Abstract
This study compared mathematical outcomes in children with predominantly moderate to severe traumatic brain injury (TBI; n =50) or orthopedic injury (OI; n=47) at 2 and 24 months post-injury. Working memory and its contribution to math outcomes at 24 months post-injury was also examined. Participants were administered an experimental cognitive addition task and standardized measures of calculation, math fluency, and applied problems; as well as experimental measures of verbal and visual-spatial working memory. Although children with TBI did not have deficits in foundational math fact retrieval, they performed more poorly than OIs on standardized measures of math. In the TBI group, performance on standardized measures was predicted by age at injury, socioeconomic status, and the duration of impaired consciousness. Children with TBI showed impairments on verbal, but not visual working memory relative to children with OI. Verbal working memory mediated group differences on math calculations and applied problems at 24 months post-injury. Children with TBI have difficulties in mathematics, but do not have deficits in math fact retrieval, a signature deficit of math disabilities. Results are discussed with reference to models of mathematical cognition and disability and the role of working memory in math learning and performance for children with TBI.
Keywords: Head injury, Cognitive addition, Math fluency, Calculation, Math problem solving, Verbal working memory, Visual-spatial working memory
INTRODUCTION
Traumatic brain injury (TBI) is the most common cause of disability in childhood (Langlois, Rutland-Brown, & Thomas, 2004). Multiple areas of cognitive functioning, such as information processing speed, memory, and executive functioning, may be adversely affected (Ewing-Cobbs, Prasad, et al., 1998; Levin et al., 2002). Difficulties in academic achievement are significant after TBI; many children either fail a grade or require special educational support (Ewing-Cobbs, Levin, Fletcher, Iovino, & Miner, 1998). Despite the importance of mathematical competence for school and vocational success (Rivera-Batiz, 1992), few studies have examined: a broad range of mathematical skills after TBI; whether TBI is associated with deficits in foundational math skills such as fact retrieval; and whether mathematical performance is related to TBI-related deficits in working memory (WM), a neurocognitive skill important for mathematical development and performance (Espy et al., 2004; Raghubar, Barnes, & Hecht, 2010). The current study addressed these questions.
Mathematical Outcomes in Children With TBI
Early studies indicated that math is particularly affected by TBI compared with other academic skills (e.g., Chadwick, Rutter, Shaffer, & Shrout, 1981; Jaffe et al., 1992). However, more recent prospective studies report variable findings: In some studies, children with more severe injuries are lower in math calculations than their typically developing peers (Catroppa, Anderson, Morse, Haritou, & Rosenfeld, 2008; Ewing-Cobbs et al., 2006) or than children with less severe TBI (Catroppa et al., 2009; Ewing-Cobbs, Levin, et al., 1998; Fay et al., 1994; Taylor et al., 2002); other studies report similar performance in children with TBI and their typically achieving peers, at least 1 year post-injury (Ayr, Yeates, & Enrile, 2005; Taylor, Yeates, Wade, Drotar, & Klein, 1999; Taylor et al., 2008). The one study that evaluated several aspects of math achievement (i.e., calculation, applied problem solving, and math fluency) found lower performance in children with moderate to severe TBI relative to a community comparison group (Ewing-Cobbs et al., 2006). Information on a range of mathematical achievement outcomes is sparse. Also understudied is the potential role that TBI-related impairments in domains such as executive functions might play in mathematical functioning of these children (Barnes, Fletcher, & Ewing-Cobbs, 2007).
Mathematical Disability
Few studies have examined mathematical processing in children following TBI based on models of mathematical development and disability (but see Ayr et al., 2005). In some models, the ability to quickly and accurately retrieve answers to single-digit arithmetic problems (efficient math fact retrieval) is considered to be a foundational skill (Geary, Fan, & Bow-Thomas, 1992; Hecht, Torgesen, Wagner, & Rashotte, 2001) that is disrupted in individuals with mathematical disabilities with and without neurodevelopmental disorder (Barnes et al., 2006; Hanich, Jordan, Kaplan, & Dick, 2001). Children with math disability retrieve answers from memory less often than their typically developing peers, demonstrate more counting errors, use less developmentally mature strategies, and have highly variable math fact retrieval times (Geary, 1990; Hanich et al., 2001).
Although deficits in math fact retrieval are considered to be a “signature” deficit in children with math disabilities, it is not known whether this is also true for children with TBI. Even though Ayr et al. (2005) found that children with TBI did not make more math fact errors (e.g., errors at the single-digit level) than orthopedic controls in a multi-digit written arithmetic task, determining the integrity of math fact retrieval processes requires knowledge about both accuracy and speed of single-digit arithmetic, which has not been studied after childhood TBI.
Injury-Related Factors and Academic Skill Development after TBI
Mild TBI does not appear to be associated with a significant decrease in math, spelling, or reading scores when scores are adjusted for prior risk factors (e.g., Bijur, Haslum, & Golding, 1990). In contrast, children with severe TBI have worse performance than either children with mild injuries or community controls in several academic achievement domains during the early stages of recovery as well as 6 months to several years after the injury (Barnes et al., 2006; Barnes, Dennis, & Wilkinson, 1999; Ewing-Cobbs, Levin, et al., 1998; Jaffe et al., 1992, but see, Kinsella et al., 1995). It is not known whether injury severity affects math fact retrieval or aspects of math achievement other than calculations.
Cognitive Processes Following Childhood TBI and Their Effect on Math Outcomes
When considering academic skill development following childhood TBI, academic difficulties may be related to impairments in domain general abilities, such as WM, a mental workspace where task relevant information is monitored, processed, and maintained to respond to environmental demands (Baddeley & Logie, 1999). WM and math are related, though whether WM plays a supportive or causal role in mathematical development, is a matter of debate (review in Raghubar et al., 2010).
Verbal WM is important for the encoding, retention, and manipulation of verbal codes used for counting, exact arithmetic, and mathematical algorithms (Dehaene, Piazza, Pinel, & Cohen, 2005). Deficits in verbal WM commonly distinguish children with math difficulties from their typically developing peers (Fuchs et al., 2008; Mabbot & Bisanz, 2008; Swanson & Jerman, 2006). Visual spatial WM may be necessary for the formation of mental models, which may be used by young children to solve mathematical problems, such as nonverbal addition and subtraction (e.g., Bisanz, Sherman, Rasmussen, & Ho, 2005; Huttenlocher, Jordan, & Levine, 1994) and by older children to accomplish more complex mathematical tasks. Verbal WM predicts performance on easier math items, while performance on more difficult items is predicted by visual-spatial WM in school-age children (Holmes & Adams, 2006; Holmes, Adams, & Hamilton, 2008).
