Abstract
Background
An excess of weight including obesity have reached epidemic rates in all age groups, both in developed and developing countries. It is notable that overweight children and adolescents have a higher likelihood of becoming obese adults and to present health-related problems early in life.
Objetives
To verify associations of the lipid and hematological profiles with adiposity in obese adolescents beginning multidisciplinary weight loss therapy.
Methods
This cross-sectional study was conducted with 85 adolescents of both genders, aged 12-19 years (Tanner staging 3 or 4) and body mass index greater than the 95th percentile. The sum of the triceps, subscapular and calf skinfolds and the waist circumference were used to estimate adiposity. Blood samples were collected from all patients after overnight fasting to analyze blood lipids (total cholesterol, high-density lipoprotein, low-density lipoprotein, very low-density lipoprotein and triglycerides), blood sugar and the hematological profile (hemoglobin, platelets and red blood cells). The Kolmogorov-Smirnov test and Spearman and Pearson correlation coefficients were used for statistical analysis with significance set for p-values ≤ 0.05.
Results
There were statistical differences between genders for red blood cells (p-value = 0.000), hemoglobin (p-value = 0.000) and platelets (p-value = 0.002). Positive correlations were found for red blood cells (p-value = 0.031) and hemoglobin (p-value = 0.024) with waist circumference. There was a negative correlation between hemoglobin and the sum of skinfolds (p-value = 0.022).
Conclusion
The results demonstrate an association between the lipid and hematological profiles and body adiposity in obese adolescents thus reinforcing the importance of treating obese adolescents early to prevent health related problems in adult life.
Keywords: Lipid metabolism disorders, Body mass index, Hematologic tests, Adiposity, Nutrition disorders/epidemiology, Obesity/epidemiology, Lipoproteins, HDL/blood, Triglycerides/blood, Cross-sectional studies, Humans, Adolescent, Female, Male
Introduction
An excess of weight including obesity have reached epidemic rates in all age groups, both overweight children and adolescents in developed and developing countries. It is notable that overweight children and adolescents have a higher likelihood of becoming obese adults and to present health-related problems early in life including diabetes, cardiovascular disease (CVD) and dyslipidemias(1,2). Dyslipidemia, characterized by altered circulating levels of blood lipids and/or lipoprotein concentrations, has a genetic or environmental etiology(3,4). Alterations in low-density lipoprotein cholesterol (LDLc), total cholesterol and triglycerides are associated with the development of atherosclerotic plaques, which in turn have a relationship with high fat mass, in particular visceral fat(5,6).
Nowadays, several methods are used to estimate body fat, including the body mass index (BMI)(6), waist circumference (WC)(6), and the sum of skinfold thicknesses(7). An estimation of fat depots are essential to better understand the effects of obesity on the health status, as fat distribution has been described as an important marker of inflammation and is directly linked to changes in cytokine concentrations and the platelet count(8). Additionally, platelets, red blood cells (RBCs) and hemoglobin are associated with cardiorespiratory conditions(9,10), the oxidative metabolism(11), and cardiovascular events(12) in obese and non-obese individuals.
However, almost no studies have been conducted to describe any possible associations between body fat and hematological variables and so this topic is poorly discussed in the current literature. This study aimed to verify the relationship between the blood lipid and hematologic profiles with obesity in adolescents beginning multidisciplinary weight loss therapy.
Methods
This cross-sectional study was conducted with 85 obese adolescents (51 girls and 34 boys) seeking weight loss treatment in the Outpatient Clinic Multidisciplinary Obesity Intervention Program at the Universidade de Pernambuco (UPE), Brazil in 2011. All adolescents had BMI > 95th percentile(13), were aged from 12-19 years old and were in pubertal stage 3 or 4 according to the Tanner scale(14,15). Exclusion criteria were the chronic use of alcohol, smoking, metabolic diseases, continuous use of anti-inflammatory drugs and having infectious or allergic diseases at the time of blood collection. The study was formally approved by the Research Ethics Committee of UPE (#154/09). Informed consent was obtained from all subjects and/or their parents.
Procedures
Subjects wearing light clothing and no shoes were weighed on a FilizolaTM scale to the nearest 0.1 kg. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer (Sanny, model ES 2030). BMI was calculated as body weight divided by height squared. Waist circumference (WC) was measured at the midpoint between the lower ribs and the iliac crest with an inextensible measuring tape with precision to 0.1 cm. All measurements were according to the procedures as previously described by Lohman et al.(16). The skinfold thickness was measured at the triceps, subscapular and calf sites to the nearest 1 mm using calipers (LangeTM).
