related Behaviors as Mechanisms
Finally, we consider health-related behaviors as a possible mechanism through which social network resources may decrease the risk of undiagnosed or uncontrolled hypertension. In Model 2 of Table 3, we find that individuals who use anti-hypertensive medications are less likely to be undiagnosed -- which makes sense because they would have received these medications from a physician. The inclusion of this variable alone (shown in the online appendix Table A2, Model 5) reduces to non-significance the associations between undiagnosed hypertension and network size, frequency of interaction, network-based health discussions, and emotional support from family and friends. This suggests that older adults who have larger networks with more discussion of health, more frequent network interactions, and access to emotional support from family and friends are less likely to have undiagnosed hypertension in part because they are more likely to utilize health care, which increases the chances that underlying hypertension is diagnosed. Consistent with this idea, in supplemental analyses we find that more frequent network interaction, more network-based discussions of health, and emotional support from one’s family are significantly associated with anti-hypertensive medication use (among older adults who are not in the non-hypertensive category).
Older adults who take anti-hypertensive medications are also less likely to be uncontrolled (compared to controlled) hypertensive, as we would expect. But the inclusion of anti-hypertensive medications in the model does not reduce the associations between social network resources and uncontrolled hypertension. Therefore, while health care utilization may serve as a mechanism through which network resources and support reduce the risk of undiagnosed hypertension, we find no evidence of this with respect to uncontrolled hypertension.
Of the health-related behaviors we examine, only alcohol consumption is associated with uncontrolled hypertension. Note that we do not observe marked reductions in the significance or magnitude of the risk ratios for undiagnosed and uncontrolled hypertension associated with social network characteristics and social support when we account for health-related behaviors. (See the online appendix, Table A2, Models 5 and 6.) Therefore, we find no support for our hypothesis that health-related behaviors are a mechanism through which social network resources and support are associated with lower risk of undiagnosed or uncontrolled hypertension.
Discussion
Most older adults do -- or will -- suffer from hypertension. Even those who have normal blood pressure at mid-life have a 90 percent risk of developing hypertension during their lifetime (Vasan et al. 2002). Yet rates of diagnosis and control are relatively low. Therefore, in this paper we move beyond a focus on predictors of disease onset to explore how social context shapes diagnosis and management. We find that the risk of undiagnosed and uncontrolled hypertension is structured by social network resources including interaction, information, and emotional support.
We had anticipated that having a spouse or partner reduces the risk of undiagnosed or uncontrolled hypertension, but we did not find any evidence of this. Our results indicate that partnership may protect against hypertension onset, which is consistent with previous research showing that married individuals have lower rates of a number of chronic conditions including hypertension (e.g., Pienta, Hayward, and Jenkins 2000). But we find that having a spouse/partner is not associated with lower risk that one’s hypertension will be undiagnosed or uncontrolled. One possibility worth further exploration is that spouses may play a less active role in the management of chronic and asymptomatic conditions such as hypertension. There is some evidence that spouses may be most beneficial when they take a “crisis caregiver” role when their partner suffers acute illness or pain, and in the time period immediately following disease diagnosis or surgical procedures (see, e.g., Idler et al. 2012:46).
Furthermore, we find that marriage/partnership does not play a different role in hypertension for men compared to women. This counters some previous research suggesting that partnership brings greater health benefits for men (Goldman et al. 1995; Lillard and Waite 1995). A closer look at partnership characteristics such as relationship quality and supportiveness is an important next step. It is possible that close and supportive partnerships have a positive impact on disease diagnosis and management while those that are more distant or conflicted are detrimental. It is also likely that gender differences stem from characteristics of partner relationships, rather than simply from partnership status. For example, women with more stressful or less supportive partnerships may be particularly disadvantaged in disease management (Kiecolt-Glaser and Newton 2001).
