Abstract
Multiple endocrine neoplasia type 1 (MEN1) is classically characterized by the development of functional or nonfunctional hyperplasia or tumors in endocrine tissues (parathyroid, pancreas, pituitary, adrenal). Because effective treatments have been developed for the hormone excess state, which was a major cause of death in these patients in the past, coupled with the recognition that nonendocrine tumors increasingly develop late in the disease course, the natural history of the disease has changed. An understanding of the current causes of death is important to tailor treatment for these patients and to help identify prognostic factors; however, it is generally lacking.
To add to our understanding, we conducted a detailed analysis of the causes of death and prognostic factors from a prospective long-term National Institutes of Health (NIH) study of 106 MEN1 patients with pancreatic endocrine tumors with Zollinger-Ellison syndrome (MEN1/ZES patients) and compared our results to those from the pooled literature data of 227 patients with MEN1 with pancreatic endocrine tumors (MEN1/PET patients) reported in case reports or small series, and to 1386 patients reported in large MEN1 literature series. In the NIH series over a mean follow-up of 24.5 years, 24 (23%) patients died (14 MEN1-related and 10 non-MEN1-related deaths). Comparing the causes of death with the results from the 227 patients in the pooled literature series, we found that no patients died of acute complications due to acid hypersecretion, and 8%–14% died of other hormone excess causes, which is similar to the results in 10 large MEN1 literature series published since 1995. In the 2 series (the NIH and pooled literature series), two-thirds of patients died from an MEN1-related cause and one-third from a non-MEN1-related cause, which agrees with the mean values reported in 10 large MEN1 series in the literature, although in the literature the causes of death varied widely. In the NIH and pooled literature series, the main causes of MEN1-related deaths were due to the malignant nature of the PETs, followed by the malignant nature of thymic carcinoid tumors. These results differ from the results of a number of the literature series, especially those reported before the 1990s. The causes of non-MEN1-related death for the 2 series, in decreasing frequency, were cardiovascular disease, other nonendocrine tumors > lung diseases, cerebrovascular diseases. The most frequent non-MEN1-related tumor deaths were colorectal, renal > lung > breast, oropharyngeal. Although both overall and disease-related survival are better than in the past (30-yr survival of NIH series: 82% overall, 88% disease-related), the mean age at death was 55 years, which is younger than expected for the general population.
Detailed analysis of causes of death correlated with clinical, laboratory, and tumor characteristics of patients in the 2 series allowed identification of a number of prognostic factors. Poor prognostic factors included higher fasting gastrin levels, presence of other functional hormonal syndromes, need for >3 parathyroidectomies, presence of liver metastases or distant metastases, aggressive PET growth, large PETs, or the development of new lesions.
The results of this study have helped define the causes of death of MEN1 patients at present, and have enabled us to identify a number of prognostic factors that should be helpful in tailoring treatment for these patients for both short- and long-term management, as well as in directing research efforts to better define the natural history of the disease and the most important factors determining long-term survival at present.
INTRODUCTION
The autosomal dominant disorder, multiple endocrine neoplasia type 1 (MEN1) has an incidence of 0.22%–0.25% in postmortem studies.32,239,418 MEN1 is caused by alterations in the 10 exon Menin gene located on chromosome 11q13, which result in abnormalities (mutations, deletions, truncations, primarily) in the 610 amino acid nuclear protein, menin.62,195,419 Although the exact mechanisms by which altered or absent menin causes the clinicopathologic changes characteristic of MEN1 are not known, numerous studies have demonstrated that menin is involved in many important cellular processes such as cell cycle regulation, transcriptional control, cell division, and genomic stability.16,50,195,419,469
Patients with MEN1 classically develop adenomas or hyperplasia of multiple endocrine glands, with parathyroid hyperplasia resulting in hyperparathyroidism (HPT) being the most frequent clinical abnormality (90%–100%), followed by pancreatic endocrine tumors (PETs) (functional [20%–70%] or nonfunctional [80%–100%]), pituitary adenomas (functional/nonfunctional [20%–65%]), adrenal tumors (occasionally functional [10%–73%]), and thyroid adenomas (primarily nonfunctional [0–10%]).48,102,140,195,228,239,262,279,280,374,388,390,418 It has been recognized recently that MEN1 patients have an increased occurrence of other endocrine and nonendocrine tumors including carcinoid tumors (thymic [0–8%], gastric [7%–35%], bronchial [0–8%], and rarely intestinal); skin tumors (angiofibromas [88%], collagenomas [72%], lipomas [34%], and melanomas); central nervous system (CNS) tumors (meningiomas, ependymomas, schwannomas [0–8%]); and smooth muscle tumors (leiomyomas, leiomyosarcomas [1%–7%]).13,46,48,49,74,131,176,209,228,261,274,354,388,393,413,465 In other reports, small numbers of other tumors have also been described, although it is unclear if they are increased in frequency or aggressiveness in MEN1 patients (lymphoma, renal cancer, hematologic disorders [thrombotic thrombocytopenic purpura, myeloma], ovarian tumors, gastrointestinal stromal tumors, seminomas, chondrosarcoma, mesothelioma, thymomas).1,77,84,89,150,214,216,256,312,341,410,432
Whereas there have been many advances in a number of aspects related to MEN1 including molecular understanding, development of molecular screening methods, and treatment of various MEN1-related disorders, the late course of the disease remains unclear, particularly the current causes of death. An understanding of the late course of disease could allow treatments to be tailored to the most significant disorders found to occur (for example, treatment of PETs), and could allow the possible identification of risk factors and prognostic factors that could alter treatment approaches. This is important because the disease has a long course in many cases, and thus there are often opportunities to institute treatments early in the course.
There is a lack of prospective studies evaluating the long-term course and causes of death of MEN1 patients at present. This lack of information is a particular problem at present because there have been numerous widespread treatment changes over the last few years that have altered the late course of MEN1, and have likely altered the causes of death. These changes include the increased ability to control various hormone excess states that were a frequent cause of death in early studies of MEN1 patients,15,43,72,73,83,88,158,180,188,224,225,240,254,279,307,353,366,386,399,438,444,458,461,465,466 accounting for up to 73%–91% of all deaths in some early series.15,195,224,254,444 These include particularly the ability to treat the gastric acid hypersecretion in Zollinger-Ellison syndrome (ZES), earlier diagnosis and better treatment of insulinomas, and the increased use of somatostatin analogues or other treatments for other hypersecretory states (vasoactive intestinal peptide secreting tumors [VIPomas], etc). This also includes an understanding of the diffuse nature of the parathyroid disease in these patients resulting in HPT, which almost all patients develop early in the disease course, and the development of effective treatment with multigland parathyroidectomies, which prevents the development of nephrolithiases, and renal failure,54,57,78,129,149,150 which not infrequently occurred in earlier series.15,32,68,88,129,224,285,438,444,465,466 Similarly, the recognition of the pituitary disease and more aggressive treatments have made this a rare cause of morbidity and death at present compared to in earlier studies.49,129,150,222,378,379,465 Lastly, it is now recognized that MEN1 patients develop neoplasms other than those classically described, such as various carcinoid tumors, CNS tumors, skin tumors, and soft tissue tumors. Of these the carcinoid tumors can be of concern because they can be aggressive and develop later in the disease course.34,40,94,131,150,151,253,326,360,465 The thymic carcinoids, which are rarely reported before 1990, are of particular concern, especially in males, because as a group they are the most aggressive tumors that MEN1 patients develop and are an increasing cause of death, later in the disease course.111,130,131,151,408,413,414,465 With the effective treatment of hormone excess states, they are becoming increasingly important.
We conducted this study to describe the current course of MEN1 patients late in the disease history, as well as the causes of death at present, and to identify prognostic factors for different causes of death. Unfortunately, to our knowledge there are no reports in the literature of prospective studies of MEN1 patients containing sufficient deaths to allow a direct comparison to the patients in the present study. To allow comparison to existing data in the literature, we compared our results to outcomes reported in 2 other groups of MEN1 patients, as described in the Methods section below. From these comparisons we were able to draw a number of conclusions and to identify a number of prognostic factors that could affect clinical management.
PATIENTS AND METHODS
NIH MEN1/ZES Patients
All patients admitted to the National Institutes of Health (NIH) Digestive Diseases Branch with a diagnosis of a PET with ZES with MEN1 over a 32-year period140 were evaluated for eligibility for this study. Eligibility requirements included the presence of MEN1 with a PET with ZES and an agreement to participate prospectively in the initial and follow-up evaluations. The present study is part of a prospective study of patients with MEN1 with MEN1/ZES at the NIH approved by the Clinical Research Committee of the National Institute of Diabetes and Digestive and Kidney Diseases.
Diagnostic Criteria
Diagnostic criteria for a PET included functional, pathologic, or imaging evidence for the presence of a PET. Diagnostic criteria for ZES were as previously described115,365 and included 1) elevated fasting serum gastrin (>100 pg/mL until 1994, >200 pg/mL since 1994);36,135 2) elevated basal acid output (BAO >15 mEq in unoperated patients, >5 mEq in patients with previous acid reducing surgery;200,290,364 3) positive provocative testing with secretin (an increase of >120 pg/mL postinjection) or with calcium (an increase of >395 pg/mL);35,85,122 4) positive histologic confirmation of gastrinoma; or 5) a combination of these criteria.115,200,365 Secretin testing and the calcium provocative test were performed as described previously.35,122 With the calcium test, an increase of >395 pg/mL over the average of the pre-injection values was considered a positive response.35,85,122 The calcium infusion test was not performed if the patient was hypercalcemic prior to starting the test.
Diagnostic criteria for MEN1 with MEN1/ZES included ZES plus either a family history of MEN1 or evidence of HPT or pituitary disease as previously described.31,189,195 Serum gastrin levels were determined by Bioscience Laboratories (New York, NY) until 1994 and subsequently by Mayo Clinic Laboratories (Rochester, MN).36,64,115,122 BAO and maximal acid output (MAO) were measured when off all antisecretory medications as described previously.115,282,364 Briefly, patients were not treated with anticholinergic agents for 3 days, oral histamine H2-receptor antagonists for at least 30 hours, proton pump inhibitors for 1 week, and all intravenous infusions of H2-receptor antagonists for at least 12 hours.282,364 MAO was assessed whenever possible if either pentagastrin or histalog was available by administering either histolog (1.5 mg/kg intramuscularly, Eli Lilly, Indianapolis, IN) or pentagastrin (6 μg/kg subcutaneously, Ayerst Laboratories, New York, NY) as described previously.115,282,364 All results were expressed as mEq/h.
Evaluations and Definitions
On the initial evaluation, a family and personal history for endocrinopathies or other illness was obtained as described previously.31,195,365 Using a questionnaire, outside records, and correspondence from referring physicians, we thoroughly reviewed the MEN1-related disease. We obtained a detailed record of the diagnosis and treatment of all endocrinopathies, with particular attention to parathyroid, pituitary, and pancreatic disorders. For parathyroid disorders the time of first determination of hypercalcemia, history of renal colic, parathyroidectomy history (time, number, type of operation, result, and time of last calcium and/or parathormone [PTH] assessment) were obtained. The time of first onset of renal colic or determination that hypercalcemia or HPT was present was taken as the time of establishment of HPT and was used in the study as the time of diagnosis of HPT as described previously.140 Each patient underwent extensive questioning regarding symptoms compatible with gastric acid hypersecretion including abdominal pain, heartburn, nausea, vomiting, weight loss, diarrhea, and gastrointestinal bleeding.140,365 We conducted a complete review of past medical history for other diseases including other gastrointestinal and hepatic disorders present at the time of the initial admission.365 The time of onset of ZES and time of diagnosis of ZES were determined as described previously.365,459 The duration of ZES from onset to diagnosis was calculated as the interval from the time of onset to the time of diagnosis of ZES. The time of onset of MEN1 was the time of the first clinical manifestation of MEN1 (renal colic, pituitary disease, symptomatic PET) or the time the disease was first detected by biochemical screening.31,140,175 Most of the study period preceded the widespread use of genetic testing, and no patients were initially identified by genetic testing. The time of diagnosis and onset of MEN1 or pituitary disease was determined as described previously.31,140,175 To establish the presence of lipomas, melanomas, smooth muscle tumors, thyroid disease, or other PETs prior to evaluation at the NIH, we reviewed the hospital pathology and physician records from pre-NIH evaluations. Family history of MEN1 was considered positive if any sibling, parent, or grandparent had any of the principal manifestations compatible with MEN1 (parathyroid, pituitary, PET).
Patients were admitted for the initial evaluation and then yearly as described previously, except for patients with advanced disease who were admitted more frequently depending on the antitumor treatment protocol (every 3–6 months).140,351,382,450,476 On the initial admission and subsequent admissions, all patients had laboratory evaluations including complete blood count, urinalysis, at least 3 fasting serum gastrin levels, tumor imaging studies, biochemistry studies including liver function tests and an upper gastrointestinal endoscopy. Cross-sectional imaging studies (ultrasound,242,335 computed tomography scan [CT] with contrast,220,335,415,456 and magnetic resonance imaging [MRI]121,335,349,415) were performed to assess tumor location and extent as described previously.335,476 If the tumor localization or extent was unclear, selective abdominal angiography was performed.132,269,335 Since 1994, all patients underwent initially and then yearly somatostatin receptor scintigraphy (SRS) using 6 mCi of [111In-DTPA-dPhe1]octreotide with spot views and single photon emission CT imaging at 4 hours and 24 hours postinjection performed as previously described.134,137,138,415,416 Liver metastases were established by biopsy in all patients as described previously.405,459,476 Bone metastases were assessed using bone scanning, SRS, and MRI of the spine as described.133,137,138,476 If imaging results remained uncertain, bone biopsy was performed.133 Gastric acid hypersecretion was controlled in all patients using either histamine receptor antagonists (cimetidine, ranitidine, famotidine) alone or with an anticholinergic agent until 1983, then primarily using proton pump inhibitors (omeprazole, lansoprazole) as described previously.123,192,200,266,281,282,283,284,294,350,417 Sufficient antisecretory drug was given to reduce acid secretion to <10 mEq/h in the hour before the next dose of medication or to <5 mEq/h (or to the absence of symptoms) in patients with prior partial gastrectomy266 or severe gastroesophageal reflux disease (GERD).266,281,283,284,295
At the initial NIH evaluation and on subsequent NIH admission all patients underwent detailed clinical, biochemical, and imaging studies to assess the possible presence of MEN1 and, if present, additional studies to assess the extent of MEN1 involvement.13,31,131,139,141,175,315 To assess parathyroid function all patients were evaluated for total serum calcium, albumin, plasma, PTH determination using an assay that identified the midportion of PTH (performed at the NIH from 1974 to 1983 and by Bioscience Laboratories from 1983 to 1991). Since 1988 an assay measuring the intact PTH molecule (Nichols Institute, San Juan Capistrano, CA) was performed.140,328 Plasma ionized calcium levels were performed in the last 10 years. To assess pituitary disease, serum prolactin, adrenocorticotropin, thyroid stimulating hormone, growth hormone, luteinizing hormone, follicle stimulating hormone, thyroid function studies (T4, T3) and urinary cortisol excretion were assessed, as were sella turcica size and pituitary imaging abnormalities using CT and/or MRI of the sella turcica.13,133,140 To assess for the presence of a functional PET in addition to fasting gastrin levels, plasma insulin, proinsulin, glucose, adrenocorticotropin, glucagon, pancreatic polypeptide, serotonin, calcitonin and urinary 5-hydroxyindolacetic acid, N-methyl histamine excretion and cortisol excretion were determined.24,139,141,267 Prior to surgery in patients with insulinomas and selected patients with gastrinomas, functional localization studies were performed assessing hormonal gradients using either selective venous sampling or hepatic vein sampling after intraarterial injections of either calcium or secretin as described previously.64,91,92,293,422 The presence of a PET was also assessed by tumor imaging studies using cross-sectional imaging (ultrasound, CT scan, MRI, and, if results were unclear, angiography) and SRS as described above. Thymic carcinoids were assessed by chest CT scanning, SRS and, since 2000, MRI of the chest as described.131 Lung/bronchial carcinoids were assessed by chest CT and chest X-ray and, since 2000, by MRI of the chest, and were confirmed by thoracotomy. The presence of gastric carcinoids was assessed by upper gastrointestinal endoscopy using a videoscope GIF 100 endoscope (Olympus America, Inc., Melville, NY) with a 3.7 mm biopsy channel.34,139,268,344 Skin lesions associated with MEN1 (collagenoma, angiofibromas, lipomas, melanomas)74,195 were investigated in all patients since 2000 as described previously.14 Other tumors that are found in MEN1 patients (smooth muscle tumors [leiomyomas, leiomyosarcomas, etc], CNS tumors [meningiomas, ependymomas, schwannomas])13,42,195,261,418 were sought for using cross-sectional imaging studies as well as upper and lower gastrointestinal endoscopy as described previously.13,131
Exploratory laparotomy was performed in patients with MEN1 with PET/ZES with an imageable lesion >2.5 cm, who did not have diffuse liver metastases or an intercurrent illness limiting life expectancy.189,195,314,315,318,324,380 At exploration all patients had a standard operation consisting of an extensive search for a PET/gastrinoma as described previously.7,250,314,315,316 Because of the frequent occurrence of gastrinomas in the duodenum,9,195,347,421 which are frequently small and multiple in MEN1,9,195,250,347 particular attention was paid preoperatively and intraoperatively to the duodenum by performing an extended Kocher maneuver, intraoperative endoscopic transillumination of the duodenum,124 intraoperative ultrasound with a 10-MHz real time transducer318 and a 3-cm longitudinal duodenotomy.124,195,324,403,421 Parathyroidectomy was performed in all patients with renal colic, nephrolithiases, reduced bone density, or symptoms due to HPT.317,328 Initially, either a 3.5 gland resection or 4 glands with an implant was performed.317,328 All lung carcinoids and thymic carcinoids were treated with surgical resection as described previously.131 Gastric carcinoids were treated by endoscopic resection, except in 3 patients who underwent total gastrectomy because of the extensiveness of the disease and the growth as described previously.326
In patients with liver metastases, after histologic confirmation no anticancer treatment was given initially, and the growth of the liver metastases was evaluated by repeated imaging studies in 3–6 months as described previously.133,351,450 If on recent imaging, no growth was seen, growth was reassessed at 3–6 month intervals. If growth was seen, patients were treated with interferon (5 × 106 units/d),351 chemotherapy (streptozotocin, fluorouracil, and doxorubicin),450 or octreotide-long-acting release (octreotide-LAR) preparation.382 Patients who initially had metastases that were limited to 1 lobe of liver or that were considered potentially resectable were considered for exploratory laparotomy and partial hepatic resection as described previously.58,315,325,327,329 For each patient the number and size of each measurable tumor were determined in transverse sections of an imaging modality and the rate of growth on serial imaging studies was calculated as described previously.141,476 The rate of change of the most rapidly growing hepatic or extrahepatic tumor was used to determine the growth category. Patients were stratified in 2 groups based on their tumor growth rate: patients were classified as having an aggressive form of MEN1 if there was >25% increase in tumor volume per month or appearance of new lesion(s) at any follow-up evaluation. Patients were classified as developing liver metastases or any new lesion(s) if during follow-up evaluations a new lesion(s) appeared either in the liver or in other sites.
Causes of Death
Any deaths during follow-up were classified as either MEN1 related or not. MEN1-related deaths were deaths due to an MEN1-associated feature, including endocrinopathy, metastatic neuroendocrine tumor (NET), and MEN1 treatment. MEN1-related deaths were also classified as being ZES related or not. ZES-related deaths were defined as deaths due to the tumor because of metastatic spread of the gastrinoma, tumor-related complications, or acute effects of gastric acid hypersecretion (n = 0) as described previously.141,476 The causes of MEN1-related deaths (including all ZES-related deaths) were further categorized into the following 5 subgroups: 1) death due to ZES/PET with progressive liver metastases causing progressive inanition or sepsis; 2) death due to the development of a progressive thymic carcinoid tumor; 3) death due to the development of a non-ZES functional PET; 4) death due to the development of another (nongastrinoma, nonthymic carcinoid tumor) MEN1-associated malignant tumor, and 5) death due to tumor-related embolism. The causes of non-MEN1-related deaths were further categorized into the following 5 subgroups: 1) death due to cardiac causes including myocardial infarction, arrhythmia, or cardiac arrest; 2) death due to the development of an additional non-MEN1-associated malignancy; 3) death due to a cerebrovascular accident; 4) death due to a drug-related cause not related to treatment of advanced metastatic disease; and 5) death due to progressive aplastic anemia.
Genetic Analysis
Sequence analysis of the MEN1 gene was performed since 1998 through our laboratory,146 the Molecular Diagnosis program of the Children’s Research Institute (Children’s National Medical Center, Washington, DC), or through GeneDx Inc. (Gaithersburg, MD). The polymerase chain reaction conditions and primers were as previously described.146,384
Literature Review of Causes of Death in MEN1 Patients With or Without PETs
Unfortunately, to our knowledge there are no series in the literature comparable to the current study in which a large number of MEN1/ZES patients have been prospectively followed, so a direct comparison is not possible. Furthermore, there are insufficient patients reported in the literature with MEN1/ZES described with causes of death defined not due to acid hypersecretion. Therefore, in an attempt to allow comparisons between our data and data from the existing literature, we used 2 specific groups from the literature for comparison, realizing that these groups of patients are not completely comparable in all aspects to our population.
First, we compared our results to the results of a pooled summary of a literature search for any case report or small series of MEN1 patients (<7 deaths) where the patients had a PET of any kind, the cause of death was reported, and the cause of death was not peptic ulcer related. This group was similar to our NIH population in that all had MEN1, all had PETs, and 67% had ZES; however, not all patients had ZES. The search for these patients included primarily reports since 1980, when effective medical/surgical treatments for the gastric acid hypersecretion of MEN1 patients with ZES became widely available and in general use. Specifically, we excluded patients in a series or report where the long-term survival was limited due to death from the complications of uncontrolled acid peptic disease. Especially in many early series of patients treated before 1980,43,60,158,225,260,265,275,307,332,366,399,404,438,445,458 this was the major cause of death, and thus few patients had long-term follow-up, which is not the case at present. In the mid-1970s adequate medical antisecretory treatments with either H2-histamine receptor antagonists or proton pump inhibitors became generally available,15,69,73,108,135,192,224,254,278,282,287,444,483 and this, in addition to the use of total gastrectomy in selected patients, has led to the current situation where few patients die of acid peptic-related disease. Because the current natural history and causes of death are thought to differ markedly from these early reports,54,57,78,88,150,217,367,378,379,448,465 we did not include patients from the early reports.
Second, we compared our results with results of larger MEN1 series in the literature that reported the cause of death of ≥10 patients who died from any cause other than a peptic ulcer-related cause. These patients were similar to our NIH patients in that all had MEN1; however, they were different in that not all had PETs or ZES: 60% had a PET and 54% had ZES. This group resembled the general population of MEN1 patients reported in large series with or without ZES. Comparing our results with this group allowed identification of similarities and differences from series more typical of a general population of MEN1 patients with advanced disease.
To accomplish these comparisons, we searched MEDLINE (National Library of Medicine, Bethesda, MD) using the key words MEN1 or multiple endocrine neoplasia combined with gastrinoma, pancreatic endocrine tumor, glucagonoma, Zollinger-Ellison syndrome, thymic carcinoid, HPT, death, survival, and pituitary tumor, either alone or in combination. We reviewed the bibliographies of all papers to identify papers, book chapters, and other reports not referenced in MEDLINE. All papers were reviewed and relevant data entered into an Excel spreadsheet (Microsoft, Redmond, WA) that was used for all analyses and comparisons. The Japanese literature was also carefully reviewed, both using MEDLINE and reviewing symposium proceedings, books, and abstracts of scientific meetings. We found 10 reports that appeared only in Japanese; for these, the titles and data were translated into English.
For the first comparison with small series or case reports of patients with MEN1 with PETs (MEN1/PET patients) with at least 1 reported death not peptic ulcer disease related, we identified 108 separate reports containing 227 patients; 62 reports contained a single case4–6,25,28,32,68,70,82,86,97,109,111,112,119,125,142,156,162,165,202,206,207,213,216,229,236,249,264,296,297,300,301,304–306,311,313,333,334,358,359,361,369,381,386,387,391,393,396,398,409,411,414,426,430,438,449,460,462,464,467,468 and 40 contained >1 case (mean, 4.3 cases/report).21,22,30,40,41,46,94,113,120,153,166,180,203,223,226,230,238,244,246,247,303,346,353,362,372,375,389,398,406,407,413,425,427,431,440,443,458,461,466,475
For the second comparison we found 18 series that reported the non-peptic cause of death in ≥7 MEN1 patients with or without a PET.15,54,57,78,88,129,150,217,224,226,254,289,367,378,379,444,448,465
Statistical Analysis
All data were entered into Excel spreadsheets and analyzed using Statistica MAC (Statsoft, Tulsa, OK) and Statview (SAS Institute, Inc., Cary, NC). Statistical analysis was performed using the Student t test for paired and unpaired values, the Mann-Whitney U test, the Fisher exact test, the chi-square test, and ANOVA. For a post hoc test the Bonferroni/Dunn test was used. P values < 0.05 were considered significant. All continuous variables are reported as mean ± SEM. Survival curves were plotted in the form of Kaplan-Meier, and 95% confidence intervals (CI) were calculated using Statview (SAS Institute, Inc., Cary, NC).
RESULTS
General Characteristics of the NIH and Literature Patients
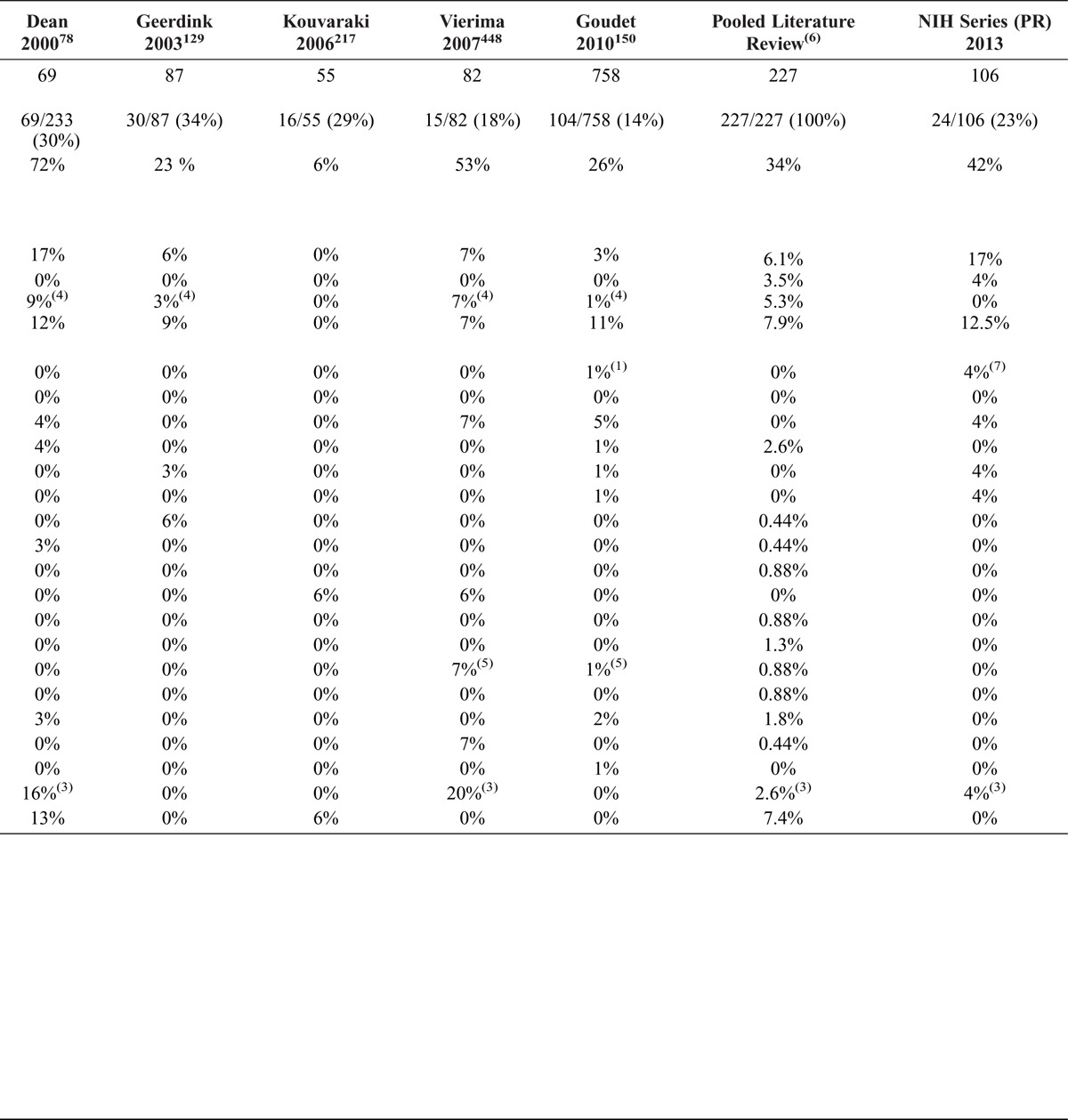
We studied 106 NIH patients with PETs with MEN1 prospectively and compared their causes of death with those of 227 MEN1/PET patients pooled from case reports or small series in the literature, who died of non-acid related causes. The general characteristics of the NIH MEN1/ZES patients are shown in Table 1, and the characteristics of those who died during follow-up (n = 24) are compared to those of the MEN1/PET patients from the pooled literature. For the 106 NIH patients, the main features of MEN1 during the course of the 32-year follow-up were that 106/106 (100%) of the patients had MEN1 with a PET, 100% had ZES, 94% had HPT, and 58% had pituitary disease, primarily prolactinomas. There was a slight preponderance of males (59%), and 30% of patients had no family history of MEN1. During the course of their disease, with repeated evaluations, almost one-half of the patients (46%) were found to have adrenal abnormalities, primarily nonfunctioning adenomas, and 51% had skin tumors, which are increasingly described in MEN1 patients (especially angiofibromas and collagenomas).14,59,74,89,313,336,370 One-third developed a carcinoid tumor, with the most common site a gastric carcinoid followed by bronchial carcinoids (10%) primarily in females and thymic carcinoids in males (6%), as reported in other series.98,131,190,195,465 Smooth muscle tumors (5%), thyroid disease (11%), and other functional PETs (primarily insulinomas) were not uncommon (10%), as were CNS tumors (meningiomas, ependymomas, schwannomas) (7%), as previously described.13,73,95,102,111,131,140,142,195,209,261,414,418,451
TABLE 1.
MEN1 Disease Characteristics of All 106 NIH MEN1/ZES Patients With PETs and 24 Who Died Compared With 227 MEN1/PET Patients From the Pooled Literature Who Died During Follow-Up
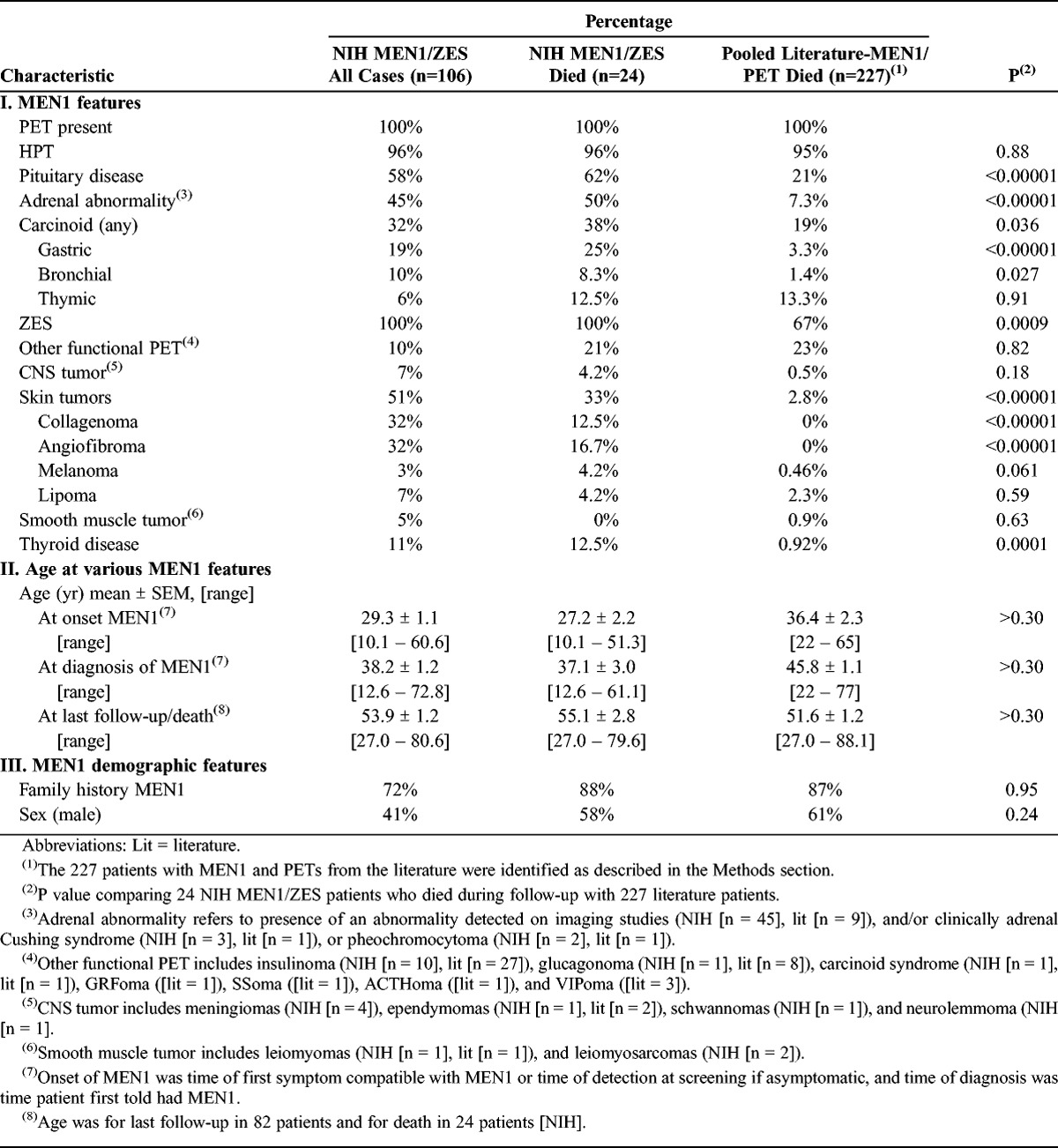
Most of the NIH patients had the onset of MEN1 in the third decade (mean age, 29.3 yr) with the development of signs and symptoms of HPT, although about 40% presented with symptoms of ZES, as reported in other studies.31,140,378,387,444 However, there was an average delay of almost 9 years in establishing the diagnosis of MEN1 (mean, 38.2 yr) (see Table 1). Patients were followed to their last evaluation or death for an average of almost 25 years (average, 24.4 yr) and for 15.5 years from their diagnosis. Patients had an average age of 53.9 years at the last follow-up; however, this varied widely from age 27 to 80.6 years at the last visit.
For the NIH MEN1/ZES patients, 24 of the 106 (23%) patients died during follow-up, which averaged 15.5 ± 0.9 years (range, 1–44 yr) from diagnosis of MEN1 (Figure 1). The general characteristics of the 24 deceased patients were similar to those of all the NIH patients (see Table 1). These 24 NIH MEN1/ZES patients had both similarities to and differences from the 227 MEN1/PET patients from the pooled literature. They were similar in all having a PET, in having a high frequency of HPT (95%–96%), in the rates of thymic carcinoids (12.5%–13.3%), and in the frequency of non-ZES functional PETs (21%–23%), CNS tumors (0.5%–4.2%), or smooth muscle tumors (0–0.9%), and some skin tumors (melanomas, lipomas) (0.5%–4.6%). The patients were also similar in the high frequency of a family history of MEN1, in having a slight male predominance (58–61%), and in their mean age at last follow-up (51.6–55.1 yr).
FIGURE 1.
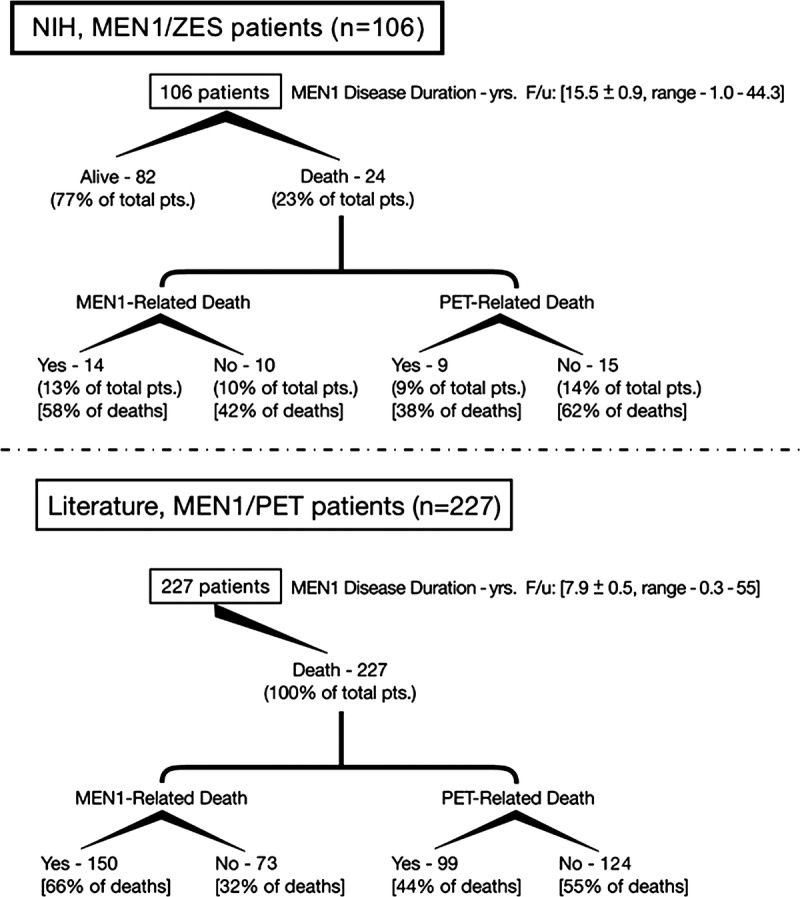
Schematic diagram of causes of death in the 2 study groups. The top panel shows the results of the 106 prospectively studied NIH MEN1/ZES patients followed for a mean of 15.5 years from the time of diagnosis of MEN1. During this time 24 patients died; 14 deaths were due to MEN1-related causes and 10 patients died of non-MEN1-related causes. The deaths were stratified as to whether they were (n = 9) or were not (n = 15) directly due to a PET causing the death. In the bottom panel a similar diagram is shown for the 227 MEN1/PET patients from the pooled literature from case reports and small series (<7 cases).
In contrast, the 24 NIH MEN1/ZES patients who died during follow-up differed from the 227 deceased MEN1/PET pooled literature patients in the following ways: the NIH patients had a 3-fold higher frequency of pituitary disease; a 5-fold higher frequency of adrenal abnormalities; a higher incidence of ZES (100% vs 67%); a 2-fold higher frequency of any carcinoids found, with an 8-fold higher frequency for gastric carcinoids and 6-fold higher frequency for bronchial carcinoids; a higher frequency of the common skin tumors found in MEN1 (collagenomas, angiofibromas); and a 12-fold higher frequency of thyroid disease (see Table 1). The deceased NIH patients also had a younger age of onset of MEN1 than the pooled literature patients (27.2 vs 36.4 yr) and were younger at the diagnosis of MEN1 (37.1 vs 45.8 yr). Many of these differences were likely due to the regular systematic follow-up visits the NIH patients underwent (mean, 15 visits) and also the more recent appreciation of the presence of various features of MEN1 (such as smooth muscle tumors, adrenal disease, skin tumors, carcinoid tumors),14,42,74,131,140,195,261,280,414,418 that were not routinely sought for in older studies.