Blood collection was performed from the cubital vein into a tube containing ethylenediaminetetraacetic acid (EDTA)-K3E (Vacutainer) between 8:00 and 9:00 am after overnight fasting. The RBC, hemoglobin and platelet counts were determined by fluorescence flow cytometry (Automated hematology analyzer -Sysmex XT 1800TM). Total cholesterol (TC), triglycerides (TG) and high-density lipoprotein cholesterol (HDLc) were analyzed using the enzymatic colorimetric method (automatic biochemistry analyzer - Cobas Integra 400 Plus - RocheTM); when TG levels were lower than 400 mg/dL, LDLc was calculated using the Friedewald equation(17).
Statistical analysis
Data were submitted to the Kolmogorov-Smirnov test of normality. Values are shown as means and standard deviation (SD) for variables that met the criteria of normality and non-parametric variables are presented as median (MD), minimum (MIN) and maximum (MAX) values. The Spearman and Pearson correlation coefficients were used to determine possible correlations between variables. Significance was set for p-values < 0.05. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, version 10.0).
Results
Table 1 show s the anthropometric characteristics and body composition of the study sample. No gender differences were observed for BMI, WC or sum of skinfolds, however, boys were taller and with more free fat mass than girls who presented more fat mass. According to the hematologic profile, there were significant differences for the RBC (p-value = 0.000), hemoglobin (p-value = 0.000) and platelet counts (p-value = 0.002) between genders (Table 2).
Table 1.
Body composition and anthropometric characteristics of obese adolescents
| Boys (n = 34) | Girls (n = 51) | ||
| Variable | Mean ± SD or Median (min-max) | Mean ± SD or Median (min-max) | p-value |
| Age (years) | 15.4 ± 1.8 | 15.8 ± 2.0 | 0.364 |
| Height (m) | 1.67 ± 0.06 | 1.59 ± 0.06 | 0.000 |
| Weight (kg) | 97.1 ± 14.6 | 91.9 ± 13.4 | 0.097 |
| BMI (kg/m2) | 34.0 ± 4.5 | 35.5 ± 4.5 | 0.147 |
| SS (mm) | 102.8 ± 19.5 | 108.8 ± 17.7 | 0.154 |
| LM (kg) | 72.3 (45.9-94.8) | 59.0 ± 7.7 | 0.000 |
| FM (kg) | 26.2 (11.8-43.1) | 32.9 ± 9.9 | 0.013 |
| WC (cm) | 99.3 ± 8.6 | 96.5 ± 8.5 | 0.884 |
BMI = body mass index; SS = sum of skinfold; LM = lean mass; FM = fat mass; WC = waist circumference.
Table 2.
Biochemical characteristics of obese adolescents according to gender
| Boys (n = 34) | Girls (n = 51) | ||
| Variable | Mean ± SD or Median (min-max) | Mean ± SD or Median (min-max) | p-value |
| TC (mg/dL) | 157.1 ± 24.4 | 167.4 ± 33.2 | 0.082 |
| HDL (mg/dL) | 36.2 ± 8.0 | 39.1 (18.9-75.5) | 0.167 |
| LDL (mg/dL) | 101.8 ± 26.3 | 105.8 ± 65.1 | 0.497 |
| VLDL (mg/dL) | 18.2 (10.7-3.0) | 17.8 (8.6-78.7) | 0.848 |
| TG (mg/dL) | 89.3 (52.8-365.2) | 88.4 (42.8-393.3) | 0.504 |
| Blood sugar (mg/dL) | 84.8 ± 6.4 | 83.6 ± 8.4 | 0.526 |
| RBC (x 1012/L) | 5.2 ± 0.4 | 4.63 ± 0.33 | 0.000 |
| Hemoglobin (g/dL) | 14.5 ± 1.1 | 12.98 ± 0.62 | 0.000 |
| Platelet (x 109/L) | 292.7 ± 73.5 | 336.0 ± 64.42 | 0.002 |
TC = total cholesterol; HDL = high-density lipoprotein; LDL = low-density lipoprotein; VLDL = very low-density lipoprotein; TG = triglyceride; RBC = red blood cell
Correlations analysis (Figure 1) demonstrated a positive correlation between the WC and RBCs and hemoglobin (p-value = 0.024; r = 0.258), conversely the hemoglobin was negatively correlated to the sum of skinfold (p-value = 0.022; r = -0.262). No associations were found for the other variables.