Children with TBI are less accurate on verbal WM (e.g., Conklin, Salorio, & Slomine, 2008; Levin et al., 2002, 2004) and visual-spatial WM tasks (Gorman, Barnes, Swank, Prasad, & Ewing-Cobbs, 2011) than typically developing children. Injury severity predicts verbal WM (Levin et al., 2002, 2004; Roncadin, Guger, Archibald, Barnes, & Dennis, 2004); however, no study has examined the contribution of WM impairments to math outcomes in children with TBI such as has been done for some neurogenetic disorders associated with high rates of math difficulties (Mazzocco, Murphy, & McCloskey, 2007).
The Present Study
This study compares mathematical outcomes in children with TBI and orthopedic injury (OI) at 2 and 24 months post-injury in a longitudinal, prospective design. The study is unique in that it investigates whether children with TBI demonstrate difficulties in math fact retrieval speed and accuracy as is seen in children with math disabilities. To replicate and broaden the research on mathematical achievement in children with TBI, we also examined the influence of age and time since injury on standardized measures of calculation, arithmetic fluency, and applied problem solving. Finally, we examine predictors and mediators of math outcomes, including injury severity and WM.
We predicted that (1) math fact speed and retrieval accuracy would not differ significantly in children with TBI and OI; (2) children with TBI would perform less well than orthopedic controls on all standardized measures of math performance at both follow-up intervals; (3) injury severity would predict performance on standardized math tasks; and (4) the effect of group on math difficulties would be mediated by impairments in WM.
METHODS
Participants
In a concurrent cohort-prospective design, children with TBI or OI were recruited from admissions to the Level 1 Pediatric Trauma Center at Children’s Memorial Hermann Hospital, affiliated with the University of Texas Health Science Center at Houston between 2004 and 2009. An OI comparison group, having a skeletal Abbreviated Injury Scale (Association for the Advancement of Automotive Medicine, 1990) score <5, was selected in lieu of a community comparison group to account for potential pre-injury risk factors predisposing children to injury (Fletcher, Ewing-Cobbs, Francis, & Levin, 1995; Taylor et al., 2002).
The sample consisted of 97 children: 47 with orthopedic injuries and 50 with TBI, with mean ages of 10.40 (2.82) and 11.29 (2.86), respectively, at 2 months post-injury. Severity of TBI was characterized by the lowest post-resuscitation Glasgow Coma Scale score (GCS; Teasdale & Jennett, 1974). Moderate and severe TBI were categorized by GCS scores from 9 to 12 and 3 to 8, respectively. Complicated mild TBI was defined by GCS scores from 13 to 15 with acute neuroimaging evidence of extra-axial hemorrhage or parenchymal injury (Levin et al., 2008).
Inclusionary criteria for children with TBI were (a) complicated mild, moderate, or severe TBI resulting from acceleration-deceleration or blunt impact injuries caused by vehicular accidents, falls, or impact with a blunt object; (b) skeletal or body Abbreviated Injury Scale score ≤2 in children with TBI to minimize any confounding influence of severe orthopedic injury on accurate assessment of GCS scores and outcome; (c) no history of previous TBI; (d) bilingual or primarily English-speaking; (e) legal alien status and residing within the 125 mile radius of the catchment area; (f) no known premorbid neurologic, metabolic, major developmental, or psychiatric disorders that would interfere with assessment of the impact of TBI on outcomes The OI group met inclusionary criteria (c) through (f). Additionally, they had to be hospitalized for their injuries and have an absence of facial injuries so as to minimize the possibility of co-occurring mild TBI.
For the TBI group, a total of 97 eligible children were hospitalized. Seventeen did not respond to contact efforts and 18 declined to participate; the primary reasons for refusal were lack of interest, concern about time commitment, and travel factors. Of the 62 patients enrolled in the study, 5 children were so severely injured they could not complete the study measures at the baseline evaluation, 2 did not have IQ information available, 3 were missing data on math outcomes at 2 months post-injury, and 2 were lost to follow-up at 24 months post-injury, resulting in a sample of 50 children with TBI, none of whom received injuries due to child abuse. Of the 253 patients admitted to the hospital for OI, 83 did not respond to contact efforts and 113 did not want to participate, giving similar reasons as the TBI group. From the total 57 patients enrolled, 1 child with suicidality was dropped and 1 child with severe dyslexia was erroneously dropped, resulting in a sample of 47 children with OI.
Demographic and injury data are presented in Table 1. Age at injury, gender, ethnicity, and the Hollingshead Index (Hollingshead, 1975) of socioeconomic status did not differ across the TBI and OI groups. Depth and duration of impaired consciousness were assessed using the lowest post-resuscitation GCS score and the duration of impaired consciousness, defined as the number of days that a child was unable to follow one-stage commands.
Table 1.
Demographic and neurologic data by group
| TBI | Control | |
|---|---|---|
| Age at injury (years) | ||
| M (SD) | 11.05 (2.84) | 10.20 (2.81) |
| Gender (% Male) | 74.0 | 57.4 |
| Ethnicity (%) | ||
| African American | 13.2 | 18.5 |
| Asian | 3.8 | 5.6 |
| Caucasian | 47.2 | 42.6 |
| Hispanic | 32.1 | 29.6 |
| Other | 3.8 | 3.8 |
| Socioeconomic status | ||
| M (SD) | 47.74 (11.36) | 46.53 (9.27) |
| WASI* | ||
| M (SD) | 101.47 (14.94) | 109.02 (13.26) |
| Days of impaired consciousness | ||
| M (SD) | 6.37 (8.80) | – |
| Glasgow Coma Scale score (%) | ||
| 3 – 8 | 72.0 | – |
| 9 – 12 | 22.0 | – |
| 13 – 15 | 6.0 | – |
Note.
Denotes a group difference and the superscripts specify the difference.
WASI =Wechsler Abbreviated Scales of Intelligence.