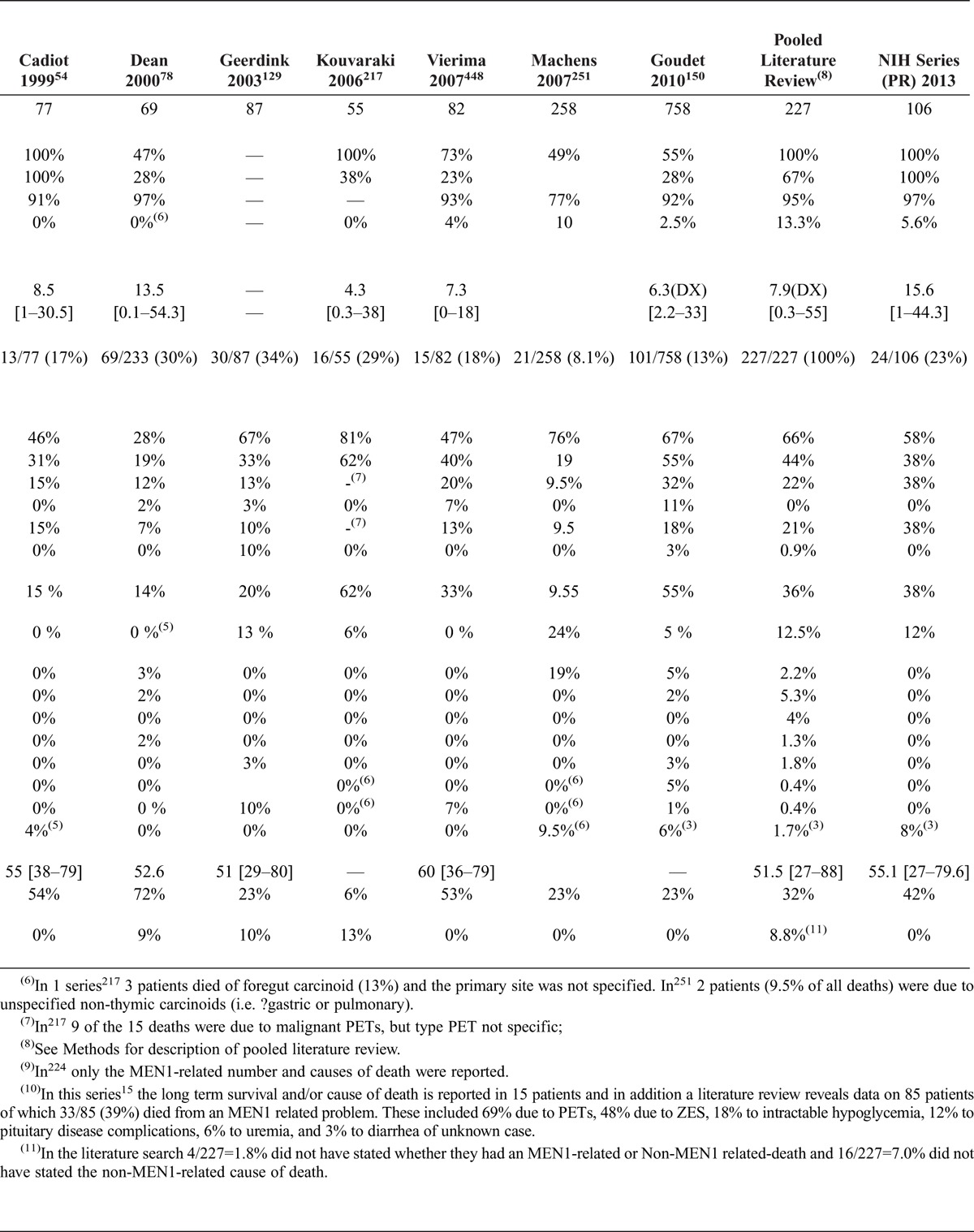
The characteristics of the 106 NIH MEN1/ZES patients and the 227 MEN1/PET patients from the pooled literature who died from a reported cause were both similar to and different from the characteristics of patients from the 15 larger literature series of all MEN1 patients whose survival data were also compared. Results were similar in all 3 groups regarding the high percentage of patients with HPT and the high frequency of PETs, which averaged 74% ± 5% (range, 36%–100%) in the larger series (see Table 12). The occurrence of ZES varied widely in the larger MEN1 literature series (range, 23%–100%; mean, 47% ± 4%); the percentage was lower in a number of these large series than in the pooled literature series and in the NIH patients.
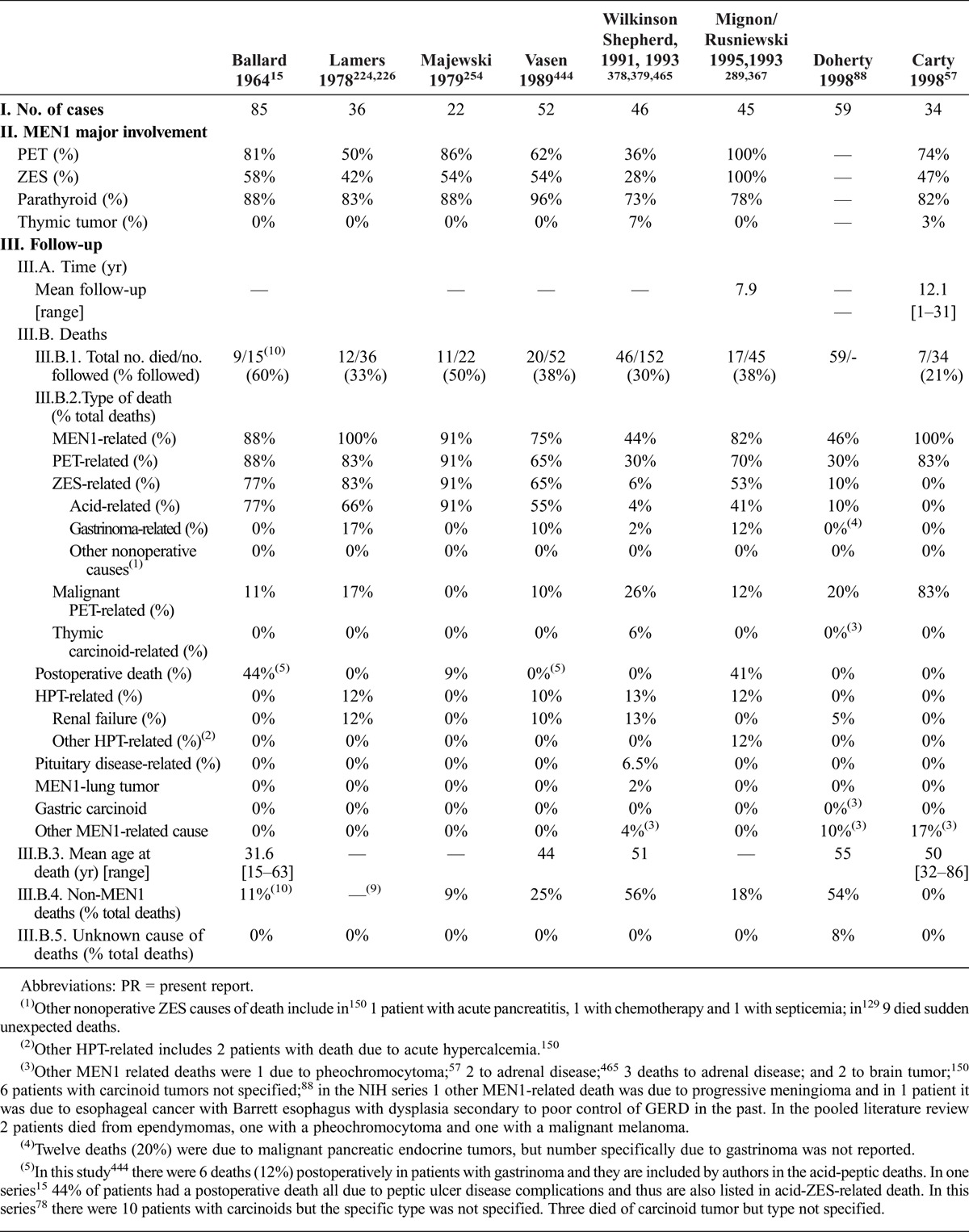
TABLE 12.
MEN1 Characteristics and MEN1-Related Causes of Death, Previous and Present Reports
Causes of Death in the 24 NIH MEN1/ZES Patients and the 227 Patients With MEN1/PET From the Pooled Literature
During the mean 15.5 years of follow-up from MEN1 diagnosis (24.1 yr from onset), 24 (23%) of the 106 NIH patients died (see Figure 1). In 14 patients (13% total, 58% of total deaths) the deaths were determined to be MEN1-related, and in 9 patients (9% of total patients, 38% of deaths) the deaths were due to a malignant PET. In no patient was death related to the acute complications of peptic ulcer disease due to uncontrolled gastric acid hypersecretion, as was commonly reported in the past.15,43,72,73,83,88,158,174,180,224,225,240,254,307,353,366,386,399,438,444,458,461,465,466 This demonstrates the effectiveness of long-term medical management of the acid hypersecretion as reported in a number of studies,69,123,136,172,192,201,268,278,279,284,287,350 because no patient underwent a total gastrectomy during follow-up at the NIH for control of the gastric acid hypersecretion. In the NIH patients all the MEN1-related deaths were due to a NET in some manner (carcinoid, PET, other endocrine tumor), and in 79% it was due to the malignant nature of the NET. In 5 patients the MEN1-related death was due to a malignant non-PET, which included 1 case of meningioma, 3 of thymic carcinoid, and 1 case of the gastrinoma causing long-standing GERD that was inadequately controlled, leading to the development of Barrett esophagus with high-grade dysplasia and esophageal cancer. A hormone excess state caused death in 2/14 patients (14%), due to an uncontrolled malignant insulinoma in 1 patient and in the 1 patient with the long-standing GERD which likely led to the development of Barrett esophagus and the development of terminal esophageal cancer. In the NIH patients a PET-related death occurred in 71% of patients, which in 64% was due to the malignant nature of the gastrinoma and in 1 case was due to a malignant insulinoma. In the NIH patients 3/14 (21%) deaths were due to carcinoid tumors and none to gastric or lung carcinoids, demonstrating the particularly aggressive behavior of thymic carcinoids, as reported in a number of studies.111,131,151,414,465 In the NIH patients there were no deaths related to pituitary disease, and, in contrast to a number of older studies,88,224,438,444,465 there were no deaths due to HPT-related disease, because the HPT was effectively treated by parathyroidectomy in all patients.104,195,317,328
When the cause of death results from the 24 NIH MEN1/ZES deceased patients are compared to the results of the 227 MEN1/PET patients from the pooled literature, the proportion dying from an MEN1-related cause was not different (68% vs 66%, p = 0.38) (see Figure 1, Table 2). The pooled literature results were similar to the NIH causes of MEN1-related death in that there were no significant differences in the percentage of deaths in all of the categories analyzed including death due to any NET, to the presence of a malignant NET, to a NET hormone excess state, to a PET, to a malignant PET, to functional PET syndrome, to pituitary disease, to HPT-related disease, or to the presence of a thymic carcinoid or other carcinoid tumor.
TABLE 2.
Causes of Death of MEN1/PET Patients (NIH Series and Pooled Literature Review)
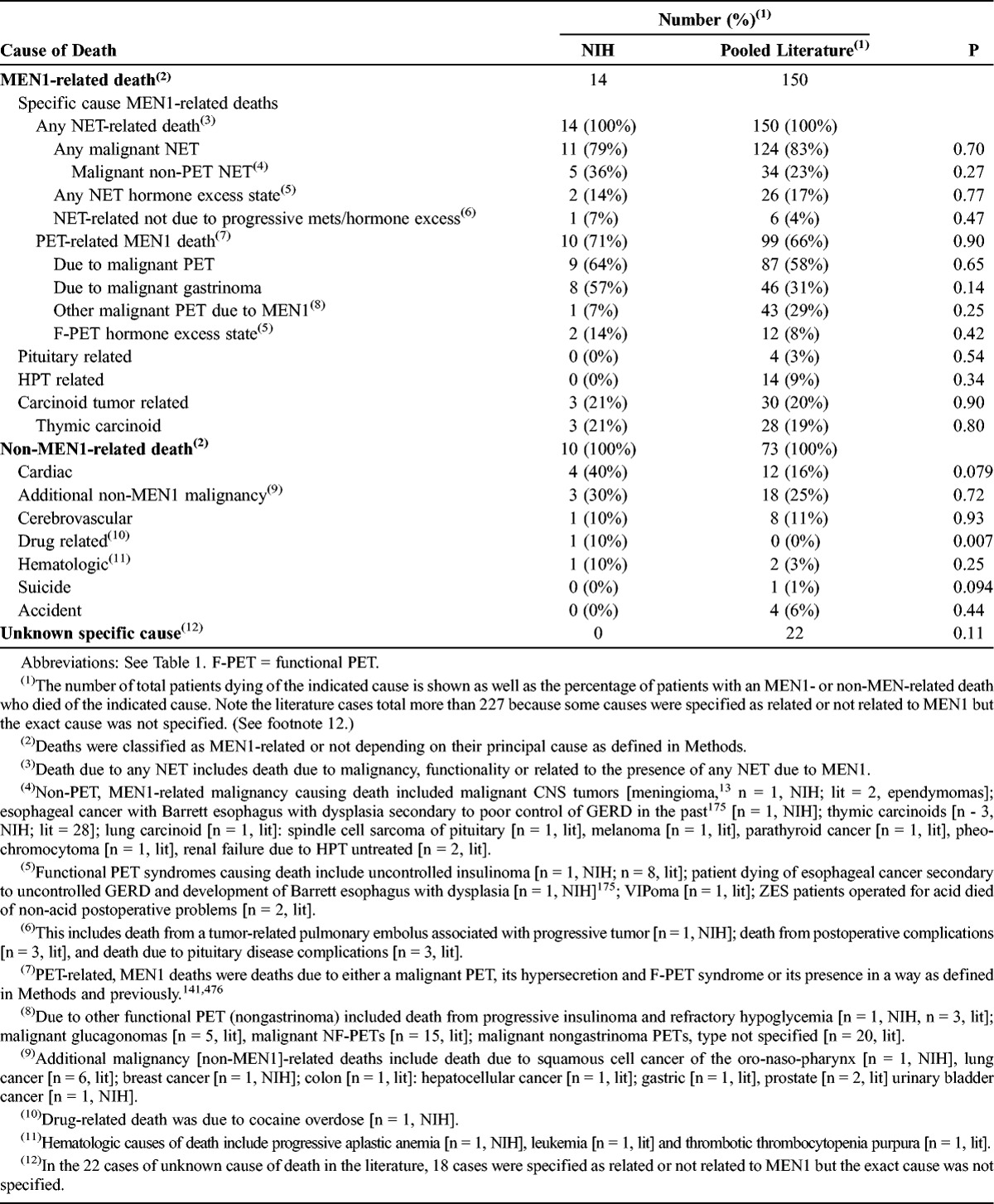
For the NIH MEN1/ZES patients, 10/24 (42% of deaths) were due to non-MEN1-related causes. The most common cause of non-MEN1 death was cardiac (4/10, 40% of non-MEN1 deaths) due to myocardial infarction, arrhythmia, or cardiac arrest (see Table 2) followed by death due to a non-MEN1-related malignancy (3/10, 30% of non-MEN1 deaths) which included 1 death due to squamous cell cancer of the oro-naso-pharynx, 1 from breast cancer, and 1 from urinary bladder cancer. Three additional non-MEN1-related deaths included 1 death from a hematologic cause (aplastic anemia), 1 from a cerebrovascular accident, and 1 from a drug overdose (cocaine). The proportion of non-MEN1-related deaths in the 227 pooled literature patients did not differ from that in the NIH MEN1/ZES patients (32% vs 42%, respectively; p = 0.38). Similarly, there were no differences in the proportion of the pooled literature patients who died of various non-MEN1-related causes, including an additional non-MEN1 malignancy, cerebrovascular disease, hematologic disorders, suicide, or accidental death. There was a significant difference in that 1 patient in the NIH series died of a drug overdose (cocaine), whereas no such death was reported in the 227 literature patients (10% vs 0 of non-MEN1 deaths, p = 0.007).
The cause of death in all 24 deaths in the NIH patients could be determined, but in 22/227 (9.7%) deaths in the pooled literature, the exact cause of death was not reported. However, in 18 cases the report specified whether the death was an MEN1-related or non-MEN1-related death, therefore in only 4/227 (1.7%) cases in the pooled literature was it unknown whether the death was MEN1 related or not MEN1 related (see Table 2).
Disease, Laboratory, and Tumoral Features in NIH MEN1/PET Patients by Survival Status
Because it is currently unknown whether the presence of MEN1 could be contributing even to the deaths that we have characterized as non-MEN1 related, to analyze for possible prognostic factors for survival we first compared various characteristics of the NIH MEN1/ZES patients who were still alive to those of the deceased NIH patients (see Tables 3–6). For general disease features of the NIH patients, there were no significant differences between patients who died and those who were alive at last follow-up in terms of sex, race, age at first visit to NIH, age at last follow-up, or duration of follow-up from onset of MEN1 or from first visit (Table 3).
TABLE 3.
General Disease Features of NIH MEN1/ZES Patients by Survival Status
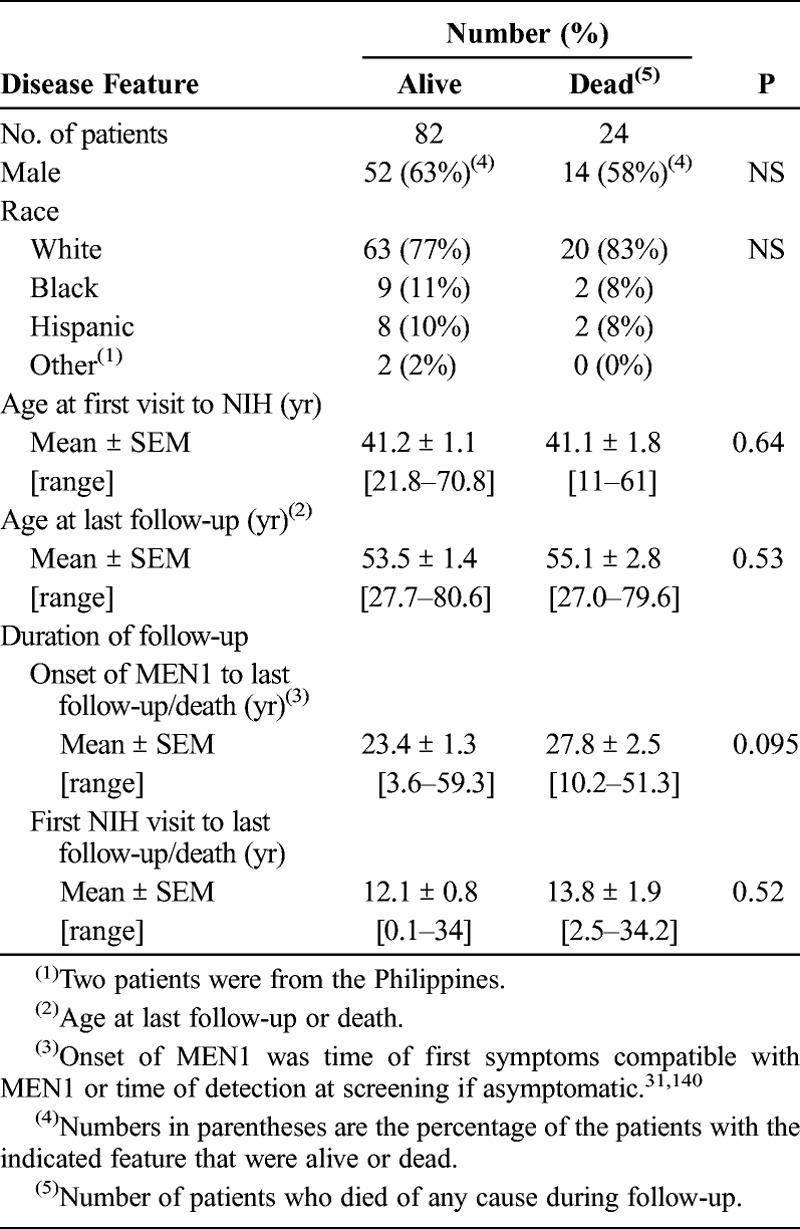
TABLE 6.
Tumoral Features in NIH MEN1/ZES Patients by Survival Status
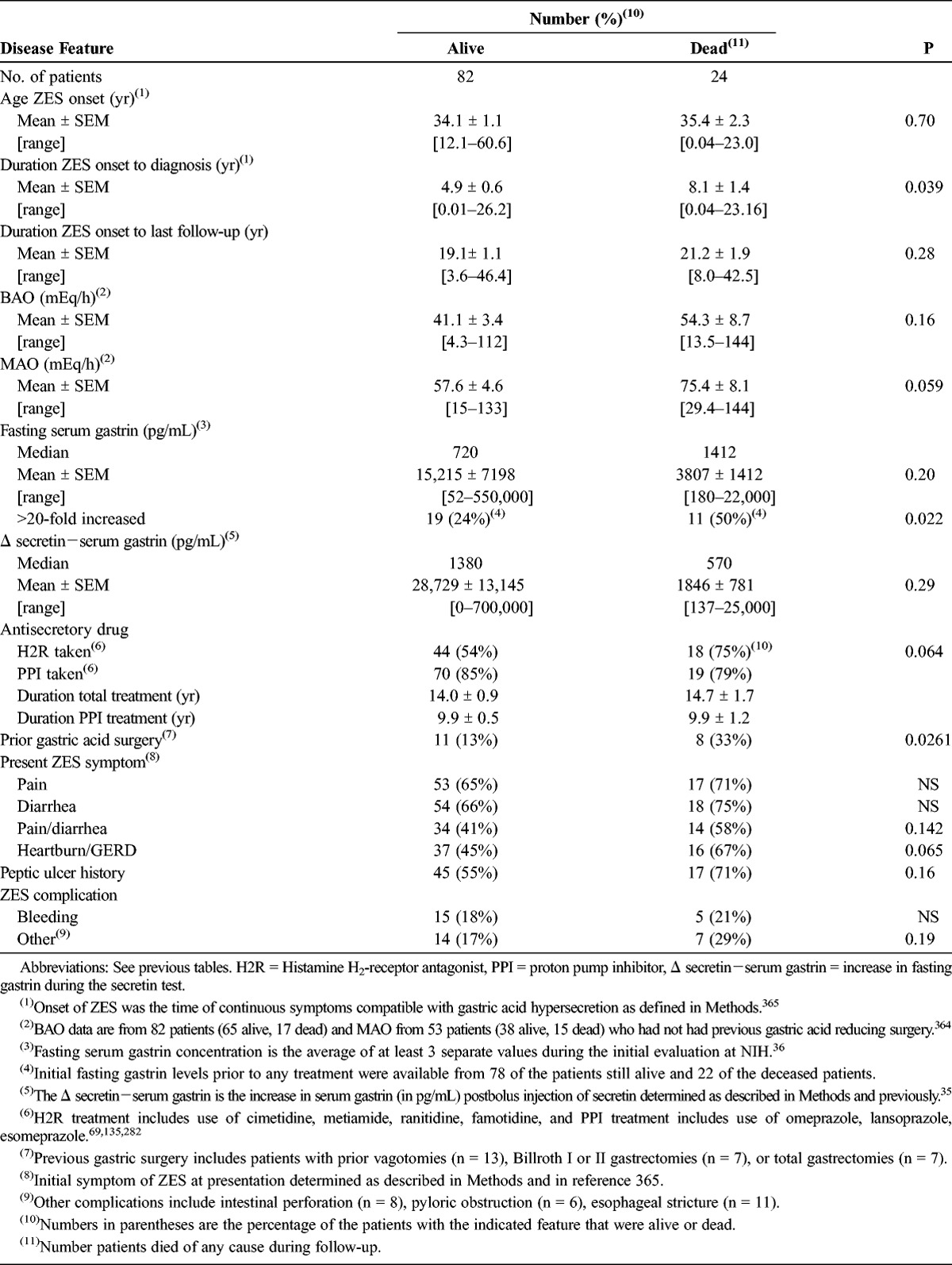
In various studies of patients with ZES a number of specific disease-related features have been reported to have prognostic significance, including disease duration,476 extent of hypergastrinemia,191,292,397,405,459,476,484 BAO,191,476 presence of peptic ulcer disease or its complications,108,117,191,199,200,483 previous gastric acid reducing surgery,476 and antisecretory drug used.476 We compared each of these features in NIH patients by survival status (Table 4). There was no significant difference between the alive and deceased NIH patients in the duration of ZES to last follow-up, the increment in gastrin during the secretin test (delta secretin), the duration or type of antisecretory treatment, peptic ulcer disease history, or occurrence of bleeding or other peptic ulcer disease complications. In contrast, deceased patients were more likely than alive patients to have had a very high fasting gastrin level (>20-fold elevated, p = 0.022), a longer delay in diagnosis (8.1 vs 4.9 yr, respectively, p = 0.039), a prior gastric acid reducing surgical procedure (33% vs 12%, p = 0.026), to have taken histamine H2-receptor antagonists for a longer time (p = 0.064), to have a history of heartburn/GERD (p = 0.065), and to have a higher MAO (p = 0.059).
TABLE 4.
Clinical and Laboratory ZES Features in the NIH MEN1/ZES Patients by Survival Status
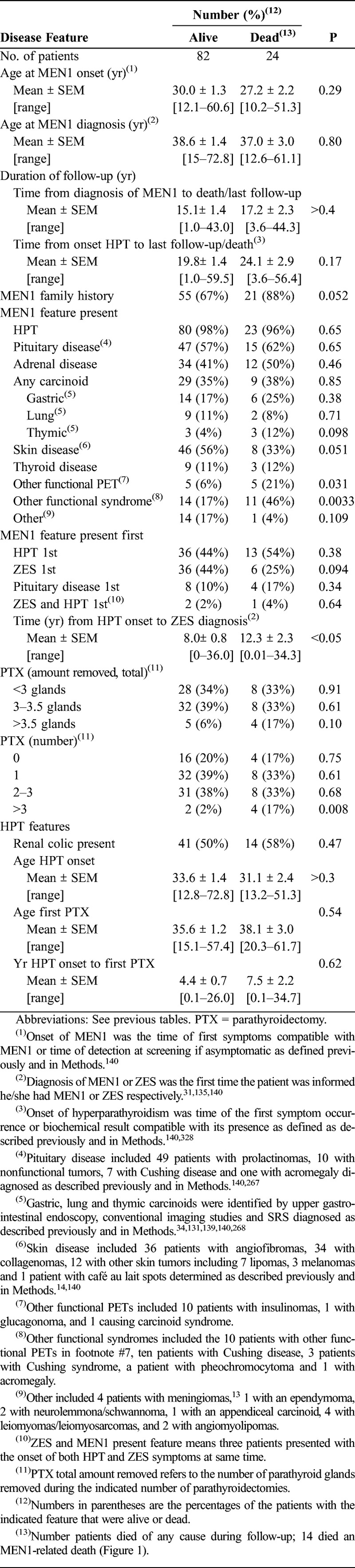
In various studies a number of features of MEN1 patients have been reported to have prognostic significance, including age at MEN1 onset/diagnosis;46,150,383 disease duration;78,141 presence of a family history;46,150 presence of any PET including gastrinoma, glucagonoma, insulinoma, VIPoma, somatostatinoma, and nonfunctional;71,88,150,217,233,234,389,465 presence of adrenal disease;150,228,388,390,465 presence of lung,368,465 gastric,141,326 or thymic carcinoid tumors;111,131,150,151,413,414,465 and severity and control of HPT.46,88,224,226,328,444,465 We compared each of these features in NIH patients by survival status (Table 5). Deceased patients, compared to alive patients, more frequently had >3 parathyroidectomies (p = 0.008) to control the HPT, suggesting they may have had more severe HPT; more frequently had a gastrinoma with another functional syndrome such as carcinoid syndrome or Cushing syndrome/disease (p = 0.0033); and more frequently had gastrinomas with another functional PET, particularly insulinomas (p = 0.031). Deceased patients tended to have a positive family history of MEN1 more frequently than alive patients (88% vs 67%, p = 0.052) and they were less likely to have had a cutaneous manifestation of MEN1 detected (p = 0.051). There was no significant difference between the 2 patient groups in their age at MEN1 onset or diagnosis or age at onset of HPT or first parathyroidectomy; in the duration of follow-up from time of MEN1 diagnosis, from onset of HPT to last follow-up, or from onset of HPT to first parathyroidectomy; in the number of parathyroid glands removed; presence of renal colic; or any other feature of MEN1 including frequency of pituitary disease, HPT, adrenal disease, any carcinoid tumor, any MEN1-related skin disorders, or the initial MEN1 presenting feature.
TABLE 5.
Clinical and Laboratory MEN1 Features in NIH MEN1/ZES Patients by Survival Status
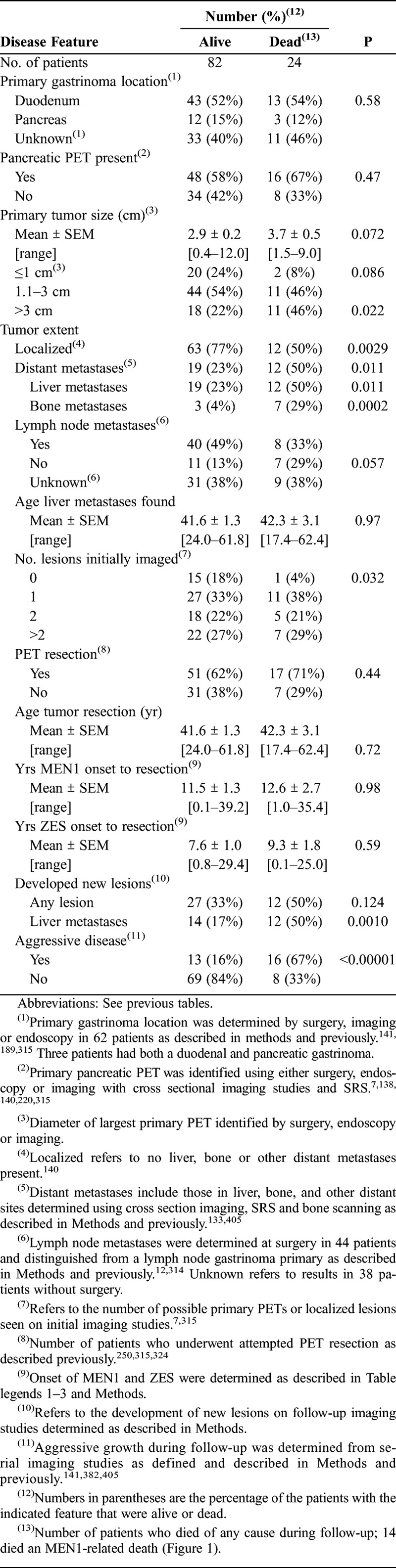
Numerous studies, but not all, report that various PET tumoral features and their treatment, such as PET size, extent, location, growth rate, distant metastases, PET resection, and duration of the PET may all have prognostic significance for either survival or for the development of liver metastases, which is the most important determinant of survival,54,141,191,288,338,340,434,459,476 in both patients with sporadic PETs90,118,133,141,252,288,320,398,405,459,476 and in a few studies of patients with MEN1.54,88,141,150,195,217,233,234,433,434 We compared each of these tumoral variables in NIH patients by survival status (Table 6). Large primary tumor size (>3 cm) (p = 0.022), presence of liver metastases initially (p = 0.011), development of bone metastases (p = 0.0002), development of liver metastases (p = 0.0010), presence of a PET on initial imaging (p = 0.0322), and aggressive tumor growth (p < 0.00001) were all more frequent in the deceased patients than in those still alive at last follow-up. In contrast, the location of the primary gastrinoma (duodenal vs pancreatic), the presence of lymph node metastases, the age when liver metastases were found, whether a PET resection was performed or not, the age a PET resection was performed, or the duration from ZES onset to the tumor of a PET resection did not differ between the 2 groups of patients.
Clinical and Tumoral Features in NIH MEN1/ZES Patients Who Died From MEN1-Related and non-MEN1-Related Causes
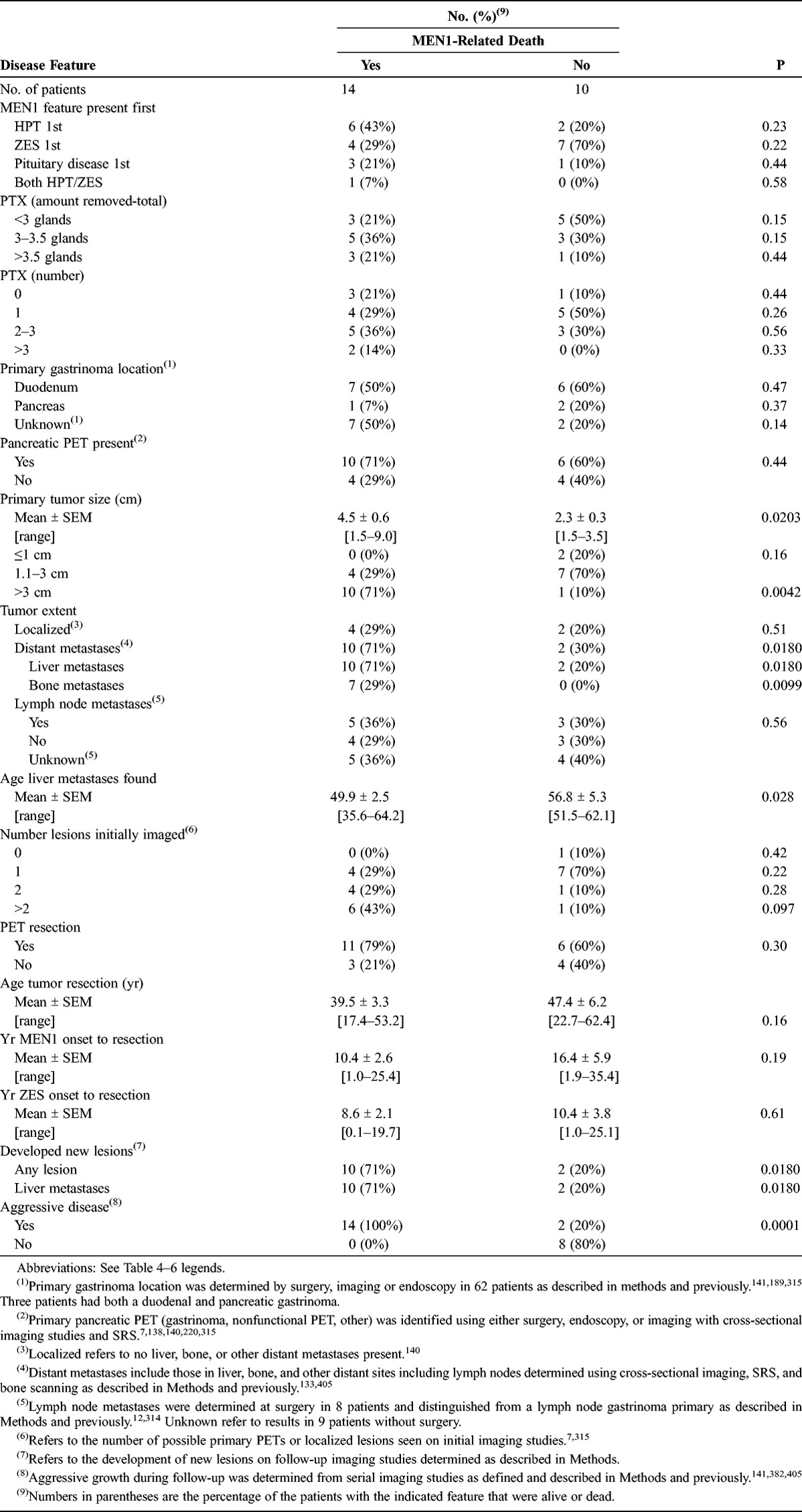
To investigate further prognostic factors that might be associated with an MEN1-related death, we compared various clinical, laboratory, and tumoral features of MEN1 and ZES for the NIH MEN1/ZES patients classified as having either an MEN1-related death or a non-MEN1-related death. We compared the clinical and laboratory features of MEN1 or ZES and tumoral features that were compared in the NIH patients by survival status in Tables 5 and 6 in patients who had either an MEN1-related death or a non-MEN1-related death (Tables 7 and 8). We found no significant differences for any of the 34 clinical or laboratory characteristics compared. In particular, there was no significant difference in fasting gastrin level, duration, or other features of various MEN1-related manifestations, many of which have been reported to have prognostic significance in some studies.46,54,71,141,151,152,414,465 In contrast, for a number of the tumoral features in the NIH patients, there was a significant difference between patients who did or did not have an MEN1-related death. Specifically, of the 42 tumor features compared, those significantly associated with an MEN1 disease-related death included an increased primary tumor size (p = 0.0203), particularly >3 cm (p = 0.0042); the presence of liver metastases (p = 0.0180), bone metastases (p = 0.0180), or any distant metastases (p = 0.0180); the number of PET lesions initially imaged, particularly if ≥2 were seen (p = 0.0180); a younger age of developing liver metastases (p = 0.028); the development of any new lesions during follow-up (p = 0.0180); the development of liver metastases during follow-up (p = 0.0180); or the presence of tumors demonstrating aggressive growth (p = 0.0001). Whether a previous PET resection occurred has been reported to be an important tumor feature in some studies of NIH MEN1/ZES patients22,150,195,217,217,234 and to have prognostic significance; however, we did not find it to be important in the current study as a prognostic factor for an MEN1-related death (p = 0.30). Similarly, in contrast to sporadic ZES, a number of tumoral features reported to have prognostic value for disease-related death118,191,201,279,287,320,459,476 were not found to be associated with an MEN1/ZES-related death in the current study, including the presence of a pancreatic PET rather than a duodenal PET (p = 0.47); the presence of any pancreatic PET (p = 0.44); the failure to undergo a PET resection (p = 0.30); or the presence of lymph node metastases (p = 0.56).
TABLE 7.
Clinical MEN1 and ZES Features in Deceased NIH MEN1/ZES Patients With or Without MEN1-Related Death
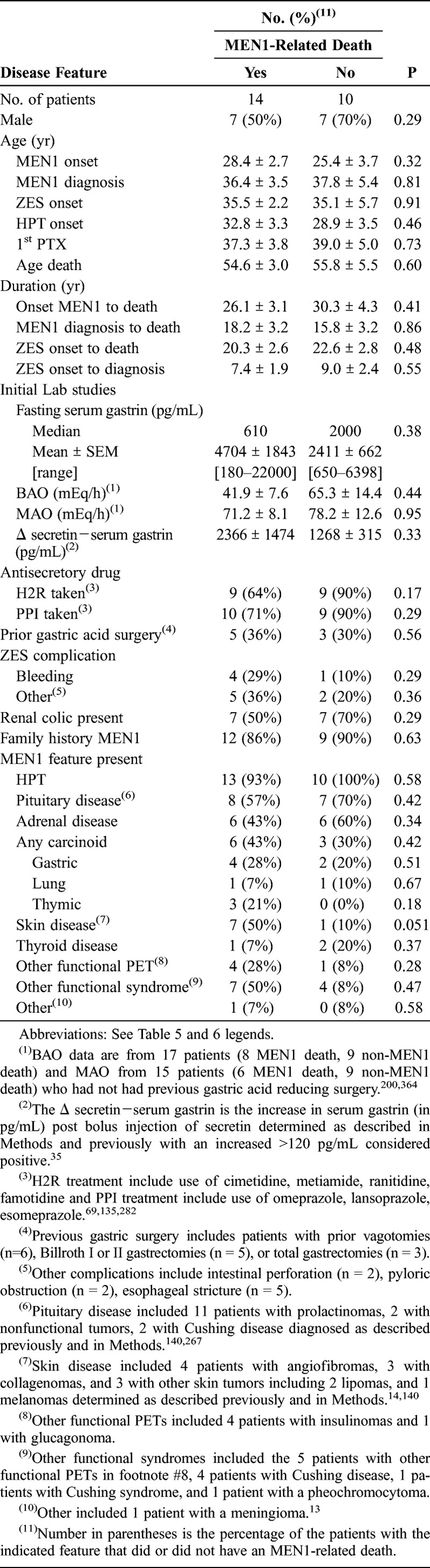
TABLE 8.