Figure 1.
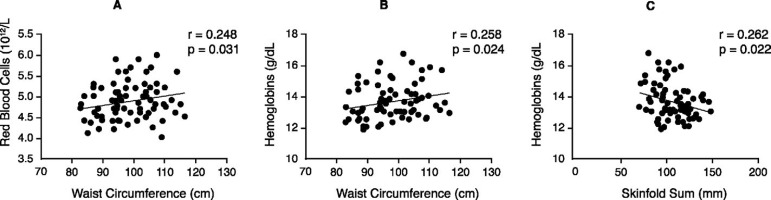
(A) Red blood cells and waist circumference; (B) Hemoglobin and waist circumference; (C) Hemoglobin and Sum of skinfolds
Discussion
It has been postulated that BMI and WC are strong predictors of central body fatness(18). Additionally the increase of body weight and adiposity, in particular central depots in childhood and adolescence, are associated to changes in the metabolic profile and cardiovascular problems, even during adolescence or early adult life(19,20).
The current study shows differences in the hematological profile between boys and girls; these differences can be explained, at least in part, by the higher BMIs seen in girls(21). Besides the effects of adiposity, the low cardiorespiratory fitness, characterized by low oxygen uptake, commonly observed in obese individuals(22), as well as the blood flow rate can contribute to decreases in RBCs and consequently in hemoglobin levels(23) in this population.
As BMI is highly associated with hypertension, hypertriglyceridemia and hypercholesterolemia(20,24), it was expected that the BMI would be associated with the lipid profile. Thus, the absence of any correlation in the present study for this parameter may be related to the characteristics of the sample, as only adolescents without health-related conditions associated to obesity were included in the study; this should be taken into account in the interpretation of the data.
Noteworthy is the fact that, different to Schiavo et al.(25) and Valverde et al.(26), our results did not show any association between BMI and blood lipid levels. This is possibly due to the efficiency of lipoprotein lipase (LpL) in blood removing very low-density lipoprotein (VLDL) and TG.
Conclusion
There is an association between blood lipid levels, hematologic profile and body fat in obese adolescents. These findings are essential to improve the quality of therapeutic interventions not only to achieve weight loss goals, but also to control lipemia and reduce cardiovascular risk in these patients.
Acknowledgments
The authors would like to thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico and the Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco (FACEPE) for financial support. Special thanks to the patients and their parents for the participation in this study.
Funding Statement
Funding Source: All phases of this study were supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPQ
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1.Wang Y, Monteiro CA, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China and Russia. Am J Clin Nutr. 2002;75(6):971–977. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 2.Lissau I, Overpeck MD, Ruan WJ, Due P, Holstein BE, Hediger ML. Health Behaviour in School-aged Children Obesity Working Group. Body mass index and overweight in adolescents in 13 European Countries, Israel, and the United States. Arch Pediatr Adolesc Med. 2004;158(1):27–33. doi: 10.1001/archpedi.158.1.27. [DOI] [PubMed] [Google Scholar]
- 3.Talmud PJ, Waterworth DM. In-vivo and in-vitro nutrient-gene interactions. Curr Opin Lipidol. 2000;11(1):31–36. doi: 10.1097/00041433-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 4.De Franca E, Alves JG, Hutz MH. Apolipoprotein E polymorphism and its association with serum lipid levels in Brazilian children. Hum Biol. 2004;76(2):267–275. [PubMed] [Google Scholar]
- 5.Goran MI, Ball GD, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab. 2003;88(4):1417–1427. doi: 10.1210/jc.2002-021442. [DOI] [PubMed] [Google Scholar]
- 6.Lee S, Bacha F, Arlanian S A. Waist circumference, blood pressure, and lipid components of the metabolic syndrome. J Pediatr. 2006;149(6):809–816. doi: 10.1016/j.jpeds.2006.08.075. [DOI] [PubMed] [Google Scholar]