Our results indicate that several aspects of social networks and the resources they may bring are critical for disease diagnosis and management. For one thing, emotional support from family and friends is associated with lower risk of undiagnosed hypertension. This is consistent with previous research pointing to the particular importance of emotional support following disease onset (e.g., Antonucci and Johnson 1994; Barth et al. 2010), and it highlights the distinctions between social network characteristics and the availability of support. Our findings indicate that regardless of network size, network interaction, and network-based health discussions, older adults who feel that they can reach out to family and friends for emotional support are more likely to have their underlying hypertension diagnosed. Emotional support from friends also reduces the risk of uncontrolled hypertension. The unique role of support from friends for disease control is consistent with a rather large literature pointing to the greater importance of friendship ties for older adults’ psychological well-being (e.g., Adams and Blieszner 1995; Fiori et al. 2006).
Our results also suggest that social networks play an important role in disease diagnosis and management. Regardless of network size, older adults who interact more frequently with their network members are less likely to have undiagnosed hypertension. This may be due to greater monitoring and control that are afforded by more frequent interaction; we find some evidence that this association is mediated by health care utilization.
The most intriguing finding here relates to the discussion of health-related issues with network members. Older adults who have larger social networks – and are likely to talk with their network members about health problems – have lower risks of undiagnosed and uncontrolled hypertension. These individuals may benefit from others’ advice, experiences, and expertise regarding accessing health care, getting preventative screenings, and managing disease (Perry and Pescosolido 2010; Warren-Findlow et al. 2010). But for those who are unlikely to communicate about health, the risk of undiagnosed and uncontrolled hypertension increases with network size. This is an important finding because it contradicts the general assumption that having more social relationships is always beneficial. Our results suggest that when lines of communication about health are closed, relationships may present more costs than benefits. A lack of communication about health may indicate that network ties are tense, conflicted, or demanding, and therefore bring additional stress for those suffering from chronic conditions (Seeman and Chen 2002).
We found evidence that emotional support, more frequent interaction with network members, and network-based discussions of health may increase health care utilization leading to less risk of undiagnosed hypertension. But the mechanisms through which social relationships shape disease management remain a puzzle (Reifman 1995). We did not find support for the idea that network resources reduce the risk of uncontrolled hypertension through behavioral pathways. However, we are not able to assess whether emotional support and health-related communication with friends and family members enhance medication adherence or changes in health behaviors, which has been suggested by previous research (DiMatteo 2004; Gallant et al. 2007; Trivedi et al. 2008). Even so, not all efforts to manage hypertension through lifestyle changes lead to blood pressure control. We have also been unable to explore whether older adults with greater social resources benefit from stress buffering and reduced physiological dysregulation (Hawkley and Cacioppo 2010; Steptoe et al. 2003), which may increase the likelihood of blood pressure control. Detailed data that link disease etiology, the process of disease management, and social relationships are needed to disentangle these possible mechanisms.
We intend this paper as an initial step toward the identification of social factors that impact disease management among older adults. The cross-sectional nature of our data and the breadth rather than depth in our measures of social integration leave a number of questions unanswered. We know that networks tend to change as adults age, with especially large differences at the oldest ages (Ajrouch, Antonucci, and Janevic 2001; Cornwell, Laumann, and Schumm 2008). Changes in health are certainly responsible, at least in part, because functional limitations and declining sensory function may make socializing more difficult (Cornwell 2009). Thus, differences in network resources that we observe may stem from health, muddying causal direction. Hypertension has no symptoms that could lead to declines in social relationships, but individuals who have been diagnosed with hypertension may be more likely to speak to network members about health, since the diagnosis raises a new health concern. And the presence of multiple chronic conditions, such as diabetes and hypertension, may pose unique challenges for both disease management and the maintenance of social relationships.
Life expectancy has risen steadily in virtually all developed countries, as have survival rates for those with chronic diseases, so that many individuals are living longer with serious disease. Cardiovascular diseases, diabetes, and cancer are among the main contributors to this trend (Crimmins and Beltran-Sanchez 2010). A crucial challenge for the future is limiting the health consequences of chronic diseases, which means maximizing the extent to which people are aware of and able to manage these conditions. Our findings suggest that social relationships and the resources they bring offer some promising avenues for improving these outcomes.