Various MEN1 Clinical and Tumoral Features in Deceased NIH MEN1/ZES Patients With or Without an MEN1-Related Death
MEN1 and Tumoral Features in 227 MEN1/PET Patients From the Pooled Literature Who Died From MEN1-Related and non-MEN1-Related Causes
We carried out a similar analysis to identify possible prognostic factors determining an MEN1-related death in the 227 MEN1/PET patients from the pooled literature (Table 9). For various MEN1 features there was no significant difference between the percentage of patients who died from an MEN1-related or unrelated cause, including HPT (95% vs 96%, respectively); pituitary disease (23% vs 20%); adrenal abnormality (8.9% vs 8.7%); ZES (66% vs 75%); another functional PET (22% vs 17%); a nonfunctional PET (29% vs 18%); or a CNS, skin, or smooth muscle tumor (0–3.5%). In contrast, MEN1/PET patients from the pooled literature with an MEN1-related death more frequently had a carcinoid tumor (26% vs 9%, p = 0.0048), and in particular a thymic carcinoid tumor (22% vs 3.3%, p = 0.006) but not a gastric, lung, or intestinal carcinoid. Almost reaching significance was the presence of PETs other than gastrinomas in patients with an MEN1-related death (47% vs 33%, p = 0.058), whereas thyroid disease showed a trend toward higher occurrence in patients with a non-MEN1-related death (0 vs 2.95%, p = 0.050).
TABLE 9.
MEN1 Features in 227 Deceased Literature MEN1/PET Patients With or Without MEN1-Related Death
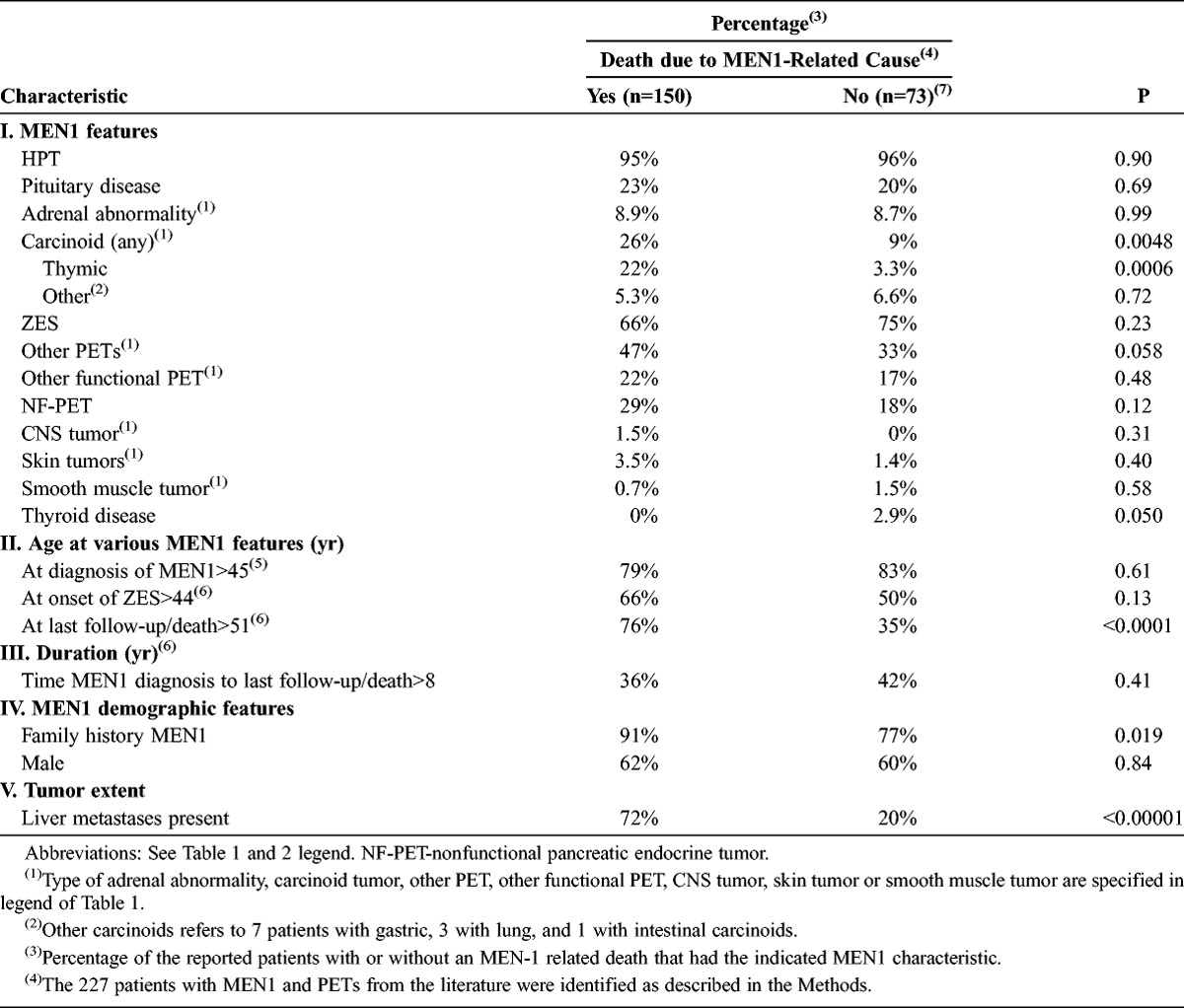
The pooled literature MEN1/PET patients with an MEN1-related death died at a younger age than those with a non-MEN1-related death (51.1 ± 1.2 vs 53.0 ± 2.1 yr), with 51% dying before age 46 years compared to 29% of patients with non-MEN1-related deaths (p = 0.002) (see Table 9). In contrast, there was no difference in the age at diagnosis of MEN1 (44.9 ± 1.2 vs 49.0 ± 2.4 yr), with 79%–83% of both groups aged >45 years at diagnosis; nor in the age of onset of ZES (43.9 ± 1.2 vs 46.6 ± 2.2 yr), with 50%–66% aged >44 years at the time of diagnosis. Similarly, there was no difference in sex frequency in patients dying from an MEN1-related- or non-MEN1-related cause (60%–62% male); however, a family history of MEN1 was significantly more frequent in patients dying from an MEN1-related cause than in patients with a non-MEN1-related cause of death (91% vs 77%, p = 0.019), as was the occurrence of liver metastases (72% vs 20%, p < 0.0001).
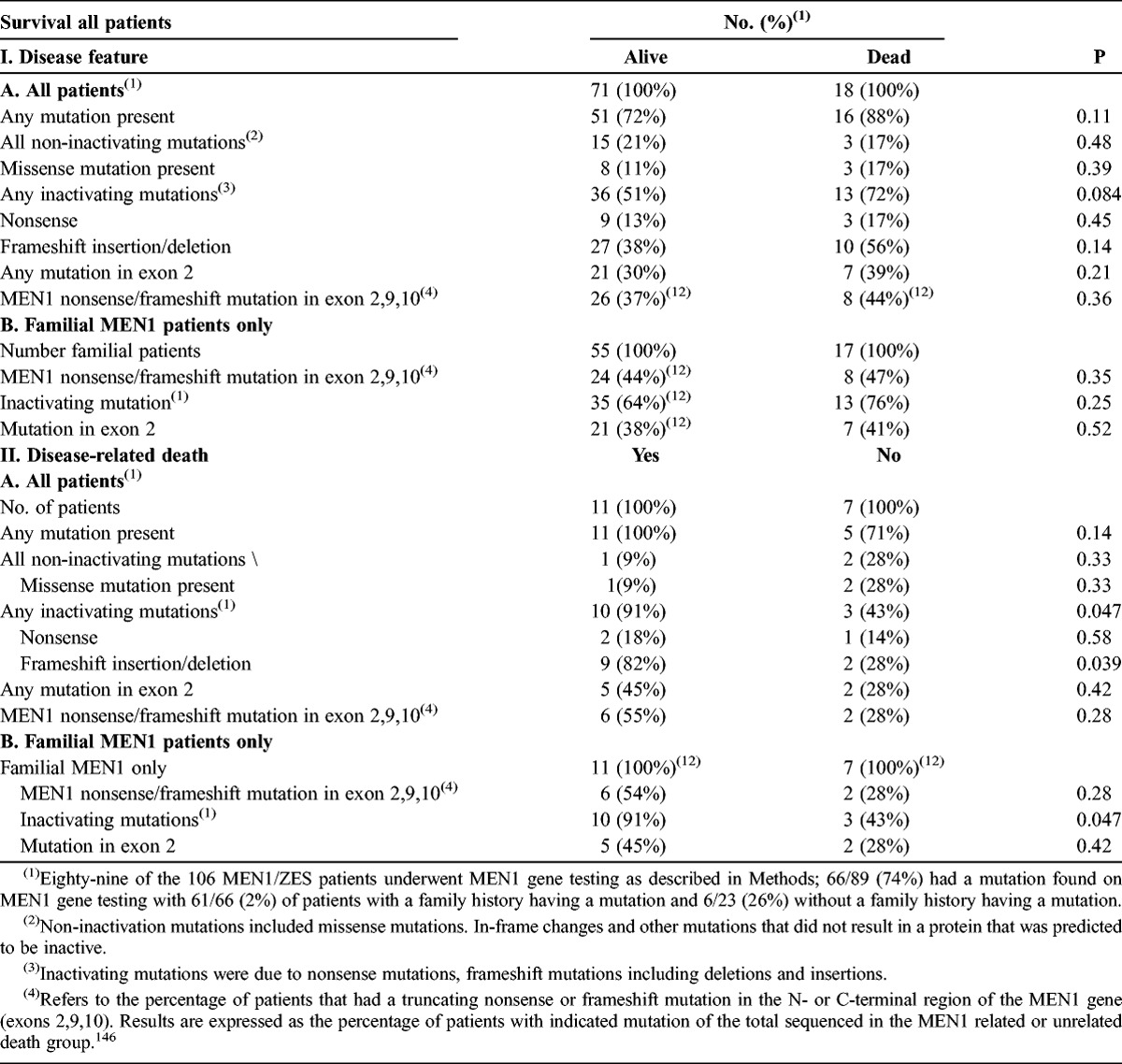
Effect of Different MEN1 Gene Mutations on Total and MEN1 Disease-Related Survival for 106 NIH MEN1/ZES Patients
Although in most studies no genotype-phenotype correlations are reported in MEN1 patients with the different manifestations or tumor features,143,419,420,457 in a few studies the presence or absence of certain MEN1 gene mutations (that is, exon 2 or nonsense/frameshift mutations in exon 2, 9, 10)22,217 is reported to have prognostic significance. To explore this possibility in the 106 NIH MEN1/ZES patients, we correlated the presence or absence of various types and locations of MEN1 gene mutations with both total survival and MEN1 disease-related survival (Table 10). For the 89 patients who underwent MEN1 gene testing, the location of the MEN1 gene mutation (exon 2, 8, or exon 9) did not have prognostic significance nor did the presence of a mutation that was not predicted to inactivate menin (missense, nonframeshift changes). However, inactivating mutations overall showed a trend to being more frequent in patients who died of any cause (p = 0.084), and were borderline more frequent in patients dying from a disease-related cause (p = 0.047) both in all patients and in those with only familial MEN1 (p = 0.047). The presence of frameshift mutations showed a similar result.
TABLE 10.
MEN1 Gene Sequencing Results With Overall Survival and With Presence or Absence of an MEN1 Disease-Related Death
Total Survival and MEN1 Disease-Related Survival for 106 NIH MEN1/ZES Patients
To assess the total survival as well as the MEN1 disease-related survival for the 106 prospectively studied NIH MEN1/ZES patients, we analyzed both types of survival in the form of Kaplan-Meier plots (Figure 2), using time from onset of MEN1 (24.5 ± 1.2 yr; range, 3.6–59.3 yr) or time from diagnosis of MEN1 (15.5 ± 0.9 yr; range, 0.96–44.3 yr). The 5-year survival was excellent (97%–100%) for each of the 4 categories assessed in the NIH patients (that is, total survival from MEN1 onset or diagnosis, and MEN1 disease-related survival from MEN1 onset or diagnosis) (Table 11). The total survival curve for the NIH MEN1/ZES patients for time from MEN1 onset was not significantly different from the MEN1 disease-related survival (hazard ratios [HR] for onset or diagnosis, 1.7; 95% CI, 0.9–3.2) (see Figure 2, panel A). The median total survival time from time of MEN1 onset was 42.8 yr (95% CI, 25–69 yr), whereas for MEN1 disease-related survival, the median survival time was >50 years. For the NIH patients, the median total survival from time of diagnosis was 36.5 yr (95% CI, 11–73 yr); it was similar for MEN1-disease related survival (see Figure 2, panel B). The 20-year disease-related survival for NIH patients, from either diagnosis or onset of MEN1, remained excellent with values of 80% and 93%, respectively, whereas the 20-year total survival was 67.5% and 90%, respectively.
FIGURE 2.
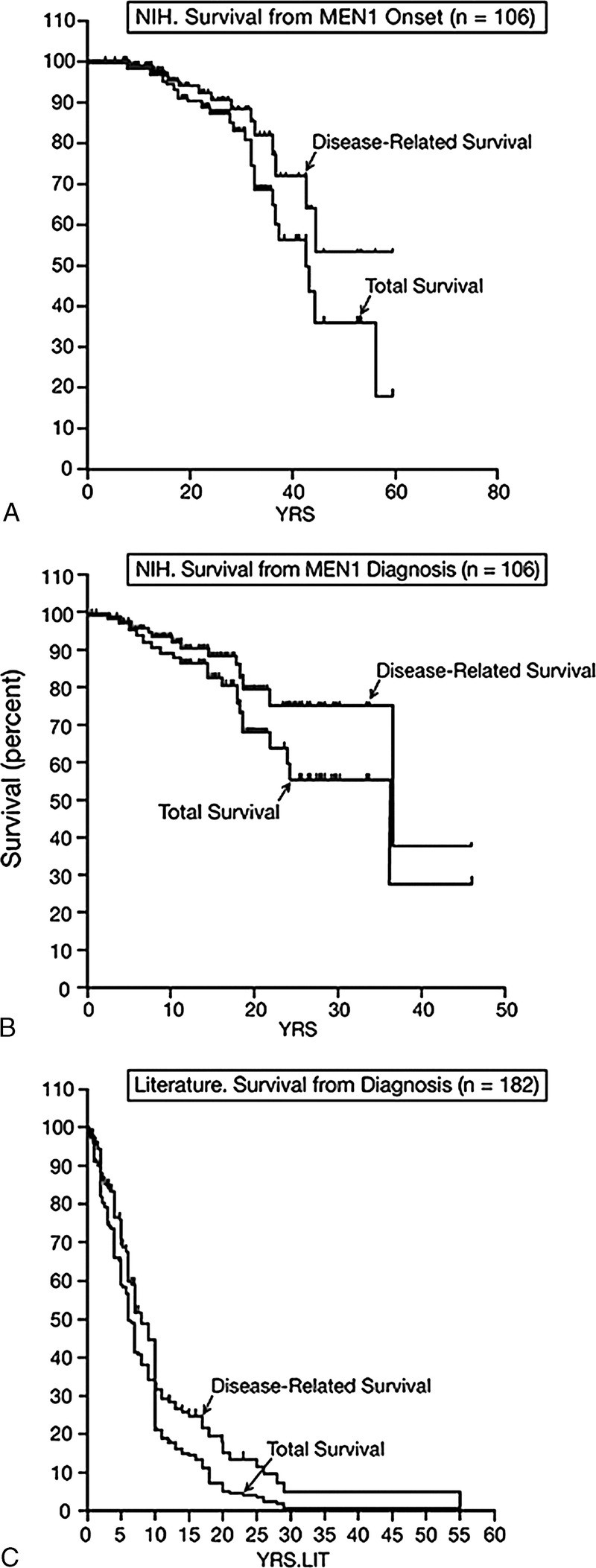
Total and disease-related survival for the 2 groups of MEN1/PET patients studied. In the top 2 panels survival data for the 106 NIH MEN1/ZES patients are shown in Kaplan and Meier plots. The top panel shows disease-related and total survival from the time of MEN1 onset and the middle panel from the time of MEN1 diagnosis. The bottom panel shows total survival and disease-related survival from the time of MEN1 diagnosis for the 227 MEN1/PET patients from the pooled literature review of case reports and small series.
TABLE 11.
Survival in MEN1/PET Patients From NIH and the Literature
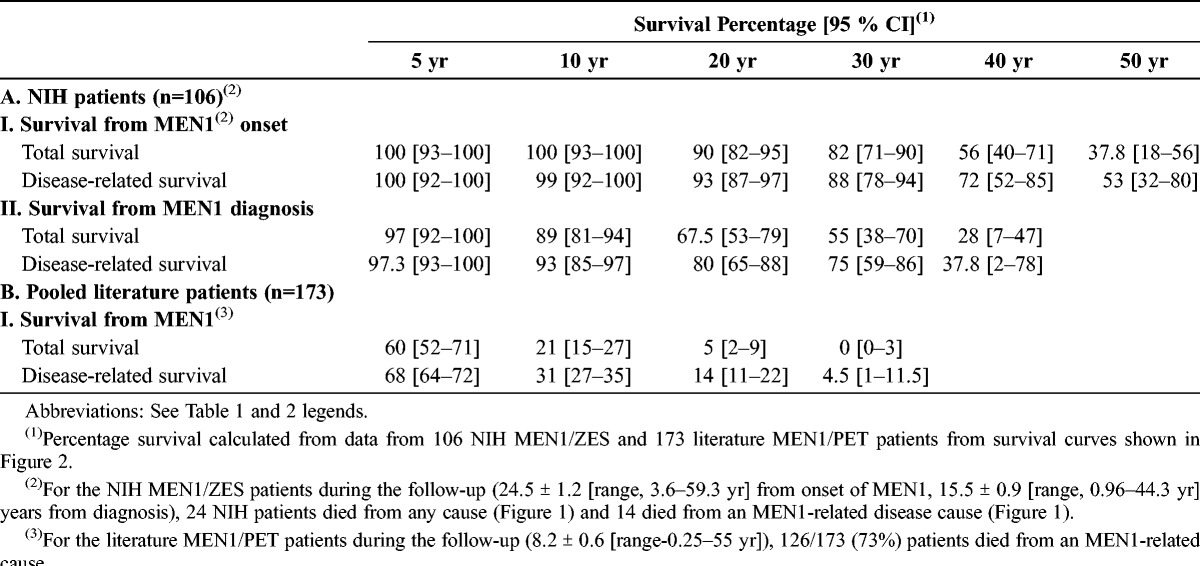
In contrast, when a similar survival analysis was performed for the 227 MEN1/PET patients from the pooled literature, both the total survival and the disease-related survival were much poorer, with 5-year survivals of 60% and 68%, respectively, and 20-year survivals of 5% and 15%, respectively (see Figure 2, panel C; Table 11). The median survival times were also shorter for the pooled literature data than for the NIH data, with a mean of 6.1 years (95% CI, 5.7–7.0 yr) for the total survival for pooled literature patients and 8 years (95% CI, 7.5–9.3 yr) for disease-related survival, which were significantly different (p = 0.0011).
DISCUSSION
Classically, patients with MEN1 develop adenomas or hyperplasia of multiple endocrine glands, with HPT due to parathyroid hyperplasia the most frequent abnormality, followed by functional or nonfunctional PETs, pituitary adenomas, adrenal tumors, and thyroid adenomas, as discussed above in the Introduction. It has been increasingly recognized that these patients develop additional tumors including carcinoid tumors (thymic, gastric, bronchial, and rarely intestinal); characteristic tumors of the skin (angiofibromas, collagenomas, lipomas, melanomas); CNS tumors (meningiomas, ependymomas, schwannomas); and smooth muscle tumors (leiomyomas, leiomyosarcomas). (See Introduction for details.)
Although many aspects of MEN1 have been well studied, one of the most important clinical areas, that affects many aspects of the management of these patients, is a clearer understanding of the natural history of the late course of the disease.140,141,276 At present there is little prospective information available, particularly related to causes of death and prognostic factors that are important to identify various disease courses of patients in the late stages of MEN1.195 This lack of information has occurred for a number of reasons, including a number of changes over the last few years that have markedly altered the natural history of MEN1, and likely the causes of death.
First, most studies in the literature are retrospective; many contain only small numbers of cases, which limits analyses; and most of the larger studies contained pooled data from different centers, leading to data variation and the frequent use of historical records or retrospective data to determine causes of death; and therefore they have limitations.
Second, in various studies where 20%–70% (mean 54%, 18 series) of the MEN1 patients developed ZES,15,49,63,73,102,152,189,208,212,261,264,298,348,387,418,436,436,444 the most common functional PET seen in patients with MEN1,140,195,261,418 the uncontrolled gastric acid hypersecretion, which is characteristic of ZES, 200,201,279,364 was a leading cause of early death.15,43,72,73,83,88,158,180,224,225,240,254,307,353,366,386,399,438,444,458,461,465,466 Gastric acid hypersecretion accounted for up to 73%–91% of all deaths in some early series.15,195,224,254,444
At present the situation is entirely different, with the development of effective means to treat the gastric acid hypersecretion; first surgically with total gastrectomy described in the 1950–1960s,108,424,483 followed by increasingly effective medical therapy, first with histamine H2-receptor antagonists69,135,178,193,197,266,272,278,295 and later with H+, K+ ATPase inhibitors (proton pump inhibitors).123,171,189,192,227,270,278,284 Proton pump inhibitors are the drugs of choice controlling the acid hypersecretion in almost every ZES patient, both acutely and long-term,123,171,189,192,227,266,270,278,281,284,295,350 because tachyphylaxis does not develop.123,171,189,192,227,270,278,281,284 The availability of proton pump inhibitors has almost completely eliminated the lethal complications of peptic ulcer disease (perforation, bleeding, penetration) in MEN1/ZES patients which were so frequent in older studies,15,17,43,72,73,83,88,107,129,140,158,180,189,195,224,225,240,254,307,310,353,366,386,399,438,444,458,461,462,465,466,474 and therefore their use has changed the natural history of MEN1 in regard to times and causes of death. To our knowledge, at present there are no prospective studies of the natural history of MEN1 and the causes of death that reflect these changes in the control of acid hypersecretion.
Third, in other older studies, uncontrolled HPT, leading to nephrolithiases and renal failure3,245,465 was not an uncommon course of death.15,32,68,88,129,224,285,438,444,465,466 With the increased understanding of the diffuseness of the parathyroid disease (hyperplasia affecting all glands) requiring either a 3.5-gland parathyroidectomy or 4-gland parathyroidectomy with a parathyroid implant to effectively control the HPT long-term,11,42,44,104,169,211,328,330,352,376 renal failure due to uncontrolled HPT is now a rarely reported cause of death (Table 12).54,57,78,129,149,150
TABLE 12.
MEN1 Characteristics and MEN1-Related Causes of Death, Previous and Present Reports
Fourth, it has become increasingly apparent that MEN1 patients develop a number of tumors that are different from the classical endocrine tumors or hyperplasia originally described. These include both other endocrine tumors (carcinoids of thymus, stomach, lung, rarely intestinal) and nonendocrine tumors (CNS tumors [meningiomas, schwannomas, ependymomas], skin tumors [angiofibromas, collagenomas, lipomas, melanomas], and smooth muscle tumors [leiomyomas, leiomyosarcomas].13,14,34,56,66,74,111,131,151,176,195,228,261,274,368,388,390,393,413,428,465 Of these, particularly thymic carcinoids, which occur primarily in males, occur characteristically later in the MEN1 course (mean age, 42–46 yr), are generally very aggressive, and hence are increasingly a cause of death.111,130,131,151,408,413,414,465 Similarly, in some studies lung carcinoid tumors as well as gastric carcinoids/NETs also can pursue an aggressive course.34,40,94,150,253,326,360,465 The fact that MEN1 patients are living longer150 is raising the likelihood that a number of these more newly described tumor types in MEN1 patients will play an increasing role in long-term survival as most occur later in the course of patients with MEN1,13,131,195,261,280,326,418 and their effect has generally not been evaluated.
Fifth, genetic diagnosis and family screening are being used increasingly to diagnose patients with MEN1 and have resulted in its earlier diagnosis.42,150,215,246,309 This earlier diagnosis combined with increasingly effective treatments of the various hormone excess states, HPT, and PETs,466 will likely have important effects on the natural history and causes of death, which will no doubt be different from older reports.
To address the issue of the largely unclear course of MEN1 patients late in their disease history at present, as well as the causes of death at present, and to attempt to identify prognostic factors for different causes of death, we conducted the present study of the long-term courses of 106 MEN1 patients with PETs who were prospectively followed over a 24 ± 1.2 year period (range, 3.6–59.3 yr) from MEN1 onset. As stated above in the previous sections, we compared these results with the results of a literature review of patients who had MEN1 with a PET who died of non-gastric acid related cause. To compare our results with a typical general population of MEN1 patients with advanced disease, we compared our series results to those of MEN1 patients reported in series with >10 cases of MEN1 patients with follow-up data (see Tables 12 and 13). In this group 60% had a PET and 54% had ZES, which are similar to the percentages reported in most large series of MEN1 patients.140,167,182,189,254
TABLE 13.
Non-MEN1-Related Causes of Death, Previous and Present Reports
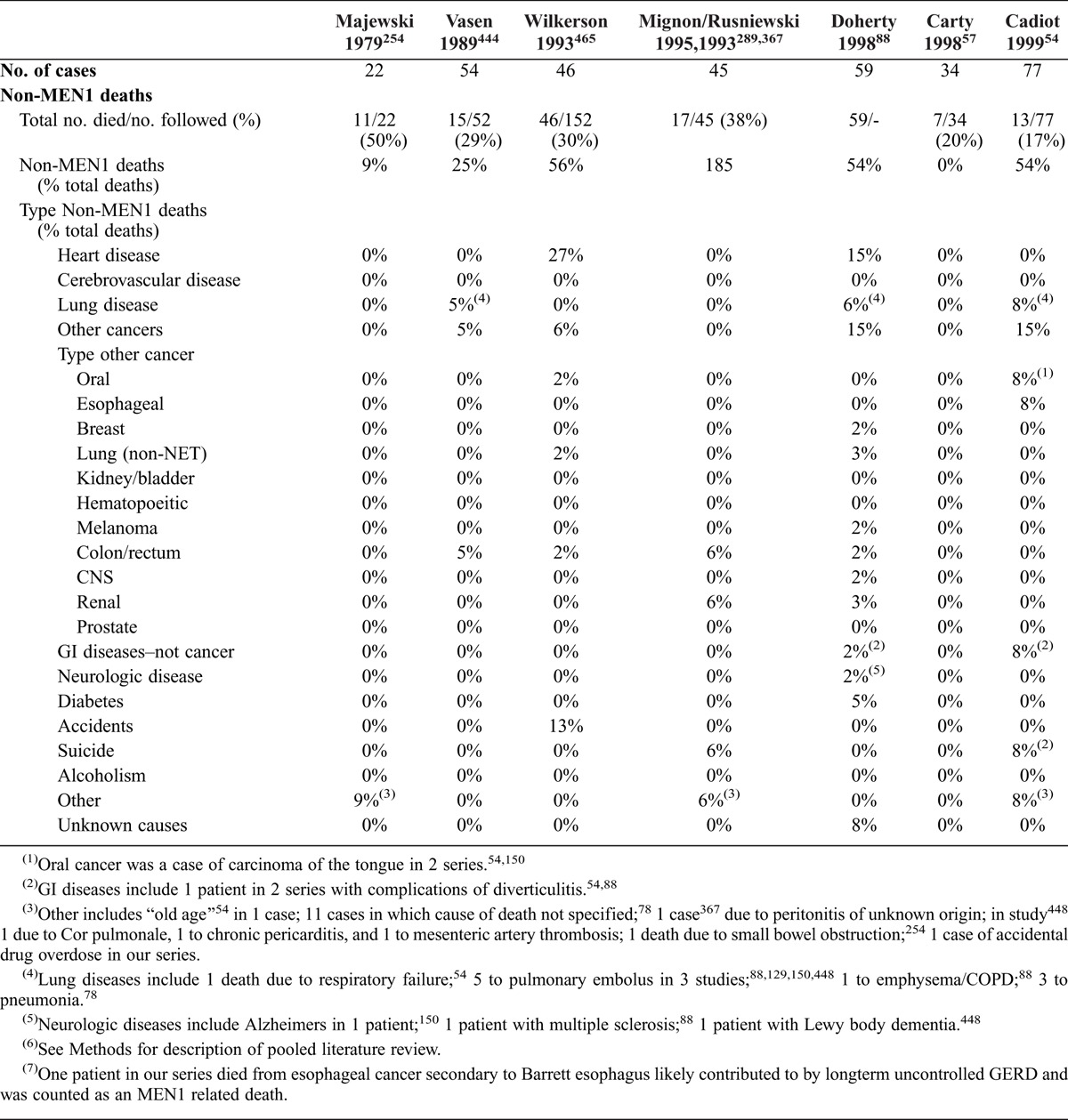
TABLE 13.
Non-MEN1-Related Causes of Death, Previous and Present Reports
The current study has none of the limitations reported in previous studies outlined above. It involves a large number (n = 106) of patients with MEN1/ZES. The patients were prospectively studied and reassessed at regular intervals using a standardized protocol. All patients received standard treatments to control hormone excess states and to deal with potentially malignant tumors or with advanced malignant disease; therefore the results are representative of the current acceptable treatment of these patients. Specifically, gastric acid hypersecretion in all patients with active ZES was controlled, no complications of peptic disease developed, and no patients died from a peptic ulcer disease-related complication. Other hormone excess states due to other PETs or NETs were treated with either surgery or medical therapy (octreotide, interferon, other medical therapies).194,196,221 Hyperparathyroidism was treated by multigland parathyroidectomies as outlined previously,104,211,317,328 and no patients developed renal failure due to nephrolithiases. Other NETs such as thymic, gastric, or lung carcinoid tumors were treated as described previously.131,326,368 Lastly, the cause of death could be established in all patients who died during follow-up and was classified as MEN1 related or non-MEN1 related using the criteria outlined in the Methods section.
Survival Data
Whether patients with MEN1 have premature death with shortened survival is controversial in some previous studies.78,88,101,129,465 In 2 studies88,101 the survival of patients with MEN1 did not differ from that of unaffected individuals; however, 3 other studies78,129,465 concluded that MEN1 patients had premature death with shortened survival. In one of the latter studies,129 the mean age at death of female MEN1 patients was 47 years and of male patients was 55 years, which was significantly younger than the age at death of Dutch control non-MEN1 female patients (75.6 yr, p = 0.032), or of control non-MEN1 male patients (70.1 yr, p = 0.001). A second series reporting premature death78 was a large, retrospective study of 228 MEN1 patients from the Mayo Clinic whose mean age at diagnosis of MEN1 was similar to that of our 106 NIH MEN1/ZES patients (39.2 vs 38.3 yr, respectively). In that study78 the expected survival at 20 years from age of diagnosis of the MEN1 for a matched control group was 80%, compared with 64% for their MEN1 patients, which was significantly less (p < 0.001) than their controls. The survival of their MEN1 patients is similar to the overall survival of our 106 MEN1/ZES patients prospectively followed, which was 67.5% at 20 years from diagnosis, suggesting that our patients also had a premature death.
However, in the current prospective study a number of results suggest that these patients are living longer than reported in many previous series. First, during the long follow-up (mean, 15.5 yr from MEN1 diagnosis; 24.5 yr from MEN1 onset), 23% of the 106 NIH MEN1/ZES patients died, which is comparable to the 28% ± 3% reported in 12 of the general MEN1 series in the literature that reported mortality percentages (1386 patients, see Table 12). However, the deaths in the NIH MEN1/ZES patients occurred over more than twice as long a follow-up period as the follow-up period reported in the literature cases (15.5 [NIH] vs 7.7 ± 1.0 yr from diagnosis of MEN1, n = 6 series]. Similarly for the 227 MEN1/PET deceased patients from the pooled literature, whose data came from 108 separate reports, they represented 18.8% ± 1.9% (data: 36 reports) of the total MEN1 patients being followed in these reports. However, similar to the 12 general MEN1 literature series, the percentage of patients that died in the pooled literature series occurred over less than half of the follow-up time (6.9 ± 1.3 yr) of the NIH series.
Second, if one compares the data from different series, the mean age at death of MEN1 patients varies markedly. In our 106 NIH MEN1/ZES patients, the mean age of patients who died was 55.1 ± 2.8 years. This age is older than that reported in a number of series in the literature, with mean ages of death of 31.7 years,15 43.3,444 45.1,254 47,88 50.3,46,57 50.9,465 and 51 years.129 However, it is similar to the ages reported in other studies, which have reported mean ages of death of 53.2 years,54 55 years, males/47 years, females,129 60,448 and 55 years.88
Third, in terms of survival calculated using the Kaplan-Meier method, the 106 NIH MEN1/ZES patients had a much better overall survival at 5, 10, 20, and 30 years postdiagnosis than the 227 pooled MEN1/PET literature patients (at 5 yr, 97.3% vs 60%, respectively; at 10 yr, 89% vs 21%; at 20 yr, 67.5% vs 5%; at 30 yr, 55% vs 0; p < 0.01). Similarly the NIH MEN1/ZES patients’ survival was significantly better than the average of 22 series in the literature,54,57,78,94,106,153,166,181,217,233,276,289,303,311,367,424,425,440,481,482 which had mean 5- and 10-year survival rates of 89% ± 1.9% and 78% ± 3.6%, respectively, compared to 97% (95% CI, 92%–100%) and 89% (95% CI, 81%–94%) (p < 0.05), respectively, in the NIH MEN1/ZES patients. If a similar comparison is made for just the MEN1/ZES patients, the survival of the NIH MEN1/ZES patients was also significantly better (p < 0.05) that that of 10 series of MEN1/ZES patients in the literature,54,106,166,181,217,276,303,311,367,424,440,481,482 which reported mean 5- and 10-year overall survival rates of 88% ± 2.9% and 80% ± 4.2%, respectively, compared to 97% (95% CI, 92%–100%) and 89% (95% CI, 81%–94%), respectively, for the NIH MEN1/ZES patients.
MEN1-Related Survival
During the follow-up period (mean, 15.5 yr from MEN1 diagnosis, 24.5 yr from MEN1 onset), 24 of the 106 (23%) NIH MEN1/ZES patients died; 14 of the 106 patients (13% of the total patients; 58% of deaths) died from an MEN1-related cause. This is similar to the results for the 227 MEN1/PET patients from the pooled literature series, in which 66% of the deaths were due to an MEN1-related cause. In contrast, in the various larger series of MEN1 patients in the literature (see Table 12), the percentage of deaths due to an MEN1-related cause varied considerably, although the mean of 68 ± 6 for 14 series reviewed was similar to our results. In 5 of the large MEN1 series in the literature the percentage of MEN1-related deaths was less than in our NIH patients and the 227 pooled literature series (28%–47%).54,78,88,378,379,448,465 In 3 of the large series it was similar to our results (67%),129,150,371 and in 8 of the large series it was a higher percentage (75%–100%) than in our series.15,57,217,224,226,251,254,289,367,444 Our results are consistent with the results of 5 large series of MEN1 patients published in the last 10 years, which reported that 60% ± 9% (range, 28%–81%) died from an MEN1-related cause, consistent with the conclusion that at present approximately two-thirds of MEN1 patients die from an MEN1-related cause. These results are lower than a mean MEN1 mortality rate of 88% ± 5% reported in 5 large early MEN1 series from the years 1960–1980,15,224,226,254,444,474 with the difference primarily due to the occurrence of acid-related deaths in the earlier series. These data demonstrate that at present, approximately two-thirds of MEN1 patients will have an MEN1-related death.
While there have been a number of studies reporting overall survival in MEN1 patients, as discussed in the previous paragraph, to our knowledge there have been only retrospective studies88,217 assessing disease-related survival in MEN1 patients. One study assessed disease-related survival in MEN1 patients as a function of the patient’s age,88 and the other as a function of follow-up time.217 The former study found that MEN1 patients who had an MEN1-related death had a shortened survival, with a mean age at death of 47 years compared to MEN1 patients dying from non-MEN1-related causes (age 60 yr; p < 0.02) or non-MEN1 carriers (age 55 yr; p < 0.05). However, there was no significant difference between the overall survival and the MEN1-disease related survival (mean age, 47 yr vs 50 yr). In the second study,217 the 10-year median MEN1 disease-related survival was 73% (95% CI, 58%–95%), which was not significantly different from the overall survival from diagnosis at 10 years of 73% (95% CI, 58%–89%), with a median overall survival of 19.5 months. Our disease-specific survival rates for 106 NIH MEN1/ZES patients as well as the 227-pooled MEN1/PET literature patients, have similarities with and differences from the rates of the latter study.217 Our results are similar, in that there was no significant difference between the overall survival rate and the MEN1-disease specific survival rates, either for time from diagnosis or time from onset of MEN1 (see Figure 2, Table 11). Our results with both patient groups (NIH and pooled literature groups) differ in that our MEN1 disease-related survival for the NIH group was much better than that reported in the above study,217 with a 10-year survival rate from diagnosis of 93% (95% CI, 85%–97%) and a 30-year survival rate of 75%, whereas our 10-year and 40-year disease-specific survival rate from onset of MEN1 was 99% and 72%. In contrast, the disease-specific survival rate of the MEN1/PET patients from the pooled literature was much worse that that of the NIH MEN1/ZES patients or of those reported in the above study,217 with 10-year survival rates from diagnosis of 31% (95% CI, 27%–35%) compared to 93% in the NIH patients and 75% in the patients in the above study.217 Many factors could have contributed to these markedly different MEN1-disease survival rates in these different groups of MEN1 patients, including the differences in study design (retrospective vs prospective); differences in the features of MEN1 patient populations studied; differences in definitions of important variables such as time of diagnosis; and differences in definitions of causes of death. The NIH population has the advantage of being studied prospectively, under a fixed protocol with preset definitions allowing standardization of the results, and thus could be used as a template for further comparative studies.
Causes of MEN1-Related Death
In both our 106 NIH MEN1/ZES patients and the 227 MEN1/PET patients from the pooled literature, all of the MEN1-related deaths were due in some way to a NET, either because of its malignancy, complication of its treatment (postoperative death, etc) or due to the hormone excess state associated with it (for example, PET hormone secretion, HPT) (see Table 2). Of the MEN1-related deaths, 79% and 83% in the 2 groups of patients were due to the malignant nature of the NET, 14%–17% due to a NET hormone excess state, and 4%–7% due to a NET-related problem not due to progressive metastatic disease or the hormone excess state. The malignant NET deaths (79%–83% of MEN1 deaths) were primarily due to deaths from malignant PETs (57%–58% total MEN1 deaths) or to deaths from thymic carcinoid tumors (19%–21% of MEN1 deaths).
To compare our data to MEN1 series in the literature, all causes of death were expressed as a percentage of the total deaths, as was done in most of these series (see Table 12). When expressed in this form, our data demonstrated the main single cause of death was due to PETs accounting for 38% (NIH) and 44% (pooled literature series) of the total deaths, followed by death from thymic carcinoid tumors (12%–13%). For 15 large series of MEN1 patients in the literature, the average percentage of death due to a PET-related illness was 53.1 ± 7% of all deaths; however, this percentage, as well as the exact causes of the PET-related death, varied widely in the individual series, with the total percentage varying from 19% of all deaths78,251 to 91% of all deaths.254 In the NIH and pooled literature series, the major cause of a PET-related death was the malignant nature of the PET, responsible for 36% of the total 44% PET-related deaths in the pooled literature series and for all 38% of the PET-related deaths in the NIH patients. In 14 of 15 of the large MEN1 literature series (see Table 12), PET-related illnesses were also the major cause of death (mean, 56% ± 7%); however, in 1 series251 the main cause of death was related to malignant thymic carcinoid tumors (24% of all deaths). Similar to our 2 groups of MEN1 patients (the NIH and pooled literature series), in 8 of the 14 literature MEN1 series where PET-related illnesses were the leading cause of death,57,78,88,129,150,217,378,379,448,465 the major cause of the PET-related death was the malignant nature of the PET, averaging 39% ± 9% of all deaths (range, 14%–83% of all deaths).