All children had an IQ of 70 or greater as estimated by the Wechsler Abbreviated Scales of Intelligence (WASI) Vocabulary and Matrix Reasoning subtests. Both groups had mean IQ scores within the Average range; however, the OI group had a higher mean IQ score than the TBI group. The two groups did not differ on pre-injury scores of inattention (M =4.19; SD =6.22 for OI group; M =1.89; SD =8.36 for TBI group; F(1,84) =1.60, ns) or hyperactivity (M =2.60; SD =5.57 for OI group; M =1.68; SD =7.42 for TBI group; F(1,84) <1, ns) as assessed by The SWAN Rating Scale for ADHD.
Measures
Cognitive addition
This task consisted of 6 practice trials and 36 experimental trials of single-digit addition equations, with an equal number of true (e.g., 9 +2 =11) and false (e.g., 9 +4 =12) equations. Problems included addends ranging from 1 to 9, excluding problems containing 0 and ties (e.g., 2 +2, 5 +5). True equations consisted of nine small-size problems (i.e., having a sum less than 10) and nine large-size problems (i.e., having a sum of 10 or greater). False equations consisted of 8 small problems and 10 large problems. The sums of the false equations deviated from the true sum by ±1, 2, or 3 (see Menon, Mackenzie, Rivera, & Reiss, 2002 for a similar paradigm).
In verification tasks, it is assumed that the operand encoding processes result in the activation of candidate answers (Ashcraft, 1992). Response times for true equations (e.g., 3 +4 =7), which involve stronger operand-correct answer associations, are shorter than those for false problems (3 +4 =8). As well, small problems are more quickly verified than large problems because the memory trace for large problem/answer associations is weaker than that for more frequently encountered small problem/answer associations.
Equations were presented on a Dell Inspiron 600 m laptop in a horizontal orientation (e.g., 3 +4 =7) using E-Prime version 1.1. Children were seated in front of the laptop approximately 20 inches from the screen. Each trial began with the presentation of a fixation point (*) for 1000 ms followed by a blank screen for 250 ms and then a single digit arithmetic equation, terminating when a response was recorded. Children indicated whether or not equations were true or false by making keyboard presses of ‘d’ or ‘l’, respectively. Accuracy and response times were recorded. Children were instructed to answer as quickly and accurately as possible. A test–retest correlation run on the OI group for response times was moderate-high at r =.86, which is quite high considering that measurements were nearly 2 years apart.
Standardized math measures
The Woodcock-Johnson: Tests of Achievement, Third Edition (Woodcock, McGrew, & Mather, 2001) Calculation and Applied Problems subtests were administered at both 2 and 24 months post-injury; Math Fluency was given only at the 2 month assessment. Subtests yielded age-based standard scores.
Applied problems
Word problems were presented in written format and were also read by the examiner. Test–retest reliabilities range from .85 to .92.
Calculation
Written problems ranged from single-digit arithmetic to multi-digit arithmetic and calculus. Test–retest reliabilities range from .76 to .87.
Math fluency
Children are required to write answers for single-digit interspersed addition, subtraction, and multiplication problems in a three-minute time period. Test–retest reliabilities range from .75 to .92.
Working memory tasks
The Category Listening Span (CLS) task assesses verbal WM (see Gorman et al., 2011 for task details). This task is composed of five levels of one, two, three, four, or five strings of three words with the number of word strings corresponding to a particular WM span. Each level has two trials, for a total of 10 trials. The child is asked to recall the last word in each string, in order, at the end of the trial. For example, in a two span trial, if the first word string is “pill, lock, water” and the next is “chin, wool, rice” recalling “water” and “rice” in that order would be correct. The task was discontinued when both trials at a span level were incorrect. Basal was established as the lowest level at which both trials were correct. Total number correct was recorded. The test–retest correlation was r =.60 for the orthopedic control group.
The Visual-Spatial Span (VSS; Cornoldi et al., 2001) task was created with the same processing demands as the CLS to directly compare verbal and visual-spatial WM. The experimenter touches three contiguous positions in a four by four matrix of small square blocks. The VSS is composed of five levels of one, two, three, four, or five strings of three blocks with the number of strings corresponding to a particular WM span. Each level consists of two trials, for a total of 10 trials. The child recalls the location of the last block touched in each string, in order at the end of each trial. The same basal and discontinue rules from the CLS were applied to VSS. Total number correct was recorded. The test–retest correlation was r =.53 for the orthopedic control group.
Procedure
For children meeting the study criteria outlined above, informed written consent was obtained from the child’s guardian. In accordance with guidelines established by the Institutional Review Board at the University of Texas Health Science Center-Houston, oral assent was obtained from children ages 6–7 and written consent was obtained from children ages 8–15. Each child was evaluated individually by a trained examiner in an outpatient clinic setting at 2, 6, 12, and 24 months post-injury. The current study presents data collected at the 2 and 24 month post-injury time points.
Statistical Analysis
Data cleaning procedures were used for the cognitive addition task. For response time analyses, only correct trial latencies were included. Median response times were calculated for each problem set. Participants achieving 50% accuracy or greater for all problem sets were included in response time analyses to ensure that median response times were based on a sufficient number of observations. Both accuracy and response time data were skewed, so a log transformation was computed.
The 2 Group (TBI vs. OI) ×2 Time (2 months vs. 24 months) ×2 Problem Type (incorrect vs. correct) ×2 Problem Size (small vs. large) repeated measures analyses of covariance (ANCOVA) were performed on accuracy and response time data, covarying age at test, to investigate the effect of group and the interaction between group and time post-injury on cognitive addition.
To determine whether there were group differences on the standardized math tasks, 2 Group ×2 Time mixed ANOVAs with repeated measures on the last factor were conducted for Math Calculation and Applied Problems. For Math Fluency, administered only at 2 months post-injury, a univariate ANOVA was run. Age at assessment was not entered as a covariate because standard scores were used.
To examine demographic and injury severity predictors of math outcomes at 2 and 24 months post-injury among children with TBI, mixed model hierarchical regressions were conducted. In the first step, demographic variables assessed the relation of age, gender, and socioeconomic status to math outcomes. In the second step, duration of impaired consciousness evaluated whether injury severity contributed to the prediction of outcomes over and above the demographic variables.