- 7.Glaner MF. Índice de massa corporal como indicativo da gordura corporal comparado às dobras cutâneas. Rev Bras Med Esporte. 2005;11(4):243–246. [Google Scholar]
- 8.Foschini D, Santos RV, Prado WL, de Piano A, Lofrano MC, Martins AC, et al. Plaqueta e leptina em adolescentes com obesidade. J Pediatr (Rio J) 2008;84(6):516–521. doi: 10.2223/JPED.1845. Comment in: J Pediatr (Rio J). 2009;85(2):179; author reply 179-80. [DOI] [PubMed] [Google Scholar]
- 9.Jones NL. An obsession with CO2. Appl Physiol Nutr Metab. 2008;33(4):641–650. doi: 10.1139/H08-040. [DOI] [PubMed] [Google Scholar]
- 10.Zamai CA, Rodrigues AA, Filocomo M, Braga LE, de Oliveira JF, Zago C. Avaliação da aptidão cardio-respiratória através do teste de caminhada em esforço controlado (TCEC) Conexões: Rev Fac Educ Fís. 2010;8(2):146–158. [Google Scholar]
- 11.Solá E, Vayá A, Martínez M, Moscardó A, Corella D, Santaolarias ML, et al. Erythrocyte membrane phosphatidylserine exposure in obesity. Obesity. 2009;17(2):318–322. doi: 10.1038/oby.2008.499. [DOI] [PubMed] [Google Scholar]
- 12.Asdie RH, Sa'adah, Jazakillah S, Sinorita H. Does insulin resistance correlate with routine blood examination? A review on erythrocytes of obese patients. Acta Med Indones. 2009;41(2):66–69. [PubMed] [Google Scholar]
- 13.Must A, Dallal GE, Dietz WH. Reference data for obesity: 85th and 95th percentiles of body mass index (wt/ht2) and triceps skinfold thickness. Am J Clin Nutr. 1991;53(4):839–846. doi: 10.1093/ajcn/53.4.839. [DOI] [PubMed] [Google Scholar]
- 14.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: 1991. Abridged edition. [Google Scholar]
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifugue. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 18.Guedes DP, Guedes JE, Barbosa DS, Oliveira JA, Stanganelli LC. Fatores de risco cardiovasculares em adolescentes: Indicadores biológicos e comportamentais. Arq Bras Cardiol. 2006;86(6):439–450. doi: 10.1590/s0066-782x2006000600006. [DOI] [PubMed] [Google Scholar]
- 19.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 20.Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thickness to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr. 1999;69(2):308–317. doi: 10.1093/ajcn/69.2.308. [DOI] [PubMed] [Google Scholar]
- 21.Samocha-Bonet D, Justo D, Rogowski O, Saar N, Abu-Abeid S, Shenkerman G, et al. Platelet counts and platelet activation markers in obese subjects. Mediators Inflamm. 2008;2008:834153. doi: 10.1155/2008/834153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leite N, Milano GE, Cieslak F, Stefanelo JM, Radominski RB. Aptidão cardiorrespiratória, perfil lipídico e metabólico em adolescentes obesos e não-obesos. Rev Bras Educ Fís Esporte. 2009;23(3):275–282. [Google Scholar]
- 23.Cazzola R, Rondanelli M, Russo-Volpe S, Ferrari E, Cestaro B. Decreased membrane fluidity and altered susceptibility to peroxidation and lipid composition in overweight and obese female erythrocytes. J Lipid Res. 2004;45(10):1846–1851. doi: 10.1194/jlr.M300509-JLR200. [DOI] [PubMed] [Google Scholar]
- 24.Mikkola I, Keinanen-Kiukaanniemi S, Laakso M, Jokelainen J, Harkonen P, Meyer-Rochowf VB, et al. Metabolic syndrome in connection with BMI in young Finnish male adults. Diab Res Clin Pract. 2007;76(3):404–409. doi: 10.1016/j.diabres.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 25.Shiavo M, Lunardelli A, Oliveira JR. Influência da dieta na concentração sérica de triglicerídeos. J Bras Patol Med Lab. 2003;39(4):283–288. [Google Scholar]
- 26.Valverde MA, Vítolo MR, Patin RV, Escrivão MA, Oliveira FL, Ancona-Lopez F. [Changes in lipid profile in obese children and adolescents] Arch Latinoam Nutr. 1999;49(4):338–343. [PubMed] [Google Scholar]