In our 2 series (the NIH and pooled literature series), death due to a malignant PET was most frequently due to a malignant gastrinoma (60% and 100% of cases). This result is similar to that reported in 6 series in the literature54,78,224,226,251,289,367,444 where the percentage of malignant gastrinomas responsible for the PET-related malignant deaths could be assessed; however, it differs from results in 4 series129,150,378,379,448,465 wherein malignant gastrinomas were responsible for only an average of 16% (range, 0–38%) of the malignant PET deaths. It is unclear from the data available in these latter reports whether this low percentage of malignant gastrinomas contributing to the overall number of malignant PETs is clearly reflective of the actual findings in these patients, because in most of these series the specific nature of the malignant PET is poorly described. Therefore, while our data and most recent literature series clearly establish that the malignant nature of the PET is now the leading cause of death in MEN1 patients, it is not clearly established what type of PET is responsible for this, particularly whether the majority of these malignant PETs are nonfunctional PETs or gastrinomas.
In 6 of the 14 literature series where a PET-related illness was the leading cause of death15,54,224,226,254,289,367,444 (see Table 12), the hormone excess state was the leading cause of death, and in each case it was primarily due to uncontrolled gastric acid hypersecretion in patients with ZES. These series generally included patients prior to the widespread availability of effective medical management for the gastric acid hypersecretory state of patients with ZES (in the 1980s). Even though a number of studies have reported that the gastric acid hypersecretion in patients with MEN1/ZES, especially those with uncontrolled HPT, may be difficult to control, compared to patients with sporadic ZES,140,189,273,281,317 the data from our NIH patients and from a number of the recent MEN1 literature studies reviewed in Table 12 support the conclusion that current medical gastric antisecretory treatment in these patients is very effective. Especially compared to earlier series prior to the effective medical treatment of the gastric acid in MEN1/ZES patients, there was a low rate of deaths due to gastric acid hypersecretion in 10 of the MEN1 series since 1990 (3.7 ± 1.3).54,57,150,217,251,286,378,379,448,465 This is similar to our results in the 106 NIH MEN1/ZES patients, where 0 patients died due to gastric acid hypersecretion.
Even though gastric acid hypersecretion is now being controlled in almost every MEN1/ZES patient, in contrast to some older studies,15 other hormone excess states per se are an uncommon cause of death in the current series and in recent series. Specifically, in the NIH patients, only 1/106 (0.9%) patients died from another hormone excess state (insulinoma), and in the 227 MEN1/PET patients from the pooled literature, 2.2% (5/227) died from another non-gastrinoma hormone excess state (8-insulinomas, 1-VIPoma). Even this may be an overestimation because 3 of the 8 insulinoma patients from the pooled literature had malignant insulinomas, and it is unclear whether they died of progression of the malignant disease or of refractory hypoglycemia. Including the 5 patients from the pooled literature series with glucagonomas who died from an MEN1-related cause, all died from progressive metastatic disease. These data support the conclusion that death from the hypersecretion of a PET other than gastrinoma is an uncommon cause of death in MEN1 patients at present. These conclusions are supported by the data from 11 various large literature MEN1 series, where in 8 series, reporting 257 deaths of MEN1 patients,57,129,251,254,277,299,371,444 no patients died from insulinoma, and in 3 other series54,78,448 comprising 161 deaths of MEN1 patients, only 2 deaths (1.2%) were due to an insulinoma. Furthermore in the Groupe d’etude des Tumeurs Endocrines (GTE) MEN1 series comprising 758 patients, the presence of an insulinoma was not associated with increased mortality, in contrast to the presence of other PETs in MEN1 patients.71,150 These data are at some variance with some older studies. Ballard et al,15 in their sentinel 1964 study of MEN1 where they reviewed findings in an extensive MEN1 kindred as well as 74 additional cases previously reported in the literature, concluded that hypoglycemia suggesting a possible insulinoma was frequent in MEN1 patients, occurring in 36% of cases, and that 5 patients (6%) died of insulinomas, suggesting that it was not an infrequent cause of death. Subsequently most studies show that insulinomas occur less frequently than this in MEN1 patients, occurring in 11.8% of 758 MEN1 patients in the GTE study148,150 and in 18% in a recent review of MEN1 cases in a number of series.102,174,189,195,212,261,348,418,436 Both the surgical curability and more effective medical control of the rare MEN1 patient with an insulinoma are contributing to the current low rate of insulinoma as a cause of death in recent MEN1. In recent large series only a small percentage (0–15%) of insulinomas in MEN1 patients are reported to be malignant,22,71,82,153,195,205,247,279,330 and the remaining 80%–100% of the MEN1 patients with insulinomas are cured postresection.21,22,71,75,82,153,195,247,319,330,425 Short-term medical control with diazoxide, diet, or somatostatin analogues prior to surgery is effective in controlling hypoglycemia in most patients,76,81,82,144,196 and therefore uncontrolled hypoglycemia resulting in death is primarily restricted at present to the small percentage with a malignant insulinoma (<1% of all patients) and to an even smaller group comprised of the few patients with malignant insulinomas not controlled by medical therapies (diazoxide, somatostatin analogue, mTOR inhibitors [everolimus, rapamycin])76,144,196,221 or more recently by peptide radio-receptor therapy using radiolabeled somatostatin analogues.76,144,441
Other functional PET syndromes (not including insulinomas or gastrinomas) were a rare cause of death in our 2 study groups (the NIH group and the patients from the pooled literature series), causing no deaths in the 106 NIH MEN1/ZES patients and 1 death (0.4%) (a VIPoma) in the 227 MEN1/PET patients from the pooled literature. These data are in agreement with the results reported in 13 large literature series54,57,78,129,224,251,254,367,371,444,448,474 which contain data of 463 MEN1 patient deaths, where only 2 deaths (0.4%) were reported due to a glucagonoma and 1 death (0.2%) to a growth hormone-releasing factor-secreting tumor (GRFoma). These rare PETs are frequently malignant when present in MEN1 patients (33%7–50% of cases).51,125,195,233,334 In the large GTE series comprising 758 MEN1 patients150,233 in which glucagonomas/VIPomas/somatostinomas were present in 3.3% of all patients, their presence was associated with decreased overall survival (HR = 4.29; 95% CI, 1.54–11.9) and with a decreased 10-year survival (54%) compared to patients with gastrinomas or insulinomas (82%–92%), and was similar to patients with only nonfunctional PETs (62%). While these latter data show that the presence of these rare PETs can affect survival in MEN1 patients, in the current series as in most of the recent literature series reviewed above, the low frequency of deaths caused by these rare PETs in the MEN1 patients is likely due to their low rate of occurrence in MEN1, reported as 1.6%–3% for glucagonomas, 1%–3% for VIPomas, and 0.65% to <1% for GRFomas or somatostatinomas.102,152,174,189,195,212,233,261,308,348,418,436
The second largest single cause of MEN1 death in our 2 groups of patients was thymic carcinoid tumors (12% of the NIH MEN1/ZES patients and 12.5% of the pooled literature series). This finding has both similarities and marked differences from the findings in the 15 large MEN1 literature series reviewed in Table 12 and other recent literature series111,150,371,373 reporting assessment of thymic carcinoids in MEN1 patients. Our results are similar to 2 series129,217 that report thymic carcinoids as the second leading cause of MEN1 death (6%–13% of all deaths) behind PET-related deaths. However, they differ from 1 study reporting thymic carcinoids as the most frequent cause of MEN1-related deaths (24% compared to 10% for malignant PETs), and from 12 series in which thymic carcinoids either caused no deaths15,54,57,78,88,226,254,289,367,394,463 or caused only a small percentage of MEN1-related deaths (5%–6%),150,378,379,465 which was much less than seen with malignant PETs. Almost all of these latter series not reporting thymic carcinoids in MEN1 patients were older series, specifically, they include patients followed before 2000. The likely reason that thymic carcinoids were not reported is because thymic carcinoids were not recognized as part of MEN1 until 1972,363 and were not recognized as a major cause of death until the 1990s;131,378,465 thus they were not specifically sought for or considered as a cause of death in many of these older series. Since the 1990s a number of studies have called attention to the increasing importance of thymic carcinoids as a cause of death in MEN1, particularly in men, because >90% occur in males.45,111,131,151,414,465,477,479 These tumors are particularly aggressive, and are associated with a poor prognosis, with more than one-half of patients in some series having metastases at diagnosis, and even more developing them during follow-up, particularly to the bone.45,111,131,151,363,414,477,479 The aggressive nature of these tumors is supported by the results of the large, retrospective GTE study composed of 758 MEN1 patients, in which the presence of thymic carcinoids was reported to be associated with a higher risk of death compared with unaffected patients (HR = 4.64; 95% CI, 1.7–12.4]. The malignant nature of the thymic carcinoid itself is responsible for almost all deaths in MEN1 patients with these tumors, because MEN1 patients with thymic carcinoids rarely develop a hormone excess state.111,130,131,151,414,470,479 In this sense thymic carcinoids in MEN1 patients differ from those occurring in patients without MEN1 (that is, sporadic thymic carcinoids), because a hormone excess state due to the thymic carcinoid is very infrequent (only 4 cases reported that we know of),111,130,408,470 and the hormone excess state was only Cushing syndrome when it occurred, whereas in patients with sporadic thymic carcinoids, a hormone excess state is more frequent (up to 40%) and more varied, with Cushing syndrome, carcinoid syndrome, and acromegaly being reported.38,111,131,185,342,392 Our results and those from a number of studies in the literature support the increasing importance of thymic carcinoids as a cause of death in MEN1 patients. In our series they occurred in 6% of all NIH patients, and in various retrospective studies they occurred in 2.6%,151 3%,45,57,151 4.2%,305 and 4.9%479 of all MEN1 patients; however, in our series they accounted for 12% (NIH) and 12.5% (pooled literature series), and in some recent series they account for up to 24%251 of all MEN1 deaths, demonstrating their increasingly important role as a cause of death in MEN1 patients.
In addition to PETs and thymic carcinoid tumors, other MEN1 features have been reported to be an important cause of MEN1-related death in a number of studies, particular some older series. Complications of uncontrolled HPT including renal failure and hypercalcemic crises are reported to contribute to MEN1-related deaths in 10%–12% of patients in 3 older series of MEN1 patients224,226,378,379,444,465 and in occasional patients in other reports.78,150 In more recent series,54,57,129,217,251,371,448,474 including all of the NIH patients in the current series, death from complications of uncontrolled HPT were not seen, because of the greater understanding of the hyperplastic nature of the parathyroid disease and the need for partial or total parathyroidectomy to control the HPT.42,104,149,168,211,328,330 Pituitary diseases (pituitary apoplexy, tumor invasion) are reported to either be a cause of or contribute to MEN1-related death in 3%–6.5% of patients in a few older series.49,129,150,222,378,379,465 Pituitary tumors in MEN1 patients are more aggressive, more frequently multiple and invasive than in patients with sporadic pituitary tumors.49,147,435,447 However, in the NIH prospective series as well as in most current series, although pituitary adenomas are frequently present (20%–65% of patients), they are recognized and adequately treated, so they rarely cause death.54,57,78,88,195,217,251,448 This latter conclusion is also supported from the findings of the GTE study involving 758 MEN1 patients, where the presence of pituitary disease was not associated with an increased risk of death in MEN1 patients (HR = 1.17; 95% CI, 0.72–1.90; p = 0.54).150
Adrenal disease is present in 10%–73% of MEN1 patients on imaging studies23,48,128,228,374,388,390,453 and is reported to cause MEN1-related deaths in occasional series (0.4%,150 4%465) and case reports.161,385 Adrenal tumors in MEN1 patients are reported to cause a number of functional hormone excess syndromes including Cushing syndrome, hyperaldosteronism, pheochromocytoma, androgen secretion, or feminization.8,27,48,57,128,157,228,261,276,385,388,390,436,453 Functional hormone excess states caused by the adrenal tumors are rarely a cause of MEN1-related death, because in most series >90% of the adrenal lesions are not associated with a functional syndrome (except 1 series228 where 38% with adrenal lesions had Cushing syndrome).48,388,390 In various series,23,48,128,140,157,374,385,390,453 0–6% of MEN1 patients develop adrenal cortical carcinomas, which can be aggressive, invasive, and associated with a functional syndrome such as Cushing syndrome, and which can contribute to or cause death in these patients. However, in both our series including the 106 NIH MEN1/ZES patients and the 227 MEN1/PET patients from the pooled literature, no patient died of adrenal disease, similar to what was reported in a number of recent large MEN1 series,23,78,129,157,217,448 supporting the conclusion that it is an uncommon cause of death at present in MEN1 patients. This conclusion is also supported by the results from the 758-patient GTE study of MEN1 patients. In that study, those with adrenal tumors had a trend toward an increased risk of death compared to unaffected patients, but it did not reach significance (p = 0.064) (HR = 1.72; 95% CI, 0.97–3.06).150
In addition to thymic carcinoid tumors, patients with MEN1 have an increased incidence of pulmonary [0–8%]47,140,190,195,261,368,378 and gastric carcinoid tumors [7%–35%],34,140,187,195,232,326,360 which are reported to be an MEN1-related cause of death in a few series in the literature and in some case reports.39,150,326,378,379,448,465 In the 106 NIH MEN1/ZES patients, neither gastric nor pulmonary carcinoid tumors caused any MEN1 deaths; however, in the 227 pooled literature series, 1 patient died from a gastric carcinoid (0.4% of all deaths) and 1 patient died from a pulmonary carcinoid (0.4% of all deaths). These data suggest that although these tumors can be malignant and also cause a hormone excess syndrome (carcinoid syndrome),40,94,98,190,360,437 they are an uncommon cause of MEN1-related death at present. This conclusion is supported by the results of 15 MEN1 series (see Table 12) and a detailed series on only pulmonary carcinoids in MEN1 patients368 in which pulmonary carcinoids were reported to be a cause of death in a mean of 0.5% ± 0.4% of total deaths (range, 0–5%) and gastric carcinoids in 1.2% ± 0.8% (range, 0–10%), with 11 series reporting no deaths from either gastric or pulmonary carcinoids. This conclusion for bronchial carcinoids was also supported by the GTE study on 758 MEN1 patients, in which the presence of a bronchial carcinoid did not increase the death rate compared to unaffected controls (HR = 1.55; 95% CI, 0.64–3.77; p = 0.332).150
Prognostic Factors for Survival
We attempted to identify prognostic factors for overall survival in the NIH patients, and for survival from an MEN1-related death in both groups of patients in our study (the NIH and the pooled literature groups). We analyzed overall survival in addition to MEN1 disease-related survival for a number of reasons. In the literature almost all studies on prognosis in MEN1 patients report overall survival, and therefore, to allow comparison we also included overall survival. Second, by including overall survival, MEN1’s effect on all disease processes leading to death can be reviewed. This is an important point because at present there is little information on what is now described as non-MEN1-related deaths and it is unknown whether MEN1 patients have increased occurrences of any of the diseases currently included in this category. Although the exact role of menin, the protein altered in patients with MEN1, in causing many of the abnormalities seen in MEN1 patients is not known, it is clear that it is involved in many important cellular processes such as cell cycle regulation, transcriptional control, cell division, and genomic stability, any of which if altered could lead to many different diseases, including various common neoplasms.16,50,195,419,469
For overall survival in the 106 NIH MEN1/ZES patients, none of 5 general disease features analyzed differed between surviving and deceased patients including sex; race; age at first NIH assessment or age at last follow-up; duration of MEN1 to death or last follow-up; or duration of follow-up at NIH. Similarly, for MEN1 disease-related survival for either the NIH patients or the 227 MEN1/PET patients from the pooled literature series, sex; age at diagnosis of MEN1 or onset of ZES; or time to death or last follow-up did not differ between patients with or without an MEN1-related death. However, the age at death was earlier for the pooled literature patients with an MEN1-related death compared to those with a non-MEN1-related death (51 vs 53 yr, p = 0.002). These results differ from a number of MEN1 series in the literature where decreased survival was associated with older age,46,54,152,217 and in 2 studies males had a decreased survival compared to females.54,150 These results also differ from a study54 that assessed the presence of liver metastases as a surrogate marker of survival in MEN1 patients, because their presence is a strong negative prognostic factor in MEN1 and in non-MEN1 patients with NETs or PETs,21,37,54,103,105,141,191,217,252,291,398,433,459,471,476,481 which reported liver metastases were more frequent in males with MEN1 than females. Our results are similar to those in various studies of MEN1 patients where survival was not affected by age,150,152,217 sex,152 and another study, which also found that MEN1-related deaths occur at an earlier age than deaths due to non-MEN1-related causes in MEN1 patients.87 Our results differ from those in some studies of patients with sporadic PETs or sporadic ZES in which a worse prognosis is associated with female sex and shorter disease histories to diagnosis.191,459,476 However, our results are similar to most studies of sporadic PETs, which show no effect of sex on survival.100,105,258,338,400,429,446,471 Nevertheless, our result showing a lack of sex effect on survival (total or MEN1-disease related) is somewhat surprising, because even though the most common cause of MEN1 death, PETs, occur approximately equally in males and females, the second most common cause of MEN1 death, thymic carcinoids, occur in >90% males, thus this would be expected to lead to a sex effect on survival.111,131,148,151,414,465,477,479 A likely factor contributing to our failure to see the sex effect of thymic carcinoids reflected in our survival results is the fact that thymic carcinoids are diagnosed relatively later in the course of MEN1 (mean age, 42–50 yr)131,151,204,362,414,479 and these patients may have a prolonged survival, therefore the full effect on mortality may require even longer follow-up than in the current study.
Previous studies have suggested that a number of clinical and laboratory MEN1-related features can be predictive of survival46,141,150,152,367,465 (see Tables 4, 5, 7, 9, 10). For the 106 NIH MEN1/ZES patients most non-PET-related features of MEN1 (HPT, pituitary, adrenal, thyroid, carcinoid) were not significantly associated with decreased overall survival, except for the occurrence of functional syndromes other than ZES (either PET-related [p = 0.031] or non-PET-related [p = 0.0033]), the requirement for a high number of parathyroidectomies (>3) (p= 0.008), a higher fasting serum gastrin level (>20-fold increase)(p = 0.022), or the need for previous gastric acid reducing surgery (p = 0.0261). Almost reaching significance for overall survival was the presence of a higher percentage of patients with family history of MEN1 among patients who died of any cause (p = 0.052) and the presence of thymic carcinoids (p = 0.098). In contrast, the presence or absence of none of these variables correlated with the presence of disease-related survival in the NIH patients. However, in the 227 MEN1/PET patients from the pooled literature, an MEN1 disease-related death was highly correlated with the presence of thymic carcinoid tumor (p = 0.0006) and the lack of a family history of MEN1 (p = 0.019), and was borderline correlated with the presence of thyroid disease (p = 0.050) or PETs other than ZES (p = 0.058). These results are consistent with the conclusion that a worse survival prognosis occurs when an MEN1 patient has severe HPT requiring more parathyroidectomies; higher functional expression of gastrinomas resulting in higher gastrin levels, with more severe gastric acid hypersecretion requiring more frequent need for gastric acid reducing surgery prior to the availability of proton pump inhibitors; the presence of additional functional hormone excess states other than ZES, and the presence of a thymic carcinoid tumor. These conclusions are consistent with a number of previous findings in various studies on MEN1 patients and sporadic PET patients. They are consistent with studies that have shown the development of liver metastases, which are associated with decreased survival in patients with PETS such as gastrinomas,37,54,103,105,252,291,398,405,459,471,476 more frequently occur in gastrinoma patients with higher gastrin levels,19,33,36,46,96,184,191,241,405,459,476 and in some studies with higher BAOs.476 Our findings that more resistant HPT is associated with a poorer survival prognosis is consistent with studies that propose that the presence of uncontrolled HPT in these patients increases the risk of developing PETs,47 that it may act as a prerequisite for the development of other neoplasms in MEN1,29 and that it may be an important factor in the release of mitogenic factors that are found in the serum of MEN1 patients, including a basic fibroblast growth factor-like substance.263,480
Our results for the prognostic value of various MEN1 clinical and laboratory features show a number of similarities and differences from other series of MEN1 patients. The are similar to almost all other studies in demonstrating that the frequency of occurrence of many of the features of the MEN1 syndrome including HPT; adrenal or pituitary disease; smooth muscle or CNS tumors; bronchial/gastric carcinoids; or dermatologic lesions does not correlate with survival, and thus these are not prognostic factors for survival.78,129,150,152,217,251,289,433,444 In contrast, almost all studies, similar to our MEN1/PET pooled literature series, report that the presence of thymic carcinoids carries a worse prognosis, due to the aggressive nature of these tumors.111,131,150,151,331,413,414,465 While our NIH MEN1/ZES series showed a trend toward significance for thymic carcinoid patients having a worse prognosis (p = 0.098), a number of factors likely contributed to it not reaching full significance as a prognostic factor. These include that we made an early diagnosis of thymic carcinoid because all patients were prospectively followed with regular imaging131 and their treatment was aggressive, because of the known progressive nature131 of these tumors, resulting in prolonged survivals. A number of large studies of MEN1 patients report that the presence of any PET (except insulinomas), is associated with decreased survival.150,331,389,465 In our study this could not be evaluated because both groups of MEN1 patients (the 106 NIH patients and the 227 patients from the pooled literature series) all had PETs. The characteristics of the PETs as prognostic factors could be studied and are dealt with in the next section. Our finding in the MEN1/PET patient pooled literature series that a family history of MEN1 carried a better prognosis agreed with the large French GTE study, which reported similar findings.150 These findings are at odds with the results of a study46 that reported that the presence of a first-degree relative with MEN1 was associated with an increased risk of developing a PET,46 which was associated with a worse prognosis.
A number of studies of MEN1 patients report that various tumoral aspects, primarily associated with PETs, have prominent prognostic significance. These include the primary PET size54,141,217,234,247,315,324,433,434 whether the PET is functional or nonfunctional;150,217 the functional type of PET;46,150 whether liver metastases are present or not,54,141,152,217,276 and the effect of various treatments, particularly whether the patient underwent surgical resection of the PET or not.152,217,433 In the 106 NIH MEN1/ZES patients, each of these variables could be analyzed and assessed for their effect on both overall survival and MEN1-specific survival. In contrast, because of incomplete data, only a few of these variables could be assessed in the 227 MEN1/PET pooled literature patient series. In the NIH series of MEN1/ZES patients, decreased overall survival (OS) (p = 0.0203) and disease-related survival (DRS) (p = 0.022) occurred in patients with increasing primary PET tumor size; in patients with liver metastases initially (OS, p = 0.011; DRS, p = 0.0180); bone metastases (OS, p = 0.0002; DRS, p = 0.0099), but not lymph node metastases (OS, p = 0.057; DRS, p = 0.56); for patients who develop liver metastases (OS, p = 0.001; DRS, p = 0.0180) and for patients whose PETs show aggressive growth (OS, p < 0.00001; DRS, p = 0.0001). Decreased overall survival also was associated with increasing number of PETs (p = 0.032); however, for MEN1 disease-related survival this did not reach significance (p = 0.097). Conversely, the development of any new lesion was associated with decreased MEN1 disease-related survival (p = 0.0180), but its effects on overall survival did not reach significance (p = 0.124). A number of these results are consistent with findings reported in other studies of MEN1 patients or patients with sporadic PETs. The presence of liver metastases initially or their development with time was associated with decreased survival in a number of studies of MEN1 patients,54,141,217,276 but not in others.152 These results are also consistent with most studies of patients with sporadic PETs, which report liver metastases are associated with a poor prognosis,37,103,105,159,200,252,255,291,338,398,429,459,471,476,481 but some studies report also their development during follow-up and the extent of the liver metastases correlate with decreasing survival.191,459,476 The exact primary source of the liver metastases in almost every study of MEN1 patients is not well defined, and it is often unclear whether it is from a PET, thymic carcinoid, or another carcinoid tumor (gastric, pulmonary). The liver metastases in MEN1 patients with a PET, without a thymic carcinoid, are almost always attributed to the PET, although this remains unproven. Furthermore, the exact source of the liver metastases becomes even more of an issue in patients with MEN1 with gastrinomas, because many of these patients also have nonfunctioning PETs in the pancreas on imaging studies, and in most cases it is unclear which PET metastasized. Lastly, the majority of patients with MEN1 that have thymic carcinoids also have PETs (57%–100%),111,131,151,414 and which of these is responsible for the liver metastases is usually not resolved. This ambiguity has occurred because until recent many of these different NETs could not be distinguished histologically or immunohistologically and even in more recent studies where numerous methods to distinguish these NETs have been reported,177,237,243,395 detailed histologic/immunohistochemical studies were not performed to resolve the primary site that metastasized. Because of this, the true metastatic rate of many of the MEN1 NETs to the liver remains unclear.
The prognostic significance of distant metastases (beyond liver) to bone, etc, has not been specifically studied in MEN1 patients. Similarly, the presence of local metastases to adjacent lymph nodes on survival in MEN1 patients has not been specifically studied. However, the prognostic effect of each of these metastatic sites has been studied in detail in patients with various sporadic PETs. In the case of local metastases to lymph nodes, studies have reported contradictory results, with most reporting no prognostic effect,54,114,145,191,201,252,279,338,377,459 whereas a few other studies have reported a negative effect on survival;37,67,219,429,476 however, the impact is much less than seen with the presence of liver metastases. A number of studies report that the presence of distant metastases, especially to bone, is a predictor of decreased survival.20,133,191,231,338,476 In 1 study of patients with advanced gastrinomas (sporadic) the presence of bone metastases was associated with a mean survival of only 1.9 years after their detection.476 Therefore, our results with MEN1 patients are similar to most studies with sporadic PETs, which report no effect of lymph node metastases on survival, and other studies, which report decreased survival in patients with sporadic PETs who develop distant metastases to bone.
Our finding that aggressive tumoral growth or the development of new lesions during the follow-up is associated with decreased survival is consistent with results of a few studies on MEN1 patients and a number of studies in patients with sporadic PETs. One prospective study of MEN1 patients with gastrinomas141 reported that 15% of patients demonstrated aggressive growth of their PETs and that it was associated with decreased survival. This is a lower percentage than the 25% of patients with sporadic ZES459,476 who are reported to develop aggressive tumor growth over time, but nevertheless, it had similar effect on decreasing survival in both groups of patients. Similarly, a number of single cases reports or small series have reported patients with MEN1 whose tumors demonstrate rapid growth51,94,160,183,333,354,454 which in most cases leads to decreased survival. Other studies with various sporadic PETs demonstrate that a subset is associated with rapid growth and the development of new lesions, which is associated with a decreased survival.100,337,382,405
In our 227 MEN1/PET pooled literature patients we did not find a difference in survival between patients with or without a gastrinoma, with or without a nonfunctional PET, or with or without another functioning PET. Our results are similar to those in 1 study of MEN1 patients150 comparing these different PETs wherein MEN1 patients with various PETs (except insulinomas) all had decreased survival rates (hazard ratios, 1.9–4.3). In contrast, our results differ from a number of other previous studies in MEN1 patients, which have reported that different PETs have different effects on survival rate.46,195,217 Insulinomas in MEN1 patients are an uncommon cause of death, especially in more recent series, with 20-year survival >90%, in contrast to gastrinomas, nonfunctional PETs, glucagonomas, and other rarer functional PETs with 20-year survivals of 52%–67%.21,57,71,78,166,195,217,233,330,345,433 In MEN1 patients insulinomas are rarely malignant (0–15%) and in most series 80%–100% of the MEN1 patients with insulinomas are cured postresection.21,22,71,75,82,153,195,247,319,330,425 In contrast >50% of gastrinomas and 20%–50% of nonfunctional PETs and other rarer functional PETs are malignant.155,195,217,233,247,250 These results differ from findings in a large Tasmanian MEN1 family46 in which it was reported that the presence of hypergastrinemia was associated with a significant increase of enteropancreatic malignancy and decreased survival. At present it is unclear what the basis is for the difference in our data from the finding in this large kindred and whether it could be due to different PET behaviors in different MEN1 kindreds.
Our prospective study of the 106 NIH MEN1/ZES patients demonstrated that patients with large PETs had decreased total survival and MEN1-DRS. There were not sufficient data on the 227 MEN1/PET patients from the pooled literature to perform a similar analysis. Our results agree with a number of studies,54,141,217,234,315,322,324,433,434 but not all217,247 studies in the literature on MEN1 patients that have examined this correlation. Most of these studies reported that in MEN1, primary PETs >2–3 cm in diameter are associated with increased development of liver metastases,141,217,234,433,434 which in many reports is also shown to be associated with decreased survival. These results in MEN1 patients are in agreement with a number of studies on sporadic PETs which also show a correlation between primary pancreatic tumor size and the development of liver metastases and in some cases an association with decreased survival is shown;37,52,103,159,173,252,339,476 however, other studies do not report this association.338,429 Our data on the NIH MEN1/ZES patients did not show an association with the presence of a pancreatic PET or the presence of a duodenal gastrinoma with survival. The situation in patients with MEN1 who develop gastrinomas/ZES is confused by the fact that most of the gastrinomas (80%–100%) occur in the duodenum;90,154,250,315,348 however, these patients also frequently develop pancreatic PETs, which are nonfunctional in most cases (80%–100%).9,90,315,348 The duodenal gastrinomas in the MEN1 patients are characteristically small, and in contrast to the sporadic cases, are invariably multiple.9,90,250,348 Similar to those in sporadic ZES, 60%–75% of the gastrinomas in MEN1 patients are now found in the duodenum, with 20%–30% in the pancreas.316,321,323,324 Studies on sporadic gastrinomas demonstrate that the duodenal and pancreatic gastrinomas behave differently in that although they are equally malignant with 40%–70% of patients having metastases in adjacent lymph nodes21,22,250,315,459 which have not been shown to affect survival,459 metastases to the liver are uncommon with the sporadic duodenal gastrinomas, whereas the sporadic pancreatic gastrinomas are aggressive and are associated with a worse prognosis.324,459,476 Fewer data are available in MEN1, but a number of studies show that these patients also frequently (30%–70% of cases) have lymph metastases associated with the duodenal gastrinomas; however, they are uncommonly associated with liver metastases and are not associated with decreased survival in MEN1 patients,54,247,250,315,321,389 similar to the results in the current study.
Causes of Non-MEN1-Related Death
While a number of studies report the frequency of all deaths that were due to non-MEN1-related deaths, there are relatively few data on the exact non-MEN1-related causes of death, and it has in general not been systematically studied. In most studies the exact causes of the non-MEN1-related deaths are not specifically stated, so it is in general more difficult to compare our data to that in the literature. In our 106 NIH MEN1/ZES patients the cause of death was determined in all cases, with 42% of the 24 deaths due to a non-MEN1-related death, and in the 227 MEN1/PET patients from the pooled literature, 34% of all the deaths (73/227 patients) were due to a non-MEN1-related cause of death. Whereas the mean overall percentage of deaths due to non-MEN1-related causes in the literature from 13 series54,57,78,88,129,150,217,251,254,289,378,379,444,448,465 was similar to the data in our 2 series (mean, 33% ± 7%), the percentage of all deaths due to a non-MEN1-related death varied widely in the different series from 0 to 72% of all the deaths reported (Table 13). In 4 series the percentage of all deaths due to non-MEN1-related deaths was <20%,57,217,254,289,367 and in 5 series >50%.54,78,88,378,379,448,465 This marked difference is not due to the time of reporting of the series, because the mean percentage of patient deaths reported due to a non-MEN1-related cause for the 4 series reported before the widespread use of proton pump inhibitors (prior to 1995),254,289,367,378,379,444,465 and the 9 series reported after their widespread use (after 1995) are similar54,57,78,88,129,150,217,251,448 (25 ± 10% vs 36 ± 9% all deaths due to non-MEN1-related death). These data demonstrate that approximately one-third of all deaths in MEN1 patients are due to a non-MEN1-related cause.
In the 106 NIH prospectively followed MEN1 patients the most frequent non-MEN1-related cause of death was heart disease (myocardial infarction, arrhythmia, or cardiac arrest), followed by death due to non-MEN1-related cancers, cerebrovascular disease, and 1 death due to a cocaine overdose (4% of deaths). The order of the main causes of non-MEN1-related deaths in the 227 MEN1/PET patients from the pooled literature was different, with the most common cause being death from other non-MEN1-related cancers. This was followed in descending frequency by death due to a non-MEN1 cause which was not specified in the report, then by heart disease, lung disease (noncarcinoid), cerebrovascular disorders, accidents, other gastrointestinal disorders (non-cancer or MEN1 related), diabetes, neurologic diseases, and suicide. These results have both similarities to and differences from previous reports of the causes of non-MEN1-related death in various large series of MEN1 patients (see Table 13). They are similar in that for the 12 series of MEN1 patients where data on the cause of non-MEN1-related deaths were reported, in 4 series heart disease either was the most frequent or the second most frequent cause of a non-MEN1-related death.78,88,129,378,379,465 Similarly, in 8 series the occurrence of non-MEN1-related cancers was either the most frequent or second most frequent cause of death.54,88,129,150,217,289,367,444,448 In contrast to these results, 8 studies do not report heart disease54,57,150,217,254,289,367,444,448 and 2 studies a non-MEN1-related neoplasm57,254 as one of the most frequently seen causes of a non-MEN1-related-death. Two studies of MEN1 patients289,367,448 report suicide as a frequent cause of death in their patients. However, it was not a cause of death in any of the 106 NIH MEN1/ZES patients, and it was the cause of only 1 death in the 227 MEN1/PET patients from the pooled literature. Cerebrovascular disease was a non-MEN1 cause of death in 4% of the 106 NIH MEN1/ZES patients (10% total non-MEN1 deaths) and 3.5% of the 227 MEN1/PET patients from the pooled literature (11% of the total non-MEN1 deaths); however, it is not reported as a cause of death in 12 large series of MEN1 patients (see Table 13).54,57,78,88,129,150,217,254,289,378,379,444,448,465
The finding that heart disease was one of the most frequent non-MEN1 causes of death in the MEN1 patients in the 106 NIH MEN1/ZES patients (20% of all non-MEN1 deaths), the 227 MEN1/PET patients from the pooled literature (40% of all non-MEN1 deaths), and in some of the other large series of MEN1 patients (24%–48% of all non-MEN1 deaths)78,88,378,379,465 raises the question of whether it is more common in MEN1 patients. Heart disease is a frequent cause of death in non-MEN1 patients, and at present, without matched controls and more MEN1 deaths, it is unclear whether cardiovascular death is more frequent in MEN1 patients with or without PETs. It has been proposed that MEN1 patients may have an increased risk of cardiovascular disease.442 Furthermore, MEN1 patients frequently develop a number of diseases, which are associated with an increased risk of cardiovascular disease. These include insulin resistance and impaired glucose metabolism which are known to be important risk factors for cardiovascular diseases,116,163,442 as well as for the development of chronic HPT, which is associated with an increased mortality, mainly due to an overrepresentation of cardiovascular death.116,210,259,455 In 3 studies of MEN1 patients271,442,452 evidence is provided to support the conclusion that these patients are more frequently insulin resistant compared to their unaffected relatives, that both increased fasting blood glucose levels and diabetes mellitus were more prevalent in MEN1 patients than unaffected family members, that the impaired glucose metabolism was associated with HPT and hypergastrinemia, and that MEN1 patients had decreased insulin sensitivity. Studies in patients with primary HPT report that it can be associated with an increased cardiovascular morbidity and mortality.116,210,259,455 Primary HPT is reported to be associated with hypertension, disturbances in the rein-angiotensin-aldosterone system, reduced coronary flow reserve resulting in dysfunction of the coronary micro-circulation, cardiac arrhythmias, as well as changes both functionally and structurally in walls of blood vessels.116,210,259,455 Furthermore, HPT has been related to the development of insulin resistance,271 and after successful parathyroidectomy, insulin sensitivity has been reported to improve.65,126 Therefore, by influencing glucose homeostasis through the development of insulin resistance, HPT could also affect cardiovascular function and play a role in the development of cardiovascular disease. While this is unproven in patients with MEN1, these patients almost invariably have HPT;102,140,189,280,418 it can be severe, especially in patients with MEN1 with gastrinomas;245,328 it is frequently long-lasting, being present before diagnosis and frequently recurring even if multigland parathyroidectomies are performed.11,44,93,104,149,169,179,211,218,257,328,330 These considerations suggest that in future studies of MEN1 patients, the occurrence and mortality of cardiovascular disease should be carefully assessed and compared to a control population to determine whether the presence of the MEN1 is having an effect, and if so, whether any of the above mechanisms seen in primary HPT are contributing.
Classically, MEN1 is associated with tumors and hyperplasia of the pituitary, parathyroid, duodenum and pancreas, thyroid or adrenal; however, over the last few years a wide spectrum of other tumors has been reported with increased frequency in MEN1.195,261,418 These include carcinoid tumors in a number of locations (thymic [0–8%], gastric [7%–35%], bronchial [0–8%], and rarely intestinal); dermatologic tumors (angiofibromas [88%], collagenomas [72%], lipomas [34%], melanomas); various tumors of the central and peripheral nervous systems (meningiomas, ependymomas, schwannomas [0–8%]); and smooth muscle tumors (leiomyomas, leiomyosarcomas [1%–7%]).6,13,14,34,46,48,49,56,66,74,111,131,151,176,195,209,228,261,274,368,371,388,390,393,413,428,465 These newer tumors show varying degrees of aggressiveness, with thymic carcinoids being highly aggressive, gastric and pulmonary carcinoids less commonly aggressive (metastasize <30% of cases), as are most smooth muscle or CNS tumors, which rarely metastasize, and the skin tumors, which all have a benign course, except for the occasional melanoma. Similar to the classical endocrine tumors in MEN1 patients,80,89,131,170,248,261,419,439 with most of the more recently described tumors associated with MEN1 (smooth muscle tumors including some leiomyomas, leiomyosarcomas, gastric carcinoids, pulmonary carcinoids),10,26,53,79,89,274,302,336,451 but not all cases (thymic, some angiofibromas, leiomyomas, and angiomyolipomas),89,131,156,170,414 molecular studies of the tumor provide evidence that these are intrinsic MEN1 tumors. Loss of heterozygosity of the MEN1 gene is found in the tumor, which is compatible with the proposal that the MEN1 gene functions as a tumor suppressor gene.195,419 These results of the increased development of various tumors in MEN1 patients is consistent with recent results exploring the cellular roles of menin, the protein altered in patients with MEN1. The exact cellular basis for the increased occurrence of these various endocrine and nonendocrine tumors in MEN1 patients remains unclear. The frequent occurrence of various nonendocrine neoplasms as a cause of death in our 106 NIH MEN1/ZES patients, the 227 MEN1/PET patients from the pooled literature, as well as in many of the large MEN1 series from the literature raises the possibly that some of these more common neoplasms could be more frequent in MEN1 patients. At present this remains unclear, and because of the small numbers of patients in most of the series, as well as the lack of systematic collection of the data in a prospective fashion in most studies, this question cannot be answered definitively by the data available at present.
In the 106 NIH MEN1/ZES patients there were 4 deaths due to 4 different non-MEN1 tumors (breast, renal, hematologic, oral cancers), which is close to the 3.2 ± 1.1 non-MEN1 tumor deaths per series found in 12 large literature series.54,57,78,88,129,150,217,254,289,378,379,379,444,448,465 In the 227 MEN1/PET patients from the pooled literature there were 18 non-MEN1 tumor related deaths in a frequency that reflected the common tumors in non-MEN1 patients with lung cancer>prostate, CNS tumors>colorectal cancer. From these limited data only a few trends can be pointed out on the frequency of the individual non-MEN1 tumoral causes of death in the MEN1 patients. For the 12 literature series54,57,78,88,129,150,217,254,289,378,379,444,448,465 and the 2 other series in the current study (that is, the 106 NIH MEN1/ZES and the 227 MEN1/PET patients from the pooled literature), the non-MEN1 tumor causing death that appeared in the most series was renal cancer and colorectal cancer (each in 6/14 series = 43%), followed by the common neoplasms causing death in non-MEN1 patients (lung cancer = 36%, 5/14 series; breast cancer = 29%, 4/14 series), followed in decreasing frequency by oral cancers (29%, 4/14 series) and then by hematologic, CNS tumors (14%, 2/14 series) followed by prostate/esophageal cancer in 7% of series (1/14 series). Renal neoplasms are reported in a number of MEN1 patients (renal cell cancer, oncocytoma, angiomyolipomas),53,84,88,89,99,176,186,217,256,289,448 and 2 reports84,186 proposed that renal tumors might be a new manifestation of MEN1. Even though renal neoplasms are reported as a cause of non-MEN1-related death equal in frequency to colorectal cancer, which occurs in >3-fold higher frequency than renal cancer in the general population (United States Cancer Statistics, Centers for Disease Control and Prevention), no definite conclusions can be drawn from the data reported above because of the low numbers of cases, lack of systematic reporting, and lack of careful epidemiologic comparison. In future studies it will be important to prospectively assess whether any of the non-MEN1 neoplasms are increased in MEN1 patients, with particular attention to renal and oral cavity neoplasms.