To examine group differences on WM variables, one-way between-subject ANCOVAs were conducted covarying for age at assessment at 24 months post-injury. Lastly, mediation analyses were conducted to examine concurrent WM as a potential mediator of the effect of group (TBI and OI) on math tasks for which there were group differences. Models covaried for age at assessment because raw scores were used. Following the recommendations of Hayes (2009), a bootstrapping sampling procedure was applied for assessing the indirect effect. Bootstrapping is a nonparametric resampling procedure where a large number of samples (5000 in the current study) are drawn with replacement from the full data set. Based on these samples, approximations of the distribution of the indirect effect are obtained and a point estimate and confidence interval calculated. The bootstrapping procedure is superior to other approaches to mediation in terms of statistical power while maintaining reasonable control over the Type I error rate (Hayes, 2009). The bootstrapping procedure was conducted using the SPSS macro provided by Preacher and Hayes (2008). The point estimate for an indirect effect was considered significant when the bias corrected and accelerated (BCa) confidence interval did not include zero.
RESULTS
Group Comparisons
Cognitive addition task
For accuracy, group interacted with time, F(1,92) =4.15, p <.05, η2 =.04; the pattern of findings suggested some improvement in scores over time for the TBI group (89% to 91%) while the OI group remained stable (89%); however, tests of simple main effects were not significant. For response time analyses, there was no main effect of group and group did not interact with time or task variables. Mean accuracies, latencies, and standard deviations are in Table 2.
Table 2.
Accuracy and response time for entire sample
| Problem type | 2 Months
|
24 Months
|
||
|---|---|---|---|---|
| TBI M (SD) |
Control M (SD) |
TBI M (SD) |
Control M (SD) |
|
| Accuracy (% correct) | ||||
| Incorrect small | 94.10 (11.13) | 93.16 (9.98) | 95.59 (8.60) | 92.50 (11.74) |
| Correct small | 93.08 (11.98) | 94.34 (10.36) | 94.61 (7.61) | 93.90 (9.83) |
| Incorrect large | 84.53 (16.82) | 85.85 (14.60) | 87.88 (12.68) | 86.46 (13.52) |
| Correct large | 83.23 (18.95) | 82.81 (20.04) | 85.40 (15.79) | 82.97 (16.85) |
| Median response time (ms) | ||||
| Incorrect small | 2417.51 (1329.09) | 2952.69 (2154.41) | 2001.89 (1296.47) | 1901.64 (825.38) |
| Correct small | 1944.85 (1061.42) | 2306.57 (1853.01) | 1754.77 (1369.45) | 1629.72 (679.11) |
| Incorrect large | 3600.80 (3023.92) | 4014.42 (3126.12) | 2744.56 (1988.16) | 2699.31 (1544.55) |
| Correct large | 3543.06 (2763.60) | 4681.78 (4706.69) | 2914.96 (2220.83) | 2798.63 (1846.05) |
Note. Group differences were not significant for accuracy or response time data.
Standardized math outcomes
For Math Calculation and Applied Problems, there was a main effect of group; the OI group outperformed the TBI group, F(1,95) =13.26, p <.001, η2 =.12; F(1,95) =10.78, p =.001, η2 =.10, respectively. For Math fluency the OI group outperformed the TBI group, F(1,101) =7.97, p <.01, η2 =.07. Means are in Table 3.
Table 3.
Achievement and cognitive data by group
| 2 Months
|
24 Months
|
|||
|---|---|---|---|---|
| TBI | Control | TBI | Control | |
| Applied problems* | 102.10 (13.12) | 110.81 (12.03) | 102.94 (13.39) | 110.15 (11.84) |
| Calculations* | 99.12 (14.72) | 108.85 (10.76) | 100.32 (14.10) | 107.83 (10.18) |
| Math fluency* | 88.62 (20.76) | 98.19 (12.98) | – | – |
| Verbal WM* | – | – | 11.22 (3.94) | 12.69 (4.01) |
| Visual-Spatial WM | – | – | 13.05 (3.92) | 13.59 (3.79) |
Note.
Denotes tasks on which significant group differences were found.
To assess whether the effect of group on higher order math tasks was due to differences in arithmetic ability, one-way ANCOVAs were run, examining group differences on Calculation and Applied Problems covarying for Math Fluency at 2 months post-injury. The OI group outperformed the TBI group on both Calculation, F(1,100) =5.94, p <.05, η2 =.06, and Applied Problems, F(1,100) =5.84, p <.05, η2 =.06, even after controlling for efficiency of single-digit arithmetic.
Demographic and Injury Severity Correlates of Math Outcomes at 2 and 24 Months Post-Injury
Zero-order correlations among math measures, demographic variables, and injury severity predictors are in Table 4. For accuracy on correct equations, the demographic variables accounted for significant variance at 2 months, F(3,45) =5.09, p <.01, R2 =.25, and 24 months, F(3,45) =5.14, p <.01, R2 =.26, post-injury with age at injury emerging as a significant predictor, F(1,45) =14.42, p <.001. Duration of impaired consciousness did not account for additional unique variance at either 2 or 24 months post-injury, F(1,44) <1, ns, ΔR2 =.01; F(1,44) <1, ns, ΔR2 =.001. For incorrect equations, demographic variables accounted for significant variance at 2 months, F(3,45) =3.66, p <.05, R2 =.20, but not 24 months post-injury, F(3,45) <1, ns. Duration of impaired consciousness did not account for additional unique variance at either time point, F(1,44) <1, ns, ΔR2 =.002; F(1,44) =1.13, ns, ΔR2 =.02, respectively.
Table 4.