Supplementary Material
Footnotes
This work and the National Social Life, Health, and Aging Project (NSHAP) are supported by the National Institutes of Health, including the National Institute on Aging, the Office of Women’s Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research [grant 5R01AG021487]. We are grateful for helpful comments from Virginia Chang and Benjamin Cornwell.
Contributor Information
Erin York Cornwell, Cornell University.
Linda J. Waite, University of Chicago
References
- Adams Rebecca G, Blieszner Rosemary. Aging Well with Friends and Family. American Behavioral Scientist. 1995;39:209–225. [Google Scholar]
- Ajrouch Kristine J, Antonucci Toni C, Janevic Mary R. Social Networks among Blacks and Whites: The Interaction between Race and Age. Journal of Gerontology: Social Sciences. 2001;56B:S112–S118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- Antonucci Toni C, Johnson EH. The Role of Social Support in the Modification of Risk Factors for Cardiovascular Disease. In: Shumaker SA, Czajkowski SM, editors. Social Support and Cardiovascular Disease. New York: Plenum Press; 1994. [Google Scholar]
- August Kristin J, Sorkin Dana H. Marital Status and Gender Differences in Managing a Chronic Illness: The Function of Social Control. Social Science & Medicine. 2010;71:1831–1838. doi: 10.1016/j.socscimed.2010.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth Jurgen, Schneider Sarah, von Kanel Roland. Lack of Social Support in the Etiology and the Prognosis of Coronary Heart Disease: A Systematic Review and Meta-Analysis. Psychosomatic Medicine. 2010;72:229–238. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- Berkman Lisa F, Glass Thomas, Rissette Ian, Seeman Teresa E. From Social Integration to Health: Durkheim in the New Millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Berkman Lisa F, Leo-Summers L, Horwitz R. Emotional Support and Survival After Myocardial Infarction: A Prospective, Population-Based Study of the Elderly. Annals of Internal Medicine. 1992:117. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- Boutin-Foster Carla. Getting to the Heart of Social Support: A Qualitative Analysis of the Types of Instrumental Support That Are Most Helpful in Motivating Cardiac Risk Factor Modification. Heart and Lung. 2005;34:22–29. doi: 10.1016/j.hrtlng.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Brummett Beverly H, Barefoot John C, Siegler Ilene C, Clapp-Channing Nancy E, Lytle Barbara L, Bosworth Hayden B, Williams Redford, Mark Daniel B. Characteristics of Socially Isolated Patients with Coronary Artery Disease who are at Elevated Risk for Mortality. Psychosomatic Medicine. 2001;63:267–272. doi: 10.1097/00006842-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Cacioppo John T, Hawkley Louise C, Berntson Gary G. The Anatomy of Loneliness. Current Directions in Psychological Science. 2003;12:71–74. [Google Scholar]
- Christakis Nicholas A, Fowler James H. The Spread of Obesity in a Large Social Network over 32 Years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial Models of the Role of Social Support in the Etiology of Physical Disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon, Williamson Gail M. Stress and Infectious Disease in Humans. Psychological Bulletin. 1991;109:5–24. doi: 10.1037/0033-2909.109.1.5. [DOI] [PubMed] [Google Scholar]
- Cornman Jennifer C, Goldman Noreen, Glei Dana A, Weinstein Maxine, Chang Ming-Cheng. Social Ties and Perceived Support: Two Dimensions of Social Relationships and Health Among the Elderly in Taiwan. Journal of Aging and Health. 2003;15:616–644. doi: 10.1177/0898264303256215. [DOI] [PubMed] [Google Scholar]