Authors of 1 study have proposed that suicide72 might be an important cause of death in MEN1 patients, and authors of another study proposed that cerebrovascular accidents due to MEN1-mediated related effects result in death.2 For the 12 literature series54,57,78,88,129,150,217,254,289,378,379,444,448,465 and the 2 other series in the current study (the 106 NIH MEN1/ZES patients and the 227 MEN1/PET patients from the pooled literature), suicide as a non-MEN1 cause of death was reported in 28% of the studies (that is, 4/14 studies).54,289,367,448 It was not a cause of MEN1 death in any of the 106 NIH MEN1/ZES patients prospectively studied, and it was a non-MEN1 cause of death in 1 of the 227 MEN1/PET patients from the pooled literature (0.44%). These latter data suggest that suicide is a relatively uncommon cause of death in these patients. Cerebrovascular disease as a cause of non-MEN1-related death was also uncommon. From the 12 literature series and the 2 other series in the current study, only 1 patient in any series died from a cerebrovascular accident.
Conclusions and Summary
From the current analysis of causes of death and identification of prognostic factors in 106 NIH MEN1/ZES patients prospectively studied compared to the results of pooled data from 227 MEN1/PET patients in case reports or small series and to data from large series of MEN1 patients,15,53,54,57,78,88,129,150,217,224,226,254,289,378,379,444,448,465 a number of conclusions can be drawn that will be important in the management of these patients; these are summarized in Table 14.
TABLE 14.
Summary and Conclusions
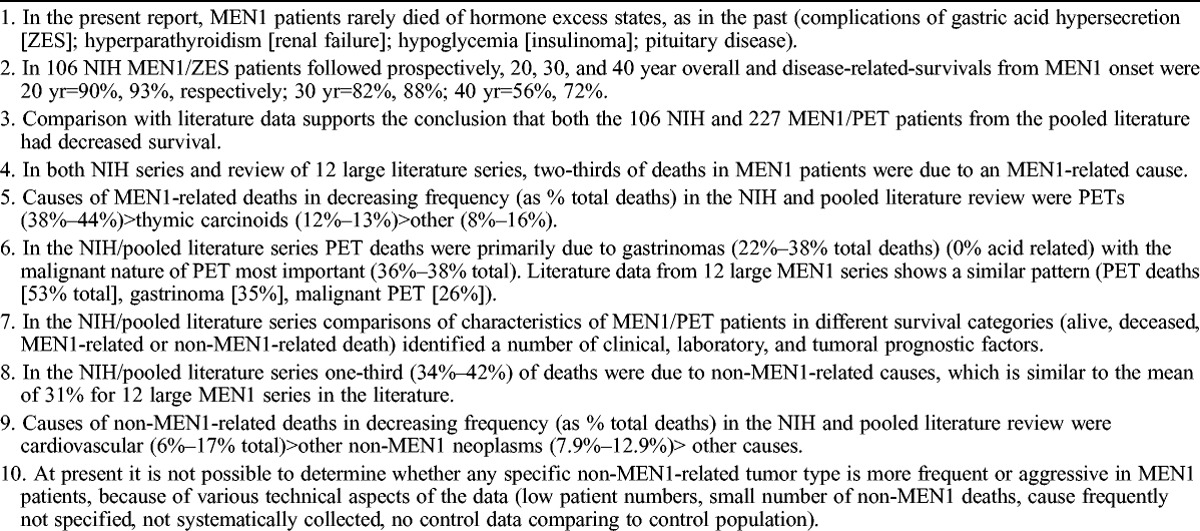
Our analyses demonstrate that in contrast to the past, in our 2 series and in recent large MEN1 literature series, MEN1 patients rarely die of causes related to the hormone excess state per se. Therefore, at present death is uncommonly due to complications of gastric acid hypersecretion, which was so frequent in the past,15,43,72,73,83,88,158,180,224,225,240,254,307,353,366,386,399,438,444,458,461,465,466 due to hormone hypersecretion by other PETs such as insulinomas;15,306,334,375,466 due to the complications of untreated HPT such as renal failure or hypercalcemic crises;15,32,68,88,129,224,359,427,438,440,444,461,465,466 due to untreated pituitary disease (apoplexy, hormone excess state, etc),222,447 or to other uncommon hormone excess states (ectopic Cushing from adrenal tumors, other functional PETs, etc).165,228,447,468,475
Analysis of the survival data of both the NIH and pooled literature series of MEN1/PET patients and comparison with the large MEN1 literature series data, supports the conclusion that MEN1 patients even today have a decreased survival compared to the healthy population, with a mean age of death of 55 years. In both the NIH and pooled literature series, two-thirds of all deaths are due to MEN1-related disease, which also agrees with the data from 12 large MEN1 series in the literature.15,53,54,57,78,88,129,150,217,224,226,254,289,378,379,444,448,465 The most frequent causes of MEN1-related deaths are from pancreatic endocrine tumors with the malignant behavior of the tumor being the major factor. Of the different PETs that MEN1 patients develop, gastrinomas account for more than one-half of the PET-related deaths (60%), and in none of the NIH/pooled literature series patients was death due to the complications of the gastric acid hypersecretion these patients develop, instead it was primarily due to the malignant behavior of the gastrinoma.199,200,290,364 The second most common cause of an MEN1-related death was thymic carcinoids, which accounted for almost 20% of the MEN1-related deaths in the NIH/pooled literature series, but only 5% of the 12 large MEN1 literature series. This marked difference can be largely attributed to the fact that thymic carcinoids have only been recognized as part of the MEN1 syndrome from the early 1980s, their aggressive nature was appreciated after this, and thus as a cause of death they were only systematically reported in more recent series.45,111,131,150,151,251,413,414,465
In both the NIH/pooled literature series as well as the average of 12 large literature series,15,53,54,57,78,88,129,150,217,224,226,254,289,378,379,444,448,465 one-third of the patients died due to non-MEN1-related causes. The most frequent causes of non-MEN1-related death in the NIH/pooled literature series were cardiovascular disease and death due to other non-MEN1 neoplasms, with numerous other causes such as cerebrovascular disease, lung disorders other than lung carcinoid tumors, and accidents making up the remainder. For the other non-MEN1 neoplasms, colorectal and renal cancers as a cause of death were reported in the most series, followed by lung cancer and breast and oral cancers. However, because of low patient numbers and other technical issues with data collection it can not be determined from the available data whether any of these non-MEN1 neoplasms are more frequently seen or have altered behavior in MEN1 patients.
In the NIH and pooled literature series, comparisons of MEN1/PET patients in different survival categories (alive, deceased, MEN1-related death, non-MEN1-related death) allowed us to identify a number of prognostic factors. These include various clinical features (disease duration, presence of non-ZES functional syndromes, parathyroidectomy number, presence of thymic carcinoid, presence of family history, in ZES previous acid reducing surgery); laboratory features (fasting gastrin levels) and various tumoral features (PET size, liver metastases, distant metastases, number lesions imaged, growth behavior of tumor).
The above results lead to a number of general conclusions related to the diagnosis and management of MEN1 patients. Even though survival of these patients has certainly improved from older studies, wherein the hormone excess states of various NETs frequently caused premature death,15,43,72,73,83,88,158,180,224,225,240,254,306,307,334,353,366,375,386,399,438,444,458,461,465,466 survival is still shortened compared to the general population and needs to be improved. This will primarily require more systematic and aggressive treatment of various MEN1 aspects, particularly treatment of PETs and carcinoid tumors, which are the principal causes of MEN1-related death. To accomplish this, earlier diagnosis of MEN1 is needed because the mean delay in diagnosis is 4–7 years from the onset of MEN1 (present study),55,140,207,357 and aggressive treatment of NETs is needed.
Because malignant PETs were the principal cause of MEN1-related deaths, particular attention should be paid to their early diagnosis and effective treatment. Particularly important are the diagnosis and treatment of gastrinomas, which were responsible for most (60%–65%) of the PET-related deaths. In almost 25% of the NIH patients liver metastases were already present at the time of MEN1 diagnosis and therefore earlier diagnosis is essential to prevent their development if possible. Also important is the effective treatment of both gastrinomas and other PETs. Their treatment remains controversial because studies show that patients with MEN1 with small nonfunctional PETs (<2 cm) have an excellent long-term prognosis, and in the GTE studies their survival did not differ from patients with MEN1 without a pancreatic PET.315,433,434 Patients with duodenal gastrinomas with tumors <2 cm also have an excellent long-term survival, with the survival being 100% of patients at 20 years.315 This has led to the recommendation that small PETs (<2 cm) in these patients can be followed without resection either by standard imaging studies or by serial endoscopic ultrasound studies.18,110,195,221,315,423,433,434 The present study as well as others in the literature in MEN1 and sporadic PETs shows that tumor size is an important prognostic factor for the development of liver metastases, that liver metastases (either their extent, rate of growth, or development), not lymph node metastases is a very important prognostic factor for long-term survival.191,315,405,459,476 One of the central problems that needs to be assessed is the actual source of the liver metastases that these patients develop. The metastases can either be from a gastrinoma if the patient has ZES; from a small occult thymic carcinoid; from a nonfunctional PET; or from a gastric carcinoid, all of which can be aggressive and malignant.111,131,151,195,326,368,413,414 There are few data on well-assessed biopsies from MEN1 patients who do develop liver metastases to allow an accurate assessment of the malignant nature of each of these NETs. At present new treatments for certain NETs (PETs especially) have been described such as with the mTOR inhibitor, everolimus;198,355,472,473 the tyrosine kinase inhibitor, sunitinib;198,356 various liver-directed therapies using embolization, chemoembolization or radiolabeled microspheres,61,127,164,343,401 and new chemotherapeutic regimes that are reported to have a high response rate (capecitabine and temozolomide).343,402 It will be important in the future that the source of the metastatic disease be established so that it can be treated appropriately and aggressively.
Thymic carcinoid tumors are generally a later feature of MEN1 and occur in most series in >90% in males, so that it is important that guidelines for screening/management for these aggressive tumors, that have been proposed in a number of recent papers, be carefully followed.42,111,131,151,196 It has been proposed that the routine use of partial thymectomy (cervical thymectomy) at the time of parathyroidectomy may reduce the occurrence of thymic carcinoids, and at present this is generally recommended; however, cases of thymic carcinoid have still occurred in MEN1 patients who have previously had this surgery, therefore careful regular follow-up is required.45,98,140,151,156,235,412,414,477,479 At present the treatment of advanced metastatic disease in patients with thymic carcinoids is not very effective, therefore the main aim at present is to prevent them if possible (with cervical thymectomy) and for their early diagnosis and aggressive surgical treatment.111,131,151
In one-third of patients with MEN1 there is a non-MEN1 cause of death, and at present it is unclear whether any of these causes are actually increased in frequency in MEN1 patients and therefore actually MEN1-related. Heart disease and non-MEN1-related tumors were the main causes in our patients and in those in the literature in large MEN1 series.15,53,54,57,78,88,129,150,217,224,226,254,289,378,379,444,448,465 In the case of heart disease there are possible MEN1-associated factors that are associated with an increased risk of cardiovascular disease which include HPT and glucose intolerance/diabetes, the latter which is reported to occur with increased frequency in MEN1.116,163,271,442,452 Similarly, because of the fundamental role that the menin protein plays in growth-related processes,16,50,195,261,419,469,478 it remains possible that other neoplasms currently thought to be non-MEN1 related might be affected either in frequency or severity in MEN1 patients. At present neither of the above possibilities can be adequately addressed because of the lack of control studies that are prospective in nature addressing either the frequency or severity of cardiovascular disease or other non-MEN1 neoplasms in MEN1 patients. These types of studies will be important in the future to manage these patients and extend their lives.
Abbreviations
- BAO
basal acid output
- CI
confidence interval
- CNS
central nervous system
- CT
computed tomography
- DRS
disease-related survival
- GERD
gastroesophageal reflux disease
- GRFoma
growth hormone-releasing factor-secreting tumor
- GTE
Groupe d’etude des Tumeurs Endocrines
- HPT
hyperparathyroidism
- HR
hazard ratio
- MAO
maximal acid output
- MEN1
multiple endocrine neoplasia type 1
- MEN1/PET
patients with MEN1 with pancreatic endocrine tumors
- MEN1/ZES
patients with MEN1 and Zollinger-Ellison syndrome
- MRI
magnetic resonance imaging
- NET
neuroendocrine tumor
- NIH
National Institutes of Health
- non-MEN1 related
not related to MEN1
- OS
overall survival
- PET
pancreatic endocrine tumor
- PTH
parathormone
- SRS
somatostatin receptor scintigraphy
- VIPoma
vasoactive intestinal peptide secreting tumor
- ZES
Zollinger-Ellison syndrome
Footnotes
Financial support and conflicts of interest: This research was supported in part by funding from the intramural research program of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health. The authors have no conflicts of interest to disclose.
REFERENCES
- 1. Abboud P, Bart H, Mansour G, Pinteaux A, Birembaut P. Ovarian gastrinoma in multiple endocrine neoplasia type I: a case report. Am J Obstet Gynecol. 2001; 184: 237– 238. [DOI] [PubMed] [Google Scholar]
- 2. Adachi K, Kudo M, Chen MN, Nakazawa S, Wakabayashi I. Cerebral aneurysm associated with multiple endocrine neoplasia, type 1—case report. Neurol Med Chir (Tokyo). 1993; 33: 309– 311. [DOI] [PubMed] [Google Scholar]
- 3. Afshar R, Sanavi S, Taheri HR. Acute renal failure as an initial manifestation of multiple endocrine neoplasia (MEN) type 1. Saudi J Kidney Dis Transpl. 2012; 23: 117– 121. [PubMed] [Google Scholar]
- 4. Akimoto T, Ohmura M, Miyamoto T, Ito H, Iizuka T, Tashiro M, Nishikawa T. [A case of pathologic autopsy of type 1 endocrine adenomatosis (MEN) which combined hypophyseal adenoma, thyroid adenoma, parathyroid adenoma, gastric carcinod, glucagonoma and adrenal cortical adenoma]. Horumon To Rinsho. 1997; 45: 251– 254. [Google Scholar]
- 5. Al-Daraji WI, Prescott RJ. Heterotropic cardiac calcification: a rare presentation of multiple endocrine neoplasia. Histopathology. 2005; 47: 651– 652. [DOI] [PubMed] [Google Scholar]
- 6. Al-Salameh A, Francois P, Giraud S, Calender A, Bergemer-Fouquet AM, de Calan L, Goudet P, Lecomte P. Intracranial ependymoma associated with multiple endocrine neoplasia type 1. J Endocrinol Invest. 2010; 33: 353– 356. [DOI] [PubMed] [Google Scholar]
- 7. Alexander HR, Fraker DL, Norton JA, Barlett DL, Tio L, Benjamin SB, Doppman JL, Goebel SU, Serrano J, Gibril F, Jensen RT. Prospective study of somatostatin receptor scintigraphy and its effect on operative outcome in patients with Zollinger-Ellison syndrome. Ann Surg. 1998; 228: 228– 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alzahrani AS, Al-Khaldi N, Shi Y, Al-Rijjal RA, Zou M, Baitei EY, Amin T. Diagnosis by serendipity: Cushing syndrome attributable to cortisol-producing adrenal adenoma as the initial manifestation of multiple endocrine neoplasia type 1 due to a rare splicing site MEN1 gene mutation. Endocr Pract. 2008; 14: 595– 602. [DOI] [PubMed] [Google Scholar]
- 9. Anlauf M, Garbrecht N, Henopp T, Schmitt A, Schlenger R, Raffel A, Krausch M, Gimm O, Eisenberger CF, Knoefel WT, Dralle H, Komminoth P, Heitz PU, Perren A, Kloppel G. Sporadic versus hereditary gastrinomas of the duodenum and pancreas: distinct clinico-pathological and epidemiological features. World J. 2006; 12: 5440– 5446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anlauf M, Perren A, Henopp T, Rudolf T, Garbrecht N, Schmitt A, Raffel A, Gimm O, Weihe E, Knoefel WT, Dralle H, Heitz PU, Komminoth P, Kloppel G. Allelic deletion of the MEN1 gene in duodenal gastrin and somatostatin cell neoplasms and their precursor lesions. Gut. 2007; 56: 637– 644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arnalsteen LC, Alesina PF, Quiereux JL, Farrel SG, Patton FN, Carnaille BM, Cardot-Vauters CM, Wemeau JL, Proye CAG. Long-term results of less than total parathyroidectomy for hyperparathyroidism in multiple endocrine neoplasia type 1. Surgery. 2002; 132: 1119– 1125. [DOI] [PubMed] [Google Scholar]
- 12. Arnold WS, Fraker DL, Alexander HR, Weber HC, Jensen RT. Apparent lymph node primary gastrinoma. Surgery. 1994; 116: 1123– 1130. [PubMed] [Google Scholar]
- 13. Asgharian B, Chen YJ, Patronas NJ, Venzon DJ, Peghini P, Reynolds JC, Vortmeyer A, Zhang ZP, Gibril F, Jensen RT. Meningiomas may be a component tumor of MEN1. Clin Cancer Res. 2004; 10: 869– 880. [DOI] [PubMed] [Google Scholar]
- 14. Asgharian B, Turner ML, Gibril F, Entsuah LK, Serrano J, Jensen RT. Cutaneous tumors in patients with MEN1 and gastrinomas: Prospective study of frequency and development of criteria with high sensitivity and specificity. J Clin Endocrinol Metab. 2004; 89: 5328– 5336. [DOI] [PubMed] [Google Scholar]
- 15. Ballard HS, Frame B, Harstock RJ. Familial endocrine adenoma-peptic ulcer complex. Medicine (Baltimore). 1964; 43: 481– 515. [PubMed] [Google Scholar]
- 16. Balogh K, Racz K, Patocs A, Hunyady L. Menin and its interacting proteins: elucidation of menin function. Trends Endocrinol Metab. 2006; 17: 357– 364. [DOI] [PubMed] [Google Scholar]
- 17. Banasch M, Schmitz F. Diagnosis and treatment of gastrinoma in the era of proton pump inhibitors. Wien Klin Wochenschr. 2007; 119: 573– 578. [DOI] [PubMed] [Google Scholar]
- 18. Barbe C, Murat A, Dupas B, Ruszniewski P, Tabarin A, Vullierme MP, Penfornis A, Rohmer V, Baudin E, Le Rhun M, Gaye D, Marcus C, Cadiot G. Magnetic resonance imaging versus endoscopic ultrasonography for the detection of pancreatic tumours in multiple endocrine neoplasia type 1. Dig Liver Dis. 2012; 44: 228– 234. [DOI] [PubMed] [Google Scholar]
- 19. Bardram L. Progastrin in serum from Zollinger-Ellison patients. An indicator of malignancy? Gastroenterology. 1990; 98: 1420– 1426. [DOI] [PubMed] [Google Scholar]
- 20. Barton JC, Hirschowitz BI, Maton PN, Jensen RT. Bone metastases in malignant gastrinoma. Gastroenterology. 1986; 91: 1179– 1185. [DOI] [PubMed] [Google Scholar]
- 21. Bartsch DK, Fendrich V, Langer P, Celik I, Kann PH, Rothmund M. Outcome of duodenopancreatic resections in patients with multiple endocrine neoplasia type 1. Ann Surg. 2005; 242: 757– 764, discussion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bartsch DK, Langer P, Wild A, Schilling T, Celik I, Rothmund M, Nies C. Pancreaticoduodenal endocrine tumors in multiple endocrine neoplasia type 1: surgery or surveillance? Surgery. 2000; 128: 958– 966. [DOI] [PubMed] [Google Scholar]
- 23. Barzon L, Pasquali C, Grigoletto C, Pedrazzoli S, Boscaro M, Fallo F. Multiple endocrine neoplasia type 1 and adrenal lesions. J Urol. 2001; 166: 24– 27. [PubMed] [Google Scholar]
- 24. Bashir S, Gibril F, Ojeaburu J, Asgharian B, Entsuah L, Ferraro G, Crafa P, Bordi C, Jensen RT. Prospective study of the ability of histamine, serotonin or chromogranin A levels to identify gastric carcinoids in patients with gastrinomas. Aliment Pharmacol Ther. 2002; 16: 1367– 1382. [DOI] [PubMed] [Google Scholar]
- 25. Becker V, Schneider HH. Das Wermer-syndrome: hereditare endokrine polyadenomatose. Deutsche Medizinsche Wochen. 1968; 93: 935– 940. [DOI] [PubMed] [Google Scholar]
- 26. Beckers A, Abs R, Reyniers E, De Boulle K, Stevenaert A, Heller FR, Kloppel G, Meurisse M, Willems PJ. Variable regions of chromosome 11 loss in different pathological tissues of a patient with the multiple endocrine neoplasia type 1 syndrome. J Clin Endocrinol Metab. 1994; 79: 1498– 1502. [DOI] [PubMed] [Google Scholar]
- 27. Beckers A, Abs R, Willems PJ, van der Auwera B, Kovacs K, Reznik M, Stevenaert A. Aldosterone-secreting adrenal adenoma as part of multiple endocrine neoplasia type 1 (MEN1): loss of heterozygosity for polymorphic chromosome 11 deoxyribonucleic acid markers, including the MEN1 locus. J Clin Endocrinol Metab. 1992; 75: 564– 570. [DOI] [PubMed] [Google Scholar]
- 28. Bekele G, Felicetta JV, Gani O, Shah IA. Malignant thymic carcinoid in multiple endocrine neoplasia type I syndrome: case report and literature review. Endocr Pract. 1998; 4: 153– 158. [DOI] [PubMed] [Google Scholar]
- 29. Benson L, Ljunghall S, Akerstrom G, Oberg K. Hyperparathyroidism presenting as the first lesion in multiple endocrine neoplasia type I. Am J Med. 1987; 82: 731– 737. [DOI] [PubMed] [Google Scholar]
- 30. Benson L, Lundqvist G, Wide L, Akerstrom G, Oberg K, Ljunghall S. Effects of secretin on parathyroid hormone and calcium in normal subjects, patients with hyperparathyroidism and patients with gastrinoma. Acta Med Scand. 1985; 217: 205– 211. [DOI] [PubMed] [Google Scholar]
- 31. Benya RV, Metz DC, Venzon DJ, Fishbeyn VA, Strader DB, Orbuch M, Jensen RT. Zollinger-Ellison syndrome can be the initial endocrine manifestation in patients with multiple endocrine neoplasia-type 1. Am J Med. 1994; 97: 436– 444. [DOI] [PubMed] [Google Scholar]
- 32. Berdjis CC. Pluriglandular syndrome. Oncologia. 1962; 15: 288– 311. [PubMed] [Google Scholar]
- 33. Berger AC, Gibril F, Venzon DJ, Doppman JL, Norton JA, Barlett DL, Libutti SK, Jensen RT, Alexander HR. Prognostic value of initial fasting serum gastrin level in patients with Zollinger-Ellison syndrome. J Clin Oncol. 2001; 19: 3051– 3057. [DOI] [PubMed] [Google Scholar]
- 34. Berna MJ, Annibale B, Marignani M, Luong TV, Corleto V, Pace A, Ito T, Liewehr DJ, Venzon DJ, Delle Fave G, Bordi C, Jensen RT. A prospective study of gastric carcinoids and enterochromaffin-like cells changes in multple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: identification of risk factors. J Clin Endocrinol Metab. 2008; 93: 1582– 1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Berna MJ, Hoffmann KM, Long SH, Serrano J, Gibril F, Jensen RT. Serum gastrin in Zollinger-Ellison syndrome: II. Prospective study of gastrin provocative testing in 293 patients from the National Institutes of Health and comparison with 537 cases from the literature. Evaluation of diagnostic criteria, proposal of new criteria, and correlations with clinical and tumoral features. Medicine (Baltimore). 2006; 85: 331– 364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Berna MJ, Hoffmann KM, Serrano J, Gibril F, Jensen RT. Serum gastrin in Zollinger-Ellison syndrome: I. Prospective study of fasting serum gastrin in 309 patients from the National Institutes of Health and comparison with 2229 cases from the literature. Medicine (Baltimore). 2006; 85: 295– 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bettini R, Boninsegna L, Mantovani W, Capelli P, Bassi C, Pederzoli P, Della Fave G, Panzuto F, Scarpa A, Falconi M. Prognostic factors at diagnosis and value of WHO classification in a mono-institutional series of 180 non-functioning pancreatic endocrine tumours. Ann Oncol. 2008; 19: 903– 908. [DOI] [PubMed] [Google Scholar]
- 38. Boix E, Pico A, Pinedo R, Aranda I, Kovacs K. Ectopic growth hormone-releasing hormone secretion by thymic carcioid tumour. Clin Endocrinol. 2002; 57: 131– 134. [DOI] [PubMed] [Google Scholar]
- 39. Boni R, Vortmeyer AO, Pack S, Park WS, Burg G, Hofbauer G, Darling T, Liotta L, Zhuang Z. Somatic mutations of the MEN1 tumor suppressor gene detected in sporadic angiofibromas. J Invest Dermatol. 2003; 111: 539– 540. [DOI] [PubMed] [Google Scholar]
- 40. Bordi C, Falchetti A, Azzoni C, D’Adda T, Canavese G, Guariglia A, Santini D, Tomassetti P, Brandi ML. Aggressive forms of gastric neuroendocrine tumors in multiple endocrine neoplasia type I. Am J Surg Pathol. 1997; 21: 1075– 1082. [DOI] [PubMed] [Google Scholar]
- 41. Botsios D, Vasiliadis K, Tsalis K, Iordanidis F, Megalopoulos A, Tsachalis T, Blouhos K, Betsis D. Management of nonfunctioning pancreatic endocrine tumors in the context of multiple endocrine neoplasia type 1 syndrome. J Gastrointestin Liver Dis. 2007; 16: 257– 262. [PubMed] [Google Scholar]
- 42. Brandi ML, Gagel RF, Angeli A, Bilezikian JP, Beck-Peccoz P, Bordi C, Conte-Devolx B, Falchetti A, Gheri RG, Libroia A, Lips CJM, Lombardi G, Mannelli M, Pacini F, Ponder BAJ, Raue F, Skogseid B, Tamburrano G, Thakker RV, Thompson NW, Tomassetti P, Tonelli F, Wells SA, Jr, Marx SJ. Guidelines for diagnosis and therapy of MEN type 1 and type 2. J Clin Endocrinol Metab. 2001; 86: 5658– 5671. [DOI] [PubMed] [Google Scholar]
- 43. Bricaire H, Courjaret J, Ferrier JP. Syndrome de Zollinger-Ellison associe a une tumeur de la loge hypophysaire. Interet pratique de la recherche du pouvoir secretagogue urinaire. Societe Medicale des Hopitaux de Paris. 1966; 117: 829– 839. [PubMed] [Google Scholar]
- 44. Burgess JR, David R, Parameswaran V, Greenaway TM, Shepherd JJ. The outcome of subtotal parathyroidectomy for the treatment of hyperparathyroidism in multiple endocrine neoplasia type 1. Arch Surg. 1998; 133: 126– 129. [DOI] [PubMed] [Google Scholar]
- 45. Burgess JR, Giles N, Shepherd JJ. Malignant thymic carcinoid is not prevented by transcervical thymectomy in multiple endocrine neoplasia type 1. Clin Endocrinol (Oxf). 2001; 55: 689– 693. [DOI] [PubMed] [Google Scholar]
- 46. Burgess JR, Greenaway TM, Parameswaran V, Challis DR, David R, Shepherd JJ. Enteropancreatic malignancy associated with multiple endocrine neoplasia type 1. Cancer. 1998; 83: 428– 434. [DOI] [PubMed] [Google Scholar]
- 47. Burgess JR, Greenaway TM, Shepherd JJ. Expression of the MEN-1 gene in a large kindred with multiple endocrine neoplasia type 1. J Intern Med. 1998; 243: 465– 470. [DOI] [PubMed] [Google Scholar]
- 48. Burgess JR, Harle RA, Tucker P, Parameswaran V, Davies P, Greenaway TM, Shepherd JJ. Adrenal lesions in a large kindred with multiple endocrine neoplasia type 1. Arch Surg. 1996; 131: 699– 702. [DOI] [PubMed] [Google Scholar]
- 49. Burgess JR, Shepherd JJ, Parameswaran V, Hoffman L, Greenaway TM. Spectrum of pituitary disease in multiple endocrine neoplasia type 1 (MEN1): clinical, biochemical, and radiological features of pituitary disease in a large MEN1 kindred. J Clin Endocrinol Metab. 1996; 81: 2642– 2646. [DOI] [PubMed] [Google Scholar]
- 50. Busygina V, Bale AE. Multiple endocrine neoplasia type 1 (MEN1) as a cancer predisposition syndrome: clues into the mechanisms of MEN1-related carcinogenesis. Yale J Biol Med. 2006; 79: 105– 114. [PMC free article] [PubMed] [Google Scholar]
- 51. Butte JM, Montero PH, Solar A, Torres J, Olmos PR, Goni I, Quintana JC, Martinez J, Llanos O. Cervical metastases of glucagonoma in a patient with multiple endocrine neoplasia type 1: report of a case. Surg Today. 2008; 38: 1137– 1143. [DOI] [PubMed] [Google Scholar]
- 52. Cadiot G, Helie C, Vallot T, Marmuse JP, Cosnes J, Riche A, Mignon M. [Stenosing esophagitis in Zollinger-Ellison syndrome]. Gastroenterol Clin Biol. 1994; 18: 1018– 1020. [PubMed] [Google Scholar]
- 53. Cadiot G, Laurent-Puig P, Thuille B, Lehy T, Mignon M, Olschwang S. Is the multiple endocrine neoplasia type 1 gene a suppressor for fundic argyrophil tumors in the Zollinger-Ellison syndrome? Gastroenterology. 1993; 105: 579– 582. [DOI] [PubMed] [Google Scholar]
- 54. Cadiot G, Vuagnat A, Doukhan I, Murat A, Bonnaud G, Delemer B, Thiefin G, Beckers A, Veyrac M, Proye C, Ruszniewski P, Mignon M. Prognostic factors in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1. Gastroenterology. 1999; 116: 286– 293. [DOI] [PubMed] [Google Scholar]
- 55. Cameron AJ, Hoffman HN. Zollinger-Ellison syndrome; clinical features and long-term follow-up. Mayo Clin Proc. 1974; 49: 44– 51. [PubMed] [Google Scholar]
- 56. Carnevale V, Romagnoli E, Remotti D, D’Erasmo E, Spagna G, Pisani D, Rosso R, Minisola S, Mazzuoli GF. Pulmonary lymphangioleiomyoma in a patient with multiple endocrine neoplasia type I. J Endocrinol Invest. 1997; 20: 282– 285. [DOI] [PubMed] [Google Scholar]
- 57. Carty SE, Helm AK, Amico JA, Clarke MR, Foley TP, Watson CG, Mulvihill JJ. The variable penetrance and spectrum of manifestations of multiple endocrine neoplasia type 1. Surgery. 1998; 124: 1106– 1114. [DOI] [PubMed] [Google Scholar]
- 58. Carty SE, Jensen RT, Norton JA. Prospective study of aggressive resection of metastatic pancreatic endocrine tumors. Surgery. 1992; 112: 1024– 1031. [PubMed] [Google Scholar]
- 59. Cavaco BM, Domingues R, Bacelar MC, Cardoso H, Barros L, Gomes L, Ruas MMA, Agapito A, Garrao A, Pannett AAJ, Silva JL, Sobrinho LG, Thakker RV, Leite V. Mutational analysis of Portuguese families with multiple endocrine neoplasia type 1 reveals large germline deletions. Clin Endocrinol. 2002; 56: 465– 473. [DOI] [PubMed] [Google Scholar]
- 60. Champault G, Chapuis Y, Patel JC, Louvel A, Ghozlan R, Cachin M, Leger L. [Zollinger-Ellison syndrome and parathyroid adenoma. Limits of Wermer’s syndrome]. J Chir (Paris). 1976; 112: 131– 144. [PubMed] [Google Scholar]
- 61. Chan JA, Kulke MH. New treatment options for patients with advanced neuroendocrine tumors. Curr Treat Options Oncol. 2011; 12: 136– 148. [DOI] [PubMed] [Google Scholar]
- 62. Chandrasekharappa SC, Guru SC, Manickam P, Olufemi SE, Collins FS, Emmert-Buck MR, Debelenko LV, Zhuang Z, Lubensky IA, Liotta LA, Crabtree JS, Wang Y, Roe BA, Weisemann J, Boguski MS, Agarwal SK, Kester MB, Kim YS, Heppner C, Dong Q, Spiegel AM, Burns AL, Marx SJ. Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science. 1997; 276: 404– 407. [DOI] [PubMed] [Google Scholar]
- 63. Chanson P, Cadiot G, Murat A. Management of patients and subjects at risk for multiple endocrine neoplasia type 1: MEN1. Horm Res. 1997; 47: 211– 220. [DOI] [PubMed] [Google Scholar]
- 64. Cherner JA, Doppman JL, Norton JA, Miller DL, Krudy AG, Raufman JP, Collen MJ, Maton PN, Gardner JD, Jensen RT. Selective venous sampling for gastrin to localize gastrinomas. A prospective study. Ann Intern Med. 1986; 105: 841– 847. [DOI] [PubMed] [Google Scholar]
- 65. Chiu KC, Chuang LM, Lee NP, Ryu JM, McGullam JL, Tsai GP, Saad MF. Insulin sensitivity is inversely correlated with plasma intact parathyroid hormone level. Metabolism. 2000; 49: 1501– 1505. [DOI] [PubMed] [Google Scholar]
- 66. Choi H, Kim S, Moon JH, Lee YH, Rhee Y, Kang ES, Ahn CW, Cha BS, Lee EJ, Kim KR, Lee HC, Jeong SY, Kim HJ, Lim SK. Multiple endocrine neoplasia type 1 with multiple leiomyomas linked to a novel mutation in the MEN1 gene. Yonsei Med J. 2008; 49: 655– 661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chu QD, Hill HC, Douglass HO, Jr, Driscoll D, Smith JL, Nava HR, Gibbs JF. Predictive factors associated with long-term survival in patients with neuroendocrine tumors of the pancreas. Ann Surg Oncol. 2002; 9: 855– 862. [DOI] [PubMed] [Google Scholar]
- 68. Cohen BD, Lubash GD, Rubin AL. Parathyroid and pancreatic adenomas. Am J Med. 1959; 26: 801– 807. [DOI] [PubMed] [Google Scholar]
- 69. Collen MJ, Howard JM, McArthur KE, Raufman JP, Cornelius MJ, Ciarleglio CA, Gardner JD, Jensen RT. Comparison of ranitidine and cimetidine in the treatment of gastric hypersecretion. Ann Intern Med. 1984; 100: 52– 58. [DOI] [PubMed] [Google Scholar]
- 70. Collins JSA, Buchanan KD, Kennedy TL, Johnston CF, Ardill JES, Sloan JM, McIlrath EM, Russell C. Changing patterns in presentation and management of the Zollinger-Ellison syndrome in Northern Ireland, 1970-1988. Q J Med. 1991; 78: 215– 225. [PubMed] [Google Scholar]
- 71. Cougard P, Goudet P, Peix JL, Henry JF, Sarfati E, Proye C, Calender A. [Insulinomas in multiple endocrine neoplasia type 1. Report of a series of 44 cases by the multiple endocrine neoplasia study group]. Ann Chir. 2000; 125: 118– 123. [DOI] [PubMed] [Google Scholar]
- 72. Craven DE, Goodman D, Carter JH. Familial multiple endocrine adenomatosis: multiple endocrine neoplasia, type I. Arch Intern Med. 1972; 129: 567– 569. [PubMed] [Google Scholar]
- 73. Croisier JC, Azerad E, Lubetzki J. Adenomatose polyendocrinenne (syndrome de Wermer): a propos d’une observation personelle. Revue de la Litterature. 1971; Paris:Sem Hopital;47: 494– 525. [PubMed] [Google Scholar]
- 74. Darling TN, Skarulis MC, Steinberg SM, Marx SJ, Spiegel AM, Turner M. Multiple facial angiofibromas and collagenomas in patients with multiple endocrine neoplasia type 1. Arch Dermatol. 1997; 133: 853– 857. [PubMed] [Google Scholar]
- 75. Davi MV, Boninsegna L, Dalle Carbonare L, Toaiari M, Capelli P, Scarpa A, Francia G, Falconi M. Presentation and outcome of pancreaticoduodenal endocrine tumors in multiple endocrine neoplasia type 1 syndrome. Neuroendocrinology. 2011; 94: 58– 65. [DOI] [PubMed] [Google Scholar]
- 76. de Herder WW, van SE, Kwekkeboom D, Feelders RA. New therapeutic options for metastatic malignant insulinomas. Clin Endocrinol (Oxf). 2011; 75: 277– 284. [DOI] [PubMed] [Google Scholar]
- 77. De Toma G, Plocco M, Nicolanti V, Brozzetti S, Letizia C, Cavallaro A. Type B1 thymoma in multiple endocrine neoplasia type 1 (MEN-1) syndrome. Tumori. 2001; 87: 266– 268. [DOI] [PubMed] [Google Scholar]
- 78. Dean PG, Van Heerden JA, Farley DR, Thompson GB, Grant CS, Harmsen WS, Ilstrup DM. Are patients with multiple endocrine neoplasia type I prone to premature death? World J Surg. 2000; 24: 1437– 1441. [DOI] [PubMed] [Google Scholar]
- 79. Debelenko LV, Emmert-Buck MR, Zhuang Z, Epshteyn E, Moskaluk CA, Jensen RT, Liotta LA, Lubensky IA. The multiple endocrine neoplasia type 1 gene locus is involved in the pathogenesis of type II gastric carcinoids. Gastroenterology. 1997; 113: 773– 782. [DOI] [PubMed] [Google Scholar]
- 80. Debelenko LV, Zhuang ZP, Emmert-Buck MR, Chandrasekharappa S, Manickam P, Guru SC, Marx SJ, Skarulis M, Spiegel AM, Collins FS, Jensen RT, Liotta LA, Lubensky IA. Allelic deletions on chromosome 11q13 in multiple endocrine neoplasia type-I-associated sporadic gastrinomas and pancreatic endocrine tumors. Cancer Res. 1997; 57: 2238– 2243. [PubMed] [Google Scholar]