Demographic and Injury Severity Correlates of Math Outcomes at 24 Months Post-Injury among Children with TBI
| Applied problems | Calculations | Accuracy
|
Response time
|
|||
|---|---|---|---|---|---|---|
| Incorrect | Correct | Incorrect | Correct | |||
| Age | .62** | .69** | −.10 | .38** | −.51** | −.44** |
| Gender | −.12 | −.12 | .05 | .26* | .24 | .25* |
| Socioeconomic status | .40** | .31* | −.01 | .26* | −.28* | −.27* |
| Impaired consciousness | −.24* | −.22 | .16 | .10 | .47** | .47** |
Note.
p <.05;
p <.01
For response time data, the demographic variables accounted for significant variance in performance on correct equations at 2 months, F(3,45) =4.73, p <.01, R2 =.24, and 24 months post-injury, F(3,45) =8.16, p <.001, R2 =.35. Age at injury was the only significant predictor across time, F(1,45) =23.07, p <.001. Duration of impaired consciousness accounted for additional variance when added to the model at 24 months, F(1,44) =13.61, p =.001, ΔR2 =.15, but not 2 months post-injury, F(1,44) =2.79, ns, ΔR2 =.05. For incorrect equations, demographic variables accounted for significant variance in performance at 2 months, F(3,45) =3.84, p <.05, R2 =.20, and 24 months, F(3,45) =9.75, p <.001, R2 =.39, post-injury, with age at injury emerging as the only significant predictor, F(1,45) =19.75, p <.001. Duration of impaired consciousness accounted for unique variance when added to the model at both time points, F(1,44) =4.98, p <.05, ΔR2 =.08; F(1,44) =13.88, p =.001, ΔR2 =.14.
For Calculation, the demographic variables accounted for significant variance in performance at 2 months, F(3,45) =3.48, p <.05, R2 =.19, and 24 months, F(3,45) =4.61, p <.01, R2 =.24, post-injury, with socioeconomic status being the only significant predictor across time, F(1,45) =9.80, p <.01. Duration of impaired consciousness accounted for additional unique variance at 2 and 24 months post-injury, F(1,44) =6.70, p <.05, ΔR2 =.11; F(1,44) =5.98, p <05, ΔR2 =.09.
Demographic variables accounted for significant variance in performance of Applied Problems at 2 months, F(3,45) =7.44, p <.001, R2 =.33, and 24 months, F(3,45) =10.66, p <.001, R2 =.42 post-injury, with age at injury, F(1,45) =9.54, p <.01, and socioeconomic status, F(1,45) =19.87, p <.001, being significant predictors. Duration of impaired consciousness accounted for unique variance at both time points, F(1,44) =13.77, p =.001. ΔR2 =.16; F(1,44) =4.16, p <.05, ΔR2 =.05.
For Math Fluency, demographic variables accounted for significant variance, F(3,42) =5.97, p <.01, R2 =.30, with gender being a significant predictor, t =−2.97, p <.01; duration of impaired consciousness accounted for unique variance, F(1,41) =13. 42, p =.001, ΔR2 =.17.
Verbal Working Memory as a Mediator of the Effect of Group on Math Outcomes
Children with TBI performed significantly worse than the OI group on the verbal WM task, CLS, F(1,93) =11.60, p =.001, η2 =.11. In contrast, the groups did not significantly differ on visual-spatial WM, F(1,84) =3.74, p =.057, η2 =.04. As such, mediation models were run to determine whether CLS mediated the relation of group with math outcomes.
Mediation analysis showed that the total effect of group on Math Calculation was significant when CLS was absent from the model; however, when verbal WM was included in the model, the direct effect was no longer significant (see Figure 1). Group had a significant indirect effect on Math Calculation through its effect on verbal WM with a point estimate of 1.346, and a 95% BCa bootstrap CI of −2.62 to −.57.
Fig. 1.
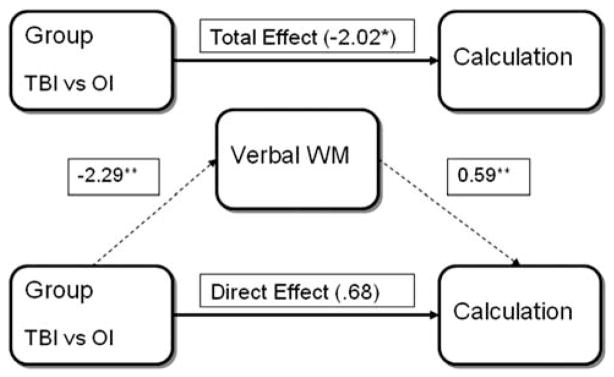
The effect of injury group on calculation performance was mediated through the effect of traumatic brain injury (TBI) on working memory. *p <.05; **p <.01.
For Applied Problems, the total effect of group was significant when CLS was not in the model. However, with the addition of CLS, the direct effect of group on Applied Problems was not significant (See Figure 2). Thus, group had a significant indirect effect on Applied Problems through its effect on verbal WM with a point estimate of −1.96 and a 95% BCa bootstrap CI of −3.66 to −.81.
Fig. 2.
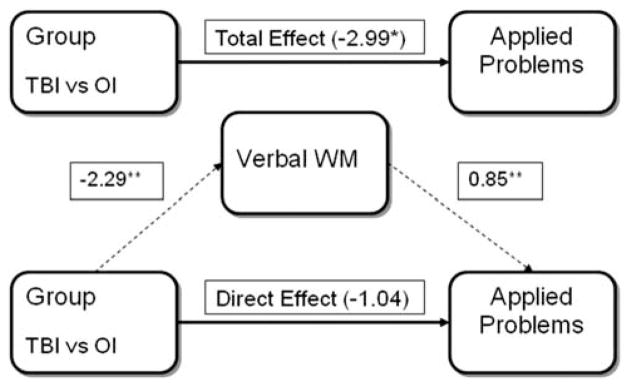
The effect of injury group on applied problems was mediated through the effect of traumatic brain injury (TBI) on working memory. *p <.05; **p <.01.
DISCUSSION
The primary aim of this study was to determine if children with TBI showed deficits in math fact retrieval, a foundational mathematical skill commonly disrupted in children with math disability. Compared to children with OI, those with TBI did not demonstrate deficits in accuracy or speed of math fact retrieval on a cognitive addition task. Furthermore, even though the groups did not differ on accuracy at either time point, children with TBI demonstrated improvement over time. These findings suggest that the math difficulties commonly observed in children with TBI are not due to a primary deficit in math fact retrieval even when efficiency of retrieval is considered.
The Effect of TBI on Achievement in Mathematics
A second aim of the study was to examine the performance of children with TBI and typically achieving peers over time on a larger variety of standardized math tasks than is typically reported. Children with TBI performed less well than typically developing peers on all math achievement measures assessed at 2 months and 24 months post-injury. Performance was stable over time, indicating that math performance in children with TBI did not catch up to performance of comparison children.