- Cornwell Benjamin. Good Health and the Bridging of Structural Holes. Social Networks. 2009;31:92–103. doi: 10.1016/j.socnet.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell Benjamin, Laumann Edward O, Philip Schumm L. The Social Connectedness of Older Adults: A National Profile. American Sociological Review. 2008;73:185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell Benjamin, Philip Schumm L, Laumann Edward O, Graber Jessica. Social Networks in the NSHAP Study: Rationale, Measurement, and Preliminary Findings. Journal of Gerontology: Social Sciences. 2009;64B:i45–i55. doi: 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins Eileen M, Beltran-Sanchez Hiram. Mortality and Morbidity Trends: Is There a Comptression of Morbidity? Journal of Gerontology: Social Sciences. 2010;66B:75–86. doi: 10.1093/geronb/gbq088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushman William C, Ford Charles E, Cutler Jeffrey A, Margolis Karen L, Davis Barry R, et al. Success and Predictors of Blood Pressure Control in Diverse North American Settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) Journal of Clinical Hypertension. 2002:4. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- DiMatteo M Robin. Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis. Health Psychology. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Fiori Katherine L, Antonucci Toni C, Cortina Kai S. Social Network Typologies and Mental Health Among Older Adults. Journal of Gerontology. 2006;61B:25–32. doi: 10.1093/geronb/61.1.p25. [DOI] [PubMed] [Google Scholar]
- Gallant Mary P. The Influence of Social Support on Chronic Illness Self-Management: A Review and Directions for Research. Health Education and Behavior. 2003;30:170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- Gallant Mary P, Spitze Glenna D, Prohaska Thomas R. Help or Hindrance?: How Family and Friends Influence Chronic Illness Self-Management among Older Adults. Research on Aging. 2007;29:375–409. [Google Scholar]
- Goldman Noreen, Korenman S, Weinstein R. Marital Status and Health Among the Elderly. Social Science and Medicine. 1995;40:1717–1730. doi: 10.1016/0277-9536(94)00281-w. [DOI] [PubMed] [Google Scholar]
- Gorin AA, Wing RR, et al. Weight Loss Treatment Influences Untreated Spouses and the Home Environment: Evidence of a Ripple Effect. International Journal of Obesity. 2008;32:1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley Louise C, Cacioppo John T. Loneliness Matters: A Theoretical and Empirical Review of Consequences and Mechanisms. Annals of Behavioral Medicine. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson Vicki S, Novak Sarah A, Lepore Stephen J, Eton David T. Spouse Social Control Efforts: Relations to Health Behavior and Well-Being Among Men with Prostate Cancer. Journal of Social and Personal Relationships. 2004;21:53–68. [Google Scholar]
- Hyman David J, Pavlik Valory N. Characteristics of Patients with Uncontrolled Hypertension in the United States. New England Journal of Medicine. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L, Boulifard David A, Contrada Richard J. Mending Broken Hearts: Marriage and Survival Following Cardiac Surgery. Journal of Health and Social Behavior. 2012;53:33–49. doi: 10.1177/0022146511432342. [DOI] [PubMed] [Google Scholar]
- Insel Kathleen, Morrow Daniel, Brewer Barbara, Figueredo Aurelio. Executive Function, Working Memory, and Medication Adherence Among Older Adults. Journals of Gerontology, Series B: Psychological and Social Sciences. 2006;61:P102–P107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- Iwashyna Theodore J, Christakis Nicholas A. Marriage, Widowhood, and Health-Care Use. Social Science & Medicine. 2003;57:2137–2147. doi: 10.1016/s0277-9536(02)00546-4. [DOI] [PubMed] [Google Scholar]
- Jackson Todd. Relationships Between Perceived Close Social Support and Health Practices Within Community Samples of American Women and Men. The Journal of Psychology. 2006;140:229–246. doi: 10.3200/JRLP.140.3.229-246. [DOI] [PubMed] [Google Scholar]