- 81. Debski MG, Makowska A, Bar-Andziak E. Insulinoma in a patient with MEN 1 syndrome—9-year follow-up: case report. Endokrynol Pol. 2010; 61: 212– 216. [PubMed] [Google Scholar]
- 82. Demeure MJ, Klonoff DC, Karam JH, Duh QY, Clark OH. Insulinomas associated with multiple endocrine neoplasia type I: the need for a different surgical approach. Surgery. 1991; 110: 998– 1005. [PubMed] [Google Scholar]
- 83. DeNeef JC, Krull GH, Vonk J, Vos AK, Bool J. Zollinger-Ellison syndrome in a patient with secondary amenorrhea; report of a case with fatal outcome. Fertil Steril. 1970; 21: 43– 63. [DOI] [PubMed] [Google Scholar]
- 84. Denker PS, Wright D, Hilscher JR, Saba SR, Ramirez G. Hypernephroma associated with multiple endocrine neoplasia type I: a case report. J Urol. 1986; 136: 896– 898. [DOI] [PubMed] [Google Scholar]
- 85. Deveney CW, Deveney KS, Jaffe BM, Jones RS, Way LW. Use of calcium and secretin in the diagnosis of gastrinoma (Zollinger-Ellison syndrome). Ann Intern Med. 1977; 87: 680– 686. [DOI] [PubMed] [Google Scholar]
- 86. Dionisi S, Minisola S, Pepe J, DeGeronimo S, Paglia F, Memeo L, Fitzpatrick LA. Concurrent parathyroid adenomas and carcinoma in the setting of multiple endocrine neoplasia type 1: presentation as hypercalcemic crisis. Mayo Clin Proc. 2002; 77: 866– 869. [DOI] [PubMed] [Google Scholar]
- 87. Doherty GM. Multiple endocrine neoplasia type 1: duodenopancreatic tumors. Surg Oncol. 2003; 12: 135– 143. [DOI] [PubMed] [Google Scholar]
- 88. Doherty GM, Olson JA, Frisella MM, Lairmore TC, Wells SA, Jr, Norton JA. Lethality of multiple endocrine neoplasia type I. World J Surg. 1998; 22: 581– 587. [DOI] [PubMed] [Google Scholar]
- 89. Dong Q, Debelenko LV, Chandrasekharappa S, Lotterman C, Skarulis M, Emmert-Buck MR, Zhuang Z, Guru SC, Manickam P, Lubensky IA, Liotta LA, Collins FS, Marx SJ, Spiegel AM. Loss of heterozygosity at 11q13: analysis of pituitary tumors, lung carcinoids, lipomas, and other uncommon tumors in subjects with familial multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1997; 82: 1416– 1420. [DOI] [PubMed] [Google Scholar]
- 90. Donow C, Pipeleers-Marichal M, Schroder S, Stamm B, Heitz PU, Kloppel G. Surgical pathology of gastrinoma: site, size, multicentricity, association with multiple endocrine neoplasia type 1, and malignancy. Cancer. 1991; 68: 1329– 1334. [DOI] [PubMed] [Google Scholar]
- 91. Doppman JL, Miller DL, Chang R, Maton PN, London JF, Gardner JD, Jensen RT, Norton JA. Gastrinomas: localization by means of selective intraarterial injection of secretin. Radiology. 1990; 174: 25– 29. [DOI] [PubMed] [Google Scholar]
- 92. Doppman JL, Miller DL, Chang R, Shawker TH, Gorden P, Norton JA. Insulinomas: localization with selective intraarterial injection of calcium. Radiology. 1991; 178: 237– 241. [DOI] [PubMed] [Google Scholar]
- 93. Dotzenrath C, Cupisti K, Goretzki PE, Yang Q, Simon D, Ohmann C, Roher HD. Long-term biochemical results after operative treatment of primary hyperparathyroidism associated with multiple endocrine types I and IIa: is a more or less extended operation essential? Eur J Surg. 2001; 167: 173– 178. [DOI] [PubMed] [Google Scholar]
- 94. Dotzenrath C, Goretzki PE, Cupisti K, Yang Q, Simon D, Roher HD. Malignant endocrine tumors in patients with MEN1 disease. Surgery. 2001; 129: 91– 95. [DOI] [PubMed] [Google Scholar]
- 95. Doumith R, de Gennes JL, Cabane JP, Zygelman N. Pituitary prolactinoma, adrenal aldosterone-producing adenomas, gastric schwannoma and colonic polyadenomas: a possible variant of multiple endocrine neoplasia (MEN) type I. Acta Endocrinol (Copenh). 1982; 100: 189– 195. [DOI] [PubMed] [Google Scholar]
- 96. Dubois A, Eerdewegh PV, Gardner JD. Gastric emptying and secretion in Zollinger-Ellison syndrome. J Clin Invest. 1977; 59: 255– 263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Duggan M, Anderson C. Mixed type Zollinger-Ellison syndrome in a florid case of multiple endocrine neoplasia type I. Am J Clin Pathol. 1984; 82: 481– 486. [DOI] [PubMed] [Google Scholar]
- 98. Duh QY, Hybarger CP, Geist R, Gamsu G, Goodman PC, Gooding GA, Clark OH. Carcinoids associated with multiple endocrine neoplasia syndromes. Am J Surg. 1987; 154: 142– 148. [DOI] [PubMed] [Google Scholar]
- 99. Duquenne M, Weryha G, Leclere J, Duriez T, Schneegans O. [Renal oncocytoma in multiple endocrine neoplasia type 1]. Presse Med. 1992; 21: 1293– 1294. [PubMed] [Google Scholar]
- 100. Durante C, Boukheris H, Dromain C, Duvillard P, Leboulleux S, Elias D, De Baere T, Malka D, Lumbroso J, Guigay J, Schlumberger M, Ducreux M, Baudin E. Prognostic factors influencing survival from metastatic (stage IV) gastroenteropancreatic well-differentiated endocrine carcinoma. Endocr Relat Cancer. 2009; 16: 585– 597. [DOI] [PubMed] [Google Scholar]
- 101. Ebeling T, Vierimaa O, Kytola S, Leisti J, Salmela PI. Effect of multiple endocrine neoplasia type 1 (MEN1) gene mutations on premature mortality in familial MEN1 syndrome with founder mutations. J Clin Endocrinol Metab. 2004; 89: 3392– 3396. [DOI] [PubMed] [Google Scholar]
- 102. Eberle F, Grun R. Multiple endocrine neoplasia, type I (MEN I). Ergeb Inn Med Kinderheilkd. 1981; 46: 76– 149. [PubMed] [Google Scholar]
- 103. Ekeblad S, Skogseid B, Dunder K, Oberg K, Eriksson B. Prognostic factors and survival in 324 patients with pancreatic endocrine tumor treated at a single institution. Clin Cancer Res. 2008; 14: 7798– 7803. [DOI] [PubMed] [Google Scholar]
- 104. Elaraj DM, Skarulis MC, Libutti SK, Norton JA, Barlett DL, Pingpark JF, Gibril F, Weinstein LS, Jensen RT, Marx SJ, Alexander HR. Results of initial operation for hyperparathryoidism (HPT) in patients with multiple endocrine neoplasia type 1 (MEN1). Surgery. 2003; 134: 858– 864. [DOI] [PubMed] [Google Scholar]
- 105. Ellison EC. Forty-year appraisal of gastrinoma. Ann Surg. 1995; 222: 511– 524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Ellison EC, Carey LC, Sparks J, O’Dorisio TM, Mekhjian HS, Fromkes JJ, Caldwell JH, Thomas FB. Early surgical treatment of gastrinoma. Am J Med. 1987; 82: 17– 24. [DOI] [PubMed] [Google Scholar]
- 107. Ellison EH. The ulcerogenic tumors of the pancreas. Surgery. 1956; 40: 147– 154. [PubMed] [Google Scholar]
- 108. Ellison EH, Wilson SD. The Zollinger-Ellison syndrome: re-appraisal and evaluation of 260 registered cases. Ann Surg. 1964; 160: 512– 530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Emi I, Akira U, Hideki K, Hideki M. [An autopsy case of a MEN1 patient complicating mucinous carcinoma of the colon with neurendocrine differentiation]. Nihon Naibunpi Gakkai Zasshi. 2001; 77: 92– 94. [Google Scholar]
- 110. Falconi M, Bartsch DK, Eriksson B, Kloppel G, Lopes JM, O’connor JM, Salazar R, Taal BG, Vullierme MP, O’Toole D. ENETS consensus guidelines for the management of patients with digestive neuroendocrine neoplasms of the digestive system: well-differentiated pancreatic non-functioning tumors. Neuroendocrinology. 2012; 95: 120– 134. [DOI] [PubMed] [Google Scholar]
- 111. Ferolla P, Falchetti A, Filosso P, Tomassetti P, Tamburrano G, Avenia N, Daddi G, Puma F, Ribacchi R, Santeusanio F, Angeletti G, Brandi ML. Thymic neuroendocrine carcinoma (carcinoid) in multiple endocrine neoplasia type 1 syndrome: the Italian series. J Clin Endocrinol Metab. 2005; 90: 2603– 2609. [DOI] [PubMed] [Google Scholar]
- 112. Fiasse R, DeGraef J, Pauwels S, Woussen-Colle MC, Rahier J, Kestens PJ, Dive C. [Hypergastrinemia. Physiopathological and clinical aspects with a study of a series of Zollinger-Ellison cases]. Acta Gastroenterol Belg. 1982; 45: 293– 309. [PubMed] [Google Scholar]
- 113. Fiasse R, Pauwels S, Rahier J, Jamar F, Ketelslegers JM, Hassoun A, deLongueville M. [Use of octreotide in the treatment of digestive neuroendocrine tumours. Seven year experience in 20 cases including 9 cases of metastatic midgut carcinoid and 5 cases of metastatic gastrinoma]. Acta Gastroenterol Belg. 1993; 56: 279– 291. [PubMed] [Google Scholar]
- 114. Fischer L, Kleeff J, Esposito I, Hinz U, Zimmermann A, Friess H, Buchler MW. Clinical outcome and long-term survival in 118 consecutive patients with neuroendocrine tumours of the pancreas. Br J Surg. 2008; 95: 627– 635. [DOI] [PubMed] [Google Scholar]
- 115. Fishbeyn VA, Norton JA, Benya RV, Pisegna JR, Venzon DJ, Metz DC, Jensen RT. Assessment and prediction of long-term cure in patients with Zollinger-Ellison syndrome: the best approach. Ann Intern Med. 1993; 119: 199– 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005; 28: 1769– 1778. [DOI] [PubMed] [Google Scholar]
- 117. Fox PS, Hofmann JW, Decosse JJ, Wilson SD. The influence of total gastrectomy on survival in malignant Zollinger-Ellison tumors. Ann Surg. 1974; 180: 558– 566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Fraker DL, Norton JA, Alexander HR, Venzon DJ, Jensen RT. Surgery in Zollinger-Ellison syndrome alters the natural history of gastrinoma. Ann Surg. 1994; 220: 320– 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Friedman NB. Chronic hypoglycemia. Arch Pathol. 1939; 27: 994– 1010. [Google Scholar]
- 120. Friesen SR. The development of endocrinopathies in the prospective screening of two families with multiple endocrine adenopathy, type I. World J Surg. 1979; 3: 753– 764. [DOI] [PubMed] [Google Scholar]
- 121. Frucht H, Doppman JL, Norton JA, Miller DL, Dwyer AJ, Frank JA, Vinayek R, Maton PN, Jensen RT. Gastrinomas: comparison of MR imaging with CT, angiography and US. Radiology. 1989; 171: 713– 717. [DOI] [PubMed] [Google Scholar]
- 122. Frucht H, Howard JM, Slaff JI, Wank SA, McCarthy DM, Maton PN, Vinayek R, Gardner JD, Jensen RT. Secretin and calcium provocative tests in the Zollinger-Ellison syndrome: a prospective study. Ann Intern Med. 1989; 111: 713– 722. [DOI] [PubMed] [Google Scholar]
- 123. Frucht H, Maton PN, Jensen RT. Use of omeprazole in patients with the Zollinger-Ellison syndrome. Dig Dis Sci. 1991; 36: 394– 404. [DOI] [PubMed] [Google Scholar]
- 124. Frucht H, Norton JA, London JF, Vinayek R, Doppman JL, Gardner JD, Jensen RT, Maton PN. Detection of duodenal gastrinomas by operative endoscopic transillumination: a prospective study. Gastroenterology. 1990; 99: 1622– 1627. [DOI] [PubMed] [Google Scholar]
- 125. Fujio Z, Fukamachi Y, Ito H, Hisaoka M, Hashimoto H, Toshiko T, Yamaguchi K. [A case report of glucagonoma with hepatic metastases in multiple endocrine neoplasia type 1]. Japanese J Clin Exp Med. 2001; 78: 567. [Google Scholar]
- 126. Furuto-Kato S, Shimatsu A, Kuzuya H, Matsuda K, Nakao K, Imura H. Insulin sensitivity and glycemic control before and after parathyroidectomy in a diabetic patient with familial multiple endocrine neoplasia type 1. Endocr J. 1994; 41: 731– 735. [DOI] [PubMed] [Google Scholar]
- 127. Garrot C, Stuart K. Liver-directed therapies for metastatic neuroendocrine tumors. Hematol Oncol Clin North Am. 2007; 21: 545– 560. [DOI] [PubMed] [Google Scholar]
- 128. Gatta-Cherifi B, Chabre O, Murat A, Niccoli P, Cardot-Bauters C, Rohmer V, Young J, Delemer B, Du Boullay H, Verger MF, Kuhn JM, Sadoul JL, Ruszniewski P, Beckers A, Monsaingeon M, Baudin E, Goudet P, Tabarin A. Adrenal involvement in MEN1. Analysis of 715 cases from the Groupe d’etude des Tumeurs Endocrines database. Eur J Endocrinol. 2012; 166: 269– 279. [DOI] [PubMed] [Google Scholar]
- 129. Geerdink EAM, van der Luijt RB, Lips CJ. Do patients with multiple endocrine neoplasia syndrome type 1 benefit from periodical screening? Eur J Endocrinol. 2003; 149: 577– 582. [DOI] [PubMed] [Google Scholar]
- 130. Ghazi AA, Dezfooli AA, Mohamadi F, Yousefi SV, Amirbaigloo A, Ghazi S, Pourafkari M, Berney D, Ellard S, Grossman AB. Cushing syndrome secondary to a thymic carcinoid tumor due to multiple endocrine neoplasia type 1. Endocr Pract. 2011; 17: e92– e96. [DOI] [PubMed] [Google Scholar]
- 131. Gibril F, Chen Y-J, Schrump DS, Vortmeyer A, Zhuang ZP, Lubensky IA, Reynolds JG, Louie JV, Entsuah L, Huang K, Asgharian B, Jensen RT. Prospective study of thymic carcinoids in patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 2003; 88: 1066– 1081. [DOI] [PubMed] [Google Scholar]
- 132. Gibril F, Doppman JL, Chang R, Weber HC, Termanini B, Jensen RT. Metastatic gastrinomas: localization with selective arterial injection of secretin. Radiology. 1996; 198: 77– 84. [DOI] [PubMed] [Google Scholar]
- 133. Gibril F, Doppman JL, Reynolds JC, Chen CC, Sutliff VE, Yu F, Serrano J, Venzon DJ, Jensen RT. Bone metastases in patients with gastrinomas: a prospective study of bone scanning, somatostatin receptor scanning, and MRI in their detection, their frequency, location and effect of their detection on management. J Clin Oncol. 1998; 16: 1040– 1053. [DOI] [PubMed] [Google Scholar]
- 134. Gibril F, Jensen RT. Diagnostic uses of radiolabelled somatostatin-receptor analogues in gastroenteropancreatic endocrine tumors. Dig Liver Dis. 2004; 36: S106– S120. [DOI] [PubMed] [Google Scholar]
- 135. Gibril F, Jensen RT. Zollinger-Ellison syndrome revisited: diagnosis, biologic markers, associated inherited disorders, and acid hypersecretion. Curr Gastroenterol Rep. 2004; 6: 454– 463. [DOI] [PubMed] [Google Scholar]
- 136. Gibril F, Jensen RT. Advances in evaluation and management of gastrinoma in patients with Zollinger-Ellison syndrome. Curr Gastroenterol Rep. 2005; 7: 114– 121. [DOI] [PubMed] [Google Scholar]
- 137. Gibril F, Reynolds JC, Chen CC, Yu F, Goebel SU, Serrano J, Doppman JL, Jensen RT. Specificity of somatostatin receptor scintigraphy: a prospective study and the effects of false positive localizations on management in patients with gastrinomas. J Nucl Med. 1999; 40: 539– 553. [PubMed] [Google Scholar]
- 138. Gibril F, Reynolds JC, Doppman JL, Chen CC, Venzon DJ, Termanini B, Weber HC, Stewart CA, Jensen RT. Somatostatin receptor scintigraphy: its sensitivity compared with that of other imaging methods in detecting primary and metastatic gastrinomas: a prospective study. Ann Intern Med. 1996; 125: 26– 34. [DOI] [PubMed] [Google Scholar]
- 139. Gibril F, Reynolds JC, Roy PK, Peghini PL, Doppman JL, Jensen RT. Ability of somatostatin receptor scintigraphy to identify patients with localized gastric carcinoids: a prospective study. J Nucl Med. 2000; 41: 1646– 1656. [PubMed] [Google Scholar]
- 140. Gibril F, Schumann M, Pace A, Jensen RT. Multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome. A prospective study of 107 cases and comparison with 1009 patients from the literature. Medicine (Baltimore). 2004; 83: 43– 83. [DOI] [PubMed] [Google Scholar]
- 141. Gibril F, Venzon DJ, Ojeaburu JV, Bashir S, Jensen RT. Prospective study of the natural history of gastrinoma in patients with MEN1: definition of an aggressive and a nonaggressive form. J Clin Endocrinol Metab. 2001; 86: 5282– 5293. [DOI] [PubMed] [Google Scholar]
- 142. Giraud S, Choplin H, Teh BT, Lespinasse J, Jouvet A, Labat-Moleur F, Lenoir G, Hamon B, Hamon P, Calender A. A large multiple endocrine neoplasia type 1 family with clinical expression suggestive of anticipation. J Clin Endocrinol Metab. 1997; 82: 3487– 3492. [DOI] [PubMed] [Google Scholar]
- 143. Giraud S, Zhang CX, Serova-Sinilnikova O, Wautot V, Salandre J, Buisson N, Waterlot C, Bauters C, Porchet N, Aubert JP, Emy P, Cadiot G, Delemer B, Chabre O, Niccoli P, Leprat F, Duron F, Emperauger B, Cougard P, Goudet P, Sarfati E, Riou JP, Guichard S, Rodier M, Meyrier A, et al. Germ-line mutation analysis in patients with multiple endocrine neoplasia type 1 and related disorders. Am J Hum Genet. 1998; 63: 455– 467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Giudici F, Nesi G, Brandi ML, Tonelli F. Surgical management of insulinomas in multiple endocrine neoplasia type 1. Pancreas. 2012; 41: 547– 553. [DOI] [PubMed] [Google Scholar]
- 145. Glanemann M, Shi B, Liang F, Sun XG, Bahra M, Jacob D, Neumann U, Neuhaus P. Surgical strategies for treatment of malignant pancreatic tumors: extended, standard or local surgery? World J Surg Oncol. 2008; 6: 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Goebel SU, Heppner C, Burns AD, Marx SJ, Spiegel AM, Zhuang ZP, Gibril F, Jensen RT, Serrano J. Geneotype/phenotype correlations of MEN1 gene mutations in sporadic gastrinoma. J Clin Endocrinol Metab. 2000; 85: 116– 123. [DOI] [PubMed] [Google Scholar]
- 147. Gordon MV, Varma D, McLean CA, Bittar RG, Burgess JR, Topliss DJ. Metastatic prolactinoma presenting as a cervical spinal cord tumour in multiple endocrine neoplasia type one (MEN-1). Clin Endocrinol (Oxf). 2007; 66: 150– 152. [DOI] [PubMed] [Google Scholar]
- 148. Goudet P, Bonithon-Kopp C, Murat A, Ruszniewski P, Niccoli P, Menegaux F, Chabrier G, Borson-Chazot F, Tabarin A, Bouchard P, Cadiot G, Beckers A, Guilhem I, Chabre O, Caron P, Du Boullay H., Verges B, Cardot-Bauters C. Gender-related differences in MEN1 lesion occurrence and diagnosis: a cohort study of 734 cases from the Groupe d’etude des Tumeurs Endocrines. Eur J Endocrinol. 2011; 165: 97– 105. [DOI] [PubMed] [Google Scholar]
- 149. Goudet P, Cougard P, Verges B, Murat A, Carnaille B, Calender A, Faivre J, Proye C. Hyperparathyroidism in multiple endocrine neoplasia type I: surgical trends and results of a 256-patient series from Groupe d’Etude des Neoplasies Endocriniennes Multiples study group. World J Surg. 2001; 25: 886– 890. [DOI] [PubMed] [Google Scholar]
- 150. Goudet P, Murat A, Binquet C, Cardot-Bauters C, Costa A, Ruszniewski P, Niccoli P, Menegaux F, Chabrier G, Borson-Chazot F, Tabarin A, Bouchard P, Delemer B, Beckers A, Bonithon-Kopp C. Risk factors and causes of death in MEN1 disease. A GTE (Groupe d’Etude des Tumeurs Endocrines) cohort study among 758 patients. World J Surg. 2010; 34: 249– 255. [DOI] [PubMed] [Google Scholar]
- 151. Goudet P, Murat A, Cardot-Bauters C, Emy P, Baudin E, du Boullay CH, Chapuis Y, Kraimps JL, Sadoul JL, Tabarin A, Verges B, Carnaille B, Niccoli-Sire P, Costa A, Calender A. Thymic neuroendocrine tumors in multiple endocrine neoplasia type 1: a comparative study on 21 cases among a series of 761 MEN1 from the GTE (Groupe des Tumeurs Endocrines). World J Surg. 2009; 33: 1197– 1207. [DOI] [PubMed] [Google Scholar]
- 152. Goudet P, Peschaud F, Mignon M, Nicoli-Sire P, Cadiot G, Ruszniewski P, Calender A, Murat A, Sarfati E, Peix JL, Kraimps JL, Henry JF, Cougard P, Proye C. Les gastrinomes dans les neoplasies endocriniennes multiples de type 1. Une etude de cohorte de 127 cas du groupe des tumeurs endocrines (GTE). Ann Chir. 2004; 129: 149– 155. [DOI] [PubMed] [Google Scholar]
- 153. Grama D, Eriksson B, Martensson H, Cedermark B, Ahren B, Kristoffersson A, Rastad J, Oberg K, Akerstrom G. Clinical characteristics, treatment and survival in patients with pancreatic tumors causing hormonal syndromes. World J Surg. 1992; 16: 632– 639. [DOI] [PubMed] [Google Scholar]
- 154. Grama D, Skogseid B, Wilander E, Eriksson B, Martensson H, Cedermark B, Ahren B, Kristofferson A, Oberg K, Rastad J. Pancreatic tumors in multiple endocrine neoplasia type 1: clinical presentation and surgical treatment. World J Surg. 1992; 16: 611– 618; discussion 618–9. [DOI] [PubMed] [Google Scholar]
- 155. Granberg D, Stridsberg M, Seensalu R, Eriksson B, Lundqvist G, Oberg K, Skogseid B. Plasma chromogranin A in patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1999; 84: 2712– 2717. [DOI] [PubMed] [Google Scholar]
- 156. Grimfjard P, Speel EJM, Stalberg P, Skogseid B. Clinics and genetics in MEN 1 related advanced thymic carcinoids—a triple case report including genome wide screening for genetic alterations. Eighth International Workshop on Multiple Endocrine Neoplasia Abstract Book. 2002;Abstract 15. [Google Scholar]
- 157. Griniatsos JE, Dimitriou N, Zilos A, Sakellariou S, Evangelou K, Kamakari S, Korkolopoulou P, Kaltsas G. Bilateral adrenocortical carcinoma in a patient with multiple endocrine neoplasia type 1 (MEN1) and a novel mutation in the MEN1 gene. World J Surg Oncol. 2011; 9: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Guida PM, Todd JE, Moore SW, Beal JM. Zollinger-Ellison syndrome with interesting variations. Am J Surg. 1966; 112: 807– 817. [DOI] [PubMed] [Google Scholar]
- 159. Gullo L, Migliori M, Falconi M, Pederzoli P, Bettini R, Casadei R, Delle Fave G, Corleto VD, Ceccarelli C, Santini D, Tomassetti P. Nonfunctioning pancreatic endocrine tumors: a multicenter clinical study. Am J Gastroenterol. 2003; 98: 2435– 2439. [DOI] [PubMed] [Google Scholar]
- 160. Gutierrez V, Cobo M, Olea D, Garcia J, Ramirez C, Bautista D, Alcalde J. Glucagonoma with two pancreatic masses and pulmonary metastases as debut of MEN-1. Clin Transl Oncol. 2007; 9: 674– 677. [DOI] [PubMed] [Google Scholar]
- 161. Haase M, Anlauf M, Schott M, Schinner S, Kaminsky E, Scherbaum WA, Willenberg HS. A new mutation in the menin gene causes the multiple endocrine neoplasia type 1 syndrome with adrenocortical carcinoma. Endocrine. 2011; 39: 153– 159. [DOI] [PubMed] [Google Scholar]
- 162. Habbe N, Waldmann J, Bartsch DK, Fendrich V, Rothmund M, Langer P. Multimodal treatment of sporadic and inherited neuroendocrine tumors of the thymus. Surgery. 2008; 144: 780– 785. [DOI] [PubMed] [Google Scholar]
- 163. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998; 339: 229– 234. [DOI] [PubMed] [Google Scholar]
- 164. Harring TR, Nguyen NT, Goss JA, O’Mahony CA. Treatment of liver metastases in patients with neuroendocrine tumors: a comprehensive review. Int J Hepatol. 2011; 2011: 154541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Hashimoto K, Suemaru S, Hattori T, Sugawara M, Ota Z, Takata S, Hamaya K, Doi K, Chretien M. Multiple endocrine neoplasia with Cushing’s syndrome due to paraganglioma producing corticotropin-releasing factor and adrenocorticotropin. Acta Endocrinol (Copenh). 1986; 113: 189– 195. [DOI] [PubMed] [Google Scholar]
- 166. Hausman MS, Jr, Thompson NW, Gauger PG, Doherty GM. The surgical management of MEN-1 pancreatoduodenal neuroendocrine disease. Surgery. 2004; 136: 1205– 1211. [DOI] [PubMed] [Google Scholar]
- 167. Hebb AL, Poulin JF, Roach SP, Zacharko RM, Drolet G. Cholecystokinin and endogenous opioid peptides: interactive influence on pain, cognition, and emotion. Prog Neuropsychopharmacol Biol Psychiatry. 2005; 29: 1225– 1238. [DOI] [PubMed] [Google Scholar]
- 168. Hellman P, Skogseid B, Juhlin C, Akerstrom G, Rastad J. Findings and long-term results of parathyroid surgery in multiple endocrine neoplasia type 1. World J Surg. 1992; 16: 718– 723. [DOI] [PubMed] [Google Scholar]
- 169. Hellman P, Skogseid B, Oberg K, Juhlin C, Akerstrom G, Rastad J. Primary and reoperative parathyroid operations in hyperparathyroidism of multiple endocrine neoplasia type 1. Surgery. 1998; 124: 993– 999. [PubMed] [Google Scholar]
- 170. Hessman O, Skogseid B, Westin G, Akerstrom G. Multiple allelic deletions and intratumoral genetic heterogeneity in MEN1 pancreatic tumors. J Clin Endocrinol Metab. 2001; 86: 1355– 1361. [DOI] [PubMed] [Google Scholar]
- 171. Hirschowitz BI, Simmons J, Mohnen J. Long-term lansoprazole control of gastric acid and pepsin secretion in ZE and non-ZE hypersecretors: a prospective 10-year study. Aliment Pharmacol Ther. 2001; 15: 1795– 1806. [DOI] [PubMed] [Google Scholar]
- 172. Hirschowitz BI, Simmons J, Mohnen J. Clinical outcome using lansoprazole in acid hypersecretors with and without Zollinger-Ellison syndrome: a 13-year prospective study. Clin Gastroenterol Hepatol. 2005; 3: 39– 48. [DOI] [PubMed] [Google Scholar]
- 173. Hochwald SN, Zee S, Conlon KC, Colleoni R, Louie O, Brennan MF, Klimstra DS. Prognostic factors in pancreatic endocrine neoplasms: an analysis of 136 cases with a proposal for low-grade and intermediate-grade groups. J Clin Oncol. 2002; 20: 2633– 2642. [DOI] [PubMed] [Google Scholar]
- 174. Hoffmann KM, Furukawa M, Jensen RT. Duodenal neuroendocrine tumors: Classification, functional syndromes, diagnosis and medical treatment. Best Pract Res Clin Gastroenterol. 2005; 19: 675– 697. [DOI] [PubMed] [Google Scholar]
- 175. Hoffmann KM, Gibril F, Entsuah LK, Serrano J, Jensen RT. Patients with multiple endocrine neoplasia type 1 with gastrinomas have an increased risk of severe esophageal disease including stricture and the premalignant condition, Barrett’s esophagus. J Clin Endocrinol Metab. 2006; 91: 204– 212. [DOI] [PubMed] [Google Scholar]
- 176. Hofmann M, Schilling T, Heilmann P, Haisken O, Wuster C, Brandi ML, Ziegler R, Nawroth PP. [Multiple endocrine neoplasia associated with multiple lipomas]. Med Klin. 1998; 93: 546– 549. [DOI] [PubMed] [Google Scholar]
- 177. Hosoda W, Takagi T, Mizuno N, Shimizu Y, Sano T, Yamao K, Yatabe Y. Diagnostic approach to pancreatic tumors with the specimens of endoscopic ultrasound-guided fine needle aspiration. Pathol Int. 2010; 60: 358– 364. [DOI] [PubMed] [Google Scholar]
- 178. Howard JM, Chremos AN, Collen MJ, McArthur KE, Cherner JA, Maton PN, Ciarleglio CA, Cornelius MJ, Gardner JD, Jensen RT. Famotidine, a new, potent, long-acting histamine H2-receptor antagonist: comparison with cimetidine and ranitidine in the treatment of Zollinger-Ellison syndrome. Gastroenterology. 1985; 88: 1026– 1033. [DOI] [PubMed] [Google Scholar]
- 179. Hubbard JG, Sebag F, Maweja S, Henry JF. Subtotal parathyroidectomy as an adequate treatment for primary hyperparathyroidism in multiple endocrine neoplasia type 1. Arch Surg. 2006; 141: 235– 239. [DOI] [PubMed] [Google Scholar]
- 180. Huizenga KA, Goodirck WIM, Summerskill WHJ. Peptic ulcer with islet cell tumor: a reappraisal. Am J Med. 1964; 37: 564– 577. [PubMed] [Google Scholar]
- 181. Imamura M, Komoto I, Ota S, Hiratsuka T, Kosugi S, Doi R, Awane M, Inoue N. Biochemically curative surgery for gastrinoma in multiple endocrine neoplasia type 1 patients. World J Gastroenterol. 2011; 17: 1343– 1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Isenberg JI, McQuaid KR, Laine L, Rubin W. Acid-peptic disorders. In: Yamada T, Alpers DH, Owyang C, Powell DW, Silverstein FE, eds. Textbook of Gastroenterology. Philadelphia: Lippincott; 1991: 1241– 1339. [Google Scholar]
- 183. Ishida E, Yamada M, Horiguchi K, Taguchi R, Ozawa A, Shibusawa N, Hashimoto K, Satoh T, Yoshida S, Tanaka Y, Yokota M, Tosaka M, Hirato J, Yamada S, Yoshimoto Y, Mori M. Attenuated expression of menin and p27 (Kip1) in an aggressive case of multiple endocrine neoplasia type 1 (MEN1) associated with an atypical prolactinoma and a malignant pancreatic endocrine tumor. Endocr J. 2011; 58: 287– 296. [DOI] [PubMed] [Google Scholar]
- 184. Jais P, Mignon M, Rehfeld JF. Processing-independent assay of serum gastrin for diagnosis of liver metastases in the Zollinger-Ellison syndrome. GRESZE (Groupe de Recherche et d’Etude du syndrome de Zollinger-Ellison). Int J Cancer. 1997; 71: 308– 309. [DOI] [PubMed] [Google Scholar]
- 185. Jansson JO, Svensson J, Bengtsson BA, Frohman LA, Ahlman H, Wangberg B, Nilsson O, Nilsson M. Acromegaly and Cushing’s syndrome due to ectopic production of GHRH and ACTH by a thymic carcinoid tumour: in vitro responses to GHRH and GHRP-6. Clin Endocrinol. 1998; 48: 243– 250. [DOI] [PubMed] [Google Scholar]
- 186. Jeddi A, Vasse N, Prunet D, Buzelin F, Bouchot O, Buzelin JM. [Wermer syndrome associated with a bilateral renal tumor]. Prog Urol. 1996; 6: 103– 106. [PubMed] [Google Scholar]
- 187. Jensen RT. Gastrinoma as a model for prolonged hypergastrinemia in man. In: Walsh JH, ed. Gastrin. New York: Raven Press; 1993: 373– 393. [Google Scholar]
- 188. Jensen RT. Peptide therapy. Recent advances in the use of somatostatin and other peptide receptor agonists and antagonists. In: Lewis JH, Dubois A, eds. Current Clinical Topics in Gastrointestinal Pharmacology. Malden, MA: Blackwell Science; 1997: 144– 223. [Google Scholar]
- 189. Jensen RT. Management of the Zollinger-Ellison syndrome in patients with multiple endocrine neoplasia type 1. J Intern Med. 1998; 243: 477– 488. [DOI] [PubMed] [Google Scholar]
- 190. Jensen RT. MEN-1 carcinoids: diagnosis and therapy. In: Seventh International Workshop on Multiple Neoplasia. Gubbio, Italy: 1999: 67– 72. [Google Scholar]
- 191. Jensen RT. Natural history of digestive endocrine tumors. In: Mignon M, Colombel JF, eds. Recent Advances in Pathophysiology and Management of Inflammatory Bowel Diseases and Digestive Endocrine Tumors. Paris: John Libbey Eurotext; 1999: 192– 219. [Google Scholar]
- 192. Jensen RT. Use of omeprazole and other proton pump inhibitors in the Zollinger-Ellison syndrome. In: Olbe L, ed. Milestones in Drug Therapy. Basel, Switzerland: Birkhauser Verlag; 1999: 205– 221. [Google Scholar]
- 193. Jensen RT. Zollinger-Ellison syndrome. In: Doherty GM, Skogseid B, eds. Surgical Endocrinology: Clinical Syndromes. Philadelphia: Lippincott Williams & Wilkins; 2001: 291– 344. [Google Scholar]
- 194. Jensen RT. Endocrine neoplasms of the pancreas. In: Yamada T, Alpers DH, Kalloo AN, Kaplowitz N, Owyang C, eds. Textbook of Gastroenterology. Oxford, England: Wiley-Blackwell; 2009: 1875– 1920. [Google Scholar]
- 195. Jensen RT, Berna MJ, Bingham MD, Norton JA. Inherited pancreatic endocrine tumor syndromes: advances in molecular pathogenesis, diagnosis, management and controversies. Cancer. 2008; 113 (7 suppl): 1807– 1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Jensen RT, Cadiot G, Brandi ML, de Herder WW, Kaltsas G, Komminoth P, Scoazec JY, Salazar R, Sauvanet A, Kianmanesh R. ENETS consensus guidelines for the management of patients with digestive neuroendocrine neoplasms: functional pancreatic endocrine tumor syndromes. Neuroendocrinology. 2012; 95: 98– 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Jensen RT, Collen MJ, McArthur KE, Howard JM, Maton PN, Cherner JA, Gardner JD. Comparison of the effectiveness of ranitidine and cimetidine in inhibiting acid secretion in patients with gastric acid hypersecretory states. Am J Med. 1984; 77 (5B): 90– 105. [PubMed] [Google Scholar]
- 198. Jensen RT, Delle Fave G. Promising advances in the treatment of malignant pancreatic endocrine tumors. N Engl J Med. 2011; 364: 564– 565. [DOI] [PubMed] [Google Scholar]
- 199. Jensen RT, Doppman JL, Gardner JD. Gastrinoma. In: Go VLW, Brooks FA, DiMagno EP, Gardner JD, Lebenthal E, Scheele GA, eds. The Exocrine Pancreas: Biology, Pathobiology and Disease. New York: Raven Press; 1986: 727– 744. [Google Scholar]
- 200. Jensen RT, Gardner JD. Gastrinoma. In: Go VLW, DiMagno EP, Gardner JD, Lebenthal E, Reber HA, Scheele GA, eds. The Pancreas: Biology, Pathobiology and Disease. New York: Raven Press; 1993: 931– 978. [Google Scholar]
- 201. Jensen RT, Niederle B, Mitry E, Ramage JK, Steinmuller T, Lewington V, Scarpa A, Sundin A, Perren A, Gross D, O’connor JM, Pauwels S, Kloppel G. Gastrinoma (duodenal and pancreatic). Neuroendocrinology. 2006; 84: 173– 182. [DOI] [PubMed] [Google Scholar]
- 202. Jiang XH, Lu JL, Cui B, Zhao YJ, Wang WQ, Liu JM, Fang WQ, Cao YN, Ge Y, Zhang CX, Casse H, Li XY, Ning G. MEN1 mutation analysis in Chinese patients with multiple endocrine neoplasia type 1. Endocr Relat Cancer. 2007; 14: 1073– 1079. [DOI] [PubMed] [Google Scholar]
- 203. Jordan PH., Jr A personal experience with pancreatic and duodenal neuroendocrine tumors. J Am Coll Surg. 1999; 189: 470– 482. [DOI] [PubMed] [Google Scholar]
- 204. Jose CC, Varghese CV, Singh AD. Thymic carcinoid in a case of Zollinger-Ellison syndrome. A case report. Australas Radiol. 1988; 32: 408– 409. [DOI] [PubMed] [Google Scholar]
- 205. Juodele L, Serapinas D, Sabaliauskas G, Krasauskiene A, Krasauskas V, Verkauskiene R, Barkauskiene D, Juozaityte E. Carcinoma of two parathyroid glands caused by a novel MEN1 gene mutation—a rare feature of the MEN 1 syndrome. Medicina (Kaunas). 2011; 47: 635– 639. [PubMed] [Google Scholar]
- 206. Kaczirek K, Prager G, Schindl M, Kaserer K, Gessl A, Vierhapper H, Niederle B. Multiple endocrine neoplasia 1—current recommendations for diagnosis and treatment. Wien Klin Wochenschr. 2002; 114: 258– 266. [PubMed] [Google Scholar]
- 207. Kaplan EL, Horvath K, Udekwu A, Straus F, Schark C, Ferguson DJ, Skinner DB. Gastrinomas: a 42-year experience. World J Surg. 1990; 14: 365– 375. [DOI] [PubMed] [Google Scholar]
- 208. Karges W, Schaaf L, Dralle H, Boehm BO. Concepts for screening and diagnostic follow-up in multiple endocrine neoplasia type 1 (MEN). Exp Clin Endocrinol Diabetes. 2000; 108: 334– 400. [DOI] [PubMed] [Google Scholar]
- 209. Kato H, Uchimura I, Morohoshi M, Fujisawa K, Kobayashi Y, Numano F, Goseki N, Endo M, Tamura A, Nagashima C. Multiple endocrine neoplasia type 1 associated with spinal ependymoma. Intern Med. 1996; 35: 285– 289. [DOI] [PubMed] [Google Scholar]
- 210. Kiernan TJ, O’Flynn AM, McDermott JH, Kearney P. Primary hyperparathyroidism and the cardiovascular system. Int J Cardiol. 2006; 113: E89– E92. [DOI] [PubMed] [Google Scholar]
- 211. Kivlen MH, Bartlett DL, Libutti SK, Skarulis MC, Marx SJ, Simonds WF, Weinstein LS, Jensen RT, McCart JA, Naik AM, Kranda KC, Brennan MF, Norton JA, Fraker DL, Alexander HR. Reoperation for hyperparathyroidism in multiple endocrine neoplasia type 1. Surgery. 2001; 130: 991– 998. [DOI] [PubMed] [Google Scholar]
- 212. Kloppel G, Willemar S, Stamm B, Hacki WH, Heitz PU. Pancreatic lesions and hormonal profile of pancreatic tumors in multiple endocrine neoplasia type I. An immunocytochemical study of nine patients. Cancer. 1986; 57: 1824– 1832. [DOI] [PubMed] [Google Scholar]
- 213. Kobayashi S, Okino T, Morikawa T, Hirakawa E, Yamadori I, Ohmori M, Takeda T, Tanaka S. [An autopsy case of MEN syndrome-type-1—unusual complication with gastric cancer]. Pathol Clin Med. 1988; 6: 703– 708. [Google Scholar]