Children with TBI were less skilled than controls on a measure of math fluency at 2 months post-injury. Given that severe TBI significantly affects processing speed (Donders & Janke, 2008; Murray, Shum, & McFarland, 1992), it is perhaps not surprising that children with TBI in this study, many of whom had severe injuries, performed less well than peers on a test of math fluency. In addition to the processing speed demands of this task, there may also be other cognitive and motor demands as children must switch among operations of addition, subtraction, and multiplication, inhibit competing responses, and write down their answers. Children with TBI have difficulty with visual-motor integration and speeded motor output (Thompson et al., 1994), which may reduce performance on tasks with written output. These additional motor and executive demands may account for why children with TBI performed more poorly than controls on math fluency but not on cognitive addition.
Children with TBI were also less skilled than their typically developing peers on an untimed measure of math computations involving single and multi-digit calculation at both assessment points. Inconsistent findings have been reported for math computations in children, with some studies reporting recovery of computations into the average range (e.g., Ayr et al., 2005) and others demonstrating lower scores in children sustaining TBI in the preschool years (Ewing-Cobbs et al., 2006) or during middle childhood or adolescence (e.g., Ewing-Cobbs, Levin, et al., 1998; Taylor et al., 2002). These variable findings may be due to injury-related factors such as the proportion of severely injured children to less severely injured children in the sample (there was a large proportion of severely injured children in the present study).
Of particular interest, while children with TBI performed less well than the OI group on standardized math measures, their scores fell in the low average to average range on all tasks. As a group, children with TBI did not have, what may be generally regarded, as math disability. However, among children with TBI, average performance on achievement measures does not necessarily translate to average academic performance in the classroom (Ewing-Cobbs, Levin, et al., 1998).
The Relation of Demographic Variables and Injury Severity to Mathematical Performance
Younger children had lower scores than older children on the age-standardized measures of word problem solving. This is consistent with the finding that younger age at injury may represent a vulnerability factor for some cognitive outcomes (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2005), particularly skills that are developing rapidly at the time of injury (Barnes et al., 1999; Ewing-Cobbs et al., 2004). Gender was related to math fluency performance, with females scoring higher. Socioeconomic status was positively related to calculation and applied problem scores. After controlling for demographic factors, longer duration of impaired consciousness significantly predicted poorer performance on standardized math outcomes and longer response time on the cognitive addition task. Changes in these aspects of mathematics may be mediated in part by deficits in processing speed, language, and executive functions, which are affected by severity of TBI.
Working Memory and its Relation to Math Outcomes
Of particular interest is that when efficiency of single-digit arithmetic (i.e., Math Fluency) was controlled for, the group differences in math computations and applied problem solving remained, suggesting that the difficulties experienced by children with TBI in math are not simply due to difficulties in basic arithmetic and speed on paper-pencil tasks. The mediation analysis suggests that differences in performance of the TBI and OI groups are related to difficulties in WM, which is affected by TBI (e.g., Gorman et al., 2011; Levin et al., 2002, 2004; Roncadin et al., 2004), and which is implicated in mathematical learning and performance more generally (e.g., Fuchs et al., 2006, 2008; Raghubar et al., 2010). Consistent with our hypotheses, verbal WM mediated the effect of group on math achievement, suggesting children with TBI have difficulty in calculation and applied problem solving that are related to weaknesses in verbal WM rather than to a disruption in foundational arithmetic skills per se.
This study is the first to consider cognitive processes as potential mediators of group differences on mathematical outcomes in TBI. Ewing-Cobbs et al. (2004) reported that visual memory and visual motor integration, but not verbal WM (digits backwards), predicted calculation scores 2 years after TBI. Ayr et al. (2005) found relations between performance on standardized and experimental calculation tasks and measures of planning, digit span, and arithmetic (from the WISC-III), declarative memory, and processing speed; however, these cognitive measures did not account for unique variance in math calculations for the TBI group. The importance of verbal WM to math outcomes in the present study compared to previous studies may be due to the complexity of the task. Compared to studies using simple span tasks that require maintenance of information in WM, the specific requirement for updating information in the CLS task may be more strongly related to mathematical outcomes. Additional research examining variables that may mediate or moderate the influence of brain injury on mathematical outcomes is needed.
LIMITATIONS AND CONCLUSIONS
One limitation of the study is that strategy data were not collected for cognitive addition. Although response times were short, suggesting that math fact retrieval rather than laborious strategies (e.g., finger counting) was used on most trials, whether answers were retrieved from memory for each problem cannot be verified.
Second, it was not possible to examine differences between participants and non-participants who fit inclusion criteria due to ethical requirements. Third, due to small sample size, the present study did not examine differences among groups with mild, moderate, and severe TBI. Differences between studies in the proportion of children with severe injuries could account for some of the variable findings in the literature for mathematical outcomes after childhood TBI. However, our enrollment accurately reflects the severity of children seen in the emergency department and subsequently hospitalized for TBI at our Level 1 Trauma Center (3.2% moderate and 15% severe TBI).
Studies investigating the contribution of supporting cognitive abilities to school difficulties experienced by these children may have practical significance for understanding academic achievement and identifying intervention targets (Holmes, Gathercole, & Dunning, 2009). Knowing that WM may be one source of math difficulties for children with TBI suggests potential accommodations and scaffolding that might be needed during instruction, practice, and application of mathematical skills. WM and some aspects of attention can be enhanced following intensive adaptive WM training (e.g., Holmes et al., 2009; Klingberg et al., 2005); however, evidence for the generalization of such effects to academic achievement remains sparse (Chein & Morrison, 2010; Melby-Lervåg & Hulme, 2012), and the efficacy of such approaches for children with TBI is unknown.
Acknowledgments
This publication was supported by Grant Number R01 NS046308 from the National Institute of Neurological Disorders and Stroke.