- Kaplan Robert M, Hartwell SL. Differential Effects of Social Suport and Social Network on Physiological and Social Outcomes in Men and Women withType II Diabetes Mellitus. Health Psychology. 1987;6:387–398. doi: 10.1037//0278-6133.6.5.387. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser Janice K, Newton Tamara L. Marriage and Health: His and Hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kim Yong-Chan, Moran Meghan B, Wilkin Holley A, Ball-Rokeach Sandra J. Integrated Connection to Neighborhood Storytelling Network, Education, and Chronic Disease Knowledge among African Americans and Latinos in Los Angeles. Journal of Health Communication. 2011;16:393–415. doi: 10.1080/10810730.2010.546483. [DOI] [PubMed] [Google Scholar]
- Kinney Anita Yeomans, Bloor Lindsey E, Martin Christopher, Sandler Robert S. Social Ties and Colorectal Cancer Screening among Blacks and Whites in North Carolina. Cancer Epidemiology, Biomarkers, and Prevention. 2005;14:182–189. [PubMed] [Google Scholar]
- Lett Heather S, Blumenthal James A, Babyak Michael A, Strauman Timothy J, Robins Clive, Sherwood Andrew. Social Support and Coronary Heart Disease: Epidemiologic Evidence and Implications for Treatment. Psychosomatic Medicine. 2005;67:869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- Lewis Megan A, Rook Karen S. Social Control in Personal Relationships: Impact on Health Behaviors and Psychological Distress. Health Psychology. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- Lillard Lee A, Waite Linda J. ‘Til Death Do Us Part:’ Marital Disruption and Mortality. American Journal of Sociology. 1995;100:1131–1156. [Google Scholar]
- Luttik Marie Louise, Jaarsma Tiny, Moser Debra, Sanderman Robbert, van Veldhuisen Dirk J. The Importance and Impact of Social Support on Outcomes in Patients with Heart Failure: An Overview of the Literature. Journal of Cardiovascular Nursing. 2005;20:162–169. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- McFall Stephanie L, Davila Marivel. Gender, Social Ties, and Cancer Screening among Elderly Persons. Journal of Aging and Health. 2008;20:997–1011. doi: 10.1177/0898264308324682. [DOI] [PubMed] [Google Scholar]
- Molloy Gerard J, Hamer Mark, Randall Gemma, Chida Yoichi. Marital Status and Cardiac Rehabilitation Attendance: A Meta-Analysis. European Journal of Cardiovascular Prevention and Rehabilitation. 2008a;15:557–561. doi: 10.1097/HJR.0b013e3283063929. [DOI] [PubMed] [Google Scholar]
- Molloy Gerard J, Perkins-Porras Linda, Bhattacharyya Mimi R, Strike Philip C, Steptoe Andrew. Practical Support Predicts Medication Adherence and Attendance at Cardiac Rehabilitation Following Acute Coronary Syndrome. Journal of Psychosomatic Research. 2008b;65:581–586. doi: 10.1016/j.jpsychores.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Molloy Gerard J, Perkins-Porras Linda, Strike Philip C, Steptoe Andrew. Social Networks and Partner Stress as Predictors of Adherence to Medication, Rehabilitation Attendance, and Quality of Life Following Acute Coronary Syndrome. Health Psychology. 2008c;27:52–58. doi: 10.1037/0278-6133.27.1.52. [DOI] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Angel Jacqueline L, Angel Ronald J. Employment, Marriage, and Inequality in Health Insurance for Mexican-Origin Women. Journal of Health and Social Behavior. 2009;50:132–148. doi: 10.1177/002214650905000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mookadam Farouk, Arthur Heather M. Social Support and Its Relationship to Morbidity and Mortality After Acute Myocardial Infarction. Archives of Internal Medicine. 2004;164:1514–1518. doi: 10.1001/archinte.164.14.1514. [DOI] [PubMed] [Google Scholar]
- Morgan Stephen L, Todd Jennifer J. A Diagnostic Routine for the Detection of Consequential Heterogeneity of Causal Effects. Sociological Methodology. 2008;38:231–281. [Google Scholar]