- 214. Kojima Y, Ito H, Hasegawa S, Sasaki T, Inui K. Resected invasive thymoma with multiple endocrine neoplasia type 1. Jpn J Thorac Cardiovasc Surg. 2006; 54: 171– 173. [DOI] [PubMed] [Google Scholar]
- 215. Kopp I, Bartsch D, Wild A, Schilling T, Nies C, Bergenfelz A, Rieder H, Simon B, Rothmund M. Predictive genetic screening and clinical findings in multiple endocrine neoplasia type I families. World J Surg. 2001; 25: 610– 616. [DOI] [PubMed] [Google Scholar]
- 216. Kouides PA, Phatak PD, Cramer SF. Fatal thrombotic thrombocytopenic purpura (TTP) presenting concurrently with metastatic multiple endocrine neoplasia (MEN) type I. Hematopathol Mol Hematol. 1996; 10: 161– 170. [PubMed] [Google Scholar]
- 217. Kouvaraki MA, Shapiro SE, Cote GJ, Lee JE, Yao JC, Waguespack SG, Gagel RF, Evans DB, Perrier ND. Management of pancreatic endocrine tumors in multiple endocrine neoplasia type 1. World J Surg. 2006; 30: 643– 653. [DOI] [PubMed] [Google Scholar]
- 218. Kraimps JL, Duh Q-Y, Demeure M, Clark OH. Hyperparathyroidism in multiple endocrine neoplasia syndrome. Surgery. 1992; 112: 1080– 1086. [PubMed] [Google Scholar]
- 219. Krampitz GW, Norton JA, Poultsides GA, Visser B, Sun L, Jensen RT. Lymph nodes and survival in pancreatic neuroendocrine tumors. Arch Surg. 2012; 147: 820– 827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Krudy AG, Doppman JL, Jensen RT, Norton JA, Collen MJ, Shawker TH, Gardner JD, McArthur KK, Gorden P. Localization of islet cell tumors by dynamic CT: comparison with plain CT, arteriography, sonography and venous sampling. Am J Roentgenol. 1984; 143: 585– 589. [DOI] [PubMed] [Google Scholar]
- 221. Kulke MH, Anthony LB, Bushnell DL, de Herder WW, Goldsmith SJ, Klimstra DS, Marx SJ, Pasieka JL, Pommier RF, Yao JC, Jensen RT. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010; 39: 735– 752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Labauge R, Pages A, Pages M, Ribstein J, Richard JL. [Haemorrhagic necrosis of a pituitary adenoma in a case of multiple endocrine neoplasia (author’s transl)]. Rev Neurol (Paris). 1982; 138: 149– 158. [PubMed] [Google Scholar]
- 223. Lairmore TC, Wells SA., Jr Cancer of the endocrine system. In: DeVita VT, Jr, Hellman S, Rosenberg SA, eds. Cancer: Principles & Practice of Oncology. Philadelphia: Lippincott-Raven; 1997: 1617– 1628. [Google Scholar]
- 224. Lamers CB. Familial multiple endocrine neoplasia type I (Wermer’s syndrome). Neth J Med. 1978; 21: 270– 274. [PubMed] [Google Scholar]
- 225. Lamers CB, Berretty PJ, Bijvoet OL, Joosten HJ, Lubbers EJ, Muller H, Nadorp JH, Nielander DO, Penn W, Prenen H, Schillings PH, Termote UA, Van Tongeren JH. The Zollinger-Ellison syndrome. Neth J Med. 1974; 17: 94– 107. [PubMed] [Google Scholar]
- 226. Lamers CB, Stadil F, Van Tongeren JH. Prevalence of endocrine abnormalities in patients with the Zollinger-Ellison syndrome and in their families. Am J Med. 1978; 64: 607– 612. [DOI] [PubMed] [Google Scholar]
- 227. Lamers CBHW, Lind T, Moberg S, Jansen JBMJ, Olbe L. Omeprazole in Zollinger-Ellison syndrome: effects of a single dose and of long term treatment in patients resistant to histamine H2-receptor antagonists. N Engl J Med. 1984; 310: 758– 761. [DOI] [PubMed] [Google Scholar]
- 228. Langer P, Cupisti K, Bartsch DK, Nies C, Goretzki PE, Rothmund M, Roher HD. Adrenal involvement in multiple endocrine neoplasia type 1. World J Surg. 2002; 26: 891– 896. [DOI] [PubMed] [Google Scholar]
- 229. Larkin CJ, Joy ES, Ardill JE, Johnston CF, Collins JS, Buchanan KD. Gastrinomas and the change in their presentation and management in Northern Ireland, UK, from 1970 to 1996. Eur J Gastroenterol Hepatol. 1998; 10: 947– 952. [DOI] [PubMed] [Google Scholar]
- 230. LeBodic MF, Heymann MF, Lecomte M, Berger N, Berger F, Louvel A, DeMicco C, Patey M, deMascarel A, Burtin F, Saint-Andre JP. Immunohistochemical study of 100 pancreatic tumors in 28 patients with multiple endocrine neoplasia, type 1. Am J Surg Pathol. 1996; 20: 1378– 1384. [DOI] [PubMed] [Google Scholar]
- 231. Lebtahi R, Cadiot G, Delahaye N, Genin R, Daou D, Peker MC, Chosidow D, Faraggi M, Mignon M, LeGuludec D. Detection of bone metastases in patients with endocrine gastroenteropancreatic tumors: bone scintigraphy compared with somatostatin receptor scintigraphy. J Nucl Med. 1999; 40: 1602– 1608. [PubMed] [Google Scholar]
- 232. Lehy T, Cadiot G, Mignon M, Ruszniewski P, Bonfils S. Influence of multiple endocrine neoplasia type 1 on gastric endocrine cells in patients with the Zollinger-Ellison syndrome. Gut. 1992; 33: 1275– 1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Levy-Bohbot N, Merle C, Goudet P, Delemer B, Calender A, Jolly D, Thiefin G, Cadiot G. Prevalence, characteristics and prognosis of MEN 1-associated glucagonomas, VIPomas, and somatostatinomas: study from the GTE (Groupe des Tumeurs Endocrines) registry. Gastroenterol Clin Biol. 2004; 28: 1075– 1081. [DOI] [PubMed] [Google Scholar]
- 234. Libe R, Chanson P. [Endocrine tumors of the pancreas (EPTs) in multiple endocrine neoplasia (MEN1): up-date on prognostic factors, diagnostic procedures and treatment]. Ann Endocrinol (Paris). 2007; 68 (Suppl 1): 1– 8. [DOI] [PubMed] [Google Scholar]
- 235. Lim L-C, Teh B-T, Rajasoorya RC. Familial MEN1—revisiting traditional dogma—unusual presentations in the first Singapore family with a novel genetic mutation. Eighth International Workshop on Multiple Endocrine Neoplasia Abstract Book. 2002; Abstract 20. [Google Scholar]
- 236. Lin FC, Lin CM, Hsieh CC, Li WY, Wang LS. Atypical thymic carcinoid and malignant somatostatinoma in type I multiple endocrine neoplasia syndrome: case report. Am J Clin Oncol. 2003; 26: 270– 272. [DOI] [PubMed] [Google Scholar]
- 237. Lin X, Saad RS, Luckasevic TM, Silverman JF, Liu Y. Diagnostic value of CDX-2 and TTF-1 expressions in separating metastatic neuroendocrine neoplasms of unknown origin. Appl Immunohistochem Mol Morphol. 2007; 15: 407– 414. [DOI] [PubMed] [Google Scholar]
- 238. Lind T, Olbe L. Long term follow up of patients with Zollinger-Ellison syndrome (ZES). Acta Chir Scand. 1989; 155: 383– 388. [PubMed] [Google Scholar]
- 239. Lips CJ, Vasen HF, Lamers CB. Multiple endocrine neoplasia syndromes. Crit Rev Oncol Hematol. 1984; 2: 117– 184. [DOI] [PubMed] [Google Scholar]
- 240. Liu DH, Crastnopol P, Phillips W. Perforation of a gastrojejunal ulcer into the pericardium. Arch Surg. 1967; 94: 294– 298. [DOI] [PubMed] [Google Scholar]
- 241. Lo CY, Chan FL, Tam SC, Cheng PW, Fan ST, Lam KS. Value of intra-arterial calcium stimulated venous sampling for regionalization of pancreatic insulinomas. Surgery. 2000; 128: 903– 909. [DOI] [PubMed] [Google Scholar]
- 242. London JF, Shawker TH, Doppman JL, Frucht HH, Vinayek R, Stark HA, Miller LS, Miller DL, Norton JA, Gardner JD, Jensen RT. Zollinger-Ellison syndrome: prospective assessment of abdominal US in the localization of gastrinomas. Radiology. 1991; 178: 763– 767. [DOI] [PubMed] [Google Scholar]
- 243. Long KB, Srivastava A, Hirsch MS, Hornick JL. PAX8 Expression in well-differentiated pancreatic endocrine tumors: correlation with clinicopathologic features and comparison with gastrointestinal and pulmonary carcinoid tumors. Am J Surg Pathol. 2010; 34: 723– 729. [DOI] [PubMed] [Google Scholar]
- 244. Lopez CL, Waldmann J, Fendrich V, Langer P, Kann PH, Bartsch DK. Long-term results of surgery for pancreatic neuroendocrine neoplasms in patients with MEN1. Langenbecks Arch Surg. 2011; 396: 1187– 1197. [DOI] [PubMed] [Google Scholar]
- 245. Lourenco DM, Jr, Coutinho FL, Toledo RA, Montenegro FL, Correia-Deur JE, Toledo SP. Early-onset, progressive, frequent, extensive, and severe bone mineral and renal complications in multiple endocrine neoplasia type 1-associated primary hyperparathyroidism. J Bone Miner Res. 2010; 25: 2382– 2391. [DOI] [PubMed] [Google Scholar]
- 246. Lourenco DM, Jr, Toledo RA, Coutinho FL, Margarido LC, Siqueira SA, dos Santos MA, Montenegro FL, Machado MC, Toledo SP. The impact of clinical and genetic screenings on the management of the multiple endocrine neoplasia type 1. Clinics (Sao Paulo). 2007; 62: 465– 476. [PubMed] [Google Scholar]
- 247. Lowney JK, Frisella MM, Lairmore TC, Doherty GM. Pancreatic islet cell tumor metastasis in multiple endocrine neoplasia type 1: correlation with primary tumor size. Surgery. 1999; 125: 1043– 1049. [DOI] [PubMed] [Google Scholar]
- 248. Lubensky IA, Debelenko LV, Zhuang Z, Emmert-Buck MR, Dong Q, Chandrasekharappa S, Guru SC, Manickam P, Olufemi SE, Marx SJ, Spiegel AM, Collins FS, Liotta LA. Allelic deletions on chromosome 11q13 in multiple tumors from individual MEN1 patients. Cancer Res. 1996; 56: 5272– 5278. [PubMed] [Google Scholar]
- 249. Lucey MR, McCann S, Weir DG. A family with multiple endocrine neoplasia type 1. Ir J Med Sci. 1983; 152: 99– 102. [DOI] [PubMed] [Google Scholar]
- 250. MacFarlane MP, Fraker DL, Alexander HR, Norton JA, Jensen RT. A prospective study of surgical resection of duodenal and pancreatic gastrinomas in multiple endocrine neoplasia-type 1. Surgery. 1995; 118: 973– 980. [DOI] [PubMed] [Google Scholar]
- 251. Machens A, Schaaf L, Karges W, Frank-Raue K, Bartsch DK, Rothmund M, Schneyer U, Goretzki P, Raue F, Dralle H. Age-related penetrance of endocrine tumours in multiple endocrine neoplasia type 1 (MEN1): a multicentre study of 258 gene carriers. Clin Endocrinol (Oxf). 2007; 67: 613– 622. [DOI] [PubMed] [Google Scholar]
- 252. Madeira I, Terris B, Voss M, Denys A, Sauvanet A, Flejou JF, Vilgrain V, Belghiti J, Bernades P, Ruszniewski P. Prognostic factors in patients with endocrine tumours of the duodenopancreatic area. Gut. 1998; 43: 422– 427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Maithel SK, Fong Y. Hepatic ablation for neuroendocrine tumor metastases. J Surg Oncol. 2009; 100: 635– 638. [DOI] [PubMed] [Google Scholar]
- 254. Majewski JT, Wilson SD. The MEN-I syndrome: an all or none phenomenon? Surgery. 1979; 86: 475– 484. [PubMed] [Google Scholar]
- 255. Malagelada JR, Edis AJ, Adson MA, Van Heerden JA, Go VLW. Medical and surgical options in the management of patients with gastrinoma. Gastroenterology. 1983; 84: 1524– 1532. [PubMed] [Google Scholar]
- 256. Mallek R, Mostbeck G, Walter RM, Herold CH, Imhof H, Tscholakoff D. Contrast MRI in multiple endocrine neoplasia type 1 (MEN) associated with renal cell carcinoma. Eur J Radiol. 1990; 10: 105– 108. [DOI] [PubMed] [Google Scholar]
- 257. Malmaeus J, Benson L, Johansson H, Ljunghall S, Rastad J, Akerstrom G, Oberg K. Parathyroid surgery in the multiple endocrine neoplasia type I syndrome: choice of surgical procedure. World J Surg. 1986; 10: 668– 672. [DOI] [PubMed] [Google Scholar]
- 258. Mao C, El Attar A, Domenico DR, Kim K, Howard JM. Carcinoid tumors of the pancreas. Int J Pancreatol. 1998; 23: 153– 164. [DOI] [PubMed] [Google Scholar]
- 259. Marini C, Giusti M, Armonino R, Ghigliotti G, Bezante G, Vera L, Morbelli S, Pomposelli E, Massollo M, Gandolfo P, Minuto F, Sambuceti G. Reduced coronary flow reserve in patients with primary hyperparathyroidism: a study by G-SPECT myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2010; 37: 2256– 2263. [DOI] [PubMed] [Google Scholar]
- 260. Markowitz AM, Slanetz CA, Jr, Franz VK. Functioning islet cell tumors of the pancreas: 25-year follow up. Ann Surg. 1961; 154: 877– 884. [PMC free article] [PubMed] [Google Scholar]
- 261. Marx S, Spiegel AM, Skarulis MC, Doppman JL, Collins FS, Liotta LA. Multiple endocrine neoplasia type 1: clinical and genetic topics. Ann Intern Med. 1998; 129: 484– 494. [DOI] [PubMed] [Google Scholar]
- 262. Marx SJ, Agarwal SK, Kester MB, Heppner C, Kim YS, Skarulis MC, Goldsmith PK, Saggar SK, Park SY, Spiegel AM, Burns AL, Debelenko LV, Zhuang Z, Lubensky IA, Liotta LA, Emmert-Buck MR, Guru SC, Manickam P, Crabtree J, Erdos MR, Collins FS, Chandrasekharappa SC. Multiple endocrine neoplasia type 1: clinical and genetic features of the hereditary endocrine neoplasias. Recent Prog Horm Res. 1999; 54: 397– 439. [PubMed] [Google Scholar]
- 263. Marx SJ, Sakaguchi K, Green J, III, Aurbach GD, Brandi ML. Mitogenic activity on parathyroid cells in plasma from members of a large kindred with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1988; 67: 149– 153. [DOI] [PubMed] [Google Scholar]
- 264. Marx SJ, Vinik AI, Santen RJ, Floyd JC, Jr, Mills JL, Green J. Multiple endocrine neoplasia type I: assessment of laboratory tests to screen for the gene in a large kindred. Medicine (Baltimore). 1986; 65: 226– 241. [PubMed] [Google Scholar]
- 265. Mathis P, Segal S, Beer Gabel M, Diebold MD, Hochlaf S. [Familial forms of endocrine tumors of the pancreas. A propos of 4 cases in the same family]. Chirurgie. 1989; 115: 461– 465. [PubMed] [Google Scholar]
- 266. Maton PN, Frucht H, Vinayek R, Wank SA, Gardner JD, Jensen RT. Medical management of patients with Zollinger-Ellison syndrome who have had previous gastric surgery: a prospective study. Gastroenterology. 1988; 94: 294– 299. [DOI] [PubMed] [Google Scholar]
- 267. Maton PN, Gardner JD, Jensen RT. Cushing’s syndrome in patients with Zollinger-Ellison syndrome. N Engl J Med. 1986; 315: 1– 5. [DOI] [PubMed] [Google Scholar]
- 268. Maton PN, Lack EE, Collen MJ, Cornelius MJ, David E, Gardner JD, Jensen RT. The effect of Zollinger-Ellison syndrome and omeprazole therapy on gastric oxyntic endocrine cells. Gastroenterology. 1990; 99: 943– 950. [DOI] [PubMed] [Google Scholar]
- 269. Maton PN, Miller DL, Doppman JL, Collen MJ, Norton JA, Vinayek R, Slaff JI, Wank SA, Gardner JD, Jensen RT. Role of selective angiography in the management of Zollinger-Ellison syndrome. Gastroenterology. 1987; 92: 913– 918. [DOI] [PubMed] [Google Scholar]
- 270. Maton PN, Vinayek R, Frucht H, McArthur KA, Miller LS, Saeed ZA, Gardner JD, Jensen RT. Long-term efficacy and safety of omeprazole in patients with Zollinger-Ellison syndrome: a prospective study. Gastroenterology. 1989; 97: 827– 836. [DOI] [PubMed] [Google Scholar]
- 271. McCallum RW, Parameswaran V, Burgess JR. Multiple endocrine neoplasia type 1 (MEN 1) is associated with an increased prevalence of diabetes mellitus and impaired fasting glucose. Clin Endocrinol (Oxf). 2006; 65: 163– 168. [DOI] [PubMed] [Google Scholar]
- 272. McCarthy DM. Report on the United States experience with cimetidine in Zollinger-Ellison syndrome and other hypersecretory states. Gastroenterology. 1978; 74: 453– 458. [PubMed] [Google Scholar]
- 273. McCarthy DM, Peikin SR, Lopatin RN, Long BW, Spiegel A, Marx S, Brennan A. Hyperparathyroidism a reversible cause of cimetidine-resistant gastric hypersecretion. Br Med J. 1979; 1: 1765– 1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. McKeeby JL, Li X, Zhuang Z, Vortmeyer AO, Huang S, Pirner M, Skarulis MC, James-Newton L, Marx SJ, Lubensky IA. Multiple leiomyomas of the esophagus, lung, and uterus in multiple endocrine neoplasia type 1. Am J Pathol. 2001; 159: 1121– 1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275. Mee AS, Ismail S, Bornman PC, Marks IN. Changing concepts in the presentation, diagnosis and management of the Zollinger-Ellison syndrome. Q J Med. 1983; 52: 256– 267. [PubMed] [Google Scholar]
- 276. Melvin WS, Johnson JA, Sparks J, Innes JT, Ellison EC. Long-term prognosis of Zollinger-Ellison syndrome in multiple endocrine neoplasia. Surgery. 1993; 114: 1183– 1188. [PubMed] [Google Scholar]
- 277. Metz DC, Forsmark C, Lew EA, Starr JA, Soffer EF, Bochenek W, Pisegna JR. Replacement of oral proton pump inhibitors with intravenous pantoprazole to effectively control gastric acid hypersecretion in patients with Zollinger-Ellison syndrome. Am J Gastroenterol. 2001; 96: 3274– 3280. [DOI] [PubMed] [Google Scholar]
- 278. Metz DC, Jensen RT. Advances in gastric antisecretory therapy in Zollinger-Ellison syndrome. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Series: Frontiers of Gastrointestinal Research. Basel, Switzerland: S. Karger; 1995: 240– 257. [Google Scholar]
- 279. Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008; 135: 1469– 1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Metz DC, Jensen RT, Bale AE, Skarulis MC, Eastman RC, Nieman L, Norton JA, Friedman E, Larrson C, Amorosi A, Brandi ML, Marx SJ. Multiple endocrine neoplasia type 1: clinical features and management. In: Bilezekian JP, Levine MA, Marcus R, eds. The Parathyroids. New York: Raven Press; 1994: 591– 646. [Google Scholar]
- 281. Metz DC, Pisegna JR, Fishbeyn VA, Benya RV, Feigenbaum KM, Koviack PD, Jensen RT. Currently used doses of omeprazole in Zollinger-Ellison syndrome are too high. Gastroenterology. 1992; 103: 1498– 1508. [DOI] [PubMed] [Google Scholar]
- 282. Metz DC, Pisegna JR, Fishbeyn VA, Benya RV, Jensen RT. Control of gastric acid hypersecretion in the management of patients with Zollinger-Ellison syndrome. World J Surg. 1993; 17: 468– 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Metz DC, Pisegna JR, Ringham GL, Feigenbaum KM, Koviack PD, Maton PN, Gardner JD, Jensen RT. Prospective study of efficacy and safety of lansoprazole in Zollinger-Ellison syndrome. Dig Dis Sci. 1993; 38: 245– 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Metz DC, Strader DB, Orbuch M, Koviack PD, Feigenbaum KM, Jensen RT. Use of omeprazole in Zollinger-Ellison: a prospective nine-year study of efficacy and safety. Aliment Pharmacol Ther. 1993; 7: 597– 610. [DOI] [PubMed] [Google Scholar]
- 285. Mieher WC, Hartsock RJ, Geokas MC, Ballard HS, Frame B. Peptic ulcer as a manifestation of familial polyendocrine disease. JAMA. 1962; 179: 854– 858. [DOI] [PubMed] [Google Scholar]
- 286. Mignon M. Natural history of neuroendocrine enteropancreatic tumors. Digestion. 2000; 62: 51– 58. [DOI] [PubMed] [Google Scholar]
- 287. Mignon M, Cadiot G. Diagnostic and therapeutic criteria in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1. J Intern Med. 1998; 243: 489– 494. [DOI] [PubMed] [Google Scholar]
- 288. Mignon M, Cadiot G. Natural history of gastrinoma: lessons from the past. Ital J Gastroenterol Hepatol. 1999; 31: S98– S103. [PubMed] [Google Scholar]
- 289. Mignon M, Cadiot G, Rigaud D, Ruszniewski Ph, Jais P, Lehy T, Lewin MJM. Management of islet cell tumors in patients with multiple endocrine neoplasia type 1. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Series: Frontiers of Gastrointestinal Research. Basel, Switzerland: S. Karger; 1995: 342– 359. [Google Scholar]
- 290. Mignon M, Jais P, Cadiot G, Yedder D, Vatier J. Clinical features and advances in biological diagnostic criteria for Zollinger-Ellison syndrome. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Series: Frontiers of Gastrointestinal Research. Basel, Switzerland: S. Karger; 1995: 223– 239. [Google Scholar]
- 291. Mignon M, Ruszniewski P, Haffar S, Rignaud D, Rene E, Bonfils S. Current approach to the management of tumoral process in patients with gastrinoma. World J Surg. 1986; 10: 703– 710. [DOI] [PubMed] [Google Scholar]
- 292. Miller CA, Melvin WS, Schirmer WJ, O’Dorisio TS, Johnson J, Sparks J, Ellison EC. Preoperative serum gastrin level as a prognostic indicator in Zollinger-Ellison syndrome. Gastroenterology. 1996; 110: A417. [Google Scholar]
- 293. Miller DL, Doppman JL, Metz DC, Maton PN, Norton JA, Jensen RT. Zollinger-Ellison syndrome: technique, results and complications of portal venous sampling. Radiology. 1992; 182: 235– 241. [DOI] [PubMed] [Google Scholar]
- 294. Miller LS, Doppman J, Maton PN, Gardner JD, Jensen RT. Zollinger-Ellison syndrome. Advances in diagnosis and treatment. Handbk Exp Pharmacol. 1991; 99: 349– 400. [Google Scholar]
- 295. Miller LS, Vinayek R, Frucht H, Gardner JD, Jensen RT, Maton PN. Reflux esophagitis in patients with Zollinger-Ellison syndrome. Gastroenterology. 1990; 98: 341– 346. [DOI] [PubMed] [Google Scholar]
- 296. Mino K, Karasaki K, Bando K, Toi H, Goto J, Kawai T, Yasuhara M, Akahane Y, Nakano S, Takahashi M. [Clinical analysis of resected cases of pancreatic endocrine tumors]. Hokkaido J Surg. 2004; 49: 69. [Google Scholar]
- 297. Miyauchi A, Sato M, Matsubara S, Ohye H, Kihara M, Matsusaka K, Nishitani A, Takahara J. A family of MEN1 with a novel germline missense mutation and benign polymorphisms. Endocr J. 1998; 45: 753– 759. [DOI] [PubMed] [Google Scholar]
- 298. Modlin IM, Lamers CBH. Multiple endocrine neoplasia. Part I. Wermer’s syndrome. S Afr Med J. 1979; 56: 485– 488. [PubMed] [Google Scholar]
- 299. Moertel CG, May GR, Martin JK. Sequential heptic artery occlusion and chemotherapy for metastatic islet carcinoid tumor and islet cell carcinoma. Proc Am Soc Clin Oncol. 1985; 4: 80. [Google Scholar]
- 300. Moldawer M. Multiple endocrine tumors and Zollinger-Ellison syndrome in families: one or two syndromes? A report of two new families. Metabolism. 1962; 11: 153– 166. [PubMed] [Google Scholar]
- 301. Moldawer MP, Nardi GL, Raker JW. Concomitance of multiple adenomas of the parathyroids and pancreatic islet cells with tumor of the pituitary; a syndrome with familial incidence. Am J Med Sci. 1954; 228: 190– 206. [DOI] [PubMed] [Google Scholar]
- 302. Morelli A, Falchetti A, Weinstein L, Fabiani S, Tomassetti P, Enzi G, Carraro R, Bordi C, Tonelli F, Brandi ML. RFLP analysis of human chromosome 11 region q13 in multiple symmetric lipomatosis and multiple endocrine neoplasia type 1-associated lipomas. Biochem Biophys Res Commun. 1995; 207: 363– 368. [DOI] [PubMed] [Google Scholar]
- 303. Mortellaro VE, Hochwald SN, McGuigan JE, Copeland EM, Vogel SB, Grobmyer SR. Long-term results of a selective surgical approach to management of Zollinger-Ellison syndrome in patients with MEN-1. Am Surg. 2009; 75: 730– 733. [PubMed] [Google Scholar]
- 304. Murakami S, Satomi A, Ishida K, Matsuki M, Koda H, Miura S. Multiple endocrine neoplasia type 1 presenting as insulinoma, gastrinoma, and postubulbar duodenal ulcers: report of a case. Surg Today. 1995; 25: 848– 851. [DOI] [PubMed] [Google Scholar]
- 305. Murat A, Heymann MF, Bernat S, Dupas B, Delajartre AY, Calender A, Despins P, Michaud JL, Giraud S, LeBodic MF, Charbonnel B. [Thymic and bronchial neuroendocrine tumors in multiple endocrine neoplasia type 1. GENEM1]. Presse Med. 1997; 26: 1616– 1621. [PubMed] [Google Scholar]
- 306. Murie N, Chauvel P, Faire J, Croisier JC, Martin E, Moreaux J, Sabouraud O. Wermer’s syndrome or familial polyendocrine adenomatous hyperplasia (2 anatomo-clinical cases). Ann Endocrinol (Paris). 1973; 34: 190– 205. [PubMed] [Google Scholar]
- 307. Murphy RT, Goodsitt E, Morales H, Bilton JL. Peptic ulceration with associated endocrine tumors. Am J Surg. 1960; 100: 764– 778. [DOI] [PubMed] [Google Scholar]
- 308. Namihira Y, Achord JL, Subramony C. Multiple endocrine neoplasia, type 1, with pancreatic cholera. Am J Gastroenterol. 1987; 82: 794– 797. [PubMed] [Google Scholar]
- 309. Newey PJ, Jeyabalan J, Walls GV, Christie PT, Gleeson FV, Gould S, Johnson PR, Phillips RR, Ryan FJ, Shine B, Bowl MR, Thakker RV. Asymptomatic children with multiple endocrine neoplasia type 1 mutations may harbor nonfunctioning pancreatic neuroendocrine tumors. J Clin Endocrinol Metab. 2009; 94: 3640– 3646. [DOI] [PubMed] [Google Scholar]
- 310. Nieto JM, Pisegna JR. The role of proton pump inhibitors in the treatment of Zollinger-Ellison syndrome. Expert Opin Pharmacother. 2006; 7: 169– 175. [DOI] [PubMed] [Google Scholar]
- 311. Nikou GC, Toubanakis C, Nikolaou P, Giannatou E, Marinou K, Safioleas M, Karamanolis D. Gastrinomas associated with MEN-1 syndrome: new insights for the diagnosis and management in a series of 11 patients. Hepatogastroenterology. 2005; 52: 1668– 1676. [PubMed] [Google Scholar]
- 312. Nishimura Y, Yamashita K, Yumita W, Yamazaki M, Katai M, Sakurai A, Hashizume K. Multiple endocrine neoplasia type 1 with unusual concomitance of various neoplastic disorders. Endocr J. 2004; 51: 75– 81. [DOI] [PubMed] [Google Scholar]
- 313. Nord B, Platz A, Smoczynski K, Kytola S, Robertson G, Calender A, Murat A, Weintraub D, Burgess J, Edwards M, Skogseid B, Owen D, Lassam N, Hogg D, Larsson C, Teh BT. Malignant melanoma in patients with multiple endocrine neoplasia type 1 and involvement of the MEN1 gene in sporadic melanoma. Int J Cancer. 2000; 87: 463– 467. [DOI] [PubMed] [Google Scholar]
- 314. Norton JA, Alexander HA, Fraker DL, Venzon DJ, Gibril F, Jensen RT. Possible primary lymph node gastrinomas: occurrence, natural history and predictive factors: a prospective study. Ann Surg. 2003; 237: 650– 659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315. Norton JA, Alexander HR, Fraker DL, Venzon DJ, Gibril F, Jensen RT. Comparison of surgical results in patients with advanced and limited disease with multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome. Ann Surg. 2001; 234: 495– 506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Norton JA, Alexander HR, Fraker DL, Venzon DJ, Jensen RT. Does the use of routine duodenotomy (DUODX) affect rate of cure, development of liver metastases or survival in patients with Zollinger-Ellison syndrome (ZES)? Ann Surg. 2004; 239: 617– 626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317. Norton JA, Cornelius MJ, Doppman JL, Maton PN, Gardner JD, Jensen RT. Effect of parathyroidectomy in patients with hyperparathyroidism, Zollinger-Ellison syndrome and multiple endocrine neoplasia Type I: a prospective study. Surgery. 1987; 102: 958– 966. [PubMed] [Google Scholar]
- 318. Norton JA, Cromack DT, Shawker TH, Doppman JL, Comi R, Gorden P, Maton PN, Gardner JD, Jensen RT. Intraoperative ultrasonographic localization of islet cell tumors. A prospective comparison to palpation. Ann Surg. 1988; 207: 160– 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319. Norton JA, Fang TD, Jensen RT. Surgery for gastrinoma and insulinoma in multiple endocrine neoplasia type 1. J Natl Compr Cancer. 2006; 4: 148– 153. [DOI] [PubMed] [Google Scholar]
- 320. Norton JA, Fraker DL, Alexander HR, Gibril F, Liewehr DJ, Venzon DJ, Jensen RT. Surgery increases survival in patients with gastrinoma. Ann Surg. 2006; 244: 410– 419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Norton JA, Fraker DL, Alexander HR, Venzon DJ, Doppman JL, Serrano J, Goebel SU, Peghini P, Roy PK, Gibril F, Jensen RT. Surgery to cure the Zollinger-Ellison syndrome. N Engl J Med. 1999; 341: 635– 644. [DOI] [PubMed] [Google Scholar]
- 322. Norton JA, Jensen RT. Unresolved surgical issues in the management of patients with the Zollinger-Ellison syndrome. World J Surg. 1991; 15: 151– 159. [DOI] [PubMed] [Google Scholar]
- 323. Norton JA, Jensen RT. Current surgical management of Zollinger-Ellison syndrome (ZES) in patients without multiple endocrine neoplasia-type 1 (MEN1). Surg Oncol. 2003; 12: 145– 151. [DOI] [PubMed] [Google Scholar]
- 324. Norton JA, Jensen RT. Resolved and unresolved controversies in the surgical management of patients with Zollinger-Ellison syndrome. Ann Surg. 2004; 240: 757– 773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. Norton JA, Kirlen MA, Li M, Schreiber D, Chuter T, Jensen RT. Morbidity and mortality of aggressive resections in patients with advanced neuroendocrine tumors. Arch Surg. 2003; 138: 859– 866. [DOI] [PubMed] [Google Scholar]
- 326. Norton JA, Melcher ML, Gibril F, Jensen RT. Gastric carcinoid tumors in multiple endocrine neoplasia-1 patients with Zollinger-Ellison syndrome can be symptomatic, demonstrate aggressive growth, and require surgery. Surgery. 2004; 136: 1267– 1274. [DOI] [PubMed] [Google Scholar]
- 327. Norton JA, Sugarbaker PH, Doppman JL, Wesley RA, Maton PN, Gardner JD, Jensen RT. Aggressive resection of metastatic disease in selected patients with malignant gastrinoma. Ann Surg. 1986; 203: 352– 359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328. Norton JA, Venzon DJ, Berna MJ, Alexander HR, Fraker DL, Libutti SK, Marx SJ, Gibril F, Jensen RT. Prospective study of surgery for primary hyperaparathyroidism (HPT) in multiple endocrine neoplasia type 1 (MEN1), and Zollinger-Ellison syndrome (ZES): longterm outcome of a more virulent form of HPT. Ann Surgery. 2008; 247: 501– 510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Norton JA, Warren RS, Kelly MG, Zurek MB, Jensen RT. Aggressive surgery for metastatic liver neuroendocrine tumors. Surgery. 2003; 134: 1057– 1065. [DOI] [PubMed] [Google Scholar]
- 330. O’Riordain DS, O’Brien T, Van Heerden JA, Service FJ, Grant CS. Surgical management of insulinoma associated with multiple endocrine neoplasia type 1. World J Surg. 1994; 18: 488– 493. [DOI] [PubMed] [Google Scholar]
- 331. Oberg K. Neuroendocrine tumors (NETs): historical overview and epidemiology. Tumori. 2010; 96: 797– 801. [DOI] [PubMed] [Google Scholar]
- 332. Oberg K, Walinder O, Bostrom H, Lundqvist G, Wide L. Peptide hormone markers in screening for endocrine tumors in multiple endocrine adenomatosis type I. Am J Med. 1982; 73: 619– 630. [DOI] [PubMed] [Google Scholar]
- 333. OByrne KJ, Goggins MG, McDonald GS, Daly PA, Kelleher DP, Weir DG. A metastatic neuroendocrine anaplastic small cell tumor in a patient with multiple endocrine neoplasia type 1 syndrome. Cancer. 1994; 74: 2374– 2378. [DOI] [PubMed] [Google Scholar]
- 334. Ogino H, Mokuda O, Ubukata E, Sakamoto Y, Toriumi M, Tanaka KKT, Sugano I, Ishida Y, Nagao K, Shimizu N. [A case of malignant insulinoma assocated with multiple endocrine neoplasia type 1 in a patient whose blood glucose has been well managed with diazoxide and octreotide]. J Japan Diabetes Soc. 1988; 41: 915– 921. [Google Scholar]
- 335. Orbuch M, Doppman JL, Strader DB, Fishbeyn VA, Benya RV, Metz DC, Jensen RT. Imaging for pancreatic endocrine tumor localization: recent advances. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Series: Frontiers of Gastrointestinal Research. Basel, Switzerland: S. Karger; 1995: 268– 281. [Google Scholar]
- 336. Pack S, Turner ML, Zhuang Z, Vortmeyer AO, Boni R, Skarulis M, Marx SJ, Darling TN. Cutaneous tumors in patients with multiple endocrine neoplasia type 1 show allelic deletion of the MEN1 gene. J Invest Dermatol. 1998; 110: 438– 440. [DOI] [PubMed] [Google Scholar]
- 337. Panzuto F, Di Francesco V, Iannicelli E, Sciuto R, Maini CL, Capurso G, Milione M, Cattaruzza MS, Falconi M, David V, Ziparo V, Pederzoli P, Bordi C, Delle Fave G. Long-term clinical outcome of somatostatin analogues for treatment of progressive, metastatic, well-differentiated entero-pancreatic endocrine carcinoma. Ann Oncol. 2006; 17: 461– 466. [DOI] [PubMed] [Google Scholar]
- 338. Panzuto F, Nasoni S, Falconi M, Corleto VD, Capurso G, Cassetta S, Di Fonzo M., Tornatore V, Milione M, Angeletti S, Cattaruzza MS, Ziparo V, Bordi C, Pederzoli P, Delle Fave G. Prognostic factors and survival in endocrine tumor patients: comparison between gastrointestinal and pancreatic localization. Endocr Relat Cancer. 2005; 12: 1083– 1092. [DOI] [PubMed] [Google Scholar]
- 339. Pape UF, Berndt U, Muller-Nordhorn J, Bohmig M, Roll S, Koch M, Willich SN, Wiedenmann B. Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer. 2008; 15: 1083– 1097. [DOI] [PubMed] [Google Scholar]
- 340. Pape UF, Jann H, Muller-Nordhorn J, Bockelbrink A, Berndt U, Willich SN, Koch M, Rocken C, Rindi G, Wiedenmann B. Prognostic relevance of a novel TNM classification system for upper gastroenteropancreatic neuroendocrine tumors. Cancer. 2008; 113: 256– 265. [DOI] [PubMed] [Google Scholar]
- 341. Papillon E, Rolachon A, Calender A, Chabre O, Barnoud R, Fournet J. A malignant gastrointestinal stromal tumour in a patient with multiple endocrine neoplasia type 1. Eur J Gastroenterol Hepatol. 2001; 13: 207– 211. [DOI] [PubMed] [Google Scholar]
- 342. Paties C, Zangrandi A, Vassallo G, Rindi G, Solcia E. Multidirectional carcinoma of the thymus with neuroendocrine and sarcomatoid components and carcinoid syndrome. Pathol Res Pract. 1991; 187: 170– 177. [DOI] [PubMed] [Google Scholar]
- 343. Pavel M, Baudin E, Couvelard A, Krenning E, Oberg K, Steinmuller T, Anlauf M, Wiedenmann B, Salazar R. ENETS consensus guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012; 95: 157– 176. [DOI] [PubMed] [Google Scholar]
- 344. Peghini PL, Annibale B, Azzoni C, Milione M, Corleto VD, Gibril F, Venzon DJ, Delle Fave G, Bordi C, Jensen RT. Effect of chronic hypergastrinemia on human enterochromaffin-like cells: insights from patients with sporadic gastrinomas. Gastroenterology. 2002; 123: 68– 85. [DOI] [PubMed] [Google Scholar]
- 345. Phan GQ, Yeo CJ, Hruban RH, Lillemoe KD, Pitt HA, Cameron JL. Surgical experience with pancreatic and peripancreatic neuroendocrine tumors: review of 125 patients. J Gastrointest Surg. 1998; 2: 472– 482. [PubMed] [Google Scholar]
- 346. Pieterman CR, Schreinemakers JM, Koppeschaar HP, Vriens MR, Rinkes IH, Zonnenberg BA, van der Luijt RB, Valk GD. Multiple endocrine neoplasia type 1 (MEN1): its manifestations and effect of genetic screening on clinical outcome. Clin Endocrinol (Oxf). 2009; 70: 575– 581. [DOI] [PubMed] [Google Scholar]
- 347. Pipeleers-Marichal M, Donow C, Heitz PU, Kloppel G. Pathologic aspects of gastrinomas in patients with Zollinger-Ellison syndrome with and without multiple endocrine neoplasia type I. World J Surg. 1993; 17: 481– 488. [DOI] [PubMed] [Google Scholar]
- 348. Pipeleers-Marichal M, Somers G, Willems G, Foulis A, Imrie C, Bishop AE, Polak JM, Hacki WH, Stamm B, Heitz PU, Kloppel G. Gastrinomas in the duodenums of patients with multiple endocrine neoplasia type 1 and the Zollinger-Ellison syndrome. N Engl J Med. 1990; 322: 723– 727. [DOI] [PubMed] [Google Scholar]