Footnotes
The authors report no conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
References
- Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116(6):1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- Ashcraft M. Cognitive arithmetic: A review of data and theory. Cognition. 1992;44:75–106. doi: 10.1016/0010-0277(92)90051-i. [DOI] [PubMed] [Google Scholar]
- Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale. Des Plaines, IL: Association for the Advancement of Automotive Medicine; 1990. (1990 revision) [Google Scholar]
- Ayr LK, Yeates KO, Enrile BG. Arithmetic skills and their cognitive correlates in children with acquired and congenital brain disorder. Journal of the International Neuropsychological Society. 2005;11:249–262. doi: 10.1017/S1355617705050307. [DOI] [PubMed] [Google Scholar]
- Baddeley AD, Logie RH. Working memory: The multiple-component model. In: Miyake A, Shah P, editors. Models of working memory: Mechanisms of active maintenance and executive control. Cambridge: Cambridge University Press; 1999. pp. 28–61. [Google Scholar]
- Barnes MA, Dennis M, Wilkinson M. Reading after closed brain injury in childhood: Effects on accuracy, fluency, and comprehension. Developmental Neuropsychology. 1999;15:1–24. [Google Scholar]
- Barnes MA, Fletcher JM, Ewing-Cobbs L. Mathematical disabilities in congenital and acquired neurodevelopmental disorders. In: Berch DB, Mazzocco MM, editors. Why is math so hard for some children? The nature and origins of mathematical learning difficulties and disabilities. Baltimore, MD: Paul H. Brookes Publishing Co; 2007. pp. 195–217. [Google Scholar]
- Barnes MA, Wilkinson M, Khemani E, Boudesquie A, Dennis M, Fletcher JM. Arithmetic processing in children with spina bifida: Calculation accuracy, strategy use, and fact retrieval fluency. Journal of Learning Disabilities. 2006;39:174–187. doi: 10.1177/00222194060390020601. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Haslum M, Golding J. Cognitive and behavioral sequelae of mild head injury in children. Pediatrics. 1990;86:337–344. [PubMed] [Google Scholar]
- Bisanz J, Sherman JL, Rasmussen C, Ho E. Development of arithmetic skills and knowledge in preschool children. In: Campbell JID, editor. Handbook of mathematical cognition. New York: Psychology Press; 2005. pp. 143–162. [Google Scholar]
- Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI) Journal of Pediatric Psychology. 2008;33:707–718. doi: 10.1093/jpepsy/jsn006. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson VA, Muscara F, Morse SA, Haritou F, Rosenfeld JV, Heinrich LM. Educational skills: Long-term outcome predictors following paediatric traumatic brain injury. Neuropsychological Rehabilitation. 2009;19:716–732. doi: 10.1080/09602010902732868. [DOI] [PubMed] [Google Scholar]
- Chadwick O, Rutter M, Shaffer D, Shrout PE. A prospective study of children with head injuries: Specific cognitive difficulties. Journal of Clinical Neuropsychology. 1981;3:101–120. doi: 10.1080/01688638108403117. [DOI] [PubMed] [Google Scholar]
- Chein JM, Morrison AB. Expanding the mind’s workspace: Training and transfer effects with a complex working memory span task. Psychonomic Bulletin & Review. 2010;17:193–199. doi: 10.3758/PBR.17.2.193. [DOI] [PubMed] [Google Scholar]
- Conklin HM, Salorio CF, Slomine BS. Working memory performance following paediatric traumatic brain injury. Brain Injury. 2008;22:847–857. doi: 10.1080/02699050802403565. [DOI] [PubMed] [Google Scholar]
- Cornoldi C, Marzocchi GM, Belotti M, Caroli MG, De Meo T, Braga C. Working memory interference control deficit in children referred by teachers for ADHD symptoms. Child Neuropsychology. 2001;7:230–240. doi: 10.1076/chin.7.4.230.8735. [DOI] [PubMed] [Google Scholar]
- Dehaene S, Piazza M, Pinel P, Cohen L. Three parietal circuits for number processing. In: Campbell JID, editor. Handbook of mathematical cognition. New York: Psychology Press; 2005. pp. 433–453. [Google Scholar]
- Donders J, Janke K. Criterion validity of the Wechsler Intelligence Scale for Children – Fourth Edition after pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2008;14:651–655. doi: 10.1017/S1355617708080752. [DOI] [PubMed] [Google Scholar]
- Espy KA, McDiarmid MM, Cwik MF, Stalets MM, Hamby A, Senn TE. The contribution of executive functions to emergent mathematical skills in preschool children. Developmental Neuropsychology. 2004;26:465–486. doi: 10.1207/s15326942dn2601_6. [DOI] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Barnes MA, Fletcher JM, Levin HS, Swank PR, Song J. Modeling of longitudinal academic achievement scores after pediatric traumatic brain injury. Developmental Neuropsychology. 2004;25:107–134. doi: 10.1080/87565641.2004.9651924. [DOI] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Levin HS, Fletcher JM, Iovino I, Miner ME. Academic achievement and academic placement following traumatic brain injury in children and adolescents: A two-year longitudinal study. Journal of Clinical and Experimental Neuropsychology. 1998;20:769–781. doi: 10.1076/jcen.20.6.769.1109. [DOI] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad M, Fletcher JM, Levin HS, Miner ME, Eisenberg HM. Attention after pediatric traumatic brain injury: A multidimensional assessment. Child Neuropsychology. 1998;4:35–48. [Google Scholar]
- Ewing-Cobbs L, Prasad M, Kramer L, Cox C, Baumgartner J, Fletcher S, Swank P. Late intellectual and academic outcomes following traumatic brain injury sustained during early childhood. Journal of Neurosurgery. 2006;105(Suppl 4):287–296. doi: 10.3171/ped.2006.105.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM. Outcome of pediatric traumatic brain injury at three years: A cohort study. Archives of Physical Medicine and Rehabilitation. 1994;75:733–741. [PubMed] [Google Scholar]
- Fletcher JM, Ewing-Cobbs L, Francis DJ, Levin HS. Variability in outcomes after traumatic brain injury in children: A developmental perspective. In: Broman SH, Michel ME, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 3–21. [Google Scholar]
- Fuchs LS, Fuchs D, Compton DL, Powell SR, Seethaler PM, Capizzi AM, Fletcher JM. The cognitive correlates of third-grade skill in arithmetic, algorithmic computation, and arithmetic word problems. Journal of Educational Psychology. 2006;98:29–43. [Google Scholar]
- Fuchs LS, Fuchs D, Stuebing K, Fletcher JM, Hamlett CL, Lambert W. Problem solving and computational skill: Are they shared or distinct aspects of mathematical cognition? Journal of Educational Psychology. 2008;100:30–47. doi: 10.1037/0022-0663.100.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geary DC. A componential analysis of an early learning deficit in mathematics. Journal of Experimental Child Psychology. 1990;49:363–383. doi: 10.1016/0022-0965(90)90065-g. [DOI] [PubMed] [Google Scholar]