- Nausheen Bina, Gidron Yori, Peveler Robert, Moss-Morris Rona. Social Support and Cancer Progression: A Systematic Review. Journal of Psychosomatic Medicine. 2009;67:403–415. doi: 10.1016/j.jpsychores.2008.12.012. [DOI] [PubMed] [Google Scholar]
- NHLBI. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. U.S. Department of Health and Human Services; 2003. [DOI] [PubMed] [Google Scholar]
- O’Muircheartaigh Colm, Eckman Stephanie, Smith Stephen. Statistical Design and Estimation for the National Social Life, Health, and Aging Project. Journals of Gerontology, Series B: Psychological and Social Sciences. 2009;64B:i12–i19. doi: 10.1093/geronb/gbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostchega Yechiam, Dillon Charles F, Hughes Jeffery P, Carroll Margaret, Yoon Sarah. Trends in Hypertension Prevalence, Awareness, Treatment, and Control in Older U.S. Adults: Data from the National Health and Nutrition Examination Survey 1988 to 2004. Journal of the American Geriatrics Society. 2007;55:1056–1065. doi: 10.1111/j.1532-5415.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- Pecchioni Loretta L, Sparks Lisa. Health Information Sources of Individuals with Cancer and their Family Members. Health Communication. 2007;21:143–151. doi: 10.1080/10410230701307162. [DOI] [PubMed] [Google Scholar]
- Perry Brea L, Pescosolido Bernice A. Functional Specificity in Discussion Networks: The Influence of General and Problem-Specific Networks on Health Outcomes. Social Networks. 2010;32:345–357. [Google Scholar]
- Pienta Amy Mehraban, Hayward Mark D, Jenkins Kristi Rahrig. Health Consequences of Marriage for the Retirement Years. Journal of Family Issues. 2000;2000:559–586. [Google Scholar]
- Qato Dima M, Philip Schumm L, Johnson Michael, Mihai Andreea, Lindau Stacy Tessler. Medication Data Collection and Coding in a Home-Based Survey of Older Adults. Journal of Gerontology: Social Sciences. 2009;64(B):i86–i93. doi: 10.1093/geronb/gbp036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen Jeppe N, Chong Alice, Alter David. Relationship Between Adherence to Evidence-Based Pharmacotherapy and Long-Term Mortality After Acute Myocardial Infarction. Journal of the American Medical Association. 2007;297:177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- Reifman Alan. Social Relationships, Recovery from Illness, and Survival: A Literature Review. Annals of Behavioral Medicine. 1995;17:124–131. doi: 10.1007/BF02895061. [DOI] [PubMed] [Google Scholar]
- Reyes Ortiz Carlos A, Freeman Jean L, Kuo Yong-Fang, Goodwin James S. The Influence of Marital Status on Stage at Diagnosis and Survival of Older Persons with Melanoma. Journal of Gerontology: Medical Sciences. 2007;62A:892–898. doi: 10.1093/gerona/62.8.892. [DOI] [PubMed] [Google Scholar]
- Robles TF, Kiecolt-Glaser Janice K. The Physiology of Marriage: Pathways to Health. Physiology and Behavior. 2003;70:409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Rosland Ann-Marie, Piette John D. Emerging Models for Mobilizing Family Support for Chronic Disease Management: A Structured Review. Chronic Illness. 2010;6:7–21. doi: 10.1177/1742395309352254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanfeld D, Scanfeld V, Larson EL. Dissemination of health information through social networks: twitter and antibiotics. Am J Infect Control. 2010;38:182–8. doi: 10.1016/j.ajic.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman Teresa, Berkman Lisa F. Structural Characteristics of Social Networks and Their Relationships with Social Support in the Elderly: Who Provides Support. Social Science & Medicine. 1988;26:737–749. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa, Chen Xinguang. Risk and Protective Factors for Physical Functioning in Older Adults With and Without Chronic Conditions: MacArthur Studies of Successful Aging. Journal of Gerontology: Social Sciences. 2002;57B:S135–S144. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- Smith Kirsten P, Christakis Nicholas A. Social Networks and Health. Annual Review of Sociology. 2008;34:405–429. [Google Scholar]