- 349. Pisegna JR, Doppman JL, Norton JA, Metz DC, Jensen RT. Prospective comparative study of ability of MR imaging and other imaging modalities to localize tumors in patients with Zollinger-Ellison syndrome. Dig Dis Sci. 1993; 38: 1318– 1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350. Pisegna JR, Norton JA, Slimak GG, Metz DC, Maton PN, Jensen RT. Effects of curative resection on gastric secretory function and antisecretory drug requirement in the Zollinger-Ellison syndrome. Gastroenterology. 1992; 102: 767– 778. [DOI] [PubMed] [Google Scholar]
- 351. Pisegna JR, Slimak GG, Doppman JL, Strader DB, Metz DC, Fishbeyn VA, Benya RV, Orbuch M, Fraker DL, Norton JA, Maton PN, Jensen RT. An evaluation of human recombinant alpha interferon in patients with metastatic gastrinoma. Gastroenterology. 1993; 105: 1179– 1183. [DOI] [PubMed] [Google Scholar]
- 352. Proye C, Carnaille B, Quievreux JL, Combemale F, Oudar C, Lecomte-Houcke M. Late outcome of 304 consecutive patients with multiple gland enlargement in primary hyperparathyroidism treated by conservative surgery. World J Surg. 1998; 22: 526– 529. [DOI] [PubMed] [Google Scholar]
- 353. Quatrini M, Castoldi L, Rossi G, Cesana BM, Peracchi M, Bardella MT. A follow-up study of patients with Zollinger-Ellison syndrome in the period 1966-2002: effects of surgical and medical treatments on long-term survival. J Clin Gastroenterol. 2005; 39: 376– 380. [DOI] [PubMed] [Google Scholar]
- 354. Raef H, Zou M, Baitei EY, Al-Rijjal RA, Kaya N, Al-Hamed M, Monies D, Abu-Dheim NN, Al-Hindi H, Al-Ghamdi MH, Meyer BF, Shi Y. A novel deletion of the MEN1 gene in a large family of multiple endocrine neoplasia type 1 (MEN1) with aggressive phenotype. Clin Endocrinol (Oxf). 2011; 75: 791– 800. [DOI] [PubMed] [Google Scholar]
- 355. Raut CP, Kulke MH. Targeted therapy in advanced well-differentiated neuroendocrine tumors. Oncologist. 2011; 16: 286– 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C, Valle J, Metrakos P, Smith D, Vinik A, Chen JS, Horsch D, Hammel P, Wiedenmann B, Van Cutsem E, Patyna S, Lu DR, Blanckmeister C, Chao R, Ruszniewski P. Sunitinib Malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011; 364: 501– 513. [DOI] [PubMed] [Google Scholar]
- 357. Regan PT, Malagelada JR. A reappraisal of clinical, roentgenographic, and endoscopic features of the Zollinger-Ellison syndrome. Mayo Clin Proc. 1978; 53: 19– 23. [PubMed] [Google Scholar]
- 358. Richard JL, Ribstein J, Bringer J, Pages M, Jaffiol C, Mirouze J. Adenomatose polyendocrinienne de type I avec tumeur a prolactine revelee par une apoplexie hypophysaire. Nouv Presse Med. 1981; 10: 3149– 3152. [PubMed] [Google Scholar]
- 359. Rigaud D, Bauer P, Hervoir P, Fasano JJ, Moreau J, Mignon M, Bonfils S. Association hyperparathyroidie-syndrome de Zollinger-Ellison. Nouv Presse Med. 1982; 11: 1299– 1303. [PubMed] [Google Scholar]
- 360. Rindi G, Azzoni C, La Rosa S, Klersy C, Paolotti D, Rappel S, Stolte M, Capella C, Bordi C, Solcia E. ECL cell tumor and poorly differentiated endocrine carcinoma of the stomach: prognostic evaluation by pathological analysis. Gastroenterology. 1999; 116: 532– 542. [DOI] [PubMed] [Google Scholar]
- 361. Rogers HM, Keating FR, Jr, Morlock CG, Barker NW. Primary hypertrophy and hyperplasia of the parathyroid glands associated with duodenal ulcer. Arch Intern Med. 1947; 79: 307– 321. [DOI] [PubMed] [Google Scholar]
- 362. Rosai J, Higa E. Mediastinal endocrine neoplasm, of probable thymic origin, related to carcinoid tumor. Clinicopathologic study of 8 cases. Cancer. 1972; 29: 1061– 1074. [DOI] [PubMed] [Google Scholar]
- 363. Rosai J, Higa E, Davie J. Mediastinal endocrine neoplasm in patients with multiple endocrine adenomatosis. A previously unrecognized association. Cancer. 1972; 29: 1075– 1083. [DOI] [PubMed] [Google Scholar]
- 364. Roy P, Venzon DJ, Feigenbaum KM, Koviack PD, Bashir S, Ojeaburu JV, Gibril F, Jensen RT. Gastric secretion in Zollinger-Ellison syndrome: correlation with clinical expression, tumor extent and role in diagnosis. A prospective NIH study of 235 patients and review of the literature in 984 cases. Medicine (Baltimore). 2001; 80: 189– 222. [DOI] [PubMed] [Google Scholar]
- 365. Roy P, Venzon DJ, Shojamanesh H, Abou-Saif A, Peghini P, Doppman JL, Gibril F, Jensen RT. Zollinger-Ellison syndrome: clinical presentation in 261 patients. Medicine (Baltimore). 2000; 79: 379– 411. [DOI] [PubMed] [Google Scholar]
- 366. Rudolf LE, Dammin GF, Moore FD. Intractable peptic ulcer and endocrine adenomas with pituitary amphophilic hyperplasia. Surgery. 1960; 48: 170– 184. [PubMed] [Google Scholar]
- 367. Ruszniewski P, Podevin P, Cadiot G, Marmuse JP, Mignon M, Vissuzaine C, Bonfils S, Lehy T. Clinical, anatomical, and evolutive features of patients with the Zollinger-Ellison syndrome combined with type I multiple endocrine neoplasia. Pancreas. 1993; 8: 295– 304. [DOI] [PubMed] [Google Scholar]
- 368. Sachithanandan N, Harle RA, Burgess JR. Bronchopulmonary carcinoid in multiple endocrine neoplasia type 1. Cancer. 2005; 103: 509– 515. [DOI] [PubMed] [Google Scholar]
- 369. Sakurai A, Katai M, Fukushima Y, Hashizume K. [The clinical course of non-functioning pancreatic neuroendocrine tumors in MEN type 1]. J Familial Tumors. 2006; 6: A41. [Google Scholar]
- 370. Sakurai A, Matsumoto K, Ikeo Y, Nishio SI, Kakizawa T, Arakura F, Ishihara Y, Saida T, Hashizume K. Frequency of facial angiofibromas in Japanese patients with multiple endocrine neoplasia type 1. Endocr J. 2000; 47: 569– 573. [DOI] [PubMed] [Google Scholar]
- 371. Sakurai A, Suzuki S, Kosugi S, Okamoto T, Uchino S, Miya A, Imai T, Kaji H, Komoto I, Miura D, Yamada M, Uruno T, Horiuchi K, Miyauchi A, Imamura MMEN Consortium of Japan. Multiple endocrine neoplasia type 1 in Japan: establishment and analysis of a multicentre database. Clin Endocrinol (Oxf). 2012; 76: 533– 539. [DOI] [PubMed] [Google Scholar]
- 372. Samaan NA, Ouais S, Ordonez NG, Choksi UA, Sellin RV, Hickey RC. Multiple endocrine syndrome type I. Cancer. 1989; 64: 741– 752. [DOI] [PubMed] [Google Scholar]
- 373. Saxena A, Chua TC, Bester L, Kokandi A, Morris DL. Factors predicting response and survival after yttrium-90 radioembolization of unresectable neuroendocrine tumor liver metastases: a critical appraisal of 48 cases. Ann Surg. 2010; 251: 910– 916. [DOI] [PubMed] [Google Scholar]
- 374. Schaefer S, Shipotko M, Meyer S, Ivan D, Klose KJ, Waldmann J, Langer P, Kann PH. Natural course of small adrenal lesions in multiple endocrine neoplasia type 1: an endoscopic ultrasound imaging study. Eur J Endocrinol. 2008; 158: 699– 704. [DOI] [PubMed] [Google Scholar]
- 375. Schmid JR, Labhart A, Rossier PH. Relationship of multiple endocrine adenomas to the syndrome of ulcerogenic islet cell adenomas (Zollinger-Ellison). Am J Med. 1961; 31: 343– 353. [DOI] [PubMed] [Google Scholar]
- 376. Schreinemakers JM, Pieterman CR, Scholten A, Vriens MR, Valk GD, Rinkes IH. The optimal surgical treatment for primary hyperparathyroidism in MEN1 patients: a systematic review. World J Surg. 2011; 35: 1993– 2005. [DOI] [PubMed] [Google Scholar]
- 377. Schurr PG, Strate T, Rese K, Kaifi JT, Reichelt U, Petri S, Kleinhans H, Yekebas EF, Izbicki JR. Aggressive surgery improves long-term survival in neuroendocrine pancreatic tumors: an institutional experience. Ann Surg. 2007; 245: 273– 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Shepherd JJ. The natural history of multiple endocrine neoplasia type I. Highly uncommon or highly unrecognized. Arch Surg. 1991; 126: 935– 952. [DOI] [PubMed] [Google Scholar]
- 379. Shepherd JJ, Challis DR, Davies PF, McArdle JP, Teh BT, Wilkinson S. Multiple endocrine neoplasm, type 1: Gastrinomas, pancreatic neoplasms, microcarcinoids, the Zollinger-Ellison syndrome, lymph nodes, and hepatic metastases. Arch Surg. 1993; 128: 1133– 1142. [DOI] [PubMed] [Google Scholar]
- 380. Sheppard BC, Norton JA, Doppman JL, Maton PN, Gardner JD, Jensen RT. Management of islet cell tumors in patients with Multiple Endocrine Neoplasia: a prospective study. Surgery. 1989; 106: 1108– 1117. [PubMed] [Google Scholar]
- 381. Shigematsu S, Shimoyama N, Sato Y, Horita M, Oribe Y, Ono J, Takaki R, Ishimatsu T, Kodama M, Iwashita K. [A case of multiple endocrine neoplasia, type 1, with parathyroid adenoma, multinodular adrenal cortical hyperplasia, islet cell tumor and hyperplasia of thyroid with concomitant hypersecretion of gastrin and total glucagon-like immunoreactivity]. Nihon Naika Gakkai Zasshi. 1989; 78: 357– 362. [DOI] [PubMed] [Google Scholar]
- 382. Shojamanesh H, Gibril F, Louie A, Ojeaburu JV, Bashir S, Abou-Saif A, Jensen RT. Prospective study of the anti-tumor efficacy of long-term octreotide treatment in patients with progressive metastatic gastrinomas. Cancer. 2002; 94: 331– 343. [DOI] [PubMed] [Google Scholar]
- 383. Shum HY, O’Neill BJ, Streeter AM. Vitamin-B 12 absorption and the Zollinger-Ellison syndrome. Lancet. 1971; 1: 1303. [DOI] [PubMed] [Google Scholar]
- 384. Simonds WF, James-Newton L, Agarwal SK, Yang B, Skarulis MC, Hendy GN, Marx SJ. Familial isolated hyperparathyroidism: clinical and genetic characteristics of 36 kindreds. Medicine (Baltimore). 2002; 81: 1– 26. [DOI] [PubMed] [Google Scholar]
- 385. Simonds WF, Varghese S, Marx SJ, Nieman LK. Cushing’s syndrome in multiple endocrine neoplasia type 1. Clin Endocrinol (Oxf). 2012; 76: 379– 386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386. Sitges Serra A. [Zollinger-Ellison syndrome. Experience in 14 cases and a review of the recent literature]. Med Clin (Barc). 1984; 83: 550– 556. [PubMed] [Google Scholar]
- 387. Skogseid B, Ericksson B, Lundqvist G, Lorelius L-E, Rastad J, Wide L, Akerstrom G, Oberg K. Multiple endocrine neoplasia type I: a 10-year prospective screening study in four kindreds. J Clin Endocrinol Metab. 1991; 73: 281– 287. [DOI] [PubMed] [Google Scholar]
- 388. Skogseid B, Larsson C, Lindgren PG, Kvanta E, Rastad J, Theodorsson E, Wide L, Wilander E, Oberg K. Clinical and genetic features of adrenocortical lesions in multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1992; 75: 76– 81. [DOI] [PubMed] [Google Scholar]
- 389. Skogseid B, Oberg K, Eriksson B, Juhlin C, Granberg D, Akerstrom G, Rastad J. Surgery for asymptomatic pancreatic lesion in multiple endocrine neoplasia type 1. World J Surg. 1996; 20: 872– 877. [DOI] [PubMed] [Google Scholar]
- 390. Skogseid B, Rastad J, Gobl A, Larsson C, Backlin K, Juhlin C, Akerstrom G, Oberg K. Adrenal lesion in multiple endocrine neoplasia type 1. Surgery. 1995; 118: 1077– 1082. [DOI] [PubMed] [Google Scholar]
- 391. Smith R. The Zollinger-Ellison syndrome. Ann R Coll Surg Engl. 1965; 37: 160– 165. [PMC free article] [PubMed] [Google Scholar]
- 392. Soga J, Yakuwa Y, Osaka M. Evaluation of 342 cases of mediastial/thymic carcinoids collected from literature: a comparative study between typical carcinoids and atypical varieties. Ann Thorac Cardiovasc Surg. 1999; 5: 285– 292. [PubMed] [Google Scholar]
- 393. Solcia E, Capella C, Fiocca R, Rindi G, Rosai J. Gastric argyrophil carcinoidosis in patients with Zollinger-Ellison syndrome due to type 1 multiple endocrine neoplasia. A newly recognized association. Am J Surg Pathol. 1990; 14: 503– 513. [DOI] [PubMed] [Google Scholar]
- 394. Spence RW, Celestin LR. Gynaecomastia associated with cimetidine. Gut. 1979; 20: 154– 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395. Srivastava A, Hornick JL. Immunohistochemical staining for CDX-2, PDX-1, NESP-55, and TTF-1 can help distinguish gastrointestinal carcinoid tumors from pancreatic endocrine and pulmonary carcinoid tumors. Am J Surg Pathol. 2009; 33: 626– 632. [DOI] [PubMed] [Google Scholar]
- 396. Stabile BE. Islet cell tumors. Gastroenterologist. 1997; 5: 213– 232. [PubMed] [Google Scholar]
- 397. Stabile BE, Braunstein GD, Passaro E., Jr Serum gastrin and human chorionic gonadotropin in the Zollinger-Ellison syndrome. Arch Surg. 1980; 115: 1090– 1095. [DOI] [PubMed] [Google Scholar]
- 398. Stabile BE, Passaro E., Jr Benign and malignant gastrinoma. Am J Surg. 1985; 49: 144– 150. [DOI] [PubMed] [Google Scholar]
- 399. Stocks AE. Problems of the syndrome of familial multiple endocrine adenomas. Australas Ann Med. 1967; 16: 278– 288. [DOI] [PubMed] [Google Scholar]
- 400. Strosberg J, Gardner N, Kvols L. Survival and prognostic factor analysis of 146 metastatic neuroendocrine tumors of the mid-gut. Neuroendocrinology. 2009; 89: 471– 476. [DOI] [PubMed] [Google Scholar]
- 401. Strosberg JR, Cheema A, Kvols LK. A review of systemic and liver-directed therapies for metastatic neuroendocrine tumors of the gastroenteropancreatic tract. Cancer Control. 2011; 18: 127– 137. [DOI] [PubMed] [Google Scholar]
- 402. Strosberg JR, Fine RL, Choi J, Nasir A, Coppola D, Chen DT, Helm J, Kvols L. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer. 2011; 117: 268– 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403. Sugg SL, Norton JA, Fraker DL, Metz DC, Pisegna JR, Fishbeyn V, Benya RV, Shawker TH, Doppman JL, Jensen RT. A prospective study of intraoperative methods to diagnose and resect duodenal gastrinomas. Ann Surg. 1993; 218: 138– 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404. Summerskill WH, Code CF, Hallenbeck GA, Priestley JT. Intractable peptic ulcer in hereditary endocrine-ulcer disease: "Gastrin" content of endocrine tissues. Proc Staff Meetings Mayo Clin. 1961; 36: 611– 617. [PubMed] [Google Scholar]
- 405. Sutliff VE, Doppman JL, Gibril F, Yu F, Serrano J, Venzon DJ, Jensen RT. Growth of newly diagnosed, untreated metastatic gastrinomas and predictors of growth patterns. J Clin Oncol. 1997; 15: 2420– 2431. [DOI] [PubMed] [Google Scholar]
- 406. Suzuki S. [The latest aspects of MEN1]. Endocrine Surgery. 2011; 28: 4– 11. [Google Scholar]
- 407. Suzuki S, Suzuki K, Kawahara M, Asahi S, Nakano K, Fukushima T, Sekikawa K, Takenoshita S. [Long-term postoperative follow-up for patients with familial hyperparathyroidism]. J Familial Tumors. 2005; 5: 82– 88. [Google Scholar]
- 408. Takagi J, Otake K, Morishita M, Kato H, Nakao N, Yoshikawa K, Ikeda H, Hirooka Y, Hattori Y, Larsson C, Nogimori T. Multiple endocrine neoplasia type I and Cushing’s syndrome due to an aggressive ACTH producing thymic carcinoid. Intern Med. 2006; 45: 81– 86. [DOI] [PubMed] [Google Scholar]
- 409. Takayama T, Kameya T, Inagaki K, Nonaka M, Miyazawa H, Ogawa N, Yano M, Morita T, Arai T, Niino S. MEN type 1 associated with mediastinal carcinoid producing parathyroid hormone, calcitonin and chorionic gonadotropin. Pathol Res Pract. 1993; 189: 1090– 1096. [DOI] [PubMed] [Google Scholar]
- 410. Tanabe T, Yasuo M, Tsushima K, Urushihata K, Yamamoto H, Hanaoka M, Koizumi T, Fujimoto K, Yamazaki Y, Hirose Y, Hamano H, Sakurai A, Kubo K. Mediastinal seminoma in a patient with multiple endocrine neoplasia type 1. Intern Med. 2008; 47: 1615– 1619. [DOI] [PubMed] [Google Scholar]
- 411. Tanaka Y, Hongo K, Tada T, Takizawa T, Kakizawa Y, Koyama J, Kobayashi S, Sakurai A, Hashizume K. [Surgical treatments for 7 pituitary adenomas in multiple endocrine neoplasia type 1]. No Shinkei Geka. 2000; 28: 1087– 1092. [PubMed] [Google Scholar]
- 412. Teh BT. Thymic carcinoids in multiple endocrine neoplasia type 1. J Intern Med. 1998; 243: 501– 504. [DOI] [PubMed] [Google Scholar]
- 413. Teh BT, McArdle J, Chan SP, Menon J, Hartley L, Pullan P, Ho J, Khir A, Wilkinson S, Larsson C, Cameron D, Shepherd J. Clinicopathologic studies of thymic carcinoids in multiple endocrine neoplasia type 1. Medicine (Baltimore). 1997; 76: 21– 29. [DOI] [PubMed] [Google Scholar]
- 414. Teh BT, Zedenius J, Kytola S, Skogseid B, Trotter J, Choplin H, Twigg S, Farnebo F, Giraud S, Cameron D, Robinson B, Calender A, Larsson C, Salmela P. Thymic carcinoids in multiple endocrine neoplasia type 1. Ann Surg. 1998; 228: 99– 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415. Termanini B, Gibril F, Doppman JL, Reynolds JC, Stewart CA, Sutliff VE, Venzon DJ, Jensen RT. Distinguishing small hepatic hemangiomas from vascular liver metastases in patients with gastrinoma: use of a somatostatin-receptor scintigraphic agent. Radiology. 1997; 202: 151– 158. [DOI] [PubMed] [Google Scholar]
- 416. Termanini B, Gibril F, Reynolds JC, Doppman JL, Chen CC, Stewart CA, Sutliff V, Jensen RT. Value of somatostatin receptor scintigraphy: a prospective study in gastrinoma of its effect on clinical management. Gastroenterology. 1997; 112: 335– 347. [DOI] [PubMed] [Google Scholar]
- 417. Termanini B, Gibril F, Sutliff VE III, Yu F, Venzon DJ, Jensen RT. Effect of long-term gastric acid suppressive therapy on serum vitamin B12 levels in patients with Zollinger-Ellison syndrome. Am J Med. 1998; 104: 422– 430. [DOI] [PubMed] [Google Scholar]
- 418. Thakker RV. Multiple endocrine neoplasia type 1. Endocrinol Metab Clin North Am. 2000; 29: 541– 567. [DOI] [PubMed] [Google Scholar]
- 419. Thakker RV. Multiple endocrine neoplasia type 1 (MEN1). Best Pract Res Clin Endocrinol Metab. 2010; 24: 355– 370. [DOI] [PubMed] [Google Scholar]
- 420. Tham E, Grandell U, Lindgren E, Toss G, Skogseid B, Nordenskjold M. Clinical testing for mutations in the MEN1 gene in Sweden: a report on 200 unrelated cases. J Clin Endocrinol Metab. 2007; 92: 3389– 3395. [DOI] [PubMed] [Google Scholar]
- 421. Thom AK, Norton JA, Axiotis CA, Jensen RT. Location, incidence and malignant potential of duodenal gastrinomas. Surgery. 1991; 110: 1086– 1093. [PubMed] [Google Scholar]
- 422. Thom AK, Norton JA, Doppman JL, Chang R, Miller DL, Jensen RT. Prospective study of the use of intraarterial secretin injection and portal venous sampling to localize duodenal gastrinomas. Surgery. 1992; 112: 1002– 1008. [PubMed] [Google Scholar]
- 423. Thomas-Marques L, Murat A, Delemer B, Penfornis A, Cardot-Bauters C, Baudin E, Niccoli-Sire P, Levoir D, Choplin HB, Chabre O, Jovenin N, Cadiot G. Prospective endoscopic ultrasonographic evaluation of the frequency of nonfunctioning pancreaticoduodenal endocrine tumors in patients with multiple endocrine neoplasia type 1. Am J Gastroenterol. 2006; 101: 266– 273. [DOI] [PubMed] [Google Scholar]
- 424. Thompson JC, Lewis BG, Wiener I, Townsend CM., Jr The role of surgery in the Zollinger-Ellison syndrome. Ann Surg. 1983; 197: 594– 607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425. Thompson NW. Current concepts in the surgical management of multiple endocrine neoplasia type 1 pancreatic-duodenal disease. Results in the treatment of 40 patients with Zollinger-Ellison syndrome, hypoglycaemia or both. J Intern Med. 1998; 243: 495– 500. [DOI] [PubMed] [Google Scholar]
- 426. Thrumurthy SG, Date RS, Mughal MM, Pursnani KG, Ward JB. The surgical management of pancreaticoduodenal tumours in multiple endocrine neoplasia type 1. BMJ Case Rep. 2009; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427. Tisell LE, Ahlman H, Jansson S, Grimelius L. Total pancreatectomy in the MEN-1 syndrome. Br J Surg. 1988; 75: 154– 157. [DOI] [PubMed] [Google Scholar]
- 428. Tobimatsu T, Kaji H, Naito J, Iu MF, Nomura R, Sowa H, Yamauchi M, Sugimoto T, Chihara K, Tsukada T. [Case Report No.143: one case of multiple endosecretory-adenomatosis accompanied with ventricula ependymoma]. Clin Calcium. 2004; 14: 150– 153. [PubMed] [Google Scholar]
- 429. Tomassetti P, Campana D, Piscitelli L, Casadei R, Santini D, Nori F, Morselli-Labate AM, Pezzilli R, Corinaldesi R. Endocrine pancreatic tumors: factors correlated with survival. Ann Oncol. 2005; 16: 1806– 1810. [DOI] [PubMed] [Google Scholar]
- 430. Tomassetti P, Migliori M, Corinaldesi R, Gullo L. Treatment of gastroenteropancratic neuroendocrine tumours with octreotide LAR. Aliment Pharmacol Ther. 2000; 14: 557– 560. [DOI] [PubMed] [Google Scholar]
- 431. Tonelli F, Fratini G, Nesi G, Tommasi MS, Batignani G, Falchetti A, Brandi ML. Pancreatectomy in multiple endocrine neoplasia type 1-related gastrinomas and pancreatic endocrine neoplasias. Ann Surg. 2006; 244: 61– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432. Toshimori H, Okamoto M, Nakatsuru K, Hidaka H, Yamaguchi H, Ushiroda Y, Kisanuki A, Tsubouchi H, Sumiyoshi A, Matsukura S. Multiple endocrine neoplasia type 1 associated with malignant lymphoma and other complications. Intern Med. 1996; 35: 849– 854. [DOI] [PubMed] [Google Scholar]
- 433. Triponez F, Dosseh D, Goudet P, Cougard P, Bauters C, Murat A, Cadiot G, Niccoli-Sire P, Chayvialle JA, Calender A, Proye CA. Epidemiology data on 108 MEN 1 patients from the GTE with isolated nonfunctioning tumors of the pancreas. Ann Surg. 2006; 243: 265– 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434. Triponez F, Goudet P, Dosseh D, Cougard P, Bauters C, Murat A, Cadiot G, Niccoli-Sire P, Calender A, Proye CA. Is surgery beneficial for MEN1 patients with small (≤2 cm), nonfunctioning pancreaticoduodenal endocrine tumor? An analysis of 65 patients from the GTE. World J Surg. 2006; 30: 654– 662. [DOI] [PubMed] [Google Scholar]
- 435. Trouillas J, Labat-Moleur F, Sturm N, Kujas M, Heymann MF, Figarella-Branger D, Patey M, Mazucca M, Decullier E, Verges B, Chabre O, Calender A. Pituitary tumors and hyperplasia in multiple endocrine neoplasia type 1 syndrome (MEN1): a case-control study in a series of 77 patients versus 2509 non-MEN1 patients. Am J Surg Pathol. 2008; 32: 534– 543. [DOI] [PubMed] [Google Scholar]
- 436. Trump D, Farren B, Wooding C, Pang JT, Besser GM, Buchanan KD, Edwards CR, Heath DA, Jackson CE, Jansen S, Lips K, Monson JP, O’Halloran D, Sampson J, Shalet SM, Wheeler MH, Zink A, Thakker RV. Clinical studies of multiple endocrine neoplasia type 1 (MEN1). Q J Med. 1996; 89: 653– 669. [DOI] [PubMed] [Google Scholar]
- 437. Ukita C, Yamaguchi M, Tanaka T, Shigeta H, Nishikawa M. A novel missense mutation of the MEN1 gene in a multiple endocrine neoplasia type 1 patient associated with carcinoid syndrome. Intern Med. 2003; 42: 1112– 1116. [DOI] [PubMed] [Google Scholar]
- 438. Underdahl LO, Woolner LB, Black BM. Multiple endocrine adenomas: report of 8 cases in which the parathyroids, pituitary and pancreatic islets were involved. J Clin Endocrinol Metab. 1953; 13: 20– 47. [DOI] [PubMed] [Google Scholar]
- 439. Valdes N, de Nanclares GP, Alvarez V, Castano L, Diaz-Cadorniga F, Aller J, Coto E. Multiple endocrine neoplasia type 1 (MEN1): clinical heterogeneity in a large family with a nonsense mutation in the MEN1 gene (Trp471Stop). Clin Endocrinol. 1999; 50: 309– 313. [DOI] [PubMed] [Google Scholar]
- 440. Van Heerden JA, Smith SL, Miller LJ. Management of the Zollinger-Ellison syndrome in patients with multiple endocrine neoplasia type 1. Surgery. 1986; 100: 971– 977. [PubMed] [Google Scholar]
- 441. van Schaik E, van Vliet EI, Feelders RA, Krenning EP, Khan S, Kamp K, Valkema R, van Nederveen FH, Teunissen JJ, Kwekkeboom DJ, de Herder WW. Improved control of severe hypoglycemia in patients with malignant insulinomas by Peptide receptor radionuclide therapy. J Clin Endocrinol Metab. 2011; 96: 3381– 3389. [DOI] [PubMed] [Google Scholar]
- 442. van Wijk JP, Dreijerink KM, Pieterman CR, Lips CJ, Zelissen PM, Valk GD. Increased prevalence of impaired fasting glucose in MEN1 gene mutation carriers. Clin Endocrinol (Oxf). 2012; 76: 67– 71. [DOI] [PubMed] [Google Scholar]
- 443. Vance JE, Stoll RW, Kitabchi AE, Hollander D, Williams RH. Familial nesidioblastosis as the predominant manifestation of multiple endocrine adenomatosis. Am J Med. 1972; 52: 211– 227. [DOI] [PubMed] [Google Scholar]
- 444. Vasen HF, Lamers CB, Lips CJ. Screening for the multiple endocrine neoplasia syndrome type I. A study of 11 kindreds in the Netherlands. Arch Intern Med. 1989; 149: 2717– 2722. [PubMed] [Google Scholar]
- 445. Vellar D, Henderson M, Vellar ID, Desmond P. The Zollinger-Ellison syndrome: a review of the St. Vincent’s hospital, Melbourne experience. Aust N Z J Surg. 1985; 55: 455– 462. [DOI] [PubMed] [Google Scholar]
- 446. Venkatesh S, Ordonez NG, Ajani J, Schultz PN, Hickey RC, Johnston DA, Samaan NA. Islet cell carcinoma of the pancreas. A study of 98 patients. Cancer. 1990; 65: 354– 357. [DOI] [PubMed] [Google Scholar]
- 447. Verges B, Boureille F, Goudet P, Murat A, Beckers A, Sassolas G, Cougard P, Montvernay C, Calender A. Pituitary disease in MEN type 1 (MEN1): data from the France-Belgium MEN1 multicenter study. J Clin Endocrinol Metab. 2002; 87: 457– 465. [DOI] [PubMed] [Google Scholar]
- 448. Vierimaa O, Ebeling TM, Kytola S, Bloigu R, Eloranta E, Salmi J, Korpi-Hyovalti E, Niskanen L, Orvola A, Elovaara E, Gynther A, Sane T, Valimaki M, Ignatius J, Leisti J, Salmela PI. Multiple endocrine neoplasia type 1 in Northern Finland; clinical features and genotype phenotype correlation. Eur J Endocrinol. 2007; 157: 285– 294. [DOI] [PubMed] [Google Scholar]
- 449. Vieto RJ, Hickey RC, Samann NA, Type I. multiple endocrine neoplasias. Curr Probl Cancer. 1982; 7: 1– 25. [DOI] [PubMed] [Google Scholar]
- 450. von Schrenck T, Howard JM, Doppman JL, Norton JA, Maton PN, Smith FP, Vinayek R, Frucht H, Wank SA, Gardner JD, Jensen RT. Prospective study of chemotherapy in patients with metastatic gastrinoma. Gastroenterology. 1988; 94: 1326– 1334. [DOI] [PubMed] [Google Scholar]
- 451. Vortmeyer AO, Lubensky IA, Skarulis M, Li G, Moon YW, Park WS, Weil R, Barlow C, Spiegel AM, Marx SJ, Zhuang Z. Multiple endocrine neoplasia type 1: atypical presentation, clinical course, and genetic analysis of multiple tumors. Mod Pathol. 1999; 12: 919– 924. [PubMed] [Google Scholar]
- 452. Wagner AM, Martin-Campos JM, Mayoral C, de Leiva A, Blanco-Vaca F. Patients with MEN-1 are more insulin-resistant than their non-affected relatives. Eur J Intern Med. 2005; 16: 507– 509. [DOI] [PubMed] [Google Scholar]
- 453. Waldmann J, Bartsch DK, Kann PH, Fendrich V, Rothmund M, Langer P. Adrenal involvement in multiple endocrine neoplasia type 1: results of 7 years prospective screening. Langenbecks Arch Surg. 2007; 392: 437– 443. [DOI] [PubMed] [Google Scholar]
- 454. Waldmann J, Habbe N, Fendrich V, Slater EP, Kann PH, Rothmund M, Langer P. Fast-growing pancreatic neuroendocrine carcinoma in a patient with multiple endocrine neoplasia type 1: a case report. J Med Case Reports. 2008; 2: 354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455. Walker MD, Silverberg SJ. Cardiovascular aspects of primary hyperparathyroidism. J Endocrinol Invest. 2008; 31: 925– 931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456. Wank SA, Doppman JL, Miller DL, Collen MJ, Maton PN, Vinayek R, Slaff JI, Norton JA, Gardner JD, Jensen RT. Prospective study of the ability of computerized axial tomography to localize gastrinomas in patients with Zollinger-Ellison syndrome. Gastroenterology. 1987; 92: 905– 912. [DOI] [PubMed] [Google Scholar]
- 457. Wautot V, Vercherat C, Lespinasse J, Chambe B, Lenoir GM, Zhang CX, Porchet N, Cordier M, Beroud C, Calender A. Germline mutation profile of MEN1 in multiple endocrine neoplasia type 1: search for correlation between phenotype and the functional domains of the MEN1 protein. Hum Mutat. 2002; 20: 35– 47. [DOI] [PubMed] [Google Scholar]
- 458. Way L, Goldman L, Dunphy JE. Zollinger-Ellison syndrome. An analysis of twenty-five cases. Am J Surg. 1968; 116: 293– 304. [DOI] [PubMed] [Google Scholar]
- 459. Weber HC, Venzon DJ, Lin JT, Fishbein VA, Orbuch M, Strader DB, Gibril F, Metz DC, Fraker DL, Norton JA, Jensen RT. Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Gastroenterology. 1995; 108: 1637– 1649. [DOI] [PubMed] [Google Scholar]
- 460. Weber JM, Lewis S, Heasley KH. Observations on small bowel pattern associated with the Zollinger-Ellison syndrome. Am J Roentgenol. 1959; 82: 973– 977. [PubMed] [Google Scholar]
- 461. Weichert R, Reed R, Creech O., Jr Carcinoid-islet cell tumors of the duodenum. Ann Surg. 1967; 165: 660– 669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462. Wermer P. Endocrine adenomatosis and peptic ulcer in a large kindred. Am J Med. 1963; 35: 205– 212. [DOI] [PubMed] [Google Scholar]
- 463. Wickbom G, Landor JH, Bushkin FL, McGuigan JE. Changes in canine gastric acid output and serum gastrin levels following massive small intestinal resection. Gastroenterology. 1975; 69: 448– 452. [PubMed] [Google Scholar]
- 464. Wilder RM, Allan FN, Power WH, Robertson HE. Carcinoma of the islands of the pancreas: hyperinsulinism and hypoglycemia. JAMA. 1927; 89: 348– 355. [Google Scholar]
- 465. Wilkinson S, Teh BT, Davey KR, McArdle JP, Young M, Shepherd JJ. Cause of death in multiple endocrine neoplasia type 1. Arch Surg. 1993; 128: 683– 690. [DOI] [PubMed] [Google Scholar]
- 466. Wilson SD, Krzywda EA, Zhu YR, Yen TW, Wang TS, Sugg SL, Pappas SG. The influence of surgery in MEN-1 syndrome: observations over 150 years. Surgery. 2008; 144: 695– 701. [DOI] [PubMed] [Google Scholar]
- 467. Yamada T, Imai T, Kikumori Y, Sawaki M, Takada H, Sato T, Sasa M, Uchida D, Watanabe R, Kagawa A. [An autopsy case of multiple endocrine neoplasia type 1 complicated by an ectopic ACTH producing tumor]. J Japan Assoc Endocr Surgeons Japanese Soc Thyroid Surg. 2009; 21: 90. [Google Scholar]
- 468. Yamaguchi K, Kameya T, Abe K. Multiple endocrine neoplasia type 1. Clin Endocrinol Metab. 1980; 9: 261– 284. [DOI] [PubMed] [Google Scholar]
- 469. Yang Y, Hua X. In search of tumor suppressing functions of menin. Mol Cell Endocrinol. 2007; 265–266: 34– 41[sic]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470. Yano M, Fukai I, Kobayashi Y, Mizuno K, Konishi A, Haneda H, Suzuki E, Endo K, Fujii Y. ACTH secreting thymic carcinoid associated with multiple endocrine neoplasia type 1. Ann Thorac Surg. 2006; 81: 366– 368. [DOI] [PubMed] [Google Scholar]
- 471. Yao JC, Eisner MP, Leary C, Dagohoy C, Phan A, Rashid A, Hassan M, Evans DB. Population-based study of islet cell carcinoma. Ann Surg Oncol. 2007; 14: 3492– 3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472. Yao JC, Lombard-Bohas C, Baudin E, Kvols LK, Rougier P, Ruszniewski P, Hoosen S, St Peter J, Haas T, Lebwohl D, Van Cutsem E, Kulke MH, Hobday TJ, O’Dorisio TM, Shah MH, Cadiot G, Luppi G, Posey JA, Wiedenmann B. Daily oral everolimus activity in patients with metastatic pancreatic neuroendocrine tumors after failure of cytotoxic chemotherapy: a phase II trial. J Clin Oncol. 2010; 28: 69– 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473. Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, Hobday TJ, Okusaka T, Capdevila J, de Vries EG, Tomassetti P, Pavel ME, Hoosen S, Haas T, Lincy J, Lebwohl D, Oberg K. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011; 364: 514– 523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474. Yoshimoto K, Saito S. Clinical characteristics in multiple endocrine neoplasia type 1 in Japan: a review of 106 patients. Folia Endocrinol. 1991; 67: 764– 774. [DOI] [PubMed] [Google Scholar]
- 475. You YN, Thompson GB, Young WF, Jr, Larson D, Farley DR, Richards M, Grant CS. Pancreatoduodenal surgery in patients with multiple endocrine neoplasia type 1: operative outcomes, long-term function, and quality of life. Surgery. 2007; 142: 829– 836. [DOI] [PubMed] [Google Scholar]
- 476. Yu F, Venzon DJ, Serrano J, Goebel SU, Doppman JL, Gibril F, Jensen RT. Prospective study of the clinical course, prognostic factors and survival in patients with longstanding Zollinger-Ellison syndrome. J Clin Oncol. 1999; 17: 615– 630. [DOI] [PubMed] [Google Scholar]
- 477. Zeiger MA, Swartz SE, MacGillivray DC, Linnoila I, Shakir M. Thymic carcinoid in association with MEN syndromes. Am Surg. 1992; 58: 430– 434. [PubMed] [Google Scholar]
- 478. Zerbi A, Capitanio V, Boninsegna L, Pasquali C, Rindi G, Delle Fave GF, Del Chiaro M, Casadei R, Falconi M. Surgical treatment of pancreatic endocrine tumours in Italy: results of a prospective multicentre study of 262 cases. Langenbecks Arch Surg. 2011; 396: 313– 321. [DOI] [PubMed] [Google Scholar]
- 479. Zhuang Z, Vortmeyer AO, Pack S, Huang S, Pham TA, Wang C, Park WS, Agarwal SK, Debelenko LV, Kester M, Guru SC, Manickam P, Olufemi SE, Yu F, Heppner C, Crabtree JS, Skarulis MC, Venzon DJ, Emmert-Buck MR, Spiegel AM, Chandrasekharappa SC, Collins FS, Burns AL, Marx SJ, Jensen RT, Liotta LA, Lubensky IA, et al. Somatic mutations of the MEN1 tumor suppressor gene in sporadic gastrinomas and insulinomas. Cancer Res. 1997; 57: 4682– 4686. [PubMed] [Google Scholar]
- 480. Zimering MB, Brandi ML, deGrange DA, Marx SJ, Streeten E, Katsumata N, Murphy PR, Sato Y, Friesen HG, Aurbach GD. Circulating fibroblast growth factor-like substance in familial multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1990; 70: 149– 154. [DOI] [PubMed] [Google Scholar]
- 481. Zollinger RM. Gastrinoma: factors influencing prognosis. Surgery. 1985; 97: 49– 54. [PubMed] [Google Scholar]
- 482. Zollinger RM, Ellison EC, O’Dorisio TM, Sparks J. Thirty years’ experience with gastrinoma. World J Surg. 1984; 8: 427– 435. [DOI] [PubMed] [Google Scholar]
- 483. Zollinger RM, Ellison EH. Primary peptic ulcerations of the jejunum associated with islet cell tumors of the pancreas. Ann Surg. 1955; 142: 709– 728. [PMC free article] [PubMed] [Google Scholar]
- 484. Zollinger RM, Martin EW, Jr, Carey LC, Sparks J, Minton JP. Observations on the postoperative tumor growth behavior of certain islet cell tumors. Ann Surg. 1976; 184: 525– 530. [DOI] [PMC free article] [PubMed] [Google Scholar]