- Geary DC, Fan L, Bow-Thomas CC. Numerical cognition: Loci of ability differences comparing children from China and the United States. Psychological Science. 1992;3:180–185. [Google Scholar]
- Gorman S, Barnes MA, Swank P, Prasad M, Ewing-Cobbs L. The effects of pediatric traumatic brain injury on verbal and visual-spatial working memory. Journal of the International Neuropsychological Society. 2011;17:1–10. doi: 10.1017/S1355617711001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanich LB, Jordan NC, Kaplan D, Dick J. Performance across different areas of mathematical cognition in children learning difficulties. Journal of Educational Psychology. 2001;93:615–626. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Hecht SA, Torgesen JK, Wagner RK, Rashotte CA. The relations between phonological processing abilities and emerging individual differences in mathematical computation skills: A longitudinal study from second to fifth grades. Journal of Experimental Child Psychology. 2001;79:192–227. doi: 10.1006/jecp.2000.2586. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. Unpublished manuscript. Yale University; 1975. Four factor index of social status. [Google Scholar]
- Holmes J, Adams JW. Working memory and children’s mathematical skills: Implications for mathematical development and mathematical curricula. Educational Psychology. 2006;26:339–366. [Google Scholar]
- Holmes J, Adams JW, Hamilton CJ. The relationship between visuospatial sketchpad capacity and children’s mathematical skills. European Journal of Cognitive Psychology. 2008;20:272–289. [Google Scholar]
- Holmes J, Gathercole SE, Dunning DL. Adaptive training leads to sustained enhancement of poor working memory in children. Developmental Science. 2009;12:F9–F15. doi: 10.1111/j.1467-7687.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- Huttenlocher J, Jordan NC, Levine SC. A mental model for early arithmetic. Journal of Experimental Psychology: General. 1994;123:284–296. doi: 10.1037//0096-3445.123.3.284. [DOI] [PubMed] [Google Scholar]
- Jaffe KM, Fay GC, Polissar NL, Martin KM, Shurtleff H, Rivara JB, Winn HR. Severity of pediatric traumatic brain injury and early neurobehavioral outcome: A cohort study. Archives of Physical Medicine and Rehabilitation. 1992;73:540–547. [PubMed] [Google Scholar]
- Kinsella G, Prior M, Sawyer M, Murtagh D, Eisenmajer R, Anderson V, Klug G. Neuropsychological deficit and academic performance in children and adolescents following traumatic brain injury. Journal of Pediatric Psychology. 1995;20:753–767. doi: 10.1093/jpepsy/20.6.753. [DOI] [PubMed] [Google Scholar]
- Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlstrom K, Westerberg H. Computerized training of working memory in children with ADHD – A randomized, controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:177–186. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2004. [Google Scholar]
- Levin HS, Hanten G, Chang C, Zhang L, Schachar R, Ewing-Cobbs L, Max JE. Working memory after traumatic brain injury in children. Annals of Neurology. 2002;52:82–88. doi: 10.1002/ana.10252. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, Swank P. Predictors of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. Journal of Neurosurgery. 2008;1:461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Zhang L, Dennis M, Barnes MA, Schachar R, Hunter JV. Changes in working memory after traumatic brain injury in children. Neuropsychology. 2004;18:240–247. doi: 10.1037/0894-4105.18.2.240. [DOI] [PubMed] [Google Scholar]
- Mabbot DJ, Bisanz J. Computational skills, working memory, and conceptual knowledge in older children with mathematics learning disabilities. Journal of Learning Disabilities. 2008;41:15–28. doi: 10.1177/0022219407311003. [DOI] [PubMed] [Google Scholar]
- Mazzocco MMM, Murphy MM, McCloskey M. The contribution of syndrome research to understanding mathematical learning disability. In: Berch D, Mazzocco MMM, editors. Why is math so hard for some children? The nature and origins of mathematical learning difficulties and disabilities. Baltimore, MD: Paul H. Brookes Publishing; 2007. pp. 173–193. [Google Scholar]
- Melby-Lervåg M, Hulme C. Is working memory training effective? A meta-analytic review. Developmental Psychology. 2012 doi: 10.1037/a0028228. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Menon V, Mackenzie K, Rivera SM, Reiss AL. Prefrontal cortex involvement in processing incorrect arithmetic equations: Evidence from event-related fMRI. Human Brain Mapping. 2002;16:119–130. doi: 10.1002/hbm.10035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray R, Shum D, McFarland K. Attentional deficits in head-injured children: An information processing analysis. Brain and Cognition. 1992;18:99–115. doi: 10.1016/0278-2626(92)90072-t. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Raghubar KP, Barnes MA, Hecht SA. Working memory and mathematics: A review of developmental, individual difference, and cognitive approaches. Journal of Individual Differences. 2010;20:110–122. [Google Scholar]
- Rivera-Batiz FL. Quantitative literacy and the likelihood of employment among young adults in the United States. The Journal of Human Resources. 1992;27:313–328. [Google Scholar]
- Roncadin C, Guger S, Archibald J, Barnes M, Dennis M. Working memory after mild, moderate, or severe childhood closed head injury. Developmental Neuropsychology. 2004;25:21–36. doi: 10.1080/87565641.2004.9651920. [DOI] [PubMed] [Google Scholar]
- Swanson HL, Jerman O. Math disabilities: A selective meta-analysis of the literature. Review of Educational Research. 2006;76:249–274. [Google Scholar]
- Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: Post-acute effects on cognitive and school readiness skills. Journal of the International Neuropsychological Society. 2008;14:734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Klein S. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Thompson NM, Francis DJ, Stuebing KK, Fletcher JM, Ewing-Cobbs L, Miner ME, Eisenberg HM. Motor, visual-spatial, and somatosensory skills after closed head injury in children and adolescents: A study of change. Neuropsychology. 1994;8:333–342. [Google Scholar]
- Woodcock RW, McGrew KS, Mather N. Woodcock-Johnson Psychoeducational Battery. 3. Itasca, IL: Riverside Publishing; 2001. [Google Scholar]