- Smith Stephen, Jaszczak Angie, Graber Jessice, Lundeen Katie, Leitsch Sara, Wargo Erin, O’Muircheartaigh Colm. Instrument Development, Study Design Implementation, and Survey Conduct for the National Social Life, Health, and Aging Project. Journals of Gerontology, Series B: Psychological and Social Sciences. 2009;64B:i20–i29. doi: 10.1093/geronb/gbn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol Michael C, McGuigan Kimberly A, Verbrugge Robert R, Epstein Robert S. Impact of Medication Adherence on Hospitalization and Healthcare Cost. Medical Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- Steptoe Andrew, Owen Natalie, Kunz-Ebrecht Sabine R, Brydon Lena. Loneliness and Neuroendocrine, Cardiovascular, and Inflammatory Stress Responses in Middle-Aged Men and Women. Psychoneuroendocrinology. 2003;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Stimpson Jim P, Wilson Fernando A. Cholesterol Screening by Marital Status and Sex in the United States. Preventing Chronic Disease. 2009;6:1–9. [PMC free article] [PubMed] [Google Scholar]
- Stoller Eleanor Palo, Pugliesi Karen L. Size and Effectiveness of Informal Helping Networks: A Study of Older People in the Community. Journal of Health and Social Behavior. 1991;32:180–191. [PubMed] [Google Scholar]
- Thoits Peggy. Mechanisms Linking Social Ties and Support to Physical and Mental Health. Journal of Health and Social Behavior. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Trivedi Ranak B, Ayotte Brian, Edelman David, Bosworth Hayden B. The Association of Emotional Well-Being and Marital Status with Treatment Adherence among Patients with Hypertension. Journal of Behavioral Medicine. 2008;31:489–497. doi: 10.1007/s10865-008-9173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino Bert N. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. Family Status and Health Behaviors: Social Control as a Dimension of Social Integration. Journal of Health and Social Behavior. 1987;28:306–319. [PubMed] [Google Scholar]
- Umberson Debra. Gender, Marital Status, and the Social Control of Health Behavior. Social Science & Medicine. 1992;34:907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Crosnoe Robert, Reczek Corinne. Social Relationships and Health Behavior Across the Life Course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasan Ramachandran S, Beiser Alexa, Seshadri Sudha, Larson Martin G, Kannel William B, D’Agostino Ralph B, Levy Daniel. Residual Lifetime Risk for Developing Hypertension in Middle-Aged Women and Men: The Framingham Heart Study. Journal of the American Medical Association. 2002:287. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- Warren-Findlow Jan, Seymour Rachel B, Shenk Dena. Intergenerational Transmission of Chronic Illness Self-Care: Results from the Caring for Hypertension in African-American Families Study. The Gerontologist. 2010;51:64–75. doi: 10.1093/geront/gnq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellman Barry, Wortley Scot. Different Strokes for Different Folks: Community Ties and Social Support. American Journal of Sociology. 1990;96:558–588. [Google Scholar]
- Westmaas J Lee, Cameron Wild T, Ferrence Roberta. Effects of Gender in Social Control of Smoking Cessation. Health Psychology. 2002;21:368–376. doi: 10.1037//0278-6133.21.4.368. [DOI] [PubMed] [Google Scholar]
- Wethington Elaine, Kessler Ronald C. Perceived Support, Received Support, and Adjustment to Stressful Life Events. Journal of Health and Social Behavior. 1986:27. [PubMed] [Google Scholar]
- York Cornwell Erin, Waite Linda J. Social Disconnectedness, Perceived Isolation, and Health among Older Adults. Journal of Health and Social Behavior. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.